2
Building a Health Workforce for the Future: Lessons from a MultiStakeholder Statewide Initiative1
Kevin Barnett from the Public Health Institute and the California Health Workforce Alliance delivered the keynote address. Barnett opened by explaining that he began working on the issue of health workforce diversity in California 16 years ago and had previously participated in an Institute of Medicine committee led by Brian Smedley that produced a report on increasing the diversity of the health professions (IOM, 2004). That study explored the topic of holding health profession educational institutions responsible for building a diverse health workforce in the future.
Following that process, Barnett and his colleague Jeff Oxendine launched an initiative called Connecting the Dots, which had the goal of developing a comprehensive strategy to build the health workforce of the future. The project was supported by The California Endowment and was completed in 2008. Since then, Barnett and colleagues have convened diverse stakeholders across California, including employers, academic institutions, and advocates, to identify ways to advance the strategy.
Barnett recounted that in 2017, he and Oxendine were approached by the five largest foundations in California, which asked if they were interested in creating a comprehensive health workforce master plan, which he had recommended be developed back in 2005. The five foundation funders included the Blue Shield of California Foundation, The California
___________________
1 This section summarizes information presented by Kevin Barnett from the Public Health Institute and the California Health Workforce Alliance. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
Endowment, the California Health Care Foundation, The California Wellness Foundation, and the Gordon and Betty Moore Foundation. He noted it was significant that the five foundations that supported the work have slightly different priorities and emphasis, but they came together to support a common goal—an exemplary type of philanthropic collaboration.
Barnett’s presentation described the process used to develop this plan, beginning with the foundational questions that were addressed as part of the project:
- What are key gaps in the health workforce pathway?
- What is a vision to meet workforce needs that will improve population health?
- Why is health workforce diversity essential to improving population health?
- How are other sectors crucial to improving population health?
- What is a holistic way to approach health workforce development?
- Who has a role in building the health workforce of the future?
The questions yielded the charge of the newly formed commission, which included developing a strategic plan, creating implementation strategies, leveraging existing efforts, and engaging stakeholders (see Box 2-1).
Barnett pointed out it was important for the commission to think both in the short term about providing access to clinical health care services, and in the long term about addressing the real drivers of poor health. The
commission had to consider legislative and executive branch solutions and ways that all sectors could come together to address the issue. The commission also had to secure commitments for effective plan implementation that went beyond simply developing a report or list of potential solutions. Key elements noted to drive the process included dialogue, rationale for data, and evidence.
The commission had three core areas of focus, which were the topics that it determined were most important and urgent: (1) primary care and prevention, (2) behavioral health, and (3) healthy aging and care for older adults. Other issues could be added later as needed. The commission was concerned with how to build a workforce of the future that reflected California’s increasingly diverse communities. As Barnett explained, the overriding issues were the misdistribution of health professionals to serve rural and disadvantaged urban communities and the role of technology in driving it.
Barnett next described some of the challenges faced in California, which he sees elsewhere in the country as well. As he explained, in the next 10 years, the state is expected to have 41 percent fewer psychiatrists than needed and a shortfall of more than 4,000 primary care clinicians and up to 600,000 home care workers. He provided examples of some of the potential drivers. For example, Latinx people represent approximately 40 percent of the state’s population but only 7 percent of physicians, contributing to the 7 million Californians—primarily people of color—who live in areas of health profession shortage. In addition, California’s provider–population ratios, particularly in inner-city and rural areas, are only about half the federal recommended levels. Compounding the situation is that one-third of practitioners and nurse practitioners (NPs) are over age 55 and are expected to retire within 10 years. Barnett noted that these statistics are even more dire in rural areas.
Barnett also provided similar statistics regarding the public health workforce. He explained that more than 60 percent of senior leadership of public health agencies is eligible for retirement. He added that more than 95 percent of the funding for the state’s public health department is categorical.
Barnett provided some statistics regarding California’s aging population to illustrate the extent of the problem and the importance of acting. He explained that an additional 4 million Californians will reach retirement age by 2030, almost a 90 percent increase from 2012. Barnett was particularly struck that a large percentage of these people live alone, implying that there may be additional challenges in ensuring that they receive the care they need. He added that more than half of these individuals rely on Social Security for more than 80 percent of their income.
Barnett also highlighted challenges with access to behavioral and mental health services, as emergency department visits related to mental health disorders increased by more than 50 percent nationally between 2006 and 2013.
Barnett sees similar challenges with provider training cost and capacity. Barnett explained that with 60 percent of California’s medical students attending school out of state, California relies on other states to educate its physicians and on them choosing to return to California afterward. However, he noted that many do not come back due to California’s high cost of living and other factors. The high cost of medical education and the higher prestige of specialties versus primary care also drive many students toward specialties. Barnett noted that California has one of the most extensive teaching health center graduate medical education training programs in the country, with six federally qualified health centers (FQHCs) providing this training. However, Barnett added, the providers that run these programs are often already stretched thin and take additional time away from clinical care to support their students.
Barnett also described challenges related to the social determinants of health. The homeless population in California has increased more than 50 percent in the past 5 years, with nearly one-quarter of the homeless population in the United States, or close to 60,000 people, living in Los Angeles alone. That has led to a 12-year waiting list for Section 8 housing and a need for an additional 1.5 million units of rental housing. He explained that close to 40 percent of the state’s population lives at or below 150 percent of the California Poverty Metric, which is based on the federal poverty level but increased to account for the higher cost of living in California. Barnett also explained that while there is a commitment to providing access to preschool, the state falls short in doing so. He noted that this is important because lack of education early in life “establishes the circumstances under which it is difficult for many of these children to pursue career and health professions, as well as an income that will support them and their families.”
An additional challenge is that California is 49th in the country in reimbursement under MediCal, the state’s Medicaid program. Providers not tied to an FQHC provide services under MediCal at highly discounted rates. Technology is also not equitably distributed across the state. Barnett explained that the health care delivery system and its linkages do not currently have the capacity to provide and extend the reach of the provider population to address these issues in low-income communities. He commented that in the future there should be an increased investment in K–12 education.
Barnett next spoke about the California Future Health Workforce Commission’s structure and processes. The 24-member commission was co-chaired by Lloyd Dean, chief executive officer of Dignity Health (now
CommonSpirit), and Janet Napolitano, president of the University of California. Most of the other commissioners were decision makers who could provide influence and command resources, including respected chancellors and presidents of higher education institutions in the state and State Senate and State Assembly health committee chairs. There was also a 40-member Technical Advisory Committee (TAC) made up of leaders and experts in the workforce arena who understood the issues and could provide insights as the process moved forward. Committee members were organized into three subcommittees, each addressing a priority area. Between September 2017 and January 2019, the commission met seven times; the TAC also met during that time.
Barnett explained that as a part of the process, the commission also conducted a statewide survey to gather input on an extensive set of draft recommendations. As of April 2018, there were 177 recommendations, which were reduced to 27. On January 15, 2019, the commission adopted the final report with its 27 recommendations (California Future Health Workforce Commission, 2019).2 Ten of them were identified as top priorities for implementation. Barnett noted that the commission is actively engaged in promoting the public report.
Barnett next described certain elements of the commission’s deliberative process. He emphasized that the commission spent a significant amount of time initially “blue sky visioning,” asking questions such as “Where do we want to go? … Where do we want our institutions to be? What kinds of transformation do we want? What [is that] going to look like by 2030?” Other elements included identifying and analyzing problems, defining success and end products, establishing strategies, engaging stakeholders, analyzing and refining strategy, developing recommendations, conducting impact assessments, and selecting top recommendations.
Barnett also described some highlights of the process used to develop the recommendations (see Figure 2-1). The subcommittees conducted an initial review of information and brought key takeaways to the TAC for its input and then to the commission for refinement. He noted that the commission co-chairs played a particularly pivotal role in establishing the final priorities near the end of the process.
The commission’s final recommendations included three main strategies and reflected the need for a comprehensive approach:
- Strategy 1, “increase opportunities for all Californians to pursue health careers,” was focused on how to create opportunities early
___________________
2 The Commission’s full report, recommendations, and impact statements are available at https://futurehealthworkforce.org (accessed May 10, 2021).
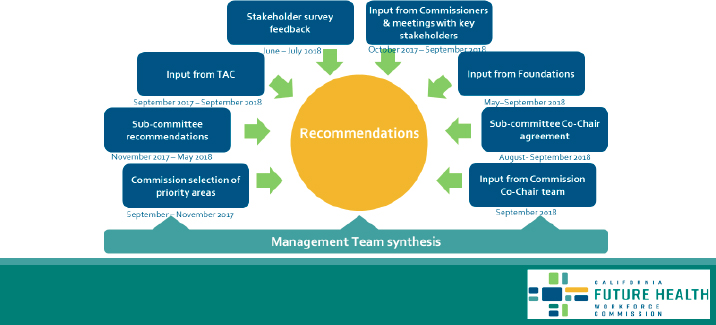
SOURCE: Barnett presentation, March 22, 2019.
- on in careers and build the health career pathways that provide opportunities to pursue higher education.
- Strategy 2, “align and expand education and training to meet Californians’ needs,” referred to necessary changes in the higher education process.
- Strategy 3, “strengthen the capacity, effectiveness, and retention of the health workforce,” was related to building the capacity and effectiveness of the current workforce to better serve communities (see Box 2-2).
Barnett next shared the commission’s recommendations for achieving each of the three main strategies, highlighting the top priorities (see Box 2-2). He emphasized the broad spectrum of recommendations and synergistic linkages between many of them. As he noted, some recommendations may be related to K–12 education and some to higher education, but all are focused on equity and addressing the underinvestment in rural and inner-city areas and underserved populations. With respect to education and training needs, Barnett noted an emphasis on drawing people from underserved communities, particularly communities of color, and supporting them in returning to and practicing in these communities after their training.
Barnett mentioned that the commission largely focused on delivery of clinical services. He explained that because there had been pent-up demand over several years to address access to primary and behavioral health care, those issues took precedence and were prioritized. However, he pointed out that scaling engagement of community health workers
(CHWs) and peer providers was identified as a top priority. Subcommittees and other leaders on the issue were also convened to develop this recommendation. Barnett explained that while there is “a fairly extensive network of promotores and CHWs in California, for the most part, the engagement of these workers by … mainstream providers is relatively limited; … their roles are relatively circumscribed.” Within this recommendation, Barnett pointed to “significant emphasis on understanding the comprehensive role CHWs could play not only in managing the care of individual patients but also working in and with communities to … begin to address the drivers of poor health, including working in the areas of policy advocacy.” He highlighted relevant issues, such as quality of housing and indoor environmental factors.
Barnett described a few other specific recommendations of the commission, including the recommendation to build the capacity of local public health agencies to support collaborative community health improvement. As he explained, that recommendation reflected a commitment to shared ownership and involved the state establishing a fund and making part of it available to match money provided by local hospitals and health systems. The funding could be used to engage someone with epidemiological expertise, preferably social epidemiological expertise, to connect the “parallel play” of each health care provider’s community benefit programs and activities, work toward focusing and aligning these efforts in communities with inequities, and provide accountability for making progress on addressing the priority issues.
Barnett explained that the recommendations reflect the overall commitment of the commission to address changes to not only the health care system but other sectors, including the community development sector, and to establish relationships between health care and other sectors. Important steps in developing the recommendations involved budgeting, conducting impact assessments, and considering where available data may be limited.
In closing, Barnett described next steps for disseminating and beginning to implement the commission’s recommendations. He noted that there would be an upcoming hearing, presentations to State Senate committees, and possible introduction of state legislation to address some of the recommendations. The five foundation funders are also considering ways to provide continued support for facilitation, monitoring, and ensuring that state infrastructure is sufficient to move the process forward. Employers and academic institutions in California are also being asked to consider their role in the process, in terms of the allocation of resources and their priorities to reflect the report recommendations.
DISCUSSION
Following Barnett’s presentation, there was a brief discussion with the audience. Donna Grande from the American College of Preventive Medicine asked Barnett for his top recommendations for congressional action in the next 3–5 years. Barnett noted that one priority is increasing investment in K–12 education in low-income communities. He elaborated by stating that increasing diversity in the health workforce requires early investment in pre-K education, targeted outreach and engagement, and support of people in low-income communities. He also pointed to the maldistribution of resources in K–12 education, with people in middle-class and affluent communities providing additional support to schools in low-income communities. Barnett believes this has led public schools to become “the most segregated institutions in our communities.”
Barnett noted that a second priority is moving from the “legacy model of health care delivery” to “fully integrating the social determinants of health into all … health profession education institutions, not as a course but as an ongoing part of the education process.”
Barnett suggested that an additional priority could be targeted training in communities and support systems for more providers to practice in rural and inner-city communities. He recommended substantial increases in funding for government public health and other entities that move away from categorical program silos and provide for more dynamic collaboration with a broad spectrum of stakeholders.
Sanne Magnan asked whether the committee discussed changing workforce needs related to baby boomers and the increase in lay health workers, and how to capitalize on these trends to address population health improvement. Barnett responded by explaining that the increase in home health care workers was addressed in several of the commission’s recommendations. In addition, the committee recognized that many retirees are still healthy and want to support population health improvement through strategies such as working in home care or mentoring young people. Magnan also noted that she appreciated Barnett’s emphasis on the diversity of the health care workforce, including not only primary care physicians but also NPs, psychiatrists, and CHWs. In response, Barnett pointed out that the commission’s recommendations included a strong emphasis on NPs, and work is under way to provide NPs with full practice authority, which they have in 22 states, including California. His group also discussed physician assistants playing a critical role in the California health care workforce, but this was not addressed in the commission’s report. Points made by the keynote speaker are highlighted below (see Box 2-3).
This page intentionally left blank.










