S
Summary
In the 20 years since publication of the landmark Institute of Medicine studies To Err Is Human: Building a Safer Health System and Crossing the Quality Chasm: A New Health System for the 21st Century many strategies have been employed to improve the safety and quality of health care in the United States. Improving the performance of the U.S. health care system to achieve the goals of better population health, enhanced patient care experiences, and lower health care costs depends in large part on clinicians, the health care professionals who provide direct patient care.1
Delivering safe, patient-centered, high-quality, and high-value health care requires a clinical workforce that is functioning at the highest level. However, there is growing recognition among health care system experts that clinician well-being, so essential to the therapeutic alliance among clinicians, patients, and families, is eroding because of occupational stress. The high rates of burnout reported among U.S. health care clinicians, and clinical students and trainees (“learners”), are a strong indication that the nation’s health care system is failing to achieve the aims for system-wide improvement.
Burnout is a syndrome characterized by high emotional exhaustion, high depersonalization (i.e., cynicism), and a low sense of personal accomplishment from work. Research shows that between 35 and 54 percent of U.S. nurses and physicians have substantial symptoms of burnout; similarly, the prevalence of burnout ranges between 45 and 60 percent for medical students and residents. Burnout among health care clinicians and learners has been most studied in the medical and nursing professions; however, a growing understanding of the epidemiology and etiology of the syndrome
___________________
1 See Chapter 2 for a discussion of the target population of clinicians in the report.
suggests that burnout among all types of clinicians and learners is a growing public health concern. The high rate of clinician and learner burnout is a strong signal to health care leaders that major improvements in the clinical work and learning environments have to become a national and organizational priority.
A growing body of research suggests that the changing landscape of the U.S. health care system—how care is provided, documented, and reimbursed—has had profound effects on clinical practice and consequently on the experiences of clinicians, learners, patients, and their families. Many mounting system pressures have contributed to overwhelming job demands for clinicians (e.g., workload, time pressures, technology challenges, and moral and ethical dilemmas) and insufficient job resources and supports such as adequate job control, alignment of professional and personal values, and manageable work–life integration. A chronic imbalance of high job demands and inadequate job resources can lead to burnout. The job demand–resources imbalance in health care is exacerbated by the increasing push for system performance improvement, which leads to greater administrative burden, production pressures, and shifts in financial incentives and payment structures; by technology implementation that hinders rather than supports patient care; by changing professional expectations; as well as by standards and regulatory policies that are insufficiently aligned with the delivery of high-quality patient care or professional values. Intensifying these and other health system pressures on the clinical workforce is the explosive increase in the amount of medical information and data collected and the growing demand for health care as the U.S. population ages, including care and services for chronic conditions and social care,2 in the face of an existing shortage of health professionals in many areas.
Burnout has high personal costs for individual workers, but it also has high social and economic costs for their organizations and for society as a whole. The personal consequences of burnout for clinicians and learners include occupational injury, problematic alcohol use, and the risk of suicide. In addition, career regret and sub-optimal professional development are other consequences experienced by learners. Stressors associated with burnout are also threats to professionalism, the fundamental ethical norms that are essential to the professional fulfillment of clinicians and learners and to the delivery of high-quality care. Clinician and learner burnout adversely affects the quality of patient care. Clinician burnout is associated with an increased risk of patient safety incidents and malpractice claims, poorer quality due to low professionalism, reduced patient satisfaction, and diminished and ineffective communication between patients and clinicians. Clinician and learner burnout also puts a strain on health care
___________________
2 Social care addresses health-related social risk factors and social needs.
organizations by increasing clinician absenteeism, presenteeism (working while sick), and turnover and by reducing individual productivity. These effects also have profound consequences for the adequacy of the U.S. health care workforce overall.
There is a strong imperative to take a systemic approach to burnout that focuses on the structure, organization, and culture of health care. A systems approach incorporates thorough knowledge of the stakeholders, their goals and activities, the technologies they use, and the environment in which they operate. Many different aspects of the health care environment have to work together in an integrated way to prevent, reduce, or mitigate burnout and improve professional well-being. To this end, the National Academy of Medicine’s Action Collaborative on Clinician Well-Being and Resilience (Action Collaborative)3 requested that the Board on Health Care Services of the National Academies of Sciences, Engineering, and Medicine (the National Academies) undertake a consensus study to examine the scientific evidence regarding the causes and consequences of clinician burnout as well as potential systems approaches to improving patient care by supporting clinician well-being (see Chapter 1, Box 1-3 for the complete Statement of Task). The National Academies appointed a committee of 17 subject-matter experts to address this task. Over the course of the 18-month study, the committee gathered evidence, reviewed and deliberated on that evidence, and developed recommendations on designing systems to reduce clinician burnout and foster professional well-being.
CONCEPTUAL FRAMEWORK
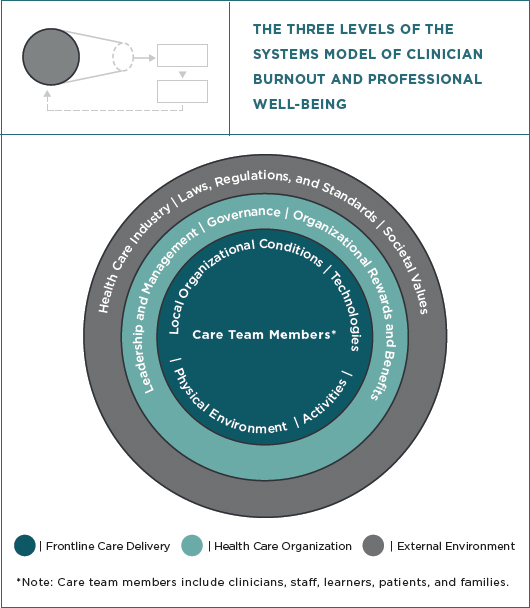
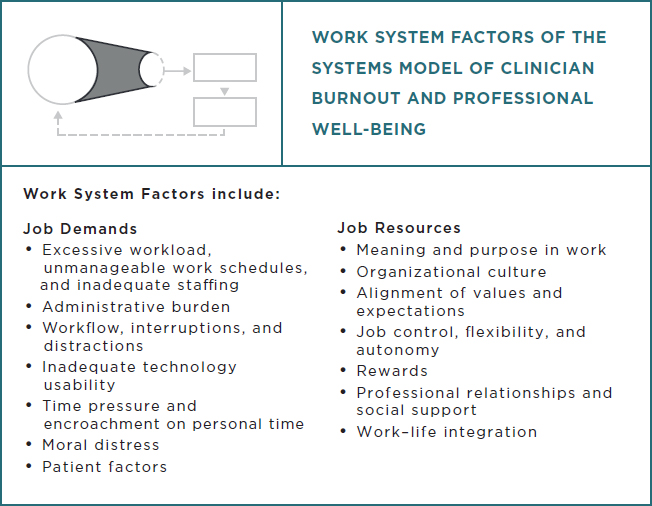
To achieve the dual objective of addressing burnout and well-being and improving patient care, the committee concluded that it will be necessary to consider clinician burnout and professional well-being in the context of a broader system.4 The committee’s framework for a systems approach to clinician burnout and professional well-being reflects theories and principles from the fields of human factors and systems engineering, job and organizational design, and occupational safety and health. The committee developed a model to articulate the systems aspects of clinician burnout and professional well-being (see Figure S-1), describe the interactions of the system levels (see Figure S-2), and identify the work system factors that influence burnout and professional well-being (see Figure S-3).
The committee’s systems model has three levels—frontline care delivery, health care organization, and the external environment—that together
___________________
3 See https://nam.edu/initiatives/clinician-resilience-and-well-being (accessed October 1, 2018).
4 The concepts articulated in the framework are intended to address burnout and professional well-being in health care clinicians and learners.
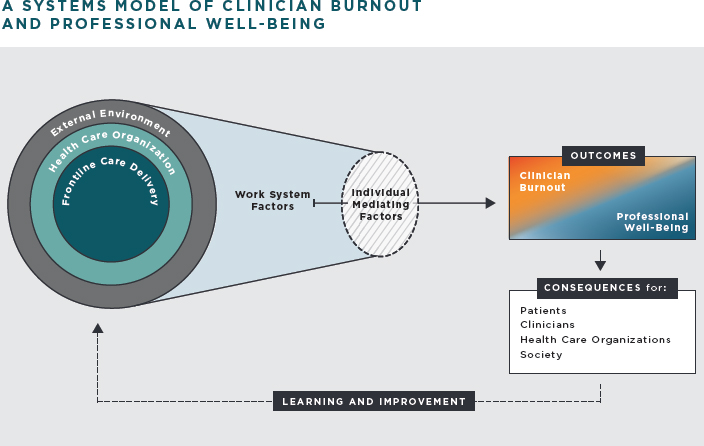
influence each other and the work system factors contributing to burnout and professional well-being. Other factors, unique to each individual (personality, coping strategies, resilience, social support), mediate the effects of these work system factors on clinician burnout and professional well-being. The outcomes of the work system factors on clinicians (i.e., burnout or professional well-being) have consequences for patients, clinicians, health care organizations, and society. To reduce clinician burnout and foster professional well-being, learning and continuous improvement processes are necessary for identifying, evaluating, and implementing effective improvements at all levels of the system.
Frontline care delivery is the “work system” where interactions among the care team, including clinicians, learners (i.e., trainees and students), patients and families, and support staff occur. Members of the care team perform activities using various tools and technologies according to the policies, procedures, resources, and infrastructure determined by the health care organization. Organizational conditions include how members of the care team perceive the organizational culture. The health care organization, the second level of the systems model, broadly applies to all types of care-providing entities and is composed of numerous elements, including organizational culture, payment and reward systems, the management of
human capital/human resources, leadership and management style, and organizational policies. The third level of the system model is the external environment, which includes political, market, professional, and societal factors. This level contains opportunities and constraints that influence decisions and actions at the health care organization level and the work done by clinicians at the frontline care delivery level.
Decisions made at the three levels of the system have an impact on the work factors that clinicians experience. Figure S-3 shows the work system factors, conceptualized as job demands and job resources that may contribute to clinician burnout and professional well-being when there is a chronic imbalance of these factors.
The different systemic factors that can cause burnout or adversely affect professional well-being are context-dependent—factors in one setting may not be present in another. The main drivers for burnout among learners are found in the learning environment and include grading schema, sub-optimal clinical experiences, inadequate preparation and support, supervisor behaviors, peer behaviors, and a lack of autonomy. Among clinicians, the job demands that contribute to burnout relate to workload and time pressure, the intrinsic aspects of clinical work (e.g., moral distress), and work inefficiencies (e.g., administrative burden, inadequate technology usability). Clinician’s job resources include tangible and intangible resources within the work environment, such as meaning in work, job control, and the availability of social support from peers and supervisors. The work system is influenced by the organization and includes job structure, local culture, values and expectations, leadership, and the amount of individual job control (e.g., flexibility or autonomy). Despite the many positive benefits, the negative impact of health information technology, including electronic health records, on care delivery, workflow, workload, and burnout is well documented. In addition, many factors within the external health care environment perpetuate the complex landscape of legal, regulatory, standards requirements, and expectations that influence the levels of stress in the everyday work of clinicians. Overall, information on clinicians’ experience of job demands and job resources may be used as feedback to change (or redesign) the system elements at each of the three levels of the system.
While many health care stakeholders are initiating important actions to address the burnout problem, there is little research indicating how effective they are in reducing burnout (and even less concerning their effectiveness in improving well-being or patient care). The committee’s systems framework emphasizes the identification of interventions aimed at tackling the critical factors contributing to burnout as a way of fostering an improved state of professional well-being while improving patient care. There is evidence that interventions focused on work organization can mitigate burnout; thus, health care organizations are a powerful determinant and have a critical
role to play in reducing clinician burnout. The evidence also indicates that individual-focused strategies may be beneficial and can be an effective part of larger organizational efforts but that, on their own, they do not sufficiently address clinician burnout.
The committee concluded there is a need to provide health care organizations with guidelines for designing, implementing, and sustaining professional well-being systems in their organizations in order to mitigate the multitude of factors contributing to burnout (see Box S-1).
The committee identified a number of gaps in the existing research literature and outlined an agenda with the following objectives:
- Build an epidemiologic foundation to better understand the prevalence of burnout across clinical professions;
- Define professional fulfillment and well-being to better understand how these constructs relate to enhanced personal, professional, and societal outcomes;
- Identify work system factors, learning environment factors, and individual mediating factors that contribute to burnout or that promote professional well-being;
- Better understand the implications of clinician burnout and professional well-being for patients, clinicians, learners, health care organizations, and society; and
- Evaluate system interventions designed to mitigate burnout and promote well-being across professions.
A multi-pronged approach involving all stakeholders to address research barriers is critical to realizing viable and sustainable strategies for improving professional well-being.
RECOMMENDATIONS
Based on its collective assessment of the available evidence, the committee concluded that taking action to address burnout requires a bold vision for redesigning clinical systems—one which focuses on the activities that patients find important to their care and which enables and empowers clinicians to provide high-quality care. Central to the committee’s vision for the way forward is an emphasis on the human aspects of care—putting patients, families, caregivers, clinicians, and staff at the center of focus; demonstrating compassion for patients, clinicians, and other care team members; and deriving professional goals and actions from the needs of patients. To lay the foundation for progress, the committee recommends that health care system stakeholders pursue the following six goals (listed in Box S-2) and associated actions as described below.
Goal 1. Create Positive Work Environments: Transform health care work systems by creating positive work environments that prevent and reduce burnout, foster professional well-being, and support quality care.
Health care organizations have a vitally important role in creating and maintaining positive work environments that clinicians find to be safe, healthy, and supportive and that foster ethical and meaningful practice. Health care organizations can enable the delivery of high-value health care by addressing burnout and its impact on the safety, health, and job satisfaction of the clinical workforce. Health care organizations should focus on adopting fundamental principles for redesigning work systems (see Box S-1) to prevent and reduce clinician burnout and foster professional well-being.
The active engagement of clinicians and patients is essential to the efforts of health care organizations to create positive work environments, including efforts to prioritize actions, procedures, and policies that will deliver the greatest value to direct patient care.
Recommendation 1A Health care organizations should develop, pilot, implement, and evaluate organization-wide initiatives to reduce the risk of burnout, foster professional well-being, and enhance patient care by improving the work environment. To accomplish this, they should:
- Commit their executive and board leadership to monitor and continuously improve the clinical work environment. Specifically, governing boards should hold organizational leaders accountable for creating and maintaining a positive and healthy work environment.
- Create and maintain, at the health care organization executive level, a leadership role and function responsible for improving and sustaining professional well-being across the organization. This leader and his or her team should strengthen coordination across all organizational programs, especially those that deal with patient care quality and safety and with occupational safety.
- Align the design of interventions to prevent and reduce burnout and promote professional well-being with desired organizational values such as respect, justice, ethical practice, compassion, and diversity.
- Assess the foreseeable impact of business and management decisions on the work environment. Specifically, health care organization leaders should evaluate how decisions may affect clinicians’ job demands (e.g., additional clerical and administrative burden on clinicians, competing demands on clinicians, unnecessary stress) and job resources (e.g., supportive managers and leaders, useful and usable technologies, effective teamwork), patient care quality and safety, and levels of burnout within the organization. Decisions and their implementation should be adjusted accordingly
- Hold leaders at all levels of the organization accountable for improving the work environment within their scope of responsibility.
Recommendation 1B To guide new systems that have been designed to promote professional well-being and patient care quality, health care organizations should adopt and apply the following principles that improve the work environment and balance job demands and job resources.
- Enhance meaning and purpose in work, and optimize workload and task distribution.
- Facilitate and incentivize interprofessional teamwork, collaboration, communication, and professionalism.
- Establish and sustain an organization-wide and unit-level culture that supports psychological safety and facilitates participatory decision making and peer support.
- Align incentives, compensation, and reward systems for clinicians and work units with organizational and professional values.
- Provide access to resources, such as coaching and adequate time for professional and personal development, to support clinicians in managing stress and adapting to change.
Recommendation 1C Health care organizations should routinely measure and monitor clinician burnout and ameliorate the work system factors that erode professional well-being. To accomplish this, they should:
- Use validated measurement tools to assess the extent of burnout in their organization and the potential contributory factors relevant to their system. It is essential to identify data capture strategies that minimize burden and protect clinicians’ privacy and address any
-
stigma or pressure that clinicians may perceive related to measurement or reporting.
- Accurately assess total workload and the complexity of the work expected of clinicians (including continuing professional education, maintenance of certification, required institutional learning modules, and work performed outside of scheduled hours). For clinicians in academic institutions, this assessment of work should include clinical work, research and scholarship, teaching, and service activities required to meet criteria for academic promotion. Clinical work involves cognitive processes, decision making, teams, and social interactions that need to be considered to optimize clinician workload so that it is sustainable.
- Obtain clinician and patient input to identify and eliminate documentation and other administrative burdens in the organization that are not mandatory and contribute little or no value to patient care. Assess opportunities to utilize clinical assistants or nonclinical staff to perform the work.
- Conduct reporting, at a minimum annually, overseen by the governing board, on the professional well-being of the organization’s clinicians, including the outcomes of interventions. These reports should be targeted internally, including to leadership, managers, and clinicians.
- Use the data to guide system-oriented efforts to prevent and reduce clinician burnout and improve professional well-being as part of a continuous learning and improvement process in which data are shared transparently within the organization.
Goal 2. Create Positive Learning Environments: Transform health professions education and training to optimize learning environments that prevent and reduce burnout and foster professional well-being.
Health professions educational institutions, affiliated clinical training sites, accreditors, and related external organizations have a responsibility to create and maintain positive learning environments that support the professional development and well-being of students and trainees (learners). Evidence indicates that there is a need to promote professional well-being and address burnout early in professional development. Health professions educational institutions should work together with health care organizations to ensure that efforts to prevent and reduce burnout are coordinated across the work and learning environments.
Recommendation 2A Health professions educational institutions and affiliated clinical training sites should develop, pilot, implement, and evaluate initiatives to improve the learning environment and support learner professional well-being. To accomplish this, they should:
- Commit their executive and board leadership to the improvement of the learning environment. Specifically, governing boards should provide the resources necessary to create and maintain a positive learning environment and then hold educational leadership accountable. At the executive level, educators should designate a leadership role and function responsible for improving and sustaining learner professional well-being across the organization and across the continuum of learners. These efforts should be coordinated with individuals charged with improving the clinical environment where learners interact with clinical teachers.
- Ensure that workload, rewards and incentives, and the professional development of faculty and other educators of health professional learners promote positive role model behaviors and the professional development and professional well-being of learners.
- Enhance the ability of learners to contribute meaningfully to patient care while learning, and implement strategies that build relationships among and between learners, faculty, and other health professionals with the intent to build social support and interprofessional practice.
- Create systems of learner evaluation that fairly evaluate competencies while mitigating undue stress and promoting a collaborative learning environment, including criterion-based grading and a consideration of pass–fail grading.
- Provide resources for learners to promote and support their own personal and professional well-being. Establish and sustain a system-wide culture that promotes help-seeking behaviors and supports psychological safety.
Recommendation 2B Health professions educational institutions and affiliated clinical training sites should routinely assess the learning environment and factors that erode professional well-being and contribute to learner burnout. The data should guide systems-oriented efforts to optimize the learning environment, prevent and reduce learner burnout, and improve professional well-being. Health professions educational institutions should:
- Use validated measurement tools to assess the extent of the burnout problem and the potential contributory factors relevant to their system. It is essential to identify data capture strategies that
-
minimize response burden, protect individual privacy, and address any stigma or pressure that learners may perceive related to measurement or reporting.
- Accurately assess the total clinical and academic workload expected of learners (including preparation for licensure examinations and required institutional and professional learning activities) with the goal of achieving a reasonable workload that is sustainable.
- Conduct at least annual reporting, overseen by the leadership of the health professions education institution and affiliated clinical training sites, on the professional well-being of its learners, including the outcomes of interventions taken to improve learner professional well-being. These reports should be targeted internally, including to leadership, learners, and faculty.
- Ensure that barriers to participation in professional well-being assessments are effectively addressed. It is essential for health professions educational institutions to protect learners’ privacy and address any stigma or pressure that learners may perceive related to assessment or reporting.
- Use the data to guide systems-oriented efforts to prevent and reduce learner burnout and improve professional well-being as part of a continuous learning and improvement process where data are shared transparently across learners’ health professions educational institutions and affiliated clinical training sites.
Recommendation 2C Accreditors, regulators, national educational organizations, health professions educational institutions, and other related external entities should partner to support the professional well-being and development of learners. To accomplish this, they should:
- Commit, at the highest level, to identifying, implementing, and continuously evaluating strategies that optimize learner professional well-being and development.
- Support the discovery and implementation of evidence-based approaches to reduce the risk of learner burnout and optimize learner professional well-being while simultaneously ensuring the appropriate development of competencies, skills, professionalism, and ethical standards.
- Engage and commit leadership at all levels to curbing learner educational debt, with such strategies as improving access to scholarships and affordable loans and building new loan repayment systems.
- Assess the foreseeable impact of decisions on learner professional well-being. Specifically, accreditors and administrators of licensure
and certifying examinations should evaluate how their policies may affect learner professional well-being and willingness to seek emotional support.
Goal 3. Reduce Administrative Burden: Prevent and reduce the negative consequences on clinicians’ professional well-being that result from laws, regulations, policies, and standards promulgated by health care policy, regulatory, and standards-setting entities, including government agencies (federal, state, and local), professional organizations, and accreditors.
Health care laws, regulations, policies, and standards in the United States are numerous and, as a whole, immensely complex, and imposed by many entities that are considered part of the external environment. The associated burden of the myriad requirements on clinicians is well documented and includes regulations and standards for the oversight of U.S. clinicians, specifically those addressing payment policies, clinical documentation, quality measurement and reporting, prescription drug monitoring, privacy rules and procedures, pre-authorization forms, and professional and legal requirements for licensure, board certification, professional liability, and health information technology.
Administrative burden is a barrier to quality care that diminishes patient care experiences and contributes to the risk of clinician burnout. Health care policy makers, regulators, and standards-setting bodies have a responsibility to identify and eliminate policies, rules, and processes that impede a clinician’s ability to perform productive work necessary for quality patient care and that negatively affect the clinician–patient relationship. These entities should engage clinicians and patients in the process to identify and eliminate health care laws, regulations, policies, standards, and administrative processes that contribute little or no value to patient care.
Recommendation 3A Health care policy, regulatory, and standards-setting entities at the federal and state levels, such as the U.S. Department of Health and Human Services’ Centers for Medicare & Medicaid Services and The Office of the National Coordinator for Health Information Technology, the National Quality Forum, state legislatures, professional boards, and departments of health, should systematically assess laws, regulations, policies, and standards to determine their effects on clinician job demands and resources as well as the effects on patient care quality, safety, and cost. To accomplish this, these entities should:
- Allocate the necessary resources to support assessment of the effects of regulations, policies, and standards on clinicians in various care settings. Formal assessment should be conducted both prior
-
to and following implementation in order to evaluate how the requirements affect clinician workload and whether they are redundant or conflict with other requirements. Regulations, policies, and standards should then be modified accordingly based on these findings.
- Apply human-centered design and human factors and systems engineering approaches in developing regulations, policies, and standards, including those related to payment and performance to minimize the potential risk for adverse effects on clinicians and patients.
- Periodically review laws, regulations, policies, and standards related to the clinical work environment for alignment and usability with new technology.
- Align licensure standards and enable broad license reciprocity for all clinicians regulated by states.
Recommendation 3B Health care policy, regulatory, and standards-setting entities, in conjunction with health care organizations, should appreciably reduce documentation requirements and adopt approaches to documentation and reporting that incorporate human-centered design and human factors and systems engineering approaches and that also are technology enabled. To facilitate this:
- Payers and health care organizations should promote the development and use of technology to streamline documentation for billing and quality reporting, with the goal of decreasing to the greatest extent possible clinicians’ workload and non-patient, care-related work.
- Professional certification and health care accrediting entities should coordinate efforts to align documentation requirements, streamline reporting, and eliminate redundant processes and requirements that contribute to unnecessary burden.
Goal 4. Enable Technology Solutions: Through collaboration and engagement of vendors, clinicians, and expert health information technology system developers, optimize the use of health information technologies to support clinicians in providing high-quality patient care.
Many challenges of health information technology (IT) are reported to affect clinician professional well-being, including problems with the usefulness and usability of health IT tools, their poor integration into clinical workflow, difficulty sharing information among clinical team members and settings, and limitations in supporting clinical decision making. Despite
nascent industry and regulatory efforts to improve health IT design and evaluation, many clinicians find these technologies excessively challenging and time consuming to use. Strategies are needed in which vendors, clinicians, health care organizations, regulators, and policy makers in the broader external environment can work together to address the current challenges and support the integration of new technologies and approaches with the overarching goal of improving patients’, caregivers’, and clinicians’ care experiences and outcomes.
Recommendation 4A Stakeholders should engage clinicians in the design and deployment of health information technology (IT), including electronic health records, using human-centered design and human factors and systems engineering approaches to ensure the effectiveness, efficiency, usability, and safety of the technology. For example:
- Regulators should use rigorous human factors usability and safety criteria to evaluate and certify health IT.
- Health IT vendors and health care organizations should design and configure systems to improve the clinical work environment, including attention to cognitive load and workflows that reduce the demand of clinical documentation and automate non-essential tasks.
- Health IT vendors, health care organizations, and regulators should closely monitor implemented technology for negative consequences and should have an existing mitigation plan to address them as they arise.
- Policy makers and organizational leaders should create incentives for, and lower barriers to, the development and implementation of new ideas, approaches, and technologies that have the promise of enhancing professional well-being as well as improving the quality of care.
Recommendation 4B Federal and state policy makers should facilitate the optimal flow of useful information among all members of the health care community through regulation and rule making. Health information sources should be shared efficiently, safely, and securely, including but not limited to electronic health records, electronic pharmacy records, digital health applications, medical devices, and quality data repositories.
Recommendation 4C Federal policy makers, in collaboration with private-sector health information technology companies and innovators and other relevant stakeholders, should develop the infrastructure and processes that
will lead to a truly patient-centered and clinically useful health information system. This would be an electronic interface that gives the entire care team, including the patient, the ability to collect and use timely and accurate data to achieve high-quality care. A major goal of this new health information system should be to allow clinicians to focus on optimizing patient and population health, while adjuvant processes and technologies derive, to the extent possible, the essential business, administrative, and research data necessary to deliver high-value care efficiently and effectively.
Goal 5. Provide Support to Clinicians and Learners: Reduce the stigma and eliminate the barriers associated with obtaining support needed to prevent and alleviate burnout symptoms, facilitate recovery from burnout, and foster professional well-being among learners and practicing clinicians.
Research shows that stigma (negative perceptions, attitudes, and discrimination) associated with seeking emotional and mental health help is pervasive in American society. Such stigma thrives in the health professions because of the culture and training, the perceptions of health professionals, and the expectations and responses of health care organizations, licensure boards, and other external organizations. Reducing stigma and eliminating barriers to help-seeking are critical to improving the professional well-being of clinicians and learners.
Recommendation 5A State licensing boards, health system credentialing bodies, disability insurance carriers, and malpractice insurance carriers should either not ask about clinicians’ personal health information or else inquire only about clinicians’ current impairments due to any health condition rather than including past or current diagnosis or treatment for a mental health condition. They should be transparent about how they use clinicians’ health data and supportive of clinicians in seeking help.
Recommendation 5B State legislative bodies should create legal protections that allow clinicians to seek and receive help for mental health conditions as well as to deal with the unique emotional and professional demands of their work through employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation.
Recommendation 5C Health professions educational institutions, health care organizations, and affiliated training sites should identify and address those aspects of the learning environment, institutional culture,
infrastructure and resources, and policies that prevent or discourage access to professional and personal support programs for individual learners and clinicians.
Goal 6. Invest in Research: Provide dedicated funding for research on clinician professional well-being.
The compelling evidence of the alarmingly high rates of burnout and its negative effects on the health care system and patient care requires the expansion and support of research and innovation in this area. Such support can be achieved through the collaborative efforts of government bodies and organizations charged with improving care quality and patient safety, improving the patient experience, reducing health care costs, and supporting the professional development of learners and clinicians in the health professions.
Recommendation 6A By the end of 2020 federal agencies, including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs, should develop a coordinated research agenda to examine:
- Organizational, learning environment, and health care system factors that contribute to occupational distress and threaten or promote the professional well-being of health care learners and practicing professionals;
- The implications of clinician and learner distress and degraded professional well-being on health care and workforce outcomes as well as personal outcomes; and
- Potential system-level interventions to improve clinician and learner professional well-being and help those with burnout to recover.
These federal agencies should commit funding to implement this research agenda. The amount of this funding should be commensurate with the magnitude of the problem and its impact on the health care delivery system. A particular area of focus should be the support of rigorous prospective empirical studies, including multi-center randomized controlled trials, of system-level interventions.
Recommendation 6B Federal agencies, including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S.
Department of Veterans Affairs, should pursue and encourage opportunities for public–private partnerships among a broad range of stakeholders, such as health professional associations, foundations, payers, health care industry, health care organizations, health professions educational institutions, and professional liability insurers, to support research on clinician and learner professional well-being and burnout. Organizations need to be willing to test, learn, and share in order to accelerate the pace of change. A public–private partnership should support the creation and ongoing management of a national registry of evidence-based interventions to facilitate research and innovation beneficial to every stakeholder with responsibility for eliminating clinician and learner burnout and improving professional well-being.
This page intentionally left blank.




















