In the final session of the first workshop day, moderated by Bruce Evans, fire chief, Upper Pine River Fire Protection District, Colorado, panelists with varied health care systems perspectives continued the exploration of communication, education, and information challenges posed by a nuclear incident; the implications of these challenges for capacity building; and opportunities and approaches for addressing them. The panelists were chosen based on their having served on the front lines of advances in responding to nuclear incidents that are either being proposed or are already works in progress. Much of the focus of the session was on burn care.
The panelists included Amanda Bettencourt, research fellow, Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, and nursing representative on the American Burn Association’s (ABA’s) Committee of Organization and Delivery of Burn Care; Cullen Case, Jr., program manager, Radiation Injury Treatment Network (RITN); James Jeng, Surgeon, Crozer-Chester Medical Center, Pennsylvania, and chair of the Disaster Subcommittee of ABA’s Committee of Organization and Delivery of Burn Care; Robert L. Jones, chief of the Inorganic and
Radiation Analytical Toxicology Branch of the Centers for Disease Control and Prevention’s (CDC’s) National Center for Environmental Health; Ziad Kazzi, associate professor, emergency medicine, Emory University School of Medicine, and board member at the American College of Medical Toxicology; and Ian Norton, director, Emergency Medical Teams, World Health Organization (WHO).
This chapter summarizes the panelists’ remarks on response capability priorities plus the open discussion with the audience that followed.
PRIORITIES FOR RESPONSE CAPABILITIES
Evans asked the panelists to describe their top priorities for response capabilities.
Perspective of a Burn Nurse
Bettencourt described burn care in a hospital environment as very nursing care intensive and very physical space intensive. Patients with the most acute burns are cared for in specialized burn intensive care unit (ICU) rooms, where plastic curtains surround a heated, humidified interior space and where nurses wear full personal protective equipment and take care of the patient through the plastic walls. Just changing a dressing on a patient can require three nurses at the bedside and can take 3–4 hours. “It is very time intensive, it is very high touch, it is very high tech, and it is very specialized,” Bettencourt said. But burn nursing is also highly variable, and most places where burn nursing occurs cover a range of levels of care—from ICU patients (both ICU and burn ICU) to ambulatory patients who are healing to even clinical patients. The intensive and variable nature of burn care creates a challenge when considering the massive amount of injuries and different types of patients that would result from a nuclear incident.
Geographic Distribution of Burn Care Across the United States
Adding to the challenge is the limited geographical distribution of burn centers across the United States (see Figure 6-1). This includes both ABA-verified (67) and non-ABA-verified (42) centers, with a total of approximately 900 burn beds. Bettencourt noted that there are three ABA-certified burn centers in Canada. Differences between ABA-verified and non-ABA-verified centers vary, although generally ABA-verified centers have all of the burn care team members, including not just nurses but also rehabilitation specialists, psychosocial support, and other necessary capabilities. As shown in Figure 6-1, there are large geographic areas in the United States
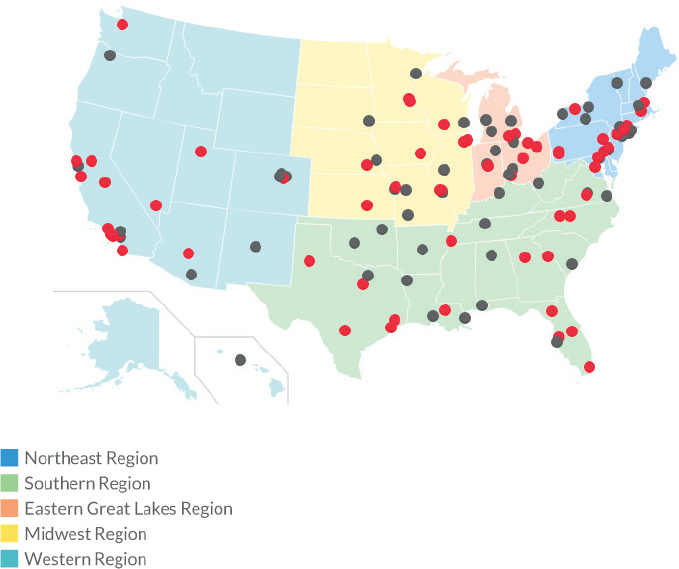
SOURCES: Bettencourt presentation, August 22, 2018, and American Burn Association, 2018.
where there are no burn centers. “If there are no burn centers, there are no nurses. That is a problem,” Bettencourt said.
Regarding pediatric burn care, only 39 of the 67 ABA-verified centers (58 percent) have combination adult/pediatric centers with the ability to take care of children varying depending on nursing staff. In some of these centers, only some of the nurses care for children. In others, all of the nurses can care for children. The three Canadian centers all have combined adult/pediatric units as well. With respect to comprehensive pediatric burn care and where most U.S. pediatric burn nurses are located, there are four freestanding pediatric burn hospitals and five burn units in freestanding children’s hospitals.
U.S. Burn Nursing Workforce: Current Status
“Nurses are on the front line of all disasters and mass casualties,” Bettencourt said. Yet most hospitals are understaffed, especially on nights and weekends. This has been evidenced during past natural disasters. Plus, she said, “there is a nursing shortage looming.”
Currently, there are approximately 3,270 registered nurses (RNs) in the United States who have burn expertise. For perspective, there are about 1.7 million hospital RNs. This means that roughly only 0.1 percent of the hospital RN workforce has any burn expertise at all, and even fewer RNs have pediatric burn expertise. Among advanced practice (AP) providers, there is, on average, only one APRN or physician assistant (PA) per burn center. Many centers do not have any AP providers with burn expertise. There are only 109 APRNs or PAs in the United States with burn expertise. Bettencourt reiterated that most burn centers cover all phases of burn care, from ambulatory to ICU, sometimes with separate workforces at each level of care but sometimes with the same nurses working across all levels of care. Either way, when thinking about an influx of the number of burn patients described earlier in the workshop (see Table 4-1), Bettencourt expressed concern about the small number of people who would be able to take care of those patients. Regarding previous workshop participants’ descriptions of burn care as the Achilles’ heel, or rate-limiting step, of medical care in the event of a nuclear incident, Bettencourt agreed: “If you do not have a nurse to care for these patients, a lot of the care is going to get delayed and not happen.”
Burn Nurse Competencies
A recent ABA task force identified nine burn nurse competencies (Carrougher et al., 2017):
- Initial assessment and management. Bettencourt explained that the definitive factor deciding the course of burn care is how big and deep a burn is. Burn nurses are uniquely trained to assess this and determine a plan for the patient.
- Physiologic support. This includes fluid resuscitation and ventilator management—again, unique skills that only burn nurses have. Although trauma nurses do have some background in fluid resuscitation, burn resuscitation is highly specialized and if done improperly can increase morbidity and mortality.
- Wound management. Burn nurses are uniquely trained to not only assess but also manage burn wounds.
- Pain, agitation, and delirium. Bettencourt explained that pain management from a nursing perspective includes things like dress-
-
ing changes and psychosocial support. A highly skilled nurse who can change a dressing quickly is often the best intervention—for children in particular—compared to narcotics or sedation. “Pain is not just drugs, but it is also technique,” she said.
- Nutritional support. Burn patients have unique nutritional needs.
- Psychosocial support. Burn nurses are highly skilled at providing the necessary psychosocial support and determining, for example, when it is right for patients to see their face or scars.
- Rehabilitation. Burn nurses receive specialized training in how to apply certain garments (e.g., burn splints) during rehabilitation.
- Discharge planning and after care support. Recovery is a large part of burn care. Burn nurses help with school reentry, work reentry, and peer support.
- End-of-life care.
Extending These Competencies to Other Types of Nurses: An Important Challenge
In Bettencourt’s opinion, all of these competencies would certainly be useful in a nuclear incident scenario. Yet they are unique to burn nurses for the most part. Most nurses do not finish nursing school with any experience caring for burn patients. For Bettencourt, one of the biggest challenges is how to extend these competencies to other types of nurses.
Top Concerns
Among Bettencourt’s top priorities or concerns, the first is that there are not enough burn nurses to care for thousands of burn patients, let alone the millions of patients predicted by some models (see Table 4-1). Pediatric burn nursing expertise in particular is extremely limited. Moreover, given the limited distribution of burn centers with pediatric care, in the event of a nuclear incident, transporting children to those centers may result in family separation and stress.
Bettencourt reiterated, however, that there is an opportunity to extend the reach of burn nursing expertise to other similar nurses. But this will require a few things, beginning with revisions to practice guidelines that take into consideration the nursing workforce. She mentioned a new type of dressing that can be kept on for about 1 week and that is being used a lot, particularly among children, as it reduces the number of visits (for outpatients) or dressing changes needed. When planning for a nuclear incident, she encouraged considering this type of strategy—tasks that can be done by other nurses as well, not necessarily burn nurses, and that conserve resources. In addition to new practice guidelines, telemedicine
or teleburn ICU capabilities could be really helpful. She also mentioned ABA’s Advanced Burn Life Support course for first responders, emergency room nurses, and burn nurses and physicians. Currently, much of the disaster training that most clinicians receive is through that course. She suggested adding nuclear event triage to the course. Finally, Bettencourt suggested thinking about opportunities where burn nurses could serve as consultants to the rest of the nursing community if one of these events were to occur.
Perspective of the American Burn Association: More on Burn Care as the Achilles’ Heel of a National Response to Thermonuclear Detonation
Jeng continued the discussion on burn care as the Achilles’ heel of a national response to a thermonuclear detonation and described some actions that ABA has taken recently that are relevant to a national response effort.
Crisis Standards of Care
First among these is ABA’s publication of peer-reviewed guidelines for burn care under austere conditions (Cancio et al., 2017a,b; Jeng, 2017; Kearns et al., 2016; Young et al., 2016). Jeng remarked that this was a difficult project to gestate and finally get into print but that, in his opinion, it is one of the more important things that ABA’s Committee on Organization and Delivery of Burn Care has done. It essentially serves as a “cookbook,” he said, with instructions for how to carry on effective burn care without resources.
Jeng encouraged other groups of experts to address crisis standards of care, get them in print, and get care providers talking about crisis standards of care and how to apply them gracefully in a cogent, deliberate, premeditated fashion.
Another component to crisis standards of care, he added, is the reality that under austere conditions most people who would otherwise receive what he described as “full-court press” care will be “black-tagged” and receive only comfort care. He called for more work on the restriction of care tables that are used to support decisions about who receives full care versus comfort care. In addition, because the restriction of care tables differs dramatically depending on the number of casualties, situational awareness is crucial. Jeng said that his greatest fear is that in the aftermath of a disaster of, say, 200 casualties, responders would act as though there had been 2,000 casualties, inappropriately black-tagging many individuals. Thus, he also called for improvements in real-time situational awareness.
Mass Casualty Burn Drills
In addition to its crisis standards of care work, ABA has also been very proactive about mass casualty burn drills. Jeng agreed with other workshop participants who had expressed that it is one thing to drill at a high level in the federal government but quite another thing to drill with people who are on the front line and will actually be providing the care.
He described a session at the ABA annual meeting in April 2018 where ABA had run participants through some of the Gotham Shield exercise. Jeng showed a snapshot of the session and pointed out the facial expressions of the participants. “They are not pretending,” he said. “There is a lot of anxiety in those faces.” Jeng and the other organizers had set up a civilian defense alarm, a siren, which they had run throughout the whole 1.5-hour session. During the exercise, many people had asked him to turn off the siren. He would explain to them that it was a way to try to address what he called the “deer in the headlights” issue, which he emphasized is very real. He and many others in the burn community have lived through mass casualties and seen it. People freeze and do not know what to do. “You drill because you do not want people to act like deer in the headlights when it really happens,” he said.
Breaking Down Silos
Jeng reflected on the fact that there are many people across the country who are working on mass casualty preparedness, yet there is also a lot of tribalism. He encouraged more efforts along the line of what ABA and RITN had begun working in the run-up to this workshop. They had scheduled a webinar to take place a couple of weeks afterward, where each organization would present to the other its response plans for a thermonuclear detonation. Then, from that platform, they will publish a practice guideline for combined care for radiation and thermal burns.
He called for trauma units in particular to break down their silos, as trauma professionals are really the “band leaders” for any big mass casualty event in the United States. “If we do not break down the silos, we are not going to make this country safer,” Jeng cautioned.
Potential Areas for Further Action
Jeng suggested four actionable items, two of which are free; the other two are not free but compulsory if the burn care community is to cogently address casualty levels at 20,000 or 200,000:
- Return burn training to the U.S. surgery curriculum. The first, free action is that burn training be returned to the general surgery curriculum in the United States. He reiterated that there has been no burn training for surgeons in the past 10 years. He explained that this is a consequence of not just the 80-hour work week but also financial constraints of academic medical centers and training programs that no longer have enough workforce to do burn rotations. Without any more burn surgeons being trained, he cautioned, “the ‘piper’ is going to have to be paid pretty soon.” The organizations responsible for the surgery curriculum include the American Board of Surgery, the American College of Surgeons (ACS), and the Accreditation Council for Graduate Medical Education.
- Arrange a summit to break down silos. Jeng’s second action, also free, is that the assistant secretary for preparedness and response, Robert Kadlec, summon the leaders of the ACS Committee on Trauma, ABA, and other relevant organizations to a “sit-down” in Washington, DC, to come up with a solution. In Jeng’s experience, when summoned by the executive branch, people show up. In his opinion, the executive branch does not use that power nearly enough. “Summon the people to break down the silos,” Jeng said. “Make them sit down, and let them know that not only the executive branch but the public has eyes on this group of people.” Later during the discussion period, James Ficke of Johns Hopkins Medicine responded to Jeng’s call for a summit by calling attention to the fact that this workshop itself was just such an event. “We are here,” he said.
- Invest in basic science and translational science research to keep second-degree burns from becoming third-degree burns. Jeng emphasized that the only way there is going to be any cogent response to 20,000 or 200,000 burn casualties is to pour “big money” into basic science and translational science research about how to stop partial thickness burns from progressing to full thickness burns. In other words, the “magic bullet,” he said, is how to keep second-degree burns from evolving, as they do, into third-degree burns. This is crucial because, by definition, second-degree burns (partial thickness burns) have the potential to heal without surgical intervention. In his opinion, this is a “fairly addressable” biological phenomenon.
- Invest in telepresence to act as an amplifier. Again, the only way that there is going to be a cogent response to 20,000 or 200,000 burn injuries that are potentially salvageable is to invest in telepresence to act as an amplifier. No amount of training of burn surgeons or trauma surgeons will create enough surgeons to deal
with that many casualties. Investing in telepresence will require also addressing infrastructure and state jurisdiction issues.
Diagnostic Laboratory Challenges After a Nuclear Incident
Although the topic of burn care would reemerge as a topic of primary concern in the open discussion with the audience at the end of this panel, in the meantime, the focus of the discussion shifted to other key challenges to building capacity within the health care system. The first of these is diagnostic laboratory capacity. Jones discussed how a nuclear incident would require some type of diagnostic tool to determine who needs what type of medical management and explained the differences between different types of tools.
Radiation Diagnostics Terms
Radiation involves both “exposure” and contamination. A person is “exposed” to radioactive materials through gamma radiation—for example, in an improvised nuclear device blast or from the “ground shine” particles in the dangerous fallout zone that Buddemeier described earlier (see Figures 2-3 and 2-4). A person is contaminated either internally through inhalation or ingestion of radioactive particles or externally when particles are actually on the body. This can occur from fallout—that huge mushroom cloud of debris that can fall 1, 10, 200, 2,000, or more miles away. Jones explained that both “exposure” and contamination result in an exposure to a dose of radiation.
Use of Biodosimetry Versus Bioassays
Jones further explained that the appropriate diagnostic test for someone who has been “exposed” to gamma rays but has no external contamination (i.e., no radioactive particles on the body or clothes) is biodosimetry. Biodosimetry determines past radiation dose from an “exposure” incident. Such exposure could result either from the initial blast or by walking through the ground shine (e.g., when first responders enter a dangerous fallout zone or the public leaves). In a mass response to a nuclear incident, the primary biodosimetry test that would be used would be lymphocyte depletion kinetics. It is a complete blood count (CBC) test. He noted that there is another type of biodosimetry test, chromosome analysis, but it has extremely limited capabilities in the United States. In terms of other applications besides a nuclear bomb, biodosimetry is limited for measuring both nuclear power plant and radiological dispersal device (RDD) “exposure” but effective for measuring “exposure” from radiation exposure devices (REDs).
For external contamination, diagnosis could be done with handheld monitoring or with people walking through a radiation portal. Although most of the radionuclides in a nuclear incident situation would be gamma, the same test can be used to detect alpha, beta, or gamma contamination.
For internal contamination (i.e., radioactive particles inside the body), bioassays are the preferred choice. The bioassay is a urine test. It determines past, current, and ongoing radiation doses from an internal contamination incident. Jones explained that a bioassay test is more effective than an external contamination test in the actual fallout zone because the initial radioactive particles close to the detonation are not very respirable. Further out, however, at 20, 30, 50, or 100 miles out, they are respirable, and people can inhale them from the debris falling on the ground. In terms of other applications besides a nuclear bomb, the bioassay is an effective diagnostic tool for measuring contamination from nuclear power plant fallout and RDDs but not for REDs. Jones explained that an RED is effectively a solid piece of cobalt-60 just emitting gamma radiation.
Following a nuclear incident, the initial priority would be to quickly determine who needs medical management and radioprotective medical countermeasures, which are available either in the Strategic National Stockpile or locally. Thus, Jones said, the preferred method of testing during the first 7–10 days would be biodosimetry. He cautioned, however, that most labs with biodosimetry capacity have only just-in-time inventory. For multiple reasons, from product expirations to the cost of floor space, most labs do not have huge stockpiles. If there are 500,000 people that need to be tested, preferably twice or more, that amounts to more than 1 million tests. He asked, “Do you have the blood tubes, the needles, the syringes, the actual CBC kits locally to do a million tests in 7–10 days? You need to think about that.”
Although bioassay testing can rapidly identify internal deposition of radionuclides and can quantify contamination, the capacity for bioassay testing is fairly limited. There is only one lab in the country, a CDC lab, that can do it. One of the issues with bioassay testing following a nuclear detonation is that the hundreds of radionuclides formed by the detonation itself constantly decay and re-decay. Thus, the tests are used only to detect and measure certain markers, such as cesium or strontium-90, based on what the U.S. Department of Energy and others are determining are present. Jones emphasized the importance of coordinating with state and federal epidemiology experts to determine the priority of bioassay testing.
One of the values of bioassay testing is that it provides information for population monitoring (i.e., based on the level of internal contamination). In many cases, bioassays provide negative test results for people who think that they may have been contaminated but are not truly contaminated, thereby relieving the stress on the public health system and overall health
care system. This raises another issue, which is that it is hard for many people to grasp the concept of a negative result. Imagine people living 20, 50, or 100 miles away from a detonation who are convinced that they are contaminated and are going to die from cancer in the next year or two. Jones referred to Yeskey’s earlier discussion of the large number of people showing up, demanding to be tested. He suggested that, in collaboration with local epidemiologists or other public health officials, perhaps only a subset of the community be bioassay tested to determine if the population really, truly has been exposed to a level of contamination that requires follow-up. Some communities may need follow-up; others may not. Conducting some bioassay testing and showing that a community is not more exposed than the rest of the unexposed population can reduce anxiety tremendously as well as reduce demands on the medical and public health communities.
Priorities
Jones concluded by emphasizing the need to think about how to prepare for the enormous amount of biodosimetry testing that will be required during the first 7–10 days. This is particularly important given the likelihood that the detonation would destroy all nearby diagnostic laboratory capabilities. The “good news,” he said, is that there are thousands of labs that do CBC tests. The question is, do they have enough blood tubes and enough CBC kits to run the number of tests needed? He suggested thinking about reception or assembly centers—that is, places where blood samples would be collected and then, from there, sent to labs in other parts of the country.
In addition to ensuring that there are enough resources to conduct the number of tests that will be needed, another challenge would be tracking multiple test results (i.e., per person) and ensuring that the people who are making decisions about care receive the data. Jones imagined people being tested in one place and then evacuated to another place or being tested in multiple places. How are those data going to be combined? What do the laboratories need to do to prepare for that scenario?
In closing, he said that 60–70 percent of medical decisions are based on a lab test. In a nuclear detonation scenario—a resource-scarce environment with limited medical countermeasures—the response community will need to be able to identify who really needs these countermeasures and who does not.
Radiation Injury Treatment Network
Case provided an overview of RITN and its potential role in a nuclear incident and discussed what he perceived as some of the most important
gaps, or priorities, in response capabilities based on his experience with RITN.
RITN is a group of 83 blood donor centers, cord blood banks, and cancer centers or hospitals with bone marrow transport (BMT) or hematology units that are working together to prepare for mass casualty incidents with radiological injuries that affect the marrow. Each year, RITN members are required to carry out a number of training and exercise tasks and to maintain institutional review board (IRB) approval of the RITN data collection forms and protocols. This is to ensure that that they are ready to receive casualties through the National Disaster Medical System (NDMS) in response to an incident.
Case described how RITN has had a lot of experience growing its network. It started with 13 centers or hospitals in 2006. He recalled a lot of resistance initially, particularly from administrators who questioned why a facility would want to receive these casualties. Case referred to the fear of contamination that previous speakers had discussed. In addition to fear, there were also concerns initially about who would pay for the care. But one of the biggest issues that they ran into initially was that most of the BMT or hematology units had only done annual evacuation drills. Most of them had no idea what NDMS was. Nor did they know what preparedness capabilities were in place at their own hospitals. “Since then, we have really engaged them into being involved in their preparedness activities at their hospitals,” Case said.
Gaps in Response Capabilities
The biggest gaps in response capabilities that Case sees in his work are fear and knowledge. “A lot of people are afraid of radiation,” he said, echoing many other workshop participants’ remarks. In addition, many medical professionals do not know how to care for people who have been exposed to radiation. Many have no idea what to do, he said. Most have heard of acute radiation syndrome (ARS), but they do not know what the signs or symptoms are, let alone how to care for it. Even within RITN centers, other than the primary physicians who work with RITN and perhaps one or two additional physicians who may be aware, the knowledge is minimal.
Regarding fear even among prepared providers, Case relayed how a few years ago, during an exercise in Salt Lake City, the trainees had had to pull patients off of a C-130 aircraft. Half of the patients had been actual kids pretending to be patients, and the other half had been dummies on stretchers. The first patient to come off the plane had been a pediatric dummy about 18–24 inches long. It had had a casualty tag on it. The trainees had brought the dummy into the hospital, where a strike team of 18 nurses and physicians had swarmed. Case said that they had been
excited. They had been planning this for months and had participated in a tabletop and other exercises. A nurse had picked the dummy up and started reading the casualty tag: “3-year-old patient, Caucasian, female, expected 10-grade exposure to radiation.” At mention of “exposure to radiation,” everyone, including the nurse, had thrown his or her hands up and run backward. “These are people that are involved in radiation preparedness, have had training on it, recently had training on it, and were expecting it, and they still freaked out,” Case said. Since that exercise, RITN has facilitated more than 650 additional exercises. He said that he would like to think that the situation is better today. Even so, in his opinion, there is a lot of work to be done in this area.
Apathy and priority are other major issues for Case. There are many people who assume that a nuclear incident is not something that will happen to them. Even in 2017, with the threat from North Korea, although there had been more interest, in Case’s opinion, still there had been a lot of people who had believed that the media was making a “big hubbub” out of nothing. RITN tries to counter this apathy by requiring each hospital to do a tabletop exercise every year. RITN provides the scenario and facilitates six Web-based exercises. It offers continuing medical education credits to draw in both physicians and nurses. Case said that the feedback they receive from health care professionals who have participated in the trainings is positive, with many people reporting that having participated broadened their awareness about other resources and activities. During the exercises, people working in BMT and hematology or oncology units interact with other people both inside and outside their hospitals whom they do not interact with on a day-to-day basis. The exercises break down barriers and build confidence.
Administrative barriers, which were especially problematic initially, remain a gap. When RITN approaches a hospital, it usually takes about 18 months for the hospital to join the network. Hospitals want to know what their return on investment will be. RITN provides a small stipend of $8,000 per year. While not enough to cover a hospital’s efforts, it is unrestricted, which Case said hopefully comes across as something worth more than something that has to be used for a specific cause. A number of RITN centers have tracked their time, reporting that they have spent about $15,000 in labor hours every year on RITN activities. So when approaching a hospital, RITN really has to convince the administration that it needs to participate—that it is going to have to become involved in the event of an incident and that it needs to be prepared. Case noted that about 89 percent of U.S. hospitals are part of NDMS.
Competing priorities are another concern, Case said. The current Joint Commission and Centers for Medicare & Medicaid Services (CMS) requirements are focused on an active shooter threat. Case mentioned having col-
leagues who have been on the road for 8 straight months conducting active shooter exercises around the country for schools, hospitals, day cares, and other facilities. “We are always going to have something that is the newest that is going to distract everyone’s attention and resources,” Case said. The challenge is how to do both or at least not interfere in accomplishing what is being pushed currently.
Dissemination is another gap. Everyone within the core group who is interested in this topic knows about it, Case said, and the information is not secret or hidden. It is readily accessible. Yet, Case said, “it does not seem to really get out there.” He commented on the lack of time that many people have to invest in keeping up and reading the resources that are available. On top of that is staff turnover. Getting people’s attention is a “never-ending cycle,” he said.
Role of Medical and Clinical Toxicologists in a Catastrophic Nuclear Emergency
Kazzi underscored the medical care challenges of a nuclear incident stemming from a very large number of victims combined with an inadequate number of health care providers and medical volunteers. However, he believes that there must be a way to close this gap. Telemedicine is one way. Medical toxicologists can also help. He described how medical toxicology serves as a resource—already they are involved with various things (e.g., linkages with RITN and other response agencies at federal, state, and local levels), and they provide specialized resources that support other providers and ensure the reach of technical knowledge to a wider area. He elaborated on many of the locations where clinical toxicologists operate, including as part of government and community planning, academic research and teaching, and poison control centers throughout the United States. Clinical toxicologists are also supporting the development of training courses for other providers to expand the specialized knowledge base around the use of medical countermeasures for radiation exposure and treatment of acute radiation sickness. Kazzi closed by highlighting the relationship between the toxicology resources and RITN, with 73 percent of RITN centers having a toxicology resource in the same geographic area.
A World Health Organization Perspective
An important lesson learned by the Global Outbreak Alert and Response Network from disasters, Ebola, trauma care in Syria, etc., is that self-deployers cannot be allowed to enter disaster areas, said Ian Norton, director, Emergency Medical Teams, WHO. It is not so much about individual expertise, he said. It is about how to plug into a system that can get
you there safely, Norton explained. In other words, good intentions are not enough. Capacity requires logistics and the power behind those logistics. It requires an organization that can carry individuals.
Several nuclear response teams in China came to mind for Norton and a couple teams in Southeast Asia, but that was about it. He wondered if there was a way to embed expertise into generic teams and then copy those teams. Furthermore, Norton emphasized the need for increased national ownership, both ownership of the capacity building necessary to meet the needs of large-scale incidents and also ownership by a country or community’s health leaders that they may face circumstances where they will not have the capacity to meet the need. In the latter case, Norton highlighted the importance of leaders owning the need to cut down on “red tape” required to properly use visiting resources in their communities. Norton pointed out the limitations of state-to-state license recognition in the United States as a significant challenge for response capacity, which he had heard in the day’s discussions. Other lessons learned from past disaster work include the need to send a message of hope, not nihilism, and the importance of “flow” in triage and lab testing. He suggested perhaps considering centers of excellence of care given that certain types of incidents, like mass burn events or an outbreak of a highly lethal disease like Ebola, have the capacity to overtax the resources of a single country. Discussing burn events, Norton echoed Jeng’s comments earlier in the session. The small absolute number of burn beds and burn specialists can mean that single events can quickly overtake the finite resources. In reflecting on the Ebola experience, Norton highlighted centers of excellence of care as a way to overcome fear and hesitation among providers. He remarked that knowing there was a center of excellence available was often a key factor in addressing the anxiety providers felt when working within a hot zone.
DISCUSSION: SHORTAGE OF BURN EXPERTISE
Following the panelists’ presentations, the panel fielded questions from the audience and from Evans. Almost all the questions and discussion revolved around the shortage of burn care expertise.
Art Cooper of the American Academy of Disaster Medicine remarked that it would be difficult for surgery residencies to include burn care given the difficult “educational milieu.” But a first step could be the excellent course offered by the ABA. In his opinion, instead of asking Kadlec to convene everyone in a room, he would suggest fundamental disaster education/training for everyone. “There are critical issues that the nation needs to address as soon as possible.” Jeng suggested some additional courses and agreed that the syllabus is too tight already. He suggested that, as a start,
at least all war surgeons receive some burn training. Many burn surgeons have military backgrounds.
This discussion prompted Evans to ask how people can be recruited into the system to help overcome some of these shortages. Kazzi pointed out that medical students need to be considered as well—they need disaster training. He noted that there is a CMS specialty course in medical toxicology.
The shortage in burn professionals applies to nursing as well, Bettencourt reminded the workshop. The number of burn nurses is related to the number of in-house burn patients. Thus, she reiterated that there are not a lot of burn nurses. However, there is an opportunity with advanced practice nurses1—having more of them might be a way to expand burn professionals.
Colleen Ryan of Harvard Medical College added that the shortage in burn expertise extends to other health care professionals as well, including therapists, pharmacists, etc. An entire team is required for burn care. She urged also extending the focus to rehabilitation and recovery.
When Evans asked the panelists what people themselves (i.e., non-providers) can do in the event of a burn given the shortage of burn expertise among health care providers, Jeng highlighted the role of bystander or buddy care2 and emphasized the need for oral rehydration, etc. Buddy care will make a huge difference in the event of 20,000 or 200,000 casualties, he said. It is already operational in the military, he said, referring to NATO Role 1,3 “buddy care” (i.e., point of injury care).
Ficke suggested that even Roles 2 and 3 could be expanded in hospitals and disaster drills conducted at these levels to really challenge the supply chain. Jeng agreed that disaster drills need to be brought down to the level of the responder.
In Jeng’s opinion, while there is a shortage of trained workforce, and there are ways to deal with it, the “right” problem is not how to increase the number of experts needed. Rather, what can be done to attract people to burn care by making it a viable life choice? What are the incentives? Jeng agreed that because burn care is a market-driven system, it is not financially viable to simply increase the number of burn centers. In his opinion, that is
___________________
1 An advanced practice registered nurse is a registered nurse educated at a master’s or postmaster’s level and in a specific role and patient population.
2Buddy care is short for self-aid and buddy care, a U.S. Air Force training program that provides all deploying personnel “knowledge and skills to minimize injury and prevent death or disability in deployed environments or home station emergencies.” See https://static.e-publishing.af.mil/production/1/af_sg/publication/afi36-2644/afi36-2644.pdf (accessed January 18, 2019).
3 Roles 1, 2, and 3 refer to various NATO standard levels of medical treatment facility capability. See https://www.nato.int/docu/logi-en/1997/lo-1610.htm (accessed January 18, 2019).
a “brick wall.” Bettencourt added that the same market effects are driving the shortage of burn nurses.
In Australia, there used to be a problem staffing Aboriginal community positions, Norton offered. To overcome this problem, it was decided that individuals would be preferentially selected from those positions to serve in overseas disaster response. The word spread quickly. Now recruiting to those communities is no longer a problem—they are competitive positions. “There are other things that drive people besides money,” Norton said.


















