4
Addressing Quality and Access: Promoting Behavioral Health in Rural Communities
This chapter summarizes the workshop session that focused on people living in rural communities, many of whom encounter barriers in accessing quality health and health care.
Jane Hamel-Lambert, Nationwide Children’s Hospital, introduced the panel by discussing the challenges rural communities face and asked participants to consider the assets and resources that can be leveraged to effect change. She noted that policy levers could be taken advantage of to build momentum for improving mental and behavioral health for children and adolescents in rural areas. Increasing the visibility of children in rural areas is essential, she said.
Kelly Kelleher, Nationwide Children’s Hospital, urged celebration of the fact that children in general are healthier today than they have been at any other time in the nation’s history. With safer health care for children, higher immunization rates, and declining infant mortality rates in most places, there is much to highlight. However, he continued, an exception is what he characterized as diseases of disconnection and despair, such as drug use, suicide, and mental and behavioral health disorders in children and adolescents. He noted that in Ohio, readmission rates have increased due to psychiatric problems, and the majority of these problems are exacerbated in rural areas. Further, prescribing rates are higher in rural areas, and the ability to access care is delayed. “We have failed miserably the behavioral health system in rural areas,” Kelleher stated.
Kelleher said geography accelerates disparities that exist by classism and racism. There are variations in rural areas, just as there are variations in urban areas. The characteristics of decreased density, cultural attributes,
and thinness of infrastructure are uniform across most rural areas, and the solutions need to consider these characteristics. Many believe that rural life is healthier for young children, Kelleher continued, but the National Survey for Child Health (2011–2012) found that mental, emotional, and behavioral health for children in rural areas was as bad or worse than in other areas of the country. This was before the onset of the opioid crisis, which many rural communities are currently facing and which has increased mortality rates to that of HIV and gun deaths among non-retired aged populations, he noted.
In advance of the presentations, Kelleher offered several questions for participants to consider:
- Why isn’t there a science of rural areas that matches the urban literature?
- Why are evidence-based interventions not specific enough and ineffective in rural areas?
- Why are cross-sector models that have proven effective outside the United States not successful in the United States?
- What anti-poverty and community healing tools can be used?
Panel presenters were Keith Mueller, University of Iowa, who gave an overview of behavioral health services in rural communities nationwide, and Christine Vining, University of New Mexico, who focused on behavioral health for tribal children and families.
ACCESSING BEHAVIORAL HEALTH SERVICES IN RURAL COMMUNITIES
To provide a high-level perspective on accessing behavioral health services in rural communities, Keith Mueller looked across progress in three areas of behavioral health services: accessibility, affordability, and availability. He began by highlighting several key messages: (1) access is a function of affordability and availability; (2) affordability is a function of cost-of-care and insurance policies, including public programs; and (3) availability is a function of provider capacity, transportation, and use of technology. When it comes to identifying solutions to address access, affordability, and availability, Mueller recognized an important principle: form follows finance.
Affordability of Services
Affordability for rural residents is highly variable in types of insurance plans, Mueller noted, including variations in premiums, cost sharing, and
networks. Individuals may buy the lowest-cost insurance plan but may have a provider who is 50 miles away and not easily accessible. Finding a closer provider may result in higher premiums. According to Mueller, while consumer education is underway so people around the country can understand their options in selecting a health care plan, messaging to consumers in rural communities about being cautious when signing up for plans has been challenging.
Variability of health care plans—across riders, deductibles, providers, medication formularies, benefit designs, copayments, and co-insurance—is a consequence of public policies that influence options for consumers. Provisions and riders, Mueller stated, may affect eligibility and coverage conditions, including preexisting condition riders and lifetime limit clauses. This variability is accentuated for rural residents, where individual and small business plans are common.
Availability of Services
In rural communities, scarcity of high-level professionals is one issue impacting the availability of services. This shortage is across every category of health care professional, including community health workers. As new models are built that provide better services for rural communities and for people who receive public benefits, a qualified and professional workforce is needed. Mueller noted this is particularly true for behavioral health and in rural communities. Figure 4-1 shows mental health professional shortage areas around the country, defined in terms of psychiatrist-to-population ratios.
In addition to the workforce shortage, there is a shortage of institutional care. Mueller said states have begun to rely on community-based care and started closing state-inpatient facilities, but community-based care in rural America is not always available. Hospital-based care has become an alternative, although Mueller shared that there have been recent closures of rural hospitals and many more are financially vulnerable.
Accessibility to Services
Mueller stated that access is defined through affordability and availability. Because form follows finance, he noted, redesigning a payment system will influence the delivery system and decisions made by health care organizations. The push toward payment linked to value is defined as outcomes per dollars spent, rather than paying for process. Changes have taken place in anticipation of, and in response to, changes in payment structures. For example, he highlighted, in the past several years, Medicare implemented a new payment code for care management services. Care management has
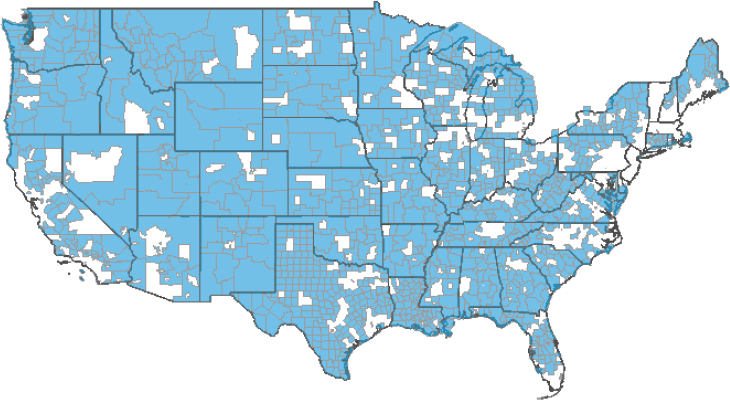
NOTE: Blue indicates shortage areas, white is non-shortage areas.
SOURCE: Health Resources & Services Administration Data Warehouse “Quick Maps,” see https://data.hrsa.gov/hdw/Topics/shortageareas.aspx.
also been adopted by commercial carriers around the country. Another recent change is the use of global budgets; Maryland took the lead in using global budgets, and other states began adopting them as well.
Accountable Care Organizations
Mueller explained that the Accountable Care Organizations (ACOs) model attracts organizations that want to rethink how health care dollars are spent. Strategies include care management that extends beyond traditional models. The benchmark is previous expenditures, and if fewer dollars are spent, the ACO shares in that savings. He said this model is an indication of provider and health care organization willingness to shift away entirely from an episode-based model and has spread rapidly in rural places (see Figures 4-2 and 4-3, which map the presence of ACOs in metropolitan and non-metropolitan areas in 2013 and 2015, respectively).
Mueller said the next stage is Accountable Health Communities (AHCs), as opposed to ACOs. An AHC broadens the network of who participates and is inclusive of other sectors, including social services. Rather than organizations approaching care management one patient at a time, AHCs think about population groups. In relation to rural communities, there are programs funded through the Centers for Medicare & Medicaid
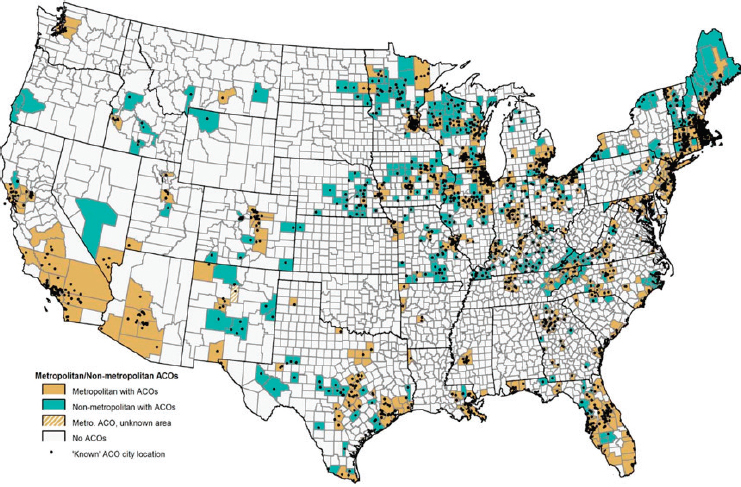
NOTE: CMS-designated sites as of January 2013. ACOs = Accountable Care Organizations, CMS = Centers for Medicare & Medicaid.
SOURCE: Mueller and Ullrich (2016), reprinted with permission from the Rural Policy Research Institute Center for Rural Health Policy Analysis.
Services Innovation Center that include rural participants, and there is a push to open up programs to be more creative in denominator definitions to include more rural communities.
Mueller highlighted several changes that have reached rural communities, including patient-centered medical homes and ACOs. He also noted the value of technology in service delivery in rural communities, as well as the establishment of AHCs. The future, he stated includes implementing a holistic approach to health and well-being (including from the health care organization), incorporating behavioral health services, and providing financial incentives that may drive desirable system change.
ADDRESSING QUALITY AND ACCESS: PROMOTING HEALTH IN RURAL NATIVE AMERICAN COMMUNITIES
Christine Vining provided the perspective of many communities throughout New Mexico. (See also Chapter 2 for her more personal account.) She identified barriers that pose a challenge for American Indian
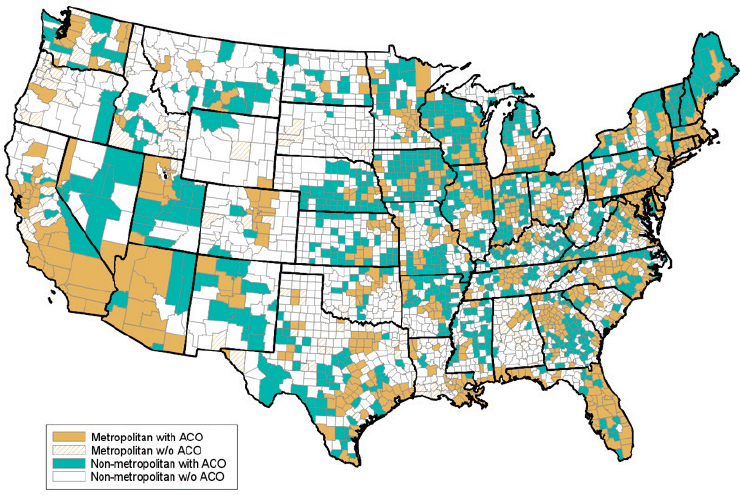
NOTE: Includes all active CMS ACOs as of August 2015. ACOs = Accountable Care Organizations, CMS = Centers for Medicare & Medicaid.
SOURCE: Mueller and Ullrich (2016), reprinted with permission from the Rural Policy Research Institute Center for Rural Health Policy Analysis.
families in accessing health, behavioral health, and disability services; described service coordination activities for communities in New Mexico; highlighted the importance of building relationships and community partnerships to increase access to services; and highlighted the importance of cultural and linguistic competencies and diversity in the workforce, particularly for rural communities in New Mexico.
Rural Native Americans in New Mexico
New Mexico tribes make up 10 percent of the population in the state and include the Apache and Navajo tribes, Vining explained. There are 19 pueblos, each bringing cultural and linguistic diversity. Native American populations experience a disproportionate disease burden because of inadequate education, disproportionate poverty, discrimination in health care services, and cultural differences. The Indian Health Service documents that death rates are higher for American Indians than the general population, with causes of death including alcoholism, diabetes, unintentional injuries, homicide, and suicide.
Vining stated that New Mexico struggles with keeping children and families healthy and thriving. According to Kids Count, New Mexico ranks 49th in child well-being, 48th in economic well-being, 50th in education, 37th in health, and 49th in family and community (Annie E. Casey Foundation, n.d). Nearly one-third of children live at or below the poverty line and have parents who lack secure employment. One-half of young children in New Mexico are not in school, and one-third of high school students do not graduate on time.
Barriers to Resources
The state’s geography impacts health and health outcomes due to lack of transportation and cost of travel, continued Vining. She shared that residents in rural areas have difficulty accessing health centers and hospitals; nearly one-half of the population lives in a Primary Care Health Professional Shortage Area, which is found in 32 of New Mexico’s 33 counties. Rural residents also have difficulty accessing grocery stores, thereby affecting access to quality food.
Further, barriers to services and resources include unfamiliarity with services and supports or lack of awareness of how to access them, stated Vining. There is also lack of recognition of neurodevelopmental disabilities, as well as specialized screenings for young children and availability of providers trained to identify and treat children with neurodevelopmental disabilities. In addition, according to Vining, families are required to navigate multisector systems of support across health, education, and social welfare.
Cultural considerations may also hinder access and use, and include linguistic and communication barriers, historical mistrust of agencies and providers, historical trauma, racism and discrimination, and stigma. Given these cultural considerations, it is critical that interventions and providers recognize that perspectives around health, development, and disability vary from tribe to tribe and incorporate traditional health options and openness to cultural beliefs.
Opportunities
Vining noted opportunities for improving behavioral health services for tribal children and families. To start, she highlighted the need to provide a full range of mental health support services for all family members using culturally sensitive approaches. She also recognized the need for providers to understand tribal American Indian health and culture.
Several solutions can improve quality and access for rural and tribal communities, Vining stated. There are a number of entities that families must interface for services, and a coordinator could assist in navigating and
coordinating these services and inform as well as advocate. Fostering community partnerships is important to addressing the needs of children and families in rural areas. Examples include creating and sustaining meaningful partnerships with key community representatives; communicating and sharing information with providers, policy makers, and families; exploring specific community strengths and needs; and embracing the communities and families in planning, implementing, and evaluating services. Vining also highlighted the value of incorporating strengths into culture-based models, which results in developing a shared sense of collective community responsibility; understanding and utilizing indigenous generational knowledge and wisdom; connecting with the past using a historical perspective; reclaiming traditional language and practices; and navigating between Western and tribal cultures.
Vining described the Indian Children’s Program Service area. It was a unique rural service model funded by the Indian Health Services that served American Indian children birth through age 18. Working across sectors and systems, it engaged families in health care, education, law, social welfare, and services for children with disabilities. An essential component was building partnerships with families and organizations at the local level and assisting with service coordination. Established as a result of a lawsuit 25 years ago, the program ended in 2014 and evolved into a telehealth model that provides training, education, and consultation to providers working with tribal children and youth.
Vining concluded by stressing several key points: (1) the importance of establishing relationships with community members; (2) recognition of culturally defined beliefs and practices regarding health; (3) providers as representatives of the populations they serve; (4) involvement of families and communities on advisory boards and in providing feedback on health practices; and (5) recognition that underserved populations go beyond racial and ethnic groups to include rural residents, low-income families, LGBTQ communities, linguistic diversity, and children and families with disabilities and complex medical and educational conditions.
DISCUSSION HIGHLIGHTS
Topics during the discussion included governance and regulations, assets of rural communities, and opportunities for new service models. Several questions addressed opportunities for changing governance and regulations to support the needs of rural communities. One participant commented that rural communities are not thriving because of policy and regulations and that industrialized medicine has devastated rural communities due to its focus on specialty and tertiary care as well as critical access hospitals. The participant noted a possible solution is to recognize
that communities are responsible for the governance of health care rather than the health care industry itself through accountable communities for health. Mueller noted that Minnesota is a leader in this area and agreed with the importance of bringing different sectors together under the same governance structure to be accountable for healthy communities. Another participant noted a potential disservice in efforts to credential, certify, and regulate services and the workforce. Opportunities for providing services to rural children and families across settings are missed due to regulations that disable certain professionals from administering services.
Another participant noted that the experiences and barriers rural communities face are similar to those in low-income countries: language and cultural barriers, lack of community capacity, and lack of terminology to name conditions in Native languages. He inquired about opportunities for building local capacity through public health strategies. Vining replied that these strategies, such as taxes to generate capacity, are inconsistent but should be further explored. Another participant said one of the biggest, and yet untapped, assets of rural communities is political power at the state and local level. Rural residents, the participant stated, can make political change at the state level and make decisions that work for rural communities.
Several questions focused on the need for a new service model for both rural and urban communities. Kelleher suggested moving toward community-based, group, and peer models that have worked in other countries. Mueller noted that transitioning delivery models needs to be methodically planned. When transitioning delivery models—for example, when closing an institution-based center for a community model of care—it is critical to avoid a gap between services. This has been a common problem when some communities transition models of care, he said.
This page intentionally left blank.










