6
Creating Healthy Living Conditions for Early Development
MEETING FUNDAMENTAL NEEDS TO SUPPORT PRENATAL AND EARLY CHILDHOOD DEVELOPMENT
I am trying to get gainful employment. . . . We all have that same thing in common of trying to do better for ourselves, trying to turn things around and do the right thing. But it’s hard, it’s hard because the resources that are available to us—we don’t know about them, we are not aware of them, we don’t know how to connect to the resources that are available to us. —Parent on caregiver panel1
As described in earlier chapters, a child’s most proximal influence in early development is the family unit, specifically the primary caregiver. Chapter 4 provides an overview of what children need from caregiver relationships and the critical role those relationships play for children to have the opportunity to flourish and thrive. However, these relationships do not exist in a vacuum, and neither do families—they are shaped by the social determinants of health (SDOH), as laid out in Chapter 3 (see also Figure 1-9). Families exist within the context of their communities, and all children need safe and healthy communities that promote optimal development. Healthy communities continuously create and improve physical and social environments and expand community resources that enable people to mutually support each other in daily life and in developing
___________________
1 This quote is from a public meeting of the committee, held on October 1, 2018. The meeting webcast is available at www.nationalacademies.org/earlydevelopment (accessed July 29, 2019).
to their maximum potential (CDC, 2009). Chapter 4 also makes the case that it is essential to mitigate caregiver stress so that caregivers have the capacity and supports to care for their children and to serve as buffers against adversities. (See Box 6-1 for an overview of this chapter. See Chapter 2 for a brief discussion of the biological mechanisms of buffering and Chapter 3 for discussion of the importance of stable and nurturing relationships.)
This chapter addresses the fundamental needs of families and children that are critical to achieving health and well-being. In the report conceptual framework (see Figure 1-9), these are the “healthy living conditions” situated in the second outermost circle, along with health systems and services (see Chapter 5) and early care and education (ECE) (see Chapter 7). Healthy living conditions are made up of the SDOH, or
more specifically, the social, economic, environmental, and cultural drivers of health and well-being. These determinants are interdependent, and together, they create conditions that influence child health and the ability of a caregiver to fulfill a child’s basic needs for healthy development.
Based on the core scientific findings in this report, this chapter seeks to address the challenges—for example, the barriers highlighted in the quote that opened this chapter—caregivers face with respect to securing economic stability and a safe and healthy living environment during the prenatal through early childhood periods. The committee reviewed promising community-level models and policy opportunities that focus on key neurobiological and socio-behavioral mechanisms needed for healthy development that yield the greatest impact to both mitigate and forestall the impacts of early life adversities on health.
Systems changes are needed to target multiple SDOH that shape early development and well-being. Systems that children interact with are most effective when they take into account developmental science and evidence when they are created, thereby meeting children’s developmental needs. There are changes that could be made based on this science to existing policies that would make them more responsive to the needs of children. The recommendations in this chapter aim to provide predictability and security in the lives of children and their families through ensuring economic stability and a healthy and safe living environment. While the chapter takes a social determinants approach to addressing early living conditions, it should be noted that there are some important contextual factors that are not discussed here. For example, research shows that factors such as public transit, access to parks and green space, and mass incarceration all shape inequities for children and families (see, for example, NASEM, 2017; Wildeman and Wang, 2017); however, these areas of programs, policies, and systems are not the focus of the solutions discussed in this report. The primary focus here is on the programs, policies, and systems changes that the committee has identified as having the most evidence and promise for improving health and wellbeing outcomes for children and their caregivers, in addition to reducing disparities. The chapter includes discussions of the existing evidence and committee recommendations for solutions to address economic stability and security, food security and nutrition, housing, neighborhood conditions, and environmental exposures and exposure to toxicants.
ECONOMIC STABILITY AND SECURITY
Children’s well-being and future health outcomes are strongly related to family income, and as the review in Chapter 3 shows, poverty is associated with significant detrimental effects on children’s health, development, and well-being. A systematic review of the literature concluded that the evidence supports the conclusion that the link between income and child outcomes is causal; that is, “money makes a difference in children’s outcomes” (Cooper and Stewart, 2013). The study also finds evidence that money in early childhood is important, particularly for cognitive outcomes. Thus, reductions in childhood experiences of poverty, and increasing the resources available to families to meet their basic needs, would be expected to improve children’s health and developmental outcomes.
Given the substantial evidence that money matters, an important factor in reducing health disparities in early childhood is to ensure that families with young children have sufficient resources. As the Council of Economic Advisers points out, current policies and public programs provide much less support for families when children are young compared to when they are school age, despite the needs and lower financial wherewithal, on average,
of families with younger children (CEA, 2014). In this section, the committee reviews the evidence about U.S. safety net programs that are intended to increase financial resources of families with children through cash transfers or tax credits. In the following paragraphs, the committee assesses programs that provide targeted benefits to address food or housing shortfalls and programs to address neighborhood conditions. To retain a reasonable scope, the focus is on the largest safety net programs run by federal and state governments that are offered to families with young children or pregnant women, while acknowledging that local governments, nonprofit organizations, and religious organizations also provide resources to help families in need.
Furthermore, the committee acknowledges the importance of providing parents and other caregivers with pathways to sustained economic security, such as educational opportunities and workforce development training. Chapter 3, for example, highlights the salience of parental educational attainment and household income as determinants of child health, wellbeing, and educational outcomes. Thus, an approach that enhances educational and economic opportunities and ultimately financial sustainability for caregivers would benefit children and families. Community-based programs that promote economic well-being for families are one promising avenue for advancing economic security. One such example is the Dudley Street Neighborhood Initiative’s Fair Chance for Family Success—funded by the Boston Promise Initiative in partnership with the Family Independence Initiative. This is a peer-to-peer financial literacy and learning program, which reports improved outcomes for participating families in terms of amount of money in savings accounts, checking accounts, total assets, and subsidy income (NASEM, 2017). Similarly, programs that enable workforce participation or retention could also help families get on a path to economic security. WorkAdvance is one program that allows employers to place individuals with moderate job skills into training programs for specific sectors that have high demand for local workers (NASEM, 2019). Evaluation data for this program suggested large increases in workforce participation, training completion, and credential acquisition at a 2-year follow-up (Hendra et al., 2016). While these types of programs are relevant to promoting healthy early development, the committee’s approach in this report was to limit its scope to program, practice, and policy changes that had the strongest evidence for direct impacts on children and their well-being. Therefore, the committee did not include in-depth discussion of these types of economic and workforce support programs for caregivers in this chapter.
Policies and programs aimed at reducing the impact of poverty on children’s health and well-being may provide cash benefits (directly, or indirectly through tax credits) or noncash or “in-kind” benefits, such as vouchers to buy food or housing. Alternatively, some programs directly provide food, housing, or education. This section first describes antipoverty programs designed to increase the level of (cash) resources families have,
focusing on the two largest direct cash grant programs, Temporary Assistance for Needy Families (TANF) and Supplemental Security Income (SSI), and then on tax credits, focusing on the Earned Income Tax Credit (EITC) and the Child Tax Credits (CTCs). Next, paid parental leave is discussed as another option for supporting families’ needs when children are young. The committee examined the evidence on the extent to which these programs (1) increase cash resources and thereby reduce poverty, (2) are associated with improved child health and development, including prenatal and birth outcomes, and (3) are associated with longer-term health,
educational, and economic outcomes. Throughout this section, the committee explores concerns about the strength of the evidence and the possibility of unintended consequences of these programs (which might directly or indirectly impact children’s health). The committee’s conclusions and recommendations build off those made in the National Academies report A Roadmap to Reducing Child Poverty (NASEM, 2019), which provides a thorough analysis of the evidence for approaches to alleviate child poverty. Box 6-2 contains the conclusions from that report that are relevant to and informed this committee’s conclusions and recommendations.
Cash Assistance Programs (TANF, SSI)
TANF provides cash assistance and sometimes other supports, such as job search support or child care subsidies, for eligible families with dependent children. Because TANF is a block grant, each state establishes its own eligibility rules, determines the type and amount of assistance to be provided, and sets other requirements and services (within broad federal guidelines). TANF participation is time limited and is intended to promote economic self-sufficiency, work, and marriage (HHS, 2012). In fiscal year 2018, 1.2 million families and nearly 2.4 million children received TANF assistance on average each month (ACF Office of Family Assistance, 2019). TANF has been a shrinking component of the nation’s social safety net for children since the passage in 1996 of the Personal Responsibility and Work Opportunity Reconciliation Act, when Aid to Families with Dependent Children (AFDC) was replaced by TANF. In 1996, 68 percent of low-income families with children received cash assistance through AFDC. In contrast, only 23 percent received TANF cash assistance in 2016 (CBPP, 2018a). In addition to reaching fewer low-income families, the size of grants has fallen in inflation-adjusted terms in most states. TANF benefits for a family of three in the median state were $447 per month in 2018 and have fallen by 20 percent in inflation-adjusted terms since 1996 (CBPP, 2018a). Overall, TANF is much less effective at reducing the severity of poverty than was the AFDC program: 18 percent compared to 56 percent of children moved out of deep poverty after receiving TANF versus AFDC grants (CBPP, 2018a).
Additional sources of direct cash support for families include the SSI for children and U.S. Social Security Administration (SSA) programs. Children “with physical or mental condition(s) that very seriously limit his or her activities” and that last for more than 1 year may qualify for SSI payments, which families can use to pay for basic needs, such as food and housing or medical care. To qualify, children need to meet the program’s definition of eligibility and the family needs to have limited income and resources. In May 2019, about 1.1 million children under age 18 received an average monthly SSI payment of $674 (SSA, 2019). Nearly half (45 percent) of low-income families with an SSI recipient were lifted out of poverty by receiving SSI, according to a 2015 National Academies report (NASEM, 2015). Another 4 million children receive benefits through the Social Security program as children of deceased workers (survivor benefits), children of workers with disabilities (through Disability Insurance), or children of retired workers. Summing across these groups, about $3.6 billion flowed to children through SSI and SSA programs (SSA, 2019). It is likely that the bulk of these monies goes to older children rather than those under age eight; nonetheless, for the
families receiving these payments, the increase in income helps them to meet basic needs.
These programs (TANF, SSI, and SSA) all have the potential to improve children’s health by raising family incomes; however, eligibility is limited, and the size of the assistance provided, especially for TANF, has not kept pace with rising costs of basic needs, particularly of housing. In terms of federal expenditures, the $12 billion of TANF spending on children and $12 billion in SSI for children with disabilities are only a small portion of federal spending on children in low-income families (Hoynes and Schanzenbach, 2018; Isaacs et al., 2017b). See Figure 6-1 for a breakdown of government spending on children by program from 1990 to 2015. The 2019 National Academies report A Roadmap to Reducing Child Poverty estimated that reductions in child poverty based on the current TANF program are small because of the low proportion of low-income children receiving TANF and the level of benefits. That report did not include expansion of TANF in the main strategies proposed to reduce
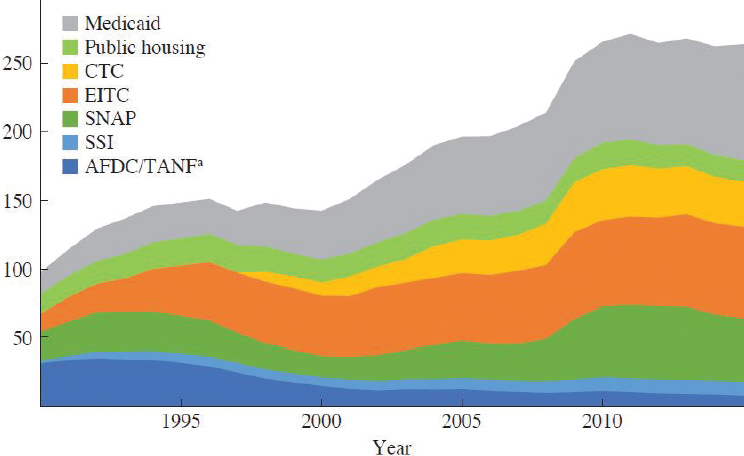
NOTE: AFDC = Aid to Families with Dependent Children; CTC = Child Tax Credit; EITC = Earned Income Tax Credit; SNAP = Supplemental Nutrition Assistance Program; SSI = Supplemental Security Income; TANF = Temporary Assistance for Needy Families.
a AFDC became TANF after the 1996 welfare reform. Dollars reported in billions of 2015 dollars.
SOURCE: Hoynes and Schanzenbach, 2018.
child poverty, primarily due to the lack of evidence and the difficulties of assessing the effects of block grants on child outcomes when states have considerable flexibility in how the money is spent (NASEM, 2019). In contrast, they estimated that the child poverty rate (based on the supplemental poverty measure) would be 1.8 and 2.3 percentage points higher without SSI and SSA benefits, respectively (NASEM, 2019). While these programs (TANF, SSI, and SSA) provide some income support for young children, much more of the spending on children is through tax credits and in-kind assistance for food and housing, which we examine next.
Supporting Children Through Tax Credits
In contrast to cash assistance received on a monthly basis, tax credits represent an alternative financing mechanism for income support. When a family receives a tax credit, the taxes they owe to the government are reduced, and when the tax credit is “refundable,” the family receives a payment if the credit exceeds the tax owed. In theory, a tax credit can provide the same amount of income assistance to a family as a direct cash transfer, although in practice, the amount and timing of the payments differ between the two types of mechanisms. Economists generally regard tax credits as having advantages over direct cash transfers in terms of the ease of administering the program (less bureaucracy) and lesser stigma from participation (Nichols and Rothstein, 2016). However, the extra income from a tax credit or refund is typically available only once per year and only if the family files a tax return. The two primary tax credits that apply to U.S. families with young children are the EITC and the CTC, sometimes jointly referred to as working family tax credits. While this section’s focus is the federal level, many states offer similar tax credits to working families. In theory, working family tax credits avoid the potential work disincentives of cash transfer programs, and research has demonstrated large increases in labor force participation, particularly for single mothers with children, as a result of the EITC (Nichols and Rothstein, 2016).
The EITC provides a refundable tax credit to eligible families based on earnings, number of children, and marital status. Initially implemented in 1975, the EITC has seen its level and coverage expanded with bipartisan support several times over the past 45 years. The Internal Revenue Service and the U.S. Census Bureau estimate that nationally, between 77 and 80 percent of eligible families claimed the EITC in 2015 (IRS, 2019). Although the take-up rate is high, outreach campaigns and use of tax preparation services or software can help increase the proportion of eligible families who receive the tax credit (Goldin, 2018). In 2016, the average EITC received by families with children was close
to $3,200, which lifted an estimated 3 million children out of poverty and reduced the severity of poverty for nearly 7 million more children (CBPP, 2018c).
The CTC2 is structured similarly to the EITC as a tax credit that is (partially) refundable. Low- and moderate-income families can claim a tax credit for each of their children up to age 16. The Tax Cuts and Jobs Act of 2018 increased the CTC from $1,000 to $2,000 per child, with a maximum of $1,400 that is refundable. More than 90 percent of American families with children receive the CTC, and the average amount received in 2018 was $2,420 (per family) (TPC, n.d.). The average credit and share of families receiving the CTC is lower for families in the lowest income quintile because some of these families will not have enough earnings to qualify and the CTC is not fully refundable. Nonetheless, the estimated effect of the CTC on poverty is notable: the Center on Budget and Policy Priorities estimates that the CTC lifted about 1.6 million children out of poverty and reduced the severity of poverty for 6.7 million children in 2017 (CBPP, 2018b). Most families in the second, third, and fourth income quintiles receive the CTC, while those in the lowest bracket benefit less (TPC, n.d.). The boost of $1,000–$2,000 in the CTC is due to expire in 2025 (TPC, n.d.).
There is extensive research on the effects of the EITC on labor force participation (particularly of single mothers) and on health and educational outcomes for children in the United States. Less research has been conducted on the effects of the CTC, mostly because it was relatively small until recently. Given the similar structure of the CTC and EITC, many of the effects are expected to be the same, with the important exception that the CTC is available to most moderate-income families, unlike the EITC, which is targeted at families with low incomes.
As noted above, the EITC and the CTC together are effective in reducing child poverty: nearly 5 million children lived in families whose incomes were brought above the poverty level after including working family tax credits, and more than 7 million additional children experienced less severe poverty (CBPP, 2018c).3 The poverty rate for children under 18 falls about 6 percentage points with the tax credits (16.4 percent compared to 22.8 percent without them) (Nichols and Rothstein, 2016). The reductions in child poverty are larger for these tax credits than other means-tested programs in the United States (Nichols and Rothstein, 2016). Given the well-established link between family income and health outcomes, by
___________________
2 The refundable portion of the CTC is called the Additional Child Tax Credit (ACTC); here, both the ACTC and the CTC are included when referring to the CTC.
3 Note that these estimates are based on data using the U.S. Census Bureau’s Supplemental Poverty Measure.
increasing family incomes, these tax credits are likely to lead to improved child health. One advantage of studying the link between the EITC and outcomes is that researchers can use exogenous policy changes that increase families’ income, avoiding the problem of endogenous income in studies of income–health links (Boyd-Swan et al., 2013).
While most studies have focused on the impacts of the EITC on labor force participation or reductions in poverty, a small but growing number of studies have examined the impacts of the EITC on health and education outcomes of children, both short and long term. Several studies found the EITC associated with higher birth weights and/or a reduction in the incidence of low birth weight (LBW) (Baker, 2008; Hoynes et al., 2012; Komro et al., 2019; Strully et al., 2010). Using quasi-experimental methods, Hoynes et al. (2012) estimated a decline of 2–3 percent in LBW occurrence for a $1,000 increase in the EITC, with larger effects for black than white women (among single women with a high school education or less). This study and one by Strully et al. (2010) also link EITC receipt with reduced rates of maternal smoking. In contrast, Baughman and Duchovny (2016) found that EITC receipt was not associated with improvements in parent-reported health status of children age birth to 5, although there were improvements for older children (age 6 to 14). Evidence linking the EITC to child cognitive or child development outcomes is limited (particularly for younger children). One study by Hamad and Rehkopf (2016) used an instrumental variable approach to estimate the impact of the EITC on child development. They found “modest but meaningful improvements” in child behavior and home environments. The article notes that one mechanism through which the EITC impacts child development is through improved mental health of mothers (Evans and Garthwaite, 2010) and that it may lead to reductions in maltreatment (Berger et al., 2017). Studies focused on older children also find positive associations with EITC receipt on test scores (Chetty et al., 2011; Dahl and Lochner, 2012) and college attendance (Manoli and Turner, 2018).
It is important to note that effects of the EITC on health outcomes may be a result of the increase in family income; however, the EITC also strongly impacts work incentives, and impacts on child health and development may be due to changes in parent employment. Increases in maternal employment may increase the family’s income but also reduce the amount of time mothers spend with their children. How these changes impact children’s health and development likely depends on the quality of nonparental child care used and the stress experienced by parents, in addition to income changes (Hoynes and Schanzenbach, 2018).
Unlike the working family tax credits, minimum-wage policies are not targeted specifically at low-income families with children.
Nonetheless, some economists argue that minimum-wage policies play an important and complementary role in reducing child poverty along with the EITC (Nichols and Rothstein, 2016). Research summarized by Nichols and Rothstein (2016) has demonstrated that the EITC provides a strong incentive for single mothers to work and has been a major factor underlying the rise in labor force participation of single mothers over the past two decades. An increase in the supply of labor, holding all else equal, could put downward pressure on wages, and the minimum wage provides a floor to keep wages from declining (Nichols and Rothstein, 2016). Parents who earn low wages benefit from a higher minimum wage in every paycheck along with receiving the tax credit when they file a tax return (CBPP, 2018c). A small number of studies also link increases in the minimum wage with health outcomes, though few examine children’s health or birth outcomes. Two studies find small improvements in birth weight outcomes related to minimum-wage increases across states over time using quasi-experimental methods (Komro et al., 2016; Wehby et al., 2016). One study also found reductions in child maltreatment associated with higher minimum wages (Raissian and Bullinger, 2017). Given the evidence linking improved child health to higher family incomes, more research on the health effects of minimum-wage increases is needed to inform the policy debate.
Child Allowances
Many wealthy countries provide support to families through a child allowance or child benefit, which may be a cash grant or through the tax code. In the current U.S. tax code, the CTC and dependent child exemption act in many ways like a child allowance. The taxable income of families with dependent children is reduced, resulting in greater disposable income to meet the costs of raising children. A child allowance, distributed monthly, has two main advantages over the tax code approach. First, it helps families with short-term needs for cash to meet expenses, compared to a once-per-year distribution through the tax system. Second, the lowest-income families often cannot take full advantage of tax credits and exemptions if their income is so low that they do not owe income tax. A child allowance paid to families on a monthly basis and not tied to earnings or employment would provide support for many of the lowest-income children in the United States whose parents do not work or have unstable and insufficient earnings.
A number of child allowance proposals have been proposed in recent years (NASEM, 2019; Shaefer et al., 2018). Schaefer et al. (2018) proposed
a universal child allowance of $250 per child per month, possibly offering $300 for children under age 6 and slightly less for each additional child. Schaefer et al. (2018) noted that while this amount would not come close to covering the full cost of raising a child, based on their review of the research, it is large enough to have a meaningful impact on families and children and is comparable to child allowances in other countries. The National Academies report A Roadmap to Reducing Child Poverty considered two options for a child allowance: about $2,000 and $3,000 per year. The reductions in child poverty are larger for these two policies than any of the other individual policy changes considered by the report (although the costs are also higher).
A few key principles are important when considering the parameters of a child allowance that is intended to improve health outcomes for young children. First, targeting payments to families with the youngest children acknowledges that families with younger children have lower incomes on average than families with older children (see Schaefer et al., 2018). In addition, some costs (particularly child care) are higher for younger than for older children. The nation provides sizable public resources to children starting at about age 5 when they enter the public K–12 education system. A child allowance targeted at children under age 5 would help to balance public investments in different age groups.
A universal program—in which all families with young children receive a child allowance—would reduce the stigma of participation relative to a means-tested program and may enhance social inclusion (NASEM, 2019, p. 148). While the costs of a universal program may exceed those of a targeted one, treating the allowance as taxable income would reduce the overall cost to the government. Alternatively, the child allowance could be phased out at 300 percent of the federal poverty level. Replacement of the current child tax credits with a monthly child allowance could provide families with a more regular source of cash income to support their children’s needs (NASEM, 2019). Determining the specifics of a child allowance policy and funding mechanism requires additional research and modeling to compare the potential impacts on child health and health equity. In sum, based on the committee’s review of the evidence and in accordance with the report A Roadmap to Reducing Child Poverty, there is strong evidence that programs that provide direct income transfers or basic necessities such as food and housing lead to improvements in child health and well-being (NASEM, 2019, p. 89). At the end of the chapter, the committee recommends expanding resources to support families with young children, with a child allowance as one important option to consider.
Paid Parental Leave
Maternal and paternal leave policies are generally intended to support mothers in recovering from childbirth and mothers and fathers in taking time off work to care for new infants. The United States remains one of the very few countries without a national paid guaranteed maternity leave policy. Across Organisation for Economic Co-operation and Development (OECD) countries, on average, mothers are entitled to 18 weeks of paid maternity leave (OECD, 2017). Although the United States is the only OECD country without a national-level policy of paid leave, California, New Jersey, New York, Rhode Island, Washington, Washington, DC, and, most recently, Massachusetts have passed legislation to implement paid leave at the state and local levels (Mass.gov, 2019; Raub et al., 2018). See Box 6-3 for more information on California as an example of a state that has implemented a paid leave policy. A number of studies of paid maternity leave have found positive health effects, particularly lower infant and child mortality (Heymann et al., 2011; Nandi et al., 2018). Stearns (2015) estimated that paid maternity leave through temporary disability insurance in the United States reduced LBW by 3.2 percent and early births by 6.6 percent, with larger effects for certain subgroups, including black and unmarried mothers (Stearns, 2015). While improved maternal and child outcomes have been associated with paid leave policies in other countries, a review by Almond et al. (2018) showed mixed findings on child health impacts across studies, depending in part on the length of the leave. They concluded that “facilitating short maternity leaves is highly beneficial, but extended maternity leaves do not have a positive effect” on child outcomes (Almond et al., 2018, p. 1406). Rossin-Slater (2011) estimated that the Family and Medical Leave Act (FMLA), which allows for 12 weeks of unpaid maternity leave, resulted in lower infant mortality and slightly higher birth weight outcomes for college-educated women. Overall, however, based on her review of the literature, Rossin-Slater stated that “while extensions in existing paid leave policies have had little impact on children’s well-being, the evidence suggests that the introduction of short paid and unpaid leave programs can improve children’s short- and long-term outcomes” (Rossin-Slater, 2011, p. 17).
Maternity leave policies have also been associated with higher rates of breastfeeding. As discussed in Chapter 3, breastfeeding provides important nutrition for developing infant brains and bodies; however, rates of exclusive breastfeeding for 6 months (as recommended by the World Health Organization and the American Academy of Pediatrics [AAP]) are low in the United States, especially among black women. Furthermore, the majority of mothers in the United States are not breastfeeding as long as they had planned (Mirkovic et al., 2014; Office of the Surgeon
General et al., 2011). While the Patient Protection and Affordable Care Act (ACA) has some protections for mothers who need to express milk while at work4 (a critical component of successful breastfeeding for working mothers), many mothers are not given the time, appropriate space, and support needed to do so when in low-paying jobs (Murtagh and
___________________
4 For example, the ACA updated the Fair Labor Standards Act to require U.S. firms with 50 or more employees to provide breastfeeding mothers with reasonable break time and space to express milk (DOL, 2018).
Moulton, 2011; Office of the Surgeon General et al., 2011). In a survey conducted by Declercq et al. (2013), 58 percent of women reported breastfeeding to be a challenge once they returned to work.
Paid leave “facilitates the initiation and continuation of breastfeeding” (Heymann et al., 2013). For example, a rigorous quasi-experimental study in California found that access to paid leave was associated with increased rates of exclusive and overall breastfeeding during the first 3, 6, and 9 months after birth (Huang and Yang, 2015). Studies (in both the United States and other developed countries) have found associations between maternity leave lasting at least 8 weeks and a higher probability of establishing breastfeeding (Guendelman et al., 2009; Ogbuanu et al., 2011; Skafida, 2012). Paid parental leave is hypothesized to increase mother–child attachment and give new mothers increased time to gain the skills and social support needed to maintain breastfeeding before returning to work.
The AEI-Brookings Working Group on Paid Family Leave published two reports in 2017 and 2018 that focused on paid parental leave and paid family care and medical leave, respectively. Based on the extant literature on paid parental leave and its impact on family outcomes, the 2017 report puts forth a federal paid parental leave proposal. In addition to physical health and cognitive outcomes for children, the report cites improved labor force participation as a positive outcome associated with paid leave. For example, California and New Jersey’s paid leave policies saw increases in labor force attachment among women in the months surrounding childbirth (Byker, 2016). This is important because continued workforce participation can help sustain household income and individual income, as well as other economic indicators that have been linked to health and well-being (see, for example, NASEM, 2017; Woolf et al., 2015). The key elements of the AEI-Brookings federal paid leave proposal are making benefits available to both mothers and fathers, wage replacement of 70 percent up to a maximum limit of $600 per week for 8 weeks, and job protection for the individuals who take leave. The authors also suggest that such a federal paid leave program could be financed by a payroll tax levied on employees and/or savings in other areas of the budget (e.g., reduced tax expenditures in areas such as unemployment insurance or Social Security and disability programs) (AEI-Brookings Working Group on Paid Family Leave, 2017).
Summary and Conclusions
There is considerable evidence that “income matters” for health outcomes, especially in early childhood. The report A Roadmap to Reducing Child Poverty concludes that “the weight of the causal evidence does
indeed indicate that income poverty itself causes negative child outcomes, especially when poverty occurs in early childhood or persists throughout a large portion of childhood” (NASEM, 2019, p. 2). There is also strong evidence that the reverse is true: increasing family resources to meet basic needs supports the health and development of young children. Given the high rate of child poverty in this country compared to other wealthy nations, as well as large disparities across racial and ethnic groups in poverty rates, reducing childhood poverty is a critical, foundational step in reducing health disparities in early childhood.
One way to increase the resources families have for basic needs is through social insurance and safety net programs that provide cash or tax credits to families. Studies demonstrate improved health outcomes when families receive assistance through government programs, such as the EITC and SSI. These programs are associated with improved birth, health, and educational outcomes for young children, which will set them on a better trajectory for lifelong health and well-being.
Much of the support provided to families with children in the United States is in the form of “work supports,” where eligibility and the level of benefits are closely tied to employment and earnings. These policies help to reduce poverty by both increasing resources and encouraging employment (which also can lead to higher family income in the future). However, the report A Roadmap to Reducing Child Poverty determined that a work-oriented package of programs and policies would be the least effective of the four packages they considered in reducing the number of children in poverty (see Table 6-1 for a summary of the components of each of the four packages). That report also concluded that mandatory “work requirements are at least as likely to increase as decrease poverty” (NASEM, 2019) (see Box 6-2).
In addition to a limited impact on reducing child poverty, further expansions of the work-oriented safety net programs may have unintended negative consequences for child health if parent employment results in
TABLE 6-1 Components of the Four Packages and Their Estimated Costs and Impact on Poverty Reduction and Employment Change from A Roadmap to Reducing Child Poverty
| 1. Work-oriented package | 2. Work-based and universal support package | 3. Means-tested supports and work package | 4. Universal supports and work package | ||
|---|---|---|---|---|---|
| Work-oriented programs and policy | Expand EITC | X | X | X | X |
| Expand Child Care Tax Credit | X | X | X | X | |
| Increase the minimum wage | X | X | |||
| Roll out WorkAdvance | X | ||||
| Income support-oriented programs and policies | Expand housing voucher program | X | |||
| Expand SNAP benefits | X | ||||
| Begin a child allowance | X | X | |||
| Begin child support assurance | X | ||||
| Eliminate 1996 immigration eligibility restrictions | X | ||||
| Percent reduction in the number of poor children | −18.8% | −35.6% | −50.7% | −52.3% | |
| Percent reduction in the number of children in deep poverty | −19.3% | −41.3% | −51.7% | −55.1% | |
| Change in number of low-income workers | +1,003,000 | +568,000 | +404,000 | +611,000 | |
| Annual cost, in billions | $8.7 | $44.5 | $90.7 | $108.8 | |
SOURCE: NASEM, 2019.
lower rates of breastfeeding or disruptions to the attachment between infant and caregiver. Evidence of the importance of attachment and breastfeeding is discussed in Chapters 3 and 4. Work-oriented programs, such as the EITC, that increase families’ incomes and increase employment are an important component of the social safety net. However, additional support for families with young children through paid parental leave or
a child allowance that is not tied to parent employment would recognize the special needs of the earliest years in which parent time and attention are critically important for children’s health and development. Both paid parental leave and income support, such as a child allowance not tied to employment, may provide parents with greater opportunity to take time out of the labor force to attend to their children’s needs.
As noted above, additional income support for families with young children through paid parental leave would recognize the special needs of infants and their caregivers. Unpaid parental leave through FMLA does not cover all employees, and many families with low incomes are unable to afford to take an unpaid leave. Paid parental leave grants parents greater opportunity to take time out of the labor force to attend to their children’s needs. Short, paid parental leave programs have been associated with positive health outcomes and higher rates of breastfeeding.
As of 2019, six states and Washington, DC, have paid leave programs, and the programs are financed through employee payroll taxes (AEI-Brookings Working Group on Paid Family Leave, 2017). Some proposals for paid family leave (PFL) follow a social insurance model in which employees contribute through payroll taxes to a government-administered social insurance fund. Other financing options include an employer mandate, tax credits to encourage employers, or general funds (Isaacs et al., 2017a). Because there are a variety of options to implement, structure, and administer a paid leave policy, cost estimates for this program vary widely. In its 2018 report, the AEI-Brookings Working Group on Paid Family Leave offered three methods for assessing the
cost of a hypothetical 8-week paid family medical leave program5 had it been operational in 2016. The three methods use (1) national-level data, assuming uptake would be similar to private-sector participation under FMLA; (2) state paid leave data, assuming participation would mirror the rates of the states with operational programs; and (3) a simulation model to combine national- and state-level data. Because these methods differ with respect to data sources and assumptions on program use, the cost estimates vary widely and drawing comparisons can be difficult. Based on their analyses, the authors estimate that the program could be expected to cost from 0.10 percent of total wages or $7.65 million total benefits paid (based on New Jersey’s state paid leave program) to 0.61 percent of total wages or $46.3 million total benefits paid (based on the FMLA national survey).
The committee did not study in depth other income-enhancement strategies to boost family resources that are not targeted particularly to health outcomes or early childhood, but these may be important for supporting the health and well-being of families and children. The National Academies report A Roadmap to Reducing Child Poverty details a number of additional strategies to reduce child poverty through, for example, increases in the minimum wage, job training programs, child care subsidies, and child support assurance, in addition to the policies discussed in this section. There is limited evidence of the impacts of these on child health, with the exception of the minimum wage (discussed earlier). The National Academies report A Roadmap to Reducing Child Poverty provides a careful assessment of a set of feasible strategies that could be used to reduce child poverty by half within 10 years (see Table 6-1). As discussed in Chapter 2, the scientific evidence amassed since From Neurons to Neighborhoods has established that access to basic resources prenatally and in early childhood impact the developing child’s brain and nervous system, immune function, and other organs (NRC and IOM, 2000). The toxic stress response of children living in poverty directly impacts behavioral and psychological well-being and substantially increases later-life risk for poor health and educational outcomes. Thus, reducing child poverty is a critically important, foundational strategy for improving child health outcomes and reducing health disparities in early childhood. Expansion of income-support programs that are not tied directly to parent earnings is likely to help those who need it most: children in deep poverty and the youngest children. Determining the specifics of a child allowance policy and funding mechanism requires additional
___________________
5 The hypothetical program provides universal access to up to 8 weeks of family and medical leave, including parental leave, with benefits paid at 70 percent of usual weekly wages up to a cap of $600 per week.
research and modeling to compare the potential impacts on child health and health equity. At the end of the chapter, the committee recommends expanding programs to increase economic resources to support families with young children, with a child allowance as one important option to consider.
Policies that build family assets and wealth also deserve consideration in developing a national strategy to ensure that all children have an equal opportunity to reach their full health and developmental potential. Individual Development Accounts and child savings accounts, for example, are typically targeted toward building savings for home ownership or postsecondary education. These strategies may have longer-term impacts on child and family well-being. Increasing education levels, particularly of mothers, also would likely lead to improved economic security for families. These policies support the broader goal of human capital development and long-term economic growth.
FOOD SECURITY AND NUTRITION
As described in Chapter 3, adequate and nutritious food is critically important for health outcomes during the preconception, prenatal, and early childhood periods. At times, adequacy of specific nutrients is crucial, such as folic acid during pregnancy. In each of these developmental periods, the overall adequacy and healthiness of food intake influence current health and development and have effects lasting into adulthood. Furthermore, food insecurity may affect both children and parents through changes in eating habits and stress related to uncertainty and inadequacy of food availability. The neurobiological (and other) mechanisms underlying these effects were described in Chapters 2 and 3. In this section, we look at the programs and policies in the United States aimed at reducing food insecurity and improving nutrition and healthy eating, with a focus on the prenatal and early childhood periods.
Current Programs and Policies
Two major federal programs in the United States target the adequacy of food and nutrition for children living in households with limited resources: the Supplemental Nutrition Assistance Program (SNAP), formerly known as the Food Stamp Program, and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). In this section we examine the evidence on the effects of these two programs on children’s health and development. Note that programs that operate primarily in schools and early education settings, such as the National School Lunch and Breakfast Program, are discussed in Chapter 7.
SNAP
SNAP provides assistance to eligible individuals and families to purchase food. Participants use an Electronic Benefit Transfer (EBT) card that functions like a debit card to purchase food from authorized retailers, which include supermarkets, grocery and convenience stores, and farmers’ markets (CBPP, n.d.). Many participants enroll in SNAP for a short time—from 2009 to 2012, approximately 48 percent of participants received benefits for 24 months or less (Irving and Loveless, 2015; RWJF, 2018).
Participants need to meet requirements regarding income (gross6 and net7 monthly income), resources (such as cash, money in checking and savings accounts, and vehicles), and nonfinancial standards to be eligible to receive SNAP benefits (Cronquist and Lauffer, 2019). Undocumented noncitizens of the United States are not eligible for SNAP, but noncitizens who have lived in the United States for at least 5 years, receive disability-related assistance, or are less than 18 years of age are eligible (if they also meet the aforementioned income, resource, and nonfinancial eligibility requirements) (USDA, 2018b). The program expects that participating households will spend about 30 percent of their own financial resources purchasing food; thus, the amount in SNAP benefits received by each participating household is calculated by multiplying the household’s net monthly income by 0.3 and subtracting the result from the maximum monthly allotment8 for the household size.
Each month of fiscal year 2017, SNAP served 42.1 million individuals in 20.8 million households. Children were 44 percent of SNAP participants and received 43 percent of SNAP benefits. On average, the program provided assistance to 8.6 million households with children (42 percent of all households served by SNAP) each month. Of the total number of SNAP participants, 8 percent were children with U.S. citizen status living with noncitizen adults (Cronquist and Lauffer, 2019).
While SNAP benefits can be spent only on eligible food items, these benefits add to the total resources the family has to spend on all necessities. The average monthly benefit of $255 per household “represents a sizable income transfer to participants, and is expected to change the amount or quality of food purchased” (Hoynes and Schanzenbach, 2018, p. 13). A recent Urban Institute report estimates that the SNAP program reduced the number of children living in poverty by more than
___________________
6 Includes a household’s total, nonexcluded income before any deductions have been made (USDA, 2018b).
7 Gross income minus allowable deductions (USDA, 2018b).
8 Maximum monthly allotments by household size are available at https://www.fns.usda.gov/snap/eligibility (accessed March 28, 2019).
one-quarter and the number in deep poverty by nearly half (Wheaton and Tran, 2018). The report also found that SNAP reduced the poverty gap (defined as the additional income needed to lift all low-income families out of poverty) by 37 percent for families with children. Given the evidence on the links between health outcomes and income, one would expect these sizable reductions in poverty to lead to improved health outcomes. A growing body of evidence shows that SNAP improves birth outcomes (Almond et al., 2011; East, 2018), although, as discussed below, relatively few studies focus on the effects of SNAP on the health outcomes of young children.
A review of studies prior to 2003 concluded that SNAP participation increased household food expenditures (USDA, 2004), which suggests that SNAP would reduce food insecurity among recipient households. Because families experiencing greater hardship are more likely to participate in SNAP, however, some studies of SNAP’s effect on food insecurity have found mixed and null results (Gibson-Davis and Foster, 2006; Gundersen and Oliveira, 2001; Huffman and Jensen, 2008; Wilde, 2007; Wilde and Nord, 2005). Gregory et al. (2016) illustrate how estimates of the relationship between SNAP participation and food insecurity vary depending on statistical methods, demonstrating positive and negative estimates along with ones that were not significantly different from zero. They did conclude, however, that food insecurity was reduced by SNAP in a dose–response type model. Furthermore, according to an Urban Institute report, “controlling for selection into SNAP is important for disentangling the effect of SNAP receipt on food insecurity” (Ratcliffe and McKernan, 2010, p. 14). The authors found that the relationship between SNAP participation and food insecurity changed direction when they controlled for selection into SNAP using an instrumental variables approach. They concluded that SNAP participation reduced food insecurity by 16 percentage points (results for children not reported separately). Using methods to account for both selection and measurement error in reporting SNAP participation, Kreider et al. (2012) found a reduction of at least 8 percentage points in food insecurity for children, depending on the model assumptions. Deb and Gregory (2018) found that the effects of SNAP on food insecurity vary across the population; while it may have no effect for some, for those starting with low food security, it resulted in a much lower likelihood of food insecurity.
While SNAP increases household resources and reduces food insecurity for (at least) some families, studies of the impact of receiving food assistance on children’s health outcomes are relatively rare. One study found that the introduction of the Food Stamp Program in California was associated with a reduction in infant birth weight, particularly among first-time teen mothers for whom birth rates increased overall
(Currie and Moretti, 2008). Potential mechanisms for this association could be related to fertility changes or the increased survival of LBW babies. The study findings also showed a small reduction in infant mortality for white babies in Los Angeles County. There is more recent evidence of a positive connection between receiving SNAP benefits (or food stamps) and improved birth outcomes. Almond et al. (2011) and East (2018) both found positive associations between food assistance during pregnancy and improved birth outcomes, using quasi-experimental methods. Almond et al. (2011) found larger improvements in birth weight outcomes for African American mothers and those living in high-poverty areas. They noted that these results occurred despite the fact that the Food Stamp Program was not designed to target pregnant women. See Figure 6-2 for data on the impact of in-utero exposures to food stamps on likelihood of birth weight below selected cut-offs.
With respect to other health outcomes for children, there is limited causal evidence. Kreider et al. (2012) reported improvements in child health outcomes (along with reductions in child food insecurity); however, the range of possible effect sizes is large. They accounted for both selection and underreporting of SNAP participation but did not specifically focus on young children. Most studies focus on adult health outcomes and found mixed results for adults (Kreider et al., 2012; see, for example,
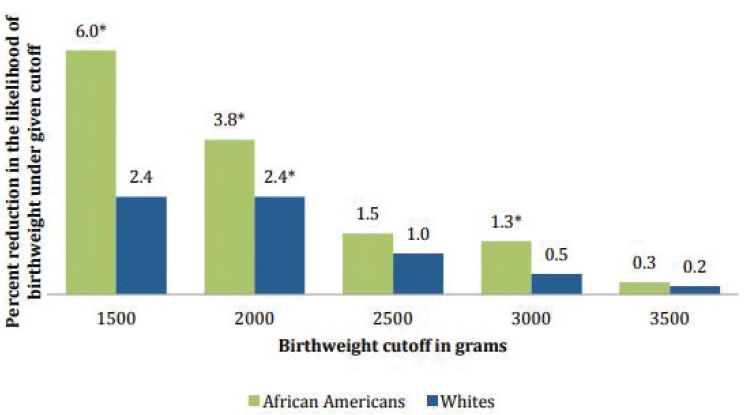
NOTES: * Denotes estimate statistically significantly different from zero. Data from Almond et al., 2011.
SOURCE: Hoynes and Schanzenbach, 2016.
Gregory and Deb, 2015; Yen et al., 2012). Overall, there is limited evidence on the causal effects of SNAP on children’s health because there have been few opportunities for random assignment9 or limited variation in policies over time or in different places to exploit with experimental or quasi-experimental methods (East, 2018).
While studies of direct or contemporaneous effects on children’s health are limited, one recent study demonstrated a link between receipt of SNAP in childhood and adult health outcomes. Hoynes et al. (2016) found that adult health measured by the metabolic syndrome index was significantly better for those whose childhood families had access to food stamps, particularly in early childhood (before age 5). Long-term positive health effects of SNAP—that is, adult health outcomes for those receiving SNAP as children—are consistent with short-term health improvements during childhood. Similarly, East (2018) found positive effects of SNAP participation before age 5 on health outcomes when children were age 6–16, using quasi-experimental methods for a sample of children born in the United States to immigrant parents. While conclusions about the immediate impacts of SNAP on young children’s health are provisional given the methodological challenges of estimating causality (Carlson and Keith-Jennings, 2018), the evidence of SNAP impacts on reduced food insecurity and later health outcomes suggests that children benefit in both the short and long run.
One of the concerns about the SNAP program has been the potential linkage between SNAP benefits and obesity, in both adults and children. Earlier studies that did not adequately control for selection into SNAP found positive correlations between SNAP and obesity, while other studies found reductions in obesity or no effects (Fan and Jin, 2015; Kreider et al., 2012). Myerhoefer and Yang concluded “the balance of evidence points to a small positive impact of SNAP participation on obesity for women” but that the results for “childhood obesity are less consistent” (Meyerhoefer and Yang, 2011, p. 313). For children, Kreider et al. (2012) concluded that the obesity rate was 5.3 percentage points lower due to SNAP.
In addition to reducing hunger and food insecurity, a second key objective of the nation’s food assistance programs is to improve the healthfulness of American food consumption and provide nutrition education. Studies have examined the effect of SNAP on the quality or healthfulness of a family’s food consumption as a possible mechanism through which SNAP might affect obesity (and other health) outcomes.
___________________
9 Random assignment demonstration projects have been conducted recently and are under way in several sites as part of the Demonstration Projects to End Childhood Hunger project and the Healthy Incentives Pilot (Olsho et al., 2017; USDA, 2018a).
Most studies have focused on adult food intake, but Yen (2010) found no effect of the SNAP program on young children’s nutrient intake. A number of demonstration projects have been conducted to evaluate ways to incentivize or influence consumption of healthful foods through SNAP. The Healthy Incentives Pilot (HIP) project provided a 30 percent rebate on purchases of a specified set of fruits and vegetables using SNAP benefits. Households receiving SNAP were randomly assigned to receive the rebate or not. The HIP evaluation reported that households receiving the rebates increased consumption of targeted fruits and vegetables by 26 percent, although some reported confusion and misunderstanding about how the rebate program worked and which vegetables and fruits were included (Olsho et al., 2017). The Summer EBT for Children pilot also was a random assignment design, but rather than targeting specific purchases, participants were provided with (an extra) $60 per month per school-age child. The evaluation study found modest improvements in several child nutritional outcomes and null effects for others (Collins and Klerman, 2017) even though this program did not specifically target or incentivize healthful food purchases. While SNAP benefits can be used to purchase almost any food item from participating retailers, recent pilot projects found that increased benefits and incentives for purchasing specific healthful foods can modestly impact some health-related and dietary outcomes. Proposals to restrict SNAP purchases to prohibit less healthful foods, such as sugary beverages, or to incentivize purchases of fruits and vegetables are highly controversial (Schwartz, 2017).
In summary, as discussed throughout this section, food assistance provided through SNAP is a major component of the nation’s social safety net and reduces poverty and food insecurity for millions of families and children (Carlson and Keith-Jennings, 2018). While the evidence of SNAP’s direct impact on children’s health is limited, Hoynes et al. (2016) found that adults who received SNAP as children experienced a reduction of 5 percent in heart disease and 16 percent reduction in obesity. Improvements in adult health outcomes related to receipt of SNAP in early childhood suggest that children are benefiting as well. Based on Hoynes and Schanzenbach’s (2018) summary of the literature examining links between SNAP participation and health outcomes, the National Academies (2019) report on reducing child poverty concluded that “many (but not all) of the methodologically strongest studies show SNAP benefits having positive impacts on health” (NASEM, 2019, p. 83). The report cites evidence that increasing SNAP benefits would substantially reduce child poverty and that current benefit levels do not account for food preparation time or geographic variation in food costs (Ziliak, 2016). Based on the evidence demonstrating the links between child health and family income or
resources, increasing SNAP benefits would likely lead to improved child health and reduced health disparities.
Special Supplemental Nutrition Program for Women, Infants, and Children
WIC provides assistance through breastfeeding support and education, healthy foods, nutrition education and counseling, screening referrals to other services, and vouchers to purchase fruits and vegetables from authorized farmers’ markets (USDA, 2015). WIC services are provided in many locations, including county health departments, hospitals, mobile clinics, community centers, schools, public housing sites, migrant health centers and camps, and Indian Health Service facilities (USDA, n.d.).
To be eligible to receive benefits, WIC participants need to meet all four categories of requirements: categorical, residential, income, and nutrition risk (USDA, 2018c). Infants younger than 1 year; children younger than 5 years; and women who are pregnant, postpartum (up to 6 months), or breastfeeding meet the WIC categorical requirement. To meet the residential requirement, participants need to reside in the state or local service area in which they apply but are not required to have lived in that area for a minimum amount of time. Participants also have to earn incomes at or below income standards that are set by state agencies, and fall within 100 and 185 percent of the federal poverty guidelines issued annually by the U.S. Department of Health and Human Services (HHS). Lastly, participants need to be determined by a health professional to have at least one medical (e.g., anemia, underweight) or dietary (e.g., poor diet) condition from a list of conditions indicating nutrition risk that is set by states (USDA, 2018c).
In fiscal year 2018, WIC served approximately 6.9 million people and cost the federal government about $5.3 billion (USDA, 2019). In 2016, it was estimated that 64 percent of individuals eligible to receive WIC benefits were children ages 1–4, 21 percent were pregnant and postpartum women, and 16 percent were infants for a total of 13.9 million individuals. Of these, 7.6 million (55 percent) received WIC benefits, with 86 percent of eligible infants receiving benefits but only 44 percent of children ages 1–4 receiving them (Trippe et al., 2019).
Numerous studies using varied methods have found evidence of improved birth outcomes for women participating in the WIC program (see, for example, Figlio et al., 2009; Fingar et al., 2017; Foster et al., 2010; Hoynes et al., 2011). These studies find reductions in the likelihood of LBW (Figlio et al., 2009; Hoynes et al., 2011) and reductions in infant mortality (Khanani et al., 2010). Figlio et al. (2009) studied the effect of WIC in Florida between 1997 and 2001 by matching infant birth records with school records for older siblings to identify those who were
marginally eligible and marginally ineligible in order to form groups for comparison. They estimated a significant reduction in the likelihood of LBW among WIC participants, although there was no significant effect on average birth weight or gestational age. Studies generally have found that the effects of WIC on birth outcomes are stronger for women with lower education levels, those living in areas of high poverty, and African Americans (Hoynes et al., 2011; Khanani et al., 2010). Fingar et al. (2017) accounted for gestational age, which might bias estimates in other studies, and reported a significantly reduced risk of preterm birth, LBW, and prenatal death.
One of the potential channels through which WIC impacts birth outcomes is through changes in dietary quality and access to nutritional information and support for healthy behaviors, such as quitting smoking, for pregnant women. Participants can use their WIC vouchers only for specific foods, and changes in the approved foods after 2008 reflect dietary recommendations from AAP and the Institute of Medicine. The U.S. Department of Agriculture published a final rule in 2014 that provides for more purchases of fruits and vegetables, whole-grain options, yogurt and soy options in place of milk, and more flexibility to tailor food packages to individuals (Carlson and Neuberger, 2018). While there has been concern about the possibility that providing infant formula to new mothers reduces breastfeeding, the changes to food packages and incentives after 2014 have encouraged breastfeeding (NASEM, 2016). The rate of breastfeeding among WIC participants has risen 45 percent over 12 years, reducing the difference between all women and WIC participants (Carlson and Neuberger, 2018).
There is solid evidence linking the WIC program to improved nutrient intake and eating more healthful food, although many of the studies report household-level consumption and do not focus specifically on children. The introduction of the improved food packages in WIC led to noticeable improvements in the percentage of families reporting that they eat more whole grains, drink lower-fat milk, and consume more fruits and vegetables (Andreyeva and Luedicke, 2013; Chiasson et al., 2013; Whaley et al., 2012). Thus, the additional resources to purchase specific food items provided by the WIC program is associated with changes in the types of food consumed by households (Whaley et al., 2012). In the case of the HIP, these changes may have been due in part to “promotional effects,” whereby the incentive for certain foods provides information to participants about which foods are healthier (Olsho et al., 2017).
By providing access to healthier foods and nutrition information, WIC would be expected to improve the health and developmental outcomes of young children. WIC may also reduce food insecurity. One study found that WIC participation reduced the number of children experiencing food
insecurity by 20 percent (Kreider et al., 2016). There is also some evidence about the impact of WIC on young children’s cognitive and socioemotional development. Jackson (2015) used matching and fixed effects estimation methods and found improvements in cognitive development at age 2 and reading and math scores at age 11 for children whose mothers participated in WIC prenatally. In contrast, Arons et al. (2016) found no significant improvement in socio-emotional development among young children receiving WIC; however, their sample size was small. Based on the current literature, the extent to which WIC supports cognitive and noncognitive development in young children is still uncertain.
Overall, the evidence is solid that WIC leads to improved birth outcomes and improved dietary intake for participants, although there is less evidence that it directly improves children’s health and development in the early years. Revisions to the food package and incentives for purchasing specific fruits and vegetables have led to improvements in dietary quality. Evidence of savings on health costs, particularly postpartum, from the mid-1990s suggested that (back then) the cost savings far exceeded program costs (GAO, cited in Carlson and Neuberger, 2018, p. 24). Nearly two-thirds of all infants and half of pregnant and postpartum women are eligible for WIC.10 The broad reach of the WIC program has been viewed as a positive attribute, but some feel that it indicates that the program is not sufficiently targeted and resources could be spent more efficiently (Besharov and Call, 2009). However, many eligible families do not receive WIC benefits. In 2014, only half of eligible pregnant women participated, while 80 percent of eligible infants did (Johnson et al., 2017). While the WIC program is largely successful in supporting the health and nutrition of its recipients, investigating the barriers to participation and further studying heterogeneous effects on different subgroups are necessary to further understand its potential to reduce health disparities in early childhood. Furthermore, better coordination between the WIC program, ECE systems, and prenatal, postpartum, and pediatric care would allow for a more integrated systems approach to addressing children’s nutrition and developmental needs. (See Chapter 8 for more on applying a systems approach to promoting equitable healthy development.) Box 6-4 describes Healthy Mothers on the Move as an example of a promising model to improve nutrition and healthy lifestyles.
Summary
Both the SNAP and WIC programs have been studied extensively, and a large body of literature points to strong associations between program participation and positive outcomes, including less food insecurity,
___________________
10 See https://www.fns.usda.gov/wic/wic-eligibility-and-coverage-rates (accessed July 14, 2019).
reductions in poverty, and greater consumption of healthy foods. The evidence is convincing that WIC, which is targeted to pregnant and postpartum women, infants, and young children, improves birth and postpartum outcomes. There is also strong evidence that SNAP improves birth outcomes and child health. In evaluating the impacts of both programs,
however, confounding factors are important to consider: participants may be more disadvantaged than nonparticipants but also may self-select into the programs, and either factor may bias study estimates. A small but increasing number of studies use experimental and quasi-experimental methods to estimate causal effects, although few focus specifically on health outcomes for young children. In addition to providing additional resources to the family to meet their basic needs, both SNAP and WIC can increase the consumption of healthful foods through nutritional education and incentives.
Because safety net programs, such as WIC and SNAP, have been shown to improve birth outcomes and to reduce food insecurity for young children, the committee recommends:
As noted earlier, the National Academies report A Roadmap to Reducing Child Poverty concludes that the current level of SNAP benefits is inadequate. That report considers two options for increasing benefit levels: a 20 or 30 percent increase (along with a higher benefit amount for households with teenagers and a boost in summer benefits). The report also notes that SNAP has a larger effect on reducing deep poverty than other government assistance programs do. Given the strong evidence linking improved child food security and SNAP, along with evidence of longer-term positive outcomes, increases in SNAP benefit amounts are likely to reduce health disparities. This committee had insufficient evidence to compare the effects on health disparities of alternative means of increasing family resources, such as increasing SNAP benefits or providing a monthly child allowance. For the most part, a dollar increase in SNAP benefits will have the same effect as a cash dollar, although some families
might increase food expenditures more with an increase in SNAP. Increasing family resources is a critical, foundational step to reduce child health disparities (see Conclusion 6-1). Careful study and modeling is needed to determine the most cost-effective way to do so, with particular attention to the potential impacts on child and caregiver health and well-being and maternal employment, attachment, and breastfeeding. At the end of the housing section in this chapter, the committee recommends expanding resources to support families with young children, with an increase in SNAP benefit levels as one important option to consider.
HOUSING
Housing Affordability and Child Health and Equity
Access to affordable housing is considered an “upstream” determinant of child development, as it has implications for housing quality (Evans et al., 2000), instability (Garboden et al., 2017; Jelleyman and Spencer, 2008), and loss of housing (Sandel et al., 2018)—all of which are well-established determinants of child health (Leventhal and Newman, 2010). Unaffordable housing, or “high housing cost burden”—typically defined as housing costs above 30 percent of household income—is a critical social issue (Desmond, 2018) that has worsened during the past several decades (Joint Center for Housing Studies at Harvard University, 2017). In 2016, 47 percent of all renters and more than three-quarters of families earning less than $30,000 had unaffordable housing (Joint Center for Housing Studies at Harvard University, 2017). At the extreme, nearly 110,000 children are estimated to be homeless on any given night in the United States, and more than half of families who used shelters in 2016 identified as African American or black (U.S. Interagency Council on Homelessness, 2018).
The evidence discussed in Chapter 3 suggests that lack of affordable and quality housing, housing instability, and overcrowding have significantly detrimental effects on the health, well-being, and development of infants, children, and families. For more information on the evidence supporting the role of affordable housing in promoting positive outcomes for child health and development, see Chapter 3.
Improving Housing Affordability and Quality
Federal housing assistance is provided through a number of programs, including the Housing Choice Voucher Program, public housing, and the Low Income Housing Tax Credit. The Housing Choice Voucher Program is the largest federal housing assistance program for people with
low incomes. Administered by the U.S. Department of Housing and Urban Development (HUD), this program provides funds to local public housing agencies (PHAs). PHAs have latitude in how the program is administered and what populations are prioritized. Eligibility is based on average median income in the geographic area and stratified by extremely low income, very low income, and low income. A PHA has to provide 75 percent of its vouchers to people with extremely low incomes (Eligibility.co, 2019). Although HUD provides housing assistance through the Housing Choice Voucher Program to more than 2 million families per year (CBPP, 2019)—which ensures that participating households contribute no more than 30 percent of their income to rent (CBPP, 2017)—only one-quarter of all income-eligible households receive housing assistance (CBPP, 2017), and the average family will spend 26 months waiting for assistance (HUD, 2016). One analysis found that the percentage of families with children receiving rental assistance decreased by 13 percent since 2004, while “the number of families that paid more than half their income for rent or lived in severely substandard housing rose by 53 percent between 2003 and 2013, to nearly 3 million” (Mazzara et al., 2016).
HUD housing assistance can help families obtain improved housing quality and residential stability (social factors that are associated with child development and disparities) (Fischer, 2015; HUD, 2014, 2015). There is some evidence to suggest that housing assistance has a beneficial impact on child health (Slopen et al., 2018), although this is an underexplored area of research. Only a small number of studies have rigorously controlled for selection bias, thereby limiting interpretation of the results for many of the existing studies (Ahrens et al., 2016; Fenelon et al., 2018; Fertig, 2007; Jacob et al., 2015; Kimbro et al., 2011; Leech, 2012; Newman and Holupka, 2017; Slopen et al., 2018). According to an analysis by Chetty et al. (2016) of the Moving to Opportunity demonstration, the benefits of the voucher program may be greater for children who move when they are young (less than 13 years of age) and may “reduce the intergenerational persistence of poverty and ultimately save the government money” (Chetty et al., 2016, p. 860). (See the section on Improving Neighborhood Conditions for more on the Moving to Opportunity study.)
Although this program is designed to provide families with choices about residential location, new evidence suggests that the program falls short on multiple neighborhood characteristics for families with children (Mazzara and Knudsen, 2019). A 2019 study by the Center on Budget and Policy Priorities using HUD administrative data and Census survey data revealed that in the 50 largest metropolitan areas in the United States, voucher-assisted families with children are disproportionately clustered into high-poverty, low-opportunity, or minority-concentrated areas relative to the distribution of voucher-affordable housing across the
metropolitan area. For example, 33 percent of families with children using vouchers reside in high-poverty neighborhoods (Census-tract poverty rate at or above 30 percent) even though only 22 percent of voucher units are in high-poverty neighborhoods. Similarly, 61 percent of voucher-assisted families of color with children reside in “minority-concentrated” areas (Census-tract percent of people of color is at least 20 percentage points greater than the proportion in the entire metropolitan area), although only 32 percent of voucher units are allocated to minority-concentrated areas (Mazzara and Knudsen, 2019). Some programs, such as the Baltimore Mobility Program, include intensive counseling and require the use of vouchers in low-poverty areas for at least 1 year (Darrah and DeLuca, 2014). However, lack of affordable units in higher-opportunity neighborhoods remains a barrier (Misra, 2016). Other barriers include inflexible limits on search periods for families to find units and landlord resistance to voucher clients (Sard et al., 2018).
A Roadmap to Reducing Child Poverty modeled “expansions of voucher availability rather than other modifications, such as an increase in the level of housing subsidies, primarily because most experts agree that limited availability is currently the primary barrier preventing subsidized housing programs from having a larger impact on poverty reduction” (NASEM, 2019, p. 146). That committee also noted that “there is as yet no consensus among researchers as to whether existing housing subsidy levels set by the government are sufficiently aligned with true market rents faced by low-income families” (NASEM, 2019, p. 146).
As discussed in Chapter 3, housing quality is also a contributor to child health and development. A systematic review found strong evidence of effectiveness for home interventions focused on addressing asthma triggers, including multifaceted, in-home, tailored interventions (including mattress and pillow covers, high-efficiency particulate air vacuums and air filters, and cleaning), cockroach control through integrated pest management (including e-strategies, reducing access points, and using low-toxicity gel-bait pesticides), and combined elimination of leaks and removal of moldy items (Krieger et al., 2010). Several of the reviewed studies focused on children. A systematic review conducted by Crocker et al. (2011) found that home-based, multitrigger, multicomponent interventions reduced asthma symptoms and school absenteeism, as well as asthma acute symptoms, among children and adolescents. These assessments and interventions are often performed by home visitors or community health workers and have been found to be effective in both urban and rural areas (Chew et al., 2003; Crain et al., 2002; Levy et al., 2006; Morgan et al., 2004). The actions taken as a result of these assessments and interventions have been found to reduce disparities in asthma-related outcomes based on race/ethnicity and income (Postma et al., 2009).
Similarly, a comprehensive review by the Health Impact Project found residential remediation to be an effective primary prevention strategy to reduce childhood lead exposure (Health Impact Project, 2017). This remediation can range from complete removal or permanent containment of lead paint to scraping and painting over existing paint and covering contaminated soil. Secondary prevention through screening by pediatricians and other health care providers of young children and treatment for those with elevated blood lead levels (BLLs) is also critical for mitigating potential long-term harm.
Several states, including Maryland and New York, have undertaken state- and municipality-level lead prevention and mitigation efforts that have led to significant decreases in childhood lead exposure and poisoning. In New York, the City of Rochester implemented a Lead-Based Paint Poisoning Prevention Ordinance in 2006, which requires inspections for lead paint as part of existing inspections of most rental properties built before 1978. In addition, New York requires that all children undergo BLL testing at ages 1 and 2, which is overseen by the state’s health department. The health department also provides educational and environmental interventions for children who are found to have elevated BLLs (City of Rochester NY, n.d.).
Enacted in 1994 and modified in 2012, Maryland’s Reduction of Lead Risk in Housing Act has helped to make housing units safer for children by requiring owners of rental properties built before 1978 to ensure their properties comply with a lead paint risk reduction standard. The state has also invested in strong public enforcement of the Act, which is coordinated by the Maryland Department of the Environment’s Lead Poisoning Prevention Program.11 Through partnerships with nonprofits that provide legal services, such as the Green & Healthy Homes Initiative,12 the state has also increased compliance with the law via private enforcement (Trust for America’s Health, n.d.). As of 2016, Maryland requires all children born in or after 2015 to undergo blood lead testing at ages 1 and 2 (Maryland Department of Health, 2016). The Maryland Department of Health and Mental Hygiene oversees the state’s BLL testing efforts and other services, including case management follow-up for children found to have elevated BLLs and community education for parents, tenants, rental property owners, homeowners, and health care providers (Trust for America’s Health, n.d.). As a result of these initiatives, from 1993 to 2015, the number of Maryland children under 6 years old whose BLLs were
___________________
11 For more information, see https://mde.maryland.gov/programs/Land/LeadPoisoningPrevention/Pages/index.aspx (accessed March 21, 2019).
12 For more information, see https://www.greenandhealthyhomes.org (accessed March 21, 2019).
10 µg/dl or higher decreased from 23.9 percent (14,564 of 60,912 children tested) to 0.3 percent (377 of 110,217 children tested). In addition, from 2013 to 2014 alone, the number of rental properties that were treated and received certification for compliance with the lead paint risk reduction standard increased from 28,000 to 57,603.
While the United States has reduced the number of children at risk of lead poisoning, it has not completely eliminated lead hazards, and those most at risk for lead exposure are low-income and minority children.
Many high-quality reviews of lead poisoning prevention have been completed and contain important recommendations for remediation and prevention. For example, a report by the Health Impact Project (2017) includes the following recommendations and findings:
- Reduce lead in drinking water in homes built before 1986 and other places children frequent. Removing leaded drinking water service lines from the homes of children born in 2018 would protect more than 350,000 children and yield $2.7 billion in future benefits, or about $1.33 per dollar invested.
- Remove lead paint hazards from low-income housing built before 1960 and other places children spend time. Eradicating lead paint hazards from older homes of children from low-income families would provide $3.5 billion in future benefits, or approximately $1.39 per dollar invested, and protect more than 311,000 children.
- Increase enforcement of the federal renovation, repair, and painting rule. Ensuring that contractors comply with the U.S. Environmental Protection Agency (EPA) rule that requires lead-safe renovation, repair, and painting practices would protect about 211,000 children born in 2018 and provide future benefits of $4.5 billion, or about $3.10 per dollar spent.
- Reduce air lead emissions. Eliminating lead from airplane fuel would protect more than 226,000 children born in 2018 who live near airports, generate $262 million in future benefits, and remove roughly 450 tons of lead from the environment every year.
- Clean up contaminated soil.
- Improve blood lead testing among children at high risk of exposure, and find and remediate the sources of their exposure.
- Ensure access to developmental and neuropsychological assessments and appropriate high-quality programs for children with elevated BLLs.
Medical–Legal Partnerships
Medical–legal partnerships (MLPs) are multisector approaches to addressing legal issues, many of which are contributors to poor child health outcomes and disparities. Typically, a health care provider (or providers) partners with a legal aid entity to resolve a person or family’s legal issues, including those related to housing, benefits, debt, or education. As discussed in more detail in Communities in Action, MLPs “play an
important role in addressing the SDOH and are a relevant community-based solution for advancing health equity” (NASEM, 2017, p. 427).
A systematic review conducted by Martinez et al. found that “researchers have established more findings regarding the capacity of MLPs to address legal outcomes than their capacity to address health outcomes” (Martinez et al., 2017, p. 267); however, longer periods of study are likely needed to see improved health outcomes. Additional research is needed to identify child-specific health outcomes associated with MLPs.
MLPs represent a promising practice that has emerged over the past 10–15 years, and according to the National Center for Medical-Legal Partnerships,13 there are now 333 MLPs in 46 states. See Box 6-5 for an example of a promising MLP between the Cincinnati Children’s Hospital and the Legal Aid Society of Greater Cincinnati.
___________________
13 See https://medical-legalpartnership.org (accessed July 19, 2019).
Promising Tools
The following section describes tools that are available to communities and show promise in addressing poor child health outcomes and disparities through solutions to improve the affordability, quality, and stability of housing.
ChangeLab Solutions and Abt Associates have created a comprehensive and detailed toolkit that describes policies and programs to help preserve, protect, and expand the number of affordable rental units in neighborhoods where demand for housing is rising (Allbee et al., 2015). The authors state that “to ensure that people of all incomes, races, and ethnicities can continue to afford housing in neighborhoods experiencing rising rents, most communities will require a multifaceted strategy,” one that includes a combination of the policies and programs described. Grouped into six areas of focus, these policies and programs are summarized in Table 6-2.
Another promising tool is the National Healthy Housing Standard,14 which “provides health-based provisions to fill gaps where no property maintenance policy exists” and is “a complement to the International Property Maintenance Code and other policies already in use by local and state governments and federal agencies for the upkeep of existing homes” (National Center for Healthy Housing, 2014). The resource details minimum standards for healthy and safe homes, with information on each provision’s public health rationale and further references and resources. Since the resource’s release, the National Center for Healthy Housing also developed an implementation tool to aid in the adoption of the standard (National Center for Healthy Housing, 2017).15
Summary
Based on the evidence discussed in this chapter and presented in Chapter 3 on the effects of housing affordability and quality on health and developmental outcomes, the committee has reached the following conclusions about housing needs.
___________________
14 The National Healthy Housing Standard is available at https://nchh.org/resource/ national-healthy-housing-standard-full-document (accessed March 21, 2019).
15 The National Healthy Housing Standard implementation tool is available at https://nchh.org/resource/national-healthy-housing-standard-implementation-tool (accessed March 21, 2019).
TABLE 6-2 A Toolkit of Policies and Programs to Preserve, Protect, and Expand Affordable Housing
| Area of Focus | Purpose | Policies and Programs |
|---|---|---|
| Preservation | Preserve the affordability of housing where low- and moderate-income renters already live |
|
| Protection | Protect residents from the effects of rising rents or condo conversions by helping to reduce the risk of displacement or by helping them relocate to new units if necessary |
|
| Inclusion | Ensure a share of new development is affordable to low- and moderate-income households |
|
| Revenue Generation | Generate funding for affordable housing in neighborhoods experiencing rising rents and home prices by leveraging the development activity and economic growth associated with new development or redevelopment |
|
| Incentives | Offer a range of incentives to stimulate development of affordable housing in targeted areas |
|
| Property Acquisition | Gain control of desirable sites for development or redevelopment at affordable prices |
|
* Rental Assistance Demonstration (RAD) is a federal program that “converts public housing subsidies into a form that can be used as the basis for securing private financing and can be combined more easily with other subsidies” (Allbee et al., 2015, p. 23).
SOURCE: Allbee et al., 2015.
Given the evidence on the impact of housing for health and healthy child development, the committee recommends:
Increasing the supply of high-quality affordable housing will likely require additional federal funding to HUD and commitment from state and other local governments, as well as additional incentives or regulations to promote the development of new housing units.
Additional collaborators for this project include the agencies and organizations that are part of the United States Interagency Council on Homelessness.16 The plan could include cross-sectoral initiatives that draw on resources from the health sector, such as a joint voucher program between HUD and HHS, MLPs to address housing problems within the clinical setting, and local investments in civil legal services and eviction prevention programs to help families stay in their homes during a short-term economic crisis.
Recognizing that reducing child poverty is a critically important, foundational strategy for improving child health outcomes and reducing health inequity, the committee recommends three key ways to ensure that families have the resources needed to meet children’s basic needs. Founded in the review of the evidence of health impacts and the committee’s expertise, the recommendation is based on increased resources for access to food and stable housing and income support in the form of a child allowance:
The costs of providing more resources to families with young children by increasing SNAP benefits, housing assistance, or a child allowance depend on many parameters, including the size of the benefit per family
___________________
16 The collaborators in this council are the Corporation for National and Community Service, General Services Administration, HHS, HUD, Office of Management and Budget, SSA, U.S. Department of Agriculture, U.S. Department of Commerce, U.S. Department of Defense, U.S. Department of Education, U.S. Department of Energy, U.S. Department of Homeland Security, U.S. Department of Justice, U.S. Department of Labor, U.S. Department of the Interior, U.S. Department of Transportation, U.S. Department of Veterans Affairs, U.S. Postal Service, and the White House Faith and Opportunity Initiative. See https://www.usich.gov (accessed June 15, 2019) for more information.
and how many families are eligible and take up the benefit. Changes in these benefits may induce changes in parent employment, earnings, and receipt of other public benefits, affecting the total cost to the government. Full-scale analysis of the cost and behavioral changes of these proposals was beyond this committee’s scope; however, the work of the National Academies’ Committee on Building an Agenda to Reduce the Number of Children in Poverty by Half in 10 Years in the report A Roadmap to Reducing Child Poverty does provide some illustrative examples of cost estimates. Using the Urban Institute’s TRIM3 simulation model, the total change in annual government spending was estimated for a range of policy options (see the full report for the policy details and model assumptions). The change in government spending of increasing SNAP benefits by 20 percent was estimated at $26,414 million, including employment and earnings adjustments (NASEM, 2019, p. 533). The cost of increasing housing vouchers by 50 percent was similar ($24,134 million) (NASEM, 2019, p. 537). In contrast, the estimate for a child allowance of $2,000 per year for families with children ages 0–16 was $32,904 million (NASEM, 2019, p. 549).17 A child allowance for families with children under age 6 would be considerably less costly. The actual costs of expanding SNAP or housing programs or creating a child allowance will depend on the size and scope of the program. Future research is needed to investigate how to implement these programs cost effectively and so that they will yield the greatest health benefits.
Increasing resources available for families with young children to meet their basic needs is of utmost urgency given the science-based connections between health and income for healthy development of young children and their later health and educational outcomes. While the National Academies’ Committee on Building an Agenda to Reduce the Number of Children in Poverty by Half in 10 Years recommended other important strategies, such as expanding the EITC or the Child and Dependent Care Tax Credit and increasing minimum wage, this committee’s recommendation focuses on strategies that are likely to have particularly important impacts on health outcomes for young children. These include a child allowance targeted at families with young children not yet in K–12 school and increasing SNAP benefit levels and housing assistance. A child allowance would fill in some of the gaps in the current safety net and particularly benefit the lowest-income children and those most at risk of poor health outcomes. The key advantage of a child allowance (over, for example, tax credits) is that funds are available to
___________________
17 It is important to note that these estimates are net costs to the government, and they are not suitable for comparison to other cost estimates cited in this chapter.
families on an ongoing, monthly basis rather than once per year. In addition, under the current structure of the child and working family tax credits, the lowest-income families receive few benefits. Children whose parents are in unstable employment or not employed suffer the short- and long-term health consequences of living in poverty. Reducing health disparities requires reaching these children during their earliest years, regardless of parental employment. Increased SNAP benefits and housing allowances would address current inadequacies in both of these programs and provide targeted support for the critical food and housing needs of young children. Paid parental leave would also recognize and support the special needs of the earliest years, in which parental time and attention are critically important for children’s health and development.
Another way to increase resources to families with young children would be to provide more funding to subsidize child care. For example, the National Academies’ Committee on Building an Agenda to Reduce the Number of Children in Poverty by Half in 10 Years included the expansion of child care subsidies as one of their options for reducing childhood poverty, and guaranteeing access to subsidies for families below 150 percent of the federal poverty level would significantly increase resources available to low-income, working families. As noted in Chapter 3, only 15 percent of eligible families received Child Care and Development Block Grant subsidies in 2012 (Walker and Matthews, 2017). However, these subsidies would flow only to families who meet the work requirements and use an eligible care provider, so these resources would be less likely to help families in deep poverty or those with intermittent employment. While child care subsidies are an important work support for low-income families, the committee focused on programs with more evidence of positive effects on children’s health and those not dependent on parental employment. As noted earlier in this chapter, expansions of the work-oriented safety net programs may have unintended negative consequences for child health if parent employment results in lower rates of breastfeeding or disruptions to the attachment between infant and caregiver. In order to provide supports for all children, it is important to supplement work-support programs with basic support for families with young children that is not tied to employment.
In addition to material resources to meet their basic needs, children need a nurturing and healthy environment, responsive and sensitive caregiving free of maltreatment, and opportunities to develop the socio-emotional and cognitive skills to be healthy and resilient. Families with adequate resources may be better able to provide these important determinants of health, yet income alone may not be sufficient to ensure positive health outcomes. Thus, while addressing families’ basic material
needs is a critically important strategy for improving health outcomes of young children, strategies that focus only on reducing child poverty are unlikely to be sufficient to eliminate poor health outcomes and health disparities in early childhood. Specific recommendations with regard to the child’s environment and the importance of relationships are discussed in other chapters of this report. The importance of confronting and eliminating structural racism in order to eliminate health disparities is discussed in Chapters 3 and 8.
NEIGHBORHOOD CONDITIONS
Neighborhoods play a critical role in the health, well-being, and development of children. Those that provide families with access to high-quality education, employment opportunities, safety, high-quality health care, and other essential services are essential to supporting children’s healthy development. Persistent and increasing economic inequality, however, has contributed to neighborhoods facing increased economic segregation and concentrated poverty whose conditions and lack of resources can negatively affect healthy development and limit opportunities for children to flourish.
Neighborhood conditions can be defined broadly as the overall community context that is shaped by the natural and built environment (e.g., housing structures and conditions, availability of sidewalks and open/green space, presence of vacant lots, environmental exposures) and the availability or lack of health-promoting goods and services (e.g., access to healthy foods, affordable and safe transportation), in addition to the social environment (e.g., community cohesion, residential segregation, violence). This section addresses neighborhood conditions broadly; other sections in this chapter discuss the evidence related to specific neighborhood-level factors, such as housing, environmental exposures, food security, and economic security.
Concentrated Disadvantage
Residential segregation persists in the United States and has contributed to neighborhoods experiencing concentrated disadvantage where intergenerational cycles of poverty and adversity can derail children’s healthy development. Data from the 2010–2014 American Community Survey show that residential segregation by race and ethnicity has begun to decline slightly (Frey, 2015); however, economic residential segregation has increased (Rusk, 2017; Taylor and Fry, 2012).
Residential segregation, by race and ethnicity and by socioeconomic status and income, increases racial health disparities and has pronounced
effects on children’s health outcomes. Its effects include socioeconomic disadvantages, such as limited opportunities for high-quality education and employment; increased exposure to crime, violence, and environmental toxicants; and limited access to transportation options, healthy food options, and health care services, which in turn leads to disparities in the quality of services and treatment (Acevedo-Garcia et al., 2008). For children in particular, segregation limits their access to high-quality schools and after-school programs and to neighborhoods in which they can play and exercise safely (Acevedo-Garcia et al., 2007, 2008).
Although policies that promote and increase segregation (including Jim Crow laws, redlining, and discriminatory banking and foreclosure practices) no longer exist overtly, their effects have persisted and remain widespread in communities experiencing intergenerational poverty and trauma. Segregation limits socioeconomic resources available to those living in concentrated poverty and has resulted in disparities in rates of disease, availability of high-quality health care providers, and opportunities to engage in health-promoting behaviors. Its effects have also included access to a higher density of alcohol, tobacco, and fast food outlets, increased risk of exposure to environmental hazards and toxicants, and higher risk of exposure to violence. For more information on the historical and contemporary effects of segregation policies, see Chapter 3 of NASEM (2017), or Reskin (2012).
Exposure to Violence
Exposure to neighborhood crime and violence can significantly affect children’s cognitive (Burdick-Will, 2018; Sharkey, 2010), emotional and behavioral (Kim et al., 2014; McCoy et al., 2016; Sharkey et al., 2012), and health outcomes. Improving neighborhood conditions to diminish exposure to crime and violence plays an important role in reducing children’s biological stress and improving their health outcomes. For more on exposure to violence as an adverse childhood experience, see Chapter 3.
In addition to adversity faced at the individual level, repeated exposure to crime and violence can contribute to community trauma. A report by the Prevention Institute describes that “community trauma is not just the aggregate of individuals in a neighborhood who have experienced trauma from exposures to violence”; rather, symptoms of community trauma “are present in the closed-cultural environment, the physical/built environment, and the economic environment” (Pinderhughes et al., 2015). The report describes several community strategies to implement within each of these three environments to mitigate the negative effects of community trauma, build more resilient communities, and improve
health and well-being outcomes (see Figure 6-3). The authors note that across all environments, approaches that are most effective will “build on indigenous knowledge, expertise, and leadership to produce strategies that are culturally relevant and appropriate” (Pinderhughes et al., 2015, p. 5).
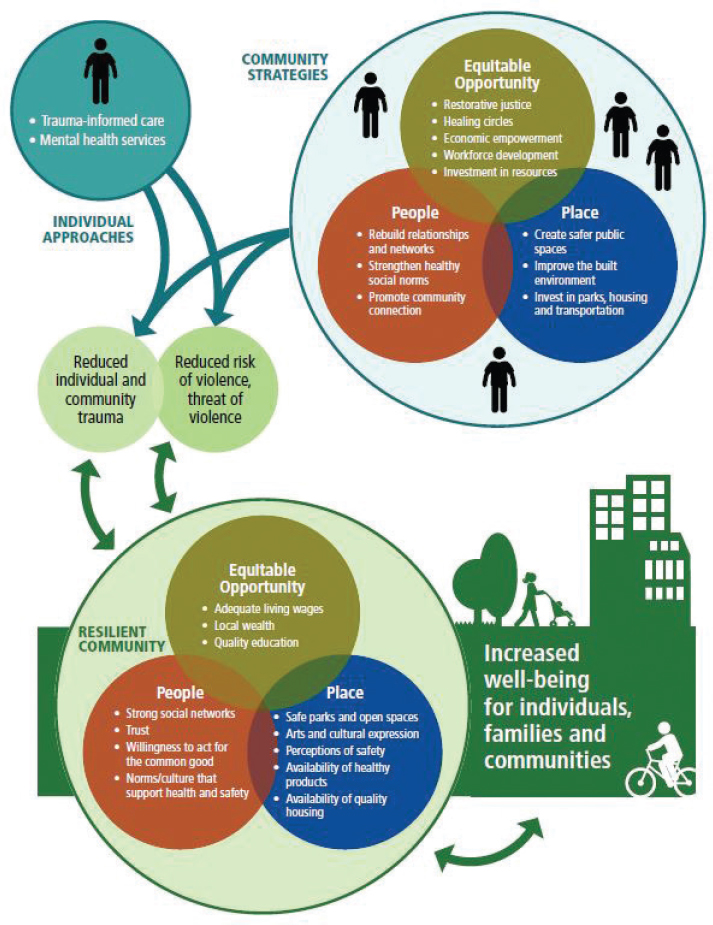
SOURCES: Pinderhughes et al., 2015; figure provided by Prevention Institute, www.preventioninstitute.org.
Improving Neighborhood Conditions
HUD’s Moving to Opportunity (MTO) study provides clear evidence that better neighborhood conditions are strongly associated with improved health and development outcomes (Kling et al., 2007; Ludwig et al., 2013). MTO randomized assistance designed to help low-income families move to less impoverished neighborhoods; after 10–15 years, adults chosen to receive that assistance had lower prevalence of obesity and diabetes and better subjective health outcomes than adults who were selected not to receive it (Ludwig et al., 2011). Despite these positive findings, the MTO experiment has also yielded mixed results. Early MTO studies resulted in findings that ran counter to the hypothesized outcomes; for example, Sanbonmatsu et al. (2006) found no evidence of improvement in academic outcomes for any age group 4–7 years after randomization. As noted previously in the chapter, Chetty et al. (2016) found strong evidence to suggest that children who moved to lower-poverty neighborhoods when they were young (i.e., under 13 years of age) were more likely to experience positive outcomes later in life, such as attending college and earning higher incomes. However, the study also showed contrary outcomes for those who moved when they were older. Other research indicates that while girls in the MTO experiment exhibited positive mental health outcomes (e.g., decreased rates of major depression and conduct disorder), boys experienced the opposite (e.g., increased rates of posttraumatic stress disorder, major depression, and conduct disorder) (Kessler et al., 2014). In terms of long-term outcomes (i.e., 10–15 years), Ludwig et al. (2013) concluded that moving to lower-poverty neighborhoods during childhood leads to improvements in adult physical and mental health, but not economic self-sufficiency.
MTO established that places matter for health but not what it is about them that matters most: it was not designed to tease apart which aspects of places drove those health improvements, nor did it specifically address prenatal or birth outcomes. Other studies have attempted to further illuminate which aspects of a neighborhood—for example, better economic environments, built environment features that promote healthy lifestyles, or improved social cohesion—might represent the most important levers for improving health and birth outcomes. Other than MTO, however, randomized studies on place and its impacts on health are extraordinarily rare, so the evidence is almost entirely limited to observational studies.
The Washington Center for Equitable Growth describes two approaches to addressing segregation within neighborhoods: (1) invest in neighborhoods to make the consequences of segregation less severe, and (2) reduce the level of segregation in neighborhoods directly (Sharkley, 2016).
Approaches to increase and shift investments to low-income communities include
- Providing work supports (including supplemental wages and guaranteed public service jobs, as in the New Hope program, and services to residents of public housing developments and rent incentives to encourage work, as in the Job Plus program) for individuals and families in high-poverty communities;
- Investing in evidence-based programs for young people, such as those that include tutoring or mentoring, sports activities, cognitive behavioral therapy, and summer jobs, which randomized trials have shown lead to increases in academic achievement and decreases in involvement in crime and violence;
- Identifying and/or establishing a single institution in every low-income neighborhood “that takes ownership over the community and takes responsibility for all the residents within it, . . . so that everyone within that neighborhood knows that there is going to be an institution serving them for the long haul and will have resources sufficient to bring about long-term change” (Sharkley, 2016).
Addressing the lack of affordable housing is crucial to reducing segregation in neighborhoods directly (Sharkley, 2016). To improve housing affordability, the Washington Center for Economic Growth provides the following approaches:
- Expanding the supply of housing vouchers. (See the following section on Housing Affordability for more on housing vouchers.)
- Providing support to allow families to access opportunity neighborhoods.
- Providing incentives and regulations to preserve and expand affordable housing in exclusive markets.
- Establishing a long-range mobility bank (Sharkley, 2016).
In developing approaches to enable families to access opportunity neighborhoods, an important consideration is ensuring that adequate supports are available to families to buffer the negative effects of stress associated with moving to other communities. For an example of a promising initiative that aims to support and strengthen families by providing community-based supportive services, see Box 6-6.
ENVIRONMENTAL EXPOSURES AND EXPOSURE TO TOXICANTS
Each year, Americans are exposed to chemicals in the environment at increasingly greater levels. EPA tracks new chemical substances in its Toxic Substances Control Act (TSCA) Chemical Substance Inventory,
which is updated every 6 months (EPA, n.d.-c). Currently, more than 85,000 chemical substances are listed in the TSCA inventory, with companies introducing about 700 new substances each year (EPA, n.d.-a; Tollefson, 2016). As described in Chapter 3, many of these substances are related to poor health outcomes for mothers, infants, and children. In its review of the literature, the committee found that children (from fetal development through early childhood) are at greater risk than adults from adverse health effects of environmental exposures due to their smaller size and proportionally large intake of food, air, and water to body weight and are subject to rapid developmental processes that may be influenced and disrupted by chemicals and toxicants. Parents’ exposures to environmental toxicants in the preconception phase also present a risk to early
child development. Furthermore, as a result of exposure to toxicants, children are more likely than adults to suffer from developmental problems, chronic conditions, and death. The committee also concludes that
The following section provides a review of the limited research currently available that specifically examines policies and practices to reduce the risk of environmental exposures among preconception, prenatal, and postnatal populations.
Reducing the Risk of Environmental Exposures in the Home and in Child Care Settings
The Center for Medicaid and CHIP Services (CMCS) serves millions of pregnant women, children, and families by providing health care access to low-income families and families who would not otherwise qualify for health insurance. CMCS also establishes reimbursement criteria for these health services, including environmental exposure screening, testing, and case management. How these criteria are implemented varies by state, though some aspects of coverage are mandatory. For example, blood lead screening is mandated for Medicaid recipients at 12 and 24 months of age. However, states vary in how this mandate is implemented (CMS, n.d.). Some states provide these screenings only to Medicaid-enrolled children, while others offer universal screenings; one state, Arizona, has chosen to implement a targeted screening approach (Arizona Department of Health Services, 2017; CMS, 2016), while still others do not currently have a lead screening program (Dickman, 2017; NASHP, 2018). Moreover, some states require reporting the results to state health departments or the state lead registry, which may result in follow-up care or case management. Other states do not have a registry or other tracking system, and still others do not provide any form of follow-up to children with elevated BLLs.
Medicaid can cover home investigations of lead exposures, case management for exposed children, and support to states to implement education, screening, and outreach efforts to areas at high risk of lead exposure (CMS, 2017), though it is unclear how these programs are applied at local levels. In addition, greater collaboration with tribal nations is needed to improve state screening and registry efforts (PTFCEH, 2018), though some federally funded research studies have led to tribal law and policy
updates to improve lead screening among children (Petersen et al., 2007). No other screening programs aimed at environmental exposures receive Medicaid support; lead exposure is an exception because of the estimated magnitude, frequency, and duration of exposure, the significance of the health impacts, and the potential for prevention (NASHP, 2017). However, several states have asserted regulatory authority over other environmental toxicants, including bisphenol A (BPA), cleaning agents in schools, and flame retardants (NCSL, 2017).
Child care settings represent another source of potential environmental exposures for children. With more than 13 million preschoolers in child care every day, including 6 million infants and toddlers (Amoah et al., 2016) (see Chapter 3 for more information on the number of children enrolled in various ECE programs), addressing potential environmental exposures in child care settings could reduce the risk of related health issues for a large proportion of children under age 6. Taking steps to address potential exposures can present challenges, as child care facilities may be located within individual homes, community centers, and office buildings, which may not be consistently assessed or regulated to reduce the risk of environmental exposures. Moreover, licensing guidelines vary, with limited requirements addressing child care provider training on mitigation of early childhood exposures. Reviewing existing state policies on the regulation of environmental exposures in child care facilities offers policy makers an opportunity to compare policy approaches and consider nonregulatory approaches to effect change (Environmental Law Institute, 2015).
In addition to reviewing existing policies, evaluating the effectiveness of training programs can also inform decision making around environmental exposure risk reduction. In a study of 60 child care centers in Washington, DC, an environmental risk assessment training was developed and tested that covered the following areas: (1) air quality, (2) arsenic, (3) asbestos, (4) built environment, (5) chemicals in art supplies, (6) lead, (7) mercury, (8) mold, (9) noise pollution, (10) pesticides and integrated pesticide management, (11) physical education and nutrition, (12) plastics, (13) radon, and (14) safe cleaning alternatives (Amoah et al., 2016). More than 580 child care workers received the training and pre-/ post-assessments, and knowledge scores increased by about 20 percent, on average, between the two assessments. Nearly 70 percent of participating child care centers reduced their environmental risk assessment scores. This training is an important approach to reducing the environmental risk for children receiving child care outside the home.
Educational approaches are also effective at the level of the individual household. In a meta-analysis of seven community health worker–delivered interventions focused on reducing asthma symptoms, most of
these significantly decreased asthma symptoms, lessened daytime activity limitations, and reduced emergency and urgent care use (Postma et al., 2009). Programs that included higher intensity and frequency of home visiting reported the most positive health outcomes. Similarly, in a systematic review of 20 studies focused on reducing the risk of asthma morbidity among children, most of them were effective in significantly reducing the number of days with asthma symptoms, school days missed, and asthma acute care visits (Crocker et al., 2011). The review examined studies expressly focused on informing multitrigger, multicomponent, home-based environmental interventions, which address the complex nature of reducing asthma risk within the home due to the many potential sources of risk. A randomized controlled trial aimed at educating pregnant women on reducing exposure to hazardous air pollutants resulted in a significant increase in preventive behaviors (Marzieh et al., 2017), demonstrating that interventions aimed at parents can also be effective in reducing the risk of toxic exposures for infants and children.
Reducing the Risk of Environmental Exposures in the Community
In a 2018 study, researchers linked 2011 National Emissions Inventory data with block groups from the 2009–2013 American Community Survey data (Mikati et al., 2018). For particulate matter of 2.5 micrometers or less in diameter (PM2.5), those living in poverty and people of color experienced significantly higher levels of exposure compared to white individuals. Racial disparities, particularly for black Americans, were greater than for those living in poverty alone (Mikati et al., 2018). In a subsequent 2019 study, researchers found that, on average, non-Hispanic whites experience a “pollution advantage” (Tessum et al., 2019). In other words, they experience 17 percent less air pollution exposure, comparing the amount to which they are exposed and the amount that they are responsible for due to their consumption levels. In comparison, black and Hispanic Americans, on average, experience 56 percent and 63 percent excess exposure, respectively, relative to the exposure caused by their consumption (Tessum et al., 2019). While PM2.5 exposure for all groups fell about 50 percent between 2002 and 2015 due to increased regulation and population density reductions near polluted areas, the inequities remain above and beyond this reduction. Scientists suggest addressing these inequities will likely require multilevel approaches, including reducing consumption levels, improving manufacturing and other processes to minimize pollution, and implementing more comprehensive measures, such as evaluating plans for construction and urban development with the purpose of reducing dependence on automobile transportation to manage and lessen current inequities, along with meaningfully involving communities in assessment processes to effect broader policy change (Schulz et al., 2016).
For example, researchers collaborated with the Rural Empowerment Association for Community Help in North Carolina to train middle schoolers to assess asthma indicators, lung function, and air pollution (Guidry et al., 2014). School administrators and students reported positive perspectives on the project, which offers an example for community-based research aimed at improving air pollution in rural settings (Guidry et al., 2014). In another example, the Community Action to Fight Asthma Initiative in California used an environmental justice approach to reduce risk factors for asthma in school-aged children. Statewide coalitions, which included local residents and technical assistance experts, supported policies to reduce children’s exposures to environmental triggers. Technical assistance, community involvement, and multilevel strategies led to policy change that addressed reduction of environmental inequities (Kreger et al., 2011).
The BREATHE Project based in Barcelona, Spain, which aimed to assess traffic-related air pollutant exposure among schoolchildren, is a promising example of using complex measures and modeling to reduce pollutant exposure (Rivas et al., 2018). Using advanced measurement and statistical techniques, researchers identified eight factors/sources of pollutants, including minerals, traffic, road dust, secondary sulfate and organics, secondary nitrate, sea spray, heavy oil combustion, metallurgy, and organic/textile/chalk, and were able to characterize the air quality within and near 39 urban schools. This novel approach allows for detailed mapping of exposure risk, which supports positive policy change through data-driven decision making.
Community Infrastructure
Sustainable infrastructure is defined as
systems that have the capacity to endure over a long period of time; enabling the human-built environment to thrive and providing an opportunity for human society to improve its quality of life, without compromising the integrity and availability of natural, economic, and social assets for future generations. (Hendricks et al., 2018, p. 2)
Properly managing infrastructure (i.e., replacing lead drinking water pipes, mitigating flood zones to reduce damage to homes and schools, and updating technology to ensure timely notification of emergent hazards) through the lens of assessing and maximizing sustainability therefore has important downstream implications for public health. This is particularly the case with respect to ensuring that the necessary environment and resources are equitably available to support early childhood development and minimizing exposures to harms that arise from poor infrastructure, lack of sustainable practices, and the concomitant effects on the environment. Moreover, reducing these risks can lead to
cost savings. For example, the annual U.S. cost of environment-related pediatric disease in 2008 was estimated to be $76.6 billion, or 3.5 percent of total health care costs (Trasande and Liu, 2011). These costs are limited to pediatric diseases caused by environmental exposures. Including costs of pediatric diseases resulting from severe climate conditions’ impact on aged or damaged infrastructure, such as heat-related deaths and illnesses and increased exposures to lead and other toxicants, mold and poor water quality from flooded and damaged dwellings, and poor air quality from increased forest fire smoke and smog, could support prioritization and decision making to best address failing infrastructure.
The United States currently faces a critical infrastructure crisis (Maxwell et al., 2018) as a result of decades of deferrals at every governmental level and lack of effective accountability on the side of private institutions to ensure essential infrastructure received necessary upgrades, including improvements that would minimize negative environmental impacts and ensure long-term sustainability (ASCE, 2017). Using strategies such as the framework put forth by Koehler et al. (2018) for improving community health through better environment decision making could provide important approaches to mitigate future harms and reduce costs. In addition, existing models do not specifically examine risks to early childhood development and ensuing costs. Additional research and environmental assessments are needed to ensure harms are minimized, especially for populations who are disproportionately impacted by harmful environmental exposures. Investing in the rebuilding of the nation’s infrastructure at every level—waste and water management, walkable streets and parks, cleanup of toxic waste sites, and so on—along with strengthening capacity for community engagement and civil rights actions around environmental justice can provide a cross-sector approach that strengthens infrastructure in the United States, reducing potential harms to infants and children and ensuring lower medical costs for pediatric injury and disease associated with severe climate effects.
The Role of Civil Rights
Civil rights strategies are an important yet underused tool to promote clean and healthy communities for developing children. This was acknowledged as a community-driven solution to promote health equity in the 2017 National Academies report Communities in Action: Pathways to Health Equity. The report asserts that “civil rights, health, and environmental justice laws and policies provide a framework to promote equal access to publicly funded resources and prohibit discrimination based on race, color, national origin, income, gender, disability, and other factors” (NASEM, 2017, p. 351). Federal laws and civil rights legislation have
historically been a codified source of rights to protect individuals and groups from harmful environmental exposures (see, for example, Title VI of the Civil Rights Act of 1964,18 the National Environmental Policy Act,19 and the Clean Water Act20). In 1994, an executive order was issued on Federal Actions to Address Environmental Justice in Minority Populations and Low-Income Populations.21 Civil rights laws and their enforcement not only aim to protect populations in at-risk contexts—thereby reducing disparities—but also allow for a crosscutting approach that can apply to many of the determinants of health and development discussed in this report (e.g., housing, environmental exposures, education). (See Hahn et al. [2018] for a brief summary of civil rights history and discussion on the relationship between civil rights laws and the determinants of health.) Specifically, civil rights strategies can be used to mitigate discriminatory burdens, lower or remove barriers to community participation in decision making, and improve access to health and environmental benefits that are foundational to safe and healthy communities (NASEM, 2017; USDA, 2012).
At the state level, California’s EPA operates an Environmental Justice Task Force, which develops initiatives in communities where compliance and enforcement can help mitigate or stop the harmful effects of exposure to pollution. At the community level, there are tools that can be employed to ensure that these rights are protected to engender equitable outcomes for children and families. For example, public health, civil rights, and environmental justice practitioners use a five-step planning framework by which to assess proposed or current environmental policies or practices for their potential to harm or benefit communities (Environmental Justice Leadership Forum on Climate Change, 2016; NASEM, 2017; The City Project, 2016)22:
- Describe what is planned in terms that are understandable to the community;
- Analyze the benefits and burdens on all people;
- Analyze alternatives to what is being considered;
___________________
18 Title VI of the Civil Rights Act of 1964 (42 U.S.C. § 2000d to 2000d-7): “No person in the United States shall, on the ground of race, color, or national origin, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity receiving Federal financial assistance” (DOL, n.d.).
19 42 U.S.C. § 4321 et seq.
20 33 U.S.C. § 1251 et seq.
21 E.O. 12898. 59 FR 7629; February 16, 1994.
22 This planning framework is based on Title VI, Executive Order 12898, case law, and best practices by federal agencies (NASEM, 2017).
- Include people of color, low-income people, and other stakeholders in every step in the decision-making process; and
- Develop an implementation plan to distribute benefits and burdens fairly and avoid discrimination.
(See NASEM [2017] for a more in-depth discussion about the planning process, in addition to a few examples of communities that have successfully applied the process.)
The Communities in Action: Pathways to Health Equity report (NASEM, 2017) also outlines some guidance for civil rights attorneys, public health professionals, community groups, public agencies, recipients of public funding, foundations, and other stakeholders to advance equity using civil rights tools (see Box 6-7 for a listing of these guiding strategies).
Finally, based on the committee’s expertise and its review of civil rights legislation, literature, and past action to address equitable access to the health-promoting social determinants, the authoring committee of
Communities in Action: Pathways to Health Equity reached the following conclusions in its report:
Civil rights approaches have helped mitigate the negative impacts of many forms of social and health discrimination. Continuing this work is needed to overcome discrimination and the structural barriers that affect health.
Using civil rights approaches in devising and implementing community solutions to promote health equity can guard against unjustified and unnecessary discriminatory impacts, as well as against intentional discrimination in programs that affect health. For example, those implementing community solutions can employ methods and data in ways that include full and fair participation by diverse communities. (NASEM, 2017, p. 362)
Given the critical role of civil rights strategies in advancing health equity in communities, the report also included a recommendation to foundations and other funders to expand their community support beyond their traditional roles by supporting education, compliance, and enforcement related to civil rights law and other areas (see Recommendation 7-1 in NASEM [2017] for the full recommendation). The report acknowledges the barriers associated with federal tax laws that may preclude foundations from supporting such activities, but it also suggests the use of general operating funds as opposed to program-specific funds (NASEM, 2017). The alignment between this report and Communities in Action with respect to health equity and the applicability of civil rights strategies for addressing environmental exposures in communities warrants serious consideration of these findings and the abovementioned recommendation for promoting healthy and equitable early development.
Leveraging Clinical Settings to Reduce Environmental Exposure Risk
Recent evidence confirms that preconception and prenatal exposures can adversely impact fetal development, which may result in long-lasting health effects (Grandjean et al., 2015). Training tools for health practitioners offer a potentially promising prevention approach to reduce harmful environmental exposures and the risk of future adverse health effects for prenatal and preconception patients (Sathyanarayana et al., 2012). In a national online survey of more than 2,500 obstetricians, nearly 80 percent agreed that they can reduce patient exposures to environmental health hazards by counseling patients. However, half of respondents reported that they rarely take an environmental health history course, and less than 20 percent reported routinely asking about environmental exposures commonly found for pregnant women in the United States. Moreover, only 1
in 15 reported having any training on how to assess environmental exposures among patients (Stotland et al., 2014), demonstrating the need for additional supports for providers, particularly given the complexity of the assessment process. There are several online tools for providers to use to triangulate exposure risk, yet the sheer number of possible chemical exposures, the relatively limited data available on possible risks, and the expertise and time commitment needed to complete an assessment may pose significant challenges for primary care or specialty providers (Koehrn et al., 2017).
Medical Education on Environmental Health
Education on the effects of preconception and prenatal exposure to environmental toxicants is largely insufficient in medical education and curricula (Gehle et al., 2011; Tinney et al., 2015). Pediatric practice, which has historically recognized the influence of environmental health exposures (Tinney et al., 2015), is an important setting to screen for exposure to environmental toxicants. However, there are also earlier opportunities to identify and ensure timely treatment for harmful exposures during the preconception and prenatal periods (Tinney et al., 2015). Many professional organizations have emphasized the urgency and importance of addressing exposure to environmental toxicants. In a joint committee opinion from the American College of Obstetricians and Gynecologists (ACOG) Committee on Health Care for Underserved Women and the American Society for Reproductive Medicine (ASRM) Practice Committee, ACOG and ASRM call for “timely action to identify and reduce exposure to toxic environmental agents while addressing the consequences of such exposure” (ACOG, 2013). The International Federation of Gynaecology and Obstetrics, a professional organization of obstetrical and gynecological associations from 125 countries that includes ACOG, states that “obstetricians, gynecologists, midwives, women’s health nurse practitioners, nurses, and other health professionals should . . . make environment health part of health care” and that “exposure to toxic environmental chemicals during pregnancy and breastfeeding is ubiquitous and is a threat to healthy human reproduction” (Di Renzo et al., 2015). However, despite broad consensus on the importance of addressing exposure to environmental toxicants, studies show that many obstetricians and gynecologists do not screen their patients for harmful environmental exposures (Grindler et al., 2018; Stotland et al., 2014).
While qualitative data suggest that pediatricians express an interest and need for more training on environmental medicine topics (e.g., environmental history) (Kilpatrick et al., 2002; Trasande et al., 2006), this type of education is not routinely included in pediatric curricula (Roberts and Gitterman, 2003). The National Environmental Education and Training
Foundation and the Children’s Environmental Health Network formed two working groups with expertise in medical and nursing education to explore opportunities to incorporate environmental health into pediatric education (McCurdy et al., 2004). After reviewing the transition from undergraduate student to professional status, the medical education working group recommended improving education about children’s environmental health in medical school curricula, residence, training, and continuing medical education in addition to expanding fellowship training in children’s environmental health. The nursing working group similarly recommended enhancing content on children’s environmental health at the undergraduate, graduate, and continuing nursing education levels. Both working groups identified leverage points (i.e., key organizations and stakeholders) that could facilitate these changes.
There are several existing resources and strategies to accelerate the integration of environmental health into existing medical education and curricula. A work group of faculty members and residents23 formed at a meeting convened by the Mid-Atlantic Center for Children’s Health and the Environment and The George Washington University’s Department of Obstetrics and Gynecology identified several approaches to better incorporate environmental health into medical education, including
- Integrating environmental health into basic science courses and the organ systems approach (Gehle et al., 2011) into medical school and residency curricula;24
- Implementing clinical training programs on environmental health, such as the model established by the University of California, San Francisco, Program on Reproductive Health and the Environment;25
- Adding questions on environmental health to resident training and board-certifying exams26 to ensure that programs will include environmental health in their curricula;
___________________
23 Faculty members and residents who participated in the meeting represented 16 academic obstetrics-gynecology programs from 5 states (Delaware, Maryland, Pennsylvania, Virginia, and West Virginia) and Washington, DC.
24 The George Washington University’s Department of Obstetrics and Gynecology has a medical school and residency curriculum on environmental health specifically for obstetricians and gynecologists (Tinney et al., 2015).
25 PHRE includes rotations programs for obstetrics-gynecology clinical trainees and maternal-fetal medicine fellows, as well as resources such as educational materials for patients and environmental health history forms for clinical practice for reproductive health professionals (Tinney et al., 2015).
26 Such as those administered by the Council on Residency Education in Obstetrics and Gynecology, American Board of Obstetrics and Gynecology, and American Osteopathic Board of Obstetrics and Gynecology (Tinney et al., 2015).
- Training leaders in medical education and faculty members on reproductive environmental health through the Association of Professors of Gynecology and Obstetrics; and
- Requiring continuing education in environmental health27 to ensure that practicing obstetricians and gynecologists receive introductory education to environmental health (Tinney et al., 2015).
There are also resources to support providers in offering their patients counseling and health education on environmental exposures. Located across the United States and Canada, Pediatric Environmental Health Specialty Units are a national network of experts in reproductive and children’s environmental health who are located at academic medical centers and provide medical information and advice and respond to requests for information on the prevention, diagnosis, management, and treatment of the effects of environmental exposures on children and adults of child-bearing age (PEHSU, n.d.). AAP publishes a guide for pediatricians, Pediatric Environmental Health, which is meant to help identify, prevent, and treat pediatric environmental health problems (AAP Council on Environmental Health, 2012).
Similarly, the Organization of Teratology Information Specialists provides an online service known as MotherToBaby that provides evidence-based information on the safety of medications and other exposures during pregnancy and while breastfeeding to health care professionals and the general public (MotherToBaby, n.d.). Lastly, a collaborative initiative28 known as SafetyNEST provides health care professionals and the general public with “accurate, evidence-based, and personalized information about the effects of toxic chemicals on prenatal and early childhood health” through an educational online platform (SafetyNEST, 2018).
Research, Monitoring, and Testing of Environmental Exposures
Existing conceptual frameworks fail to encapsulate the complexities inherent in early childhood development. The Public Health Eposome Conceptual Model attempts to capture the changing nature of these exposures, along with the life course considerations needed to accurately assess risk (Tulve, 2016). In particular, children may experience chemical
___________________
27 The Agency for Toxic Substances and Disease Registry has created online resources on environmental health, including case studies on environmental medicine, for health professionals completing continuing education (Gehle et al., 2011; Tinney et al., 2015).
28 Partners include the University of California, San Francisco, Program on Reproductive Health and the Environment; Icahn School of Medicine at Mount Sinai, American Medical Women’s Association, and Universidade Federal do Paraná in Brazil (SafetyNEST, 2018).
exposures from their environments at every life stage throughout the life course. Children are exposed to chemicals in foods, water, air, and surfaces they touch, such as chemical residues on surfaces or in dust and soil. Revising existing conceptual models aims to improve evaluation and assessment of environmental exposures to improve accuracy, enhance the overall fit of statistical modeling, and ensure improved predictive power in research studies examining environmental exposures and effects on early childhood development.
In another approach, a conceptual framework relying on a holistic approach to maternal and child health research includes both psychosocial stressors and environmental hazards to better explain factors that influence poor health outcomes for populations that experience higher risks of environmental exposure. This approach makes it possible to include chronic stressors and environmental hazard exposures to better understand health inequities evident across income levels and racial and ethnic groups in the United States (Morello-Frosch and Shenassa, 2006).
Given the effect that environmental exposures have on some child mental health problems, researchers suggest “broadening outcomes to include dimensional measures of autism spectrum disorders (ASDs), attention-deficit hyperactivity disorder (ADHD), and child learning capacity, as well as direct assessment of brain function” (Rauh and Margolis, 2016, p. 1). Longitudinal studies examining these outcomes may inform how key exposures result in child mental health problems, which may better address or prevent these issues (Rauh and Margolis, 2016).
Existing Regulatory Approaches
The federal government plays an essential role in enhancing the resources and technical assistance available to states, tribes, and local agencies through programs, policy development, and implementation by the Centers for Disease Control and Prevention (CDC), EPA, U.S. Food and Drug Administration (FDA), U.S. Consumer Product Safety Commission (CPSC), and other relevant rule- and policy-making entities focusing on environmental exposures and children’s health. In addition, many of these agencies collaborate on joint initiatives to address environmental exposures among American children and families. For example, CDC monitors environmental chemicals in children’s blood, reports on trends over time, and establishes key recommendations for safe levels among children (CDC, 2019a). CDC also provides training and other resources to state, local, and tribal governments to support environmental health services, including tools focused on ensuring food safety and safe water (CDC, 2019b).
EPA also provides critical resources and supports to state, local, and tribal governments to reduce the risk of environmental exposures among children and to mitigate, if necessary, environments with high levels
of contaminants. For example, through the America’s Children and the Environment report, EPA reports on environmental health data, specifically concerning children, and establishes indicators to minimize potential adverse health outcomes related to environmental exposures. Areas of focus include criteria for air pollutants, drinking water contaminants, lead, mercury, cotinine, perfluorochemicals, phthalates, BPA, perchlorate, and certain health outcomes, such as respiratory diseases, childhood cancer, and neurodevelopmental disorders (EPA, n.d.-b). However, as EPA has noted, several scientific challenges exist with regard to children’s environmental health, including (1) the dispersion of data and information across systems that are difficult to access, (2) the need to assess environmental health from a systems perspective, (3) the need for new and more complex methods and models to evaluate risks specific to the early life stage of development and how exposures could result in health outcomes in later life stages, and (4) the need for translational research to better support community action and decision making (EPA, 2015). FDA regulates products and ensures the safety of food, including infant formula, the levels of BPA in food, and ingredients in cosmetics. For example, in 2014, the FDA BPA Joint Emerging Science Working Group reviewed the scientific literature on BPA effects on humans and found existing margins of safety to be adequate for exposure to BPA due to food contact (e.g., BPA exposures from coatings used in food containers) (FDA, 2014). Similarly, CPSC regulates products that are manufactured for children and that may be used by children. For example, CPSC limits the levels of phthalates in toys (GPO, 2017).
In addition to federal regulations, state environmental and public health agencies engage in efforts to prevent environmental exposures and to translate existing data and research findings into actionable policies and practices. For example, Washington State has enacted the Washington Children’s Safe Products Act to limit levels of lead, cadmium, phthalates, and certain flame retardants in children’s products (Department of Ecology, 2008). California (DTSC, n.d.) and Oregon (Oregon Health Authority, 2017) have implemented similar efforts to reduce the levels of toxic chemicals in consumer products. In all, there are at least 72 laws in 25 states addressing BPA, green chemistry, decabromodiphenyl ether, biomonitoring, and chemical safety (NCSL, 2014). However, the development and implementation of state regulations vary widely from state to state.
Frank R. Lautenberg Chemical Safety for the 21st Century Act
The Frank R. Lautenberg Chemical Safety for the 21st Century Act was enacted in 2016, with overwhelming bipartisan support, and gives EPA the authority to regulate or ban new and existing chemicals that pose a
risk to human health or health of the environment. Prior to this law, which amended the Toxic Substances Control Act, EPA bore the burden of proof to demonstrate that a chemical posed an “unreasonable risk” to public health or the environment. In addition, the law also required EPA to choose the “least burdensome” regulation with consideration of both public health and impact on the manufacturer (Gerlach, 2016). The law included new requirements for premarket testing of new chemicals (“EPA has to make an affirmative finding on the safety of a new chemical or significant new use of an existing chemical before it is allowed into the marketplace” [Camacho-Ramos, 2016]); ongoing risk evaluation of the toxicity of chemicals already in commerce (“EPA must develop a screening process for all existing chemicals that ranks them according to their level of risk, then develop a risk management strategy for chemicals that raise concerns” [Gerlach, 2016], and it is no longer required to select the “least burdensome” option); and a user fee (up to $25 million) charged to companies to cover the costs of risk evaluation. Importantly, for the first time, the law required EPA to specifically assess health threats to children, pregnant women, and other vulnerable populations (EDF, 2016). As of June 25, 2019, 60 new chemical reviews had been completed in May 2019. More than 2,300 new chemical reviews have been completed since enactment (EPA, 2019).
The President’s Task Force on Environmental Health Risks and Safety Risks to Children
The President’s Task Force on Environmental Health Risks and Safety Risks to Children was established by Executive Order 13045 in 1997.29 The Task Force was created with multidisciplinary and cross-sector membership, including representation from the U.S. Departments of Agriculture, Education, Energy, Housing and Urban Development, Justice, Labor, and Transportation. According to the executive order, the mission of the Task Force is to
Recommend to the president federal strategies for children’s environmental health and safety, within the limits of the administration’s budget, to include the following elements:
- statements of principles, general policy, and targeted annual priorities to guide the federal approach to achieving the goals of this order;
- a coordinated research agenda for the federal government, including steps to implement the review of research databases described in Section 4 of the executive order;
___________________
29 For more information, see https://ptfceh.niehs.nih.gov (accessed April 8, 2019).
- recommendations for appropriate partnerships among federal, state, local, and tribal governments and the private, academic, and nonprofit sectors;
- proposals to enhance public outreach and communication to assist families in evaluating risks to children and in making informed consumer choices;
- an identification of high-priority initiatives that the federal government has undertaken or will undertake in advancing protection of children’s environmental health and safety; and
- a statement regarding the desirability of new legislation to fulfill or promote the purposes of this order (Executive Order 13045, 1997).
Over the years, the Task Force has developed and published guidance on federal strategies to protect children from environmental health and safety risks. These publications include information on strategies and programs to address topics such as childhood asthma (PTFCEH, n.d.), healthy housing (Federal Healthy Homes Work Group, 2013), and lead exposures (PTFCEH, 2016a). The Task Force’s 2016 work plan identifies three areas of priority: (1) reducing lead exposures by addressing sources of lead (e.g., paint, drinking water, and consumer products), (2) protecting health in a changing climate by preparing families and communities to understand and mitigate the effects of climate change on children’s health, and (3) reducing the burden of environment-related illnesses by addressing the environmental origins of diseases to promote health and reduce health disparities (PTFCEH, 2016b). The work plan also delineates short- and long-term strategies for making progress on these three priority areas. The strategies offer a multipronged approach by identifying opportunities for communication and engagement, educational innovation, regulation and policy, and research.
National Research Approaches to Establish the Effects of Environmental Exposure
Fifteen years ago, spending on federal maternal and child health programs neared $57.5 billion. Most spending fell within HHS, but it also included several HHS agencies, as well as the U.S. Departments of Agriculture, Defense, Education, and HUD and EPA. A 2012 study examining these spending trends noted that supporting a continued focus on data sharing and integration of funding streams could yield synergistic effects and economies of scale. With a goal of realizing a coordinated, integrative maternal and child health (MCH) system, researchers recommended that federal, state, and local partners eliminate existing silos and increase community and consumer involvement (Kenney et al., 2012). It is unclear whether the federal government has attained these goals, and more
research would support a re-evaluation of whether the implementation of federal MCH funding has resulted in improvements in outcomes, data sharing, or improved community participation. In particular, it is unclear how federal spending furthers goals related to the elimination or mitigation of environmental exposures from preconception through age 8. Additional research examining federal funding linked to environmental exposures for these populations could support decision making at multiple levels and across agencies charged with regulation of environmental exposures.
In 2016, the National Institutes of Health introduced the Environmental influences on Child Health Outcomes (ECHO) Program, a group of more than 70 cohort studies aimed at understanding the relationship between environmental exposures and five main domains: upper and lower airways; obesity; pre-, peri-, and postnatal outcomes; neurodevelopment; and positive health outcomes (ECHO, 2019a,b). ECHO has enrolled a combined sample of more than 50,000 children (ECHO, 2019a,b). Exposures are measured from before birth to 5 years of age, and outcome data are collected through adolescence (Forrest et al., 2018). Nearly 150 cohort-focused articles have been published in the first 3 years of the project. In February 2019, the project received single institutional review board approval to begin the ECHO-wide cohort data collection protocol (ECHO, 2019a). While the multiple measures over time on the same participants in longitudinal research provide important information on possible cause and effect relationships, pooled cohort studies offer the advantage of being able to include a variety of different population groups and multiple variables at the same time.
National survey data also continue to play a vital role in our understanding of environmental exposures among children. Biomonitoring data in the National Health and Nutrition Examination Survey (NHANES) among preschool-aged children are limited (Calafat et al., 2017) but offer an important key to establishing exposure trends among children as young as 3 years old, using both parental report and analysis of biomarkers within urine samples. With these methods, researchers detected more than 37 chemicals in children aged 3–5 years, including plasticizers, combustion products, personal care–product chemicals, and pesticides (Calafat et al., 2017). NHANES data also offer the opportunity to establish benchmarks for environmental exposures among children, which enables programs and community-based efforts to improve interventions to reduce the risk of environmental exposures. For example, in a recent study of farmworkers, researchers measured a significant reduction in the levels of pesticide metabolites among parents and children who received an educational intervention on steps to reduce transmission of pesticides in the home (Griffith et al., 2018). Moreover, NHANES data were key in establishing that children exposed to higher levels of one chemical were
also exposed to higher levels of other chemicals (Hendryx and Luo, 2018), which may place them at higher risk for poor health outcomes.
Conclusions and Recommendations to Reduce Exposure to Environmental Toxins
Given the importance of safe early learning environments, as discussed above, the committee recommends:
Training professionals who regularly interact with children and their families on how to prevent and mitigate exposure to environmental toxicants during early development is an important opportunity to advance health equity; therefore, the committee recommends:
Given the need to continually monitor, prevent, and mitigate the impact of environmental toxicants in the preconception through early childhood period, it is critical that federal, state, local, tribal, and territorial governments continue their efforts in this area.
- Continued allocation of resources and technical assistance from the federal government through the Centers for Disease Control and Prevention (CDC), EPA, U.S. Food and Drug Administration (FDA), and the U.S. Consumer Product Safety Commission to translate existing data and research findings into actionable policies and practices.
- Ongoing review and updating of environmental exposure levels by federal agencies to reflect health and safety standards specific to the unique vulnerability of children (from fetal development through early development).
Other ongoing governmental activities that should be continued include regularly examining children and adolescents in NHANES and other national surveys for conditions related to environmental exposures, to track and monitor national and regional trends; development of policies and regulations requiring the remediation of persistent environmental exposure risks, including but not limited to children’s exposures to lead, mercury, arsenic, and chemicals and by-products of manufacturing, and the continuation of environmental evaluations; and case management of children with demonstrated risk of environmental exposures, particularly within communities experiencing higher risk levels, such as those with disproportionate poverty rates, substandard housing, higher concentrations of air pollutants, and other risky exposures.
In summary, while the approaches discussed in this chapter offer a few promising practices or approaches, several unknowns continue to pose challenges to a comprehensive exposure reduction effort. For example, more research and monitoring is needed to assess the effects of multiple long-term chemical exposures, paternal exposure burden and effects, and potential interactions between chemical exposures and gene expression. Evaluation of new, systemic approaches to policy development and implementation with demonstrable effects of reducing or mitigating chemical exposures remains key (Wang et al., 2016). One possible example is genetic studies examining gene variations that may increase susceptibility to environmental exposures. Combining these data with prospective, longitudinal studies could expand our knowledge of the role of critical developmental stages in the etiology of childhood diseases related to chemical exposures and human development (Wright and Christiani, 2010) and lead to novel approaches to further reduce environmental exposure risk.
CONCLUSION
Creating healthy living conditions to promote optimal development requires a multipronged approach to support caregivers and families so that they may meet the fundamental needs of their children. This chapter
builds on the evidence presented in Chapter 3 on early life influences and discusses the evidence on programs, policies, and systems changes to ensure that all children have access to healthy living conditions. Among the critical needs discussed in this chapter are access to nutrition, safe and stable housing, protection from environmental exposures, and importantly, economic resources to ensure these basic needs are met.
Based on its review of the extent literature and committee expertise, the committee offers program and policy recommendations to support families in promoting optimal development from the prenatal through early childhood periods. The conclusions and recommendations in this chapter emphasize the importance of public programs to provide access to economic resources, healthy foods, and stable housing. Furthermore, the recommendations highlight the many roles of government at all levels in shaping healthy early living conditions (e.g., removing barriers to accessing public nutrition programs, creating a comprehensive plan for healthy housing, passing legislation to authorize and fund paid parental leave, strengthening environmental protections in ECE settings). Implementation of the program and policy solutions in this chapter would enable families and caregivers to care for young children in healthy communities.
This chapter takes a systems perspective by delving into the multiple, interactive systems that shape the social, economic, and environmental determinants of health for children (see Chapter 8 for more on a systems approach to promote health equity during the prenatal through early childhood periods). The following chapter focuses on the ECE system and the various programs and policies that can be leveraged to promote health equity among children.
REFERENCES
AAP (American Academy of Pediatrics) Council on Environmental Health. 2012. Pediatric environmental health, 3rd ed., edited by R. A. Etzel. Elk Grove Village, IL: American Academy of Pediatrics.
Acevedo-Garcia, D., N. McArdle, T. L. Osypuk, B. Lefkowitz, and B. K. Krimgold. 2007. Children left behind: How metropolitan areas are failing America’s children. Boston, MA: Harvard School of Public Health and the Center for the Advancement of Health.
Acevedo-Garcia, D., T. L. Osypuk, N. McArdle, and D. R. Williams. 2008. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Affairs 27(2):321–333.
ACF (Administration for Children and Families) Office of Family Assistance. 2019. TANF caseload data 2018. https://www.acf.hhs.gov/ofa/resource/tanf-caseload-data-2018 (accessed May 2, 2019).
ACOG (American College of Obstetricians and Gynecologists). 2013. Committee opinion no. 575: Exposure to toxic environmental agents. Obstetrics & Gynecology 122(4):931–935.
AEI (American Enterprise Institute)-Brookings Working Group on Paid Family Leave. 2017. Paid family and medical leave: An issue whose time has come. Washington, DC: The Brookings Institution.
Ahrens, K. A., B. A. Haley, L. M. Rossen, P. C. Lloyd, and Y. Aoki. 2016. Housing assistance and blood lead levels: Children in the United States. American Journal of Public Health 106(11):2049–2056.
Allbee, A., R. Johnson, and J. Lubell. 2015. Preserving, protecting, and expanding affordable housing: A policy toolkit for public health. Oakland, CA: ChangeLab Solutions and Abt Associates.
Almond, D., H. W. Hoynes, and D. W. Schanzenback. 2011. Inside the war on poverty: The impact of food stamps on birth outcomes. Review of Economics and Statistics 93(2):387–403.
Almond, D., J. Currie, and V. Duque. 2018. Childhood circumstances and adult outcomes: Act II. Journal of Economic Literature 56(4):1360–1446.
Amoah, A. O., N. O. Witherspoon, J. Perodin, and J. A. Paulson. 2016. Findings from a pilot environmental health intervention at early childhood centers in the District of Columbia. Journal of Public Health (Oxford) 38(3):e209–e217.
Andreyeva, T., and J. Luedicke. 2013. Federal food package revisions: Effects on purchases of whole-grain products. American Journal of Preventative Medicine 45(4):422–429.
Applebaum, E., and R. Milkman. 2011. Leaves that pay: Employer and worker experiences with paid family leave in California. Washington, DC: Center for Economic and Policy Research.
Arizona Department of Health Services. 2017. 2018 Arizona targeted lead screening plan. Phoenix, AZ: Arizona Department of Health Services.
Arons, A., C. Bolbocean, N. R. Bush, F. A. Tylavsky, and K. Z. LeWinn. 2016. Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children is not associated with early childhood socioemotional development: Results from a longitudinal cohort study. Preventive Medicine Reports 4:507–511.
ASCE (American Society of Civil Engineers). 2017. Infrastructure report card: A comprehensive assessment of America’s infrastructure. Reston, VA: ASCE.
Baker, K. 2008. Do cash transfer programs improve infant health: Evidence from the 1993 expansion of the Earned Income Tax Credit. Notre Dame, IN: University of Notre Dame.
Baughman, R., and N. Duchovhy. 2016. State earned income tax credits and the production of child health: Insurance coverage, utilization, and health status. National Tax Journal 69(1):103–132.
Beck, A. F., M. D. Klein, J. K. Schaffzin, V. Tallent, M. Gillam, and R. S. Kahn. 2012. Identifying and treating a substandard housing cluster using a medical-legal partnership. Pediatrics 130(5):831–838.
Beck, A. F., B. Huang, R. Chundur, and R. S. Kahn. 2014. Housing code violation density associated with emergency department and hospital use by children with asthma. Health Affairs 33(11):1993–2002.
Berger, L. M., S. A. Font, K. S. Slack, and J. Waldfogel. 2017. Income and child maltreatment in unmarried families: Evidence from the Earned Income Tax Credit. Review of Economics of the Household 15(4):1345–1372.
Besharov, D. J., and D. M. Call. 2009. The expansion of WIC eligibility and enrollment: Good intentions, uncontrolled local discretion, and compliant federal officials. Washington, DC: American Enterprise Institute for Public Policy Research & University of Maryland Welfare Reform Academy.
Boyd-Swan, C., C. M. Herbst, J. Ifcher, and H. Zarghamee. 2013. The Earned Income Tax Credit, health, and happiness. IZA DP No. 7261. Bonn, Germany: The Institute for the Study of Labor.
Burdick-Will, J. 2018. Neighborhood violence, peer effects, and academic achievement in Chicago. Sociology of Education 91(3):205–223.
Byker, T. S. 2016. Paid parental leave laws in the United States: Does short-duration leave affect women’s labor-force attachment? American Economic Review 106(5):242–246.
Calafat, A. M., X. Ye, L. Valentin-Blasini, Z. Li, M. E. Mortensen, and L.-Y. Wong. 2017. Co-exposure to non-persistent organic chemicals among American pre-school aged children: A pilot study. International Journal of Hygiene and Environmental Health 220(2):55–63.
California Senate Office of Research. 2014. California’s paid family leave program: Ten years after the program’s implementation, who has benefited and what has been learned? https://sor.senate.ca.gov/sites/sor.senate.ca.gov/files/Californias%20Paid%20Family%20Leave%20Program.pdf (accessed April 7, 2019).
Camacho-Ramos, I. A. 2016. U.S. EPA/OPPT regulatory perspective on acute inhalation toxicity testing. https://www.piscltd.org.uk/wp-content/uploads/2016/09/Camacho-presentation_acute-inhalation-tox-workshop_092206_v3_FINAL.pdf (accessed July 9, 2019).
Carlson, S., and B. Keith-Jennings. 2018. SNAP is linked with improved nutritional outcomes and lower health care cost. Washington, DC: Center on Budget and Policy Priorities.
Carlson, S., and Z. Neuberger. 2018. WIC works: Addressing the nutrition and health needs of low-income families for 40 years. Washington, DC: Center on Budget and Policy Priorities.
CBPP (Center on Budget and Policy Priorities). 2017. Policy basics: Federal rental assistance. Washington, DC. https://www.cbpp.org/research/housing/policy-basics-federal-rental-assistance (accessed June 25, 2019).
CBPP. 2018a. Chart book: Temporary assistance for needy families. Washington, DC: Center on Budget and Policy Priorities.
CBPP. 2018b. Policy basics: The child tax credit. https://www.cbpp.org/research/federal-tax/ policy-basics-the-child-tax-credit (accessed May 1, 2019).
CBPP. 2018c. Policy basics: The Earned Income Tax Credit. https://www.cbpp.org/research/federal-tax/policy-basics-the-earned-income-tax-credit (accessed May 1, 2019).
CBPP. 2019. National and state housing fact sheets & data. https://www.cbpp.org/research/housing/national-and-state-housing-fact-sheets-data (accessed July 15, 2019).
CBPP. n.d. SNAP retailers database. https://www.cbpp.org/snap-retailers-database (accessed June 25, 2019).
CDC (Centers for Disease Control and Prevention). 2009. Healthy places terminology. https://www.cdc.gov/healthyplaces/terminology.htm (accessed April 18, 2019).
CDC. 2019a. Fourth national report on human exposure to environmental chemicals. 2019. https://www.cdc.gov/exposurereport/pdf/FourthReport_UpdatedTables_Volume1_Jan2019-508.pdf (accessed June 25, 2019).
CDC. 2019b. Environmental health services. https://www.cdc.gov/nceh/ehs (accessed June 25, 2019).
CEA (Council of Economic Advisers). 2014. The economics of early childhood investments. Washington, DC: Executive Office of the President.
Chetty, R., J. N. Friedman, and J. Rockoff. 2011. New evidence on the long-term impacts of tax credits. Paper read at Annual Conference on Taxation and Minutes of the Annual Meeting of the National Tax Association.
Chetty, R., N. Hendren, and L. F. Katz. 2016. The effects of exposure to better neighborhoods on children: New evidence from the moving to opportunity experiment. American Economic Review 106(4):855–902.
Chew, G. L., M. S. Perzanowski, R. L. Miller, J. C. Correa, L. A. Hoepner, C. M. Jusino, M. G. Becker, and P. L. Kinney. 2003. Distribution and determinants of mouse allergen exposure in low-income New York City apartments. Environmental Health Perspectives 111(10):1348–1351.
Chiasson, M. A., S. Findley, J. Sekhobo, R. Scheinmann, L. S. Edmunds, A. Faly, N. McLeod, and D. Gregg. 2013. Changing WIC changes what children eat. Obesity 21(7):1423–1429.
Cincinnati Children’s. n.d. Cincinnati child health-law partnership (child HeLP). https://www.cincinnatichildrens.org/service/g/gen-pediatrics/services/child-help (accessed April 17, 2019).
City of Rochester NY (New York). n.d. Lead paint—get prepared. https://www.cityofrochester.gov/article.aspx?id=8589936091 (accessed March 20, 2019).
CMS (Centers for Medicare & Medicaid Services). 2016. CMCS informational bulletin: Coverage of blood lead testing for children involved in Medicaid and the Children’s Health Insurance Program. https://www.medicaid.gov/federal-policy-guidance/downloads/cib113016.pdf (accessed July 15, 2019).
CMS. 2017. Frequently asked questions (FAQs) health services initiatives. https://www.medicaid.gov/federal-policy-guidance/downloads/faq11217.pdf (accessed June 25, 2019).
CMS. n.d. 2019. Lead screening. https://www.medicaid.gov/medicaid/benefits/epsdt/lead-screening/index.html (accessed June 25, 2019).
Collins, A. M., and J. A. Klerman. 2017. Improving nutrition by increasing Supplemental Nutrition Assistance Program benefits. American Journal of Preventive Medicine 52(2 Suppl 2):S179–S185.
Cooper, K., and K. Stewart. 2013. Does money affect children’s outcomes? A systematic review. York, UK: Joseph Rowntree Foundation.
Crain, E. F., M. Walter, G. T. O’Connor, H. Mitchell, R. S. Gruchalla, M. Kattan, G. S. Malindzak, P. Enright, R. Evans, 3rd, W. Morgan, and J. W. Stout. 2002. Home and allergic characteristics of children with asthma in seven U.S. urban communities and design of an environmental intervention: The Inner-city Asthma Study. Environmental Health Perspectives 110(9):939–945.
Crocker, D. D., S. Kinyota, G. G. Dumitru, C. B. Ligon, E. J. Herman, J. M. Ferdinands, D. P. Hopkins, B. M. Lawrence, and T. A. Sipe. 2011. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: A community guide systematic review. American Journal of Preventive Medicine 41(2):S5–S32.
Cronquist, K., and S. Lauffer. 2019. Characteristics of Supplemental Nutrition Assistance Program households: Fiscal year 2017. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service, Office of Policy Support.
Currie, J., and E. Moretti. 2008. Did the introduction of food stamps affect birth outcomes in California. In Making Americans healthier: Social and economic policy as health policy, edited by R. F. Schoeni, J. S. House, G. A. Kaplan, and H. Pollack. New York: Russell Sage Foundation. Pp. 122–144.
Dahl, G., and L. Lochner. 2012. The impact of family income on child achievement: Evidence from the Earned Income Tax Credit. American Economic Review 102:1927–1956.
Darrah, J., and S. DeLuca. 2014. “Living here has changed my whole perspective”: How escaping inner-city poverty shapes neighborhood and housing choice. Journal of Policy Analysis and Management 33(2):350–384.
Deb, P., and C. A. Gregory. 2018. Heterogeneous impacts of SNAP on food insecurity. Economic Letters 173(C):55–60.
Declercq, E., C. Sakala, M. Corry, S. Applebaum, and A. Herrlich. 2013. Listening to Mothers III: New mothers speak out. Report of the National Survey of Women’s Childbearing Experiences conducted October–December 2012 and January–April 2013. New York: Childbirth Connection.
Department of Ecology, Washington State. 2008. Children’s Safe Products Act. https://ecology.wa.gov/Waste-Toxics/Reducing-toxic-chemicals/Childrens-Safe-Products-Act (accessed June 25, 2019).
Desmond, M. 2018. Heavy is the house: Rent burden among the American urban poor. International Journal Urban and Regional Research 42(1):160–170.
Detroit URC (Urban Research Center). n.d. Healthy Mothers on the Move/Madres Saludables en Movimiento (Healthy MOMS). http://www.detroiturc.org/index.php?option=com_content&view=article&id=15&Itemid=28 (accessed April 17, 2019).
Di Renzo, G. C., J. A. Conry, J. Blake, M. S. DeFrancesco, N. DeNicola, J. N. Martin, Jr., K. A. McCue, D. Richmond, A. Shah, P. Sutton, T. J. Woodruff, S. Z. van der Poel, and L. C. Giudice. 2015. International Federation of Gynecology and Obstetrics opinion on reproductive health impacts of exposure to toxic environmental chemicals. International Journal of Gynecology & Obstetrics 131(3):219–225.
Dickman, J. 2017. Children at risk: Gaps in state lead screening policies. https://saferchemicals.org/sc/wp-content/uploads/2017/01/saferchemicals.org_children-at-risk-report.pdf (accessed June 8, 2019).
DOL (U.S. Department of Labor). 2018. Wage and Hour Division (WHD). https://www.dol.gov/whd/regs/compliance/whdfs73.htm (accessed July 9, 2019).
DOL. n.d. Title VI, Civil Rights Act of 1964. https://www.dol.gov/agencies/oasam/regulatory/statutes/title-vi-civil-rights-act-of-1964 (accessed October 1, 2019).
DTSC (Department of Toxic Substances Control, State of California). n.d. Safer consumer products. https://dtsc.ca.gov/scp (accessed January 29, 2019).
East, C. N. 2018. The effect of food stamps on children’s health: Evidence from immigrants’ changing eligibility. The Journal of Human Resources 0916-8197R2.
ECHO (Environmental influences on Child Health Outcomes). 2019a. ECHO program activates first sites under the ECHO-wide cohort data collection protocol. https://echochildren.org/echo-program-activates-first-sites-under-the-echo-wide-cohort-data-collectionprotocol (accessed July 15, 2019).
ECHO. 2019b. ECHO program receives green light to begin expansive child health research. https://echochildren.org/echo-program-receives-green-light-to-begin-expansive-child-health-research (accessed July 15, 2019).
EDF (Environmental Defense Fund). 2016. A new chemical safety law: The Lautenberg Act. https://www.edf.org/health/new-chemical-safety-law-lautenberg-act (accessed July 15, 2019).
Eligibility.com. 2019. Section 8 housing. https://eligibility.com/section-8 (accessed March 26, 2019).
Environmental Justice Leadership Forum on Climate Change. 2016. Environmental justice state guidance: How to incorporate equity and justice into your state clean power planning approach. http://www.eesi.org/files/EJ-State-Guidance-Final-v5-jan-15-2016.pdf (accessed June 8, 2019).
Environmental Law Institute. 2015. Reducing environmental exposures in child care facilities: A review of state policy. https://www.eli.org/buildings/reducing-environmental-exposures-child-care-facilities (accessed June 25, 2019).
EPA (U.S. Environmental Protection Agency). 2015. Children’s environmental health: Research roadmap. Washington, DC: U.S. Environmental Protection Agency, Office of Research and Development.
EPA. 2019. Reviewing new chemicals under the Toxic Substances Control Act (TSCA). https://www.epa.gov/reviewing-new-chemicals-under-toxic-substances-control-act-tsca (accessed July 15, 2019).
EPA. n.d.-a. About the TSCA Chemical Substance Inventory. https://www.epa.gov/tsca-inventory/about-tsca-chemical-substance-inventory (accessed July 15, 2019).
EPA. n.d.-b. Basic information about ACE. https://www.epa.gov/ace/basic-information-about-ace (accessed July 12, 2019).
EPA. n.d.-c. TSCA chemical substance inventory. https://www.epa.gov/tsca-inventory (accessed July 12, 2019).
Evans, W., and C. Garthwaite. 2010. Giving mom a break: The impact of higher EITC payments on maternal health. NBER Working paper 16296. NBER Working Paper Series. Cambridge, MA: National Bureau of Economic Research.
Evans, G. W., N. M. Wells, H. Y. Chan, and H. Saltzman. 2000. Housing quality and mental health. Journal of Consulting and Clinical Psychology 68(3):526–530.
Executive Order 13045. 1997. Protection of children from environmental health risks and safety risks. Federal Register 62(78):19885–19888.
Fan, M., and Y. Jin. 2015. The Supplemental Nutrition Assistance Program and childhood obesity in the United States: Evidence from the National Longitudinal Survey of Youth 1997. American Journal of Health Economics 1(4):432–460.
FDA (U.S. Food and Drug Administration). 2014. Bisphenol A (BPA): Use in food contact application. https://www.fda.gov/food/food-additives-petitions/bisphenol-bpa-use-food-contact-application (accessed July 12, 2019).
Federal Healthy Homes Work Group. 2013. Advancing healthy housing: A strategy for action. https://www.hud.gov/sites/documents/STRATPLAN_FINAL_11_13.PDF (accessed June 25, 2019).
Fenelon, A., N. Slopen, M. Boudreaux, and S. J. Newman. 2018. The impact of housing assistance on the mental health of children in the United States. Journal of Health and Social Behavior 59(3):447–463.
Fertig, A. R. 2007. Public housing, health, and health behaviors: Is there a connection? Journal of Policy Analysis and Management 26(4):831–860.
Figlio, D., S. Hamersma, and J. Roth. 2009. Does prenatal WIC participation improve birth outcomes? New evidence from Florida. Journal of Public Economics 93(1–2):235–245.
Fingar, K. R., S. H. Lob, M. S. Dove, P. Gradziel, and M. P. Curtis. 2017. Reassessing the association between WIC and birth outcomes using a fetuses-at-risk approach. Maternal and Child Health Journal 21(4):825–835.
Fischer, W. 2015. Research shows housing vouchers reduce hardship and provide platform for long-term gains among children. Washington, DC: Center on Budget and Policy Priorities.
Forrest, C. B., C. K. Blackwell, and C. A. Camargo, Jr. 2018. Advancing the science of children’s positive health in the National Institutes of Health Environmental influences on Child Health Outcomes (ECHO) Research Program. The Journal of Pediatrics 196:298–300.
Foster, E. M., M. Jiang, and C. M. Gibson-Davis. 2010. The effect of the WIC program on the health of newborns. Health Services Research 45(4):1083–1104.
Frey, W. H. 2015. Census shows modest declines in black-white segregation. https://www.brookings.edu/blog/the-avenue/2015/12/08/census-shows-modest-declines-in-black-white-segregation (accessed January 29, 2019).
Garboden, P. M., T. Leventhal, and S. Newman. 2017. Estimating the effects of residential mobility: A methodological note. Journal of Social Service Research 43(2):246–261.
Gehle, K. S., J. L. Crawford, and M. T. Hatcher. 2011. Integrating environmental health into medical education. American Journal of Preventive Medicine 41(4 Suppl 3):S296–S301.
Gerlach, C. 2016. New Toxic Substances Control Act: An end to the Wild West for chemical safety? http://sitn.hms.harvard.edu/flash/2016/new-toxic-substances-control-act-end-wild-west-chemical-safety (accessed March 21, 2019).
Gibson-Davis, C., and E. M. Foster. 2006. A cautionary tale: Using propensity scores to estimate the effect of food stamps on food insecurity. Social Service Review 80(1):93–126.
Goldin, J. 2018. Tax benefit complexity and take-up: Lessons from the Earned Income Tax Credit. Stanford law and economics Olin working paper 514. https://ssrn.com/abstract=3101160 (accessed May 2, 2019).
GPO (U.S. Government Publishing Office). 2017. Prohibition of children’s toys and child care articles containing specified phthalates. Federal Register 82(207):49938–49982. https://www.govinfo.gov/content/pkg/FR-2017-10-27/pdf/2017-23267.pdf (accessed July 12, 2019).
Grandjean, P., R. Barouki, D. C. Bellinger, L. Casteleyn, L. H. Chadwick, S. Cordier, R. A. Etzel, K. A. Gray, E.-H. Ha, C. Junien, M. Karagas, T. Kawamoto, B. Paige Lawrence, F. P. Perera, G. S. Prins, A. Puga, C. S. Rosenfeld, D. H. Sherr, P. D. Sly, W. Suk, Q. Sun, J. Toppari, P. van Den Hazel, C. L. Walker, and J. J. Heindel. 2015. Life-long implications of developmental exposure to environmental stressors: New perspectives. Endocrinology 156(10):3408.
Gregory, C., and P. Deb. 2015. Does SNAP improve your health? Food Policy 50:11–19.
Gregory, C., M. P. Rabbitt, and D. C. Ribar. 2016. The Supplemental Nutrition Assistance Program and food insecurity. In SNAP matters: How food stamps affect health and wellbeing, edited by J. Bartfeld, C. Gundersen, T. M. Smeeding, and J. P. Ziliak. Stanford, CA: Stanford University Press. Pp. 74–106.
Griffith, W. C., E. M. Vigoren, M. N. Smith, T. Workman, B. Thompson, G. D. Coronado, and E. M. Faustman. 2018. Application of improved approach to evaluate a community intervention to reduce exposure of young children living in farmworker households to organophosphate pesticides. Journal of Exposure Science & Environmental Epidemiology 29(3):358–365.
Grindler, N. M., A. A. Allshouse, E. Jungheim, T. L. Powell, T. Jansson, and A. J. Polotsky. 2018. OB-GYN screening for environmental exposures: A call for action. PLoS ONE 13(5):e0195375.
Guendelman, S., J. L. Kosa, M. Pearl, S. Graham, J. Goodman, and M. Kharrazi. 2009. Juggling work and breastfeeding: Effects of maternity leave and occupational characteristics. Pediatrics 123(1):e38–e46.
Guidry, V. T., A. Lowman, D. Hall, D. Baron, and S. Wing. 2014. Challenges and benefits of conducting environmental justice research in a school setting. NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy 24(2):153–170.
Gundersen, C., and V. Oliveira. 2001. The food stamp program and food insufficiency. American Journal of Agricultural Economics 83(4):875–887.
Hahn, R. A., B. I. Truman, and D. R. Williams. 2018. Civil rights as determinants of public health and racial and ethnic health equity: Health care, education, employment, and housing in the United States. SSM—Population Health 4:17–24.
Hamad, R., and D. H. Rehkopf. 2016. Poverty and child development: A longitudinal study of the impact of the Earned Income Tax Credit. American Journal of Epidemiology 183(9):775–784.
Health Impact Project. 2017. 10 policies to prevent and respond to childhood lead exposure. Washington, DC: The Pew Charitable Trusts and Robert Wood Johnson Foundation.
Hendra, R., D. H. Greenberg, G. Hamilton, A. Oppenheim, A. Pennington, K. Schaberg, and B. L. Tessler. 2016. Encouraging evidence on a sector-focused advancement strategy: Two-year impacts from the WorkAdvance demonstration. New York: MDRC.
Hendricks, M., M. Meyer, N. G. Gharaibeh, S. Van Zandt, J. Masterson, J. Cooper, Jr., J. Horney, and P. Berke. 2018. The development of a participatory assessment technique for infrastructure: Neighborhood-level monitoring towards sustainable infrastructure systems. Sustainable Cities and Society 38:265–274.
Hendryx, M., and J. Luo. 2018. Children’s environmental chemical exposures in the USA, NHANES 2003–2012. Environmental Science and Pollution Research 25(6):5336–5343.
Heymann, J., A. Raub, and A. Earle. 2011. Creating and using new data sources to analyze the relationship between social policy and global health. Public Health Reports 126:127–134.
Heymann, J., A. Earle, and K. McNeill. 2013. The impact of labor policies on the health of young children in the context of economic globalization. Annual Review of Public Health 34(1):355–372.
HHS (U.S. Department of Health and Human Services). 2012. What is TANF? https://www.hhs.gov/answers/programs-for-families-and-children/what-is-tanf/index.html (accessed May 2, 2019).
Hoynes, H. W., and D. W. Schanzenbach. 2018. Safety net investments in children. Working paper 24594. NBER Working Paper Series. Cambridge, MA: National Bureau of Economic Research.
Hoynes, H., M. Page, and A. H. Stevens. 2011. Can targeted transfers improve birth outcomes?: Evidence from the introduction of the WIC program. Journal of Public Economics 95(7–8):813–827.
Hoynes, H., D. Miller, and D. Simon. 2012. Income, the Earned Income Tax Credit, and infant health. American Economic Journal: Economic Policy 7(1):172–211.
Hoynes, H., D. W. Schanzenbach, and D. Almond. 2016. Long-run impacts of childhood access to the safety net. American Economic Review 106(4):903–934.
Huang, R., and M. Yang. 2015. Paid maternity leave and breastfeeding practice before and after California’s implementation of the nation’s first paid family leave program. Economics & Human Biology 16:45–59.
HUD (U.S. Department of Housing and Urban Development). 2014. Housing’s and neighborhoods’ role in shaping children’s future. https://www.huduser.gov/portal/periodicals/em/fall14/highlight1.html (accessed June 4, 2019).
HUD. 2015. HUD reports continued high levels of “worst case housing needs.” https://archives.hud.gov/news/2015/pr15-014.cfm (accessed June 4, 2019).
HUD. 2016. Picture of subsidized households. https://www.huduser.gov/portal/datasets/assthsg.html (accessed June 4, 2019).
Huffman, S. K., and H. H. Jensen. 2008. Food assistance programs and outcomes in the context of welfare reform. Social Science Quarterly 89(1):95–115.
IRS (Internal Revenue Service). 2019. EITC participation rate by states. https://www.eitc.irs.gov/eitc-central/participation-rate/eitc-participation-rate-by-states (accessed May 1, 2019).
Irving, S. K., and T. A. Loveless. 2015. Dynamics of economic well-being: Participation in government programs, 2009–2012: Who gets assistance? Washington, DC: U.S. Department of Commerce, Economic and Statistics Administration, U.S. Census Bureau.
Isaacs, J., O. Healy, and H. E. Peters. 2017a. Paid family leave in the United States: Time for a new national policy. Washington, DC: The Urban Institute.
Isaacs, J. B., C. Lou, H. Hahn, J. Ovalle, and C. E. Steurle. 2017b. Kids’ share 2017: Report on federal expenditures on children through 2016 and future projections. Washington, DC: The Urban Institute.
Jackson, M. I. 2015. Early childhood WIC participation, cognitive development and academic achievement. Social Science & Medicine 126:145–153.
Jacob, B. A., M. Kapustin, and J. Ludwig. 2015. The impact of housing assistance on child outcomes: Evidence from a randomized housing lottery. Quarterly Journal of Economics 130(1):465–506.
Jelleyman, T., and N. Spencer. 2008. Residential mobility in childhood and health outcomes: A systematic review. Journal of Epidemiology and Community Health 62(7):584–592.
Johnson, P., D. Betson, L. Blatt, and L. Giannarelli. 2017. National- and state-level estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) eligibles and program reach in 2014, and updated estimates for 2005–2013. Special Nutrition Programs Report No. WIC-17-ELIG. Washington, DC: U.S. Department of Agriculture, Food and Nutrition Service, Office of Policy Support.
Joint Center for Housing Studies of Harvard University. 2017. America’s rental housing 2017. Cambridge, MA: Harvard University.
Kenney, M. K., M. D. Kogan, S. Toomer, and P. C. van Dyck. 2012. Federal expenditures on maternal and child health in the United States. Maternal and Child Health Journal 16(2):271.
Kessler, R. C., G. J. Duncan, L. A. Gennetian, L. F. Katz, J. R. Kling, N. A. Sampson, L. Sanbonmatsu, A. M. Zaslavsky, and J. Ludwig. 2014. Associations of housing mobility interventions for children in high-poverty neighborhoods with subsequent mental disorders during adolescence. JAMA 311(9):937–947.
Khanani, I., J. Elam, R. Hearn, C. Jones, and N. Maseru. 2010. The impact of prenatal WIC participation on infant mortality and racial disparities. American Journal of Public Health 100(Suppl 1):S204–S209.
Kieffer, E. C., D. B. Welmerink, B. R. Sinco, K. B. Welch, E. M. Rees Clayton, C. Y. Schumann, and V. E. Uhley. 2014. Dietary outcomes in a Spanish-language randomized controlled diabetes prevention trial with pregnant Latinas. American Journal of Public Health 104(3):526–533.
Kilpatrick, N., H. Frumkin, J. Trowbridge, C. Escoffery, R. Geller, L. Rubin, G. Teague, and J. Nodvin. 2002. The environmental history in pediatric practice: A study of pediatricians’ attitudes, beliefs, and practices. Environmental Health Perspectives 110(8):823–827.
Kim, S., J. Mazza, J. Zwanziger, and D. Henry. 2014. School and behavioral outcomes among inner city children: Five-year follow-up. Urban Education 49(7):835–856.
Kimbro, R. T., J. Brooks-Gunn, and S. McLanahan. 2011. Young children in urban areas: Links among neighborhood characteristics, weight status, outdoor play, and television watching. Social Science and Medicine 72(5):668–676.
Klein, M. D., R. S. Kahn, R. C. Baker, E. E. Fink, D. S. Parrish, and D. C. White. 2011. Training in social determinants of health in primary care: Does it change resident behavior? Academic Pediatrics 11(5):387–393.
Klein, M. D., A. F. Beck, A. W. Henize, D. S. Parrish, E. E. Fink, and R. S. Kahn. 2013. Doctors and lawyers collaborating to help children—outcomes from a successful partnership between professions. Journal of Health Care for the Poor and Underserved 24(3):1063–1073.
Kling, J. R., J. B. Liebman, and L. F. Katz. 2007. Experimental analysis of neighborhood effects. Econometrica 75(1):83–119.
Koehler, K., M. Latshaw, T. Matte, D. Kass, H. Frumkin, M. Fox, B. F. Hobbs, M. Wills-Karp, and T. A. Burke. 2018. Building healthy community environments: A public health approach. Public Health Reports 133(Suppl 1):S35–S43.
Koehrn, K., J. Hospital, A. Woolf, and J. Lowry. 2017. Pediatric environmental health: Using data on toxic chemical emissions in practice. Current Problems in Pediatric and Adolescent Health Care 47(11):281–302.
Komro, K. A., M. D. Livingston, S. Markowitz, and A. C. Wagenaar. 2016. The effect of an increased minimum wage on infant mortality and birth weight. American Journal of Public Health 106(8):1514–1516.
Komro, K. A., S. Markowitz, M. D. Livingston, and A. C. Wagenaar. 2019. Effects of state-level earned income tax credit laws on birth outcomes by race and ethnicity. Health Equity 3(1):61–67.
Kreger, M., K. Sargent, A. Arons, M. Standish, and C. D. Brindis. 2011. Creating an environmental justice framework for policy change in childhood asthma: A grassroots to treetops approach. American Journal of Public Health 101(Suppl 1):S208.
Kreider, B., J. Pepper, C. Gundersen, and D. Jolliffe. 2012. Identifying the effects of SNAP (food stamps) on child health outcomes when participation is endogenous and misreported. Journal of the American Statistical Association 107(499):958–975.
Kreider, B., J. V. Pepper, and M. Roy. 2016. Identifying the effects of WIC on food insecurity among infants and children. Southern Economic Journal 82(4):1106–1122.
Krieger, J., D. E. Jacobs, P. J. Ashley, A. Baeder, G. L. Chew, D. Dearborn, H. P. Hynes, J. D. Miller, R. Morley, F. Rabito, and D. C. Zeldin. 2010. Housing interventions and control of asthma-related indoor biologic agents: A review of the evidence. Journal of Public Health Management and Practice 16(Suppl 5):S11–S20.
Leech, T. G. 2012. Subsidized housing, public housing, and adolescent violence and substance use. Youth & Society 44(2):217–235.
Leventhal, T., and S. Newman. 2010. Housing and child development. Children and Youth Services Review 32(9):1165–1174.
Levy, J. I., D. Brugge, J. L. Peters, J. E. Clougherty, and S. S. Saddler. 2006. A community-based participatory research study of multifaceted in-home environmental interventions for pediatric asthmatics in public housing. Social Science & Medicine 63(8):2191–2203.
Ludwig, J., L. Sanbonmatsu, L. Gennetian, E. Adam, G. J. Duncan, L. F. Katz, R. C. Kessler, J. R. Kling, S. T. Lindau, R. C. Whitaker, and T. W. McDade. 2011. Neighborhoods, obesity, and diabetes—a randomized social experiment. New England Journal of Medicine 365(16):1509–1519.
Ludwig, J., G. J. Duncan, L. A. Gennetian, L. F. Katz, R. C. Kessler, J. R. Kling, and L. Sanbonmatsu. 2013. Long-term neighborhood effects on low-income families: Evidence from Moving to Opportunity. American Economic Review Papers and Proceedings 103(3):226–231.
Manoli, D., and N. Turner. 2018. Cash-on-hand and college enrollment: Evidence from population tax data and the Earned Income Tax Credit. American Economic Review: Economic Policy 10(2):242–271.
Martinez, O., J. Boles, M. Muñoz-Laboy, E. C. Levine, C. Ayamele, R. Eisenberg, J. Manusov, and J. Draine. 2017. Bridging health disparity gaps through the use of medical legal partnerships in patient care: A systematic review. Journal of Law, Medicine & Ethics 45(2):260–273.
Maryland Department of Health. 2016. Lead poisoning prevention in Maryland: What’s new? https://phpa.health.maryland.gov/OEHFP/EH/Pages/LeadTesting.aspx (accessed March 21, 2019).
Marzieh, A., T. Sedigheh Sadat, Z. Saeed Motesaddi, H. Ali Reza, B. Andrea, and M. Ali. 2017. A behavioral strategy to minimize air pollution exposure in pregnant women: A randomized controlled trial. Environmental Health and Preventive Medicine 22(1):1–8.
Mass.gov. 2019. Department of Family and Medical Leave (DFML). https://www.mass.gov/orgs/department-of-family-and-medical-leave (accessed July 15, 2019).
Maxwell, K., S. Julius, A. Grambsch, A. Kosmal, L. Larson, and N. Sonti. 2018. Built environment, urban systems, and cities. In Impacts, risks, and adaptation in the United States: Fourth national climate assessment, Vol. 2, edited by D. R. Reidmiller, C. W. Avery, D. R. Easterling, K. E. Kunkel, K. L. M. Lewis, T. K. Maycock, and B. C. Stewart. Washington, DC: U.S. Global Change Research Program. Pp. 438–478.
Mazzara, A., and B. Knudsen. 2019. Where families with children use housing vouchers: A comparative look at the 50 largest metropolitan areas. Washington, DC: Poverty & Race Research Action Council.
Mazzara, A., B. Sard, and D. Rice. 2016. Rental assistance to families with children at lowest point in decade. Washington, DC: Center on Budget and Policy Priorities.
McCoy, D. C., A. L. Roy, and C. C. Raver. 2016. Neighborhood crime as a predictor of individual differences in emotional processing and regulation. Developmental Science 19(1):164–174.
McCurdy, L. E., J. Roberts, B. Rogers, R. Love, R. Etzel, J. Paulson, N. O. Witherspoon, and A. Dearry. 2004. Incorporating environmental health into pediatric medical and nursing education. Environmental Health Perspectives 112(17):1755–1760.
Meyerhoefer, C. D., and M. Yang. 2011. The relationship between food assistance and health: A review of the literature and empirical strategies for identifying program effects. Applied Economic Perspectives and Policy 33(3):304–344.
Mikati, I., A. F. Benson, T. J. Luben, J. D. Sacks, and J. Richmond-Bryant. 2018. Disparities in distribution of particulate matter emission sources by race and poverty status. American Journal of Public Health 108(4):480–485.
Mirkovic, K. R., C. G. Perrine, K. S. Scanlon, and L. M. Grummer-Strawn. 2014. Maternity leave duration and full-time/part-time work status are associated with US mothers’ ability to meet breastfeeding intentions. Journal of Human Lactation: Official Journal of International Lactation Consultant Association 30(4):416–419.
Misra, T. 2016. Baltimore’s housing voucher program almost gets it right. CityLab. https://www.citylab.com/equity/2016/01/baltimore-affordable-housing-voucheropportunity/421722 (accessed March 26, 2019).
Morello-Frosch, R., and E. D. Shenassa. 2006. The environmental “riskscape” and social inequality: Implications for explaining maternal and child health disparities. Environmental Health Perspectives 114(8):1150–1153.
Morgan, W. J., E. F. Crain, R. S. Gruchalla, G. T. O’Connor, M. Kattan, R. Evans, 3rd, J. Stout, G. Malindzak, E. Smartt, M. Plaut, M. Walter, B. Vaughn, and H. Mitchell. 2004. Results of a home-based environmental intervention among urban children with asthma. New England Journal of Medicine 351(11):1068–1080.
MotherToBaby. n.d. About us. https://mothertobaby.org/about-us (accessed April 5, 2019).
Murphy, J. S., E. M. Lawton, and M. Sandel. 2015. Legal care as part of health care: The benefits of medical-legal partnership. Pediatric Clinics 62(5):1263–1271.
Murtagh, L., and A. D. Moulton. 2011. Working mothers, breastfeeding, and the law. American Journal of Public Health 101(2):217–223.
Nandi, A., D. Jahagirdar, M. C. Dimitris, J. A. Labrecque, E. C. Strumpf, J. S. Kaufman, I. Vincent, E. Atabay, S. Harper, A. Earle, and S. J. Heymann. 2018. The impact of parental and medical leave policies on socioeconomic and health outcomes in OECD countries: A systematic review of the empirical literature. The Milbank Quarterly 96(3):434–471.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2015. Mental disorders and disabilities among low-income children. Washington, DC: The National Academies Press.
NASEM. 2016. Review of WIC food packages: Proposed framework for revisions: Interim report. Washington, DC: The National Academies Press.
NASEM. 2017. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press.
NASEM. 2019. A roadmap to reducing child poverty. Washington, DC: The National Academies Press.
NASHP (National Academy for State Health Policy). 2017. Lead screening and treatment in Medicaid and CHIP. https://nashp.org/wp-content/uploads/2017/02/Lead-Screening.pdf (accessed June 25, 2019).
NASHP. 2018. State health care delivery policies promoting lead screening and treatment for children and pregnant women (5.21.18). https://nashp.org/wp-content/uploads/2018/05/NASHP-Lead-Policy-Scan-5-21-18_updated.pdf (accessed June 25, 2019).
National Center for Healthy Housing. 2014. National healthy housing standard (full document, 2018 update). Columbia, MD: National Center for Healthy Housing.
National Center for Healthy Housing. 2017. National healthy housing standard—implementation tool. https://nchh.org/resource/national-healthy-housing-standard-implementation-tool (accessed March 21, 2019).
NCSL (National Conference of State Legislators). 2014. Toxic Substances Control Act reform. http://www.ncsl.org/research/environment-and-natural-resources/state-chemicalstatutes.aspx#statelaws (accessed July 12, 2019).
NCSL. 2017. NCSL policy update: State statutes on chemical safety. http://www.ncsl.org/research/environment-and-natural-resources/ncsl-policy-update-state-statutes-onchemical-safety.aspx (accessed June 25, 2019).
Newman, S., and C. S. Holupka. 2017. The effects of assisted housing on child well-being. American Journal of Community Psychology 60(1–2):66–78.
Nichols, A., and J. Rothstein. 2016. The Earned Income Tax Credit. In Economics of means-tested transfer program in the United States, Vol. 1, edited by R. A. Moffitt. Chicago, IL: University of Chicago Press. Pp. 137–218.
NRC and IOM (National Research Council and Institute of Medicine). 2000. From neurons to neighborhoods: The science of early childhood development. Washington, DC: National Academy Press.
OECD (Organisation for Economic Co-operation and Development). 2017. PF2.1: Key characteristics of parental leave systems. https://www.oecd.org/els/soc/PF2_1_Parental_leave_systems.pdf (accessed July 15, 2019).
Office of the Surgeon General, CDC (Centers for Disease Control and Prevention), and Office on Women’s Health. 2011. The Surgeon General’s call to action to support breastfeeding. Rockville, MD: Office of the U.S. Surgeon General.
Ogbuanu, C., S. Glover, J. Probst, J. Liu, and J. M. Hussey. 2011. The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics 127(6):e1414–e1427.
Olsho, L. E. W., J. A. Klerman, S. H. Bartlett, and C. W. Logan. 2017. Rebates to incentivize healthy nutrition choices in the Supplemental Nutrition Assistance Program. American Journal of Preventative Medicine 52(2 Suppl 2):S161–S170.
Oregon Health Authority. 2017. Toxic-free kids: A report to the governor and the 79th Oregon legislative assembly. Portland, OR: Oregon Health Authority, Public Health Division.
PEHSU (Pediatric Environmental Health Specialty Units). n.d. About the PEHSU program. https://www.pehsu.net/About_PEHSU.html (accessed April 5, 2019).
Petersen, D. M., M. Minkler, V. B. Vasquez, M. C. Kegler, L. H. Malcoe, and S. Whitecrow. 2007. Using community-based participatory research to shape policy and prevent lead exposure among Native American children. Progress in Community Health Partnerships: Research, Education, and Action 1(3):249–256.
Pinderhughes, H., R. A. Davis, and M. Williams. 2015. Adverse community experiences and resilience: A framework for addressing and preventing community trauma. Oakland, CA: Prevention Institute.
Postma, J., C. Karr, and G. Kieckhefer. 2009. Community health workers and environmental interventions for children with asthma: A systematic review. Journal of Asthma 46(6):564–576.
PTFCEH (President’s Task Force on Environmental Health Risks and Safety Risks to Children). 2016a. Key federal programs to reduce childhood lead exposures and eliminate associated health impacts. https://ptfceh.niehs.nih.gov/features/assets/files/key_ federal_programs_to_reduce_childhood_lead_exposures_and_eliminate_associated_ health_impactspresidents_508.pdf (accessed June 25, 2019).
PTFCEH. 2016b. President’s task force on environmental health risks and safety risks to children work plan. https://ptfceh.niehs.nih.gov/activities/assets/files/presidents_task_force_work_plan_508.pdf (accessed April 17, 2019).
PTFCEH. 2018. Federal action plan to reduce childhood lead exposures and associated health impacts. Washington, DC: President’s Task Force on Environmental Health Risks and Safety Risks to Children.
PTFCEH. n.d. Asthma and the environment: A strategy to protect children. https://ptfceh.niehs.nih.gov/activities/assets/files/asthma_and_the_environment_a_strategy_to_protect_children.pdf (accessed June 25, 2019).
Raissian, K. M., and L. R. Bullinger. 2017. Money matters: Does the minimum wage affect child maltreatment rates? Children and Youth Services Review 72:60–70.
Ratcliffe, C., and S. McKernan. 2010. How much does SNAP reduce food insecurity? Washington, DC: Urban Institute.
Raub, A., A. Nandi, A. Earle, N. D. G. Chorny, E. Wong, P. Chung, P. Batra, A. Schickedanz, B. Bose, J. Jou, D. Franken, and J. Heymann. 2018. Paid parental leave: A detailed look at approaches across OECD countries. Los Angeles, CA: World Policy Analysis Center.
Rauh, V. A., and A. E. Margolis. 2016. Research review: Environmental exposures, neurodevelopment, and child mental health—new paradigms for the study of brain and behavioral effects. Journal of Child Psychology and Psychiatry 57(7):775–793.
REACH (Racial and Ethnic Approaches to Community Health) Detroit. 2018. Healthy Mothers on the Move (Healthy MOMS)/Madres Saludables en Movimiento (Madres Saludables). http://www.reachdetroit.org/about/HealthyMoms (accessed April 17, 2019).
Reskin, B. 2012. The race discrimination system. Annual Review of Sociology 38:17–24.
Rivas, I., X. Querol, J. Wright, and J. Sunyer. 2018. How to protect school children from the neurodevelopmental harms of air pollution by interventions in the school environment in the urban context. Environment International 121:199–206.
Roberts, J. R., and B. A. Gitterman. 2003. Pediatric environmental health education: A survey of U.S. Pediatric residency programs. Ambulatory Pediatrics 3(1):57–59.
Rosenberg, T. 2014. When poverty makes you sick, a lawyer can be the cure. The New York Times, July 17.
Rossin-Slater, M. 2011. The effects of maternity leave on children’s birth and infant health outcomes in the United States. Journal of Health Economics 30(2):221–239.
Rossin-Slater, M., C. J. Ruhm, and J. Waldfogel. 2011. Effects of California’s paid family leave program on mothers’ leave-taking and subsequent labor market outcomes. Cambridge, MA: National Bureau of Economic Research.
Rusk, D. 2017. Economic segregation is replacing racial segregation in large U.S. metro areas. https://www.dcpolicycenter.org/publications/economic-polarization (accessed January 29, 2019).
RWJF (Robert Wood Johnson Foundation). 2018. SNAP supports children and families. Princeton, NJ: Robert Wood Johnson Foundation.
SafetyNEST. 2018. SafetyNEST science. https://uploads.strikinglycdn.com/files/3770c2fa680a-4eb7-b1e0-116bdf601a64/SafetyNEST_Summary_2018.pdf (accessed April 5, 2019).
Sanbonmatsu, L., J. R. Kling, G. J. Duncan, and J. Brooks-Gunn. 2006. Neighborhoods and academic achievement: Results from the Moving to Opportunity experiment. NBER Working paper 11909. NBER Working Paper Series. Cambridge, MA: National Bureau of Economic Research.
Sandel, M., M. Hansen, R. Kahn, E. Lawton, E. Paul, V. Parker, S. Morton, and B. Zuckerman. 2010. Medical-legal partnerships: Transforming primary care by addressing the legal needs of vulnerable populations. Health Affairs 29(9):1697–1705.
Sandel, M., R. Sheward, S. Ettinger de Cuba, S. M. Coleman, D. A. Frank, M. Chilton, M. Black, T. Heeren, J. Pasquariello, P. Casey, E. Ochoa, and D. Cutts. 2018. Unstable housing and caregiver and child health in renter families. Pediatrics 141(2):e20172199.
Sard, B., D. Rice, A. Bell, and A. Mazzara. 2018. Federal policy changes can help more families with housing vouchers live in higher-opportunity areas. https://www.cbpp.org/research/housing/federal-policy-changes-can-help-more-families-with-housing-vouchers-livein-higher (accessed June 25, 2019).
Sathyanarayana, S., J. Focareta, T. Dailey, and S. Buchanan. 2012. Environmental exposures: How to counsel preconception and prenatal patients in the clinical setting. American Journal of Obstetrics and Gynecology 207(6):463–470.
Schulz, A., G. Mentz, N. Sampson, M. Ward, R. Anderson, R. de Majo, B. Israel, T. Lewis, and D. Wilkins. 2016. Race and the distribution of social and physical environmental risk. Du Bois Review 13(2):285–304.
Schwartz, M. B. 2017. Moving beyond the debate over restricting sugary drinks in the Supplemental Nutrition Assistance Program. American Journal of Preventive Medicine 52(2):S199–S205.
Shaefer, L., S. Collyer, G. Duncan, K. Edin, I. Garfinkel, D. Harris, T. M. Smeeding, J. Waldfogel, C. Wimer, and H. Yoshikawa. 2018. A universal child allowance: A plan to reduce poverty and income instability among children in the United States. The Russell Sage Foundation Journal of the Social Sciences 4(2):22–42.
Sharkey, P. 2010. The acute effect of local homicides on children’s cognitive performance. Proceedings of the National Academy of Sciences of the United States of America 107(26):11733–11738.
Sharkey, P. T., N. Tirado-Strayer, A. V. Papachristos, and C. C. Raver. 2012. The effect of local violence on children’s attention and impulse control. American Journal of Public Health 102(12):2287–2293.
Sharkley, P. 2016. Confronting neighborhood segregation. https://equitablegrowth.org/ confronting-neighborhood-segregation (accessed January 11, 2019).
SHIELDS for Families. 2011. Annual report. https://www.shieldsforfamilies.org/download/annual-reports/SHIELDS_ANNUAL_10-11.pdf (accessed April 17, 2019).
Skafida, V. 2012. Juggling work and motherhood: The impact of employment and maternity leave on breastfeeding duration: A survival analysis on growing up in Scotland data. Maternal and Child Health Journal 16(2):519–527.
Slopen, N., A. Fenelon, S. Newman, and M. Boudreaux. 2018. Housing assistance and child health: A systematic review. Pediatrics 141(6):e20172742.
SSA (U.S. Social Security Administration). 2019. Monthly statistical snapshot, May 2019. https://www.ssa.gov/policy/docs/quickfacts/stat_snapshot (accessed July 15, 2019).
Stearns, J. 2015. The effects of paid maternity leave: Evidence from temporary disability insurance. Journal of Health Economics 43:85–102.
Stotland, N. E., P. Sutton, J. Trowbridge, D. S. Atchley, J. Conry, L. Trasande, B. Gerbert, A. Charlesworth, and T. J. Woodruff. 2014. Counseling patients on preventing prenatal environmental exposures—a mixed-methods study of obstetricians. PLoS ONE 9(6):e98771.
Strully, K. W., D. H. Rehkopf, and Z. Xuan. 2010. Effects of prenatal poverty on infant health: State earned income tax credits and birth weight. American Sociological Review 75(4):534–562.
Taylor, P., and R. Fry. 2012. The rise of residential segregation by income. Washington, DC: Pew Research Center.
Tessum, C. W., J. S. Apte, A. L. Goodkind, N. Z. Muller, K. A. Mullins, D. A. Paolella, S. Polasky, N. P. Springer, S. K. Thakrar, J. D. Marshall, and J. D. Hill. 2019. Inequity in consumption of goods and services adds to racial–ethnic disparities in air pollution exposure. Proceedings of the National Academy of Sciences of the United States of America 116(13):6001.
The City Project. 2016. U.S. Civil Rights Commission civil rights and environmental justice and enforcement by EPA. The City Project Blog. http://www.cityprojectca.org/blog/archives/43798 (accessed June 3, 2019).
Thornton, P. L., E. C. Kieffer, Y. Salabarria-Pena, A. Odoms-Young, S. K. Willis, H. Kim, and M. A. Salinas. 2006. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: The role of social support. Maternal and Child Health Journal 10(1):95–104.
Tinney, V. A., J. A. Paulson, S. L. Bathgate, and J. W. Larsen. 2015. Medical education for obstetricians and gynecologists should incorporate environmental health. American Journal of Obstetrics & Gynecology 212(2):163–166.
Tollefson, J. 2016. US chemicals law set for overhaul. Nature 534. https://www.nature.com/news/polopoly_fs/1.19973!/menu/main/topColumns/topLeftColumn/pdf/nature.2016.19973.pdf?origin=ppub (accessed July 15, 2019).
TPC (Tax Policy Center). n.d. What is the Child Tax Credit? https://www.taxpolicycenter.org/briefing-book/what-child-tax-credit (accessed May 1, 2019).
Trasande, L., and Y. Liu. 2011. Reducing the staggering costs of environmental disease in children, estimated at $76.6 billion in 2008. Health Affairs (Millwood) 30(5):863–870.
Trasande, L., M. L. Schapiro, R. Falk, K. A. Haynes, A. Berhmann, M. Vohmann, E. D. Stremski, C. Eisenberg, C. Evenstad, H. A. Anderson, and P. J. Landrigan. 2006. Pediatrician attitudes, clinical activities and knowledge of environmental health in Wisconsin. Wisconsin Medical Journal 105(2):45–49.
Trippe, C., C. Tadler, P. Johnson, L. Giannarelli, and D. Betson. 2019. National- and state-level estimates of WIC eligibility and WIC program reach in 2016. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service, Office of Policy Support.
Trust for America’s Health. n.d. Maryland’s efforts to prevent and respond to childhood lead exposure. https://www.tfah.org/story/marylands-efforts-to-prevent-and-respond-to-childhood-lead-exposure (accessed March 20, 2019).
Tulve, N. 2016. Development of a conceptual framework depicting a child’s total (built, natural, social) environment in order to optimize health and well-being. Journal of Environment and Health Science 2(2):1–8.
Tyler, E. T. 2012. Aligning public health, health care, law and policy: Medical-legal partnership as a multilevel response to the social determinants of health. Journal of Health & Biomedical Law 8:211–247.
University of Michigan Prevention Research Center. n.d. Promoting healthy lifestyles among women. http://prc.sph.umich.edu/projects/promoting-healthy-lifestyles-among-women (accessed April 17, 2019).
U.S. Interagency Council on Homelessness. 2018. Homelessness in America: Focus on families with children. Washington, DC: U.S. Interagency Council on Homelessness.
USDA (U.S. Department of Agriculture). 2004. Effects of food assistance programs on nutrition and health. Washington, DC: Economic Research Service.
USDA. 2012. Environmental justice strategic plan: 2012–2014. Washington, DC: U.S. Department of Agriculture.
USDA. 2015. Women, infants and children (WIC): About WIC—WIC at a glance. https://www.fns.usda.gov/wic/about-wic-wic-glance (accessed March 28, 2019).
USDA. 2018a. Evaluation of demonstration projects to end childhood hunger: Interim evaluation report (summary). Washington, DC: USDA Food and Nutrition Service.
USDA. 2018b. Supplemental Nutrition Assistance Program (SNAP). Am I eligible for SNAP? https://www.fns.usda.gov/snap/eligibility (accessed March 28, 2019).
USDA. 2018c. Women, infants and children (WIC). WIC eligibility requirements. https://www.fns.usda.gov/wic/wic-eligibility-requirements (accessed March 28, 2019).
USDA. 2019. WIC program. https://www.ers.usda.gov/topics/food-nutrition-assistance/ wic-program (accessed April 1, 2019).
USDA. n.d. Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). https://www.fns.usda.gov/wic (accessed July 15, 2019).
Walker, C., and H. Matthews. 2017. CCDBG participation drops to historic low. Washington, DC: Center for Law and Social Policy.
Wang, A., A. Padula, M. Sirota, and T. J. Woodruff. 2016. Environmental influences on reproductive health: The importance of chemical exposures. Fertility and Sterility 106(4):905–929.
Wehby, G., D. Dave, and R. Kaestner. 2016. Effects of the minimum wage on infant health. NBER working paper 22373. NBER Working Paper Series. Cambridge, MA: National Bureau of Economic Research.
Whaley, S. E., L. D. Ritchie, P. Spector, and J. Gomez. 2012. Revised WIC food package improves diets of WIC families. Journal of Nutrition Education and Behavior 44(3):204–209.
Wheaton, L., and V. Tran. 2018. The antipoverty effects of the Supplemental Nutrition Assistance Program. Washington, DC: The Urban Institute.
Wilde, P. 2007. Measuring the effect of food stamps on food insecurity and hunger: Research and policy considerations. Journal of Nutrition 137:307–310.
Wilde, P., and M. Nord. 2005. The effect of food stamps on food security: A panel data approach. Review of Agricultural Economics 27(3):425–432.
Wildeman, C., and E. A. Wang. 2017. Mass incarceration, public health, and widening inequality in the USA. The Lancet 389(10077):1464–1474.
Woolf, S. H., L. Aron, D. L, S. M. Simon, E. Zimmerman, and K. X. Luk. 2015. How are income and wealth linked to health and longevity? Washington, DC, and Richmond, VA: Urban Institute and Center on Society and Health.
Wright, R., and D. Christiani. 2010. Gene-environment interaction and children’s health and development. Current Opinion in Pediatrics 22(2):197–201.
Yen, S. T. 2010. The effects of SNAP and WIC programs on nutrient intakes of children. Food Policy 35(6):576–583.
Yen, S. T., D. J. Bruce, and L. Jahs. 2012. Supplemental Nutrition Assistance Program participation and health; evidence from low-income individuals in Tennessee. Contemporary Economic Policy 30(1):1–12.
Ziliak, J. P. 2016. Modernizing SNAP benefits. Policy proposal 2016-06, The Hamilton Project. Washington, DC: The Brookings Institution.




















































































