Proceedings of a Workshop
| IN BRIEF | |
|
August 2019 |
Toward Understanding the Interplay of Environmental Stressors, Infectious Diseases, and Human Health
Proceedings of a Workshop—in Brief
“Pull a thread here and you’ll find that it it’s attached to the rest of the world.” —Nadeem Aslam, The Wasted Vigil
Infectious diseases are among the top five leading causes of death worldwide. Scientists have long known that the environment plays a defining role in the emergence and spread of infectious diseases. However, the relationships among human exposures to environmental pollution; rapid environmental change; and the emergence, spread, and persistence of infectious diseases are not yet well understood. Emerging findings suggest that exposure to environmental pollutants such as airborne particulate matter, industrial chemicals, and heavy metals may alter the immune system, increasing human susceptibility to infection. New research findings show that the microbiome1 of humans and ecosystems also play important roles in infection. Nonetheless, the fields of environmental health2 and infectious diseases largely operate distinctly from one another even though research on the interplay between these fields could inform new health practices, public health research, and public health policy.
On January 15–16, 2019, the National Academies of Sciences, Engineering, and Medicine’s Standing Committee on the Use of Emerging Science for Environmental Health Decisions (ESEHD) held a 2-day workshop to explore emerging evidence on the interactions among environmental stressors, infectious diseases, and human health. The workshops of the ESEHD committee are an “important place for horizon scanning to anticipate what is coming, to make sure that people are communicating with each other to ensure that we are on the cutting edge of environmental health sciences and technologies,” said Melissa Perry of The George Washington University, and co-chair of the ESEHD committee. To that end, the workshop brought together a multidisciplinary group, including experts in infectious disease, global public health, toxicology, epidemiology, and science policy, to discuss the emerging science and its implications for decisions about research and public policy. The workshop was sponsored by the National Institute of Environmental Health Sciences (NIEHS). This Proceedings of a Workshop—in Brief summarizes the discussions that took place at the workshop, with emphasis on the comments from invited speakers.
POLLUTION AND INFECTION: TRENDS AND INTERCONNECTIONS
At the beginning of the workshop, keynote speakers outlined how global trends and interconnections demonstrate the need for the environmental health and infectious disease communities to converge. “We live in an incredibly interconnected world,” opened Robert Newman of The Aspen Institute. Infectious diseases can travel around the planet in a matter of hours. There are also complex interconnections among the environment, humans, and infectious diseases. Newman outlined major factors influencing those interconnections, including the rapidly increasing global population,
___________________
1 All of the microorganisms in a community, including bacteria, viruses, protists, and fungi.
2 Environmental health is the science and public health practice focused on the relationship between the environment and human health.
![]()
urbanization, mega-infrastructure projects, globalization of food production and distribution, climate change, and environmental pollution. Despite this interconnectedness, “our responses remain remarkably siloed” among the animal health, human health, and environmental research communities, said Newman.
Environmental threats such as pollution and climate change have historically gone “largely ignored in global health” despite the enormous impact they have on the health of people and the planet, stated Keith Martin of the Consortium of Universities for Global Health (CUGH). Factors that influence the spread of infectious diseases include climate change, environmental pollution, poor water quality and sanitation, food insecurity, environmental degradation, biodiversity loss, natural and anthropogenically caused disasters, and poor governance. Martin asked, “how do we deal with a planet that is crying out 911 as we are destroying the ecosystem services that keep us and all species alive on this planet?” Newman noted that One Health, EcoHealth, and Planetary Health3 are three paradigms that “present opportunities for us to get out of our lanes and think.” He acknowledged that it can be easy to get caught in debates about the differences among these three patterns, but argued that people should focus on how they “bring together ways of thinking that are multidisciplinary.” Martin agreed, and described that the mission of CUGH involves bringing these three paradigms together to “improve the well-being of people and the planet across research, education, and service—paying homage to the intersections between biomedical and non-biomedical disciplines.” Linda Birnbaum, director of NIEHS, explained that her institute’s strategic plan also aims squarely at breaking down the silos between disciplines to drive its mission of discovering how the environment affects people as a means of promoting healthier lives. Birnbaum emphasized that carrying out research in basic sciences, translating research findings into knowledge and action training people and increasing scientific literacy also “have to work in an interactive way.”
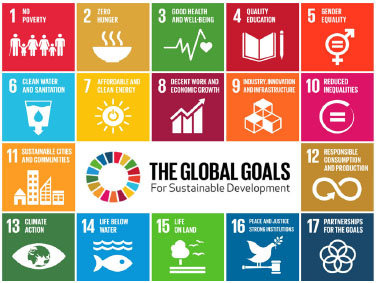
FIGURE 1 United Nations’ Sustainable Development Goals.
SOURCE: Newman presentation, slide 23.
Newman and Martin both discussed the importance of examining the interplay between environmental stressors and infectious diseases within the context of the United Nations’ 17 Sustainable Development Goals (SDGs) (see Figure 1). The SDGs are a blueprint for achieving a better and more sustainable future for all. In this context, Martin stated that an important opportunity will be for researchers and policy makers to demonstrate the links among environmental health, infectious diseases, noncommunicable diseases (NCDs), and the SDGs. A second opportunity, he said, will be to connect One Health and environmental degradation to health and security outcomes. Newman argued that making progress on achieving the SDGs requires breaking down silos. For example, many SDG targets related to human health, including environmental targets, are not part of SDG3 on good health and well-being. “You cannot achieve sustainable development goals for health unless you’re thinking outside of health,” said Newman.
TOXICANT EXPOSURES, THE IMMUNE SYSTEM, AND INFECTION
Why does the interplay between human exposure to environmental pollution and the spread or persistence of infectious diseases matter? “We’ve got a two-way street,” said Birnbaum. She explained that environmental contaminants can alter the immune response to infectious pathogens, and pathogens can alter the response to environmental toxicants (see Figure 2). In order to examine that interplay, environment needs to be defined. “We’re not just talking about synthetic chemicals. We’re not just talking pesticides,” she said. Environment includes food, consumer products such as cosmetics and prescription drugs, infectious agents, and the microbiome.
Birnbaum highlighted research from more than 20 years ago that demonstrated that an acute dose of dioxin reduced the ability of mice to survive exposure to influenza virus.4 Since then the effects of dioxin and other environ-
___________________
3 Lerner, H., and C. Berg. 2017. A comparison of three holistic approaches to health: One health, ecohealth, and planetary health.
4 Burleson, G. R., H. Lebrec, Y. G. Yang, J. D. Ibanes, K. N. Pennington, and L. S. Birnbaum. 1996. Effect of 2,3,7,8-tetrachlorodibenzo-
mental pollutants, such as polychlorinated biphenyls (PCBs) and Per- and polyfluoroalkyl substances (PFAS), on infectious diseases outcomes have been observed in many other animals, including non-human primates.
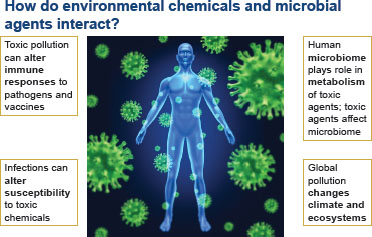
FIGURE 2 How do environmental chemicals and microbial agents interact?
SOURCE: Birnbaum presentation, slide 3.
What about humans? Does exposure to environmental toxicants influence infectious diseases outcomes in humans? “The answer is yes,” said Birnbaum. For example, human exposure to PCBs in the weeks before birth appears to decrease the immune response to childhood vaccines.5 Workshop speakers in the afternoon of the first day detailed a range of emerging evidence on the links between human exposure to different environmental pollutants—including particulate matter, industrial chemicals, and toxic metals—and human susceptibility to infectious diseases. These new findings are highlighted below.
Air Pollution
Air pollution is associated with a wide range of infectious diseases, including tuberculosis (TB), severe acute respiratory syndrome, and bacterial meningitis, said Aaron Cohen of the Health Effects Institute. He emphasized that the global burden of lower respiratory tract infections (LRIs)6 attributable to outdoor and household air pollution is particularly concerning. “Lower respiratory infection is the number one global cause of infectious diseases mortality. It is responsible for 2.6 million deaths in 2017, and air pollution is a major risk factor,” asserted Cohen, citing estimates from the latest update of the Global Burden of Disease (GBD) project.7,8 The GBD 2017 results also show that outdoor and household particulate matter 2.5 microns or smaller (PM2.5) is the leading global risk factor for LRI mortality. This is largely because of the high rates of PM-attributable mortality in children under 5 years and adults over 70 years of age, particularly in low- and middle-income countries (LMICs) in Asia and sub-Saharan Africa. Other recent work demonstrates that exposure to ambient PM2.5 reduced average global life expectancy by approximately 1 year, and reduced average life expectancy of people by 1.2 to 1.9 years in countries with high levels of air pollution.9
Cohen pointed out that LRI mortality caused by exposure to ambient and household PM2.5 has declined since 1990, mostly in children. However, he anticipates LRI will remain a leading cause of death in the future, particularly due to the effects of ambient PM2.5 exposure on older adults. Cohen stated that reducing the burden of disease and mortality will require concerted policy action to reduce PM2.5 air pollution and other LRI risk factors. Interactions among air pollution and other major LRI risk factors, such as low birthweight, and the relationship of air pollution exposure and TB are some other important areas for future research, he said.
Laboratory animal studies on air pollution and respiratory infections recapitulate epidemiological findings in human populations, said Kymberly Gowdy from East Carolina University. For example, mice exposed to a criteria air pollutant, ozone, have a significant increase in morbidity from Klebsiella pneumoniae (K. pneumoniae), a bacterial cause of community-acquired pneumonia. Similarly, Gowdy has shown in her own work that mice exposed to diesel exhaust are more susceptible to infection by influenza virus.10 However, researchers still have not nailed down the exact molecular mechanisms for how exposure to air pollution increases human susceptibility to respiratory infections.
___________________
5 Heilmann, C., P. Grandiean, P. Weihe, F. Nielsen, and E. Budtz-Jørgensen. 2006. Reduced antibody responses to vaccinations in children exposed to polychlorinated biphenyls.
6 Infections in the lungs or below the voice box such as pneumonia and bronchitis.
7 GBD 2017 Causes of Death Collaborators. 2018. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017.
8 The GBD project is an international collaboration of more than 3,000 scientists from more than 100 countries funded by the Bill & Melinda Gates Foundation. The most recent update, GBD 2017, quantifies the magnitude of health loss and death from 200 diseases and injuries in 195 countries from 1990 to 2017.
9 Apte, J. S., M. Brauer, A. J. Cohen, M. Ezzati, and C. Arden Pope III. 2018. Ambient PM2.5 reduces global and regional life expectancy.
10 Gowdy, K., Q. T. Krantz, M. Daniels, W. P. Linak, I. Jaspers, and M. I. Gilmour. 2008. Modulation of pulmonary inflammatory responses and antimicrobial defenses in mice exposed to diesel exhaust.
Gowdy outlined three potential mechanisms that scientists are beginning to explore, all of which involve the host’s immune system. The first proposed mechanism is that exposure to air pollutants inflame the lining of the lung, disrupting its barrier defenses. As a result, bacteria and viruses may be able to more easily infect lung cells and cause a systemic infection, Gowdy said. She discussed multiple laboratory studies that have shown that when particulate matter, diesel exhaust particles, or ozone interact with lung lining fluid, they create what are called damage-associated molecular patterns through their oxidation reactions with lipids, proteins, and DNA. Particulate matter can also carry bacterial toxins into the lung, triggering an inflammatory response that causes the barrier function of lung cells “to become more leaky,” she explained. A second possible mechanism involves impairing the ability of macrophages, the scavenger cells of the immune system, to engulf, or phagocytize, pathogens. Gowdy explained that experiments have shown that ozone exposure impairs the ability of macrophages to take up K. pneumoniae and Staphylococcus aureus (S. aureus). Gowdy has unpublished work that shows that air pollution exposure can break open red blood cells, releasing hemoglobin that can alter macrophage phagocytosis and decrease resistance to K. pneumoniae growth in the lung. A third potential mechanism, which Gowdy said is the least characterized so far, involves the increased production of the lung cell receptors that bacteria and viruses can use to invade lung cells. Expression of some of these receptors increase after exposure to air pollutants.11 “We don’t know why basically a non-infectious agent [air pollutant] is triggering the upregulation of different receptors, and I think that is something we need to pursue in future studies,” stated Gowdy.
Chemical Contaminants
Meghan Davis of Johns Hopkins University discussed her research on interactions between toxic contaminants and S. aureus. One-third of the U.S. population is colonized by S. aureus, said Davis. Her research has found S. aureus and methicillin-resistant S. aureus (MRSA) on multiple household surfaces, such as bathroom counters, video game controllers, refrigerator doors, and bedding and food bowls of companion pets. In the homes of people with a recent MRSA infection, MRSA is also found on a variety of surfaces, with bedroom pillows being the most contaminated. Davis emphasized the need for infectious diseases to have a place in the environmental health toxicological paradigm, particularly given that disease-causing bacteria like S. aureus are ubiquitous in the environment. Davis highlighted a 2010 publication she co-authored, which outlines evidence for expanding the environmental health toxicological paradigm.12 She explained that in the traditional environmental health paradigm “we think about how exposure to chemical toxicants will lead to clinical disease through a pathophysiologic mechanism.” If infectious disease is included within that paradigm, the infectious agent is considered an “exposure,” and immunology and infectious diseases dynamics within the host could be considered instead of pathophysiology.
Davis also described how she carries out her work within a One Health framework, examining the interactions and feedback loops among environmental conditions, animal health, and human health. Through this framework, she explored whether chemicals present in the environment could change the virulence of pathogens while they are still in the environment or within animals that serve as a reservoir or vector for the pathogen, as well as when chemicals themselves cause human disease. The presence of chemical exposure may “exert selective pressure” on pathogen populations, she explained. This might have some potential for co-selection13 of resistance and for differential effects in terms of immune responses in humans. In one study she identified that risk factors for drug resistance include human or pet use of antibiotics, living in a rural area, or household use of disinfectants on the U.S. Environmental Protection Agency’s list of products designed to kill MRSA. The latter suggests that disinfectants could co-select for antibacterial resistance if the bacteria have genes that help them survive exposure to both a disinfectant and an antibiotic, Davis stated. Other researchers have shown that blood levels of lead are associated with increased nasal colonization by MRSA and decreased colonization by methicillin-susceptible S. aureus. This finding prompted Davis to look at MRSA colonization and exposure to phthalates, a class of chemicals used to increase the flexibility, transparency, durability, and longevity of plastics. Phthalates are often found in household dust, where MRSA can survive outside of a human host. Her early research results suggest that high molecular weight phthalates in urine correlate with MRSA colonization.
___________________
11 Snow, S. J., W. Y. Cheng, A. Henriquez, M. Hodge, V. Bass, G. M. Nelson, G. Carswell, J. E. Richards, M. C. Schladweiler, A. D. Ledbetter, B. Chorley, K. M. Gowdy, H. Tong, and U. P. Kodavanti. 2018. Ozone-induced vascular contractility and pulmonary injury are differentially impacted by diets enriched with coconut oil, fish oil, and olive oil.
12 Feingold, B. J., L. Vegosen, M. Davis, J. Leibler, A. Peterson, and E. K. Silbergeld. 2010. A niche for infectious diseases in environmental health: Rethinking the toxicological paradigm.
13 Co-selection is the incorporation of multiple resistance genes within a bacterial genome following a microbe’s inclusion of a single resistance gene that enabled the microbe to survive a specific xenobiotic exposure.
Davis emphasized that chemical exposures may also influence non-infectious health outcomes of pathogens. She explained that S. aureus can drive inflammation in different ways—through pathways associated with typical immune responses to infection and through immune pathways more often associated with allergies. Davis is conducting research to understand the connections between immune responses to S. aureus and the incidence of asthma in inner-city children. Phthalate exposure is also associated with asthma, raising the question of whether chemical toxicant exposure and pathogen exposure can operate along the same inflammatory pathways and therefore both cause the same disease. Davis said a way to model this interaction is to consider that a first exposure might cause acute disease while sensitizing the host. When the host is exposed a second time, the immune system may respond through an allergic immune pathway that results in worse disease. Her research has shown that host factors could modify this association. Adolescents without a history of eczema had worse asthma symptoms when exposed to S. aureus enterotoxin A found in dust from their bedrooms. Davis is continuing to investigate the reasons behind that research finding.
Berit Granum from the Norwegian Institute of Public Health discussed how exposure to PFAS may influence human immune response to pathogens and vaccines. PFAS are found in a wide range of consumer product and food packaging, and once ingested they can remain in the body for 3–7 years. In 2016, the U.S. National Toxicology Program concluded, based on published studies in humans and animals, that two PFAS in particular—perfluorooctanesulfonic acid (PFOS) and perfluorooctanoic acid (PFOA)—are hazardous to the immune system because they may reduce the body’s response to vaccines, suppress antibody responses to pathogens, and reduce the ability to respond to infectious diseases. Human studies have found that prenatal exposure to PFOS and PFOA reduced vaccination response to diphtheria and rubella and, particularly in girls (ages 3 and 7), had positive associations with airway infections, viral gastroenteritis, fever, and the overall occurrence of infectious diseases, said Granum.14
Responding to these and other studies, Europe banned PFOS in 2008 and PFOA starting in 2020, and major U.S. manufacturers have agreed to eliminate these and related chemicals from their products.15 Though the use of these compounds is dropping, both the European Food Safety Authority and the U.S. Agency for Toxic Substances and Disease Registry concluded in 2018 that a considerable proportion of the population still has higher exposure than what are considered tolerable intake levels. Granum stated that the immune system is a sensitive target for chemicals in the environment, but the lack of validated guidelines makes it difficult to determine the best approach to test chemicals for immunotoxic effects.
Metal Toxicants
Mercury and arsenic are two of the most toxic and widely used metals. Research has shown that both can adversely affect the immune system. All forms of mercury, for example, are immunotoxic in some manner, said Jennifer Nyland of Salisbury University. Even mercury’s well-documented neurotoxicity is driven by interactions with immune system cells in the brain, she emphasized. There is also evidence that co-exposure to low levels of mercury—the equivalent of eating one can of tuna per week for 2 weeks—and some “trigger,” such as exposure to a virus or another pathogen, can increase the body’s autoimmune response. This, in turn, can damage the heart or suppress the immune response, depending on individual genetic susceptibility. Nyland noted there are inconsistencies in what is seen in cell culture studies, animal studies, and human epidemiologic studies. The inconsistencies are likely related to differences in exposure level; the species of mercury (i.e., elemental, inorganic, or organic forms); genetic background; and co-exposures to infection, xenobiotics,16 and medicines. “Mercury itself is likely to be insufficient on its own to induce these immune-related adverse outcomes,” she said. “There needs to be some other trigger.”
Nyland’s studies of how mercury interacts with the immune system have focused on the inflammasome, a multiprotein intracellular complex whose assembly is induced through a variety of pathogen and damage-associated signals. Her research has suggested that environmentally relevant levels of mercury activate the inflammasome, which would result in the release of various cytokines. She noted it would be interesting to see how the microbiome reacts to mercury exposure and how that reaction would affect the immune response.
Molly Kile from Oregon State University discussed emerging epidemiologic evidence on the links between arsenic exposure and infectious diseases. Arsenic, which is ubiquitous in the environment, is immunotoxic, stated Kile.
___________________
14 Impinen, A., M. P. Longnecker, U. C. Nygaard, S. J. London, K. K. Ferguson, L. S. Haug, and B. Granum. 2019. Maternal levels of perfluoroalkyl substances (PFASs) during pregnancy and childhood allergy and asthma related outcomes and infections in the Norwegian Mother and Child (MoBa) cohort.
15 PFOS and PFOA are no longer manufactured in the United States, but can be found in imported consumer goods, including carpet, textiles, packaging, rubber, and plastics.
16 Chemicals found within an organism that are not naturally produced by or expected to be found within the organism.
Most people are exposed to arsenic by drinking water drawn from contaminated groundwater aquifers and consuming crops grown in contaminated soils. Arsenic can accumulate in rice, a dietary staple for large parts of the world. Arsenic is also found in brown rice syrup, which is present in many manufactured food products, she explained. Kile’s research group has found that higher arsenic levels in urine correlate with a failure to produce protective antibodies in response to vaccination for varicella zoster virus, the causative agent of chickenpox and shingles.17 They concluded that arsenic may be associated with a waning of the natural immunity against varicella, which is “nearly ubiquitous in the general population.”
Kile also discussed studies on children exposed to arsenic early in life. Children exposed to arsenic in utero had a strong decrease in antibody production in response to diphtheria vaccination. The odds of having insufficient diphtheria antibodies by age 5 have increased by 8 percent for every doubling of arsenic exposure in the drinking water during pregnancy. She noted research in New Hampshire18 and Bangladesh19 that show similar associations between arsenic exposure during pregnancy and increased risk of lower respiratory infection and diarrheal disease in children in their first year. Kile questioned whether children in places where arsenic exposure is common, such as Bangladesh, need to receive booster shots of vaccines to compensate for a suppressed immune response.
MICROBIAL MEDIATORS OF RESISTANCE
“Earth is a microbial planet,” said Rodney Dietert of Cornell University. Of all of the genes in the human body, approximately 99 percent are microbial and more than half of all of the cells in the human body belong to the organisms in its microbiome. Dietert noted that an estimated 3.3 million microbial genes code for enzymes and cell signaling molecules that affect the human body directly or through epigenetic interactions, such as regulating inducible enzymes in the liver. “The microbiome is the lens through which the body sees its external environment,” including chemicals and pathogens, Dietert explained. He predicted that “managing the microbiome–immune system interface is going to be a significant part of both preventive and therapeutic health, whether it is in humans or animals.”
The belief that newborns are fully prepared immunologically to fight all diseases is one dogma from the 20th century that should be discarded, stated Dietert. The truth, said Dietert, is that babies’ immune systems require the development of a robust microbiome to fully mature. In the infant, gut microbes at microbial surfaces produce a host of molecules that influence immune system development. Experiments in newborn mice, for which there are parallels in humans, found that a specific bacterium produces a molecule that dampens the burst of immune system cells known as invariant natural killer T cells. As a result, adult mice are protected from autoimmune inflammatory bowel-like diseases and colitis. Dietert noted that babies delivered by Caesarian section run the risk of not being seeded with a robust microbiome as they pass through the vaginal canal, which can leave them open to acquiring their microbiomes from the hospital environment.
What happens, then, when gut microbes are exposed to chemicals and drugs? Dietert explained that microbes can metabolize drugs or other substances in a variety of ways that may change the bioavailability of those substances. A healthy microbiome can serve as a barrier to infection by pathogens. Experiments suggest that as few as 15 bacterial species will produce a metabolic environment to protect the body from colonization by salmonella.20 But, the microbiome can also modify chemicals in ways that can be harmful to the human host. Multiple studies have also shown that individual risk from drinking arsenic-contaminated water depends on how many sulfate-reducing bacteria, which produce some of the most toxic arsenic metabolites, are in a person’s colon, he said.
Dietert noted that most drugs and other substances humans ingest have not been screened for microbial safety. For example, studies have shown that food emulsifiers can kill a keystone21 microbiome organism that helps
___________________
17 Cardenas, A., E. Smit, E. Andres Houseman, N. I. Kerkvliet, J. W. Bethel, and M. L. Kile. 2015. Arsenic exposure and prevalence of the varicella zoster virus in the United States: NHANES (2003–2004 and 2009–2010).
18 Farzan, S. F., A. Gossai, Y. Chen, L. Chasan-Taber, and M. Karagas. 2016. Maternal arsenic exposure and gestational diabetes and glucose intolerance in the New Hampshire birth cohort study.
19 Rahman, A., M. Vahter, E. Ekström, and L. Persson. 2011. Arsenic exposure in pregnancy increases the risk of lower respiratory tract infection and diarrhea during infancy in Bangladesh.
20 Brugiroux, S., M. Beutler, C. Pfann, D. Garzetti, H. J. Ruscheweyh, D. Ring, M. Diehl, S. Herp, Y. Lötscher, S. Hussain, B. Bunk, R. Pukall, D. H. Huson, P. C. Münch, A. C. McHardy, K. D. McCoy, A. J. Macpherson, A. Loy, T. Clavel, D. Berry, and B. Stecher. 2016. Genome-guided design of a defined mouse microbiota that confers colonization resistance against Salmonella enterica serovar Typhimurium.
21 Any species whose effect on its ecosystem is disproportionate to its relative abundance.
maintain the protective intestinal mucin layer. These food emulsifiers were thought to be safe, but they were never tested for microbial safety, he said. Arsenic exposure can also change the microbiome and microbial gene expression in a manner that increases the risk of certain infections, including hepatitis B. However, at low acute exposures certain microbiome species can protect the immune system by blocking the uptake of arsenic.
In her talk, Kile noted that the microbiome is also affected by arsenic exposure, changing the relative abundance of different microorganisms. She highlighted her recent work that identified a connection between the presence of metals in different environmental reservoirs, such as soil or manure piles, and the presence of antibiotic-resistance genes.22 In fact, the genes coding for a protein that pumps arsenic out of bacteria occurs on the same gene mobile genetic element as the genes responsible for multidrug resistance. “As we increase our exposure to arsenic, either through tapping into groundwater or through how we are manipulating coal and fossil fuels on this planet, are we increasing pressures that are also going to push more toward a greater prevalence of antibiotic resistant bacteria, because of the arsenic, not because of the overprescription of antibiotic drugs?” asked Kile.
Laura Kahn of Princeton University gave an overview of the challenges of “biotic environmental contamination”—human and animal fecal matter in the environment—and its role in the spread and persistence of antibiotic resistance. Humans, domesticated animals, and livestock produce “massive amounts of fecal matter,” said Kahn. She calculates that the total amount of fecal matter produced by humans and their livestock could fill more than 26 Olympic-size swimming pools by 2030. Much of human exposure to antimicrobial resistant bacteria and to pathogenic bacteria that cause foodborne illness can be attributed to the fecal contamination of food, water, and the broader environment, said Kahn. According to the United Nations Children’s Fund, approximately 1 billion people—600 million of them in India—defecate in fields. India has some of the most microbial-laden environments and some of the most antibiotic resistant organisms in the world, Kahn said. In high-income countries, manure lagoons on concentrated livestock farms run the risk of spilling their contents into waterways, as was seen in North Carolina in the aftermath of Hurricane Florence, she remarked. In addition, livestock fecal matter is applied to fields as a crop fertilizer, where rain causes it to run off into waterways. Besides spreading bacteria, the runoff is rich in nitrogen and phosphorous, leading to eutrophication23 in lakes and coastal waters and to the death of fish and other aquatic organisms. Kahn said that widespread fecal contamination in the environment is disrupting the global resistome, antimicrobial resistance genes that are ubiquitous and ancient. “We are adversely affecting the global resistome through our poor sanitation and indiscriminate antibiotic use, whether in humans or animals,” Kahn emphasized.
Antibiotic resistance accounts for an estimated 700,000 human deaths annually, a figure projected to rise to 10 million per year by 2050 if no action is taken, said Kahn. Nations in Asia and Africa are likely to be most affected, with huge economic impacts. To address antibiotic resistance, the World Health Organization, the Food and Agriculture Organization of the United Nations, and the World Organisation for Animal Health developed a manual to help countries create national action plans to fight antibiotic resistance. Strategic objectives included improving awareness through education and training, strengthening knowledge and the evidence base through surveillance and research, and improving sanitation, hygiene, and infection control. However, Kahn pointed out that the objectives fail to mention animal or human fecal matter in the environment.
DISRUPTED ENVIRONMENTS
Environmental disruptions, both of human and natural origin, can have a significant impact on the incidence of infectious diseases. Human disruptions, such as rapid urbanization and huge water transfer projects, can expose immunologically naïve populations to new pathogens, stated Justin Remais from the University of California, Berkeley, as can natural disasters such as drought, flooding, earthquakes, and hurricanes. He noted that environmental health sciences should be well equipped to contribute to studying the link between environmental disruptions and infectious diseases.
Kahn described a study on the relationship between rainstorms and cholera outbreaks in Bangladesh.24 The researchers found that storms disrupt the normal homeostasis between Vibrio cholera strains and the bacteriophages
___________________
22 Dong, X., N. Shulzhenko, J. Lemaitre, R. L. Greer, K. Peremyslova, Q. Quamruzzaman, M. Rahman, O. S. Hasan, S. A. Joya, M. Golam, D. C. Christiani, A. Morgun, and M. L. Kile. 2017. Arsenic exposure and intestinal microbiota in children from Sirajdikhan, Bangladesh.
23 High concentrations of nutrients in a lake or other body of water that cause a dense growth of plant life and death of animal life from lack of oxygen.
24 Faruque, S. M., M. J. Islam, Q. Shafi Ahmad, A. S. G. Faruque, D. A. Sack, G. B. Nair, and J. J. Mekalanos. 2005. Self-limiting nature of seasonal cholera epidemics: Role of host-mediated amplification of phage.
in the environment that infect and kill Vibrio cholera. These outbreaks do not subside until that equilibrium is reestablished, stated Kahn. This finding points to the possibility that bacteriophages could be an important tool for combating antibiotic resistance, and in fact, the U.S. Food and Drug Administration approved some bacteriophage products for use in the food safety market.
Remais pointed out that modeling work shows that the public health community underestimates the impact of extreme weather on infectious diseases outcomes and also on the importance of human gatherings as drivers of infectious diseases outbreaks. Modeling has also been used to better understand how different agricultural chemicals affect the life cycle of the parasitic flatworms that cause schistosomiasis and helminth infections that affect almost one-quarter of the world’s population. Remais explained that one such model identified pesticide and fertilizer combinations that amplify transmission of these flatworms and enabled the identification of new agrochemical regimes that achieve pest control and productivity targets while minimizing adverse infectious diseases outcomes. However, there are few methods available to detect many environmentally mediated pathogens of global importance in the environment, said Remais. For example, there is currently no good way to measure Coccidioides spores in dust. This fungus causes coccidioidomycosis, also known as valley fever, which has spiked in California since 2001. Lacking a method for detecting it in soil and dust, it remains unclear how recent drought, increased exposure to air pollution, and changes in population susceptibility to Coccidioides spores have contributed to the increased incidence in cases of valley fever. “We do not know much about how it disperses against the landscape or how close you have to be to a putative source,” said Remais. “We know nothing about exposure and can do little to protect workers.” To solve this problem, he called for environmental health scientists to work with their colleagues in the infectious diseases space who have developed novel detection methods such as quantitative polymerase chain reaction.
Maureen Lichtveld of Tulane University pointed out that communities impacted disproportionately by natural disasters suffer from historic health disparities and are more likely to face persistent environmental health threats. For example, there were historic health disparities in Louisiana and Mississippi and a general lack of disaster preparedness and available resources prior to Hurricane Katrina, and in the aftermath of the hurricane, West Nile Virus neuro-invasive disease increased in both Louisiana and Mississippi, with unaffected regions showing only minor increases compared to those devasted by the hurricane. Chagas disease increased in the 9 months following Hurricane Katrina because of an increase in the population of armadillos, which are a host for insects that harbor the organism that causes this disease.
The 7.8 magnitude earthquake and 7.3 magnitude aftershock that struck Nepal in 2015 left 10 percent of the nation’s population homeless and destroyed 400 health facilities. Acute gastroenteritis increased significantly in children from families substantially affected by the earthquakes, with preexisting health disparities playing a role. Fragile infrastructure played a significant role in the outbreak of disease, said Lichtveld, and continued political instability is hampering aid from China and Japan that would go toward installing facilities to supply clean drinking water. “We can look at infectious diseases in isolation, and we will not get the problem solved,” she said.
Hurricane Maria had devastating impacts on the fundamental needs of food and water, electricity, communications, and medical care in Puerto Rico, as well as on the ability to monitor infectious diseases in the hurricane’s aftermath. What is known is that in the 6 months after the hurricane, there were 26 deaths attributed to leptospirosis, a bacterial disease spread by contact with animal urine or environmental contamination in water and soil. In contrast, massive floods that affected parts of Suriname in 2006 resulted in a decrease in malaria cases because the mosquito vector could not lay its eggs in the turbulent water created by the floods, though there was a small increase in diarrheal disease that fell quickly. Residents of the affected region have now turned to large- and small-scale gold mining as a means of diversifying their income source, leading to an increase in mercury levels in the local environment. A study is now following 1,000 pregnant women and their children to examine the impact of mercury exposure on pediatric neurodevelopment.
What all of this means is that environmental disruptions can include slow-moving shocks and stressors in addition to the acute shocks associated with the disruption, said Gowdy. Infectious diseases control after such disruptions should be an integral component of disaster preparedness, response, and recovery. She also noted that maternal and child health can serve as a “sentinel” for vulnerable conditions and populations when looking at infectious diseases’ exposure, transmission, and outcomes, but only if a well-developed data collection capacity is established using trained community health workers to build longitudinal baseline assessments before a disruption occurs.
DEVELOPING TRANSDISCIPLINARY, TRANSLATIONAL RESEARCH STRATEGIES
“How do you connect and collaborate? How do you draw in methods and ways of thinking from different disciplines? How do you actually go from research to action? How do you go from knowing something to doing something?”
asked Niladri Basu from McGill University. To answer these questions, Basu drew from his experience conducting an integrated assessment of mercury pollution from artisanal and small-scale gold mining (ASGM) in Ghana.25 ASGM mainly takes place in LMICs, said Basu. Mercury is used to remove gold from mined rocks. The final step in the process involves burning off the mercury from the mercury-gold amalgam, leaving behind pure gold. The vaporized mercury contaminates the work environment, the community, and regional environmental systems. The mercury concentrations in people who live in these communities are orders of magnitude higher than places without ASGM, said Basu. Though the health hazards associated with mercury contamination are significant, Basu was surprised to find few community members cared. He was concerned about “grim levels of mercury” in the people and their environment. However, a representative from the Minerals Commission Ghana explained to Basu that ASGM communities view mercury as magic. The mining of mercury is bringing roads into the villages, creating connections that never existed before, enabling people to double their incomes from $3 to $6 per day, and bringing better quality food to the table. The people revere mercury so much that “when you build a house, you impregnate the foundation with mercury in it,” explained Basu. This was a defining moment in his early career that changed his perspective and approach to research. “I needed to be more pluralistic in my thinking and ways of doing things,” instead of “sitting in my toxicology echo chamber,” said Basu. Balancing the risks and benefits of mercury in society is what now drives his research agenda.
Basu shared key lessons from how his thinking has evolved with time and experience. First, you need to bring multiple researchers together to form a team, said Basu. He emphasized that it is not always necessary to bring the smartest researchers into a team. “Thinking about the individual, what they bring to the table, and whether they can work in a team environment is just as important, if not more important, than the quality of that individual in terms of their scientific thought.” Second, it is important to bring together multiple disciplines. Basu collaborates with colleagues in the natural sciences, social sciences, human health, infectious diseases, policy, and economics. Where Basu saw puddles of water in a village laden with mercury and other toxic chemicals, the ecologists noticed tremendous land degradation and environmental change. The epidemiologists noticed an agrarian society with people moving around with their cattle, effectively communicating from village to village. The physicians noted that in addition to mercury exposure and the physically taxing nature of ASGM, the air in the village was filled with dust and there were babies everywhere exposed to that dust. The anthropologists, after talking to the women in the community, saw “water as life.” Women in the communities collect water to bathe, cook, launder, make an income, and support the community. Basu emphasized that the role of the social scientists is underappreciated and much needed. “When you look at the grand challenges in pollution and infectious diseases, these are ones that touch upon human rights, economics, and security issues.” Multidisciplinary teams are able to take on grand challenges “in a grander way,” stated Basu. Third, grand challenges take time, both for the research to progress and for collaborators to build trust, understand one another, and overcome linguistic barriers, said Basu. Developing and improving on “core methods” is critical, he added. Basu said to “look at the frontiers and interfaces” of methods and determine whether methods can be shared and improved. Finally, Basu emphasized the importance of project management. “Few of us are trained to adequately run scientific research projects, so it is important to hire professionals,” he said. All of these factors work together so that “we can get a more holistic and deeper understanding of whatever challenges we face.”
The key, though, is in translating this broader perspective into actions and solutions that are feasible economically, socially, and politically. For example, the environmental toxicologist on Basu’s team suggested promoting mercury-free methods for refining gold that if implemented would benefit both community health and the environment. However, when the social scientists surveyed an ASGM community, they found that although the villagers liked the idea generically, there was a low chance it could be implemented. Similarly, when nongovernmental organizations (NGOs) pass out masks in an ASGM community, they go unused because the NGO workers did not speak with physicians and occupational health experts about how difficult it is to promote mask use. It is too difficult for community members to fit masks properly without training, Basu explained.
What is most important, stated Basu, is getting as many stakeholders involved as possible—from high-level deputy ministers and high-level officials from NGOs to members of the community and local scientists—to create a stable and trusted environment in which discussions can occur over the long term. “Working with the same group for years builds trust and provides the flexibility and power to make progress,” he said. “Money is important, and the more the better, and sustainability requires training members of the community to become involved in and take over at least some of the work rather than simply relying on researchers from the global north.” Toward that end, the United
___________________
25 Basu, N., E. P. Renne, and R. N. Long. 2015. An integrated assessment approach to address artisanal and small-scale gold mining in Ghana.
States and Canada have partnered to create the Global Environmental and Occupational Health (GEOHealth) program that will invest $21 million in creating environmental and occupational health research hubs in seven LMICs.26 Basu underscored the importance of building “in-country” capacity so that local communities can lead their own research and education programs, and so that funding goes to experts that are in-country.
At the end of his talk, Basu emphasized that charts of the global burden of disease demonstrate that we face grand challenges with environmental, infectious diseases, and pollution issues. However, scholarly communities best suited to examine those intersections are not yet connecting, he said. To illustrate the disconnect, Basu shared the results of a PubMed search for articles published on “environmental health” and “infectious diseases” since 2009 (see Figure 3). In the past 10 years more than 40 000 articles were published on environmental health and more than 53,000 on infectious diseases. But fewer than 500 articles of the approximately 93,000 search results focused on both environmental health and infectious diseases. “There is so much innovation in each of our fields, we need to look for ways to interface and work at the frontier,” Basu concluded.
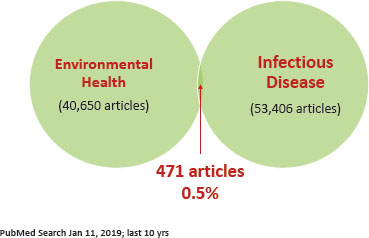
FIGURE 3 PubMed search of articles published on environmental health and infectious diseases since 2009.
SOURCE: Basu presentation, slide 60.
Enabling Translational Research
On the second day, workshop participants explored ways in which different research communities can collaborate, brainstormed about research opportunities, and discussed ideas to facilitate the use of research in decision making. There are many vulnerabilities from the microscopic level of cells and cytokines to macroscopic scale of populations and global stresses. “These systems need to be balanced,” stated Gary Ginsberg of the New York State Department of Health. He encouraged workshop participants to identify “where transdisciplinary work and translational work needs to occur” in order “to decrease the vulnerabilities that we see within populations confronted with infectious diseases.” Several workshop participants commented that there are important disciplinary perspectives missing from the conversation, including data science, community resilience, nutrition, veterinary medicine, geology, exposure science, and social sciences. Lichtveld also emphasized the importance of statisticians. “Without predictive modeling, we will not be able to answer questions that deal with complex interactions,” she said. Several workshop participants noted that statistics will need to go beyond looking at non-linear effects but encompass multiple stressors and also buffering effects. “Are there any ecologists in the room?” asked Mark Johnson of the U.S. Army Public Health Center. Johnson said past mistakes in research resulted from insufficient understanding about host–vector interaction. Understanding the ecology “is a big piece,” he emphasized. To Gina Solomon of the University of California, San Francisco, the scope of the discussion about the interplay between environmental stressors and human health should include organisms other than humans. As examples, she cited how colony collapse disorder that is decimating honey bee populations will affect humans indirectly through the impact on the food supply and how global climate change has allowed the western bark beetle to infect large swaths of California’s pine forests, fueling the massive fires that affected Californians.
Ginsberg pointed to large-scale endeavors like One Health, and asked whether they could be augmented to include ideas and gaps identified from research on the intersection of environmental pollution and infectious diseases. Speaking from a personal perspective, and not in an official capacity, John Balbus of NIEHS expressed doubt that existing infrastructure could be co-opted without significant renovations. Lichtveld agreed. She said that some major new projects are not progressing well, because they do not fit within existing infrastructures. “We can use the existing projects or programs as good building blocks, but they can’t be the foundation,” Lichtveld argued. Davis pointed out that how to build a research infrastructure and funding system that supports transdisciplinary science is a challenge that still needs to be overcome. One Health could be the beneficiary from this kind of thinking, Davis remarked. Balbus mentioned that the Belmont Forum, which focuses on global environmental science and explicitly includes the social sciences in its work, is building a collaborative research program in climate, environment, and health that could serve as an overarching infrastructure. Joshua Rosenthal of the National Institutes of Health’s (NIH’s) Fogarty International
___________________
26 See https://www.fic.nih.gov/Programs/Pages/environmental-occupational.aspx (accessed July 19, 2019).
Center pointed out that creating new paradigms for research and training entails a lot of work. “Who really needs to be at the table for those kinds of discussions?” he asked. In addition to federal agencies like NIH and the National Science Foundation, Rosenthal accentuated the increasing role for large private philanthropies. The Rockefeller Foundation, Gates Foundation, and Bloomberg among others are champions in this field and need to be part of the conversation, he argued. Rosenthal suggested that creating a consortium of funding organizations might be another way “to enable transformational kinds of investments within a new paradigm.”
At the conclusion of the second day, Carlos Santos-Burgoa from The George Washington University applauded the efforts made so far to integrate environmental and infectious diseases surveillance, which he said also need to happen at the national level and involve national decision makers. Basu commented that students who have yet to be inducted into an academic silo and are eager to work on interdisciplinary problems may offer the best opportunity to bring disparate fields together. Students interacting with students in lower- and middle-income communities may also be a bridge to those understudied communities.
In the end, science will only take us so far, said Basu. “To have a truly transformational impact, it will be necessary to hand knowledge gained through science off to those who can make an impact in the work of policies, laws, and legislation.” When he hears that these things take time and money, he counters that the cost of inaction is far higher than the cost of action, and somehow this needs to be documented through economic studies, security studies, and engagement with a range of disciplines that are not yet at the table. Solomon noted the challenges of formulating policy for substances whose immunotoxic effects are tied to environmental factors. Ginsberg remarked that economic models used for cost–benefit analyses for regulating air and water pollution do not incorporate the chemical and non-chemical factors that can affect immune health and health in general. The fact that science is starting to make inroads in understanding the connection between environmental factors and infectious diseases, which is monetizable, will directly affect these cost–benefit analyses used to set policy, he observed. Martin seconded this idea and added that demonstrating a rate of return on evidence-based solutions and democratizing that knowledge by making it comprehensible to the public and policy makers will help drive change.
CLOSING THOUGHTS
Change was a consistent message throughout the workshop, said Newman in his concluding remarks, starting with the importance of changing the way researchers engage communities in deciding what issues to study, providing feedback to those communities, and developing grand solutions to the grand problems that are so well articulated. Change is needed regarding how researchers fail to distinguish between adults and children concerning how they react to environmental stressors and infectious diseases, yet at the same time create artificial distinctions between communicable diseases and NCDs, synthetic and natural chemical compounds, and beneficial and harmful microorganisms, he said. Newman also emphasized that changes need to occur in the way researchers work with—and are trained to work with—one another across fields to break down silos and expand the range of disciplines engaged to address the increasingly complex public health issues arising from the interplay of environmental stressors, infectious diseases, and human health.
Newman noted the critical role that good leadership and management, both on the ground and at the national and international level, can play in increasing both the success and the impact of research and in better managing valuable resources for efforts to meet SDGs. He pointed to the need to incorporate design thinking into the design of research and to consider the role of the social environment and other non-tangible factors that are difficult to quantify but that certainly mediate the interplay among environmental stressors, infectious diseases, and human health.
As research provides new insights into the links between the microbial world and human health, it also identifies new gaps in knowledge, said Newman. Better methods are needed, for example, to assess environmental exposures, quantify routes of exposure, and explore the role that human microbiomes can play in exacerbating or ameliorating exposures to environmental stressors. Advances have also led to new concepts that deserve further exploration, including the global resistome that acts as a microbial reservoir of antibiotic resistance mechanisms; the microbiome-immune host defense barrier known as the microimmunosome; the multiprotein inflammasome that responds to infection; and the exposome, which measures the sum of all exposures an individual has during a lifetime.
One of the challenges that Newman noted regarded how to deliver a balanced message to the public that everything is not terrible, that while research is identifying various ways in which environmental stressors can increase the risk of infectious diseases and adverse consequences for human health, advances in public health have produced a
dramatic increase in human lifespan. In the same vein, he said, there is a great deal to learn from success stories, such as the progress made in removing lead from many environments, and in terms of understanding how science, politics, and public opinion can unite to produce change. At the same time, he suggested that the limited funding opportunities might bring some humility to the field of global health. He hoped that would translate into increased openness to collaborating across disciplines, involving communities more than just superficially, and communicating to the public at large about the importance of this work for improving public health locally and globally. As a final comment, he implored the community to go forward with a sense of urgency. “The problems we are facing are real, and while we have made progress, that progress is going to be undone unless we tackle the problems ahead of us with great urgency,” said Newman.
Disclaimer: This Proceedings of a Workshop—in Brief was prepared by Joe Alper and Keegan Sawyer as a factual summary of what occurred at the workshop. The planning committee’s role was limited to planning the workshop. The statements made are those of the rapporteurs or individual workshop participants and do not necessarily represent the views of all workshop participants, the planning committee, or the National Academies of Sciences, Engineering, and Medicine.
Workshop Planning Committee on Toward Understanding the Interplay of Environmental Stressors, Infectious Diseases, and Human Health: Robert Newman (Chair), The Aspen Institute; John Balbus, National Institutes of Health; Meghan Davis, Johns Hopkins University; Gary Ginsberg, New York State Department of Health; Margaret Karagas, Dartmouth College; Melissa Perry, The George Washington University; Joshua Rosenthal, National Institutes of Health; David Savitz, Brown University; John Vandenberg, U.S. Environmental Protection Agency.
Reviewers: To ensure that it meets institutional standards for quality and objectivity, this Proceedings of a Workshop—in Brief was reviewed by Kevin Elliot, Michigan State University; B. Paige Lawrence, University of Rochester; and Robert Newman, The Aspen Institute.
Sponsor: This workshop was supported by the National Institute of Environmental Health Sciences.
About the Standing Committee on the Use of Emerging Science for Environmental Health Decisions: The Standing Committee on the Use of Emerging Science for Environmental Health Decisions convenes public workshops to explore the potential use of new science, technologies, and research methodologies to inform personal, public health, and regulatory decisions. These workshops provide a public venue for multiple sectors—academic, industry, government, and nongovernmental organizations among others—to exchange knowledge and discuss new ideas about advances in science, and the ways in which these advances could be used in the identification, quantification, and control of environmental impacts on human health. More information about the standing committee and this workshop can be found online at http://nas-sites.org/emergingscience.
Suggested citation: National Academies of Sciences, Engineering, and Medicine. 2019. Toward Understanding the Interplay of Environmental Stressors, Infectious Diseases, and Human Health: Proceedings of a Workshop—in Brief. Washington, DC: The National Academies Press. doi: https://doi.org/10.17226/25493.
Division on Earth and Life Studies
Copyright 2019 by the National Academy of Sciences. All rights reserved.












