The workshop began with a keynote address delivered by Admiral Brett P. Giroir, Assistant Secretary of Health at the U.S. Department of Health and Human Services (HHS), followed by a panel session that laid the groundwork for the rest of the day’s presentations and discussions. The panelists were John Auerbach, President and Chief Executive Officer of Trust for America’s Health; Dave Chokshi, Chief Population Health Officer for New York City Health + Hospitals; and Monica Bharel, Commissioner of the Massachusetts Department of Health. Discussions moderated by Daniel Polsky, Bloomberg Distinguished Professor of Health Policy and Economics at Johns Hopkins University’s Bloomberg School of Public Health, followed the keynote address and the panelists’ short presentations.
KEYNOTE ADDRESS
Admiral Brett P. Giroir began his presentation by noting that the nation’s spending on health care has not translated into better health for Americans. Though the United States currently spends 17.9 percent of the gross national product on health care—a number that far exceeds that of the other 35 members of the Organisation for Economic Co-operation and
Development (OECD)—U.S. life expectancy ranks 28th out of 36 OECD countries, while infant mortality ranks 33rd and suicide rate ranks 30th. He also pointed out that for the first time in decades, life expectancy of U.S. residents decreased in 2018.
Though the United States spends a bulk of its health care dollars on clinical care, access to medical care and the quality of care each accounts for only about 10 percent of an individual’s health outcomes, while social and economic factors determine some 40 percent of health outcomes (see Figure 2-1).
Research shows, in fact, that basic measures of health in OECD countries and among U.S. states are more closely and positively associated with social service spending than with health spending (Bradley et al., 2011, 2016). Giroir reminded the workshop attendees of the following:
- Forty-two percent of all U.S. cancer cases are tied to behavior and are thus preventable (Islami et al., 2018).
- Simple dietary changes could prevent at least half of the estimated 700,000 annual deaths from heart disease (Micha et al., 2017).
- The United States would save $117 billion in annual health care costs and eliminate 10 percent of all premature mortality if everyone were moderately active for 150 minutes per week (Piercy et al., 2018).
He noted, too, that some 60 percent of today’s 2-year-olds, if projections hold, will be clinically obese by the time they turn 35 years old (Ward et al., 2017), and that 75 percent of 18- to 24-year-olds cannot qualify for military service because of obesity, lack of fitness, educational background, or drug use (Christeson et al., 2015). One of the more shocking statistics Giroir said he learned upon taking the role of assistant secretary of health was that except for specific circumstances, zip code matters more than genetic code in terms of health outcomes (Dwyer-Lindgren et al., 2017) (see Figure 2-2). Moreover, his principal deputy informed him that this map has changed little if any over the past 30 years.
Giroir believes that a confluence of biological advances and the availability of policy options creates a unique set of opportunities to effect change with regard to the trajectory of U.S. health care spending. Research has shown, for example, social determinants can have long-lasting biological effects on health (Braveman and Gottlieb, 2014; Cockerham et al., 2017), and he believes this is a message the public needs to hear to disabuse it of the idea that social determinants are some fuzzy concept. Infection with Zika virus, for example, is both a medical condition and a condition of the cramped living quarters and poor sanitation that accompanies poverty. Similarly, hookworm infection, which causes chronic anemia and
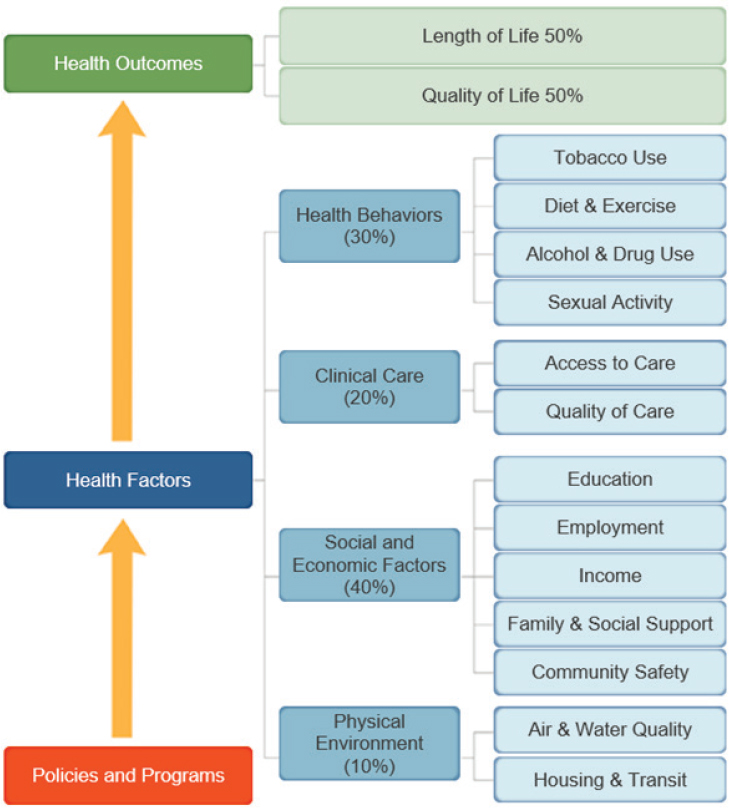
SOURCES: Presented by Admiral Brett P. Giroir, April 26, 2019, at the Workshop on Investing in Interventions That Address Non-Medical, Health-Related Social Needs. Reproduced with permission from the University of Wisconsin Population Health Institute. County Health Rankings & Roadmaps 2019.
delays in cognitive development, is endemic in some parts of the southern United States that lack modern sanitation. “Tell me where the investment should be for those children who are going to have a lifetime of infectious poverty,” said Giroir. Research has also shown that life experiences, including child abuse and even the educational level of the mother, can
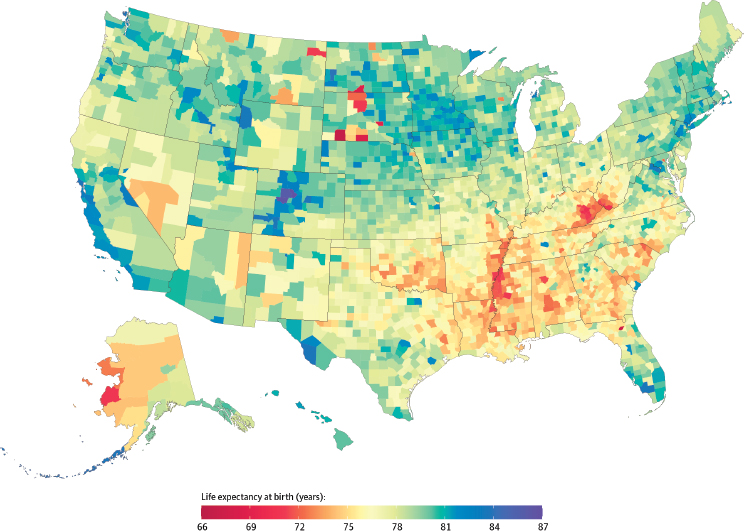
SOURCES: Presented by Admiral Brett P. Giroir, April 26, 2019, at the Workshop on Investing in Interventions That Address Non-Medical, Health-Related Social Needs; Dwyer-Lindgren et al., 2017. Reproduced with permission from JAMA Internal Medicine. 2017. 177(7):1003–1011. Copyright © (2017). American Medical Association. All rights reserved.
change an individual’s epigenetics over the long term (Kanherkar et al., 2014; Suderman et al., 2014).
Addressing the social determinants of health will be one of four overarching objectives in the upcoming Healthy People 2030 report, said Giroir. He also noted that one of four priorities for the Secretary of HHS, Alex Azar II, is to transform the nation’s health care system to one that pays for value, which will most certainly include addressing the social determinants of health as part of the value equation. Giroir emphasized how important it was for the workshop to begin assembling the theoretical and academic knowledge bases that will be required to create such a value-based agenda.
As part of this effort, the Centers for Medicare & Medicaid Services (CMS) announced on April 22, 2019, that it was rolling out a value-based reimbursement model that will affect 11 million Medicare fee-for-service
beneficiaries, 25 percent of primary care practitioners, and as many as 12 million individuals eligible for both Medicare and Medicaid. The focus of this model, explained Giroir, is on preventing disease before it occurs and progresses as it eases the connection of Medicare beneficiaries to primary care physicians, and it will give doctors the freedom, rewards, and tools to keep people healthy. The private sector, he said, has started moving in this direction, too. As an example, he cited Humana’s screening of more than 500,000 seniors for food insecurity and loneliness and the associated 2.7 percent reduction in “unhealthy days” Humana’s beneficiaries have experienced since this effort started in 2015.
Giroir concluded his keynote address by asking the workshop participants to answer two questions over the course of the day:
- Are there specific recommendations on how, where, and when to demonstrate the effectiveness of investments in the social determinants of health?
- How do we create a universal business case (and to whom) when the benefits of investing may be far removed from the effect on health or financial savings and dissociated from the people making the investment?
This second question, he said, bothers him a great deal, whether it arises in treating people for hepatitis C or screening people with HIV and providing them with state-of-the-art drug regimens, both of which have huge upfront costs but produce great societal savings in the future. “Often, the benefits are dissociated from the people making the investment,” said Giroir.
Discussion
Stacy Lindau from The University of Chicago began the discussion by suggesting that investments in addressing non-medical factors affecting health could be treated as an infrastructure investment, which would change the business model and ROI expectations. Giroir responded that both he and the Secretary of HHS are considering how to do that. Part of his job is to preach on a daily basis to senior administration officials that health is not just a medical care issue. He points out regularly that it is hard to exercise if the neighborhood is not safe and hard to eat a healthy diet and avoid obesity when one is food insecure.
Shreya Kangovi from the University of Pennsylvania raised the concern that many estimates for ROI are based on studies plagued by regression to the mean and she wondered to what extent decision makers are aware of this issue. Giroir replied that he was not aware of that problem
and hoped that the workshop would help him better understand this methodological issue. He noted that the Surgeon General is conducting a detailed study that will develop a set of business cases to support investments into health and the social determinants. Along the same lines, Karen DeSalvo from The University of Texas at Austin asked how HHS and the National Institutes of Health are thinking about building a strong, methodologically sound evidence base on interventions to address social determinants. Giroir replied that one reason for including in this workshop a session on research gaps was to understand where the needs are in developing just such an evidence base. He noted that HHS recently announced a $350 million project that will study four communities for 3 years to determine whether a comprehensive approach that includes housing and social services can reduce drug overdose rates by 40 percent.1
Elizabeth Marshall from the Society for Public Health Education asked Giroir if his office was working on addressing some of the social determinants that affect pregnant women, and he replied that HHS is taking a deep dive into maternal mortality and maternal health care. He noted that the department is broadening this effort to include the mother–child dyad.
Jeffrey Levi from The George Washington University asked if HHS is thinking about how it might invest in creating the community-based infrastructure and resources that health care systems can partner with to address the social determinants of health as part of CMS’s new value-based payment system about which Giroir spoke. While Giroir was not sure of the details, he said the administration’s across-the-board emphasis is on trying to find community-based solutions to health-related problems. Though not directly connected to the CMS payment initiative, Giroir said his office’s HIV/AIDS program is focused on community-based solutions and is investing $30 million in those solutions. Levi then pointed out that the Ryan White HIV program is an example of where the government invested over many decades in building the right infrastructure to address not just immediate health care needs but also social determinants. “It took an investment in infrastructure in every community across the country, and there needs to be a parallel effort if we are going to succeed more broadly in addressing social determinants,” said Levi.
Uche Uchendu from Health Management Associates commented that during her time at the U.S. Department of Veterans Affairs (VA), she and her colleagues connected social determinants with health care quality measures as part of the VA’s quality improvement initiatives. For example, blood A1C measures were connected to food insecurity and
___________________
1 Information available at https://www.hhs.gov/about/news/2019/04/24/hhs-factsheet-combating-the-opioid-crisis.html (accessed July 29, 2019).
walkability in a community. Connecting quality measures to social factors informs the practical management options provided by the clinical health care team. She also pointed to the importance of building bridges between the health care sector and communities to address the social determinants that health care systems are not well equipped to tackle. Giroir replied that the VA has done exceptional work on the social determinants of health, particularly in the area of veteran housing insecurity and homelessness. One advantage the VA has, though, is that it keeps its patient population for a long time, allowing it to recapture the investments it makes in the area of social determinants. Having said that, he noted that most everyone is going to be a Medicare beneficiary at some point, and as a result, there is a strong case to make for the federal government to make such investments.
TWO DIFFERENT BUT COMPLEMENTARY MEANINGS
To start his presentation, John Auerbach described two different concepts—(1) non-medical, health-related social needs and (2) social determinants of health—and the different approaches their solutions require. Solutions for non-medical, health-related social needs require “identifying and helping address the social and economic needs of patients.” Offering some examples, he listed helping patients find stable, safe housing; helping patients sign up for assistance from the Supplemental Nutrition Assistance Program (SNAP) or the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); helping patients connect to a medical–legal partnership; or helping patients get protection from violence or abuse. Non-medical, health-related social needs, he explained, can be resolved or addressed through referrals to various community organizations.
Addressing the social determinants of health requires a different approach. Solutions to social determinants of health require “changing the law or implementing a policy that affects an entire community.” His examples included significantly increasing affordable housing, improving economic or educational opportunities, or reducing racial and other discrimination. Social determinants of health are the root causes of non-medical, health-related social needs, and Auerbach said it is important to distinguish between these two different—but related—concepts because they require different approaches to address them. He shared a visual representation of how the social determinants of health and non-medical, health-related social needs lie on a continuum (see Figure 2-3).
He explained that upstream solutions address the social determinants or root causes of health disparities at the population level. Midstream solutions address non-medical, health-related social needs.

SOURCE: Presented by John Auerbach, April 26, 2019, at the Workshop on Investing in Interventions That Address Non-Medical, Health-Related Social Needs.
Downstream solutions are those medical interventions that occur in the clinic.
While it is important to work simultaneously at multiple levels to address non-medical social needs and social determinants of health, individual institutions, agencies, and sectors may focus on one particular level or context, said Auerbach. For example, health care organizations may choose to implement screening for non-medical social needs and provide in-house assistance with social services. However, those organizations are likely to work in partnership with, or even help establish, community-based organizations to provide various services outside of the health sector, such as food or housing assistance. Health care and community-based organizations may work together to advocate for changing laws or regu-
lations that affect the social determinants, such as a regulation requiring developers to designate 10 percent of the housing units they build to be affordable or to include retail space in a development that would house a grocery store.
The good news, said Auerbach, is that policy resources exist to make large, population-wide changes that would address social determinants of health and non-medical social needs (see Box 2-1). Moreover, it is possible to use these resources to improve overall social and economic conditions.
For example, the federal earned income tax credit provided $27 million in income assistance to 44,000 families in Vermont, reducing poverty levels in the state. He also noted that fair hiring regulations, such as state Ban the Box laws that require employers to consider a job candidate’s qualifications first, without the stigma of having checked a box on their job application denoting they had been arrested or convicted of a crime, can increase employment of those who have served time in jail or prison.
Though it may seem overwhelming to tackle policy and regulatory changes, Auerbach said there are policy resources available to help organizations with this task. For example, his organization released a report in February 2019 that includes 13 evidence-based policies that promote health and help control costs at the state level (Lustig and Cabrera, 2019), while the Centers for Disease Control and Prevention’s (CDC’s) Hi-5 (Healthy Impact in Five Years) initiative and the de Beaumont Founda-
tion’s CityHealth program both provide evidence-based and city- and community-level policy recommendations that organizations can use to foment change in their local communities that will improve health.2,3
Auerbach’s final comment was that there is no one solution to meet all of the non-medical social needs and social determinants that negatively affect health. “We need to mobilize multiple sectors, and they need to be around the table working together,” said Auerbach. He added that it is important that sectors outside of health care have the resources, beyond those provided by the health care sector and insurers, to invest in housing, combat segregation at the community level, and create economic security and quality educational opportunities throughout the community.
ADDRESSING HEALTH-RELATED SOCIAL NEEDS AT NEW YORK CITY HEALTH + HOSPITALS
Dave Chokshi started his presentation by recognizing that people have been working on the social determinants of health for decades. The U.S. community health center movement, for example, was rooted in the idea that health care alone is not enough and that it is imperative to address social determinants alongside of health care. Chokshi’s hope was that the workshop would consider how to move from addressing social determinants to addressing issues of social justice (see Figure 2-4).
In his view, accepting that the social determinants are root causes of many health issues is the first step in a trajectory linking the concepts of social needs, social services, and social care toward social justice. Ultimately moving from social determinants to social justice requires taking on structural inequities such as racial discrimination, mass incarceration, and poverty.
To provide some context to how his organization thinks about social determinants of health, Chokshi noted that it is the public health care system for New York City, caring for more than 1 million culturally and ethnically diverse patients across all five boroughs. It accounts for nearly half of the city’s mental health inpatient admissions and alcohol/detox inpatient admissions. Tens of thousands of its patients do not have a home, thousands are considered “high need,” and hundreds of its patients spent more days in the hospital than out of it over the past year.
New York City Health + Hospitals’ strategy for addressing the social determinants, based on CMS’s Accountable Health Communities model
___________________
2 Information available at https://www.cdc.gov/policy/hst/hi5/index.html (accessed May 15, 2019).
3 Information available at https://www.debeaumont.org/programs/cityhealth (accessed May 15, 2019).
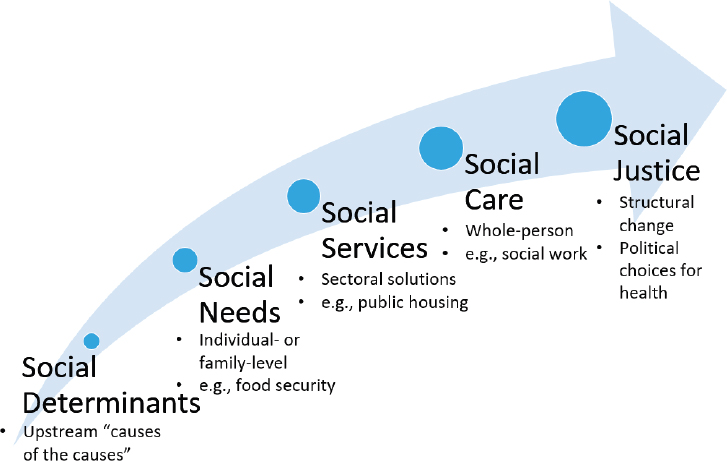
SOURCE: Presented by Dave Chokshi, April 26, 2019, at the Workshop on Investing in Interventions That Address Non-Medical, Health-Related Social Needs.
(Alley et al., 2016; Gottlieb et al., 2017a; Tipirneni et al., 2015)4 has four key tenets: raise awareness among providers of their patients’ social needs, provide assistance for patients, align services and accessibility, and advocate for improved services and supports for its patients. The key domains in which the organization is working to better serve its patients include housing stability and quality, food security, legal services, and income support. In the legal services domain, for example, New York City Health + Hospitals has established one of the largest medical–legal partnerships in the nation with the New York Legal Assistance Group to deal with a range of issues, including immigration, housing, employment, and other issues that can adversely affect health. Specific examples of what this partnership tackles include preventing eviction, creating Permanently Residing Under Color of Law status as a pathway to Medicaid eligibility, helping with Social Security disability appeals, handling a reasonable accommodation in the workplace, and processing visa or other applications for family members who want to serve as organ donors for a patient.
___________________
4 Information available at https://innovation.cms.gov/initiatives/ahcm (accessed May 15, 2019).
This medical–legal partnership also provides a channel for advocacy and for addressing proposed changes in laws and regulations such as the proposed public charge rule that might exacerbate unmet social needs.
MOVING HEALTH CARE UPSTREAM IN MASSACHUSETTS
Monica Bharel noted that in addition to being commissioner of Massachusetts’s Department of Public Health, she is a primary care physician who has spent more than 20 years trying to improve her patients’ health from a medical perspective only to realize that their social needs and social determinants of health far outweighed the capacity of her efforts to help them achieve health. She then described the model she and her colleagues are following to address the social determinants of health, one that starts by placing a deliberate focus on social determinants and health disparities. The model calls for generating and using data, as well as making it available to researchers, the press, and the general public, to drive initiatives that target disparities and improve health outcomes. Health equity is embedded in everything her department does.
As an example of how this model is put into practice, Bharel described the Massachusetts Determination of Need (DoN) program.5 DoN, also known in some states as a Certificate of Need, is a legal construct regulated by the Department of Public Health. It requires that investments made on improvements in the health care system must go through a determination of need and public health valuation. Massachusetts’s regulations requires DoN applicants to set aside 5 percent of capital expenditures for addressing state-defined health priorities through community-based health initiatives that engage the community to address social determinants of health. The department’s health priorities focus on violence, the social environment, housing, employment, education, and the built environment to tackle those areas that the state’s mortality and morbidity data indicate are the highest areas of inequity: mental health and wellness, homelessness and housing stability, substance use disorder, and preventable chronic disease. The DoN program also requires applicants to include plans for addressing structural racism in their communities.
Bharel explained that Massachusetts has deliberately linked its DoN process into the community health improvement plans required every 3 years from all not-for-profit health systems to influence what goes into those plans. In fact, the Massachusetts Attorney General now requires each not-for-profit health system to report on how they are addressing her department’s health priorities.
___________________
5 Information available at https://www.mass.gov/determination-of-need-don (accessed May 15, 2019).
As an example of an early success, Bharel described Boston Medical Center’s community health investments through a social impact fund to build affordable housing and provide a zero-interest loan to build a grocery store in a community in which food insecurity is common. Boston Medical Center has also put money toward an innovative community-empowering housing stability fund. More recently, all 13 of Boston’s hospitals have come together to produce a unified community health needs assessment and community health improvement plan that stands to reduce duplication of efforts and waste of resources. Two other hospitals have also chosen to invest in the same project, enhancing the power of that project, said Bharel.
DISCUSSION
Session moderator Daniel Polsky began the discussion period by saying he heard clearly that the health sector, community, and regulatory environment can complement each other in efforts to address social needs and social determinants of health. His question to the panel, then, was: if the health sector investments that subsequent workshop sessions would tackle are to thrive and have a strong return on investment, what would they recommend the assistant secretary’s office to focus on going forward?
Auerbach replied that he would make affordable housing a priority area given that evidence from multiple sources show that housing insecurity is the most common impediment to good health. He added that providing affordable housing will not be enough without providing wraparound components to help individuals who have a history of housing insecurity or chronic homelessness, for example, and to create safe, walkable neighborhoods and ensure healthy food is accessible to those living in affordable housing.
Bharel suggested creating mechanisms to help bring together the health system and community-based social services and to establish templates that would guide state efforts to better account for how community benefit funds are spent. Toward that end, Auerbach proposed creating a fund that CDC could use to provide a grant that each state and large city would use to create a social determinants unit headed by someone who can connect multiple stakeholders and hold them accountable for how they are spending community benefit funds. Chokshi agreed that creating partnerships will be critical for promoting collective action in a community. He also pointed out that the health care sector and other social service sectors, such as the criminal justice system, have a great deal of overlap in the people they serve, so it may be possible to pool resources from across sectors to address social needs and social determi-
nants of health. Auerbach suggested establishing a committee comprising leadership of every federal agency that has some connection with health, including the U.S. Department of Housing and Urban Development and the U.S. Department of Education.
Responding to a question from Marilyn Lynk of the Adventist HealthCare Center for Health Equity and Wellness, Bharel explained that the 5 percent set-aside for community health benefits is separate from any community benefit funds a health system might also be spending. Between 2015 and spring of 2019, that 5 percent added up to more than $143 million in obligations going to communities. She also explained that the Boston-wide community health assessment is a work in progress and that the participating hospitals are still figuring out how their efforts can be synergistic with one another. The 13 hospitals are not pooling their funds, though individual hospitals can decide to work together on a project when it meets both of their communities’ health needs.
Alexandra King from the Community Transportation Association commented that she supported the idea of creating a federal office that would foster cross-sector collaborations and pointed out that other sectors are already doing this. The U.S. Department of Transportation, for example, has a coordinating council on access and mobility that includes representatives from multiple agencies. She then asked the panelists for recommendations on how her organization, which represents rural and small urban specialized public transit providers, could get a foothold in the health care sector. Chokshi replied that health care can be hard to break into and that this is something that needs to be fixed. He suggested pitching these types of services as a way to address imperatives under value-based payment, an argument that he said was particularly germane for transportation interventions. He also recommended approaching the population health or social determinants group in a health system, if one exists. Auerbach noted that CMS has released new guidelines that include the option of paying for transportation for non-medical visits, such as to go to the grocery store, as well as interventions to address other social needs.
Genevieve Kenny from the Urban Institute asked Bharel if her department was intending to identify opportunities, challenges, and potential effects of repurposing and dedicating funds in a more community-centric and forward-looking way. Bharel replied that assessment of impact is going to be challenging because the money is going out to the community, and she wondered if the roundtable might recommend increasing resources for assessment as a means of answering questions about ROI. Her department will be asking for annual reports on community health investments that include data and statistics, but because this is a statewide program, there will not be a control group within Massachusetts.
The final comment in this session came from Lawrence McNeely with the American Diabetes Association, who noted that bending the curve for type 2 diabetes, for example, will require taking action early in life, which means thinking about what happens in the family unit, both during pregnancy and in the early years of life. This is a collective action problem that will require long-term investments, and he wondered who will provide those investments. Chokshi acknowledged that securing long-term investments is tough and proposed looking for places where the incentives align to make those investments, develop an evidence base, and then drive change more generally.
















