5
Regulations and Guidelines on Legionella Control in Water Systems
In the United States, management of Legionella in water systems occurs on an ad hoc basis, spanning from regulations that require some buildings to have water management plans that include monitoring of water samples for Legionella along with treatment, to no requirements at all. In between exists a range of codes, standards, and guidance documents that have been sporadically adopted and typically target some of the high-risk zones for Legionella growth. Contributing to this widespread inconsistency in approaches to managing Legionella is the lack of any federal law that targets Legionella contamination of water supplies and building water systems as sources to be controlled.
This chapter begins by describing why the Safe Drinking Water Act does not provide any substantial control of Legionella in water systems. It then describes the many regulations, directives, codes, and guidance documents that can affect whether Legionella management occurs in the United States and the resulting significant lack of coverage. The chapter also describes the approach Europe and other countries have taken to manage Legionella, where stricter regulations have been imposed, and discusses how effective the regulations have been to date. For both the national and international regulations or guidance, this chapter describes the regulation, the control methods advocated, whether there is a Legionella monitoring requirement (and if so, whether it is based on percentage positive or concentration), and demonstrated effects of the guidance or regulations on Legionnaires’ disease rates or results of environmental sampling for Legionella. Finally, the chapter’s conclusions and recommendations suggest how the universe of approaches in the United States can be improved upon to better protect the public from exposure to Legionella.
LACK OF FEDERAL LAWS AND REGULATIONS PERTINENT TO LEGIONELLA
The Safe Drinking Water Act (SDWA) was originally passed by the U.S. Congress in 1974 to protect public health by regulating the nation’s public drinking water supplies. The law was amended in 1986 and 1996 and requires actions by the U.S. Environmental Protection Agency (EPA) to protect drinking water and its sources—rivers, lakes, reservoirs, springs,
and groundwater. (The SDWA does not regulate private wells or systems that serve fewer than 25 individuals.) Congress directed EPA to address Legionella through the development of a treatment technique requirement, which is used when monitoring for the contaminant is deemed infeasible or unreliable. In 1989, EPA enacted the Surface Water Treatment Rule (SWTR), which requires public water systems using a surface water supply, or a groundwater supply under the direct influence of surface water, to filter and disinfect the water (the latter of which is meant to control microbial contamination including Legionella). The SWTR requires disinfectant residual to be monitored in the distribution system and at the entry point to the distribution system. The disinfectant level must be at least 0.2 milligrams per liter (mg/L) at the point of entry and detectable in at least 95 percent of samples collected within the distribution system. Public water systems must maintain a residual disinfectant level of less than 4.0 mg/L as a running annual average within the distribution system, as outlined in the Stage 1 Disinfectant/Disinfection By-Product Rule. The SWTR established a Maximum Contaminant Level Goal (a non-enforceable guideline) of zero Legionella organisms in drinking water. This scenario of having no Legionella present in a drinking water system is consistent with the Centers for Disease Control and Prevention’s (CDC) position that there is no known safe level of Legionella.1 However, potable water supplies are not sterile, and Legionella exists in distributed water at some non-zero frequency of detection (LeChevallier, 2019a,b).
The SWTR has been effective for controlling enteric organisms, such as norovirus, Giardia, and Cryptosporidium, using a multiple-barrier approach at the treatment plant. These pathogens are reduced via filtration and can be inactivated via disinfection given the correct disinfectant and contact time (e.g., Cryptosporidium is resistant to chlorination but can be inactivated with ozone or ultraviolet [UV] light). These enteric viruses and protozoa do not multiply in the distribution system or in premise plumbing. Unfortunately, these principles do not extend to Legionella and some other environmental pathogens, which can grow in the pipe network after treatment. Hence, even a few cells that enter the distribution system can seed plumbing downstream. As discussed in Chapter 4, municipal water systems are not thought to be a major source of Legionella because tap water suitable for potable consumption is disinfected and is usually below the optimum temperature for growth of Legionella. However, low levels of Legionella may break through treatment barriers when the microbes are entrapped in the cysts of free-living amoebae or inside protozoa hosts where they are protected from disinfection (Dupuy et al., 2011). Legionella can also grow in oligotrophic environments where the disinfectant residual has declined and biofilms have developed (LeChevallier, 2019b).
Although there are many reports of Legionella proliferation in building water systems (see Chapter 3), there are relatively few monitoring studies of the organism in the distribution systems of U.S. public water supplies. Wang et al. (2012) detected Legionella species (spp.) using quantitative polymerase chain reaction (qPCR) in two chloraminated drinking water distribution systems: Legionella pneumophila was detected in 5.6 percent of samples and Legionella spp. concentrations were reduced 45-fold after tap samples were flushed for three minutes (suggesting that the microbes were primarily in the distal lines of the sampling taps). Lu et al. (2016) examined large volume (90 L) ultrafiltration concentrates from six sites within a distribution system in Georgia and frequently (57 percent) detected Legionella spp. by qPCR at an average concentration of 85 cell equivalents per liter. L. pneumophila was detected at similar frequency (6 percent) as the previous study. Concentrations of
___________________
1 See https://www.cdc.gov/washington/testimony/2013/t20130205.htm.
Legionella spp. were 0.4- to 78-fold higher in the distal sections of the distribution system compared to the entry point, suggesting growth within the distribution system.
Some municipal drinking water systems have summertime water temperatures that are favorable for the growth of Legionella, especially in southern climates where water temperatures may be greater than 30°C. LeChevallier (2019a,b) detected culturable L. pneumophila using the Legiolert™ assay in 15 of 1,087 (1.4 percent) distribution system samples (after flushing the taps for three to five minutes), and all positives occurred when water temperatures were greater than 18°C. Concentrations of L. pneumophila were less than 100 MPN/L except when chlorine residuals were less than 0.1 mg/L. The studies concluded that it was important that water utilities maintain at least a 0.1 mg/L chlorine residual, particularly when water temperatures are greater than 18°C. Riffard et al. (2001) detected Legionella by both culture and molecular methods in warm and cold groundwater, which under the EPA Groundwater Rule (Federal Register, Volume 71, Number 216, 2006) may not be required to be disinfected. Many water supplies have storage tanks that may be prone to high water temperatures where water stratification can prevent mixing and cause subsequent loss of a disinfectant residual. Lu et al. (2015) detected Legionella spp. including L. pneumophila, L. pneumophila serogroup 1, and L. anisa by qPCR in 66.7 percent of municipal drinking water storage tank sediments from 18 sites across the United States. At least one outbreak of Legionnaires’ disease has been associated with a community water system storage tank whose chlorine residuals were low (Cohn et al., 2015).
Despite the water utilities’ maintenance of a distribution system residual, the responsibility for most public water systems ends at the meter or property line; utilities have little control over how building owners maintain their premise plumbing systems. Thus, even the best water quality delivered by a public water supply can degrade once it enters a large building. Large building complexes may contain miles of internal plumbing with features much more favorable for bacterial growth than the main distribution system (NRC, 2006); thus, it is not reasonable to expect that minimal disinfectant residuals in the distribution system persist throughout the premise-plumbing network. Flushing specific devices (e.g., showerheads or faucets) may be practical (albeit time consuming) in such large buildings, but may be impractical for the entire building system and could negate water conservation practices. For small buildings and single-family residences, the plumbing network is much simpler. Although stagnation occurs, intervals of high water use (e.g., showering, bathing, washing clothes) will periodically bring a disinfectant residual into the building. Building owners and homeowners should be made aware of the practices that can reduce disinfectant levels and increase the risk of bacterial growth (such as whole-house filters and water softeners). Thus, a partnership between the building owners (or those maintaining the plumbing system) and the public water utility is vital. Such shared responsibility requires communication, coordination, and close consultation, which is lacking in most cases.
Ironically, the SDWA itself can be a barrier to improving water quality in some building systems. As an added measure to manage Legionella risk, hospitals and long-term care facilities are increasingly using on-site disinfectants. However, the addition of disinfectant to a water system serving 25 or more people deems the building a “consecutive water system” under the SDWA. This means that the building owner can be required to comply with all the requirements that apply to a public water system, including bacteriological monitoring, control of disinfection byproducts, corrosion, and water quality reports to consumers, among others—a substantial burden and cost to building owners. Some have claimed that such an interpretation of the SDWA would make implementation of building water treatment systems untenable, as there would be hundreds of thousands of water systems to regulate. For many systems, the disinfectant boost would be only on the hot-water system
(where Legionella tends to proliferate), which some do not consider a potable supply. EPA, however, defines water “intended for human consumption” as water used for drinking, bathing, showering, hand washing, food preparation, dishwashing and maintaining oral hygiene (40 Code of Federal Regulations [CFR] §141.801 and 63 FR 41940, Aug. 5, 1998), which clearly encompasses hot-water systems.
A provision in the SWDA (40 CFR §141.29) allows states to combine consecutive systems for monitoring and compliance purposes. This provision could substantially reduce the transactional complexity of implementing treatment in building water systems. Yet EPA has provided no guidance on this provision, and there are no examples of any state using it. At the current time, buildings that have installed some type of secondary control for Legionella protection can technically be regulated as public water supplies; in practice, whether they are depends on the intensity of enforcement by state environmental and public health agencies.
Given the lack of concrete requirements stemming from the SDWA and the limited jurisdiction of water utilities responsibility, it can be concluded that the SDWA is not protective of the end user with respect to Legionella contamination. Water leaving drinking water distribution systems is not intended to be, nor is it sterile, and Legionella spp. will be found in building water systems if looked for (e.g., Donohue et al., 2019).
STATE AND LOCAL REGULATIONS AND OTHER ENFORCEABLE POLICIES
Despite the absence of federal regulations or laws that could broadly control the presence of Legionella in water systems, there are local and state regulations that attempt to do just that. Likewise, agencies of the federal government have certain enforceable policies that affect buildings under their control. This section discusses the policies of the U.S. Department of Veterans Affairs and the Centers for Medicare & Medicaid Services (CMS), as well as New York City and State regulations for Legionella control in cooling towers and in certain healthcare facilities. Plumbing and building codes can also significantly impact control of Legionella amplification and transmission in buildings and can be widely enforced, but only at certain times during the life of a building.
Department of Veterans Affairs Directive 1061
Veterans Health Administration (VHA) Department of Veterans Affairs Directive 1061 establishes policy for the prevention and control of healthcare-associated Legionnaires’ disease in VHA-owned buildings in which patients, residents, or visitors stay overnight (DVA, 2014a). Included are 170 medical centers that provide acute care, 134 community living centers, and 48 domiciliaries. The 2014 policy is premised on the notion that healthcare-associated Legionnaires’ disease is most likely caused by the building’s water systems, particularly the hot-water system. VHA follows the CDC definitions for “definite” and “possible” healthcare-associated Legionnaires’ disease described previously (see p.100). The 2014 Directive replaces VHA policies that took effect in 2008, 2009, and 2012.
The Directive outlines a comprehensive approach to Legionella management, similar to some of the U.S. guidance documents and standards discussed later in this chapter, as well as several European regulations. The VHA approach consists of assessing risks, monitoring water quality, and implementing commensurate engineering controls to limit the growth of Legionella. Also included is monitoring of implemented controls, validating that the control measures are effective at inhibiting Legionella growth, and modifying measures as necessary. The Directive relies primarily on temperature control and biocides to control Legionella amplification in building water systems.
The preamble to the Directive sets up the tradeoff between temperature control of Legionella and scalding. Legionella are killed at temperatures greater than 50°C (124°F), but at temperatures greater than 110°F people are at risk of scalding. Hence, the directive does not require 50°C to be maintained in the distal parts of the hot-water system. Although this tradeoff complicates Legionella control in the VHA system, it was thought necessary because of its elderly and vulnerable patient population. The cold-water system is not thought to support Legionella growth, but it could if piped water temperatures remain greater than 25°C for several weeks.
The Directive is structured around the various responsibilities of many people within VHA who will implement it. In particular, the director of every medical facility must establish a multi-disciplinary Facility Water Safety Committee to be chaired by the medical facility associate director and to include representatives from engineering and facilities management, infectious diseases, infection prevention and control, pathology and laboratory medicine, hemodialysis (if performed on site), safety and industrial hygiene, and occupational health. The facility directors must ensure that each building subject to the Directive has a written Legionnaires’ disease prevention plan in compliance with the Directive. This plan must include:
- Schematics of the building water systems (hot and cold) that show how water is distributed, circulated, stored, heated and cooled, treated, and monitored.
- A risk assessment of the building for healthcare-associated Legionnaires’ disease. This is an annual evaluation of factors that may indicate increased risk, such as patient population risk factors, presence of building units associated with increased risk (e.g., transplant units), past cases of healthcare-associated Legionnaires’ disease, and past positive environmental test results.
- Identification of water system management points for the building’s potable water system(s), where monitoring and controls can be implemented to prevent the growth of Legionella and prevent scald injury.
- Establishment of engineering control strategies including control limits, a monitoring schedule, and a dead-leg elimination and prevention plan.
- Documentation of water quality monitoring for control measures, including process flow diagrams of the different control strategies, and each building’s hot- and cold-water plumbing systems.
- Validation that the control measures are effectively inhibiting Legionella growth, which involves monitoring for both Legionella and Legionnaires’ disease.
The engineering controls discussed in the Directive are more expansive than in the 2009 directive and rely primarily on temperature control supported by biocide use. The particular temperature requirements are that hot-water storage tanks must be maintained at a minimum of 140°F (60°C), instantaneous and semi-instantaneous heat exchangers must be at 130°F (54.4°C), and water in the potable hot-water system piping must be no less than 124°F (51.1°C). To avoid scalding, the water at outlets must not exceed 110°F (43.3°C), so thermal mixing valves must be used (as discussed in Appendix B of the Directive). Biocide use is considered optional, but if used, monitoring of the residual is required in various locations. Their accompanying Plumbing Design Manual (DVA, 2014b) better explains all the engineering controls. When a case of Legionnaires’ disease is found at a facility, then emergency remediation is needed, which may include thermal eradication or shock chlorination.
Validation of the control measures requires both monitoring for Legionnaires’ disease and environmental monitoring of Legionella. The environmental monitoring consists of quarterly testing of Legionella in the hot- and cold-water systems (at least ten
outlets each per building). The facility can choose to test additional areas and to take swab samples. If samples are positive, then additional testing of that outlet and nearby outlets and remediation are required. Depending on where positive hits occur, the entire building water system may require remediation. Notably, any amount of Legionella detected is considered positive and requires action (although Legionella concentrations are recorded).
Clinical testing of pneumonia patients at VHA facilities for Legionnaires’ disease uses both the urine antigen test (UAT) and culture methods, especially if there are environmental samples that test positive for Legionella. When a definite healthcare-associated case of Legionnaires’ disease is found at a VHA facility, remediation of potentially implicated water systems is required followed by environmental testing to confirm remediation success. Possible healthcare-associated cases of Legionnaires’ disease trigger a slightly less heightened response that may involve environmental testing and remediation. Investigation of environmental sources of definite or possible healthcare-associated cases can go beyond the building premise plumbing to other systems. After publication of the Directive in 2014, to oversee the program implementation VHA staff began to collect clinical and environmental data and performed site visits as needed (Ambrose et al., 2019). Among many of the challenges observed was how difficult it is to maintain hot-water temperatures and biocide residuals at end points, particularly in large water storage tanks. It also became apparent that diagnosis of Legionnaires’ disease relied primarily on use of only the UAT instead of both the UAT and clinical culture. Ambrose et al. also noted a lack of habitual follow-up on optimizing implementation of engineering controls.
Despite these challenges and others, an analysis of the clinical data from the first three years of Directive 1061 implementation was recently published (Gamage et al., 2018). Almost 50,000 UATs were performed for VHA patients during this time period. The highest percentage of positives for the UATs were in the summer months and in the Northeast. Of the total 491 Legionnaires’ disease cases diagnosed in VHA facilities from 2014 to 2016, 67 percent of patients had no VHA exposure, 3 percent had definite VHA exposure, and 31 percent had “possible” VHA exposure (most of these cases were outpatient, making exposure difficult to attribute to a particular source). Most of the “definite” VHA exposure patients were in long-term care, which is a high-risk healthcare setting. According to Gamage et al. (2018), the total and the non-VHA-associated Legionnaires’ disease rates increased from 2014 to 2016. This was true both when calculating the number of cases either per total number of VHA enrollees or per number of VA enrollees who used the system. These cases were thought to be community-acquired Legionnaires’ disease. In contrast, the rate of VHA-associated cases of Legionnaires’ disease with overnight exposure decreased from 2014 to 2016. While it cannot be proven that implementation of the 1061 Directive was the cause for this decrease, it did occur over the time period of implementation of the Directive.
The environmental data collected from 2014 to 2016 are not yet published but were made available on a preliminary basis during a presentation to the Committee on October 22, 2018, and at a subsequent conference (Gamage and Roselle, 2018, 2019). Included are Legionella, biocide, temperature, and pH data collected quarterly from at least ten hot- and ten cold-water samples. In fiscal years 2015 to 2017, almost 150,000 samples were recorded from routine quarterly testing representing data from 790 buildings. Forty-four (44) percent of the 361 buildings with three full years of data had no detection of Legionella. In fiscal year 2015, Legionella was detected in less than 8 percent of the samples, and the percentage of positive Legionella samples decreased significantly over the three-year period (fiscal years 2015 to 2017).
These clinical and environmental data sets being collected by the VHA are unique in their number of sites and their broad scope. Their comprehensive analysis offers enormous potential for understanding the effectiveness of measures required by the Directive to control Legionella contamination of water systems and to monitor risk of Legionnaires’ disease for individuals.
Centers for Medicare & Medicaid Services Memorandum
CMS has regulatory authority over hospitals, critical access hospitals, and long-term care facilities that receive Medicare or Medicaid funds. The pertinent regulations include 42 CFR §482.42 for hospitals, which states: “The hospital must provide a sanitary environment to avoid sources and transmission of infections and communicable diseases. There must be an active program for the prevention, control, and investigation of infections and communicable diseases.” Similarly, 42 CFR §483.80 for skilled nursing facilities and nursing facilities states: “The facility must establish and maintain an infection prevention and control program designed to provide a safe, sanitary, and comfortable environment and to help prevent the development and transmission of communicable diseases and infections.” Finally, 42 CFR §485.635(a)(3)(vi) for critical access hospitals states that policies must include “a system for identifying, reporting, investigating, and controlling infections and communicable diseases of patients and personnel.”
On June 2, 2017, CMS wrote a directive that requires Medicare-certified healthcare facilities to have water management policies and procedures to reduce the risk in building water systems of growth and spread of Legionella and other pathogens (e.g., Pseudomonas, Acinetobacter, Burkholderia, Stenotrophomonas, nontuberculous mycobacteria, fungi) (CMS, 2017). The directive endorsed the American Society of Heating, Refrigerating and Air-Conditioning Engineers’ (ASHRAE) 188 standard and mentioned the CDC (2017) tool kit to aid hospitals and other facilities in implementing the ASHRAE standard. Quoting from the memo: “Healthcare facilities are expected to comply with CMS requirements to protect the health and safety of its patients. Those facilities unable to demonstrate measures to minimize the risk of Legionnaires’ disease are at risk of citation for non-compliance with the CMS Conditions of Participation. Accrediting organizations will be surveying healthcare facilities deemed to participate in Medicare for compliance with the requirements listed in this memorandum, as well, and will cite non-compliance accordingly.” In accordance with ASHRAE 188, the CMS memo does not explicitly require hospitals and nursing homes to conduct monitoring of Legionella within facilities.
In the United States more than 15,000 nursing homes and 4,784 hospitals are registered with Medicare.2 These numbers do not represent individual buildings because one hospital can have multiple buildings associated with it. These numbers, however, are similar to those cited in Circle of Blue (2018), which says that the CMS memo applies to 15,688 nursing homes and 6,862 hospitals, which includes children’s care, psychiatric, and rehabilitation centers. According to the Circle of Blue report from December 9, 2018, it is too early to know whether hospitals are complying with the CMS memo. Many of the larger hospitals that receive Medicare and Medicaid reimbursements independently instituted Legionella management in their buildings years ago. Given that nursing homes are surveyed for compliance annually and hospitals are surveyed only every three years, it may take time for CMS to obtain enough data to establish the level of compliance. CMS has yet to announce how many of the compliance surveys completed since the memo’s publication in 2017 found inadequate Legionella management plans.
___________________
2 See data.medicare.gov.
Given its brevity and reliance on ASHRAE 188, the CMS memo does not provide any specifics; for example, it does not indicate the required temperatures for building hot-water systems (unlike the VHA Directive 1061, which is very prescriptive, as detailed above). However, CMS defines “immediate jeopardy” with respect to scalding as “access to hot water of sufficient temperature to cause tissue injury” (CMS, 2014). This vague definition has been interpreted differently by states, from South Dakota allowing an operating hot-water temperature of 125°F (52°C) to other states that have defined immediate jeopardy as 105°F (40.5°C). CMS could have a rapid, profound impact on Legionella management in facilities that receive Medicare and Medicaid reimbursements if it specified that immediate jeopardy is not reached until hot-water temperatures are greater than 125°F (52°C) (see Table 4-3).
New York City and New York State Cooling Tower Regulations
The first regulation in the United States to require registering and monitoring cooling towers for Legionella was enacted in 2005 in Garland, Texas, for cooling towers associated with multifamily housing; it was later revised to include hotels and places of accommodation (Whitney et al., 2017). The ordinance was simple and implemented at low cost to the health department, resulting in a decrease in the number of contaminated cooling towers over time. All testing was required to be independent of those responsible for maintenance.
Ten years later, New York City (NYC) passed similar legislation following recent outbreaks of Legionnaires’ disease caused by cooling towers in the city. Local Law 77 went into effect in 2015, with the New York City Department of Health and Mental Hygiene implementing the law. New York State followed by creating Title 10 Part 4 of the New York Codes of Rules and Regulations (10 NYCRR Part 4 “Protection against Legionella”). Final adoption of the New York State regulations occurred in July 2016. The state’s regulations apply statewide, including in NYC, such that there is overlap between the city and state regulations.
The NYC and New York State regulations require cooling tower owners to take the following actions:
- Register existing and new cooling towers with the city and state.
- Sample each cooling tower for Legionella every 90 days.3 Notify the city within 24 hours if Legionella culture results are greater than 106 CFU/L; the state every 90 days while the cooling tower is in operation; and the local health department within 24 hours for any result greater than 106 CFU/L.
- Perform daily chemical treatment of system water.
- Monitor temperature, pH, conductivity, and biocides at least three times per week. Microbial monitoring (heterotrophic plate counts) must be performed weekly, wetted surfaces are visually inspected weekly, and chemical treatment equipment is also checked.
- Inspect the cooling towers every 90 days and obtain annual certification, by a qualified person.
- Develop and follow maintenance program and plan in line with the ASHRAE 188 standard.
___________________
3 All monitoring thresholds in this chapter are expressed in CFU/L for consistency. However, this is not meant to imply that all samples are 1 L in volume. Sampling protocols differ between jurisdictions.
- There are various other requirements for drift eliminators, materials, cleaning, and documentation.
- If an owner does not register, have a maintenance program and plan, obtain certification, disinfect, perform, or obtain culture sampling and analysis, or inspect a cooling tower within the required time and manner, New York State or the local health department may determine that the situation constitutes a nuisance and may take action, as authorized by law. New York State or the local health department may also take any other action authorized by law, including imposing any and all applicable civil and criminal penalties.
More details on reporting, enforcement, penalties, and updates can be found in the official documentation (NYC, 2016a,b).
As of April 2019, approximately 6,100 cooling towers were registered in NYC and about 11,000 in New York State (including NYC). Currently, results from the NYC Legionella sampling are not publicly available, but this will change in October 2019. Cooling tower data for New York State are publicly available.4 Both the city and state programs have seen progress in implementation and adherence to the existing regulations. For New York State, rates of cooling tower compliance with current regulations increased from 30 percent in 2017 to 67 percent in 2018. In NYC, the cooling tower registry has been invaluable in providing real-time information for Legionnaires’ disease cluster response. Promptly locating cooling towers and having a history of operations and maintenance records has provided valuable information for identifying potential sources and evaluating risk. Additional benefits of the regulations include:
- An increase in the proportion of cooling tower systems that have a maintenance program and plan;
- An increase in the proportion of cooling tower systems that have water treatment including biocide, anti-corrosion, and anti-scaling treatment;
- An increase in the proportion of cooling tower systems that document and maintain operational records; and
- An increase in Legionella and bacterial monitoring during cooling tower operation.
The proportion of cooling towers testing positive for Legionella in samples collected by the department is typically less than 30 percent and has remained relatively stable in the first two years of implementation of the regulations.
New York State Healthcare Facility Requirements for Legionella
As of July 2016, all general hospitals and residential healthcare facilities in New York State are required to perform an environmental assessment, prepare and implement a sampling and management plan to sample their potable water systems for Legionella, and institute control measures in the event of a Legionella exceedance. The New York State regulations apply to buildings of general hospitals that provide in-patient services or buildings of residential healthcare facilities that provide a “health-related service,” such as lodging, board, and physical care. The regulation does not apply to administrative buildings of such
___________________
4 See https://health.data.ny.gov/Health/Registered-Cooling-Towers-Beginning-August-2015/24a4-muw7.
facilities, general hospital buildings that only provide outpatient services, or to diagnostic and treatment centers providing only outpatient services.
All covered facilities must perform an environmental assessment of the facility using a specified environmental assessment form prior to providing services, and when specified by the New York State Department of Health (NYS DOH), such as when there are suspected or actual cases of legionellosis, after certain construction and repairs, and after expansion and relocation of certain medical units. Furthermore, all covered facilities must adopt and implement a Legionella culture-based sampling and management plan for their potable water systems. New covered facilities must adopt this plan prior to providing services. Legionella culture sampling and analysis must occur at 90-day intervals during the first year of sampling and management plan implementation, and annually thereafter. Portions of any potable water system that serve hematopoietic stem cell transplant or solid organ transplant patients must continue to be sampled and analyzed at intervals not to exceed 90 days. Legionella culture sampling and analysis must also occur in a timeframe determined by the state health department.
All Legionella culture analyses must be performed by a laboratory that is approved to perform such analysis by the New York State Environmental Laboratory Approval Program (ELAP). When 30 percent or more of Legionella culture samples contain Legionella, regardless of species, facilities are required to institute control measures, resample their water system, and notify the NYS DOH. (This 30 percent threshold stems from the Allegheny County guidance mentioned in a subsequent section.) The covered facility must maintain the required environmental assessment and any associated sampling results on the facility premises for at least three years. These records must be made available to the NYS DOH immediately on request. The department may conduct an assessment and/or Legionella culture sampling and analysis of the potable water system at any time. A violation of any provision of the regulation is subject to civil and criminal penalties. Each day that an owner remains in violation of any provision of this Subpart constitutes a separate and distinct violation of each such provision.5 Citations during routine facility inspections are issued by healthcare facility surveyors, who are tasked with implementing the 2017 CMS memo on Legionella prevention in healthcare facilities. NYS DOH reports that letters of non-compliance sent to healthcare facilities have had positive effects (mostly immediate responses and compliance).
Legionella data stemming from this regulation are not currently available on a public platform, nor is direct reporting of culture data to the NYS DOH a requirement of the regulations. NYS DOH is developing measures to evaluate the effectiveness of the regulations, while recognizing that several more years of data will be needed to identify meaningful trends.
Plumbing Codes
Plumbing codes dictate almost every facet of building plumbing design and installation, including insulation, materials used, allowable pipe size and length, allowable volume from a hot-water source to a tap, control of heated water systems including storage and circulation, drain water heat recovery, and commissioning. Building owners have to be in compliance with plumbing codes when a building is being built or renovated; hence, codes are mainly enforceable prior to a certificate of occupancy being signed. Some plumbing codes can be used to partially manage Legionella in building water systems, and those codes are the focus of this section.
___________________
5 See https://www.health.ny.gov/environmental/water/drinking/legionella/hospitals_health_care.htm, https://regs.health.ny.gov/content/subpart-4-2-health-care-facilities.
Plumbing codes can provide a backstop for buildings, such as residences, that would otherwise not fall under any guidance documents or other enforceable policy for Legionella management.
The three main plumbing codes are the International Plumbing Code (ICC, 2018), the Uniform Plumbing Code (IAPMO, 2018a), and the National Standard Plumbing Code (IAPMO, 2018b). Plumbing codes are adopted at the state level but are generally enforced at the county or municipal level by the relevant inspection entity. The International Plumbing Code is revised every three years by the International Code Council (ICC). It has been adopted at the state or local level in 35 states. The Uniform Plumbing Code was developed by the International Association of Plumbing and Mechanical Officials (IAPMO), also on a three-year cycle, and has been adopted in 13 states, mainly in the west and northwest United States including California. The National Standard Plumbing Code was developed by the Plumbing Heating and Cooling Contractors of North America (which was recently purchased by IAPMO) and has been adopted in New Jersey and parts of Maryland and is not discussed further here. It should be noted that in states with state-wide codes, these codes may be modified by local ordinances. For example, California adopts a statewide plumbing code, but in Colorado each jurisdiction (individual cities and counties) can adopt different codes. For all three codes, product manufacturers tend to drive the code change proposals.
Historically, plumbing codes were not written with the goal of managing building water systems for Legionella. In fact, some codes (unintentionally) work against the control of Legionella. For example, pipe-sizing requirements that were set more than 50 years ago remain unchanged, even though plumbing fixture flow rates, flush volumes, and appliance volumes have been reduced every decade since the 1950s. Because there have been significant reductions in average residential water use since the 1980s without concomitant reductions in pipe sizes, household flow rates have been drastically reduced. There are many unintended consequences of having lowered water use in conjunction with oversized pipes. Foremost among them is that hot water takes much longer to arrive at taps. As discussed in Chapter 4, increased water residence times in premise plumbing systems can lead to conditions highly conducive to Legionella growth. A related issue is that plumbing codes were created under the assumption of fixed-orifice devices. Today, however, many devices have pressure-compensating aerators, which provide a constant flow rate to the consumer above 20 psi pressure. The use of such aerators should allow builders to more correctly size pipes, but these corrections have not yet found their way into plumbing codes.
A second plumbing code feature that affects Legionella management is the temperature requirement, particularly in public bathrooms. Since 2006, the International Plumbing Code has stipulated that, for public bathrooms, the temperature of hot water at handwashing stations must be between 85°F (29.4°C) and 110°F (43.3°C)—the definition of tempered water. Hence, the codes require delivery of water in the temperature range optimal for Legionella growth. The 2018 International Plumbing Code defines “hot water” as greater than 110°F (43.3°C), while the Uniform Plumbing Code defines it as 120°F (48.9°C).
To meet the temperature requirements, plumbing codes mandate the use of certain devices, such as thermal mixing valves, to deliver water of various temperatures to various locations in premise plumbing, particularly near end-use points and at emergency stations. The International Plumbing Code also requires thermal mixing valves for every public handwashing sink. As discussed in Chapter 4, these devices tend to fail without warning in a few years, especially when substandard devices are used. The plumbing codes do not require periodic testing of thermal mixing valves. Another device requirement found in plumbing codes is for combination tub and shower valves that deliver cold, warm, or hot water. Often, the highest flow rate that can be achieved with these devices is for the mixed temperature water, not the hot water, leading to oversized pipes.
Material requirements in plumbing codes can affect Legionella management. Both the International Plumbing Code and the Uniform Plumbing Code dictate materials to be used for piping, devices, and joints, among others, with the list of acceptable materials being determined mainly by the manufacturers. To avoid future liability, manufacturers tend to avoid promoting materials that leach compounds. Nevertheless, it would be preferable if the requirements in the plumbing codes were based on robust studies of what materials are more or less favorable to growth of Legionella.
Indeed, to have the greatest positive effect on Legionella management, plumbing code changes would suggest new ways to design plumbing systems before a building is constructed. The main tenet of an ideal code would be to correctly size pipes to reflect lowered water use and measured pressure drops in systems with modern pipe materials and fittings. In addition, builders should be incentivized, perhaps with energy credits, to build compact plumbing cores with no more than ten feet between the hot-water source and fixtures. Another practice to incentivize would be the use of electric tankless water heaters that would require no mixing valves, or the use of heat trace to maintain adequately high temperatures in pipe branches. Finally, the plumbing codes could define tempered water to be between 120°F and 130°F (48.9°C to 54°C), such that water delivered to taps would not be in the range of optimum Legionella growth.
GUIDANCE DOCUMENTS
Many guidance documents that outline steps to manage Legionella in building water systems have appeared over the past five years. The most prominent of these are discussed below, including the ASHRAE 188 standard, guidance from the American Industrial Hygiene Association (AIHA, 2015), National Sanitation Foundation International (NSFI) standard 453, and the guidelines from the Allegheny County Health Department in Pennsylvania.
In general, like the VHA Directive, the major guidance documents take a risk-based approach to managing Legionella in building water systems. To a greater or lesser extent, they each follow the general principles of risk management and require development of a plan or program to mitigate the risk (variously called water safety plans, water management programs, and other terms). Each plan or program typically follows the basic steps shown below (which are similar to those within the VHA Directive):
- Establish a program team.
- Describe each water system.
- Analyze where potential hazards may exist, develop, or propagate.
- Identify control measures and where they should be applied to stay within limits.
- Monitor certain parameters (not necessarily Legionella) to determine whether control measures are working.
- Confirm that the program is being implemented as designed (verification) and that the program effectively controls the hazardous conditions (validation).
- Document everything.
Depending on the guidance document and its developers, certain specifics for managing Legionella in water systems are enhanced or expanded to meet the needs of their organizations. Interestingly, each guidance document is sufficiently vague to permit individual users the flexibility and latitude to address those program aspects either unique or specific to their own buildings or uses. On the other hand, the lack of strong commonality among these documents on the details and specifics of managing Legionella in water systems collectively
creates confusion. In fact, one of the primary drivers for the creation of CDC’s tool kit (CDC, 2017) was to specify how to actually apply the ASHRAE 188 standard. Highlights of each major guidance document and their particular differences are identified below.
Allegheny County Health Department Legionella Guidelines
Guidance documents produced by the Allegheny County Health Department (1993, 1997, 2014) were some of the first to address Legionella in building water systems. These guidance documents state that all facilities should take a risk management approach regarding Legionella in their water systems. A key recommendation is development of a water safety plan, the elements of which are described above. However, there is no requirement in the water safety plan for a program team or for documentation in the Allegheny County Health Department guidance. The guidance specifically outlines different types of control measures, from thermal disinfection to point-of-use filters. Finally, unlike the other guidance documents, this guidance includes a section on managing Legionnaires’ disease in patients.
The Allegheny County Health Department guidance documents are the basis for the 30 percent positivity rule that has permeated many other guidance documents as well as the previously described New York State regulations for healthcare facilities. Best et al. (1983) found that whenever monthly site positivity of environmental testing for Legionella in a large building exceeded 30 percent, cases of Legionnaires’ disease appeared in those months. Furthermore, when positivity fell to 20 percent or less, no cases of disease were observed. The 30 percent value is very controversial, as is noted in the 2014 guidance from Allegheny County. The Committee notes substantial difficulties with using this guidance, including the fact that the analysis has not been repeated and validated elsewhere and it has frequently been applied in situations that lack an adequate number of samples. While it was useful in the 1990s, comprehensive guidance based on Legionella concentration along with the frequency of detection would be more consistent with the available science.
ASHRAE Standard 188 on Legionella in Building Water Systems
The ASHRAE 188 standard (ASHRAE, 2015) is a guidance document for all types of buildings and their water systems, with the exception of residential single-family homes. The core of the standard is for each building to have a water management program that has seven elements, as described in the bulleted list above. For ASHRAE 188, the most important element is the creation of a program team to make decisions about other aspects of the water management program. Notably, ASHRAE 188 does not specify that monitoring of Legionella in the building water system is necessary unless the program team decides that it is. Instead, to manage Legionella occurrence, the focus is on controlling and monitoring certain physicochemical factors (e.g., temperature, disinfectant residual, and maintenance).
ASHRAE 188 considers individual types of water systems, from the potable water system to cooling towers and evaporative condensers, spas, fountains, and aerosol-generating misters. There are some peculiarities for each type of water system, and the standard states that details are given in ASHRAE Guideline 12 (ASHRAE, 2000). The standard also covers requirements for designing building water systems, such as documenting potential hazards in all major water systems, as well as documentation of all the water systems themselves upon installation, including what was built and where, what materials were used, and corresponding manuals. Detailed instructions for commissioning, including flushing and disinfection, have to be provided.
Annexes treat specific issues or building types, such as Annex A for healthcare facilities. This Annex calls for a yearly evaluation of the likelihood of legionellosis in healthcare facilities, which is not mentioned in the main part of the standard. Annex C states that any Legionella testing must be done by accredited laboratories.
CDC Tool Kit
The CDC tool kit (CDC, 2017) was created to help building owners and managers develop and implement a water management program to reduce a building’s risk for growing and spreading Legionella. The tool kit both simplifies and explains ASHRAE 188, and it applies the principles to healthcare facilities. For example, there are a series of questions to be answered to determine whether a particular building is at risk of Legionella contamination, as well as sections that specify how to assemble the program team. There is a useful flow diagram of a building’s water system, which is then used repeatedly throughout the water management program to identify areas that may be susceptible to Legionella growth and to show where control measures will be applied. Examples are given of when a control limit is exceeded and corrective actions are necessary, and what to do if Legionella is found in a building. The tool kit provides further details for healthcare facilities, which are more likely to suffer adverse effects from Legionella contamination.
AIHA Guidance on Legionella in Building Water Systems
AIHA (2015) is a guidance document intended to help building managers anticipate, recognize, evaluate, and control Legionella in buildings. It covers premise plumbing; cooling towers and evaporative condensers; hot tubs, whirlpools, and spas; decorative fountains and water features; humidifiers; the water supply system; and sprinklers, eyewash stations, and safety showers. The guidance differentiates its approach to Legionella management (which comes from the industrial hygiene field) from what is labeled “current health practice” that goes into action only after a case of Legionnaires’ disease has occurred. The guidance describes such “current health practice” as appropriate for diseases transmitted between persons, but ineffective when the environment is the source of the etiologic agent. Hence, AIHA (2015) focuses on identifying sites of Legionella amplification and exposure pathways using measurements of viable Legionella bacteria; it does not endorse sampling surrogates such as disinfectant residual.
Similar to other guidance documents, AIHA (2015) is based on risk assessment, but it tends to be more descriptive. It specifically calls for Legionella samples to be collected (to be assayed via the culture method) from selected water systems on an ongoing basis to determine the effectiveness of control strategies and identify potential hazards. AIHA (2015) recommends that, although PCR techniques can be used as a complementary analysis, they should not replace culture-based methods. Table 5-1, taken from the guidance document, provides levels of Legionella that can be thought of as action levels to compare to routine sampling results. For all water system types (except cooling towers), a measured concentration below 1 CFU/mL (1,000 CFU/L) is considered to be at the detection limit. Between 1 and 10 CFU/mL (1,000 to 10,000 CFU/L), Legionella amplification could be possible. A sample above 10 CFU/mL (10,000 CFU/L) indicates that amplification has occurred, and action needs to be taken (for cooling towers, the document suggests that 100 to 1,000 CFU/mL [105 to 106 CFU/L] is indicative of possible amplification). These values mirror those of the Occupational Safety and Health Administration (OSHA), which used
TABLE 5-1 AIHA Data Interpretation Guidelines
| Sample Source | Non Detectable | Acceptably Low* | Action | Possible Amplification | Action | Indicates Amplification | Action |
|---|---|---|---|---|---|---|---|
| Humidifiers & Misters | < CFU/mL | < CFU/mL | 1 | 1-10 CFU/mL | 2 | >10 CFU/mL | 3 |
| Decorative Fountains and Water Features | < CFU/mL | < CFU/mL | 1 | 1-10 CFU/mL | 2 | >10 CFU/mL | 3 |
| Hot Tubs, Whirlpools and Spas | < CFU/mL | < CFU/mL | 1 | 1-10 CFU/mL | 2 | >10 CFU/mL | 3 |
| Potable Water | < CFU/mL | < CFU/mL | 1 | 10-100 CFU/mL | 2 | >100 CFU/mL | 3 |
| Industrial Working Flulds | < CFU/mL | < CFU/mL | 1 | 10-100 CFU/mL | 2 | >100 CFU/mL | 3 |
| Cooling Towers & Evaporative Condensers | < CFU/mL | < CFU/mL | 1A | 100-1,000 CFU/mL | 2A | >1,000 CFU/mL | 3A |
* May be limited by Legionella levels in the building source water supply (e.g., municipal water).
NOTES: Action levels (see AIHA, 2015 for complete details): (1) Continue to monitor as per the plan. (2) If no cases of legionellosis, reassess maintenance and treatment plans; make adjustments as necessary. If cases of legionellosis occur, take immediate steps to clean and disinfect the system. Notify appropriate health authorities. (3) Take immediate steps to clean and disinfect the system. Adjust control plan as needed.
SOURCE: AIHA (2015).
to suggest guidelines for Legionella to assess the effectiveness for water system maintenance but no longer does.6
Unlike the other guidance documents, AIHA (2015) discusses side effects of various treatment techniques that should be taken into account. The guidance also provides considerable detail about how to protect workers and building occupants (such as with point-of-use devices) during remediation activities.
NSFI Standard 453 for Cooling Towers
NSFI standard 453 (NSFI, 2017) provides minimum practices for treating, operating, and maintaining cooling towers to avoid Legionella growth. The standard uses the terms program (all the conducted activities) and plan (the documentation of the program) and adheres to the bulleted list of risk management elements discussed previously.
Standard 453 requires treatment of cooling towers with an oxidizing biocide as well as maintenance of pH, corrosion control, scale and deposit control, and conductivity. Startup procedures for cooling towers are outlined, including initial startup and after a system shut-down. Routine inspection, service, and maintenance are outlined, including weekly, quarterly, and when there is an issue. Cycles of concentration are a key operating parameter for cooling towers that need to be monitored, managed, and documented.
Monitoring of biocides is required as part of standard 453, as is testing for heterotrophic plate counts and Legionella. If concentrations of Legionella are less than 10 CFU/mL (10,000 CFU/L), no action is needed. If concentrations are between 10 and 100 CFU/mL (10,000-100,000 CFU/L), then the entire program must be reviewed and on-line remedial treatment is needed. Between 100 and 1,000 CFU/mL (105 to 106 CFU/L), a visual inspection is also required (in addition to the above) to determine whether full draining and repair are required. Greater than 1,000 CFU/mL (106 CFU/L) requires off-line remedial treatment, and the standard describes the conditions for completely shutting down the cooling tower.
___________________
6 See https://www.osha.gov/dts/osta/otm/otm_iii/otm_iii_7.html#app_iii:7_3.
This standard will be superseded by NSFI standard 444, which, when released, will cover all building water systems, not just cooling towers.
REGULATIONS AND POLICIES FROM OTHER COUNTRIES
Although there are no nationwide regulations for Legionella management in the United States, several other countries, notably those in Europe, have enacted regulations meant to manage Legionella in various types of water systems. Some of these mirror documents produced by the World Health Organization (WHO), which advocated that buildings have a water safety plan and monitor temperature, pH, and (for validation purposes only) Legionella (WHO, 2007, 2011)). This section summarizes information gathered by the Committee from representatives of six countries about their Legionella laws, regulations, guidance documents, and codes. Their presentations described the regulations, noted what water systems they apply to, and discussed the extent of compliance with the regulations. Each presenter described the environmental monitoring that must accompany the regulations, including threshold levels above which remedial or preventive action is taken. Finally, they talked about whether the regulations have had an impact on reducing rates of Legionnaires’ disease or environmental concentrations of Legionella. The six countries are Australia, Canada, France, Germany, the Netherlands, and the United Kingdom.
The European Working Group for Legionella Infections (EWGLI) published guidelines for the prevention, control, and investigation of infections caused by Legionella spp. (EWGLI, 2017), but their recommendations have no legal standing. A new European Drinking Water Directive was developed in 2018 (European Commission, 2018), which makes risk assessment in domestic building water systems obligatory. This risk assessment includes risks linked to products and materials in contact with drinking water and monitoring for lead and Legionella. Legionella was included in the directive because (1) it has been found by the WHO to cause the highest health burden of all waterborne pathogens in the European Union (EU) and (2) the European Centre for Disease Prevention and Control recommended regular checks and appropriate control measures to human-made water systems to prevent cases of Legionnaires’ disease at tourist accommodation sites, hospitals, long-term healthcare facilities, or other settings where sizable populations at higher risk may be exposed (ECDC, 2017). How Legionella sampling and analysis should be performed is also defined in the new EU drinking water directive. One-liter samples must be taken at the consumer’s tap without prior flushing and analyzed for culturable Legionella according to ISO 11731 (ISO, 2017). When the culturable Legionella number in a drinking water sample does not comply with 1,000 CFU/L, resampling has to be performed, and new samples have to be screened for L. pneumophila. When L. pneumophila is detected, action has to be taken. If L. pneumophila is not detected during resampling and cultivable Legionella is less than 10,000 CFU/L, no action has to be taken. Each EU member state determines what action their country will take when these action levels are exceeded. After the first vote in the EU parliament, several amendments were suggested, but the expectation is that the new directive will be adopted soon by the EU parliament. EU countries without Legionella regulations will have to comply with the new action levels. Those countries that already have Legionella regulations in place (discussed below) tend to be more strict than the new European directive; as a result, they will not have to modify their regulations.
The Netherlands
Four laws in the Netherlands were revised to include Legionella spp., in each case following an outbreak. For the first Legionella outbreak, in 1999, a hot tub on display in Bovenkarspel was found to be the source of the bacteria, resulting in more than 200 cases of Legionnaires’ disease with 32 fatalities (den Boer et al., 2002). This outbreak led to the addition of regulations to the Drinking Water Act, the Hygiene and Safety Act, and the Safety at Work Act. In 2006, a second outbreak caused by a contaminated cooling tower in Amsterdam led to the creation of new regulations in the Environmental Protection Act. Legionella is the only pathogen in premise plumbing to be a target of Dutch regulations.
The Drinking Water Act regulations apply only to buildings labeled “priority premises” such as hospitals and other healthcare facilities with overnight stays, hotels and other accommodations that house more than five people, truck stops with showers, harbors, and marinas with showers, asylum centers, and prisons. The Act requires that a risk management plan for the building be created, and include such risks as water stagnation, tepid temperature, formation of aerosols, presence of high-risk individuals, past cases of Legionnaires’ disease, whether the building accommodates travelers, whether it is used for temporary events, and lack of proper maintenance. The owner of the building must periodically update the risk management plan. Management plans are generally created by certified consultants and must conform to technical guidelines (e.g., about how, when, and where to sample).
The highest priority control methods discussed in the Act are temperature control, flushing, UV treatment, and filtration. Secondary methods include electrochemical treatment such as copper-silver ionization. Chlorination is a tertiary treatment, although it conflicts with the long-standing Dutch paradigm of not carrying a disinfectant residual in finished water. In terms of temperature control, cold water must be maintained at less than 25°C, while hot water must be hotter than 60°C throughout the hot-water system. The Act requires that buildings be sampled every six months for Legionella spp. using culture methods. If the concentrations are less than 100 CFU/L, no further action is taken. Above 100 CFU/L and especially above 1,000 CFU/L, certain response actions are required such as informing the users of the building, taking appropriate measures to prevent a public health threat, and notifying the Inspectorate. It is noteworthy that these numbers were chosen for practical reasons and are not health-based. The detection limit for the laboratories is 100 CFU/L, and 1,000 CFU/L was a practical number larger than 100 CFU/L.
The Hygiene and Safety Act is similar to the Drinking Water Act, but it applies to swimming and bathing facilities above a certain size and where aerosols are dispersed. It does not apply to hot tubs. As above, a risk management plan is required, and the monitoring requirements are the same as in the Drinking Water Act. Major differences are that certification of consultants is not required, there are no technical guidelines available, and any disinfection method can be used.
The Environmental Protection Act applies to wet cooling towers only. Like the previous two Acts, it requires a risk assessment and management plan that includes treatment and monitoring. Technical guidelines are also available to help guide the creation of such plans. However, no specific treatment is required as long as an effective method is used. Similarly, the monitoring requirements are loose, with no specific threshold above which action must be taken and no recommended frequency of monitoring. This Act does not require that the consultant creating the risk management plan be certified, but the plan must be updated when cooling tower operations change or the surroundings change. The Act requires all cooling towers built after 2010 to be registered; currently, about one-third of all towers are registered.
The Safety at Work Act aims to protect workers from Legionella exposure. As with the other Acts, a risk assessment and management plan is needed. The Act does not require particular treatment methods or monitoring frequency, although it does specify a threshold of 100 CFU/L as measured by culture.
Implementation of the Drinking Water Act regulations has been tracked since 2009 via facilities inspections. The trends suggest that more and more of the facilities are becoming “no risk.” For cooling towers, data from 2011 and 2015 suggest that municipalities are identifying their cooling towers (88 percent) and that a substantial portion of towers are being registered (30 percent). On the other hand, inspections lag behind, with two-thirds of inspectorates not visually inspecting their cooling towers. Less information is available on implementation of the Hygiene and Safety Act and the Safety at Work Act. All of the regulations, except the Safety at Work Act, are supposed to be enforced via inspections, which could then lead to warnings, fines, and facility closure.
There is no information on whether these regulations have affected either rates of Legionnaires’ disease or environmental sampling of Legionella. In the Netherlands in general, Legionnaires’ disease rates are still increasing (they were 3.3/100,000 in 2017—ECDC, 2019), although travel-associated cases seem to have leveled off. Many believe the national data are insufficient to evaluate the impact of the regulations, particularly given the lack of data on both Legionnaires’ disease rates and Legionella concentrations collected at the same location.
Germany
German regulations for Legionella spp. extend drinking water regulations into premise plumbing. In 1987, the German Federal Health Department said that drastic reduction in Legionella concentrations was necessary to reduce infections, further emphasizing that the goal should be “as low as reasonably achievable.” The country’s federal Protection Against Infection Act regulates water for consumption as well as swimming pools and bathing water and all wastewater treatment plants. For drinking water in particular, there is not only the Protection Against Infection Act, but also the EU Drinking Water Directive (discussed previously), a German ordinance on the quality of water for human consumption, and proposals of the German federal Environmental Protection Agency. The Protection Against Infection Act requires a Legionella risk management plan for every large building that has more than 400 liters of hot water or more than three liters of hot water between the water heater and the last tap at the end of the pipe. Healthcare facilities are required to maintain a temperature of 60°C at hot-water heaters and 50°C at distal points of hot-water systems. To facilitate compliance with the regulations, there are at least six technical standards that stem from the Act.
The federal German Emissions Control Act and technical guidance cover every open cooling tower. They have similar requirements for a management plan, monitoring, and concentration thresholds above which action must be taken.
The Protection Against Infection Act also targets Legionella that may stem from the disposal of wastewater, both industrial and municipal. The impetus for its implementation was a 2013 outbreak caused by outflow from a wastewater treatment plant. Specifically, a brewery was disposing of warm (38°C) wastewater, which was found to have high levels of Legionella (107 CFU/L), and the receiving river was contaminated for 12 kilometers downstream of the outfall with some 200,000 CFU/L of Legionella (Maisa et al., 2015). Therefore, it was decreed that wastewater treatment plants must be monitored for Legionella by culture methods. It has now become evident that warm wastewaters from breweries, paper mills, and sugar processing plants can have very high Legionella concentrations.
These regulations require monitoring of environmental samples for Legionella spp. at various locations in a building; measured concentrations must be less than 100 CFU/100mL (1,000 CFU/L). This concentration is called a technical action level and, as in the Netherlands, it is not a health-based number, but rather a value above which certain additional precautions must be taken, including checking the sanitary and technical condition of the drinking water installation in the form of a risk analysis and informing public health agencies.
The regulations are accompanied by many technical guidance documents and rules for planning and construction, much like plumbing and building codes in the United States. Code of Practice W551 (DVGW, 2004) addresses measures to reduce Legionella growth in buildings and is particularly relevant, as it recommends that one keep the volume of stored hot water small, keep the hot water hot and the cold water cold, avoid stagnation, maintain and inspect, rehabilitate, and perform more microbiological examinations. There is also a code for remedying microbial irregularities in drinking water installations (W556, 2015), and one for cleaning and disinfecting drinking water installations (W557, 2012). Guideline 6023 deals with qualifications and staff training. Cooling towers are subject to a Cooling Tower Code of Practice, which has threshold concentrations above which remedial actions are required.
All of Germany has to comply with the regulations, and compliance is high because building owners can be punished by law for not complying. Implementation of the regulations in large cooling towers and most building water systems is now broad, although the implementation is not as widespread for small cooling towers. The sewage regulations are only being enforced in North Rhine Westphalia. In general, the government tries to educate water consumers about Legionella by posting information on every public health department’s website. If monitoring data are above the action level for a large apartment building, the building owner has to inform the occupants. As a result, people have become much more aware of Legionella. There are also guidelines for the homes of immunosuppressed people.
Germany has been trying to determine the impact of its regulations with the LeTriWa (Legionellen in der Trinkwasser) Project conducted in Berlin from 2017 to 2019, which is reviewing outbreak reports and follow-up surveillance. There is no indication that cases of Legionnaires’ disease have decreased since the regulations came into effect. In 2017, the case rate in Germany was 1.6 per 100,000 people (ECDC, 2019). However, the LeTriWa study has shown that since the regulations went into effect, the percentage of buildings that have culturable Legionella has declined from 70 percent to just 10 percent (Exner, 2018). There is also anecdotal evidence that a hospital that had 11 cases of Legionnaires’ disease in 1990 has had no cases since the implementation of controls (Exner, 2018).
England
England’s regulations for Legionella management have evolved from two pages of guidance in 1980 to hundreds of pages today. The primary impetus for creating regulations was the 1985 outbreak of Legionnaires’ disease at Stafford Hospital. Engineering guidance was then developed for cooling towers and evaporative condensers. In 1991, the Health and Safety Commission published the Approved Code and Practice for the Prevention of Legionellosis. In 1998, there was specific guidance for hot- and cold-water systems. In 2000, everything was combined into one guidance called L8, in which there are various levels of documents: laws, regulations, approved codes of practice, and technical guidance.
Much of the guidance stems from the 1974 Health and Safety at Work Act, which aims “to ensure the health and safety of employees and non-employees so far as reasonably practicable.” Although the term “reasonably practicable” is ambiguous, it has held up over the
years because the risks of Legionnaires’ disease are significant and the consequences may be deadly, so high cost is justified. The various UK laws and regulations have many facets in common. The Control of Substances Hazardous to Health regulations have a series of requirements, including a risk assessment and control measures. The Management of Health and Safety at Work regulations also require risk assessment, more planning control, monitoring, and review of preventive measures. The Notification of Cooling Towers and Evaporative Condensers Regulations of 1992 are the only regulations that specifically address Legionella. Cooling towers must also be registered, and more than 90 percent are.
The main L8 regulations have four accompanying guidance documents that cover evaporative cooling systems, hot- and cold-water systems, spas and pools, and other systems. The regulations apply to all systems containing water likely to exceed 20°C for which there is a means of creating and transmitting water droplets that may be inhaled. The building types covered include shops, offices, factories, hospitals, industrial plants, entertainment facilities, and rented properties, among others, but private residences are excluded. Healthcare facilities have a slightly different set of regulations stemming from the Health and Social Care Act of 2008, a new set of regulations, a new Code of Practice, and new technical memos. To maintain their registration, all healthcare facilities must follow the Code of Practice. The latest version of the technical memo uses the terms water safety groups or water safety plans and highlights the role of climate change. It applies not only to Legionella but also to Pseudomonas aeruginosa and mycobacteria, among other pathogens.
The maintenance of an adequate temperature control regimen is presented as the preferred approach for Legionella control (Department of Health and Estates and Facilities Division, 2006a,b; HSE, 2013). Hot-water temperature leaving the water heater should be maintained at greater than 60°C, temperatures in the return loop should be greater than 50°C, and temperature at determined sentinel points (including the farthest draw-off point) should exceed 50°C for all types of buildings and, for healthcare facilities, above 55°C after draw-off of one minute (HSE, 2013).
The monitoring requirements for cooling towers are quarterly sampling for Legionella spp. with a target of less than 100 CFU/L. Heterotrophic plate counts have to be less than 10,000/mL. For hot- and cold-water systems, Legionella tests are not required, although they are recommended if biocide failure has occurred, if there are high-risk individuals in the building, where biocides are used as the primary control and not high temperature, or if a case of Legionnaires’ disease has been associated with the premises. At concentrations above 100 CFU/L and 1,000 CFU/L, certain actions have to be taken. More stringent requirements for monitoring of healthcare facilities and for spas and pools exist as well.
Health and safety executive inspectors enforce the Health and Safety at Work Act for hospitals, heavy industry, and manufacturing premises. Unfortunately, due to a shortage of funding, no preventive inspections are conducted. England has not had the resources to determine what percentage of buildings are colonized with Legionella, although there is no reason to believe that the proportion of buildings with Legionella has changed. To make the regulations more enforceable, fines have been raised and are now in the millions of pounds. England has not measured the effectiveness of its Legionella regulations. In 2017, the case rate for Legionnaires’ disease in the United Kingdom was 0.8 per 100,000 people (ECDC, 2019).
In England, specific Legionella regulations exist for dentistry, managed by the Care Quality Commission (CQC). To comply with these requirements of the CQC, the Department of Health’s Health Technical Memorandum 05-01 (Department of Health and Estates and Facilities Division, 2013) requires all dental practices to perform a comprehensive Legionella risk assessment to identify potential hazards relating to exposure to Legionella
bacteria from their water systems. In part, this involves decontaminating reusable instruments and daily flushing of dental unit water lines in primary care dental practices.
France
Regulations for Legionella surveillance and control in France were first introduced in 1997 for hot-water systems in healthcare facilities and more recently strengthened and extended to all public buildings (République Française 2005a,b, 2010a,b,c). The revised regulations set mandatory minimum temperatures and require L. pneumophila monitoring at defined points within hot-water systems, including outlets serving vulnerable persons.
In healthcare facilities, temperature is to be monitored daily or continuously at the hot-water heater outlet and at each return loop and weekly at service points. Temperatures must be greater than 55°C at hot-water heaters and greater than 50°C at distal points in the system. Furthermore, L. pneumophila concentrations by culture should be below the detection limit for all samples in hospitals with immunocompromised populations, otherwise immediate corrective measures must be taken. For non-immunocompromised patients, the threshold for immediate corrective measures is 1,000 CFU/L.
Environmental monitoring is also required in other public buildings with collective warm-water systems (e.g., hotels, nursing homes, senior residences, campsites, and tourist accommodation sites) and in some specific types of equipment such as cooling towers, atomizers used in public places, and thermal equipment. In public buildings with collective warm-water systems, the regulations state that the L. pneumophila concentration should not be greater than 1,000 CFU/L in hot water. If monitoring results are above the threshold, remedial actions should be taken immediately by the facility manager to protect the public and restore water quality. In spas, L. pneumophila should not be detected. In cooling towers, L. pneumophila concentration should not be greater than 1,000 CFU/L. When results come back higher than 100,000 CFU/L, the cooling tower should be stopped immediately, remedial actions should be taken by the facility manager, and the environmental authority must be informed. In thermal equipment supplied with natural mineral water, L. pneumophila and Legionella spp. should not be detected. In collective water-misting systems, L. pneumophila should not be detected. If the concentration is between 10 and 1,000 CFU/L, remedial actions should be started; when the concentration exceeds 1,000 CFU/L, the system must be stopped immediately.
Unlike other European countries, the French regulations are mainly based on environmental monitoring and specify what should be done by the facility manager in case of Legionella contamination or legionellosis cases, with less emphasis on a water management plan. Regional health and environmental agencies are the enforcement agencies for these regulations.
There has been no consolidation or analysis by the health ministry of environmental monitoring of Legionella for the many types of building hot-water systems and devices discussed above. Hence, it is not known whether the regulations have reduced the detection of Legionella in the environment. Nonetheless, the number of legionellosis cases has stabilized (2.4 cases per 100,000 in 2017), and there have been no recent outbreaks (ECDC, 2019).
Australia
Regulations for management of Legionella in Australia are enforced by states or territories. As such, they vary in some details between jurisdictions, but they are all based on joint Australia and New Zealand standards (AS/NZS). These regulations are generally
administered by state health agencies. Renewed interest in Legionella arose after a large outbreak at the Melbourne aquarium in 2000, attributed to a badly managed cooling tower. A hospital outbreak in 2013 led to increased testing at healthcare facilities. The regulations now focus on cooling towers and hot-water systems in buildings such as hospitals and other healthcare facilities. Spas are regulated under recreational water legislation (which is not discussed further).
Three national standards are enforced by the states and territories. The enHealth (2015) guidelines are for Legionella control during operation and maintenance of premise plumbing in healthcare and aged-care facilities. First published in 1991, the AS/NZS 3896 standard specifies sampling for Legionella spp. in water, while AS/NZS 3666 focuses on air handling and water systems of buildings, with an emphasis on cooling towers. These standards all have a general requirement for a risk management plan, as well as monitoring requirements for Legionella and other variables.
As per AS/NZS 3666, most jurisdictions in Australia require cooling towers to be registered, and they require dosing with a biocide, fitting of drift eliminators, regular servicing (monthly), and cleaning (every six months)—all of which are documented in a risk management plan. Some jurisdictions require monitoring of Legionella, with a range of required frequencies, and all testing is undertaken by standard culture methods. According to the regulations, a concentration of less than 10 CFU/mL (10,000 CFU/L) is considered to be non-detect. If samples exceed 10 CFU/mL twice consecutively, the building must be investigated, disinfected, and retested. If the concentration is greater than 1,000 CFU/mL (106 CFU/L) then decontamination is required. This concentration is not a science-based number; rather, it is based on what a well-maintained cooling tower can stay below. AS/NZS 3666 also specifies testing of heterotrophic plate counts (HPC), with thresholds of (1) less than 100,000 CFU/mL, (2) between 100,000 and 5 million CFU/mL, and (3) greater than 5 million CFU/mL. Some jurisdictions require notification of the public health regulator at lower Legionella or HPC levels, such as 10 CFU/mL.
The Australian regulations applicable to premise plumbing have taken two approaches. The first is to regulate only hot-water systems, allowing water delivered to bathrooms to be no more than 45°C (although they operate the hot-water system at 55°C to 60°C and have thermostatic mixing valves). The second is a risk assessment approach for all water systems, which is similar to ASHRAE 188 and other countries’ regulations. The second approach is becoming more popular and stems from the enHealth guidelines for Legionella control in healthcare and aged-care facilities. There are no prioritized treatments of contaminated systems, but some hospitals do booster chlorination. As in the United States, this process can make the hospital a drinking water provider, but there is little oversight or regulatory burden involved. If a hospital has such a treatment system, it must hire professionals to manage the system. In general, the frequency of Legionella monitoring in premise plumbing is lower than in cooling towers.
There have not been any documented, quantitative impacts of the regulations on rates of Legionnaires’ disease or environmental detection of Legionella. Australia has approximately 340 Legionnaires’ disease cases reported each year, equally divided between L. pneumophila and L. longbeachae (see Figure 5-1 for cases in Queensland). L. longbeachae is more common in the south of Australia and generally associated with soil and compost exposures. Cases have been relatively constant from 1997 to 2017, and the 2018 rate was 1.6 per 100,000 people. In Victoria, there was an increasing trend in Legionnaires’ disease rates that peaked with the Melbourne aquarium outbreak. Program administrators state the regulations have helped to improve understanding of locations of higher risk and have led to better communication between building owners and operators (Cunliffe, 2018). In the next
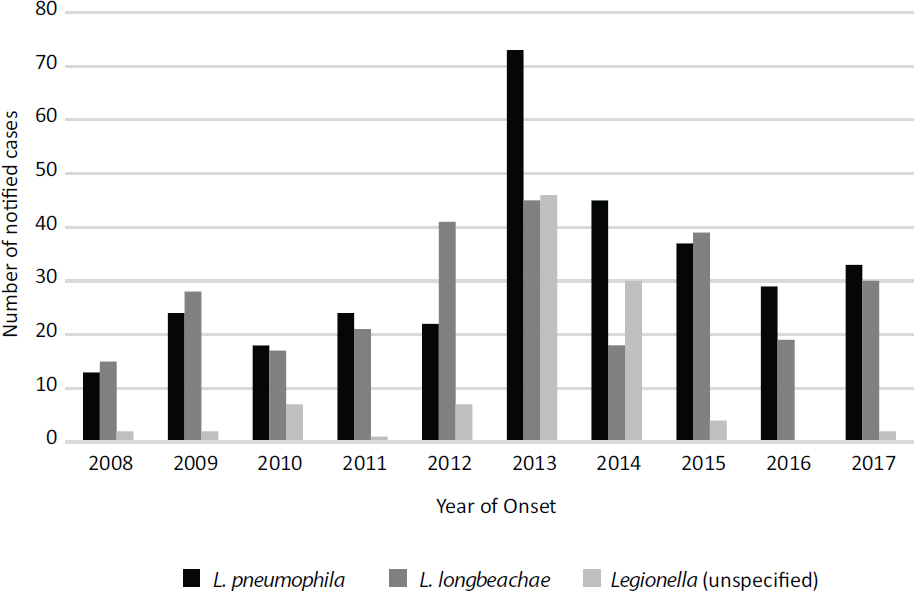
SOURCE: Queensland Health (2018).
one to two years, Legionella-related regulations will be undergoing review in several jurisdictions and may be updated to include refinements in monitoring Legionella. In many ways, the Australian regulations are less strict than the Dutch regulations: their implementation varies by jurisdiction, some have not yet fully embraced the risk management paradigm, the suite of buildings covered is more limited (hotels are not covered unless they have a cooling tower), and the concentration thresholds for action are higher.
Canada
Compared with Europe, Canada has more limited and provincial regulations for Legionella management in buildings. After a Legionnaires’ disease outbreak in Quebec City, the Public Services and Procurement Canada (PSPC) standard MD-15161 for control of Legionella in mechanical systems was created in 2013, covering the 360 buildings that are federally owned and managed by PSPC. The PSPC portfolio is comprised mostly of office buildings across Canada. MD-15161 mandates minimum design, installation, operation, maintenance, and validation testing requirements to reduce the risks associated with Legionella. There are specific requirements for cooling towers; open water systems (e.g., ornamental water features); other heating, ventilation, and air conditioning (HVAC) components (e.g., humidifiers, drain pans); and domestic hot- and cold-water systems. Like other industry standards, MD-15161 requires the development of a site-specific plan (Legionella Bacteria Control Management Program) to identify susceptible systems, their risks and hazards, and site-specific considerations, and to ensure that appropriate mitigation measures and maintenance procedures are put in place. The plan must be reviewed and updated every
five years, when there is a major change in procedures or replacement of equipment, or when Legionella testing has triggered an unscheduled disinfection of a system.
Temperature requirements are similar to many other countries, with greater than 60°C for hot-water heaters and greater than 50°C for distal points in hot-water systems (PWGSC, 2016). The monitoring required is specific to total L. pneumophila. The methods for cooling towers include monthly culture testing for total L. pneumophila, with action levels of less than 10 CFU/mL (104 CFU/L); 10 to 1,000 CFU/mL (105 to 106 CFU/L), which triggers cleaning and disinfection of the system; and more than 1,000 CFU/mL (106 CFU/L), which additionally requires the immediate cessation of any aerosol dispersal. qPCR for total L. pneumophila is conducted at system start-up, with action levels of less than 10 GE/mL; 10 to 100 GE/mL, which triggers a review of operations and treatment; and more than 100 GE/mL, which triggers cleaning and disinfection of the system. A residual oxidant test on a building’s incoming water service is also required. To support implementation of the MD-15161 standard, a separate communications protocol has been developed that ensures timely, consistent, and appropriate communication to required stakeholders based on the maintenance action level triggered by the Legionella testing result.
Although MD-15161 is required of all the Crown-owned buildings managed by PSPC, the standard is starting to be adopted and applied by other federal departments that manage federal property. There is periodic reporting of compliance to MD-15161 to PSPC senior management and periodic auditing of facilities to ensure compliance to MD-15161. Nonconformities are identified through reporting and auditing and, when identified, a plan is put in place to rectify the problem.
PSPC started implementing MD-15161 in its portfolio in 2013 and started monitoring compliance in 2014, which has led to increased awareness of Legionella control from project inception to building operation and maintenance. There has also been a concomitant reduction in the number of positive results in cooling towers, as shown in Table 5-2, which provides data on the number of times unscheduled cleaning and disinfection of a cooling tower system was triggered by the Legionella testing required by MD-15161. There are approximately 200 cooling towers in the PSPC inventory.
Quebec Cooling Tower Regulations
Following the 2012 Quebec City Legionnaires’ disease outbreak of 181 cases and 16 fatalities, the Régie du Bâtiment du Quebec (RBQ) introduced cooling tower regulations in 2013. Since then, all cooling towers in the Province of Quebec must be registered with provincial authorities. Cooling towers are defined as all open recirculating cooling systems,
TABLE 5-2 Effects of MD-15161 on Cooling Tower Performance
| Year | Number of times a cooling tower system required unscheduled cleaning and disinfection as per MD15161 |
|---|---|
| 2014 | 48 |
| 2015 | 27 |
| 2016 | 10 |
| 2017 | 11 |
| 2018 | 10 |
SOURCE: Data courtesy of Public Services and Procurement Canada.
including cooling towers, fluid coolers, and evaporative condensers. The regulation requires a documented mechanical maintenance program and a documented water treatment program, including mandatory decontamination procedures. Mandatory monthly culture-based sampling for L. pneumophila was added in 2014 (RBQ, 2014). At levels less than 104 CFU/L, no action is required. At levels between 104 and 106 CFU/L, the cause of these high levels must be identified, and the owner must apply and confirm the efficacy of corrective measures. The health-based emergency threshold is set at levels greater than 106 CFU/L, at which all equipment producing aerosols must be stopped and the owner must apply the emergency decontamination procedure and verify the efficacy of the corrective treatment. Compared to similar regulations in Europe, higher numbers were chosen as thresholds so as to not alarm people and to avoid the ambiguous implications of violating lower numbers.
Racine et al. (2019) collected and analyzed cooling tower treatment results from more than 323 evaporative cooling systems, along with corresponding L. pneumophila regulatory sampling results (n = 8,936) from July 2014 to June 2017. Water quality (i.e., hardness, alkalinity, chlorides, free and total chlorine, pH, conductivity) and treatment (corrosion and scale inhibitor, dispersant dosages) were determined. The analysis suggests that the introduction of the Quebec regulations raised the level of awareness and accountability in the management of cooling tower treatment programs, which led to a reduction in levels and incidences of Legionella positivity over the three-year period (see Figure 5-2). Interestingly, L. pneumophila control was most effective in systems using halogen-based biocides and on-line control of dosage. The study suggests that a regular review of the cooling tower treatment program and monitoring results, including L. pneumophila sampling, leads to a willingness to continue implementing control measures.
The Société Québécoise des Infrastructures (SQI) manages all cooling towers for provincial government buildings, which totals 39 buildings and 58 cooling towers. The buildings are located in different cities throughout the province and are fed by different water sources. Although all cooling towers are managed by SQI, each has a separate maintenance contract and, therefore, various disinfectants and frequencies of application. In total, 24 different biocides, both oxidants and non-oxidants, are used at various concentrations. Among cooling towers, 43 of 58 have two different disinfectants with continuous, daily, or weekly application. Only 13 of 58 cooling towers are operated year-round; the others are not operated during the winter months.
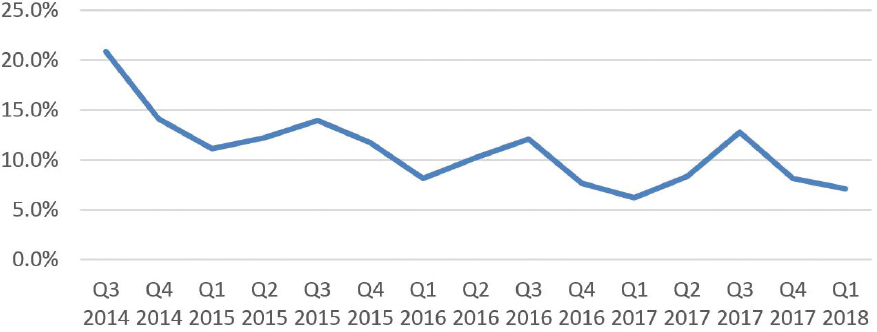
SOURCE: Adapted from Racine et al. (2019).
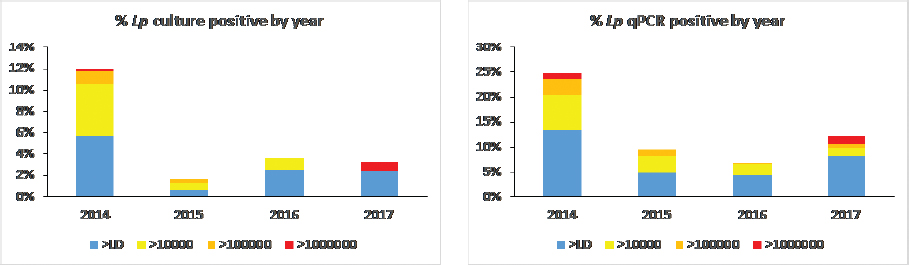
SOURCE: Created using data from SQI.
Monitoring results by culture and qPCR obtained between January 2014 and June 2017 were analyzed for temporal trends. Overall, larger number of samples were positive by qPCR than by culture, as expected. As seen in Figure 5-3, the regulations were followed by a rapid decrease of positivity in cooling towers as measured by qPCR and culture. The small number of positive samples reveals significant progress in establishing efficient treatment regimes.
In 2017, case rates for Legionnaires’ disease in Canada were reported at 1.17 per 100,000 people.7
***
Table 5-3 summarizes the above information on international laws and regulations governing Legionella management in water systems. The table illustrates the ubiquitous presence of temperature control as a control strategy for Legionella in buildings, as well as a requirement for monitoring of Legionella in building water systems—with the threshold for taking action between 103 and 104 CFU/L. This is consistent with Van Kenhove et al. (2018) who analyzed regulations in a much larger suite of countries and found that maintaining temperatures above 60°C and below 25°C, as well as monitoring of critical points, were common principles among the regulations.
For most of the countries, it is too early to make conclusions about the impact of regulations on rates of legionellosis, although there is evidence that the regulations are leading to declines in environmental detection of Legionella. Both the German building water system and Canadian government and Quebec cooling tower regulations have coincided with declines in the frequency of detection of Legionella. Lam et al. (2011) suggest that enactment of Environmental Public Health Regulations for cooling towers and water fountains in 2001 may have contributed to the decline of Legionnaires’ disease cases in Singapore. The percentage of cooling towers testing positive for Legionella decreased from 58 percent during 2000–2002 to 13.7 percent during 2004–2008. While these examples do not provide direct evidence that regulations can decrease disease rates, they suggest that making Legionella control a priority is useful public policy.
In almost all cases, regulations for Legionella monitoring and control in Europe and elsewhere stemmed from a large outbreak. Prior to the existence of the regulations, there were few if any monitoring data, making the background level of Legionella in building
___________________
TABLE 5-3 International Laws and Regulations regarding Legionella Management in Building Water Systems
| Country | Regulation/Standard/Guideline | Buildings/Devices Covered | Risk Management Plan Required? | Preferred Treatment | Monitoring Thresholds (All Converted To CFU/L) | Enforcement/Implementation |
|---|---|---|---|---|---|---|
| Netherlands |
|
|
Yes | Temperature control, flushing, UV, filtration | <100 CFU/L, no action >1,000 CFU/L, take response actions | National. Implementation of the Acts is increasing, but not yet 100%. Enforcement is via inspections, fines, possible facility closure. |
| Germany |
|
|
Yes | None, though temperature control and avoiding stagnation evident in codes | >1,000 CFU/L, take response actions | National. Very high compliance. Small cooling towers slowly coming under regulation. |
| England |
|
|
Yes | Temperature control, biocides | <100 CFU/L, no action 100-1000 CFU/L, take response actions >1,000 CFU/L, alarm bell | England only. Enforced by inspectors, but they can do no preventative work. |
| France | Regulations began in 2002 (République Française 2005a,b, 2010a,b,c) | Buildings except private residences, cooling towers | Only for cooling towers at this time | None apparent | <1,000 CFU/L target for public facilities <100 CFU/L target for prevention of nosocomial infections < 50 CFU/L target for hospitalized at-risk patients | Regional health and environmental agencies enforce the regulations. |
| Australia |
|
|
Yes for cooling towers; becoming more risk-based for buildings |
|
<104 CFU/L, no action >106 CFU/L, take response actions | Varies by state and province. |
| Canada | Standard MD-15161 (2013) | Cooling towers, open water systems, HVAC components, and hot- and cold-water systems in 360 buildings | Yes | None | <104 CFU/L, no action >106 CFU/L, take response actions | Oversight from Public Services and Procurement Canada, who does reporting and auditing. |
| Quebec Cooling Tower Regulations | Régie du Bâtiment RBQ (2014) | Cooling towers | Yes | Biocides | <104 CFU/L, no action ≥104 to <106 CFU/L, take response actions ≥106 CFU/L, alarm bell | Oversight from Société Québécoise des Infrastructures. |
water systems impossible to determine. The regulations have led to increased recognition of Legionnaires’ disease, which may be contributing to increasing rates observed in the past few years. As more monitoring data are collected and analyzed, it is anticipated that the role of these regulations in preventing disease will become clearer.
STEPS FORWARD FOR U.S. LEGIONELLA MANAGEMENT
In the United States, there are no national regulations or guidance documents similar to those described in Table 5-3 for other countries, despite the 8,453 reported cases of Legionnaires’ disease in the United States in 2018 (or 2.29 cases per 100,000, which is likely a gross underestimation of the actual burden—see Chapter 3). Furthermore, even among the directives, regulations, and guidance documents that extend to U.S. buildings, guidelines for interpreting Legionella monitoring data are lacking because of uncertainties over how to respond to certain values. These uncertainties have effectively hindered water utilities and building managers from testing for Legionella. Guidelines on routine environmental testing for Legionella vary among different documents:
- AIHA (2015) recommends that Legionella testing be conducted for validation of the water management plan or as part of an outbreak investigation. The goal is to have no positive samples, but corrective actions are required if samples have more than 103 CFU/L (see Table 5-1).
- ASHRAE 188 recommends that the team responsible for developing and implementing the building’s risk management plan for Legionella control decide whether Legionella testing should be conducted. CMS (2017) requires that all healthcare facilities be consistent with ASHRAE 188.
- DVA (2014a) recommends routine environmental testing for Legionella in VHA facilities with prescribed actions required for any positive Legionella sample, regardless of the concentration.
- NSFI 453 requires monitoring for Legionella in cooling towers. Legionella is to be maintained at less than 104 CFU/L and investigations and corrective actions taken if levels are higher.
- The New York State regulations require hospitals and healthcare facilities to monitor their potable water systems for culturable Legionella and institute control measures and notify authorities when 30 percent or more of the samples contain Legionella spp.
Only the New York State regulations are enforced by law and impose civil and criminal penalties. The VHA guidelines are internally mandated, and the policy outlines specific responsibilities for various individuals. The CMS memo (2017) requires that all hospitals and healthcare facilities receiving Medicare or Medicaid funds have a water management plan or potentially lose funding (e.g., be “at risk of citation for non-compliance with the CMS Conditions of Participation”). Thus, all VHA facilities along with cooling towers and healthcare facilities in New York State are currently required to implement water management plans and monitor for Legionella. The CMS requirements, which cover hospitals and nursing homes nationwide, do not require monitoring for Legionella because ASHRAE 188 leaves the decision to the water management team. All other buildings and private residences are potentially protected from Legionella only through the application of building and plumbing codes, which have not been historically written to manage Legionella in building water systems. There is a need for more uniform protection of public health from Legionella in
hospitals and healthcare facilities, cooling towers, and building water systems across the country. The following recommendations are made to develop a more comprehensive policy for Legionella management in the United States.
Recommendation 1. Expand the CMS Memorandum to Require Monitoring for Legionella in Environmental Water Samples
The CMS memo, which has high enforceability, requires that hospitals and long-term care facilities develop and implement water management plans. This memorandum has appropriately targeted buildings in which the mortality rates of Legionnaires’ disease are high because of vulnerable patient populations, and it has increased awareness within healthcare organizations and provided needed focus on waterborne pathogens (e.g., Legionella). Routine quantitative Legionella monitoring programs would enable these institutions to assess the effectiveness of their water management programs. All healthcare organizations should have the capacity and expertise to use these data proactively to help limit nosocomial legionellosis. Such enhanced data collection from within hospital systems structures could help to refine the data thresholds needed for prevention. This emphasis on monitoring is supported by the international regulations discussed above, by the VHA Directive and the New York State regulations, by AIHA (2015), and by the recent position paper from the Association of Water Technologies (AWT, 2019). The latter states that “Legionella testing is the only direct or ‘active’ way (currently) to validate program effectiveness, short of proving there is no Legionnaires’ disease associated with the water management plan systems.” Such an effort would also require strengthening of environmental laboratory capacity to process, evaluate, and interpret results from water samples, and it would necessitate documentation of laboratory proficiency. See below for a discussion of how to respond to the Legionella monitoring data that would stem from enforcement of an updated memo.
Recommendation 2. Register and Monitor Cooling Towers
Regulations and guidelines requiring the registration of cooling towers provide a demonstrable public health benefit with minimal regulatory burden to building owners and managers. Cooling tower registries enable a rapid public health response to community clusters of legionellosis cases, including timely remediation of possible sources of infection, and they can also be used to assess the contribution of cooling towers to overall disease incidence. In addition, regulations requiring ongoing Legionella monitoring of cooling towers have been shown to reduce cooling tower colonization rates in several jurisdictions where they have been implemented (e.g., Quebec Cooling Tower Regulations, Lam et al., 2011; Garland, Texas, Whitney et al., 2017). Unless the location of cooling towers is known, it is impossible to react quickly to identify the source of an outbreak or to assess the overall contribution of cooling towers to the occurrence of Legionnaires’ disease.
Recommendation 3. Require Water Management Plans for All Public Buildings
The standard of care specified for water management plans (see the seven bullets on page 256) should be considered best management practice for all public buildings, including hotels, businesses, schools, apartments, and government buildings. This would extend the spirit of the Safe Drinking Water Act (particularly when building water treatment is used) into building water systems not covered by the CMS memo. The recommendation here is to make water management plans a requirement for all public buildings. This re-
quirement would target the buildings likely to be sources of sporadic legionellosis, which constitutes 96 percent of all cases (see Chapter 3). ASHRAE 188, AIHA (2015), and other guidance documents are available to help create a water management plan that can meet this requirement. Derivative products that provide details for specific building types and devices, much like the CDC Toolkit has done for healthcare facilities, would be useful to help implement this recommendation.
The team developing and implementing the water management plan would outline the operation, monitoring, and maintenance of building water treatment systems using licensed and trained individuals to collect and retain appropriate records and monitoring data. (The required training of professionals is discussed in a subsequent section.) Similar to other public health certifications, application records and monitoring results could be required only on inspection, which would minimize unnecessary compliance reporting activities. Should inspections reveal serious defects in the execution of the building water management plans, penalties, including loss of certification and public notices on building entrances, could be used.
Ideally, this requirement would be codified by either local jurisdictions with authority (e.g., building inspectors) or state authorities (e.g., departments of environmental protection or health). Once codified, the requirements could be supported by insurance companies—that is, without a water management plan, a building would not qualify for insurance.
Recommendation 4. Require a Temperature of 60°C (140°F) at Hot-Water Heaters and 55°C (131°F) to Distal Points
Optimal operating temperatures at critical points in the hot-water system are based on an international consensus that maintaining minimum temperatures across the different parts of a hot-water system is the first barrier to implement to restrict Legionella growth, even if continuous disinfection is present. Typically, the requirements include maintaining temperatures of greater than 60°C at the water heater and in reservoirs, greater than 55°C in the return loop, and ensuring that distal points reach a minimum temperature of 55°C within one minute of use. Monitoring temperature at the distal points of hot-water systems would be necessary to verify that this requirement is being met. As discussed in Chapter 4 and shown in Table 4-3, 55°C carries a scalding risk that can be reduced with the use of thermal mixing valves in buildings with sensitive populations.8
The countries previously discussed in this chapter all include objectives for optimal operating temperatures in the hot-water system; design and operational specifications for water heaters, storage, and recirculation systems; and recommendations for maximum temperature at distal points. In England, France, Germany, and the Netherlands, periodic monitoring of Legionella and temperature is mandatory, with a frequency varying from continuous to weekly or annually depending on the parameters, the risk classification, and the location of the point of use. The change recommended here would align the United States with these countries.
These temperature requirements could be codified by changing building and plumbing codes. However, to impact healthcare facilities more immediately, this requirement could be instituted by modifying the CMS memo. It is also possible to incorporate these requirements into ASHRAE or other guidance; ASHRAE 12-2000 section 4.1.6 already states: “In a high-risk system, cold water should be below 20°C, hot water should be stored above 60°C and
___________________
8 The language of this paragraph was modified after release of the publication to the sponsors in order to avoid ambiguities regarding the location of the temperature requirement.
returned and circulated at above 51°C.” A required temperature at distal points could be inserted into ASHRAE 12-2000 as it undergoes revision in the near future.
Recommendation 5. Require a Minimum Disinfectant Residual Throughout Public Water Systems and Concomitant Monitoring for Legionella
It is important that water entering domestic and public buildings be of the highest quality possible. Currently, federal regulations allow for no disinfectant residual in 5 percent of the measurements in distribution systems that use surface water as a source (EPA, 1989). Federal law does not require groundwater systems to maintain any disinfectant residual within their distribution systems. L. pneumophila has been shown to grow in public water systems in which chlorine residuals were less than 0.1 mg/L (LeChevallier, 2019b). EPA should require a minimum disinfectant residual throughout public water systems and validate treatment performance by routine monitoring for L. pneumophila from sampling sites representative of the distribution system. Monitoring could focus on warm-water conditions and be triggered once water temperatures consistently exceed 20°C although some detection may occur above 15°C (LeChevallier, 2019b). Corrective actions should be taken once the concentration of L. pneumophila, or the frequency of occurrence, exceeds specific trigger levels consistent with science-based and developing guidelines and risk assessments.
Legionella has been on the EPA Candidate Contaminant List for the past ten years, which means that the agency should be evaluating methods to determine the occurrence of the organism in public water systems. However, no action has been taken because the agency is unsure how to interpret or communicate positive Legionella results in treated water supplies. The development of guidelines for interpreting monitoring data, outlined below, could provide the framework for including Legionella in the next round of unregulated contaminant monitoring (UCMR 5) scheduled to begin in 2022.9 However, utilities need not wait until EPA conducts the UCMR monitoring; they could start collecting this information now and set internal targets for distribution system optimization.
Develop Guidelines for Interpretation of Legionella Monitoring Data Using a Risk-Based Framework
The lack of clear guidelines from EPA or the CDC has hampered collection by building owners and water utilities of Legionella occurrence data over fears that a single detection could trigger onerous remediation requirements by public health and environmental regulators. In fact, monitoring for Legionella in the absence of any cases of Legionnaires’ disease has not been recommended by the CDC.10 ASHRAE 188 does not require Legionella monitoring as part of the building water management plan. Yet, three of the five recommendations above incorporate monitoring of Legionella in building water systems, which will require a framework in order to interpret the data.
There are at least two contexts in which monitoring results might be used to make decisions. The first is to detect the imminent threat of an outbreak of legionellosis based on monitoring and quantifying Legionella at points close to end uses. The Committee’s review of available data, presented in Chapter 3, indicates that when a series of measurements show Legionella levels in excess of 5 × 104 CFU/L, there is an imminent risk of an outbreak occurring. At this point, urgent action to discontinue exposure and implement a remediation
___________________
9 See https://www.epa.gov/dwucmr.
10 See https://www.cdc.gov/legionella/health-depts/ashrae-faqs.html.
plan is appropriate. For individuals who are highly susceptible (e.g., immunocompromised patients in hospital and healthcare settings), or where a greater safety factor is desired, it would be appropriate to reduce this action level multifold. The 5 × 104 CFU/L action level, which would be relevant to all building water systems, falls between the lower thresholds found in the European countries and the higher thresholds found in Australia and Canada, as discussed above. This action level is also consistent with the AIHA (2015) guidelines for all building water systems (except cooling towers). Notably, none of the numeric thresholds from these other regulations or guidances stems from any risk-based assessment but rather from practicality and expert judgement.
The second context for data-based decisions is when there is a routine program of quantifying L. pneumophila11 to determine that the risk of legionellosis is acceptably low. In this case, quantitative microbial risk assessment (QMRA) can be used to develop routine operational targets for different types of building water systems. For example, based on an analysis of acceptable risk levels, and using a 10-6 DALY/person-year as a target (Hamilton et al., 2019; see Chapter 3) single sample water concentrations of L. pneumophila of less than 1,060 CFU/L, 8,840 CFU/L, and 14.4 CFU/L in faucets, toilets, and showers, respectively, could be regarded as acceptable. In practice, one would use the most stringent number, which would be the 103 CFU/L for buildings with just toilets and sinks and 10 CFU/L for buildings with showers. For buildings with showers, the number 10 CFU/L equates to 1 CFU/100 mL, which is the detection limit of current monitoring approaches for many laboratories (ISO, 2017). From a risk protection standpoint, this value substantiates the very reasonable goal of having only non-detects in a hospital environment (see Box 3-8).
Cooling towers have been more difficult to model with QMRA because the exposure pathway from the water column via aerosols to individuals is much more complex and poorly described. Further research using dispersion models will be necessary to further refine L. pneumophila concentrations that correspond to specific risk values from cooling towers.
Train and Educate Those in Relevant Disciplines and Occupations Who Are Responsible for the Safety of Water Systems
The five recommendations above will require training and education on legionellosis and on the prevention and control of Legionella amplification in water systems for a variety of professionals, including building owners and operators, engineering consultants, clinicians and epidemiologists, laboratory technicians, inspectors, and architects, among others. The medical community curriculum should be expanded to include all aspects of diagnosing and treating legionellosis in the most effective manner. This education should also include sufficient aspects of water management to effectively educate patients on inherent risks within their homes that may require attention when they are released from the hospital. Education and training are also needed for those designing water systems, for those overseeing municipal water supplies, for those developing and implementing plumbing codes, and for those in government responsible for the safety of buildings, cooling towers, and the potable water supply. Building operators and their staff require a basic understanding of Legionella, their ecology and growth conditions, as well as sampling collection techniques for Legionella. Initial training, as well as continuing education, should be required for individuals responsible for maintenance of water operations and premise plumbing. Box 5-1 discusses two recent training programs specific to Legionella.
___________________
11L. pneumophila is indicated here, rather than Legionella spp., only because the current dose-response relationship is for L. pneumophila.
In addition to being trained, those managing building water systems should be part of the water management program team, and they should be certified to operate any water treatment system. This way, the operator’s certification can be held responsible, and possibly lost, if the building water systems are not properly maintained (in addition to any possible criminal liabilities for failure to act upon their training and certification). The certification should also require on-going educational training. Multiple entities could, and in some cases have, developed certification programs.
Disconnect Between Experts in Design, Construction, Operations, and Materials
Building water system design is often compromised because water management plans and their successful implementation are currently not understood across the building professional landscape. Even in cases where the building owner is very specific on a plan or a design to prevent waterborne pathogens, the building industry has multiple fragmented or siloed participants who preclude successful Legionella prevention. Without continuous, almost daily, interaction with all participants in the building and construction process, the likelihood of achieving the desired result can be marginal.
One challenge to progress is that the largest portion of tacit knowledge resides with the building owner and building operations professionals. In many instances, barriers to success can be associated with a general lack of understanding about water management plans by other professionals represented across the paradigm of building construction—engineers and architects who design the building, construction managers and general contractors who hire and manage the trades, and the trade groups that build the building. Although building commissioning professionals add to oversight on behalf of the owner and the operators, unless these individuals are specifically educated and understand the relevance of water safety, their value in preventing waterborne pathogens via effective design and plans is negligible. In most cases, construction design and plans to specifically reduce the incidence of waterborne pathogens come at a higher cost than standard construction methods.
Building design and construction professionals are further segregated by building type, with commercial building construction being highly specialized. Each of the major categories of building type (e.g., commercial offices, factories, warehouses, schools, retail, entertainment, data facilities, healthcare) has specific subgroups with special needs and requirements. Requirements regarding aesthetics and specific use are developed by architects and design professionals while infrastructure systems are developed by mechanical and design engineers. The design professionals may be highly specialized and segregated, whereas the building trades (e.g., carpenters, plumbers, electricians) are common to all. Training and certification are mechanisms for overcoming this inherent segregation, such that all professionals involved in building design, construction, and operation have an equivalent Legionella knowledge base.
Implementation and Cost Considerations
Although ordered 1 to 5, the five recommendations discussed above are not prioritized. In fact, accomplishing any one of them would lead to important legionellosis risk reduction, with the effect being cumulative as more recommendations are instituted. The five goals differ substantially in the necessary implementation schedule, what entities would provide oversight, their cost, and what other capacities need to be in place to support them.
Adding a requirement for monitoring within the CMS memo (Recommendation #1) could be expanded relatively quickly. Meeting this goal would entail an initial assessment of the current laboratory capacity for testing and an estimate of the number of samples that might be added to the annual work load. Most labs that are ELITE certified (see Chapter 3) can accurately identify Legionella bacteria, but quantification needs to be improved and should be made part of every proficiency testing program before Legionella monitoring can occur on a large scale. Once capacity is adequate, the implementation of monitoring could be accomplished in phases over the next three years, based on populations at risk, with oversight from the U.S. Department of Health and Human Services. Examples of hospitals already conducting such monitoring (e.g., see Box 3-8) will provide case studies and protocols.
Registering cooling towers (Recommendation #2) could follow New York’s lead, and is most appropriately coordinated at the state level, including state and city departments of health or departments of environmental protection. Any state with an outbreak or some threshold number of legionellosis cases could be prioritized, with the objective of all states meeting the requirement over a five-year time frame.
The requirement to develop water management plans in public buildings (Recommendation #3) may be the most complex and costly recommendation by the Committee, as it would require that building owners become trained and incentivized to conform via governance structures. Hopefully, with oversight from the states and assistance from OSHA, this recommendation would be implemented over the next decade by those with expertise in engineering and building water quality. Key business chains, such as hotels, could take national leadership roles, and insurance companies could require water management plans before insuring buildings.
Increasing temperature requirements (Recommendation #4) will require education and oversight via local jurisdictions and plumbing codes. Given the three-year cycles inherent to changing most plumbing codes, this requirement could not be expected to happen quickly, nor would the requirements reach a broad swath of at-risk buildings, given the limited time frames of code enforcement. However, if the temperature requirement was codified in the CMS memo, then much more rapid risk reduction, based on elevating building water temperatures, could occur.
And finally, water utilities will be responsible for managing, monitoring, and addressing disinfectant residuals and new requirements for Legionella monitoring in drinking water distribution systems (Recommendation #5). EPA should be involved, and ultimately a few of the larger utilities will likely provide guidance on best practices to implement the strategy. It is anticipated that implementation of the recommendation would take five to ten years.
Clearly, capacity building will be needed, including training programs (discussed previously), accreditation and certification of laboratory programs, and education of qualified and proficient consultants. In addition, the many work streams that will be created must be devoid of conflicts of interest, which is challenging given that many professionals are linked to a specific mitigation strategy or promote a specific product or service. For example, any individual, vendor, or contractor who develops a water management plan or provides a mitigation modality should not be responsible for monitoring the effectiveness of the plan.
None of the five recommendations for Legionella risk reduction is without implementation costs, although these are currently unknown. For this reason, cost-benefit analyses conducted by the appropriate responsible entities (such as water utilities for Recommendation #5) would be worthwhile to better understand the costs involved in carrying out the individual recommendations. Some costs will likely be passed from building and cooling tower owners onto building occupants. It may be possible, however, to meet some of the financial needs imposed by the five recommendations by adding a fee onto user water bills. Such a fee is similar in nature to the fees charged or collected by other utilities and subsequently used to subsidize improvements, conduct research, or to enhance existing utility processes. The fees could also support education and training for individuals to become competent professionals in waterborne pathogens and disease mitigation and prevention.
REFERENCES
AIHA (American Industrial Hygiene Association). 2015. Recognition, evaluation and control of Legionella in building water systems. Falls Church, VA: AIHA.
Allegheny County Health Department. 1993. Approaches to prevention and control of Legionella infection in Allegheny County health care facilities. Pittsburgh, PA: ACHD.
Allegheny County Health Department. 1997. Approaches to prevention and control of Legionella infection in Allegheny County health care facilities. Pittsburgh, PA: ACHD.
Allegheny County Health Department. 2014. Updated guidelines for the control of Legionella in western Pennsylvania. Pittsburgh, PA: ACHD.
Ambrose, M., S. M. Kralovic, G. A. Roselle, O. Kowalskyj, V. Rizzo, Jr., D. L. Wainwright, and S. D. Gamage. 2019. Implementation of Legionella prevention policy in health care facilities: The United States Veterans Health Administration experience. Journal of Public Health Management and Practice doi: 10.1097/PHH.0000000000000986.
American Society of Heating, Refrigerating, and Air-Conditioning Engineers (ASHRAE). 2015. Standard 188 legionellosis: Risk management for building water systems. Atlanta, GA: ASHRAE.
ASHRAE. 2000. Minimizing the risk of legionellosis associated with building water systems. Atlanta, GA: ASHRAE.
Australian/New Zealand Standard (AS/NZS). 2011. Air-handling and water systems of buildings-Microbial control. Part 2: Operation and maintenance.
AWT (Association of Water Technologies). 2019. Legionella 2019: A Position Statement and Guidance Document. Rockville, MD: AWT.
Best, M., J. Stout, R. Muder, V. Yu, A. Goetz, and F. Taylor. 1983. Legionellaceae in the hospital water-supply: Epidemiological link with disease and evaluation of a method for control of nosocomial Legionnaires’ disease and Pittsburgh pneumonia. Lancet 322(8345):307-310.
CDC (Centers for Disease Control and Prevention). 2003. Guidelines for environmental infection control in healthcare facilities. Atlanta, GA: CDC, U.S. Department of Health and Healthcare Infection Control Practices Advisory Committee.
CDC. 2017. Developing a water management program to reduce Legionella growth and spread in buildings: A practical guide to implementing industry standards. Version 1.1. Atlanta, GA: CDC.
Circle of Blue. 2018. Too soon to know hospital compliance with federal government Legionella policy. December 9, 2018. In Water News by Brett Walton.
CMS (Centers for Medicare & Medicaid). 2014. State operations manual Appendix Q. Guidelines for determining immediate jeopardy. Rev. 102, Issued: 02-14-14.
CMS. 2017. Requirement to reduce Legionella risk in healthcare facility water systems to prevent cases and outbreaks of Legionnaires’ disease. Atlanta, GA: CDC.
Cohn, P. D., J. A. Gleason, E. Rudowski, S. M. Tsai, C. A. Genese, and J. A. Fagliano. 2015. Community outbreak of legionellosis and an environmental investigation into a community water system. Epidemiology and Infection 143:1322-1331.
Cunliffe, D. 2018. Presentation at the 3rd meeting of the Committee on Legionella Management in Waters Systems. Woods Hole, MA. July 30, 2018.
den Boer, J. W., E. P. Yzerman, J. Schellekens, K. D. Lettinga, H. C. Boshuizen, J. E. Van Steenbergen, A. Bosman, S. Van den Hof, H. A. Van Vliet, M. F. Peeters, R. J. Van Ketel, P. Speelman, J. L. Kool, and M. A. Conyn-Van Spaendock. 2002. A large outbreak of Legionnaires’ disease at a flower show, The Netherlands, 1999. Emerging Infectious Diseases 8:37-43.
Department of Health and Estates and Facilities Division. 2006a. Water systems: Health technical memorandum 04-01. The control of Legionella, hygiene, “safe” hot water, cold water and drinking water systems. Part A: Design, installation and testing. Department of Health, London, UK.
Department of Health and Estates and Facilities Division. 2006b. Water systems: Health technical memorandum 04-01. The control of Legionella, hygiene, “safe” hot water, cold water and drinking water systems. Part B: Operational management. Department of Health, London, UK.
Department of Health and Estates and Facilities Division. 2013. Health Technical Memorandum 01-05: Decontamination in primary care dental practices. Department of Health, London, UK.
Donohue, M. J., D. King, S. Pfaller, and J. H. Mistry. 2019. The sporadic nature of Legionella pneumophila, Legionella pneumophila sg1 and Mycobacterium avium occurrence within residences and office buildings across 36 states in the United States. Journal of Applied Microbiology 126(5):1568-1579.
Dupuy, M., S. Mazoua, F. Berne, C. Bodet, N. Garrec, P. Herbelin, F. Menard-Szczebara, S. Oberti, M. H. Rodier, S. Soreau, F. Wallet, and Y. Héchard. 2011. Efficiency of water disinfectants against Legionella pneumophila and Acanthamoeba. Water Research 45:1087-1094.
DVA (U.S. Department of Veterans Affairs). 2014a. Prevention of healthcare-associated Legionella disease and scald injury from potable water distribution systems. Washington, DC: VHA.
DVA. 2014b. Plumbing design manual. November 2014. Washington, DC: VHA.
DVGW (German Technical and Scientific Association for Gas and Water). 2004. Technical Rule: Code of Practice W551. Drinking water heating and drinking water piping systems; technical measures to reduce Legionella growth; design, construction, operation and rehabilitation of drinking water installations, p. 21.
ECDC (European Centre for Disease Prevention and Control) and European Working Group for Legionella Infections (EWGLI). 2017. European technical guidelines for the prevention, control and investigation, of infections caused by Legionella species, p. 125.
ECDC. 2019. Legionnaires’ disease: Annual epidemiological report for 2017. Stockholm: ECDC.
EnHealth. 2015. Guidelines for Legionella control in the operation and maintenance of water distribution systems in health and aged care facilities. Canberra, Australia: Biotext Pty Ltd for SA Health.
EPA (U.S. Environmental Protection Agency). 1989. National primary drinking water regulations: filtration and disinfection; turbidity, Giardia lamblia, viruses, Legionella, and heterotrophic bacteria. Final rule. Federal Register 54(124):27486-27541.
European Commission. 2018. Proposal for a directive of the European Parliament and of the council on the quality of water intended for human consumption. http://ec.europa.eu/environment/water/water-drink/review_en.html.
European Working Group for Legionella Infections (EWGLI), the European Commission, and the European Centre of Disease Prevention and Control (ECDC). 2011. EWGLI technical guidelines for the investigation, control and prevention of travel-associated Legionnaires’ diseases. p. 80.
Exner, M. 2018. Presentation at the 3rd meeting to the Committee on Legionella Management in Waters Systems. Woods Hole, MA. July 30, 2018.
Gamage, S., and G. Roselle. 2018. Presentation at the 4th meeting to the Committee on Legionella Management in Waters Systems. Washington, DC.
Gamage, S., and G. Roselle. 2019. Abstracts 279 and 283 presented at the Society for Healthcare Epidemiology of America Spring Conference, Boston, MA, April 2019.
Gamage, S., M. Ambrose, S. Kralovic, L. A. Simbartl, and G. A. Roselle. 2018. Legionnaires’ disease surveillance in U.S. Department of Veterans Affairs medical facilities and assessment of health care facility association. JAMA Network Open 1(2):e180230. doi:10.1001/jamanetworkopen.2018.0230.
Hamilton, K. A., M. T. Hamilton, W. Johnson, P. Jjemba, Z. Bukhari, M. LeChevallier, C. N. Haas, and P. L. Gurian. 2019. Risk-based critical concentrations of Legionella pneumophila for indoor residential water uses. Environmental Science and Technology https://doi.org/10.1021/acs.est.8b03000.
HSE. 2013. Legionnaires’ disease: technical guidance. Part 2: The control of Legionella bacteria in hot and cold water systems. HSE Books, United Kingdom.
IAPMO (International Association of Plumbing and Mechanical Officials). 2018a. 2018 Uniform Plumbing Code. Ontario, CA: IAPMO.
IAPMO. 2018b. National Standard Plumbing Code Illustrated. Ontario, CA: IAPMO.
ICC (International Code Council). 2018. International Plumbing Code.
ISO (International Organization for Standardization). 2017. Water Quality – Enumeration of Legionella. ISO 11731:2017. Geneva, Switzerland: ISO.
Lam, M. C., W. L. Ang, A. L. Tan, L. James, and K. T. Goh. 2011. Epidemiology and control of legionellosis, Singapore. Emerging Infectious Diseases 17(7):1209-1215.
LeChevallier, M. W. 2019a. Monitoring distribution systems for Legionella pneumophila using Legiolert. AWWA Water Science. https://doi.org/10.1002/aws2.1122.
LeChevallier, M. W. 2019b. Occurrence of culturable Legionella pneumophila in drinking water distribution systems. AWWA Water Science. https://doi.org/10.1002/aws2.1139.
Lu, J., I. Struewing, S. Yelton, and N. Ashbolt. 2015. Molecular survey of occurrence and quantity of Legionella spp., Mycobacterium spp., Pseudomonas aeruginosa and amoeba hosts in municipal drinking water storage tank sediments. Journal of Applied Microbiology 119:278-288.
Lu, J., I. Struewing, E. Vereen, A. E. Kirby, K. Levy, C. Moe, and N. Ashbolt. 2016. Molecular detection of Legionella spp. and their associations with Mycobacterium spp., Pseudomonas aeruginosa and amoeba hosts in a drinking water distribution system. Journal of Applied Microbiology 120(2):509-21.
Maisa, A., A. Brockmann, F. Renken, C. Lück, S. Pleischl, M. Exner, I. Daniels-Haardt and A. Jurke. 2015. Epidemiological investigation and case-control study: A Legionnaires’ disease outbreak associated with cooling towers in Warstein, Germany, August–September 2013. Eurosurveillance 20(46). https://doi.org/10.2807/1560-7917.ES.2015.20.46.30064.
NRC (National Research Council). 2006. Drinking water distribution systems: Assessing and reducing risks. Washington, DC: National Academies Press.
NSFI (National Sanitation Foundation International). 2017. Standard 453 cooling towers—Treatment, operation and maintenance to prevent Legionnaires’ disease. Ann Arbor, MI: NSFI.
NYC (New York City). 2016a. Notice of Adoption of Chapter 8 (Cooling Towers) of Title 24 of the Rules of the City of New York.
NYC. 2016b. Cooling Tower Requirements: What Building Owners Should Know.
PWGSC (Public Works and Government Services Canada). 2016. Control of Legionella in mechanical systems. MD 15161-2013. Ottawa, Canada: PWGSC.
Queensland Health. 2018. Legionellosis in Queensland. State of Queensland (Queensland Health): Brisbane, Australia, 2018.
Racine, P., S. Elliott, and S. Betts. 2019. Legionella regulation, cooling tower positivity and water quality in the Quebec context. ASHRAE Transactions; Atlanta 125:350-359.
RBQ (Régie du bâtiment du Québec). 2014. Modifications du Québec applicables au Code national de la plomberie Canada 2010. p. 67.
République Française. 2005a. Arrêté du 30 novembre 2005 modifiant l’arrêté du 23 juin 1978 relatif aux installations fixes destinées au chauffage et à l’alimentation en eau chaude sanitaire des bâtiments d’habitation, des locaux de travail ou des locaux recevant du public. p. 3.
République Française. 2005b. Circulaire n°DGS/SD7A/DHOS/E4/DGAS/SD2/2005/493 du 28 octobre 2005 relative à la prévention du risque lié aux légionelles dans les établissements sociaux et médico-sociaux d’hébergement pour personnes âgées. p. 14.
République Française. 2010a. Arrêté du 1er février 2010 relatif à la surveillance des légionelles dans les installations de production, de stockage et de distribution d’eau chaude sanitaire (JORF n°0033 du 9 février 2010).
République Française. 2010b. Arrêté du 21 janvier 2010 modifiant l’arrêté du 11 janvier 2007 relatif au programme de prélèvements et d’analyses du contrôle sanitaire pour les eaux fournies par un réseau de distribution, pris en application des articles R. 1321-10, R. 1321-15 et R. 1321-16 du code de la santé publique, p. 8, Journal Officiel de la République Française.
République Française. 2010c. Circulaire N° DGS/EA4/2010/448 du 21 décembre 2010 relative aux missions des Agences régionales de santé dans la mise en oeuvre de l’arrêté du 1er février 2010 relatif à la surveillance des légionelles dans les installations de production, de stockage et de distribution d’eau chaude sanitaire, p. 22.
Riffard, S., S. Douglass, T. Brooks, S. Springthorpe, L. G. Filion, and S. A. Sattar. 2001. Occurrence of Legionella in groundwater: An ecological study. Water Science and Technology 43(12):99-102.
Van Kenhove, E., K. Dinne, A. Janssens, and J. Laverge. 2018. Overview and comparison of Legionella regulations worldwide. American Journal of Infection Control 47(8):968-978.
Wang, H., M. A. Edwards, J. O. Falkinham, and A. Pruden. 2012. Molecular survey of the occurrence of Legionella spp., Mycobacterium spp., Pseudomonas aeruginosa, and amoeba hosts in two chloraminated drinking water distribution systems. Applied and Environmental Microbiology 78(17):6285-6294.
Whitney, E. A., S. Blake, and R. L. Berkelman. 2017. Implementation of a Legionella ordinance for multifamily housing, Garland, Texas. Journal of Public Health Management and Practice 23(6):601-607.
WHO (World Health Organization). 2007. Legionella and the prevention of legionellosis. Geneva, Switzerland: WHO.
WHO. 2011. Water safety in buildings. Geneva, Switzerland: WHO.






































