3
Disability Determination Process for Veterans with Traumatic Brain Injury
The Department of Veterans Affairs (VA) requested that the committee review the adjudication process by which impairments that result from traumatic brain injury (TBI) are assessed for awarding disability compensation. The committee specifically was asked to assess the adequacy of the tools and protocols used by the VA to provide examinations and also to review the credentials and training of the providers who perform examinations. Chapter 3 begins by defining disability and providing an overview of the VA’s disability determination process for the residuals of TBI (i.e., those conditions which result from sustaining a TBI) from the submission of the claim through the appeals process. The chapter then focuses on the tools and protocols used in evaluating the residuals of TBI as well as the credentials and training required in the clinical assessment and disability rating of TBI residuals. Finally, the chapter describes the VA’s efforts at quality assurance for the adjudication process.
DISABILITY AND DISABILITY COMPENSATION
Disability compensation is a monetary benefit awarded to veterans for one or more injuries or illnesses that the VA determines were “service connected,” that is, were incurred during active military service (VA, 2018a).1 Each disabling, service-connected condition is assigned a rating, ranging from 0 to 100 percent disability, in 10 percent increments. The degree of disability for a given disabling condition depends on a number of factors, including the diagnosis (coded according to the Veterans Affairs Schedule for Rating Disabilities [VASRD], which provides criteria for translating medical information into a disability rating) associated with the disability and a variety of functional measures. A veteran who has more than one service-connected disability receives a rating for each condition, and the VA then applies a formula to determine the overall disability rating (VA, 2018a). Finally, the overall disability rating is mapped to a benefits table (see Chapter 1, Table 1-1), which shows the monthly amount paid by VA to the veteran commensurate with the degree of disability and the number of eligible dependents (VA, 2015a).
___________________
1 In addition to monetary benefits, veterans may be eligible for other benefits, including health care, housing, and insurance benefits. The focus of this chapter is monetary benefits.
The VA regards disability as an intersection of service connection, diagnosis, and function, and the compensation decision is for the most part not associated with the veteran’s ability to work.2 This can be contrasted with how the Social Security Administration (SSA) views disability. SSA, another federal agency that provides disability benefits, views disability compensation as a binary decision where the compensation is awarded based on the claimant’s inability to work or perform “substantial gainful activity” by reason of a medical impairment (SSA, 2017). While SSA awards disability compensation to individuals who cannot work, the VA awards disability compensation to people who sustain injuries from military service, regardless of their ability to work. Veterans may also receive disability benefits from SSA while receiving benefits from the VA, although eligibility for one does not necessarily confer eligibility for the other (VA Law, 2018).
In fiscal year 2017, 155,321 veterans received compensation benefits for residuals of TBI. Table 3-1 shows the number of unique veterans who received VA disability compensation benefits for residuals of TBI, displayed by their overall disability ratings, inclusive of TBI and any other non-TBI rated conditions.
TABLE 3-1 Overall Disability Ratings for Veterans with a Rating for Residuals of Traumatic Brain Injury
| Overall Disability Rating | FY 2017 | FY 2018 to date (as of July 2018) |
|---|---|---|
| 0% | 39,494 | 41,314 |
| 10% | 55,648 | 56,999 |
| 20% | 485 | 465 |
| 30% | 8,779 | 9,168 |
| 40% | 20,757 | 21,676 |
| 50% | 8,113 | 9,371 |
| 60% | 163 | 159 |
| 70% | 15,698 | 18,077 |
| 80% | 143 | 137 |
| 90% | 18 | 18 |
| 100% | 6,023 | 6,654 |
| Total | 155,321 | 164,038 |
NOTE: Fiscal year (FY) to date includes data from October 1, 2017, to June 30, 2018. Those with 0% were evaluated but determined to have no disability.
SOURCE: Communication with Veterans Benefits Administration, July 2018.
DEPARTMENT OF VETERANS AFFAIRS DISABILITY DETERMINATION PROCESS FOR RESIDUALS OF TRAUMATIC BRAIN INJURY
The adjudication process for VA disability compensation involves the following key stakeholders: the veteran, the Veterans Health Administration (VHA), the Veterans Benefits Administration (VBA), and staff offices that work with veterans on appeals; however, not all
___________________
2 An exception is that for certain disabilities a veteran receiving a 100 percent disability rating cannot work full time or make over a certain income (usually the federal poverty line) (VA Law, 2018).
cases involve all of those stakeholders. This section describes the process by which the stakeholders work together to adjudicate claims for residuals of TBI. The overall adjudication process is not unique to residuals of TBI claims, but there are specific tools and protocols that are unique to those claims. Figure 3-1 provides a simplified version of the adjudication process:
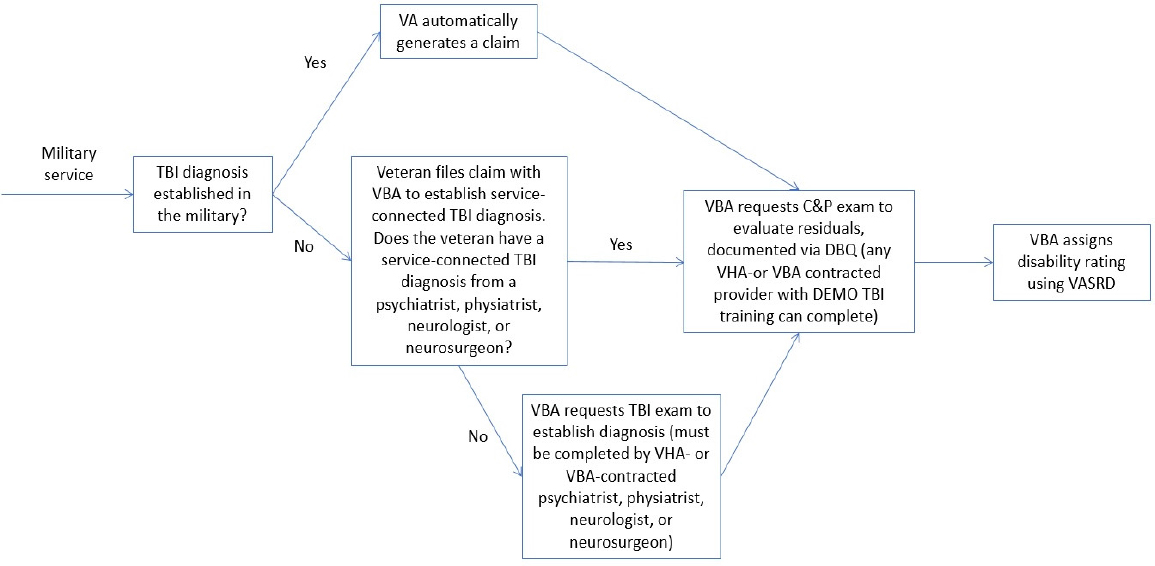
NOTES: A veteran may file for an appeal at any step in the process (e.g., service connection, initial decision, a decision for an increased rating). C&P = compensation and pension; DBQ = Disability Benefits Questionnaire; DEMO = Disability Examination Management Office; TBI = traumatic brain injury; VA = Department of Veterans Affairs; VASRD = Veterans Affairs Schedule for Rating Disabilities; VBA = Veterans Benefits Administration; VHA = Veterans Health Administration.
Broadly speaking, the VA disability determination process for residuals of TBI involves the following steps, as described in the VA’s Compensation and Pension Manual, M21 (see Appendix I for M21 Table of Contents) (VA, 2018b):
- If the service member is being medically discharged from the military because of residuals of TBI that render him or her unfit for duty, the disability evaluation process begins while the service member is still serving in the military. At any point after leaving the military, a veteran may file a claim with the VA for a disability. Disability claims can be filed through the VA’s eBenefits, in person with a veterans service organization (VSO), or with a VA representative at a military installation (health.mil, 2018).
- VBA receives the claim. If VBA receives a “substantially complete application,” meaning it includes sufficient information to verify the veteran’s service and claimed medical condition, it will begin to process the claim. If VBA does not receive a substantially complete application, VBA must give the claimant written notice of the evidence necessary to substantiate the claim. It must also inform the claimant whether
-
the VA or the claimant is responsible for obtaining that evidence. A veteran submitting a claim for residuals of TBI must first establish a TBI diagnosis by a psychiatrist, physiatrist, neurologist, or neurosurgeon if the veteran did not receive a diagnosis while on active duty (VA, 2018b).
- Once the TBI diagnosis has been established, the residuals of TBI must be assessed. That may happen in a number of ways. VBA might accept a medical report from a private physician if it determines that report is “adequate for rating purposes.”3 However, in most cases, standard medical examinations are not “adequate for rating purposes” because the diagnostic and treatment information obtained in a standard medical examination does not cover functional impacts of the impairment. In those cases, VBA orders a compensation and pension (C&P) examination performed by a VHA clinician or a VBA clinician contractor. The C&P examiner evaluates the degree of impairment, functional limitation, and disability, which is recorded in the Disability Benefits Questionnaire (DBQ), which is unique to residuals of TBI (see Appendix D).
- The C&P examination results are sent to VBA via the C&P record interchange. A VBA rating specialist determines the percentage rating by comparing medical evidence recorded in the DBQ for residuals of TBI with criteria in the VASRD for residuals of TBI, in addition to other information such as the veteran’s medical and service records.
- The veteran begins receiving disability benefits. The disability rating may be adjusted as the veteran’s condition worsens or improves over time. That adjustment requires reevaluation of the veteran’s condition(s). Veterans receiving benefits for residuals of TBI may request to be reevaluated at any time.
- If the veteran does not agree with the rating decision, he or she can submit an appeal to have the case reviewed by the Board of Veterans Appeals. The appeals process gathers and develops new evidence and re-reviews the case to issue a final decision on behalf of the VA secretary for disability compensation claims (and other veterans’ benefits).
In December 2018, the average reported length of time for the VA to process disability claims was 110 days (VA, 2018c).
THE RATING PROCESS
VBA is the administration within the VA that makes the decision about the rating, with information gathered from the veteran’s records and, often, with health information established from VHA or VBA-contracted clinicians. VBA staff work across 57 regional offices to process claims. Claims processors are veterans service representatives (VSRs), who gather the evidence needed to determine entitlement, and rating veterans service representatives (RVSRs), who decide rating percentages. In fiscal year (FY) 2017, 50,155 veterans submitted claims for TBI: 38,659 were filed for service connection, while 11,496 were filed for an increase in benefits (communication with VBA, July 2018). In 2018 the maximum award was $2,973.86 per month for 100 percent disability rating for a veteran alone, and $3,261.10 for 100 percent disability rating for a veteran with a spouse and child (Veterans Aid Benefit, 2018).
The VBA’s predetermination team and the rating team work together to make a rating decision. Those teams include VSRs, who gather the evidence needed to determine entitlement,
___________________
3 38 CFR 3.326.
including requesting medical exams, reviewing information from VHA, and gathering other data required to make a claim decision, and RVSRs, who determine whether the condition is service connected, determine the disability rating, and assign an effective date. The predetermination team’s job of developing the evidence necessary to make a rating decision is often time-consuming, as multiple requests might be necessary to obtain all the needed information. The predetermination team sets deadlines for receipt of requested information and determines whether VHA should complete a C&P exam (IOM, 2007).
The rating team makes decisions on claims that require the consideration of medical evidence. In addition to medical records, VSRs retrieve the military personnel file.4 A routing tool determines whether the examination goes to a VA medical center clinician or a VBA-contracted clinician, based on the veteran’s zip code. The determination is made based on the distance and availability of VHA clinicians. If there are no VHA clinicians available within a month of the scheduling goal, the veteran may see a VBA contractor. However, VA does set a limit for the number of exams performed by contractors (personal communication with VBA, August 6, 2018).
RVSRs take the information from the cases determined by the VSR to be “ready to rate” and make a decision on service connection, percent disability, the need for reexamination, and the competency of veterans and dependents for self-support. The information from the DBQ is entered into the Veteran Benefits Management System evaluation builder, which populates all the information inputted by the rater. Then the RVSR assigns an effective date (the date the veteran will begin to receive benefits). Only RVSRs or decision review officers (DROs) may prepare complex medical opinion requests, including conflicting medical diagnoses and questions concerning the credibility of evidence presented to the examiner. Journey-level VSRs who have completed training specified by the central office may prepare basic medical opinion requests without RVSR or DRO review (VA, 2018b).
It should be noted that in determining a disability percentage for residuals of traumatic brain injury, an RVSR might consider information from more than one DBQ. The order in which DBQs are completed should be taken into consideration, given the likelihood that additional DBQs will be required and answers to questions on one might be required in another. For example, because the posttraumatic stress disorder (PTSD) DBQ requires information from the TBI DBQ, the TBI DBQ should be completed before the PTSD DBQ. A protocol should be implemented requiring the TBI DBQ to be conducted prior to the PTSD DBQ. (See Appendixes D and J for the TBI and PTSD DBQs, respectively.)
THE APPEALS PROCESS
Veterans have the right to appeal any benefits decision made by VBA. Once VBA has made a decision on the veteran’s claim (whether the initial decision, a decision for an increased rating, or any other decision), the veteran has 1 year to appeal some or all of the decision, including, but not limited to, entitlement to service connection, the percentage of evaluation assigned, and the effective date (see Notice of Disagreement, Appendix K). The appeals process is a multistage, nonlinear process set in law that has evolved over decades, with a continuous
___________________
4 Prior to leaving the military, all service members undergo a medical examination that is used by both the Department of Defense (DoD) and the VA called the separation health assessment (VA, 2018b). The examination documents and assesses the service member’s medical history, medical concerns identified during his or her service career, and current health status.
open record which allows the submission of new evidence at any time. Each submission of evidence requires a new cycle of review and decision making. The appeals process is described in Box 3-1 below.
There are two levels of appeals. The first level of appeal is heard by the Board of Veterans’ Appeals (BVA). The BVA’s mission is to conduct hearings and decide appeals in a timely manner.5 To initiate an appeal, the veteran must submit a Notice of Disagreement (see Appendix K). Additionally, the veteran must submit VA Form 9, which is the official appeal (see Appendix L). If, after the decision is made, the veteran still disagrees with the BVA’s decision, then the second level of appeal available to the veteran is the U.S. Court of Appeals for Veterans Claims. The veteran must submit a notice of appeal within 120 days of the BVA decision (VA, 2018b). Once the appeal has been docketed, the court clerk will send a notice of docketing to all parties advising them of the date the clerk received the notice of appeal. The clerk also notes what will be required of both the veteran and the VA secretary (VA, 2015b). The court is a national court of record and has exclusive jurisdiction to provide judicial review of final decisions by the BVA. The court provides the highest level of appeals within the VA.
The appeals process is complex and takes a considerable amount of time. In FY 2017, the BVA issued 52,661 decisions. For those appeals that were resolved by the BVA, veterans waited on average 7 years from the date that they initiated their appeal until resolution (BVA, 2017).6
THE DISABILITY BENEFITS QUESTIONNAIRE AND A SCHEDULE FOR RATING DISABILITIES FOR RESIDUALS OF TBI
The committee was tasked with making a determination of the adequacy of the tools and protocols used by the VA to provide TBI examinations and to make recommendations for
___________________
5 38 United States Code (U.S.C.) § 7101 (a)
6 See figure 1 in GAO’s 2017 report Additional Planning Would Enhance Efforts to Improve the Timeliness of Appeals Decisions for a detailed appeals timeline: https://www.gao.gov/assets/690/683637.pdf (accessed March 21, 2019).
legislative or administrative action for improving the adjudication of veterans’ claims for all impairments arising from TBI. While Chapter 2 described the protocols for diagnosing and assessing TBI, this section will describe the tools that VHA and VBA use for evaluating residuals of TBI (i.e., the DBQ and the VASRD). The clinician using the DBQ will evaluate the veteran’s condition, and the RVSR will determine a rating using the VASRD.7 The DBQs were developed to assist the VBA in addressing TBI rating criteria (correspondence with VHA, 2018); therefore, the criteria in the DBQ have been developed to mirror those in the VASRD.
As previously discussed, in order to assess the level of impairment resulting from residuals of TBI, VHA clinicians and VBA-contracted clinicians use the DBQ, a form that elicits the medical information needed to make claims. The DBQ provides a standardized report format for medical examinations and opinions to guide the documentation of C&P exams. The C&P examiners use DBQs to provide medical information that is directly relevant to determining a disability rating, which enables the VA’s rating specialists, the RVSRs, to have the information they need to start processing a claim by using the VASRD.
The disability rating for residuals of TBI derives from the levels of impairment contained in the “assessment of cognitive impairment and other residuals of TBI” section of the DBQ for residuals of TBI. In the VASRD, the disability rating for residuals of TBI can only take on five values: 0 percent, 10 percent, 40 percent, 70 percent, or 100 percent. If the outcome of the DBQ indicates that the veteran is completely impaired in one or more of the 10 facets on the DBQ, VBA awards the veteran a 100 percent disability. If no facet is evaluated as total, the overall percentage is based on the highest facet as follows: 0 = 0 percent; 1 = 10 percent; 2 = 40 percent; and 3 = 70 percent. For example, a veteran might be awarded 70 percent disability if 3 is the highest level of evaluation among the facets evaluated (see Appendix E).8
Comments on the 10 Facets
The committee reviewed the “assessment of cognitive impairment and other residuals of TBI” section of the DBQ as well as comments on the 10 facets that are evaluated in that section (see Appendix D for the DBQ). In the following subsections the committee comments on those facets and on the difficulty that a rater may have with providing a rating on the VASRD because of the lack of flexibility in applying the rating.
Memory, Attention, Concentration, and Executive Functions
Section II of the DBQ, “assessment of cognitive impairment and other residuals of TBI,” identifies deficits in memory, attention, concentration, and executive functions that are commonly observed following TBI (Rosenthal et al., 1999). The definition of executive function used in the rating schedule emphasizes the cognitively based functions, such as planning and organization, while the difficulties with the regulation of emotions and behavior often experienced following TBI are not evaluated in the VASRD under residuals of TBI. Difficulties with executive functions following TBI are wide ranging and include problems with information processing, reasoning and problem solving, planning and organization, goal setting, self-
___________________
7 TBI is rated in the VASRD under 38 CFR 4.124a, Diagnostic Code 8045—residuals of TBI (see Appendix D).
8 Overall disability ratings for multiple disabilities are not additive, but are calculated according to a combined ratings table and rounded to the nearest ten. As an example, for a veteran who is awarded a rating of 40 percent disability for residuals of TBI and 20 percent for a second condition (e.g., back pain), the combined rating according to the table is 52 percent, which the VA rounds down to 50 percent. The table can be found at VA (2018c).
awareness, and mental flexibility. Executive function deficits can be observed in persons with TBI of any severity level and might be short-lived or chronic (Wood and Worthington, 2017).
The committee notes that the DBQ specifies that cognitive impairment includes memory, attention, concentration, or executive functioning. Ratings of impairment greater than the mild level rely on objective evidence in testing. Evaluators should be aware, however, that appropriate tests for evaluating a cognitive or executive function can take different forms (e.g., from an evaluation of functional problem solving in the kitchen by an occupational therapist to a full neuropsychologic test battery).
Furthermore, memory, attention, concentration, and executive function are grouped into one facet, leaving the VHA or VBA clinician to choose one level of functional status for those four areas (see Appendix D TBI DBQ). That assumes that each of these four functions has been affected to the same degree, which might not be the case. The DBQ does not provide guidance on how a clinician should address different levels of impairments for the four functions evaluated in this facet.
Judgment
Judgment, which includes decision making, is rated separately on the DBQ from the first facet of memory, attention, concentration, and executive functions. The committee found that to be appropriate, given the importance of judgment for independent functioning. The decisionmaking process includes identifying alternative choices, weighing the pros and cons of the choices, understanding the outcomes of decisions, and making reasonable choices. Judgment and decision making can remain impaired for years following TBI exposure and can have a substantial impact on an individual’s successful return to community participation (Agoston and Kamnaksh, 2015; Wood and Worthington, 2017).
The DBQ requires an evaluation of judgment based on the complexity or novelty of decision making and the frequency of difficulty with decision making. However, the latter criterion can be problematic when a poor decision made infrequently has serious consequences. For example, an individual might decide to forego taking a medication to prevent seizures on a day that she or he wants to drink alcohol. While the individual is heeding a recommendation not to mix alcohol with the medication, the individual has inappropriately weighed the risk of a seizure against the perceived pros of drinking alcohol. On the continuum of complexity, the decision to take or forego the medication and to consume or not consume the alcohol falls in the moderate range; however, the consequences of making the wrong decision even once can be serious. The physician filling out the DBQ must check the box on the frequency of the occurrence, but a more refined DBQ (and the VASRD) might take into account both the complexity of the decision and the consequences of poor decision making, rather than the frequency with which a poor decision is observed.
Social Interaction
Social interactions might deteriorate following a TBI. For example, individuals might experience difficulties using the historic and current context to fully comprehend meaning in a conversation, might have difficulties with turn-taking and tending to dominate the interaction, or might have trouble with the violation of social norms and maintaining boundaries (Angeleri et al., 2008; Rowley et al., 2017). Many individuals have problems perceiving and reading affective cues in themselves and others (Bornhofen and McDonald, 2008; Neumann et al., 2014). Individuals with TBI might not be aware of how their behavior is affecting social interaction and,
as a result, fail to modify their behavior (Prigatano, 2009; Sherer et al., 1998). Impaired social interaction can lead to negative outcomes, such as social isolation and job loss.
On the DBQ, social interaction is evaluated with regard to the frequency in which it is inappropriate. While frequency is an important consideration, the impact of the social interaction deficits should also be considered. For example, individuals who fail to take turns in conversations can quickly find themselves without a conversational partner after only a couple of interactions.
Orientation
Disorientation following TBI is normally considered within the context of posttraumatic amnesia. During the acute stage of recovery, individuals might not be fully aware of their location (place orientation), the passage of time (time orientation), or their situation, and in rare circumstances they cannot identify themselves (person orientation). The extent to which the individual is oriented to time, place, situation, and person is used an indicator of progress in recovery from posttraumatic amnesia (McKinlay and Watkins, 1999). However, it is also possible that individuals might become disoriented in certain circumstances, even months or years post-injury. While even persons without TBI might temporarily lose track of time during prolonged circumstances without scheduled activities (e.g., vacation), the difference is that an individual with TBI might have greater difficulty reorienting in those circumstances. Periods of disorientation might also be a signal of underlying deterioration due to aging, or they might be a function of multiple factors common to TBI, such as a disrupted sleep-wake cycle, medications and their interactions, or stress. Persons with comorbid PTSD may experience dissociation and its associated disorientation (McKinnon et al., 2016).
The DBQ assesses orientation with regard to person, time, place, and situation in accordance with the four areas that are impaired and how frequently they are impaired. However, while not being able to identify oneself or one’s current circumstances is the least frequent outcome of the four, it is also potentially the most concerning, as it can have a catastrophic impact on overall function.
Motor Activity
The committee noted that the motor facet is limited to apraxia, the inability to execute skilled actions, which can result from multiple types of brain lesions and can affect multiple systems, including speech and limb movements (Worthington, 2016). The assessment of this facet is more specifically defined as slowed or decreased motor activity due to apraxia. Due to the nature of the impairments, individuals with apraxia may have functional limitations in day-to-day function that are difficult to assess on clinical exam (Worthington, 2016).
Visual–Spatial Orientation
Deficits in visual–spatial orientation can affect route finding and the ability to work with three-dimensional objects. Left neglect or inattention can cause an individual to run into doorways or not be aware of dangerous situations if they only occur on the person’s left side. Veterans and other persons with mild TBI have been found to have deficits in spatial attention that have affected their ability to walk around in the community (Catena et al., 2009; Kearns et al., 2015). The TBI DBQ focuses primarily on a person’s ability to find his or her way in familiar and unfamiliar surroundings and to use assistive devices such as GPS, a global positioning system. At the most severe level of impairment, an individual may not be able to identify his or
her body parts (which can be affected by left neglect) or identify spatial relationships between two objects. The DBQ would more accurately reflect the full spectrum of deficits if each level under visual–spatial orientation also included additional visual–spatial problems, such as left inattention.
Subjective Symptoms
The DBQ provides examples of subjective symptoms that may be considered based on their impact on work, the instrumental activities of daily living, or family or other close relationships. Example symptoms include headaches, anxiety, dizziness, tinnitus, insomnia, hypersensitivity to light or sound, marked fatigability, and blurred or double vision. The physical and sensory sequelae of TBI, including concussion (Junn et al., 2015), depend on such factors as the brain region involved (e.g., olfactory tracts, motor cortex, visual association areas, cerebellum) and can affect many organ systems. There are conditions that may be subjective symptoms attributable to TBI that are not listed in the facets on the DBQ, such as olfactory changes (Bratt et al., 2018) or postural instability or gait disturbance (Meadows and Williams, 2009); however, they are addressed in Section III of the DBQ and require additional questionnaires to be completed.
Neurobehavioral Effects
After TBI, individuals can have numerous difficulties in behavioral regulation, including impulsivity, poor initiation, disinhibition, anosognosia (impaired self-awareness), irritability, aggression, inappropriate sexual behavior, apathy, and difficulties with emotional control (Wood and Worthington, 2017; Wortzel and Arciniegas, 2014). Difficulties with behavioral and emotional regulation are often poorly understood by others, and there is a tendency to attribute the maladaptive behavior to the person or their “personality” rather than recognizing the brain injury as the source (or, at a minimum, as an exacerbating factor). The misattribution creates a barrier to the development of accommodations and strategies in the environment designed to maximize more adaptive behavior. Individuals who have difficulties with activation and initiation may be viewed as “lazy,” while those who are disinhibited may be perceived as “rude” and “obnoxious.” Unfortunately, employers and the general public are often not informed about TBI and its effects and are thus likely to react quickly to single significant incidents by terminating employment, avoiding future interactions, or barring the individual from public places.
The DBQ acknowledges that some deficits in neurobehavioral regulation can have a more serious impact than others. However, the rating of the severity of this effect focuses on the frequency in which the behavior interferes with work or social interactions. Given that a single occurrence of some behaviors (e.g., physical aggression, inappropriate touching) could lead to immediate termination, basing the ratings on frequency does not adequately capture the severity of the neurobehavioral deficits. The criteria could be improved by focusing directly on the extent of the behavior’s impact on work or social interactions. For example: Is the individual able to self-monitor and apply compensatory strategies to avoid affecting interactions? Does the behavior disrupt an interaction to the extent that the interaction ceases whenever the behavior occurs? Does the behavior result in formal or informal sanctions or restrictions?
Communication
Communication impairments after TBI may be secondary to aphasia (primary language impairment) or manifest themselves through an interaction with other cognitive impairments that decrease the effectiveness of communication such as an inability to attend to conversation or difficulty with appropriate social interactions associated with communication (Togher et al., 2014). The DBQ groups together comprehension and expression under the communication facet and categorizes levels of difficulty based on the communication of complex ideas and basic needs and the frequency with which the veteran experiences communication limitations. However, an inability to communicate, even when infrequent, implies a more severe disabling effect. Thus, the DBQ should take into account functional impact in addition to frequency.
Consciousness
The committee notes that this facet is a dichotomous yes/no indication of whether the veteran manifests impaired arousal. While it is appropriate that a vegetative state, a minimally responsive state, or coma are equated with total disability, there are manifestations of impaired arousal between “normal” and “persistent altered state of consciousness,” and those disorders of consciousness should be rated.
Cumulative Effects
As previously described, the facets diagnosed by a VHA clinician or VBA clinician contractor on the DBQ are translated by a non-clinician to provide a disability percentage of 0, 10 percent, 40 percent, 70 percent, or 100 percent, and the facet with the highest level of impairment is translated into the final rating. The committee found this approach to be problematic as it does not allow for cumulative effects of multiple residuals. For example, eight facets rated as mild might carry more consequences than a single facet rated moderate.
Other Comments
The TBI DBQ has a section for additional residuals, other findings, diagnostic testing, functional impacts, and remarks from the clinician. It is not clear how information from that section would be incorporated into the rating decision.
Since the DBQ mirrors the VASRD, the same issues described for facets of TBI on the DBQ hold for the VASRD.
The committee recommends that the Department of Veterans Affairs convene experts from both the Veterans Health Administration and the Veterans Benefits Administration, including clinicians who diagnose and assess residuals of traumatic brain injury (TBI), to regularly update the Veterans Affairs Schedule for Rating Disabilities and the Disability Benefits Questionnaire for residuals of TBI to better reflect the current state of medical knowledge.
Additional Aspects of TBI Not Adequately Addressed in the DBQ
In the committee’s review of the residuals of the TBI DBQ, the committee found additional important residuals that were not included. In particular, injuries to cervical muscles, ligaments, nerve roots, vertebrae, and intervertebral discs are common contributors to post-TBI headache as well as to vestibular dysfunction (Morin et al., 2016). Thus, the committee believes
that the VA should add the residuals in the Neck (Cervical Spine) Conditions DBQ to the list of residuals attributable to TBI in Section III of the DBQ Initial Evaluation of Residuals of Traumatic Brain Injury (see Appendix D for TBI DBQ and Appendix M for Neck DBQ).
In addition, there are three important residuals of TBI that are not adequately covered by any of the existing DBQs: insomnia, vestibular dysfunction, and near vision dysfunction (near point accommodative and convergence insufficiency).
Insomnia
Isolated questions related to insomnia and sleep disruption can be found on four DBQs (mental disorders, chronic fatigue syndrome, PTSD, and sleep apnea), but no single DBQ combines them all in a way that captures the full extent of disability associated with post-TBI sleep disruption. Sleep disruption occurs commonly after TBI, contributing to fatigue, cognitive dysfunction, and disrupted mood (Viola-Saltzman and Watson, 2012).
Vestibular Dysfunction
Isolated questions and physical exam elements related to vestibular dysfunction can be found on two DBQs (cranial nerves diseases and ear conditions), but no single DBQ combines them in a way that captures the full extent of disability associated with post-TBI vestibular dysfunction. Such dysfunction is typically a mix of both peripheral (ear and vestibulocochlear nerves) and central (vestibulo-spinal and vestibulo-ocular) vestibular structure disruption. Vestibular dysfunction occurs commonly after TBI, producing symptoms related to (1) altered postural stability (imbalance and abnormal gait), (2) altered oculomotor function (reduced dynamic visual acuity, dizziness with head movement, dizziness with movement of objects in visual field), and (3) reduced concentration or “fogginess” when in motion (Akin et al., 2017). Vestibular dysfunction may also contribute to altered mood, particularly anxiety (Franke et al., 2012).
Near-Vision Dysfunction
Although the eye conditions DBQ provides questions related to diplopia, no existing DBQ provides questions or physical exam elements intended to capture the full extent of disability associated with near-point accommodative and convergence insufficiency. These near-vision problems occur commonly after TBI and can result in not only diplopia but also blurred vision, headache, nausea, and an inability to maintain focus while reading and doing other close-range visual activities (Brahm et al., 2009; Thiagarajan et al., 2011).
The committee recommends that the Department of Veterans Affairs add insomnia, vestibular dysfunction, and near-vision dysfunction to the Disability Benefits Questionnaire for residuals of traumatic brain injury.
CREDENTIALS AND TRAINING REQUIRED IN EVALUATING RESIDUALS OF TBI FOR VA DISABILITY COMPENSATION
Examinations of disabling conditions of TBI, also referred to by the VA as residuals of TBI, may be completed by generalists or by specialists appropriate to the residual being examined—for example, by a psychiatrist or psychologist for mental illness or by an
ophthalmologist for visual disorder—who have completed the Disability Examination Management Office (DEMO) TBI training module in the Talent Management System (VA, 2016a).
Training Required for Providers Diagnosing TBI
In addition to the requirement that a provider diagnosing TBI be board certified in one of four specialties noted above, providers must complete Web-based training through the VA’s Talent Management System (VA, 2016b). The training includes the following modules (correspondence with VHA Office of Disability and Medical Assessment [DMA], April 30, 2018):
- VHI Veterans Health Initiative Traumatic Brain Injury Independent Study (VA 8339) This is a one-time mandatory training for all clinical providers treating TBI patients and highly encouraged for all VHA providers. The independent study presents an overview of TBI issues that primary care practitioners might encounter when providing care to veterans and active-duty personnel. It provides a review of the diagnostic criteria for TBI and of management principles.
- Traumatic Brain Injury Module 1: Diagnosing Combat-Related Concussion (VA 27851) This is the first module of a three-part video series on traumatic brain injury. The module is focused on diagnosing combat-related concussion. A pre- and post-test are provided to document knowledge transfer. The VA’s stated purpose for this module is to provide education in the foundations of TBI and in the nuances of diagnosing combat-related TBI.
- Traumatic Brain Injury Module 2: Expected Outcomes from Combat-Related Concussion (VA 27852) The second module of a three-part video series on TBI is concentrated on expected outcomes from combat-related concussion. A pre- and post-test are provided to document knowledge transfer. The VA’s stated purpose for the module is to provide education on the outcomes of combat-related TBI.
- Traumatic Brain Injury Module 3: Treatment of Combat-Related Concussion (VA 27853) The third module of the three-part series focuses on the treatment of combat-related concussions. A pre- and post-test are provided to document knowledge transfer. The VA’s stated purpose for this module is to provide education on treatment recommendations for combat-related TBI.
- VA/DoD CPG Management of Concussion–Mild Traumatic Brain Injury—Summary Guide (VA 5440) This publication contains a summary of the Clinical Practice Guideline (CPG) for Management of Concussion/Mild Traumatic Brain Injury. The guideline was developed by a group of expert VA and Department of Defense (DoD) clinicians under the auspices of the VA/DoD Evidence-Based Clinical Practice Work Group.
Those training modules for C&P examiners are provided by VHA’s Office of Disability and Medical Assessment (DMA). The committee is not aware of a schedule to review or update the DMA training. Updates are based on regulatory changes to the TBI exam or the C&P process. On average, the courses are updated every 5 years, but if there are significant changes that affect the examination process, updates may be undertaken sooner. Generally, VHA C&P
disability examination courses are overview courses that assist clinicians with a basic understanding of how to conduct specific examinations based on the legal and administrative requirements for conducting the examination (correspondence with VHA DMA, April 30, 2018).
Thus, the VA provides additional, required training to the physicians who are currently allowed to diagnose TBI. And, as noted in Chapter 2, the committee recommends that the VA allow other health care professionals with TBI training and experience to make TBI diagnoses. The committee believes that it is the training and experience in diagnosing and treating TBI over time, not necessarily the medical specialty, that render a health care specialist capable of an accurate TBI diagnosis.
Training Required for Providers Assessing Residuals of TBI
The assessments for the residuals of the TBI (using the TBI DBQ) may be completed by a generalist clinician (e.g., a physician, physician assistant or nurse practitioner, psychologist) or a specialist appropriate to the residual being examined (e.g., a psychiatrist or psychologist for mental illness or an ophthalmologist for vision disorders) who has completed the DEMO TBI training module. The DEMO training module takes approximately 1 hour to complete (VA, 2016c). At the completion of the course, the clinician takes a 21 multiple-choice question examination.
The objectives of the DEMO course are to:
- Define the criteria to diagnose TBI;
- Describe best practices for activities performed prior to conducting a C&P TBI examination;
- Apply best practices for opening, conducting, and closing a C&P TBI examination, as well as for guiding the veteran through the interview and examination process;
- Identify signs and symptoms of TBI sequelae;
- Explain when additional testing is indicated;
- Incorporate the interpretation of diagnostic tests into the C&P report;
- Apply best practices for using the DBQ or other documentation protocol to document a C&P TBI examination; and
- Learn through case studies.
The DEMO module defines TBI as any of the following occurring after a traumatic event:
- Memory loss for events immediately before or after injury (posttraumatic amnesia)
- Altered mental state at the time of injury, such as confusion, disorientation, slow thinking
- Neurologic deficits, such as weakness, balance disturbance, praxis, paresis/plegia, change in vision, other sensory alterations, and aphasia
- Intracranial lesion
The committee found the information provided in the training materials for those who diagnose TBI and those who assess residuals of TBI to be outdated and inaccurate, given the current knowledge about TBI and its sequelae at all levels of severity. In addition to the previously raised concerns related to the facets in the DBQ, there was particular concern on the
committee about the repeated assertion in the training materials that only symptoms that emerge soon after the injury can be confidently attributed to the TBI. The committee notes that TBI, including mild TBI, can be associated with later health consequences (see Chapter 2 and, for example, Aldag et al., 2017; Barnes et al., 2018; Corrigan and Hammond, 2013; Crane et al., 2016; Dams-O’Connor et al., 2013; Fann et al., 2018; Gardner et al., 2017, 2018; IOM, 2009; Masel and DeWitt, 2010; McKee et al., 2009). As described in Chapter 2, there are multiple reasons why the sequelae of TBI can manifest at any time following the injury. Thus, the VA should be aware that training materials should be updated frequently to reflect the current state of the science.
Exams Provided by VHA Clinicians Compared to Those Provided by VBA Contractors
One theme that recurred throughout the committee’s deliberations about the adjudication process was the differences between C&P exams performed by VHA clinicians and those performed by VBA contractors.
In recent years there has been a substantial increase in the percentage of exams ordered for contractors. Table 3-2 shows a breakdown of C&P exams ordered for claims that included a diagnosis of TBI by VHA clinicians versus VBA contractors from 2016 through 2018. The percentage of exams performed by contractors for claims that include a diagnosis of TBI has increased from 26 percent in 2016 to 58 percent in 2017 to 71 percent to date in 2018, including claims that ordered both VHA- and VBA-contract exams.
TABLE 3-2 VHA- and VBA-Contract Exams Ordered for Claims That Included a Diagnosis of TBI
| Fiscal Year | Number of Exams Ordered | VBA-Contract Exams Ordered | VHA Exams Ordered | Both* |
|---|---|---|---|---|
| 2016 | 39,524 | 7,100 (18%) | 29,340 (74%) | 3,084 (8%) |
| 2017 | 42,765 | 15,574 (36%) | 17,855 (42%) | 9,336 (22%) |
| 2018 (through July 2018) | 28,199 | 12,777 (45%) | 7,999 (29%) | 7,423 (26%) |
NOTE: The number of exams ordered includes both those for service connection and those for increased benefits.
*Both VHA- and VBA-contract examinations were ordered for a single veteran during the pendency of a claim that included TBI. However, the examinations may or may not have been for the claimed condition of TBI.
SOURCE: Communication with VBA, July 2018.
The increase in the percentage of exams performed by contractors is notable because there are several differences in how VHA clinicians and VBA contractors conduct C&P exams. First, VBA contractors often do not have the same access to VHA medical records that VHA clinicians do. VHA clinicians have access to a veteran’s full medical record, but contractors only have access to the information that VBA (or VHA) provides to them. If a veteran is receiving care at the VA, his or her thorough TBI assessment will be part of the medical record, and access to that information for the purposes of completing the DBQ might favor the veteran. A contractor would have access to the TBI assessment only if VHA/VBA supplies it (personal communication with VBA, June 18, 2018).
Furthermore, the committee learned through its conversations with VBA that VHA clinicians and VBA contractors do not receive the same training. Hiring standards are different for VHA clinicians and VBA contractors. Contractors might not have the military cultural competence that VHA clinicians do. In addition, contractors might be more isolated geographically from VA medical centers, and might not have access to other examiners if questions arise regarding their ability to assess residuals (personal communication with VBA, June 18, 2018).
Another potential difference between VHA clinicians and VBA-contracted clinicians is that VHA clinicians typically work with a team of individuals with specific training related to the components included within the DBQ, while it is not clear if contracting clinicians have the same additional expertise available to them. That could be a problem for sections on the DBQ that might require a referral to a clinician with different expertise from the examining physician (personal communication with VBA, June 18, 2018). In cases where contracting clinicians in geographically isolated areas do not have access to additional expertise needed to complete a DBQ, it might be appropriate to consider telehealth as an alternative to an in-person examination. The VA provides standards for telehealth examinations in its M21 manual. Specifically, the examiner must be able to “see clearly, and fully appreciate all non-verbal cues, mannerisms, and manifestations displayed by the Veteran in a manner on par with an in-person examination” (VA, 2018b).
Finally, the committee learned from VBA that there might be a disparity between VHA clinicians and VBA contractors in the amount of time spent with veterans. Contractors are typically paid according to the number of exams completed. Thus, there might be an incentive to minimize the time spent with each patient and complete more exams. Additionally, the average VHA C&P provider is fully trained in 6–8 months and his or her work is reviewed by senior providers. Contractors generally do not spend as much time on training and oversight, which might lead to differing examination results (personal communication with VBA, June 18, 2018).
It is important to note that while differences exist in the way that VHA clinicians and VBA contractors perform C&P exams, the committee could find no evidence regarding whether there are differences in outcome between the two groups. VBA does not collect data relevant to that issue from its contractors. Nonetheless, given that differences exist, the committee provides a recommendation regarding the use of contractors to perform C&P exams.
The committee recommends that the Department of Veterans Affairs provide the Veterans Benefits Administration contractors with the same training and access to medical records as Veterans Health Administration clinicians to ensure equitable disability determinations for all veterans.
QUALITY ASSURANCE IN THE ADJUDICATION OF DISABILITY COMPENSATION CLAIMS FOR RESIDUALS OF TBI
Given its broader task of providing recommendations for legislative or administrative action for improving the adjudication of veterans’ claims for impairments arising from TBI, the committee reviewed the protocols the VA has in place for assuring quality of its processes.
The VA’s Efforts to Ensure Consistency
The committee sent the VA questions about how the department ensures consistency in translating information from the DBQ into a disability percentage. The VA sent written responses to the committee’s questions and answered that it promotes consistency through automating decision-making processes, by providing training and oversight of its raters, and conducting national reviews of rater compliance with the department’s procedures (personal communication with VBA, July 6, 2018).
The VA explained that consistency in decision making is promoted by automating some of the decisions that would otherwise be left to the discretion of raters, using decision assistance tools, such as the evaluation builder within VBA’s electronic claims processing system (i.e., the Veterans Benefits Management System). Using the evaluation builder, the rater inputs information from all DBQs related to the claim, and the evaluation builder translates the rater’s selections into a disability evaluation percentage by applying the disability evaluation criteria from the VASRD. According to the VA, that automation allows for greater consistency between ratings.
The VA believes that the training and oversight of decision makers also promote consistency in the ratings process (personal communication with VBA, July 6, 2018). VBA’s Adjudication Procedures Manual, M-21, requires that TBI raters complete training, which will be described in the next section.
Finally, the VA explained that it promotes consistency through national quality reviews and that these reviews are “designed to gauge the quality of the claims process to maintain and improve the consistency and compliance of all claims based on current policy and procedures” (personal communication with VBA, July 6, 2018).
The VA’s training and oversight for raters and its quality reviews are described in detail in the following sections.
Training Required for Veterans Service Representatives
As described previously, RVSRs are the personnel within VBA who determine if a veteran’s condition is service-connected and, if so, provide the veteran with a disability rating percentage using criteria in the VASRD. The committee spoke with a former RVSR to understand the training and oversight that the VA requires of RVSRs (personal communication with VBA, August 6, 2018).
RVSRs receive 3 months of training, including 1 at a regional office and 2 at a national location. During the first month of training at a regional office, new RVSRs are taught by a DRO various processes, rules, and regulations related to providing ratings. They are also taught how to use VBA rating tools and how to navigate the VA information technology (IT) system, and they are given an overview of diseases by body system. After this month of training, RVSRs attend challenge training at a national location, where they are divided into classrooms of 20 students with whom they spend the 2 months of training. Each group is provided with an initial set of three instructors from various regional offices across the nation for the first month of challenge training. Instructors are seasoned ratings specialists, including DROs.
RVSRs are taught the curriculum provided from the training department, including some of the same material provided in the regional training—IT systems, diseases by body systems, and protocols. For the second month of challenge training, the instructors are replaced by three different instructors who teach the same material. Thus, new RVSRs repeat the same lessons
with different teachers who might have different teaching styles and perspectives. During challenge training, new RVSRs rate practice cases that are graded against a gold standard.
When the training is completed, the new RVSRs return to their regional offices, where they are assigned teams and official mentors, who are DROs or seasoned raters. Every case reviewed by a new RVSR goes to the DRO for review and then to quality review (QR) for more review. RVSRs can specialize in certain areas that require additional training, such as TBI, sexual trauma, cases with VA employees, or cases with veterans represented by an attorney.
When assigned specialty cases, such as TBI, the new RVSR must have 100 percent of their cases reviewed by a mentor until they “correctly” (as determined by the mentor) rate 10 consecutive cases. Then, they are released to “single signature” status, meaning they can determine a rating without mentor review (personal communication with VBA, August 6, 2018).
Quality Review in the VA
According to the VA’s Adjudication Procedures Manual, M-21-4 (VA, 2018b), VBA assesses the quality of its rating process using two systems: a compensation service quality review team (QRT), which operates at each facility where claims are processed for disability, and the national level Systematic Technical Accuracy Review (STAR).
Compensation Service Quality Review Teams
The compensation service QRT places quality review specialists at each VBA facility that processes claims to assess the performance of individual raters’ work. The QRT routinely reviews claims before a final determination is made in an effort to identify and avoid common errors (GAO, 2014; VA, 2018b). According to the VA, the QRT’s purpose is to improve the quality and timeliness of claims processing and to decrease the amount of work performed on individual cases. The focus is on evaluating the quality of each facility that processes claims, identifying error trends (i.e., where a decision rises to the level of a clear and unmistakable error or a clear violation of current regulations or directives), and ensuring that employee reviews are performed monthly. The QRT’s primary work is to provide feedback and training on error trends identified via individual quality reviews and in-process reviews.
Individual Quality Reviews
Individual quality reviews are randomly selected from the previous month based on national performance standards. Five randomly selected completed cases are reviewed per month per rater (RVSR, VSR, or DRO). The goal is to perform 60 individual quality reviews every fiscal year per rater in order to assess quality (VA, 2018b).
In-Process Review
Another process called in-process review (IPR) occurs prior to finalization of the rating in an effort to identify errors. Cases are again randomly reviewed. According to the VA, the focus of IPR is on identifying errors early in the claims process, identifying training opportunities, and improving employees’ understanding of why errors occurred and how to prevent them in the future. Errors that are detected are provided to employees immediately so that prompt corrective action can be taken. These are non-punitive and not used for individual performance management purposes. The IPR process does not occur regularly (VA, 2018b).
Systematic Technical Accuracy Review (STAR)
Quality review also occurs at the national level through VBA’s national quality assurance program, using the STAR process. VBA began employing STAR in 2012 to measure the accuracy of decisions on individual medical conditions within each claim (GAO, 2014). STAR staff members randomly select completed claims and review them against specific aspects of the claim in the STAR checklist. These include the following critical items: (1) benefit entitlement (address all issues, proper development, grant or deny, and award actions); (2) decision documentation and notification; and (3) administrative (appropriate signatures, examination and medical opinion requests, and expedited favorable decision). The review focuses on the outcome of the claim, not the process by which the decision was reached. The stated purpose of the reviews is to gauge the quality of the claims process in order to maintain and improve the consistency and compliance of all claims based on current policy and procedures (VA, 2018b).
The STAR review has two main components, as noted in a 2014 Government Accountability Office (GAO) report:
- Benefit entitlement review: assesses whether the correct steps were followed in addressing all issues in the claim, collecting appropriate evidence, and whether the resulting decision was correct, including effective dates and payment rates.
- Accuracy performance measures: calculated based on the results of the benefit entitlement review.
The STAR system also assesses whether claims processors appropriately documented the decision and notified claimants. Data are produced on a monthly basis by each regional office. In 2018, claims-based and issue-level accuracy were reported for 3-month and 12-month periods. The claims-based accuracy rate is determined by dividing the total number of error-free cases by the total number of cases reviewed. Issue-level accuracy is a measure of individual medical issues contained within a compensation claim. For the 12-month period preceding September 15, 2018, the national claim-based accuracy ranged from 85 to 91 percent and the issue-based accuracy from 94 to 96.5 percent (VA, 2018d).
Progress on Institute of Medicine 2007 Recommendations for Improving the Disability Adjudication Process
In 2007 the Institute of Medicine (IOM), in a report titled A 21st Century System for Evaluating Veterans for Disability Benefits, offered a number of recommendations to the VA on updating the disability evaluation process. Two of the recommendations bear on the question of assuring and improving the quality of the system, and the current committee asked the VA to comment on progress related to these recommendations.
Recommendation 5-3 was:
VA should establish a recurring assessment of the substantive quality and consistency, or inter-rater reliability, of examinations performed with the templates, and if the assessment finds problems, take steps to improved quality and consistency, for example, by revising the templates, changing the training, or adjusting the performance standards for examiners.
In its written response, VHA replied that the VA Office of Disability and Medical Assessment conducts “focused ratability reviews of disability evaluation requests and reports” using an audit tool (communication with VHA, May 7, 2018). This process is designed for clinical evaluation. VHA reports that it draws a randomized stratified sample of Veterans Integrated Services Network disability evaluations, which are added to the VA Corporate Data Warehouse each month (although it is not clear who does the auditing). The results are shared with the facilities and might trigger additional training or suggestions for improvement to the DBQ.
Recommendation 5-4 was: “The rating process should have built-in checks or periodic evaluations to ensure inter-rater reliability as well as the accuracy and validity of rating across impairment categories, ratings, and regions.” In its written response, VBA stated that it conducts quality reviews at both the local and national level to assess the accuracy of claims processing (personal communication with VBA, May 2018). As described earlier in this chapter, the reviews are conducted by QRTs at each of the VA’s 57 regional offices and can result in individual employee feedback and training. At the national level, this process is conducted by the STAR staff. VBA also examines consistency and variance across certain disability categories and decision types. In 2017, VBA initiated a quality management system, which is a database that contains all the quality measurement processes in a single system.
The committee notes that VHA and VBA’s responses did not address measures of inter-rater reliability, as recommended by the 2007 IOM report.
Inter-Rater Reliability
The committee asked the VA if it was aware of any studies that examine inter-rater reliability or the degree of agreement among independent raters. VBA responded by describing its consistency study program. VBA developed its consistency study program to assess nationwide consistency among raters and to identify regional offices that require further training. In this training exercise, raters from all regional offices are provided the same body of evidence. Working independently, raters must make disability determinations of granting versus denying, assigning percentages, and assigning effective dates (personal communication with VBA, July 6, 2018).
According to a 2014 GAO report, VBA relied on inter-rater reliability studies to assess consistency, but the studies were time-consuming and resource-intensive, so VBA limited the scope of the studies to about 25–30 percent of its raters. However, since 2009, VBA has expanded its consistency program to include questionnaires, which are less resource-intensive, resulting in the VA’s ability to administer the questionnaire to all raters, and more frequently—about 3 to 24 questionnaires per year (GAO, 2014). GAO reported that VBA stopped conducting consistency studies in favor of the more efficient questionnaires for assessing decision-making consistency. GAO reports that VBA did not pretest the consistency questionnaires to ensure the clarity of the questions or the validity of the expected results. (Appendix N includes a summary table of GAO reports on improving the VA disability compensation process.)
Chapter 4 will expand on this issue and others related to the quality of the adjudication process and will discuss the characteristics of a high-quality process for determining disability resulting from TBI.
SUMMARY AND RECOMMENDATIONS
The VA requested that the committee review the adjudication process by which the impairments that result from TBI are assessed for awarding disability compensation. The committee was asked in particular to assess the adequacy of the tools and protocols used by the VA to provide examinations and to review the credentials and training of the providers who perform examinations.
The adjudication process for VA disability compensation involves several stakeholders, including the veteran, VBA, VHA, and staff offices that work with veterans on appeals. First, the veteran—or a VSO acting as the veteran’s proxy—submits a claim to VBA. If all necessary information is provided, VBA will process the claim. Once a service-connected TBI diagnosis has been established, the residuals of TBI must be assessed to assist VBA with determining the disability rating. VBA sometimes accepts a medical report from a private physician if the agency determines it is “adequate for rating purposes.” In most cases, medical information submitted is not “adequate for rating purposes,” and VBA orders a C&P exam. A VHA physician or VBA clinician contractor evaluates the degree of impairment, functional limitation, and disability of the resulting TBI residuals. The C&P examiner records information using the DBQ for residuals of TBI, which is then submitted to VBA. If there is enough evidence, an RVSR makes a percentage disability rating decision by comparing DBQ results and other evidence to criteria in the VASRD and assigns an effective date. The veteran begins receiving disability benefits and may appeal to have his case reviewed if he or she does not agree with the rating decision. The appeals process re-reviews the case.
The DBQ guides the documentation of C&P exams by providing a structure for the standardized reporting of results. The VA developed the DBQs to mirror the VASRD in order to simplify decision making for raters in determining a disability rating. Although the DBQ is completed by a clinician, the disability rating is made by a non-clinician VBA rater, who applies medical information from the DBQ and other information from the veteran’s records, if available, to the criteria in the VASRD. The clinician essentially plays no role in applying the diagnosis and medical information to the VASRD.
The DBQ and the VASRD provide a list of common sequelae9 of TBI that are used to rate the level of disability associated with TBI. For the most part, the identified residuals accurately reflect the problems that are most likely to disrupt quality of life following TBI. However, some of the characteristics of the sequelae used to rate the severity of the disability (e.g., the frequency at which the problem is observed) do not fully capture the sequela’s potential impact. Furthermore, they fail to take into account some basic medical knowledge concerning how residuals of TBI might manifest and affect disability.
The committee recommends that the Department of Veterans Affairs convene experts from both Veterans Health Administration and Veterans Benefits Administration, including clinicians who diagnose and assess residuals of traumatic brain injury (TBI), to regularly update the Veterans Affairs Schedule for Rating Disabilities and Disability Benefits Questionnaire for residuals of TBI to better reflect the current state of medical knowledge.
___________________
9 Referred to by the VA as residuals.
In the committee’s review of the residuals of TBI DBQ, it found that there are important residuals that were not included. In particular, three important residuals of TBI are not adequately covered by any of the existing DBQs: insomnia, vestibular dysfunction, and near-vision dysfunction (near-point accommodative and convergence insufficiency).
Isolated questions related to insomnia and sleep disruption can be found on four DBQs (mental disorders, chronic fatigue syndrome, PTSD, and sleep apnea), but no single DBQ combines them all in a way that captures the full extent of disability associated with post-TBI sleep disruption. Sleep disruption occurs commonly after TBI, contributing to fatigue, cognitive dysfunction, and disrupted mood.
Isolated questions and physical exam elements related to vestibular dysfunction can be found on two DBQs (cranial nerves diseases and ear conditions), but no single DBQ combines them in a way that captures the full extent of disability associated with post-TBI vestibular dysfunction. This dysfunction is typically a mix of both peripheral (ear and vestibulocochlear nerves) and central (vestibulo-spinal and vestibulo-ocular) vestibular structure disruption. Vestibular dysfunction occurs commonly after TBI, producing symptoms related to (1) altered postural stability (imbalance and abnormal gait); (2) altered oculomotor function (reduced dynamic visual acuity, dizziness with head movement, dizziness with movement of objects in visual field); and (3) reduced concentration or “fogginess” when in motion. Vestibular dysfunction may also contribute to altered mood, particularly anxiety.
Although the eye conditions DBQ includes questions related to diplopia, no existing DBQ includes questions or physical exam elements intended to capture the full extent of disability associated with near-point accommodative and convergence insufficiency. These near-vision problems occur commonly after TBI and can result in not only diplopia but also blurred vision, headache, nausea, and an inability to maintain focus while reading and doing other close-range visual activities.
The committee recommends that the Department of Veterans Affairs add insomnia, vestibular dysfunction, and near-vision dysfunction to the Disability Benefits Questionnaire for residuals of traumatic brain injury.
Additionally, through conversations with the VA, the committee learned that there are differences in training and access to medical records between VHA clinicians and VBA-contracting clinicians who conduct C&P evaluations. This is notable, given the recent increase in the percentage of C&P evaluations performed by contractors for TBI claims (from 26 percent in 2016 to 58 percent in 2017 and 71 percent to date in 2018).
The committee recommends that the Department of Veterans Affairs provide the Veterans Benefits Administration contractors with the same training and access to medical records as Veterans Health Administration clinicians to ensure equitable disability determinations for all veterans.
Finally, the committee was tasked with making recommendations for improving the overall adjudication process for disability claims for residuals of TBI. The committee examined the structures the VA has in place for assuring the quality of its adjudication process. Although VBA has systems in place to review the consistency of the rating process, the VA does not measure reliability or validity. Chapter 4 will expand on this issue and discuss characteristics of a high-quality process for determining disability resulting from TBI.
REFERENCES
Agoston, D. V., and A. Kamnaksh. 2015. Modeling the neurobehavioral consequences of blast-induced traumatic brain injury spectrum disorder and identifying related biomarkers. In F. H. Kobeissy (ed.), Brain neurotrauma: Molecular, neuropsychological, and rehabilitation aspects. Boca Raton, FL: CRC Press. Pp. 309–328.
Akin, F. W., O. D. Murnane, C. D. Hall, and K. M. Riska. 2017. Vestibular consequences of mild traumatic brain injury and blast exposure: A review. Brain Injury 31(9):1188–1194.
Aldag, M., R. C. Armstrong, F. Bandak, P. S. F. Bellgowan, T. Bentley, S. Biggerstaff, K. Caravelli, J. Cmarik, A. Crowder, T. J. DeGraba, T. A. Dittmer, R. G. Ellenbogen, C. Greene, R. K. Gupta, R. Hicks, S. Hoffman, R. C. Latta, M. J. Leggieri, D. Marion, R. Mazzoli, M. McCrea, J. O’Donnell, M. Packer, J. B. Petro, T. E. Rasmussen, W. Sammons-Jackson, R. Shoge, V. Tepe, L. A. Tremaine, and J. Zheng. 2017. The biological basis of chronic traumatic encephalopathy following blast injury: A literature review. Journal of Neurotrauma 34(S1):S26–S43.
Angeleri, R., F. M. Bosco, M. Zettin, K. Sacco, L. Colle, and B. G. Bara. 2008. Communicative impairment in traumatic brain injury: A complete pragmatic assessment. Brain and Language 107(3):229–245.
Barnes, D. E., A. L. Byers, R. C. Gardner, K. H. Seal, W. J. Boscardin, and K. Yaffe. 2018. Association of mild traumatic brain injury with and without loss of consciousness with dementia in U.S. military veterans. JAMA Neurology 75(9):1055–1061.
Bornhofen, C., and S. McDonald. 2008. Emotion perception deficits following traumatic brain injury: A review of the evidence and rationale for intervention. Journal of the International Neuropsychological Society 14(4):511–525.
Brahm, K. D., H. M. Wilgenburg, J. Kirby, S. Ingalla, C. Y. Chang, and G. L. Goodrich. 2009. Visual impairment and dysfunction in combat-injured service members with traumatic brain injury. Optometry and Vision Science 86(7):817–825.
Bratt, M., T. Skandsen, T. Hummel, K. G. Moen, A. Vik, S. Nordgard, and A. S. Helvik. 2018. Frequency and prognostic factors of olfactory dysfunction after traumatic brain injury. Brain Injury 32(8):1021–1027.
BVA (Board of Veterans’ Appeals). 2016. Life cycle of a VA appeal. https://www.bva.va.gov/docs/LifeCycle-of-a-VA-Appeal-FY2016.pdf (accessed November 21, 2018).
BVA. 2017. Department of Veterans Affairs Board of Veterans’ Appeals—Annual report, fiscal year (FY) 2017. https://www.bva.va.gov/docs/Chairmans_Annual_Rpts/BVA2017AR.pdf (accessed September 28, 2018).
Catena, R. D., P. Van Donkelaar, C. I. Halterman, and L. S. Chou. 2009. Spatial orientation of attention and obstacle avoidance following concussion. Experimental Brain Research 194(1):67–77.
Corrigan, J. D., and F. M. Hammond. 2013. Traumatic brain injury as a chronic health condition. Archives of Physical Medicine and Rehabilitation 94(6):1199–1201.
Crane, P. K., L. E. Gibbons, K. Dams-O’Connor, E. Trittschuh, J. B. Leverenz, C. Dirk Keene, J. Sonnen, T. J. Montine, D. A. Bennett, S. Leurgans, J. A. Schneider, and E. B. Larson. 2016. Association of traumatic brain injury with late-life neurodegenerative conditions and neuropathologic findings. JAMA Neurology 73(9):1062–1069.
Dams-O’Connor, K., L. E. Gibbons, J. D. Bowen, S. M. McCurry, E. B. Larson, and P. K. Crane. 2013. Risk for late-life re-injury, dementia and death among individuals with traumatic brain injury: A population-based study. Journal of Neurology, Neurosurgery, and Psychiatry 84(2):177–182.
Fann, J. R., A. R. Ribe, H. S. Pedersen, M. Fenger-Grøn, J. Christensen, M. E. Benros, and M. Vestergaard. 2018. Long-term risk of dementia among people with traumatic brain injury in Denmark: A population-based observational cohort study. The Lancet Psychiatry 5(5):424–431.
Franke, L. M., W. C. Walker, D. X. Cifu, A. L. Ochs, and H. L. Lew. 2012. Sensorintegrative dysfunction underlying vestibular disorders after traumatic brain injury: A review. Journal of Rehabilitation Research and Development 49(7):985–994.
GAO (Government Accountability Office). 2014. Improvements could further enhance quality assurance efforts. https://www.gao.gov/assets/670/667027.pdf (accessed May 18, 2018).
Gardner, R. C., C. B. Peltz, K. Kenney, K. E. Covinsky, R. Diaz-Arrastia, and K. Yaffe. 2017. Remote traumatic brain injury is associated with motor dysfunction in older military veterans. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences 72(9):1233–1238.
Gardner, R. C., A. L. Byers, D. E. Barnes, Y. Li, J. Boscardin, and K. Yaffe. 2018. Mild TBI and risk of Parkinson disease: A Chronic Effects of Neurotrauma Consortium study. Neurology 90(20):e1771–e1779.
Health.mil. 2018. Medical evaluation board. http://www.health.mil/Military-Health-Topics/Conditionsand-Treatments/Physical-Disability/Disability-Evaluation/Medical-Evaluation (accessed November 20, 2018).
IOM (Institute of Medicine). 2007. A 21st century system for evaluating veterans for disability benefits. Washington, DC: The National Academies Press.
IOM. 2009. Gulf War and health: Volume 7: Long-term consequences of traumatic brain injury. Washington, DC: The National Academies Press.
Junn, C., K. R. Bell, C. Shenouda, and J. M. Hoffman. 2015. Symptoms of concussion and comorbid disorders. Current Pain and Headache Reports 19(9):46.
Kearns, W. D., J. L. Fozard, L. Schonfeld, S. Scott, and K. Marshall. 2015. Elevated movement path tortuosity in voluntary outdoor ambulation in community-dwelling veterans with a history of traumatic brain injury. Journal of Head Trauma Rehabilitation 30(1):E8–E14.
Masel, B. E., and D. S. DeWitt. 2010. Traumatic brain injury: A disease process, not an event. Journal of Neurotrauma 27(8):1529–1540.
McKee, A. C., R. C. Cantu, C. J. Nowinski, E. T. Hedley-Whyte, B. E. Gavett, A. E. Budson, V. E. Santini, H. S. Lee, C. A. Kubilus, and R. A. Stern. 2009. Chronic traumatic encephalopathy in athletes: Progressive tauopathy after repetitive head injury. Journal of Neuropathology and Experimental Neurology 68(7):709–735.
McKinlay, W., and A. Watkins. 1999. Cognitive and behavioral effects of brain injury. In M. Rosenthal, E. R. Griffith, J. S. Kreutzer, and B. Pentland (eds.), Rehabilitation of the adult and child with traumatic brain injury, 3rd ed. Philadelphia, PA: Davis Company. Pp. 74–86.
McKinnon, A., R. Meiser-Stedman, P. Watson, C. Dixon, N. Kassam-Adams, A. Ehlers, F. Winston, P. Smith, W. Yule, and T. Dalgleish. 2016. The latent structure of acute stress disorder symptoms in trauma-exposed children and adolescents. Journal of Child Psychology and Psychiatry and Allied Disciplines 57(11):1308–1316.
Meadows, L., and J. Williams. 2009. An understanding of functional movement as a basis for clinical reasoning. In S. Raine, L. Meadows, and M. Lynch-Ellerington (eds.), Bobath concept: Theory and clinical practice in neurological rehabilitation. New York: Wiley. Pp. 23–42.
Morin, M., P. Langevin, and P. Fait. 2016. Cervical spine involvement in mild traumatic brain injury: A review. Journal of Sports Medicine 2016:1590161.
Neumann, D., B. Zupan, J. F. Malec, and F. Hammond. 2014. Relationships between alexithymia, affect recognition, and empathy after traumatic brain injury. Journal of Head Trauma Rehabilitation 29(1):E18–E27.
Prigatano, G. P. 2009. Anosognosia: Clinical and ethical considerations. Current Opinion in Neurology 22(6):606–611.
Rosenthal, M., J. S. Kreutzer, E. R. Griffith, and B. Pentland. 1999. Rehabilitation of the adult and child with traumatic brain injury. Philadelphia, PA: Davis Company.
Rowley, D. A., M. Rogish, T. Alexander, and K. J. Riggs. 2017. Cognitive correlates of pragmatic language comprehension in adult traumatic brain injury: A systematic review and meta-analyses. Brain Injury 31(12):1564–1574.
Sherer, M., P. Bergloff, E. Levin, W. M. High Jr, K. E. Oden, and T. G. Nick. 1998. Impaired awareness and employment outcome after traumatic brain injury. Journal of Head Trauma Rehabilitation 13(5):52–61.
SSA (Social Security Administration). 2017. Substantial gainful activity. https://www.ssa.gov/oact/cola/sga.html (accessed May 27, 2018).
Thiagarajan, P., K. J. Ciuffreda, and D. P. Ludlam. 2011. Vergence dysfunction in mild traumatic brain injury (mTBI): A review. Ophthalmic and Physiological Optics 31(5):456–468.
Togher, L., C. Wiseman-Hakes, J. Douglas, M. Stergiou-Kita, J. Ponsford, R. Teasell, M. Bayley, and L. S. Turkstra. 2014. INCOG recommendations for management of cognition following traumatic brain injury, part IV: Cognitive communication. Journal of Head Trauma Rehabilitation 29(4):353–368.
VA (Department of Veterans Affairs). 2015a. Chapter 2: Service-connected disabilities. https://www.va.gov/opa/publications/benefits_book/benefits_chap02.asp (accessed May 11, 2018).
VA. 2015b. Information and instructions for completing notice of disagreement (NOD). https://www.vba.va.gov/pubs/forms/VBA-21-0958-ARE.pdf (accessed August 24, 2018).
VA. 2016a. VHA directive 1184: Screening and evaluation of traumatic brain injury. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=5376 (accessed May 11, 2018).
VA. 2016b. VHA directive 1603: Training and certification of clinicians performing VA disability examinations. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3295 (accessed May 11, 2018).
VA. 2016c. DEMO traumatic brain injury examination course. Department of Veterans Affairs. http://www.vesservices.com/VESWP/wp-content/uploads/2016/01/DEMO_TBI-course_0116.pdf (accessed May 11, 2018).
VA. 2018a. Compensation. https://www.benefits.va.gov/compensation (accessed August 24, 2018).
VA. 2018b. M21-1 adjudication procedures manual. Department of Veterans Affairs. https://www.knowva.ebenefits.va.gov/system/templates/selfservice/va_ssnew/help/customer/locale/en-US/portal/554400000001018/topic/554400000004049/M21-1-Adjudication-Procedures-Manual (accessed May 11, 2018).
VA. 2018c. The VA claims process after you file your claim. https://www.va.gov/disability/after-you-file-claim (accessed January 9, 2019).
VA. 2018d. Veterans Benefits Administration reports: Detailed claims data. https://www.benefits.va.gov/reports/detailed_claims_data.asp (accessed May 18, 2018).
VA Law (Veterans Law Group). 2018. Frequently asked questions. https://www.veteranslaw.com/faq (accessed August 28, 2018).
Veterans Aid Benefit. 2018. VA 2018 compensation, SMC, and DIC rates. https://www.benefits.va.gov/COMPENSATION/resources_comp01.asp (accessed August 28, 2018).
Viola-Saltzman, M., and N. F. Watson. 2012. Traumatic brain injury and sleep disorders. Neurology Clinics 30(4):1299–1312.
Wood, R. L., and A. Worthington. 2017. Neurobehavioral abnormalities associated with executive dysfunction after traumatic brain injury. Frontiers in Behavioral Neuroscience 11:195.
Worthington, A. 2016. Treatments and technologies in the rehabilitation of apraxia and action disorganisation syndrome: A review. NeuroRehabilitation 39(1):163–174.
Wortzel, H. S., and D. B. Arciniegas. 2014. The DSM-5 approach to the evaluation of traumatic brain injury and its neuropsychiatric sequelae. NeuroRehabilitation 34(4):613–623.
This page intentionally left blank.


























