Speakers in the workshop’s final session offered perspectives from obesity treatment and health care settings. David Fukuzawa, managing director of The Kresge Foundation’s health program, co-moderated the session with Jennifer Fassbender, director of program initiatives at the Reinvestment Fund.
HEALTH EQUITY BY DESIGN: REENGINEERING THE DELIVERY OF PRIMARY HEALTH CARE TO REDUCE DISPARITIES IN OBESITY CARE
Melissa Simon, George H. Gardner Professor of Clinical Gynecology at the Feinberg School of Medicine, Northwestern University, spoke about reengineering the delivery of primary health care to reduce disparities in obesity care. She began by listing basic elements of architectural design, highlighting such concepts as balance, space, and scale and proportion, and described this discipline’s methodical and iterative process for creating functional outputs. She compared this process to the designing of primary care, including health professionals’ training, the spaces where primary care delivery occurs, the flow of the electronic health record, the structure of partnerships between communities and primary care, and the nature of laws concerning health care delivery and reimbursement. According to Simon, the design of places and relationships in primary care impacts health equity upstream, downstream, and in between.
Many obesity interventions in primary care settings help families circumvent obstacles, Simon continued, but most programmatic interventions are only temporary solutions. Short-term interventions, she elaborated, are generally characterized by a high “dose” and intensity, but they end rather abruptly, and little follow-up information is gathered. Moreover, she added, there is a lack of knowledge about how multiple interventions could merge and work cohesively to improve longer-term outcomes.
Simon highlighted the complexity of integrating obesity interventions in primary care settings. She detailed reasons for this complexity, including the need for multiple, simultaneous strategies to address the many interrelated causal factors involved and the host of barriers related to healthy lifestyle behaviors and their associated social determinants to be overcome. Additional factors include time delays, she pointed out, such as the 1- to 2-year lag for metabolism to stabilize after caloric intake changes and the years-long processes of maturing programs and enforcing changes, let alone the ability to measure the impact of those changes. Most important, she insisted, the system of individual-level and society-wide factors that influence obesity is dynamic.
Simon reviewed the U.S. Preventive Services Task Force (USPSTF) guidelines for obesity screening, highlighting its two B recommendations:
that clinicians screen for obesity in children beginning at 6 years of age and offer or refer them to comprehensive, intensive behavioral interventions that can promote improvements in weight status, and that clinicians offer or refer adults with a body mass index of 30 or higher to intensive multicomponent behavioral interventions (USPSTF, 2017, 2018). But how accessible are such interventions, she asked, especially for underserved or isolated populations? Despite a reasonable degree of certainty that screening for obesity in adults has a moderate net benefit and that intensive behavioral interventions can lead to meaningful weight loss and improvements in physiological risk factors, Simon continued, direct evidence about such interventions’ effect on long-term health outcomes is inadequate.
Simon expressed the caveat that the high level of rigor in study design and the high threshold for sample size that are required for evidence to be considered in the development of USPSTF guidelines make it difficult to find eligible studies in which populations that are underserved and/or underrepresented are included. Therefore, she reasoned, the guidelines are not necessarily applicable to all populations. This lack of representation in research has historical roots, she suggested, emphasizing that the design of research can perpetuate inequities.
Simon briefly reviewed evidence on effective diet and physical activity strategies for addressing obesity in primary care, underscoring that without a long-term plan, patients “overwhelmingly” regain the weight they lose, and that behavioral therapy and physical activity are key to maintaining weight loss. High-intensity interventions are most effective, she asserted, echoing earlier presenters’ points that such interventions are more difficult to access, especially for certain populations. She called for better training and more resources to help physicians deliver counseling on healthy eating and exercise during office visits, and emphasized the importance of a supportive primary care framework that recognizes a patient’s environmental and community influences while addressing the other priorities for care. How to address all of these issues for each patient effectively is the “$50 million question,” she remarked.
Reducing stigma and building trust with patients is a precursor to effective primary care prevention and treatment, Simon stressed, urging primary care providers to recognize and control their stereotypes and implicit biases about obesity (Phelan et al., 2015; Schwartz et al., 2003; Tomiyama et al., 2018). Key knowledge about obesity’s pathophysiology and social and environmental determinants can help change the treatment approach, she proposed, as can training to increase providers’ empathy, alter perceived norms, and educate on patient-centered approaches and welcoming health care environments.
Shifting to discuss obstetrics care, Simon noted that more than half of women in the United States exceeded recommendations for gestational
weight gain (GWG) in 2010–2011 (Deputy et al., 2015; IOM and NRC, 2009). She briefly reviewed the varying global guidelines for GWG, noting a research challenge that GWG is considered both an exposure and an outcome (IOM and NRC, 2009; Kominiarek and Chauhan, 2016). Pregnancy is an ideal time to intervene, she maintained, because of the high frequency of and patient engagement in care, and because it is considered a “window to future health” for both mother and baby. She cited as an example that maternal weight gain in excess of pregnancy guidelines is related to daughters being classified as overweight 40 years later (Houghton et al., 2016). Simon acknowledged that the available data have not yielded clear strategies for modifying the delivery and type of perinatal care that can impact GWG and maternal morbidity, but noted that additional trials are under way, including one that integrates social determinants of health into traditional prenatal care. She concluded by stressing that health inequities “don’t just happen,” arguing that eliminating disparities “really does take a village” and is about modifying the architecture and design of health care policies, clinical care settings, reimbursement, and provider training.
LESSONS FOR ACHIEVING EQUITY IN HEALTH CARE SETTINGS FROM NONOBESITY FIELDS
Marshall Chin, Richard Parrillo Family Professor of Health Care Ethics in the Department of Medicine, The University of Chicago, shared insights from nonobesity fields with relevance for achieving equity in health care settings. The equity goal, he said, is to move the national numbers on disparities, such as those presented in the Agency for Healthcare Research and Quality’s National Healthcare Quality and Disparities Report (AHRQ, 2016). Chin presented five lessons derived from his research with multilevel interventions designed to reduce health disparities and his experience conducting health equity programs.
First, Chin began, there is no “magic bullet” solution because context matters. He highlighted an organization’s historical origins, financial structure, and political environment as examples of contextual factors that affect how interventions play out. He explained that organizations value a menu of evidence-based interventions that they can tailor to develop their own solutions. A sobering reality, he continued, is that there are few common themes as to what works to reduce health disparities in health care settings. He then listed six themes derived from a review of more than 400 intervention articles: multifactorial interventions that target different drivers of disparities; culturally tailored quality improvement approaches; team-based care, especially nurse-led interventions; engagement of families and community partners; involvement of community health workers; and
interactive skills-based training with patients (Chin et al., 2012). He displayed a model of the multiple levels for potential clinical and policy actions to reduce disparities (see Figure 6-1).
The second lesson, Chin continued, is that achieving equity is a process. He outlined a roadmap for reducing disparities, highlighting six of its concepts (Chin et al., 2012). First is to create a culture of equity, which he said goes beyond cultural competency trainings and stratifying of performance measures by race/ethnicity. In the business world, he observed, it is said that “culture eats strategy for breakfast.” He explained that even the best programs and strategies will not be successful if people do not care about equity. He identified the second and third concepts as embedding equity interventions as an integral part of quality improvement (QI) infrastructure and processes, and the fourth as designing interventions with an equity lens. He remarked that organizations often use the same generic QI intervention that improves care for everyone without tailoring the intervention to different populations. He enumerated as the fifth and sixth concepts implementing, evaluating, adjusting, and sustaining interventions.
Identifying the root causes of inequity is critical for diagnosing the problem and developing solutions, Chin stressed, declaring that it is an iterative, complex process with no substitute for talking with the affected patients and communities to fully understand their lived experiences. He referenced the Consolidated Framework for Implementation Research,
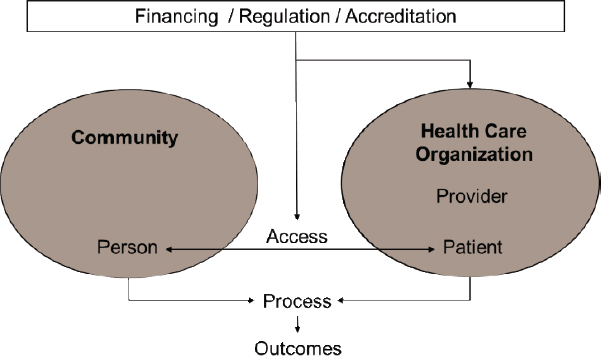
SOURCES: Presented by Marshall Chin, April 1, 2019 (Chin et al., 2012). Reprinted with permission.
proposing that stakeholders consider each of its elements when planning interventions for real-world settings (Damschroder et al., 2009).
Chin went on to discuss the third lesson: the importance of addressing social determinants of health. He implored health care organizations to go beyond addressing a patient’s social needs through screening and referrals to also having what he called “free, frank, fearless” discussions about such underlying structural drivers as racism, colonialism, and social privilege. According to Chin, people of all backgrounds can contribute to this discussion if they are committed to the issue. “We really cannot get to where we need to go unless we have these discussions as a country,” he asserted, acknowledging that the conversation is difficult. Power is the issue, he suggested, defining it as control over resources, the historical narrative, and the framing of the health disparity issue as one of personal responsibility versus structural drivers. He urged people of all backgrounds to contribute to the discussion.
The fourth lesson discussed by Chin is to address payment and incentives. He advocated for a business case to address equity, pointing out the policy gap between U.S. health agencies’ “rhetoric” about valuing health equity and a lack of policies to support and incentivize the pursuit of this purported value. He suggested three policy goals to help fill the gap: explicitly design quality-of-care and payment policies to achieve equity, hold the health care system accountable through public monitoring and evaluation, and support it with adequate resources. He shared three examples of the National Quality Forum’s recommendations for incentivizing the reduction of health disparities and the achievement of health equity (NQF, 2017): (1) emphasizing accountability, including clinical performance measures stratified by race, ethnicity, socioeconomic status, disability status, etc.; (2) redesigning payment models to support health equity, such as by funding community health workers and integrating health and social services; and (3) tailoring quality improvement and funding for the safety net.
Chin highlighted a new Robert Wood Johnson Foundation program for advancing health equity by leading transformation in care, payment, and systems. He described its goal as aligning state Medicaid agencies, Medicaid managed care organizations, and front-line health care organizations to achieve health equity because, he insisted, no single group can do it alone.
The fifth and final lesson is to frame equity as a moral and social justice issue, which Chin argued is a prerequisite for success with any of the technical solutions discussed during the workshop. He quoted Martin Luther King, Jr.’s 1966 statement that “of all the forms of inequality, injustice in health is the most shocking and the most inhumane,” and referenced philosopher John Rawls’s concept of the “veil of ignorance.” The latter theory, Chin explained, postulates that the most fair, just laws in society would be created if people did not yet know what their race/ethnicity or
socioeconomic position would be, because once that determination has been made, it is difficult to avoid self-interest.
Chin then displayed a conceptual model for achieving health equity that illustrates its primary drivers as culture, history, and values (see Figure 6-2). “There are only so many things you can incentivize,” he said, asserting that intrinsic motivation is essential for framing health equity as a moral and social justice issue.
Chin shared an example of admirable intrinsic motivation from a site visit with one of his organization’s grantees in Idaho—Clearwater Valley and St. Mary’s Hospitals and Clinics. The grantee’s employees develop their own personal mission statement, he said, which is inscribed on a badge worn alongside their identification badge. He argued that, despite living in a politically divided country, health equity can be a common-ground issue even for people of disparate political ideologies. In closing, he shared a quotation from one of his publications: “Leadership matters. It is our professional responsibility as clinicians, administrators, and policymakers to improve the way we deliver care to diverse patients. We can do better” (Chin, 2014).
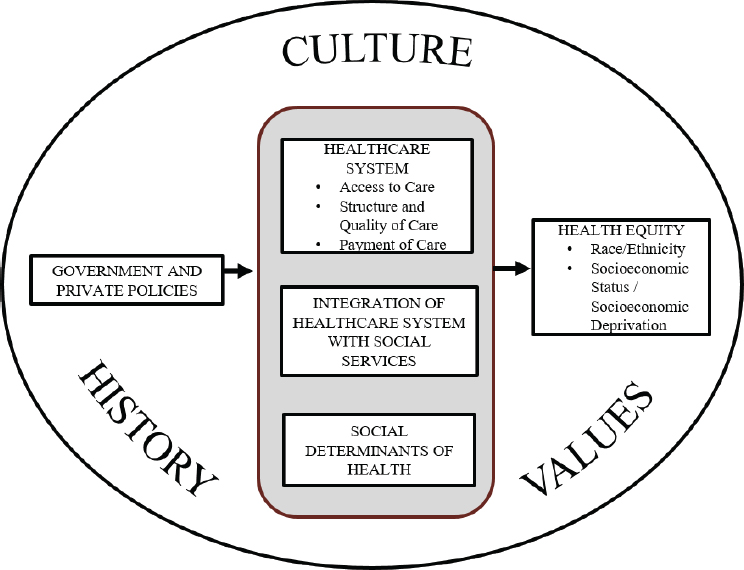
SOURCES: Presented by Marshall Chin, April 1, 2019 (Chin et al., 2018). Reprinted with permission from Elsevier.
DISCUSSION
During a brief discussion period following their presentations, Simon and Chin answered participants’ questions about health care provider training, caregivers as health care partners, and an infrastructure for identifying and allocating resources for addressing health equity issues.
Health Care Provider Training
Simon was asked for suggestions for formats to help train health care providers in reducing bias. She listed examples that included engaging in role play; conducting implicit association tests with students, fellows, or trainees to assess implicit attitudes; intentionally infusing health equity into all curricula; and achieving buy-in from university leadership for actively addressing health equity.
Caregivers as Health Care Partners
A participant proposed that caregivers be included as collaborative partners in health care systems given their role in rendering care. Simon agreed, advocating for the inclusion of significant others or partners as well. For cultures in which family plays a key role in decision making, she continued, care provider teams are faced with determining how best to integrate family members. She pointed out that some medical specialties, such as palliative medicine and oncology care, have suggested how to do this, and obstetrics care in group provider settings allows patients to bring a support person to appointments. But this practice has not been shown to improve outcomes for every obstetric outcome of interest, she said, noting that there is still a long way to go in terms of practice and integration.
Infrastructure for Identifying and Allocating Resources to Health Equity Issues
A participant remarked on the lack of an integrative infrastructure requiring a systematic, accountable way of identifying health equity issues and allocating resources to address them. Community health planning may be the missing link, he suggested, referencing this discipline’s history of developing community certificates of need and making recommendations to political leaders for the allocation of resources to address the disparities in an efficient, effective, and equitable way.
Chin reiterated his presentation’s appeal for health equity policies incorporating accountability and adequate funding, suggesting that such policies could be pursued using a free market approach, regardless of the political environment of the day. Conversations about values using strategic messaging and framing are critical, he asserted, to influence people to care about health equity as a moral issue.
This page intentionally left blank.










