2
Collaboration at the Intersection of Faith and Health
National Academies roundtable workshops are designed to open up a subject for consideration, said session moderator Gary Gunderson, vice president for faith and health at the Wake Forest Baptist Medical Center, professor of public health science at the Wake Forest University School of Medicine, and professor of faith and the health of the public at the Wake Forest University School of Divinity. This workshop was intended to open up the discussion of the potential for collaboration at the intersection of faith and health. He added that such collaboration must occur within the context—grounded in the Constitution—of the separation between structures of faith and public structures. (Highlights of this session are presented in Box 2-1.)
To inform the discussion of faith–health collaboration Gunderson shared a matrix from the African Religious Health Assets Programme that lists examples of tangible and intangible religious health assets relative to the continuum of proximal and distal health outcomes (see Figure 2-1). He encouraged participants to identify religious health assets that could be relevant to the population scale challenges that the roundtable is seeking to address. For example, a clinic, a prayer group, a recovery shelter, or a needle exchange program in a church are all both tangible and intangible assets and have health effects that are both proximal and distal. It is important to consider who owns or influences a religious health asset, he said, and the optimal alignment of that asset with other equally complex, relevant health assets. He also offered the term “communities of spirit” as a more inclusive alternative to “religion” when discussing these social structures of faith.
THE FOUNDATIONS OF FAITH–HEALTH COLLABORATION1,2
Continuing the theme of “opening up the conversation” about population health and faith-based assets, Prabhjot Singh offered a perspective on the foundations of faith–health collaboration. Singh is a physician, director of the Arnhold Institute for Global Health, and chair of the Department of Health System Design and Global Health at the Icahn School of Medicine at Mount Sinai.
Singh began by noting that in its 40-year history, Leonard Medical School at Shaw trained 400 doctors, among them Clinton Caldwell Boone, a 1910 graduate. After graduating, Singh narrated, Boone went to work as a medical missionary and pastor in the new Republic of Liberia, helping to bring high-quality care to a nation that was formed by formerly enslaved people. After noting the lack of dental care in Liberia, Boone traveled to New York City to be trained as a dentist as well. Boone built a congregation in Liberia, Singh said, and that congregation formed the
___________________
1 This section is the rapporteur’s synopsis of the presentation by Prabhjot Singh, and the statements are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
2 Singh’s presentation drew heavily on an unpublished lecture by Gary Gunderson, available at http://ihpemory.org/good-news-for-the-whole-community-reflections-on-the-history-of-the-first-century-of-the-social-gospel-movement (accessed January 24, 2019).
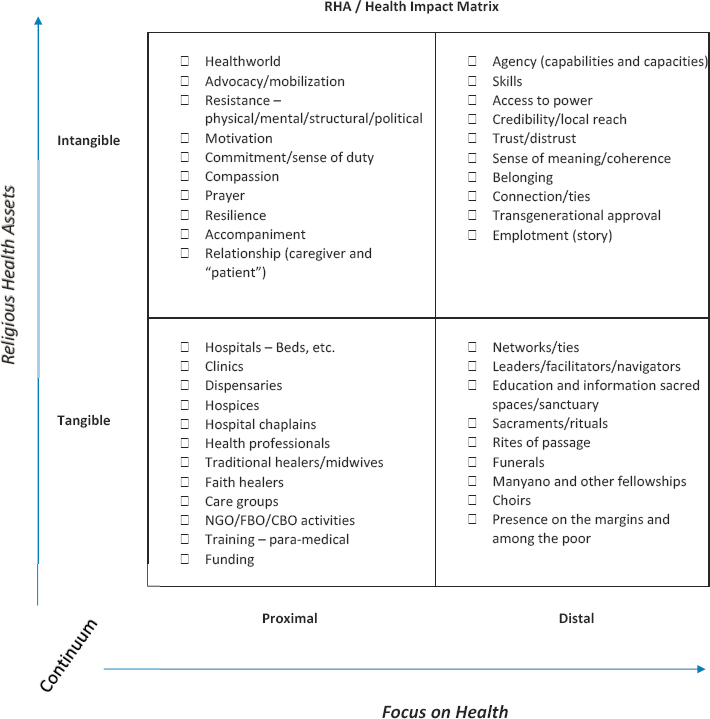
NOTE: CBO = community-based organization; FBO = faith-based organization; NGO = nongovernmental organization.
SOURCES: Gunderson presentation, March 22, 2018; developed by James Cochrane, African Religious Health Assets Programme.
base of social support for his medical work. The congregation served as a means to organize the community and to begin the challenging work of building institutions that could serve in both invisible and material ways, he said.
This story could have taken place in nearly any corner of the world, at any time in history, with any set of people who faced their human condition and realized that they needed to look beyond for the strength to move forward, Singh observed. Somehow, he continued, people find the spirit to organize, to act, and to build a better future. The resulting communities of spirit, to use the term of art introduced by Gunderson,
are “intangible and powerful field[s] of human energy that drive voluntary associations across the population, and in service of it.” By elevating the idea of communities of spirit, Singh said, all individuals can find themselves to be part of the discussion, regardless of how they come to it. Communities of spirit are often involved in building public health and health care institutions, he said, bringing the core values of justice and compassion together with scientific rigor, to improve population health. Singh highlighted the work of John Hatch (who was present at the workshop), who he said intuitively understood the concept of communities of spirit and built a movement that led to the development of community health centers across the country. Singh also referred to the foundational work on faith-based health assets that was carried out by James Cochrane (also present at the workshop) of the International and African Religious Health Assets Programmes. Cochrane surveyed countries across Africa to better understand how faith and health institutions productively aligned to serve people.
Singh described his own journey toward understanding the relationships between faith and health as unexpected. Singh said that after he earned a Ph.D. and an M.D. and completed postdoctoral work in economics, his thoughts were focused on deciphering diagnoses and solving problems, and he was not always thinking about the people in his care. That changed during his first year of medical residency when a patient named Ray died in his care. Singh lived in the same neighborhood in Harlem in New York City as Ray had, and Ray’s daughter invited him to the funeral. Singh shared the story of that experience, which changed his perspective (see Box 2-2).
Years later, Singh was motivated to write about his experience at Ray’s funeral after his own relationship with his Harlem neighborhood changed significantly. While out walking at dusk, Singh (who describes himself as a visible member of the Sikh faith tradition) was attacked by about 20 to 30 men who called him a terrorist and fractured his jaw. After sharing his story with local media, he said he was unprepared for the thousands of letters and e-mails he received that both expressed sorrow for what had happened and affirmed his identity. As a physician, he had felt that he was supposed to take care of a community, yet in this case, he felt the power of the community taking care of him and saw firsthand how the invisible bonds that connect individuals locally and nationally were made visible in the community’s response.
In an effort to learn more about those bonds, Singh traveled across the country. In Minneapolis, for example, he said he learned how a faith-based community organization, ISAIAH, had used a health impact assessment to change transportation policy. In Dallas, he learned how the Parkland Health Center worked with many faith-based organizations to develop
shared technologies that support their most vulnerable clients. Singh said he was inspired by these and other movements of people across the country, and how they are thinking about faith–health collaborations on a large scale.
To provide context for this scale, Singh said that in the United States, there are approximately 350,000 social entities identified as congregations. Faith identities are diverse and include some that do not identify as formal religions. To put the number of congregations in context, he said there are about 250,000 neighborhoods or geographic communities in America. Singh said that faith-based assets form a connective tissue of
social infrastructure that supports, connects, and protects neighborhoods, and that is also well-positioned to be a partner in health.
As public health and health care institutions endeavor to work in concert to improve population health, Singh said, they are finding common ground in neighborhoods. The science of population health is identifying how clinical and nonclinical factors shape people’s health. This increasingly includes an emphasis on the social context of people’s lives, including the availability of social support, financial stability, food security, and housing.
Although the science of population health can identify these social factors, public health and health care institutions cannot address them alone, Singh said. He added that, as the health sector grapples with decreasing life expectancy, the costs of health care (which can destroy people’s lives), income inequality, and social injustice are all growing, and “the moral voice of our allied health professions is difficult to hear.” Singh noted that the relationship between the health sector and faith institutions has not always been positive, with a history of sometimes disrespectful interactions. However, “people’s lives hang in this balance,” he said, and it is incumbent on both fields to acknowledge this history and deploy “the wisdom of faith and the methods of science” in facilitating dialogue and building partnerships.
In closing, Singh emphasized three areas for consideration at the workshop.
- Understanding the role of faith communities in the larger community. A better understanding is needed of the nature of the social connective tissue that faith-based assets have with their populations, not only within their congregations, but across other non-faith-based organizations and institutions in their communities, Singh said. He added that Robert Putnam and other social and behavioral scientists have “documented how the social fabric influences the ability to survive and thrive, and how faith communities play an important role in health in measurable and well-described ways.” Health sector institutions need to embrace new approaches and technologies that can help them be better partners.
- Recognizing the value of faith-based assets for health. The growing understanding of faith-based assets can be used in practical ways, Singh said. There are many examples of faith–health partnerships across the nation that call for larger investments in children, the dismantling of racist housing policies in neighborhoods, the protection of undocumented immigrants, and helping to address social isolation and loneliness among older adults.
- Communicating relevant health messages through trusted partners. It is important to work with faith leaders to ensure that key
- public health messages and health care recommendations are more relevant to communities of spirit. For example, the polio eradication campaigns worldwide required deep partnerships with faith leaders to reach the last mile. Today, misinformation about health spreads faster than evidence-based information, he said, and partnering with congregational leaders is key.
The workshop presentations will provide practical, tangible examples of important partnerships forming between faith communities and health institutions, and of the role of policy makers who are forging a new dialogue while respecting the separate roles of faith and government, Singh said. He encouraged participants to identify practical insights they could take back to their respective communities, and to identify what research is needed to better understand faith–health relationships and build better collaborations.
DISCUSSION
In the discussion that followed, participants considered the role of faith-based assets in bringing an understanding of the whole individual and their context to the health arena. Participants also discussed approaches to establishing genuine partnerships among health and faith organizations and raised specific issues around religious exemptions to vaccines and overcoming the barriers to providing mental and behavioral health services.
Understanding the Whole Person and Their Context
Matt Guy with the Communities of Spirit Hub of 100 Million Healthier Lives highlighted the general lack of focus on the individual person in health care, despite current patient-centric efforts, and the role of faith in focusing on the individual. Singh agreed that this is a foundational concept for the workshop dialogue. He shared that the most profound result of his speaking with people in faith communities was learning to understand the whole person and their context. He also recognized that there are real limits to being able to develop that understanding in his role as a health professional. This is a journey of humility, he said—of recognizing that everyone holds a piece of the puzzle and no one can see the whole picture. The challenge is to design institutions and systems that can provide pathways to understanding those individual perspectives. This is an opportunity to see how each puzzle piece fits into the bigger picture.
Eva Powell of CommonPurpose Health noted an opportunity for the faith community and traditional health entities to work more collabora-
tively on a macro level as well. What happens at the individual level is constrained by decisions that have been made around investments and priorities, she said. When a service is not available for an individual, it is the direct result of decision making on behalf of people who are often not at the table. She suggested that discussion is needed on how the faith community can be active in decision-making circles in order to provide input to help hospital boards, public health entities, and legislatures.
Angeloe Burch of the Interdenominational Ministerial Alliance of Durham emphasized the need to have the “right conversations” that demonstrate an understanding of the specific context in each case. For example, Missionary Baptists and Primitive Baptists are split over the issue of conducting missionary work, and understanding this is important. It is also important to consider how to best communicate with different populations. Regarding vaccines, for example, African Americans are often wary of immunization due to a long history of abuse and unethical treatment that has led to a lack of trust of the health care system. Finally, Burch noted, health providers need to acknowledge that patients know themselves better than a provider can. Providers interact with patients briefly, and having the right conversations with the patient is critical to providing quality care for that individual.
Singh agreed with the need to be aware of the historical and personal depth of these issues, and to build the dialogue needed to move toward a common purpose. In this regard, Gunderson raised the concept of “healthworlds,” which was proposed by Cochrane and colleagues. James Cochrane, professor from the University of Cape Town in South Africa and co-director of the African Religious Health Assets Programme, expanded on the concept of healthworlds.
An early research project done by the African Religious Health Assets Programme for the World Health Organization (WHO) was focused on mapping assets owned by religious entities that might have clinical relevance. Cochrane said that WHO was interested in tangible assets that could be measured, such as personnel, equipment, materials, and transportation. This information was intended to inform decisions by national health ministries about where to prioritize resources, including finances and personnel. It became very clear to researchers that there was a need to also understand intangible networks and assets. In the philosophical and scientific literature there is a concept called the lifeworld, Cochrane said. The lifeworld is the taken-for-granted assumptions that affect the way people make decisions and behave in the world. These go far beyond the rational, calculated decisions that one makes between benefit and cost. Unless these elements of the lifeworld are understood, it is not possible to understand what is happening with the applicable technical, scientific, and instrumental capacities. Cochrane highlighted treating patients
with HIV in Southern Africa as an example. Medications are available, but there are complex dynamics that impact whether and how people take their medicines. For example, said Cochrane, if a patient with HIV receives medication and has a sibling or parent who is HIV positive but does not have medication or is unable to even acknowledge his or her own status, the patient will share their medication with them, which negatively impacts the medical protocol designed for the patient.
Expanding on the notion of lifeworld, Cochrane and colleagues coined the phrase “healthworld” to encompass the way that people construct their own sense of health and then behave accordingly (Germond and Cochrane, 2010). Every individual makes decisions based on whether they like the advice they received or not, or whether they trust it or not, Cochrane said. Even when an individual accepts the medical advice they receive, they frequently choose other alternatives anyway; one field where this happens not infrequently is cancer treatment. Cochrane and colleagues have argued that it is critical to understand the interface between the self-understanding of individuals and how those individuals are embedded in families with traditions, cultures with traditions, and religions with traditions, and the impact of this interface on the practice of health science.
Establishing True Partnerships
Ella Auchincloss of ReThink Health (participating via webcast) asked about approaches that clinical organizations might take in reaching out to and engaging faith-based organizations so that the faith-based organizations are true partners and not simply venues or assets. Drawing on his prior experience working at the Carter Center, Gunderson said that one theory of collaboration is built around limited domain collaboration, in which the area of partnership is not the sovereign space of either partner. The art of creating that collaborative space, he continued, is to define the limited domain in such a way that it has both integrity and potential efficacy for the goals of all of the partners. The limited domain also excludes aspects that are not specifically included. In other words, it is a safe space where the partners know that they are not buying into every possible implication of the collaboration; it is restricted to the limited domain (Gunderson, 1997).
Religious Exemptions to Vaccines
Robert McLellan, chief of occupational medicine at the Dartmouth-Hitchcock Medical Center in New Hampshire, raised the issue of exemption from vaccination based on religious or deep philosophical commit-
ment, and suggested that this is one very practical area where there is friction between the faith and health communities. He noted that public health law is constructed for the good of the population and sometimes finds itself at odds with the principle of individual autonomy. He reiterated Singh’s comment about how health organizations need to work with communities of faith to connect with people in relevant ways. Singh agreed that this issue around vaccination is a vital, practical area of work. Gene Matthews of the Network for Public Health Law and the University of North Carolina at Chapel Hill said that the challenge is how to encourage, but not coerce, those who are hesitant to receive vaccines. He mentioned recent research that found that parents who were hesitant to have their children vaccinated scored the moral value of liberty as being very important to them (i.e., they do not want the government telling them what to do). He suggested that one approach might be to emphasize to them the need to be able to free their children from having vaccine-related illnesses. Another moral value emphasized by parents hesitant to vaccinate was sanctity (e.g., not polluting one’s body). A different approach would be needed to encourage these parents.
Meeting Mental and Behavioral Health Needs
Mylynn Tufte, state health officer for North Dakota, shared that the governor and first lady of North Dakota have been focused on efforts to reduce the shame and stigma associated with addiction. She added that there is limited access to behavioral health services in rural areas of the state. She asked about leading practices or evidence related to tapping into faith-based assets for mental and behavioral health as they relate to decreasing the shame and stigma of addictions. Gunderson called on Melissa Stancil of CareNet Counseling to share an example. CareNet is an affiliate of Wake Forest Baptist Health, Stancil said, specializing in spiritually integrated psychotherapy and community-based work. The challenge of meeting behavioral health needs in rural settings can be daunting, she said. Collaboration with community partners usually starts with a mutual education process, she explained. People want to help, she observed, but they just do not know how. There is a lot of misinformation about substance use disorders, even within the health care professions, and a lot of internalized stigma in the health care industry around working with individuals who are living with addiction. Trust is essential, and CareNet works with congregations on educational events and relationship building with the goal of developing sustainable partnerships. There are also specific best practices that can be shared (e.g., needle-sharing programs, leveraging unused facilities for addiction recovery services). Amy Moyer of Kaiser Permanente said that Kaiser is looking to work with faith-based
organizations as an integral part of a collective impact plan, working with synagogues, temples, churches, pastoral associations, and others to understand the total health of the community and the social determinants of health. She expressed interest in hearing more discussion on how to formulate private, nonprofit, and governmental relationships around faith-based initiatives in mental health.
This page intentionally left blank.












