2
Five Health Care Sector Activities to Better Integrate Social Care
Health care sector leaders often make decisions about improving-social care through care integration and investment in the absence of information about different strategies (Alderwick et al., 2018; Bickerdike et al., 2017; De Milto and Nakashian, 2016; Gottlieb et al., 2017b; Institute for Alternative Futures, 2012). An evidence-informed taxonomy of health care–based strategies that can be used to support and strengthen integration may help guide activities in this area.
Based on the existing literature and other sources, as described in Chapter 1, the committee identified five mutually complementary categories of activities that health systems can adopt to strengthen integration (see Figure 2-1). While all of the categories will ultimately benefit patients, two of these (adjustment and assistance) focus on improving care delivery provided specifically to individual patients based on information about their social risks and protective factors (conditions or attributes that may mitigate or eliminate risk). Two others (alignment and advocacy) relate to roles that the health care sector can play in influencing and investing in social care resources at the community level. All of these delivery and community-level activities are informed by efforts that increase awareness (the fifth category) of individual or community-level socioeconomic risks and assets relevant to a health system’s geographic region or served population. Health care stakeholders—including providers, care delivery organizations, health plans, and government payers—that are exploring opportunities to launch or strengthen integration should understand the challenges of and interplay among these different strategies as well as the range of activities possible within each category. Each of
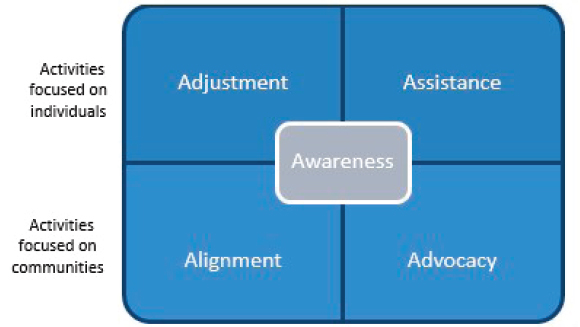
the five categories (awareness, adjustment, assistance, alignment, and advocacy) depends on systems-level changes to implement and sustain integration—including a defined and well-trained workforce, data and digital tool innovations, and new financing models. These systems-level elements are the focus of subsequent chapters of this report.
HEALTH CARE ACTIVITIES TO STRENGTHEN SOCIAL CARE AND HEALTH CARE INTEGRATION
The five complementary types of integration activities correspond to different roles that health systems can play to strengthen the delivery of social care in health care settings. These activities build on the community-informed and patient-centered care1 recommendations from a previous National Academies of Sciences, Engineering, and Medicine (the National Academies) report, Systems Practices for the Care of Socially At-Risk Populations (NASEM, 2016) (see Figure 2-2), by illustrating how these two approaches can most efficiently interact to enable high-quality care, whether to keep people healthy or reduce the burden of disease.
In developing its overall strategy to social care integration, the committee drew on this report’s overarching theme—moving upstream to
___________________
1Patient-centered care is defined as providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions (IOM, 2001).
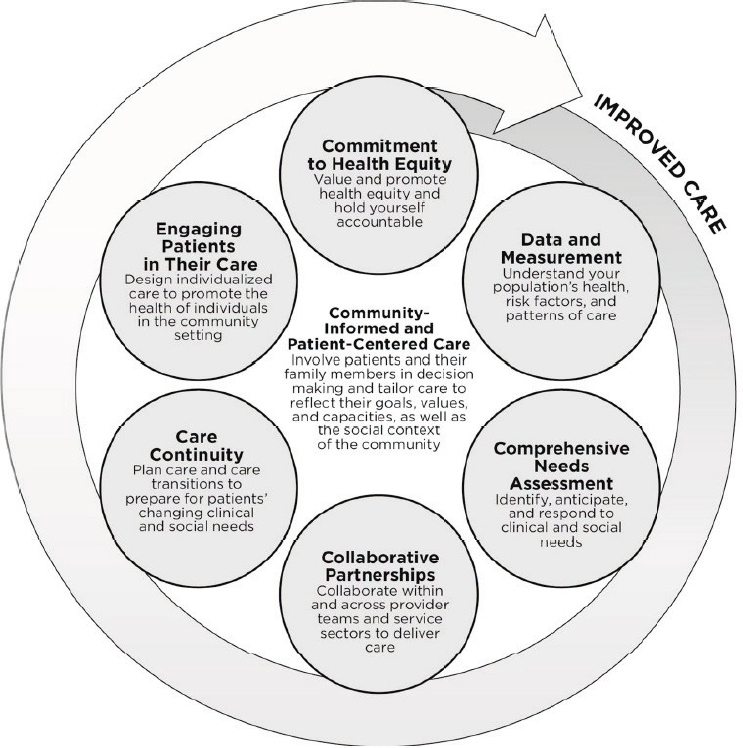
SOURCE: NASEM, 2016.
improve the nation’s health—and recognized that there are both “near” and “far” upstream activities for strengthening integration. Near-upstream activities are targeted toward interactions that individuals have with health care clinical providers or clinical systems, whether for primary prevention or treatment of acute and chronic illness. They include ensuring that health care providers adjust traditional medical care decision making based on social risk and assets data and that patients with social risk factors then receive assistance connecting with and securing available government and community resources related to identified social needs. Far-upstream activities are more community-oriented. They involve aligning health care resources and investments to facilitate
collaborations with community and government sectors as well as bringing health care assets into broader advocacy activities that augment and strengthen social care resources. As an example of how this could work in practice, Table 2-1 describes ways in which individuals’ access to transportation might be improved using the five categories of activities.
The five broad categories are not part of a sequential process; they instead complement one another, and health care stakeholders might engage in multiple strategies simultaneously. These categories provide multiple pathways to achieving integration based on the evidence considered by the committee. Therefore, it would be a disservice to the field to suggest rules, guidelines, or a one-size-fits-all approach because one size does not fit all. Any of these categories is an umbrella for many specific activities that may take different forms, including similar activities that involve different levels of intensity. For example, assistance programs can range from light touch (e.g., providing patient handouts with basic information about social resources) to high touch (offering intensive case management to patients who need more help obtaining resources). These activities are described in more detail below, accompanied by relevant examples.
Awareness: Strategies to Increase the Health Care Sector’s Awareness of Social Risks
Both national and local health sector activities seeking to increase social and health care integration frequently begin with elevating and sustaining awareness about the influence of social risk and protective factors
TABLE 2-1
Transportation-Related Examples Highlighting Different Categories of Social and Health Care Integration Activities
| Awareness | |||
|---|---|---|---|
| Ask people about their access to transportation. | |||
| Adjustment | Assistance | Alignment | Advocacy |
| Reduce the need for in-person health care appointments by using other options such as telehealth appointments. | Provide transportation vouchers so that patients can travel to health care appointments. Vouchers can be used for ride-sharing services or public transit. | Invest in community ride-sharing or time-bank programs. | Work to promote policies that fundamentally change the transportation infrastructure within the community. |
on health outcomes. Across both social and health sectors, the general awareness of the relevance of social factors on health is increasing rapidly. The committee documented an exponential increase in medical literature published over the past 18 years that (1) refers to the social determinants of health (SDOH); and (2) links those determinants with health care delivery (see Figure 2-3).
The committee defined awareness as those activities that identify the social risks and assets of defined patients and populations. Awareness strategies are not limited to sector-level awareness of the intersection of social risks and health outcomes. Instead, the committee recognized that building stakeholders’ investments in social care also involves a more active, immediate awareness of a specific population’s social risks and assets. Though the committee acknowledged that awareness is an important component of both individual- and community-level activities aimed at improving care integration, no consensus exists regarding the most effective or efficient strategies to increase awareness in ways that can facilitate subsequent actions. The strategies that health care systems already invest in to increase awareness vary across settings. The Kaiser Permanente Social Needs Network for Evaluation and Translation (SONNET) has highlighted five different pathways through which information about social risks and assets can be brought to the attention of health care systems (see
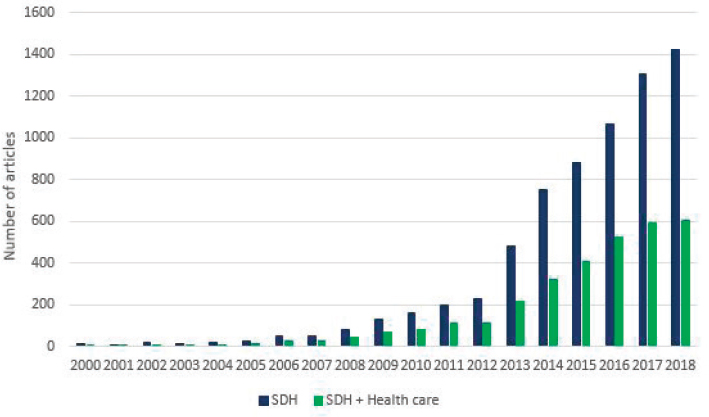
NOTES: Number of results of PubMed searches for “social determinants of health” (SDH) and for “social determinants of health AND health care” (SDH + Health care). Search performed by the committee on January 15, 2019.
SOURCE: Adapted from Gottlieb et al., 2017a.
Figure 2-4): clinical care, screening large populations, screening high-risk groups, hotspotting, and identifying vulnerable communities.
On the clinical side, patients visiting health care organizations are increasingly being asked to answer social risk screening questions in the context of their care and care planning. In some places, screening is incentivized by payers. As part of the MassHealth Medicaid program, for instance, Massachusetts accountable care organizations now include social screening as a measure of care quality (MassHealth, 2018a,b). Similar initiatives are under way in North Carolina and Rhode Island. Clinic-based screening can be universal (everyone in a health care setting is asked about social risks, such as housing or food, either at each visit or at defined intervals; see Pathway 1 in Figure 2-4), or it can be more directed at specific age groups (e.g., children and seniors) or high-risk groups (e.g., people with certain diseases or who are on government insurance) (see Pathways 2 and 3 in Figure 2-4). As an example, Geisinger Health directs food security screening and interventions specifically at patients with diabetes (Feinberg et al., 2017). It is important to note that efforts to raise awareness by collecting data (both on patient clinical history and overall community health) may be affected by unconscious or implicit biases held by program leaders and practitioners, which can create new implementation barriers and workforce training demands (detailed further in Chapters 3 and 6) (Garg et al., 2005; Gottlieb and Alderwick, 2019).
A wide array of social risk screening tools has emerged to meet the demand for clinic-based social risk awareness activities (UCSF, 2019). Existing screening tools vary in the social domains covered, length, language accessibility, and other characteristics (UCSF, 2019) (see Table A-1 for adult screening tools; pediatric screening tools also are available).
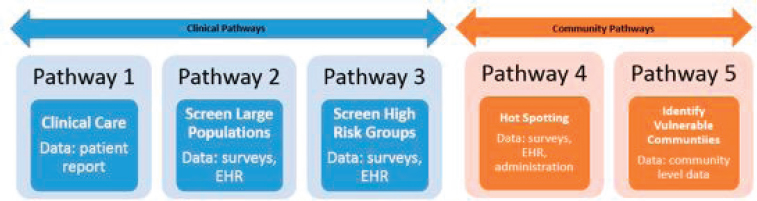
NOTE: EHR = electronic health record
SOURCE: Steiner JF, Adams JL, Clausen D, Clift KM, Millan A, Nau CL, Roblin D, Schmittdiel JA, Schroeder EB. Predictive Models for Social Determinants of Health in KP Members and Communities: An Issue Brief from Kaiser Permanente’s Social Needs Network for Evaluation and Translation (SONNET). Kaiser Permanente SONNET and Kaiser Permanente Community Health, September 2018.
Often these tools use different measures to assess social risks even under a single domain.
Though some screening tools use items from domain-specific validated instruments (e.g., hunger vital signs) (Hager et al., 2010), scant research is available on the psychometric validity of grouped items (Lewis et al., 2019). Existing studies generally indicate that a strong majority of patients find clinic-based social risk screening acceptable (Fleegler et al., 2007), though the unintended consequences (Garg et al., 2016) and possible opportunity costs of clinic-based screening have not been clearly articulated (NASDOH, 2019).
Some health systems use neighborhood- or community-level data to help select patients for more targeted social risk screening or to help identify high-risk communities (see Pathway 5 in Figure 2-4). For example, Cincinnati Children’s Hospital conducts particularly intensive outreach with patients from two high-poverty zip codes to identify children with social needs (Auger et al., 2017). To facilitate such targeted outreach activities, the American Board of Family Medicine and the University of Missouri’s Center for Applied Research and Engagement Systems have together developed the Population Health Assessment Engine (PHATE), which is provided to clinical providers enrolled in the American Board of Family Medicine’s PRIME registry (American Board of Family Medicine, 2019). PHATE uses patient address data to incorporate “community vital signs” into patient charts based on publicly available census-tract-level characteristics. These and other uses of PHATE are summarized in Box 2-1. Some nonprofit hospitals, federally qualified health centers, and local public health departments also use the community-level social risk data in community health needs assessments, which are required by the Internal Revenue Service and are intended to influence community-level investments (Alberti et al., 2014).
The committee searched for indicators of the prevalence of awareness activities (e.g., social risk assessments or data linkages across social and medical sectors). Though multiple surveys targeting different health care stakeholders (e.g., payers, health systems executives, providers, and consumers) have asked about the prevalence of social screening in health care settings, there are limited data that can be synthesized across these surveys (findings from 23 surveys are summarized by SIREN) (Cartier et al., 2019). The majority of the existing surveys ask whether the health care system conducts some form of social risk assessment broadly without asking further questions about the specific strategies undertaken to obtain information. For example, survey items typically fail to distinguish among universal, clinic-based social screening, targeted screening for high-risk patients, and community data integration; they do not ask respondents to report the numbers of patients who complete social risk
assessments; and they do not ask about the capacity of the workforce or activities undertaken in general or by discipline to respond to any identified risks. Some research has explored the adequacy of using electronic health record (EHR) documentation (e.g., LOINC, SNOMED, International Statistical Classification of Diseases and Related Health Problems, 10th Revision [ICD-10], Current Procedural Terminology [CPT] codes) to gauge the prevalence of individual-level social risk screening, though this would fail to capture other related activities that facilitate social needs and asset awareness. At this time, the lack of both coding standards and capacity in medical coding systems and documentation incentives makes EHRs an unreliable source of information (Arons et al., 2018; DeSilvey et al., 2018; Lewis et al., 2016; Navathe et al., 2018; Torres et al., 2017). These and other technology-based opportunities to strengthen care integration are the focus of Chapter 4.
In reviewing different strategies to increase the health care sector’s awareness of patient and population social risk and protective factors, the committee went on to ask whether increasing the health care sector’s recognition of social risks alone could contribute to changes in health outcomes in the absence of dedicated social care interventions. Specifically, does asking equate to an intervention? This question could be especially relevant to the awareness strategies in which individual patients are asked about their social risks in the context of a health care delivery encounter. Does asking about social risks without coupling screening activities with a related social care intervention, such as, at a minimum, making a referral for a patient to follow up at his or her discretion, affect the
provider–patient relationship in some way? Could asking have negative consequences, such as triggering or creating trauma (Garg et al., 2016)? The committee did not find a strong body of evidence to support either positive or negative consequences of implementing awareness strategies in isolation. This is likely because there are few clinical systems implementing clinic-based screening without some form of intervention.
Even in settings when relevant interventions are offered, patients do not consistently desire assistance, making it important to consider shared decision-making principles as part of patient-centered care planning that results from identifying social risk factors and social needs (Swavely et al., 2018; Tong et al., 2018). Some research suggests that patients do not believe that social screening needs to be accompanied by interventions and may have salutary effects in isolation, although the evidence is mixed (Byhoff et al., in press; Palakshappa et al., 2017). As an example, patients’ perceptions that they are receiving equity-oriented care—including care that is trauma-, culture-, and context-informed—are linked with comfort and confidence in care, which itself is associated with improved confidence in managing health problems (Ford-Gilboe et al., 2018). Lower rates of patient–provider discussions about social demographic circumstances were found to be associated with six times higher odds of poor medication adherence (Schoenthaler et al., 2017). More research is needed on how screening activities themselves affect patient–provider relationships.
Adjustment: Activities Where Social Risk Information Is Used to Inform Clinical Care Decision Making
There are many different ways in which an awareness of social risks (collected through any of the awareness strategies described above) can subsequently influence health care sector activities, leading to such things as providing social care coordination and services and augmenting the availability of social care resources (see assistance, alignment, and advocacy sections below). Social risk data also could be used to inform adjustments to care that focus not on resolving social risks directly but instead on altering clinical care to accommodate identified social barriers. Thus, social and economic barriers to high-quality care may be mitigated by changes to how the health care services are delivered in addition to any attempts to resolve the social risk itself.
Many examples of adjustment strategies were identified in the literature, including the delivery of language and literacy-concordant services; smaller doctor-patient panel sizes for cases with socially complex needs (e.g., teams caring for homeless patients in the U.S. Department of Veterans Affairs [VA] health system have panel sizes smaller than the
size of other VA care teams); offering open-access scheduling or evening and weekend clinic access; and providing telehealth services, especially in rural areas (Felland et al., 2003; VA, 2019). Other examples of ways that providers can adjust care based on known social risks involve changing insulin dosages at the end of the month when food benefits are more likely to run out (Seligman et al., 2014) and shifting to indoor or supervised physical activity recommendations for patients who live in unsafe neighborhoods (Waite, 2018). These adjustments can have a significant impact; for instance, providing last-shift or overnight dialysis beds, offering longer acting anti-hypertensive medications, or changing visit schedules may improve outcomes in homeless patients with end-stage renal disease (Holley et al., 2006; Podymow and Turnbull, 2013). These examples highlight adaptations to traditional care designed to accommodate patients’ social contexts but are not interventions focused on changing the underlying social risk.
The amount of evidence suggesting that adjustment interventions affect health varies depending on the type of intervention because there are many different activities in this general category. For example, a strong body of evidence supports providing interpreter services, which can be considered a form of adjusted care delivery since care modifications (as opposed to English classes) are provided based on an understanding of patient social and cultural characteristics that can be gained through better communication (Ku and Flores, 2005; Wasserman et al., 2014). As described in the awareness section above, some evidence suggests that context-informed care can influence patients’ experience of care, health behaviors, and health outcomes. Health services researchers have described clinical care that incorporates an understanding of social context as “contextualized care” (Weiner et al., 2010). And while there is a relevant, intersecting body of evidence on shared decision making and patient-centered care approaches, research in those areas has not consistently and explicitly focused on care modifications or interventions that mitigate the impacts of social and economic adversity (Sambare et al., 2017).
Social risk–adjusted payments also could be considered adjustment strategies if they are not linked explicitly to requirements like social care coordination or housing supports. Massachusetts is currently experimenting with Medicaid capitation rates that change based on patients’ social risks (e.g., neighborhood deprivation and housing status) (Breslin et al., 2017; Commonwealth of Massachusetts, 2017; Crumley and Marlise, 2018). Chapter 5 provides more details about risk-adjusted payments.
The increased focus on the intersection of social risk and health outcomes at a national level provides an opportunity to recognize, evaluate,
and potentially incentivize contextualized care so that it can be implemented more systematically throughout the U.S. health care sector. The adjustment approach to social care integration is potentially the least controversial of health care strategies to strengthen social care since the focus of care remains within the traditional wheelhouse of medical care. Nonetheless, substantial gaps in knowledge exist about how adjustment strategies should affect disease-specific care decisions. For example, though many expert care guidelines on diabetes, hypertension, and obesity recognize the influence of social context, sparse information is provided in those social guidelines about how providers should alter their care based on specific social risks (American Diabetes Association, 2017; Armstrong and Joint National Committee, 2014; Eckel et al., 2014; Jensen et al., 2014; Stone et al., 2014). Thus, it is not surprising that some research shows that clinical care is not systematically context-informed in U.S. health care settings. When social risk data are provided via verbal cues, for instance, providers inconsistently incorporate the information into care decisions (Levinson et al., 2000; Tong et al., 2018; Weiner et al., 2010). In one study, providers given verbal cues about patients’ complex contextual circumstances subsequently provided contextually appropriate care in less than 23 percent of cases (Weiner et al., 2010). Health care workers may resist universal screening given the limited evidence on how to screen most effectively, insufficient support for referrals and follow up, and changes in procedures and workflow that may be necessitated by screening.
There are many outstanding questions about whether there should be more explicit adjustments to care recommended for patients with specific social risks (e.g., food or housing insecurity) in order to maximize the uptake of guideline-concordant care. For instance, the potential for such adjustments to widen rather than lessen health inequities must be considered. Concerns have arisen from concrete examples in the health care system where social risk factors have been wielded to deny evidence-based care to select populations. For instance, history suggests African Americans have been systematically denied adequate pain management due to both conscious and unconscious biases about pain perception and racialized depictions of addiction, substance abuse, social support, and a perceived inability to comply with pain management practices (Primm et al., 2004). To avoid such discrimination caused by the presence of social risks, new care management guidelines must be thoughtfully designed both to incorporate social risks into personalized care and to provide guardrails against discrimination. As these guidelines emerge, appropriately applying them will require relevant training curricula and incentives (Weiner and Schwartz, 2016). Training of the social care workforce is discussed in Chapter 3, and payment and financing reform that can support this work is the focus of Chapter 5.
Assistance: Strategies to Link Patients with Social Needs to Government and Community Resources
Beyond increasing awareness of patients’ social risks and adjusting care to accommodate endorsed risks, there is a new focus on health care–based interventions on reducing social risk by providing assistance in connecting patients with relevant social care resources. The literature contains descriptions of a variety of assistance activities that have been undertaken by health systems and communities. These assistance activities vary in intensity, from lighter touch (one-time provision of resources, information, or referrals) to longer and more intensive interventions that attempt to assess and address patient-prioritized social needs more comprehensively (Bickerdike et al., 2017; Gottlieb et al., 2017b; Hannigan and Coffey, 2011).
Lighter-touch assistance activities can include providing information or vouchers for patients to obtain resources in the community (e.g., through curated resource lists) or referring patients to specific programs (e.g., to medical–legal partnerships to address legal barriers to housing or benefits, to eligibility counselors to enroll in Medicaid, or to social workers to obtain help with heating bills or short-term rental assistance). These lighter-touch interventions can include direct assistance (e.g., sending patients home with food if they report being hungry, providing rides directly to and from appointments, or offering respite care activities to support caregivers) (Berkowitz et al., 2018; Chaiyachati et al., 2018; Lindau et al., 2016; Martin et al., 2015).
More intensive assistance activities are often directed to medically and socially complex patients, and they typically include processes such as relationship building, comprehensive biopsychosocial needs assessments, care planning, interventions (e.g., resource connections, ongoing case management, and behavioral activation interventions, such as motivational interviewing), and long-term community-based supports (Burns and Essing, 2018; Lukens and McFarlane, 2004; Miller and Rollnick, 2012; NEJM Catalyst, 2017; Rizzo and Rowe, 2016). These more intensive assistance activities can enable the identification of co-occurring mental health concerns (such as low self-esteem, loneliness, and a history of trauma) and physical health barriers. As a result, intensive assistance activities can contribute to care adjustments at the same time as they are supporting the different processes. This has made the impacts of social care assistance activities difficult to disentangle from other intervention activities targeted at high-complexity patients (Gottlieb et al., 2017b). The AIMS care coordination model and the IMPaCT model are two examples of a higher-intensity assistance approach (see Box 2-2).
Assistance is sometimes provided directly by clinical care team members, such as primary care providers or registered nurses. Other times,
these activities are assigned to individuals whose roles are more focused on social care, such as social workers (Altfeld et al., 2012; Boutwell et al., 2016; Fabbre et al., 2011; Fraser et al., 2018; Gehlert et al., 2015; Rizzo and Rowe, 2016; Stanhope and Straussner, 2017), patient navigators, community health workers, or care coordinators (Berkowitz et al., 2018; Chinman et al., 2015; Dale et al., 2008; Gunderson et al., 2018; Kangovi et al., 2015; Repper and Carter, 2011; Salzer et al., 2010). These staff may be employed by health systems or by partner community-based organizations (Schrage, 2018). Systematically integrating assistance activities into health care organizations may necessitate changes in workflow, team dynamics, and organizational culture, and it may demand strategies to engage patients that depart from usual care. Together these requirements can present substantial barriers to implementation (Helfrich et al., 2016; also see Chapter 6).
Despite substantial evidence concerning the connection between social risks and health outcomes and use, there are few rigorously designed studies on the impact of assistance interventions on outcomes or use among participants (Gottlieb et al., 2017a). Rather, most evaluations of interventions have focused on process outcomes, such as patient satisfaction and self-reported health-related measures, and have not differentiated between specific intervention components (Gottlieb et al., 2017a). Moreover, many assistance interventions have evolved over time under principles of continuous quality improvement and learning health systems, using techniques such as pre–post analyses rather than more rigorous randomized control trials (McGinnis et al., 2014). Further research is needed in this area on the wide range of interventions that are and could be used to reduce patients’ social risk. This research will need to more clearly articulate the added value of providing assistance services, particularly for specific populations who may report the same social need but have differing complexities and benefit eligibility that should inform assistance activities. The health care sector’s approach of providing assistance with basic material needs, for instance, to patients who are medically complex is likely to differ from providing assistance to healthier populations.
Alignment and Advocacy: Activities Where Health Care Organizations Partner and Collaborate with Other Sectors
Increasingly, health care delivery organizations, health plans, and other health care stakeholders play roles in aligning health care assets with existing social care assets in communities and advocating for more social resources to improve community health and well-being. The committee defined alignment activities to include those undertaken by health care systems to understand existing social care assets in the community,
organize them in such a way as to encourage synergy among the various activities, and invest in and deploy them to prevent emerging social needs and improve health outcomes. The committee defined advocacy activities as those in which health care organizations work with partner social care organizations to promote policies that facilitate the creation and redeployment of assets or resources in order to improve health outcomes and prevent emergence of unmet social needs. While providers, patients, and caregivers also can advocate to improve social resources for individual patients, the committee defined health care sector advocacy as activities that are aimed more broadly at increasing the availability of community resources for groups of patients. The net effect of both of these types of activities (alignment and advocacy) is to achieve what the Centers for Medicare & Medicaid Services defined as the objective of the alignment track of the Accountable Health Communities Model, which is to “optimize community capacity to address health-related social needs” (CMS, 2019).
In both the alignment and advocacy categories, health care organizations leverage their political, social, and economic capital within a community or local environment to encourage and enable health care and social care organizations to partner and pool resources, such as services and information, to achieve greater net benefit from the health care and social care services available in the community. Since 2009, reports from the Agency for Healthcare Research and Quality; the National Academies of Sciences, Engineering, and Medicine;2 the U.S. Preventive Services Task Force; and other organizations have recommended improving the integration of clinical, public health, and community-based services and focusing on increasing the uptake of clinical preventive services (AHRQ, 2016; ASTHO, 2015; Dzau et al., 2017; IOM, 2012; Long et al., 2017; Ockene et al., 2007). Cross-sector collaboration is also a foundational strategy in the Robert Wood Johnson Foundation’s Action Framework to build a Culture of Health and has been described in multiple reports on how partnership-driven work can integrate health care and social care services to improve population health (Plough, 2015; Towe et al., 2016). An important limitation of these collaborations is that they often occur in the context of uneven power dynamics and historical fragmentation between sectors due to differing funding sources and workforces.
Though such partnerships are not new, health care organizations are engaging in collaborative work in increasingly varied ways. However,
___________________
2 As of March 2016, the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine continues the consensus studies and convening activities previously carried out by the Institute of Medicine (IOM). The IOM name is used to refer to publications issued prior to July 2015.
despite national recommendations and increasing activity concerning the use of intersectoral work to strengthen community resources, the literature on the effectiveness of the health care sector’s alignment and advocacy work in large part remains limited to case studies. Some evidence suggests that alignment and advocacy activities can improve a variety of health outcomes, from infection control to asthma and cardiovascular outcomes (Boex et al., 1998). One study demonstrating effectiveness found significantly lower death rates from potentially preventable conditions among communities with multi-sector networks supporting population health activities with alignment and advocacy strategies extending well beyond the boundaries of the traditional health care system to include policy changes supporting improved health outcomes (e.g., smoking bans and increasing access to healthy food) (Mays et al., 2016). Reporting bias may skew the literature toward positive outcomes narratives, including impacts on health care use, expenditures, and overall population-level health outcomes.
With the above caveats, a handful of illustrative examples are available to demonstrate three strategies that health care stakeholders have taken to increase alignment and advocacy in their communities.
- Partner with social care agencies to fill known gaps in services for beneficiaries. One approach used by health care organizations to improve alignment and advocacy is to strengthen collaborations with social care organizations to directly provide needed services. For instance, the network Area Agencies on Aging coordinates with community-based organizations to provide community case management, home-delivered meals, and caregiver respite to aging populations (Brewster et al., 2018). This partnership formalized the referral infrastructure and established a compensation mechanism for these services that supports the assistance activities of the clinics while also aligning and investing in local resources and helping sustain and strengthen local, trusted institutions. In another example, the Henry Ford Health System partnered with Uber, Lyft, and Ford Motor Company to provide transportation to its patient population, with a particular focus on those in underserved communities (Knowles, 2018; Martinez, 2018). At the same time they are campaigning to modify existing transportation infrastructure in the city of Detroit in order to facilitate access in vulnerable communities. An increasing number of health care organizations are also investing in low-income housing. For example, UnitedHealth Group invested $50 million in low-income housing tax credit funds managed by the Greater Minnesota Housing Fund and Enterprise Community Investment,
-
resulting in the development of multi-family rental units for very low-income and special needs households (UnitedHealth Group, 2013).
- Develop anchor institution strategies. A growing number of health care initiatives explore roles that the health care sector can play in improving the social, economic, and political landscape of local economies. In these cases, health care organizations adopt place-based, health-equity-focused strategies that recognize that social and economic determinants are largely responsible for health outcomes. These organizations often describe an “anchor mission” that helps them realign institutional assets to broadly combat social and economic disparities by investing in communities. Hospitals and health systems spend $782 billion annually, employ more than 5.6 million people, and hold investment portfolios of more than $400 billion (Ubhayakar et al., 2017). Investments made through anchor institution strategies sometimes rely on community development financial institutions, which provide access to capital often unavailable from traditional lenders, or on social impact bonds, in which case private funds are used to catalyze initiatives to address community needs. In 2019, more than 40 health care delivery organizations were participating in an anchor institution collaborative activity (Healthcare Anchor Network, 2019). For example, Rush University Medical Center’s (RUMC’s) anchor strategy involves hiring individuals from underserved communities to provide them with economic opportunity, establishing local and minority-owned business preferences for vendor and supply chain contracts, and creating a local financial investment strategy (Harkavy, 2016; Ubhayakar et al., 2017). As part of this approach, since 2017 RUMC has provided $6 million in loans to community development financial institutions, such as one supporting the city of Chicago’s Neighborhood Rebuild Training pilot program. In programs like these the funding can be used in various aspects of the community, including renovations to homes in high crime areas and providing on-the-job training and credentialing opportunities to youth and ex-offenders (Chicago Community Loan Fund, 2018; Community Development Financial Institutions, 2019; RUMC, 2017). While it is difficult to gauge the impact of such long-term investments and collaborations, more outcome data will become available as more health care stakeholders undertake and report on their anchor activities. Another example is Stephen and Sandra Sheller 11th Street Family Health Services, a federally qualified health center in Philadelphia, Pennsylvania (Waite, 2018). 11th Street
-
works with neighborhood residents in cooperation with schools, churches, and community groups and agencies to provide for the biological, psychological, and social needs of its patients by offering a wide range of services, including creative arts therapies, fitness training, and nutrition classes.
- Organize and engage in cross-sector coalitions. Other alignment and advocacy activity involves more actively organizing and engaging in multi-sector coalitions generally aimed at place-based community improvement. Johns Hopkins University, located in Baltimore, Maryland, is a member of the East Baltimore Development Initiative, a multi-stakeholder coalition seeking to revitalize the East Baltimore neighborhood (East Baltimore Development Inc., 2010). The university has engaged with the community through the Homewood Community Partners Initiative (HCPI) in 10 neighborhoods located around its main campus (JHU, 2019). HCPI has worked with the Central Baltimore Partnership, various community and neighborhood organizations, and other stakeholders, such as foundations and anchor institutions, to develop an implementation plan for the area. This plan contains 29 priority recommendations for action, including blight removal, housing and commercial development, and fundraising. From 2013 to 2016 Maryland established health enterprise zones in five communities to stimulate alignment and advocacy activities among local health departments, health care delivery organizations, and social care and community-based organizations; the effort resulted in a net cost savings of $93.39 million (across all zip codes that participated) due to reduced inpatient hospital visits (Gaskin et al., 2018). Hennepin Health, a Minnesota-based managed care program, reported similar notable gains coordinating assets at the county level, including across social care agencies, county-based health departments, multiple health systems, and a nonprofit health plan (Vickery et al., 2018). Together these agencies reported reductions in emergency department use and increased primary and preventative care use for Medicaid beneficiaries.
These strategies alone or in combination may be funded by health care organizations via community benefit programs—the required contributions that nonprofit health care delivery systems must make to earn their tax-exempt status.
The committee recognizes that health care organizations can bring funds, data, and political and other forms of capital to catalyze community activities—including through the various strategies described in this chapter. But the health care sector has not consistently wielded this capital
in the interest of primary prevention of clinical conditions or prevention of the complicating social conditions. Effective strategies to strengthen social and health care integration are likely to require more attention to the experience and expertise of community stakeholders. This will demand organizational humility from the health care sector, particularly as it moves from health care delivery to community-focused activities. Alignment and advocacy initiatives should incorporate patients, families, and community members in program planning and execution to help avoid historical missteps.
As effective strategies emerge, attention will need to be given to implementation feasibility and program sustainability, including the workforce, technology, and payment models that will support the strategies and enable long-term interventions and corresponding reductions in health disparities.
FINDINGS
- Five complementary types of activities can facilitate the integration of social and health care. They are awareness, adjustment, assistance, alignment, and advocacy.
- These types of activities should not be considered mutually exclusive, and one does not necessarily build on another. The exception involves awareness activities, which typically are foundational to the others.
- Some health care systems have had success with using these strategies to strengthen social care services and, subsequently, to link social care activities with improved health outcomes.
- Robust outcome evaluations have not been conducted on social care integration activities, which limits the committee’s ability to draw conclusions and make recommendations about specific evidence-based practices.
- A one-size-fits-all approach is neither feasible nor advisable, since context should influence the adoption of specific social and health care integration activities.
REFERENCES
AHRQ (Agency for Healthcare Research and Quality). 2016. Clinical–community linkages. https://www.ahrq.gov/professionals/prevention-chronic-care/improve/community/index.html (accessed February 7, 2019).
Alberti, P. M., K. Sutton, I. Baer, and J. Johnson. 2014. Community health needs assessments: Engaging community partners to improve health. Washington, DC: Association of American Medical Colleges.
Alderwick, H. A. J., L. M. Gottlieb, C. M. Fichtenberg, and N. E. Alder. 2018. Social prescribing in the U.S. and England: Emerging interventions to address patients’ social needs. American Journal of Preventive Medicine 54(5):715–718.
Altfeld, S. J., E. Avery, R. L. Golden, T. J. Johnson, K. Karavolos, V. Nandi, M. Rooney, G. E. Shier, and A. J. Perry. 2012. Effects of an enhanced discharge planning intervention for hospitalized older adults: A randomized trial. Gerontologist 53(3):430–440.
American Board of Family Medicine. 2019. PHATE: The Population Health Assessment Engine. https://primeregistry.org/phate (accessed April 12, 2019).
American Diabetes Association. 2017. Standards of medical care in diabetes—2017, abridged for primary care providers. Diabetes Care 35(1):5–26.
Armstrong, C., and Joint National Committee. 2014. JNC8 guidelines for the management of hypertension in adults. American Family Physician 90(7):503–504.
Arons, A., S. DeSilvey, C. Fichtenberg, and L. Gottlieb. 2018. Documenting social determinants of health-related clinical activities using standardized medical vocabularies. Journal of the American Medical Informatics Association Open. doi: 10.1093/jamiaopen/ooy051.
ASTHO (Assocation of State and Territorial Health Officials). 2015. Community–clinical linkages to improve hypertension identification, management, and control. Issue brief. http://www.astho.org/Prevention/Community-Clinical-Linkages-Issue-Brief (accessed May 26, 2019).
Auger, K. A., R. S. Kahn, J. M. Simmons, B. Huang, A. N. Shah, K. Timmons, and A. F. Beck. 2017. Using address information to identify hardships reported by families of children hospitalized with asthma. Academic Pediatrics 17(1):79–87.
Berkowitz, S. A., S. Parashuram, K. Rowan, L. Andon, E. B. Bass, M. Bellantoni, D. J. Brotman, A. Deutschendorf, L. Dunbar, S. C. Durso, A. Everett, K. D. Giuriceo, L. Hebert, D. Hickman, D. E. Hough, E. E. Howell, X. Huang, D. Lepley, C. Leung, Y. Lu, C. G. Lyketsos, S. M. E. Murphy, T. Novak, L. Purnell, C. Sylvester, A. W. Wu, R. Zollinger, K. Koenig, R. Ahn, P. B. Rothman, P. M. C. Brown, and Johns Hopkins Community Health Partnership (J-CHiP) team. 2018. Association of a care coordination model with health care costs and utilization: The Johns Hopkins Community Health Partnership (J-CHiP). JAMA Network Open 1(7):e184273.
Bickerdike, L., A. Booth, P. M. Wilson, K. Farley, and K. Wright. 2017. Social prescribing: Less rhetoric and more reality. A systematic review of the evidence. BMJ Open 7(4):e013384.
Boex, J. R., J. Cooksey, and T. Inui. 1998. Hospital participation in community partnerships to improve health. Joint Commission Journal on Quality Improvement 24(10):541–548.
Boutwell, A. E., M. B. Johnson, and R. Watkins. 2016. Analysis of a social work–based model of transitional care to reduce hospital readmissions: Preliminary data. Journal of the American Geriatrics Society 64(5):1104–1107.
Breslin, E., A. Lambertino, D. Heaphy, and T. Dreyfus. 2017. Medicaid and social determinants of health: Adjusting payment and measuring health outcomes. Health Management Associates. https://www.healthmanagement.com/wp-content/uploads/SHVS_SocialDeterminants_HMA_July2017.pdf (accessed May 26, 2019).
Brewster, A. L., S. Kunkel, J. Straker, and L. A. Curry. 2018. Cross-sectoral partnerships by area agencies on aging: Associations with health care use and spending. Health Affairs (Millwood) 37(1):15–21.
Burns, A., and P. Essing. 2018. Integrating psychosocial risk factors into ongoing care. Advisory Board. https://www.advisory.com/-/media/Advisory-com/Research/PHA/ResearchBriefings/2018/PHA-Psychosocial%20Risk%20Factors%20Brief.pdf (accessed May 26, 2019).
Byhoff, E., E. H. De Marchis, D. Hessler, C. Fichtenberg, N. Adler, A. J. Cohen, K. M. Doran, S. Ettinger de Cuba, E. W. Fleegler, N. Gavin, A. G. Huebschmann, S. T. Lindau, E. L. Tung, M. Raven, S. Jepson, W. Johnson, A. L. Olson, M. Sandel, R. S. Sheward, and L. M. Gottleib. In press. Part II: A qualitative study of social risk screening acceptability in patients and caregivers. American Journal of Preventive Medicine.
Cartier, Y., M. Pantell, E. De Marchis, and L. Gottlieb. 2019. National surveys gauging the prevalence of social care-related activities in the health care sector. https://sirenetwork.ucsf.edu/tools-resources/mmi/national-surveys-gauging-prevalence-social-care-related-activities-health-care (accessed February 25, 2019).
Chaiyachati, K. H., R. A. Hubbard, A. Yeager, B. Mugo, J. A. Shea, R. Rosin, and D. Grande. 2018. Rideshare-based medical transportation for Medicaid patients and primary care show rates: A difference-in-difference analysis of a pilot program. Journal of General Internal Medicine 33(6):863–868.
Chicago Community Loan Fund. 2018. Chicago neighborhood pilot launches workforce services component. https://cclfchicago.org/news/about-us/chicago-neighborhood-rebuild-pilot-launches-workforce-services-component (accessed August 4, 2019).
Chinman, M., R. S. Oberman, B. H. Hanusa, A. N. Cohen, M. P. Salyers, E. W. Twamley, and A. S. Young. 2015. A cluster randomized trial of adding peer specialists to intensive case management teams in the Veterans Health Administration. Journal of Behavioral Health Services & Research 42(1):109–121.
CMS (Centers for Medicare & Medicaid Services). 2019. Accountable health communities model. https://innovation.cms.gov/initiatives/ahcm (accessed May 26, 2019).
Commonwealth of Massachusetts. 2017. FAQs for MassHealth’s 2017 payment model. https://www.mass.gov/files/documents/2017/11/07/social-determinants-of-health-faq.pdf (accessed February 5, 2019).
Community Development Financial Insitutions Coalition Report. 2019. http://cdfi.org/wp-content/uploads/2019/03/2019-CDFI-Report-Complete-FINAL.pdf (accessed August 4, 2019).
Crumley, D., and P.-W. Marlise. 2018. Addressing social determinants of health through Medicaid accountable care organizations. CHCS Blog: Center for Health Care Strategies. https://www.chcs.org/addressing-social-determinants-health-medicaid-accountable-care-organizations (accessed May 26, 2019).
Dale, J., I. O. Caramlau, A. Lindenmeyer, and S. M. Williams. 2008. Peer support telephone calls for improving health. Cochrane Database of Systematic Reviews (4):CD006903.
De Milto, L., and M. Nakashian. 2016. Using social determinants of health data to improve health care and health: A learning report. Robert Wood Johnson Foundation. https://www.rwjf.org/en/library/research/2016/04/using-social-determinants-of-health-data-to-improve-health-care-.html (accessed May 26, 2019).
DeSilvey, S., A. Ashbrook, R. Sheward, H. Hartline-Grafton, S. Ettinger de Cuba, and L. Gottlieb. 2018. An overview of food insecurity coding in health care settings: Existing and emerging opportunities. Boston, MA: Hunger Vital Sign National Community of Practice. http://www.frac.org/wp-content/uploads/Overview_of_Food_Insecurity_Coding_Report_Final-1.pdf (accessed May 26, 2019).
Dzau, V. J., M. McClellan, J. M. McGinnis, and E. M. Finkelman (eds.). 2017. Vital directions for health & health care: An initiative of the National Academy of Medicine. Washington, DC: National Academy of Medicine.
East Baltimore Development Inc. 2010. About. http://ebdi.org/about (accessed February 8, 2019).
Eckel, R. H., J. M. Jakicic, J. D. Ard, J. M. de Jesus, N. H. Miller, V. S. Hubbard, I. M. Lee, A. H. Lichtenstein, C. M. Loria, B. E. Millen, C. A. Nonas, F. M. Sacks, S. C. Smith, L. P. Svetkey, T. A. Wadden, and S. Z. Yanovski. 2014. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk. Circulation 129(25 Suppl 2):S76–S99.
Fabbre, V. D., A. S. Buffington, S. J. Altfeld, G. E. Shier, and R. L. Golden. 2011. Social work and transitions of care: Observations from an intervention for older adults. Journal of Gerontological Social Work 54(6):615–626.
Feinberg, A. T., J. R. Slotkin, A. Hess, and A. R. Erskine. 2017. How Geisinger treats diabetes by giving away free, healthy food. https://hbr.org/2017/10/how-geisinger-treats-diabetes-by-giving-away-free-healthy-food (accessed March 25, 2019).
Felland, L. E., C. S. Lesser, A. B. Staiti, A. Katz, and P. Lichiello. 2003. The resilience of the health care safety net, 1996–2001. Health Services Research 38(1 Pt. 2):489–502.
Fleegler, E. W., T. A. Lieu, P. H. Wise, and S. Muret-Wagstaff. 2007. Families’ health-related social problems and missed referral opportunities. Pediatrics 119(6):e1332–e1341.
Ford-Gilboe, M., C. Herbert, B. E. Jackson, J. G. Lavoie, B. Pauly, N. A. Perrin, V. Smye, C. Varcoe, B. Wallace, N. C. Wathen, S. T. Wong, and A. J. Browne. 2018. How equity-oriented health care affects health: Key mechanisms and implications for primary health care practice and policy. Milbank Quarterly 96(4):635–671.
Fraser, M. W., B. M. Lombardi, S. Wu, L. de Saxe Zerden, E. L. Richman, and E. P. Fraher. 2018. Integrated primary care and social work: A systematic review. Journal of the Society for Social Work and Research 9(2):175–215.
Garg, A. X., N. K. Adhikari, H. McDonald, M. P. Rosas-Arellano, P. J. Devereaux, J. Beyene, J. Sam, and R. B. Haynes. 2005. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: A systematic review. JAMA 293(10):1223–1238.
Garg, A., R. Boynton-Jarrett, and P. H. Dworkin. 2016. Avoiding the unintended consequences of screening for social determinants of health. JAMA 316(8):813–814.
Gaskin, D. J., R. McCleary, and R. J. Thorpe. 2018. The Maryland Health Enterprise Zone Initiative reduced hospital cost and utilization in underserved communities Determinants of Health 37(10):1546–1554.
Gehlert, S., S. Collins, R. Golden, and P. Horn. 2015. Social work participation in accountable care organizations under the Patient Protection and Affordable Care Act. Health & Social Work 40(4):E142–E147.
Gottlieb, L. M., and H. Alderwick. 2019. Integrating social and medical care: Could it worsen health and increase inequity? Annals of Family Medicine 17(1):77–81.
Gottlieb, L., C. Fichtenberg, and N. Adler. 2017a. Introducing the Social Interventions Research and Evaluation Network.. Social Interventions Research and Evaluation Network. http://sirenetwork.ucsf.edu/sites/sirenetwork.ucsf.edu/files/SIREN%20Issue%20Brief.pdf (accessed May 26, 2019).
Gottlieb, L. M., H. Wing, and N. E. Adler. 2017b. A systematic review of interventions on patients’ social and economic needs. American Journal of Preventative Medicine 53(5):719–729.
Gunderson, J. M., M. L. Wieland, O. Quirindongo-Cedeno, G. B. Asiedu, J. L. Ridgeway, M. W. O’Brien, T. M. Nelson, R. Buzard, C. Campbell, and J. W. Njeru. 2018. Community health workers as an extension of care coordination in primary care: A community-based cosupervisory model. Journal of Ambulatory Care Management 41(4):333–340.
Hager, E. R., A. M. Quigg, M. M. Black, S. M. Coleman, T. Heeren, R. Rose-Jacobs, J. T. Cook, S. A. Ettinger de Cuba, P. H. Casey, M. Chilton, D. B. Cutts, A. F. Meyers, and D. A. Frank. 2010. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 126(1):e26–e32.
Hannigan, B., and M. Coffey. 2011. Where the wicked problems are: The case of mental health. Health Policy 101(3):220–227.
Harkavy, I. 2016. Engaging urban universities as anchor institutions for health equity. American Journal of Public Health 106(12):2155–2157.
Healthcare Anchor Network. 2019. About the healthcare anchor network. https://www.healthcareanchor.network/about.html (accessed May 24, 2019).
Helfrich, C. D., P. W. Sylling, R. C. Gale, D. C. Mohr, S. E. Stockdale, S. Joos, E. J. Brown, D. Grembowski, S. M. Asch, S. D. Fihn, K. M. Nelson, and L. S. Meredith. 2016. The facilitators and barriers associated with implementation of a patient-centered medical home in VHA. Implementation Science 11:24.
Holley, J. L., C. DeVore, T. Obrero, and L. Noland. 2006. Managing homeless dialysis patients. Nephrology News & Issues 20(1):49–50, 52–53.
Institute for Alternative Futures. 2012. Community health centers leveraging the social determinants of health. http://www.altfutures.org/wp-content/uploads/2016/04/2012_Report_Community-Health-Centers-Leveraging-the-Social-Determinants-of-Health.pdf (accessed May 23, 2019).
IOM (Institute of Medicine). 2012. An integrated framework for assessing the value of community-based prevention. Washington, DC: The National Academies Press.
Jensen, M. D., D. H. Ryan, C. M. Apovian, J. D. Ard, A. G. Comuzzie, K. A. Donato, F. B. Hu, V. S. Hubbard, J. M. Jakicic, R. F. Kushner, C. M. Loria, B. E. Millen, C. A. Nonas, F. X. Pi-Sunyer, J. Stevens, V. J. Stevens, T. A. Wadden, B. M. Wolfe, and S. Z. Yanovski. 2014. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. Circulation 129(25 Suppl 2):S102–S138.
JHU (John Hopkins University). 2019. Homewood Community Partners Initiative. https://president.jhu.edu/anchor-initiatives/homewood-community-partners-initiative (accessed February 8, 2019).
Kangovi, S., K. Kellom, C. Sha, S. Johnson, C. Chanton, T. Carter, J. A. Long, and D. Grande. 2015. Perceptions of high-risk patients and their providers on the patient-centered medical home. Journal of Ambulatory Care Management 38(2):134–143.
Kangovi, S., N. M. Mitra, L. Norton, R. Harte, X. Zhao, T. Carter, D. Grande, and J. A. Long. 2018. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: A randomized clinical trial. JAMA Internal Medicine 178(12):1635–1643.
Knowles, M. 2018. Henry Ford Health partners with SPLT, Lyft to get patients to appointment. https://www.beckershospitalreview.com/patient-flow/henry-ford-health-partnerswith-splt-lyft-to-get-patients-to-appointments.html (accessed February 8, 2019).
Ku, L., and G. Flores. 2005. Pay now or pay later: Providing interpreter services in health care. Health Affairs (Millwood) 24(2):435–444.
Levinson, W., R. Gorawara-Bhat, and J. Lamb. 2000. A study of patient clues and physician responses in primary care and surgical setting. JAMA 284(8):1021–1027.
Lewis, J. H., K. Whelihan, I. Navarro, and K. R. Boyle. 2016. Community health center provider ability to identify, treat, and account for the social determinants of health: A card study. BMC Family Practice 17:121.
Lindau, S. T., J. Makelarski, E. Abramsohn, D. G. Beiser, V. Escamilla, J. Jerome, D. Johnson, A. N. Kho, K. K. Lee, T. Long, and D. C. Miller. 2016. CommunityRx: A population health improvement innovation that connects clinics to communities. Health Affairs (Millwood) 35(11):2020–2029.
Long, P., M. Abrams, A. Milstein, G. Anderson, K. Lewis Apton, M. Lund Dahlberg, and D. Whicher (eds.). 2017. Effective care for high-need patients: Opportunities for improving outcomes, value, and health. Washington, DC: National Academy of Medicine.
Lukens, E. P., and W. R. McFarlane. 2004. Psychoeducation as evidence-based practice: Considerations for practice, research, and policy. Brief Treatment and Crisis Intervention 4(3):205–225.
Martin, J., A. Martin, C. Schultz, and M. Sandel. 2015. Embedding civil legal aid services in care for high-utilizing patients using medical–legal partnership. Health Affairs blog. https://www.healthaffairs.org/do/10.1377/hblog20150422.047143/full (accessed May 26, 2019).
Martinez, M. 2018. Ford partners with Beaumont Health on medical transport service. https://www.crainsdetroit.com/article/20180418/news/658481/ford-partners-with-beaumont-health-on-medical-transport-service (accessed February 8, 2019).
MassHealth. 2018a. MassHealthaccountable care organizations (ACOs). https://massdocs-digital-mass-gov.s3.amazonaws.com/s3fs-public/2018/MassHealth%2520ACO%2520One-Pager_0.pdf?HQAkdYxhMJTUv2ZGcn9IODj0Dm72uVJV (accessed May 26, 2019).
MassHealth. 2018b. MassHealth flexible services program. https://www.mass.gov/files/documents/2018/11/14/MassHealth%20Flexible%20Services%20One%20Pager.pdf (accessed May 26, 2019).
Mays, G. P., C. B. Mamaril, and L. R. Timsina. 2016. Preventable death rates fell where communities expanded population health activities through multisector networks. Health Affairs (Millwood) 35(11):2005–2013.
McGinnis, T., M. Crawford, and S. A. Somers. 2014. A state policy framework for integrating health and social services. Issue Brief (Commonwealth Fund) 14:1–9.
Miller, W. R., and S. Rollnick. 2012. Motivational interviewing: Helping people change, 3rd ed. New York: Guilford Press.
NASDOH (National Alliance to Impact the Social Determinants of Health). 2019. Who we are. http://www.nasdoh.org (accessed March 25, 2019).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Systems practices for the care of socially at-risk populations. Washington, DC: The National Academies Press.
Navathe, A. S., F. Zhong, V. J. Lei, F. Y. Chang, M. Sordo, M. Topaz, S. B. Navathe, R. A. Rocha, and L. Zhou. 2018. Hospital readmission and social risk factors identified from physician notes. Health Services Research 53(2):1110–1136.
NEJM Catalyst. 2017. What is patient-centered care? January 1. https://catalyst.nejm.org/what-is-patient-centered-care (accessed May 26, 2019).
Ockene, J. K., E. A. Edgerton, S. M. Teutsch, L. N. Marion, T. Miller, J. L. Genevro, C. J. Loveland-Cherry, J. E. Fielding, and P. A. Briss. 2007. Integrating evidence-based clinical and community strategies to improve health. American Journal of Preventative Medicine 32(3):244–252.
Palakshappa, D., S. Doupnik, A. Vasan, S. Khan, L. Seifu, C. Feudtner, and A. G. Fiks. 2017. Suburban families’ experience with food insecurity screening in primary care practices. Pediatrics 140(1):e20170320.
Plough, A. L. 2015. Measuring what matters: Introducing a new action framework. Robert Wood Johnson Foundation Culture of Health Blog. https://www.rwjf.org/en/blog/2015/11/measuring_what_matte.html (accessed May 26, 2019).
Podymow, T., and J. Turnbull. 2013. Management of chronic kidney disease and dialysis in homeless persons. Kidney International Supplements (2011) 3(2):230–235.
Primm, B. J., L. Perez, G. C. Dennis, L. Benjamin, H. W. Clark, K. Keough, W. D. Leak, R. Payne, D. Smith, and L. W. Sullivan. 2004. Managing pain: The challenge in underserved populations: Appropriate use versus abuse and diversion. Journal of the National Medical Assocation 96(9):1152–1161.
Repper, J., and T. Carter. 2011. A review of the literature on peer support in mental health services. Journal of Mental Health 20(4):392–411.
Rizzo, V. M., and J. M. Rowe. 2016. Studies of the cost-effectiveness of social work services in aging: An updated review of the literature. Research on Social Work Practice 26(6):609–621.
Rizzo, V. M., J. M. Rowe, G. Shier Kricke, K. Krajci, and R. Golden. 2016. AIMS: A care coordination model to improve patient health outcomes. Health & Social Work 41(3):191–195.
Rowe, J., V. Rizzo, D. Guthrie, M. Vail, S. Kang, and R. Golden. 2019. The electronic health record: Documenting the unique contributions of social workers. Health & Social Work 44(2):123–128. doi: 10.1093/hsw/hlz006.
Rowe, J., V. Rizzo, S. Kang, R. Kukowski, M. Newman, B. Ewald, and R. Golden. In press. Time contribution of social workers in care management: Value for older adults. Professional Case Management.
RUMC (Rush University Medical Center). 2017. Rush to make $6 million in impact investments. https://www.rush.edu/news/press-releases/rush-makes-first-impact-investment?mc_cid=2f88162828&mc_eid=98430b86a6 (accessed April 12, 2019).
Salzer, M., E. Schwenk, and E. Brusilovskiy. 2010. Certified peer specialist roles and activities: Results from a national survey Psychiatric Services 61(5):520–523.
Sambare, T., L. Uhler, and K. J. Bozic. 2017. Shared decision making: Time to get personal. NEJM Catalyst, October 12. https://catalyst.nejm.org/shared-decision-making (accessed April 10, 2019).
Schoenthaler, A., G. J. Knafl, K. Fiscella, and G. Ogedegbe. 2017. Addressing the social needs of hypertensive patients: The role of patient–provider communication as a predictor of medication adherence. Circulation: Cardiovascular Quality and Outcomes 10(9):e003659.
Schrage, D. 2018. Building partnerships with primary care to become a hub for service delivery for older adults in our community. Aging and Disability Business Institute blog, June 28. https://www.aginganddisabilitybusinessinstitute.org/building-partnerships-with-primary-care-to-become-a-hub-for-service-delivery-for-older-adults-in-our-community (accessed May 26, 2019).
Seligman, H. K., A. F. Bolger, D. Guzman, A. Lopez, and K. Bibbins-Domingo. 2014. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Affairs (Millwood) 33(1):116–123.
Stanhope, V., and S. Straussner. 2017. Social work and integrated health care. New York: Oxford University Press.
Steiner, J. F., J. L. Adams, D. Clausen, K. M. Clift, A. Millan, C. L. Nau, D. Roblin, J. A. Schmittdiel, and E. B. Schroeder. 2018. Predictive Models for Social Determinants of Health in KP Members and Communities: An Issue Brief from Kaiser Permanente’s Social Needs Network for Evaluation and Translation (SONNET). Kaiser Permanente SONNET and Kaiser Permanente Community Health, September 2018.
Stone, N. J., J. G. Robinson, A. H. Lichtenstein, C. N. Bairey Merz, C. B. Blum, R. H. Eckel, A. C. Goldberg, D. Gordon, D. Levy, D. M. Lloyd-Jones, P. McBride, J. S. Schwartz, S. T. Shero, S. C. Smith, Jr., K. Watson, P. W. Wilson, K. M. Eddleman, N. M. Jarrett, K. LaBresh, L. Nevo, J. Wnek, J. L. Anderson, J. L. Halperin, N. M. Albert, B. Bozkurt, R. G. Brindis, L. H. Curtis, D. DeMets, J. S. Hochman, R. J. Kovacs, E. M. Ohman, S. J. Pressler, F. W. Sellke, W. K. Shen, S. C. Smith, Jr., G. F. Tomaselli, and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129(25 Suppl 2):S1–S45.
Swavely, D., V. Whyte, J. F. Steiner, and S. L. Freeman. 2018. Complexities of addressing food insecurity in an urban population. Population Health Management 22(4):300–307.
Tong, S. T., W. R. Liaw, P. Lail Kashiri, J. Pecsok, J. Rozman, A. Bazemore, and A. H. Kirst. 2018. Clinician experiences with screening for social needs in primary care. Journal of the American Board of Family Medicine 31(3):351–363.
Torres, J. M., J. Lawlor, J. D. Colvin, M. R. Sills, J. L. Bettenhausen, A. Davidson, G. J. Cutler, M. Hall, and L. M. Gottlieb. 2017. ICD social codes: An underutilized resource for tracking social needs. Medical Care 55(9):810–816.
Towe, V. L., L. Leviton, A. Chandra, J. C. Sloan, M. Tait, and T. Orleans. 2016. Cross-sector collaborations and partnerships: Essential ingredients to help shape health and wellbeing. Health Affairs (Millwood) 35(11):1964–1969.
Ubhayakar, S., M. Capeless, R. Owens, K. Snorrason, and D. Zuckerman. 2017. Anchor Mission playbook. Chicago: Rush University Medical Center. https://www.rush.edu/sites/default/files/anchor-mission-playbook.pdf (accessed May 26, 2019).
UCSF (University of California, San Francisco). 2019. SIREN: Social Needs Screening Tools Comparison Table (Pediatric Settings). http://sirenetwork.ucsf.edu/tools-resources/mmi/screening-tools-comparison/peds (accessed May 10, 2019).
UnitedHealth Group. 2013. UnitedHealth Group, Minnesota Equity Fund, and community leaders celebrate opening of affordable-housing community in Ramsey. November 14. https://www.unitedhealthgroup.com/newsroom/2013/1114mnaffordablehousing.html (accessed February 8, 2019).
VA (U.S. Department of Veterans Affairs). 2019. VA research on homelessness. https://www.research.va.gov/topics/homelessness.cfm (accessed April 12, 2019).
Vickery, K. D., N. D. Shippee, J. Menk, R. Owen, D. M. Vock, P. Bodurtha, D. Soderlund, R. A. Hayward, M. M. Davis, J. Connett, and M. Linzer. 2018. Integrated, accountable care for Medicaid expansion enrollees: A comparative evaluation of Hennepin Health. Medical Care Research and Review, May 1 [Epub ahead of print].
Waite, R. 2018. Synergy: Bridging the gap between intentionality and actuality: Building resilience and wellbeing through partnership, courage, connection and compassion. Presentation to the Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation’s Health, September 24, 2018, Washington, DC.
Wasserman, M., M. R. Renfrew, A. R. Green, L. Lopez, A. Tan-McGrory, C. Brach, and J. R. Betancourt. 2014. Identifying and preventing medical errors in patients with limited English proficiency: Key findings and tools for the field. Journal of Healthcare Quality 36(3):5–16.
Weiner, S., and A. Schwartz. 2016. Listening for what matters: Avoiding contextual errors in health care. New York: Oxford University Press.
Weiner, S. J., A. Schwartz, F. Weaver, J. Goldberg, R. Yudkowsky, G. Sharma, A. Binns-Calvey, B. Preyss, M. M. Schapira, S. D. Persell, E. Jacobs, and R. I. Abrams. 2010. Contextual errors and failures in individualizing patient care. Annals of Internal Medicine 153(2):69–75.


























