3
Barriers to Integration
The following sections outline nine barriers brought up in the committee’s search of the literature and during interviews with 11 programs seeking to integrate opioid use disorder (OUD) and infectious disease services. As discussed in Chapter 1, interviews were conducted to obtain information about the program’s history of integrated services, their current services provided and model of care, major barriers to integration, and the clinical consequences of integration, when available. As the following sections make clear, the primary barriers to integration for many programs were typically at the federal, state, or local policy levels.
PRIOR AUTHORIZATION POLICIES
Medicaid funds a significant proportion of buprenorphine prescriptions for treating OUD (Ducharme and Abraham, 2008; Stein et al., 2012). Before generic formulations of buprenorphine were available, it was relatively costly. To avoid diversion at high doses (Clark and Baxter, 2013; Lofwall and Havens, 2012) and contain costs, Medicaid administrators at the state level introduced measures to limit prescriptions (SAMHSA, 2018a). While states have increasingly adopted coverage for medications for opioid use disorder (MOUD), there has been a concurrent increase in policy measures to limit their use (Burns et al., 2016). This is typically accomplished through several mechanisms, such as not including buprenorphine on a preferred drug list, requiring concurrent psychosocial treatment in order to prescribe MOUD, instituting quantity-level limits, or
requiring step therapy (SAMHSA, 2018a). State and private insurers vary in their use of these mechanisms (Clark et al., 2014; Rinaldo and Rinaldo, 2013). One such measure—which encompasses many of the benefit design requirements mentioned above and is used by both public and private insurers—is prior authorization (Mark et al., 2014).
Prior authorization varies by state (Andrews et al., 2018) but requires obtaining approval from the insurer to prescribe buprenorphine to a patient. A provider may be required to prescribe doses on the lower end of the therapeutic range (Accurso and Rastegar, 2016; DHCF, 2016), demonstrate that a patient has not met a lifetime or annual limit on their prescriptions (Rinaldo and Rinaldo, 2013), or prescribe a particular formulation or route of administration (e.g., sublingual versus implantable) (Weber and Gupta, 2019). Gaining prior authorization is an impediment by definition, as it raises the administrative burden and delays providing the medication. As is described below, prior authorization exacerbates the challenge of sustaining patient willingness for OUD treatment. Notably, as coverage for buprenorphine has increased over time, prior authorization requirements have also increased (Hartung et al., 2019).
In 2018, the Centers for Medicare & Medicaid Services (CMS) reported that it would not approve Medicare Part D formularies that require prior authorization more than once per year for at least one formulation of buprenorphine, which decreased the number of programs with prior authorization policies (Mark et al., 2019). Still, as of 2019, a majority of state Medicaid programs required some prior authorization procedures for buprenorphine (or the commonly used mixture of buprenorphine and naloxone) (SAMHSA, 2018a; Weber and Gupta, 2019).
Seven of the 11 programs interviewed for this study mentioned prior authorization as a current or past barrier to providing quality, timely care to patients with OUD. Prior authorization represents a significant barrier to creating integration between OUD and infectious disease care, as continued injection of opioids—as well as co-occurring risky sexual behaviors—maintains a high risk of infectious diseases (MHAF, 2018).
There were several themes across the programs mentioning prior authorization as a barrier. The first was that it is a time-consuming or burdensome process. That is, providers or staff spend significant time to obtain prior authorization from payers, and this limits staff time spent engaging in patient-centered care. To overcome this barrier, programs (such as the Greater Lawrence Family Health Center) rely on skilled staff to obtain prior authorizations.
Another theme was that prior authorization requirements are not legitimate from a medical perspective. Health professionals would prefer to have choice and control over how to treat individual patients, and if a payer only allows one particular formulation to be prescribed without
prior authorization, this limits their ability to deliver individualized or patient-centered care. As an example, while the District of Columbia Medicaid program has recently loosened prior authorization requirements, it still requires that providers obtain special approval if they provide more than 24 mg/day of buprenorphine (DHCF, 2016). This is despite the fact that evidence suggests treatment retention is improved at 32 mg/day (Hser et al., 2014).
Some programs suggested that having at least one medication formulation available without prior authorization eases the time-consuming process. Several of the programs interviewed are located in states where prior authorization requirements were recently lifted or eased (Indiana, Louisiana, New York, and Washington, DC), and these programs commented on how this has improved their practice and ability to prescribe necessary medications to their patients.
As revealed in the case studies, providers believe that prior authorization requirements produce unnecessary administrative burden that hinders timely care and prevents the delivery of evidence-based treatment to patients with OUD. There is evidence that prior authorization is correlated with a reduced overall availability of MOUD among treatment programs. In a 2019 study, Andrews and colleagues (2019) found that only 17 percent of drug treatment programs in states with prior authorization requirements were prescribing buprenorphine for OUD. This is relative to 43 percent of programs in states where no prior authorization was required to prescribe (Andrews et al., 2019). Fewer medications available to treat OUD translates into increased drug use and therefore increased risk of infectious diseases at the population level.
States that have already lifted prior authorization rules on MOUD have done so for this reason. For instance, Governor Phil Murphy of New Jersey removed the state Medicaid’s prior authorization requirements because they were viewed as an administrative barrier to treatment (New Jersey also announced plans to increase accessibility to MOUD through several other mechanisms) (Kultys, 2019). In Pennsylvania, an agreement was reached between the state and the seven largest health insurers to loosen prior authorization requirements; at least one formulation of buprenorphine-naloxone, methadone,1 oral naltrexone, and nasal naloxone would be covered under insurance without prior authorization. The stated goal of this agreement was to remove barriers to MOUD (Rementer, 2018).
___________________
1 Unlike buprenorphine and naltrexone, methadone can only be dispensed through a SAMHSA-certified opioid treatment program, and federal law requires that patients undergoing treatment in this setting must receive “medical, counseling, vocational, educational, and other assessment and treatment services, in addition to prescribed medication” (SAMHSA, 2019c).
For similar reasons, then Attorney General Eric Schneiderman of New York announced a settlement with Anthem (and Cigna prior to that) to end prior authorization requirements for MOUD (Parks, 2017). These examples provide precedence for how these medications, paid for by either state Medicaid programs or private insurers, can be made more widely available by removing prior authorization restrictions.
One reason prior authorization and associated requirements (e.g., lifetime limits, step therapy, or restrictions on high doses) have been instituted was to reduce the risk of diversion of MOUD or the chance of accidental poisoning (Clark and Baxter, 2013; Gaither et al., 2018). Prescribers have cited diversion as a barrier to treating individuals with OUD. A national survey found that one-third of providers thought that diversion of MOUD was a significant concern, and half stated they would no longer see a patient who was diverting medications (Lin et al., 2018; NASEM, 2019). While some studies show high rates of diversion of buprenorphine (Sansone and Sansone, 2015), others demonstrate that diversion may stem from a lack of patient access (Lavonas et al., 2014; Lofwall and Havens, 2012). Some providers have concerns about diversion, though increased awareness about the positive effects of MOUD may change these perceptions: a 2017 survey found that 26 percent of non-waivered physicians had concerns about diversion, whereas only 10 percent of waivered physicians shared those concerns, suggesting that education may change perceptions about the relative risks and benefits of this medication (Huhn and Dunn, 2017; NASEM, 2019). Importantly, adherence to buprenorphine treatment is associated with fewer hospital admissions (Sittambalam et al., 2014), and buprenorphine is associated with fewer admissions for life-threatening situations compared to the more frequently used heroin or oxycodone (SAMHSA, 2018a). In addition, lower doses and fewer initial days of buprenorphine supply are associated with treatment discontinuation and higher risk of adverse opioid-related events (Meinhofer et al., 2019). Still, there are some risks of increased buprenorphine prescribing: studies have shown that buprenorphine can be the cause of poisoning, particularly among children (Kim et al., 2012), and that individuals may sell their prescriptions.
One 2018 study showed that, among 303 individuals with OUD, 58 percent reported using diverted buprenorphine (Cicero et al., 2018). Yet, the self-reported motivations for using diverted medication reveal that the most common reasons were therapeutic: 79 percent claimed they used buprenorphine to prevent withdrawal, 67 percent to maintain abstinence, and 53 percent to self-wean off other opioid drugs. In this same sample, while half of patients reported they used buprenorphine for euphoria, only 4 percent said it was their drug of choice (Cicero et al., 2018). Furthermore, 33 percent of those who had used diverted
buprenorphine reported difficulty finding a prescriber to obtain the medication themselves, and 81 percent would have preferred to have their own prescription. Similarly, a 2016 study of individuals with OUD in New York City using MOUD without a prescription found that the primary motivations were to reduce withdrawal, control their ongoing drug use, or self-manage a treatment plan. Only several participants reported using buprenorphine for euphoric effects, and none reported using it as their drug of choice (Allen and Harocopos, 2016). A 2018 study in Rhode Island found similar results for data collected in 2009 and 2016 (Carroll et al., 2018b). In a 2012 study, Lofwall and Havens showed that—among 471 individuals in an Appalachian community sample of people using prescription drugs—up to 70 percent had used buprenorphine for euphoric effects at some point in their lives. Nonetheless, the strongest risk factor for using diverted buprenorphine was an inability to access buprenorphine treatment directly, and only 4.5 percent of this population engaged in daily use of diverted buprenorphine (Lofwall and Havens, 2012). At the same time, the motivations of those who divert drugs may be to help others struggling with OUD. In a 2015 study, Johnson and Richert conducted interviews with more than 400 patients in opioid treatment programs. More than 80 percent of patients perceived that diversion was mostly positive, and more than 75 percent considered it morally right to do so (Johnson and Richert, 2015). Another motivation to divert medications may be to fund ongoing drug use. Allen and Harocopos (2016) showed that, among those who diverted buprenorphine, some did so primarily as a means of funding the purchase of their preferred opioid following a resumption of street opioid use (though it is possible that the buyers did not have access to the medication themselves for managing withdrawal symptoms). In this study, none reported diverting buprenorphine as a chief source of income (Allen and Harocopos, 2016).
Some formulations of buprenorphine contain naloxone (e.g., Suboxone) to reduce the euphoric effects of the medication. Rates of misuse for the combined formulation are lower than buprenorphine alone. According to the Researched Abuse, Diversion, and Addiction-Related Surveillance System, past-month injection use of buprenorphine/naloxone in the United States among people with OUD was less than half as common as buprenorphine alone (16 percent versus 45 percent), mirroring data in other countries (Lofwall and Walsh, 2014). Formulations and routes of administration continue to be developed that aim to reduce illicit use potential while mitigating the effects of withdrawal and cravings (Dunn et al., 2017; Rosenthal and Goradia, 2017; Soper et al., 2018), and developing and deploying such medications should be a high priority.
Overall, this evidence suggests that limiting the availability of MOUD via mechanisms such as prior authorization may not be effective in reducing illicit use or diversion. Instead, diversion may increase, since supply is limited because patients are not able to access their own prescriptions for therapeutic purposes. This, in turn, would increase the number of people using diverted buprenorphine without the supervision of a health professional. Moreover, while not medically optimal, obtaining buprenorphine by diversion is far safer (and life-saving) (NASEM, 2019) than using other illicit opioids (e.g., untested heroin that is obtained illegally). It remains important to understand why and how medications are diverted, although it is clear that increased access to buprenorphine and other MOUD is essential for quelling the opioid epidemic (NASEM, 2019) and reducing the spread of infectious diseases. Similarly, it is crucial to package medications safely and take steps to reduce accidental poisonings, which have increased in frequency in recent years (Budnitz, 2016; Gaither et al., 2018).
Another reason to limit the supply of MOUD via prior authorization would be to reduce costs for unnecessary prescriptions. Yet, as demonstrated in peer-reviewed studies, prior authorization may produce only minimal savings (Park et al., 2017) and instead increase costs by creating administrative burden on providers and limiting access to medication that improves OUD outcomes (Abouzaid et al., 2010; Clark et al., 2011, 2014; Law et al., 2008; Lu et al., 2011). Because buprenorphine is now manufactured in generic form and can be purchased at a significantly reduced cost, prior authorization may not prove useful in containing costs (Clark et al., 2014).
If prior authorization policies increase administrative burden on health professionals—as demonstrated in the case studies—it is plausible that a smaller number of patients will receive cost-effective, beneficial, and safe treatments for OUD (Andrews et al., 2019; CMS, 2019c; NASEM, 2019). It is unclear that unsafe diversion or cost-control metrics are substantially improved with prior authorization requirements. In line with this evidence, in 2018 SAMHSA noted that prior authorization requirements limit access to MOUD and increase burdens on providers (SAMHSA, 2018a).
The federal government and some states have begun to take steps toward removing prior authorization requirements for MOUD. In 2017, the Food and Drug Administration (FDA) issued a relabeling of buprenorphine products to emphasize that it may be necessary for patients to remain on the medications indefinitely. In response to this, CMS issued a new policy that prevents Medicare Part D programs from requiring that a beneficiary needs to obtain prior authorization more than once per year for buprenorphine products (CMS, 2018). Following this change, the number
of Medicare Part D plans retaining prior authorization was drastically reduced (Mark et al., 2019). Some have suggested that CMS institute similar policy changes to Medicaid, and that states that have not removed or reduced prior authorization requirements should do so (Mark et al., 2019; Weber and Gupta, 2019), whereas others have called for abolishing prior authorization for buprenorphine (AMA, 2019; Beetham, 2019). At the federal level, CMS creates agreements between state Medicaid programs and the federal government outlining how the states can administer their Medicaid programs (CMS, 2019b). Currently, states are not required to remove prior authorizations for MOUD in order to reach receive federal matching funds for their program activities. Still, some states have done so regardless (Lambrew, 2019), demonstrating that it would be possible for CMS to include this as a contingency in future agreements with other states.
Findings
- Programs interviewed mentioned that gaining prior authorization to prescribe various formulations of buprenorphine (i.e., dosages) was a barrier to providing quality care to patients with opioid use disorder.
- Programs in states that have removed prior authorization requirements (from either the state Medicaid program or private health insurers) mentioned that this policy change has facilitated timely treatment.
Conclusion
- Prior authorization policies represent a barrier to prescribing efficiently that reduces the number of patients offered medications for opioid use disorder, is inconsistent with the urgency of the epidemic, and increases the risk of infectious diseases.
Recommendation 3-1: The Centers for Medicare & Medicaid Services (CMS) should withhold approval of a Medicaid state plan amendment from states that require prior authorization for medications to treat opioid use disorder (OUD). Independent of CMS action, states should remove prior authorization requirements for all Food and Drug Administration–approved medications to treat OUD in state Medicaid programs and state-regulated private insurers, allowing providers to prescribe whichever formulation and dose is best for an individual patient and without restrictions such as concurrent psychosocial therapy, step therapy, or lifetime limits.
DATA WAIVER REQUIREMENT
In 2000, Congress passed the Drug Addiction Treatment Act (DATA) as part of the Children’s Health Act of 2000, later amended in 2006. DATA 2000—which amended Section 303 of the Controlled Substances Act—intended to increase buprenorphine treatment by allowing office-based providers to prescribe it. According to the law, physicians could obtain approval from the federal government to prescribe by either obtaining a certification in addiction medicine or completing an 8-hour training (SAMHSA, 2019a). Such physicians are said to be “DATA waivered” or “X waivered,” as they are waived from the requirements for annual registration with the Drug Enforcement Administration (DEA) and to practice in a regulated opioid treatment program (Davis and Carr, 2019). While many of the required online and in-person trainings can be found for free through the Providers Clinical Support System (PCSS, 2019a), DEA registration has a first-time application fee of $731 for providers and a 3-year
renewal fee of $551 to become eligible to prescribe controlled substances (including buprenorphine) (DEA, 2019).
The 2006 DATA amendment increased the allowable patient limit of a waivered physician from 30 to 100 patients. In 2016, recognizing an increased need to treat OUD, the Department of Health and Human Services (HHS) ruled that this 100-patient limit could be increased to 275 (SAMHSA, 2017) with appropriate reporting requirements, as outlined in 42 CFR Part 8 (this increase may have only a marginal effect on overall prescribing rates, as described below).2 In addition, the Comprehensive Addiction and Recovery Act of 2016 included a provision that further extended DATA waiver prescribing privileges to nurse practitioners (NPs) and physician assis-
___________________
2 See https://www.ecfr.gov/cgi-bin/text-idx?tpl=/ecfrbrowse/Title42/42cfr8_main_02.tpl (accessed October 30, 2019).
tants (PAs) (SAMHSA, 2019g), which is projected to considerably increase the number of medications available to patients with OUD (Andrilla et al., 2018b). The Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) Act in 2018 further extended prescribing privileges to qualifying clinical nurse specialists, certified registered nurse anesthetists, and certified nurse midwives. However, non-physicians must take a 24-hour training course (Davis and Carr, 2019). Not all states have adjusted policies to allow these other qualifying providers to prescribe with full autonomy (AANP, 2018); as of April 2017, for instance, 28 states had certain “scope of practice” laws that prevent PAs or NPs from prescribing buprenorphine without physician oversight (SAMHSA, 2018a).
Eight of the 11 programs interviewed mentioned some part of the waiver process as being a barrier to providing quality, integrated care. Recognizing that intravenous drug use is a major risk factor for contracting an infectious disease, many of the programs acknowledged that treating OUD effectively and taking a harm-reduction approach is the most effective way to provide integrated care between OUD and infectious diseases.
Programs often cited the time-consuming nature of the waiver training. Several programs mentioned that very little training (if any) is required to prescribe other medications, including those like oxycodone with more potential for harm than buprenorphine. In addition, programs mentioned that the waiver training itself is clinically irrelevant to their day-to-day practice. Recognizing that the required training was inadequate and that providers were still hesitant to prescribe, several programs instituted their own in-house training for DATA-waivered providers so they could tailor the training to their specific clinical practice and ensure that providers take into account the risk of infectious diseases that comes with intravenous drug use.
Several programs adopted strategies to work around the difficult aspects of the DATA waiver process. One program trained its medical residents to work with an attending physician so that they have the necessary training to understand how to prescribe MOUD. Another program uses a medical home model3 in which specialists initiate medication for patients, and primary care physicians (PCPs) are in charge of maintenance for stable patients. In this way, all providers are able to stay below the waiver’s annual patient limit requirements.
These strategies to provide quality care, even in the face of perceived bureaucratic hurdles, are emblematic of the overall push from providers to
___________________
3 The National Institute on Drug Abuse, SAMHSA, and the National Council for Behavioral Healthcare have described various models for integrating behavioral and primary health care, including a set of best practices for treating SUD in a medical home model (e.g., concurrent screening and treatment of infectious diseases) (Mauer, 2010; Steinberg, 2014; Volkow, 2011).
increase patient access to MOUD. A study published in 2019 revealed that the number of PCP and non-psychiatry specialist office visits resulting in a buprenorphine prescription increased significantly between 2006 to 2014 (Wen et al., 2019). This suggests that a broader group of clinicians has recognized the importance of obtaining a DATA waiver and are beginning to prescribe MOUD, especially in counties with high rates of opioid overdose (Knudsen, 2015). In general, overall rates of prescribing and the number of DATA-waivered providers have increased (Dick et al., 2015). Still, studies have demonstrated a significant shortage of waivered providers: just prior to 2018, less than 4 percent, 2 percent, and 1 percent of eligible physicians, nurses, and PAs, respectively, had received a waiver (Andrilla et al., 2019a). In 2016, 60 percent of rural counties had zero authorized physicians (Andrilla et al., 2017b). In 2017, almost 20 million residents lived in a county without any waivered provider (Andrilla et al., 2019b).
Yet, the low number of waivered providers is only one component of the problem; providers’ comfort with and actual prescribing practices for MOUD is another. According to a 2018 survey of 4,225 DATA-waivered clinicians, only about 13 percent were prescribing at or near their buprenorphine limit. All had received their waiver at least several months before (up to 16 months before), yet 24.5 percent had not yet prescribed. According to these clinicians, a lack of demand from patients, time constraints, difficulty with insurance reimbursement, or prior authorization requirements were the top reasons for not prescribing more (Jones and McCance-Katz, 2019). This suggests that obtaining the DATA waiver itself is not a guaranteed mechanism for providers to prescribe (Stein et al., 2016; Thomas et al., 2017) and that patient demand and access—and time constraints, difficulty with insurance, and concerns about diversion—may also play an important role (Andrilla et al., 2017a, 2018a; Cicero et al., 2018; Gordon et al., 2008; Li et al., 2016).
There is evidence that effective education about MOUD and mentorship would increase the number of providers comfortable treating OUD (and infectious diseases) in an integrated manner. A 2006 study conducted in New York State implemented an 8-hour course about OUD for 257 physicians and then conducted a survey. About 44 percent of the physicians were trained in HIV care, and afterward, 66 percent of this group planned to pursue a DATA waiver to prescribe buprenorphine. In general, the physicians felt they would be more comfortable prescribing in the future if they had telephone contact with an expert mentor and could visit the mentor periodically to discuss prescribing practices (Sullivan et al., 2006). A survey conducted the same year of 375 HIV physicians suggested that a primary concern among those not currently prescribing buprenorphine was the lack of access to substance use disorder (SUD) experts (Cunningham et al., 2007). The PCSS does offer mentorship networks through its SAMHSA grant funding (PCSS, 2019b). Still, some have
argued that the continued training for health professionals on opioid-related issues in general—even opioid prescribing—is too low to meet the needs of patient populations with SUD (Davis and Carr, 2016).
As mentioned, a 2016 policy change at the federal level allowed physicians to treat up to 275 patients with buprenorphine at any given time (SAMHSA, 2017). A 2019 longitudinal study examined the characteristics of physicians who elected to increase their prescribing limit from 2016 to 2018. The number of physicians with a 275-patient waiver increased from 253 to 4,009 nationally, exceeding HHS’s predictions for waiver uptake (Knudsen et al., 2019). Yet, this distribution of 275-patient physicians was not uniform: states with medium and high levels of uninsured residents experienced lower growth, consistent with another study demonstrating that Medicaid expansion states saw the greatest increase in waivered providers (Knudsen et al., 2015, 2019). States with high overdose rates, high rates of other drug treatment programs, and high unmet SUD treatment need also saw the greatest increases in the number of physicians electing to prescribe at the 275-patient limit (Knudsen et al., 2019). There was a significant correlation between previous prescribing and an increase in physicians electing to increase their patient limit to 275. That is, those who were already prescribing were likely to prescribe more (Knudsen et al., 2019). This may be, at least in part, a function of the rule itself: only those prescribing at the 100-patient limit for at least 1 year were eligible to increase (SAMHSA, 2017). These data suggest that physicians in high-need areas recognize the importance of increasing their prescribing limit to 275, though it is unknown whether they will indeed prescribe at that level (due to either insufficient demand from patients or other factors). Nonetheless, program informants who had recently become waivered stated that the initial 30-patient limit was too low to meet the demand of their patients.
A number of solutions have been proposed with respect to the DATA waiver. Some have called for additional curricula for medical students in order to make them eligible to prescribe MOUD by the time they graduate (McCance-Katz et al., 2017; Weems, 2019). This may be especially needed, as there is evidence that students do not feel adequately prepared to treat OUD (Bäck et al., 2018), let alone concurrent OUD and infectious diseases. Others have called for removing the waiver entirely, freeing providers to prescribe buprenorphine without the burden of training and reporting requirements (Fiscella et al., 2019; Frank et al., 2018; Knopf, 2019). In line with this, the Mainstreaming Addiction Treatment Act of 2019, sponsored by Representative Paul Tonko of New York, was introduced in the House of Representatives in May 2019. This bill seeks to remove the DATA waiver and would require that HHS conduct outreach and encourage providers to become educated about SUD treatment (Davis and Carr, 2019; Stein et al., 2019; U.S. Congress, 2019). Just as with other areas of medicine, training to treat OUD (and concurrent infectious diseases) is
crucial for providing effective care to patients. Removing the current DATA 2000 requirements from the Controlled Substances Act—including the mandatory training—may therefore only prove beneficial if providers have easy access to high-quality training, either in their training programs or continuing medical education.
Findings
- The training to obtain a Drug Addiction Treatment Act waiver to prescribe buprenorphine was mentioned by several programs as a time-consuming, clinically irrelevant process for providers, and they stated that it therefore prevents the timely delivery of care to patients.
- The limit on the number of patients a provider can treat, particularly the 30 patients allowed in the first year of prescribing buprenorphine, was mentioned as being too low to meet the demand of patients.
- There is evidence that, to feel comfortable prescribing medications for opioid use disorder, some providers need mentorship from a more senior provider or someone with expertise in substance use disorder treatment.
Conclusions
- The Drug Addiction Treatment Act waiver training represents a barrier to maximizing the number of health care providers who can prescribe buprenorphine to patients with opioid use disorder.
- The patient limit in the first year of prescribing is too low to meet the number of patients who would benefit from buprenorphine.
- Providers could benefit from increased opportunities for mentorship from those already comfortable prescribing medications for opioid use disorder.
Recommendation 3-2: Congress should amend Section 303 of the Controlled Substances Act to allow buprenorphine and other medications for opioid use disorder to be prescribed by physicians, physician assistants, nurse practitioners, clinical nurse specialists, certified registered nurse anesthetists, or certified nurse midwives without undergoing the mandatory training currently required by law, requiring a Drug Addiction Treatment Act waiver, or limiting the number of patients that can be treated.4
___________________
4 The committee notes that clinically relevant training should nonetheless be widely available to trainees and providers, as outlined in the remaining recommendations of this report.
Recommendation 3-3: To improve and expand education and training on medications for opioid use disorder (OUD) and infectious diseases:
- The Providers Clinical Support System—as the primary federal grantee for training clinicians on evidence-based training, mentoring, and educational resources on medications for OUD—should consult further with practicing providers and amend their training programs to ensure they are clinically relevant and commensurate with the practitioner’s intended role and needs (including for prescribing of medications for OUD), and should prioritize growth of its mentorship system.
- The Substance Abuse and Mental Health Services Administration should provide additional funding in future grant announcements specifically to expand mentorship networks for providers.
LACK OF DATA INTEGRATION AND SHARING
Barriers to efficient data integration and sharing are numerous, including lack of interoperability and infrastructural, financial, deployment, and regulatory challenges (Ghitza et al., 2011). Regulatory challenges are especially relevant in the context of integrating OUD and infectious disease services, and interviewed programs mentioned them as barriers.
In the 1970s—well before the Health Insurance Portability and Accountability Act of 1996 (HIPAA)—a federal confidentiality law (42 CFR Part 2) was passed aimed at protecting the privacy of those with SUD. Specifically, the law was intended to encourage individuals with SUD to seek treatment without the fear of their SUD becoming known outside of the treatment context, so that they need not risk arrest, loss of guardianship/parental rights, or discrimination in employment or insurance contexts. The law placed protections around information relevant to SUD, such that diagnoses and treatment could only be shared with other entities in narrow situations (such as in a medical emergency, court order, or child abuse case), and then only the minimum amount of information necessary (Ghitza et al., 2011; Schaper et al., 2016). In the majority of cases, however, patient records pertaining to SUD can only be shared with the patient’s consent, even including situations when it would be for the purposes of that patient’s treatment (Pating et al., 2012).
HIPAA, adopted much later, is a looser restriction on protected health information, stipulating that individuals’ records could be shared without consent if that information was needed for treatment, payment, or health care operations (OCR, 2013).
Title 42, Part 2, of the Code of Federal Regulations applies to “federally assisted programs,” meaning they are operated, certified, or authorized by the federal government, receive federal funding, are tax-exempt, or dispense methadone and other controlled substances under DEA certification. Any entity that “holds itself out” as a SUD treatment entity is also subject to 42 CFR Part 2. In practice, this means that any entity advertising treatment for SUD, has received state licensure to provide SUD, or has health care teams devoted to treating SUD will fall under these regulations (Schaper et al., 2016). As a result, any entity providing integrated care for SUD and infectious diseases—wherein generalist health care providers may offer both types of care—is very likely to be subject to 42 CFR Part 2 (Antonini et al., 2012; Ghitza et al., 2011), although states have interpreted the federal regulations differently (SAMHSA, 2018a).
Though 42 CFR Part 2 was updated in 2017 (APA, 2017) and 2018 (SAMHSA, 2018b) to allow for greater flexibility and data sharing, it is still viewed by some providers as burdensome, confusing, and contrary to the delivery of effective, patient-centered health care (MACPAC, 2018b). Six of the 11 programs interviewed reported data sharing (or lack thereof) as a barrier to providing integrated care. One program’s staff suggested that “holding themselves out” as a drug treatment program is not in their patients’ best interest, as it would prevent the organization from sharing patient information between primary care and drug treatment providers. Additionally, several programs mentioned that integrated case managers and near-peer advisors were unable to see relevant medical information about patients, preventing them from having the necessary knowledge to guide patients through their care. Several programs also mentioned the general difficulty in creating integrated data systems from an information technology infrastructure and deployment perspective (e.g., various branches of care are unable to coordinate because they do not share the same electronic medical record systems).
The interviewed programs found ways to manage data integration and sharing barriers. First, programs had become diligent about asking patients for consent to share information about OUD with other health professionals. With that consent, behavioral health information could be shared with PCPs and better care could be delivered. Second, several programs mentioned a concerted effort and investment in electronic medical record (EMR) systems that could serve a wide range of health care needs. Indeed, the importance of investing in data collection up front was a primary lesson learned from several of the programs interviewed.5
___________________
5 Germane to this point, SAMHSA has developed several toolkits for organizations to ensure that they are ready for integration from an administrative perspective, including with respect to data collection and sharing (SAMHSA, 2015c,d).
These issues and solutions are similar to those found among other programs documented in the literature. The authors of a 2015 study interviewed eight primary care clinics and three community mental health centers about implementing integrated care (Cifuentes et al., 2015). Common challenges with respect to data sharing and integration were (1) documenting and tracking both behavioral and physical health information, (2) coordinating between different care teams on the EMRs, and (3) exchanging information between devices and across EMRs. These challenges resulted in duplicated efforts, reliance on outdated methods of tracking information, missed opportunities for care coordination, and inconsistent verbal information exchange between providers about patients (Cifuentes et al., 2015).
A 2016 study found similar results stemming from interviews with 76 health care providers and administrators. Those interviewed generally found that information exchange was significantly limited due to 42 CFR Part 2 restrictions. These restrictions caused confusion between providers and prevented communication between SUD treatment and medical care providers. Respondents were unsure when and in what ways confidentiality regulations applied, and while they were aware of the importance of gaining patient consent, they found it difficult to do so (McCarty et al., 2016). For these reasons, some have called for the removal of 42 CFR Part 2 entirely, instead replacing it with the more modern rules in HIPAA (Stein et al., 2019).
With respect to data integration and sharing more generally, there is ongoing debate about the balance between protecting patient confidentiality and promoting data openness for quality care (Lopez and Reid, 2017; Wakeman and Friedmann, 2017). HIPAA and 42 CFR Part 2 are often at the center of this debate. In August 2019, HHS released several proposed changes to 42 CFR Part 2 to maintain patient privacy but also enhance care for patients with OUD through care coordination (HHS, 2019b).
A primary argument in favor of stringent confidentiality regulations is the public’s genuine concern about maintaining privacy. A 2010 survey of a representative sample of 1,849 general health care consumers found that 68 percent of respondents were concerned with the privacy of their personal health records, and 75 percent of those not using an online patient health record system listed concerns about privacy as their top barrier (Undem, 2010). Moreover, 42 percent stated they would not feel comfortable if their health information was shared with insurance plans, researchers, companies, and others (relative to 31 percent answering that they would feel comfortable, and 25 percent answering “not sure”). Nevertheless, 66 percent agreed with the idea that privacy concerns should not detract from learning about how technology can improve health care, suggesting that the public is open to the idea of greater data sharing if it brings about better health (Undem, 2010).
Individuals’ interest in maintaining confidentiality about a SUD may speak to concerns about feeling stigmatized. However, some argue that maintaining stringent privacy practices only serves to reinforce that stigma by continuing to segregate SUD from other medical care (Schaper et al., 2016). While the treatment of SUD as a medical condition has gained significant traction in the past several decades, it has not fully translated into medical practice. In 2000, McLellan and colleagues argued that SUD should be viewed as similar to other chronic diseases, including type 2 diabetes. Both illnesses are a function of heritability, have environmental contexts that influence their onset and disease course, and can be managed with medication or appropriate lifestyle changes (McLellan et al., 2000). The automatic segregation of medical information related to SUD may therefore perpetuate stigmatization of SUD as a different kind of illness, one that is important to keep confidential even from other health professionals (Schaper et al., 2016).
Some have argued that this bias toward SUD confidentiality has material consequences for medical care. For instance, privacy regulations may prohibit coordinated, integrated care because health professionals will be unaware of a patient’s SUD. Additionally, a mere lack of shared information and coordination between SUD providers and PCPs may prohibit the exchange of information necessary for a holistic treatment plan (Schaper et al., 2016). This could include knowledge about drug interactions, including those used to treat OUD (McCance-Katz et al., 2003). In support of this, a 2009 study reviewed EMRs of 84 patients in an opioid treatment program (where methadone is prescribed) in Boston, and primary care records from an affiliated medical center; 69 percent were receiving at least one medication from the medical center that had a known negative interaction with methadone (e.g., oversedation, withdrawal, overdose, cardiac dysrhythmia), and 19 percent had three or more potentially interacting medications. This study showed that while OUD was documented in most primary care medical records, it was omitted from 30 percent of them, suggesting a lack of robust information exchange between providers and a failure to diagnose OUD among PCPs (Walley et al., 2009). Notably, the SUPPORT for Patients and Communities Act appropriated $7 million over 5 years to promote communication between SUD providers and other health care providers (Pub. L. No. 115-271), though it is unclear whether such efforts will be successful.
Findings
- Title 42, Part 2, of the Code of Federal Regulations, intended to protect the privacy of patients with substance use disorder, is seen by some providers and programs interviewed as burdensome and a hindrance to delivering effective, patient-centered, high-quality care.
- There are legitimate privacy concerns surrounding the sharing of substance use disorder information.
- The regulation can limit how providers speak about their services. Part 2 of Title 42 applies to any program that “holds itself out as providing, and provides, substance use disorder diagnosis, treatment, or referral to treatment.” This “holding itself out” is not specifically defined in the regulation, but could mean public outreach to patients about specific treatments the program offers.
Conclusions
- Further data sharing between providers promotes better care. Though enacted to protect the privacy of patients with substance use disorder and to encourage treatment retention, 42 CFR Part 2 limits important information exchange and represents a barrier to delivering patient-centered, high-quality care.
- In part due to high levels of stigma for patients with substance use disorder (SUD), and the material consequences of information being shared, it is important to respect patients’ desire to maintain confidentiality of SUD information.
- Part 2 inhibits integration of primary care services (including infectious disease prevention) with treatment for opioid use disorder and prevents providers from advertising an important service that they offer.
Recommendation 3-4: The Substance Abuse and Mental Health Services Administration (SAMHSA) should either further align 42 CFR Part 2 with the Health Insurance Portability and Accountability Act of 1996 or alter the definition of which specific service delivery programs fall under 42 CFR Part 2. To inform this decision, SAMHSA should formally engage with patients, advocacy groups, the general public, and legal experts to better understand the benefits (e.g., greater data access for providers) and costs (e.g., loss of privacy for patients, danger of uncoordinated care) of changing regulations around sharing of substance use information. This engagement should focus on the effects of allowing disclosures of substance use disorder information for treatment rather than solely for payment, health care operations, audits, and evaluations; on the strengths and weaknesses of informed consent as a method for sharing information; and on clinics’ current data-sharing practices.
INADEQUATE WORKFORCE AND TRAINING
The number of people with OUD is far greater than those who access treatment (Haffajee et al., 2018), leading to continued drug use and an increased risk of infectious diseases. One of the reasons posited for this gap in care is the lack of a medical workforce to provide the care. The workforce deficit is more than a number; additional barriers include training and education deficits, poor support from institutions, a lack of care coordination for providers delivering treatment (Haffajee et al., 2018), and the segregation of SUD treatment from primary care. This hinders the medical workforce’s ability to provide integrated care for OUD and infectious diseases.
There are several components to the workforce shortage. The first is related to the paucity of providers willing or able to provide evidence-based treatment for OUD (Kepple et al., 2019). As mentioned previously, in 2016, 47 percent of all U.S. counties were without a DATA-waivered physician (Christie, 2017). Under 4 percent of physicians are authorized to provide buprenorphine treatment (Haffajee et al., 2018). Even among some of those who are authorized are less likely to prescribe if they lack institutional and peer-clinician support, adequate reimbursement mechanisms, coordination of OUD care, or a favorable regulatory environment (Haffajee et al., 2018; Hutchinson et al., 2014).
A second component of the workforce shortage relates to geographic distribution. There is a dearth of providers in rural areas who are equipped for integrated treatment. In 2016, 72 percent of rural counties did not have a DATA-waivered physician (Christie, 2017). In general, rural communities have greater barriers to care (Joudrey et al., 2019) and opioid overdose rates similar to those in urban areas (Hedegaard et al., 2019). The problem is magnified if providers in rural areas either do not have the ability to prescribe MOUD, or elect not to (Andrilla et al., 2019b). A 2018 study found that only 56 percent of rural DATA-waivered physicians were accepting new patients for buprenorphine treatment (Andrilla et al., 2018a).
Third, as mentioned in the DATA waiver section, there is a tendency for providers to treat fewer patients than allowed by the limits. In a large study of more than 3,000 buprenorphine prescribers nationwide, Stein and colleagues (2016) found that the median number of patients per month was 13—well below even the lowest DATA-waiver limit. Moreover, the median treatment duration was 53 days, which is below the clinically recommended length. There is reason to think this lack of prescribing is due to workforce barriers: those who had recently become waivered reported lack of access to experienced providers and to OUD counseling to be used in tandem with medications (Stein et al., 2016). In rural areas, those who were treating patients were prescribing well below their limit: physicians waivered for 30 patients were treating only 8.8 on average, and those waivered for 100 patients were treating only 56.9 (Andrilla et al., 2018a). Though program informants stated that the 30-patient limit was too low to meet patient demands, there is clearly a high degree of geographic variability in prescribing rates.
Fourth, infectious diseases and OUD are complex and co-occurring conditions that require an interprofessional constellation of workers—adequately trained throughout their careers—to promote health, from prevention to recovery and support services across multiple settings (SAMHSA, 2019k). The health care team includes but is not limited to health professionals, psychologists, advanced practice registered nurses, PAs, clinical addiction counselors, social workers, marriage and family therapists, mental health counselors, community health workers, and peer-support specialists (SAMHSA, 2019k). Education and training are needed to build the knowledge, skills, and attitudes of this diverse interprofessional workforce. Some programs exist to promote training opportunities around OUD, such as the Health Resources and Services Administration’s (HRSA’s) Opioid Workforce Expansion Programs (HRSA, 2019b), which provides grants to train behavioral health professionals and paraprofessionals to address behavioral health needs—including OUD and SUD—in high-need, underserved, and rural populations. In addition, HRSA posted an announcement for an addiction medicine fellowship program grant, aiming to establish new and innovative programs to expand addiction medicine programs in underserved areas (ACAAM, 2019). Nevertheless, government-sponsored training specific to the integration of OUD and infectious disease services for a wide constellation of providers is not readily available.
A final issue related to the workforce landscape is the historical dissociation of methadone treatment for OUD from primary care. As of 2018 there were more than 1,600 opioid treatment programs delivering methadone throughout the United States, serving more than 380,000 patients annually (Vestal, 2018). Methadone treatment is often quite different
from other medical care, and opioid treatment programs must be registered under the DEA and must receive certification from SAMHSA (2015a). Opioid treatment programs also do not frequently provide other medical care—including testing or treatment for infectious diseases—even though evidence suggests HIV outcomes can be improved when HIV care is delivered in such a setting (Lucas et al., 2004; Simeone et al., 2017) and that referrals out result in less care delivered (Umbricht-Schneiter et al., 1994). In interviews with experts on this topic, the committee was informed that opioid treatment programs have few financial incentives to provide medical care, including testing and treatment for infectious diseases. The clinics are often small, with little space for examination rooms and storage of medical supplies, and providing such care would require more staffing.6 In addition, as opioid treatment programs have been historically divorced from medical care, a shift to including it would likely require a cultural change.7 Because opioid treatment programs have a large number of patients with OUD in both urban and rural settings, they represent an opportunity to provide greater integration of infectious disease and OUD care, if a professional workforce were trained and able to offer such services. In at least one way, this integration of OUD care and medical care has begun already: in a majority of states, Medicaid funding can be used for OUD treatment in opioid treatment programs (Vestal, 2018). Furthermore, some screening for infectious diseases already exists in these programs (for tuberculosis and intermittent, opt-in HIV testing), though this is not widespread (CDC, 2014).
Methadone cannot be prescribed in primary care settings to treat OUD (though it can be prescribed for pain), despite several decades of research demonstrating its effectiveness for OUD (SAMHSA, 2019e). Federal regulations stem from two congressional actions that gave authority to HHS to regulate methadone and DEA to require registration for providers to dispense it: the Controlled Substances Act—Title II of the Comprehensive Drug Abuse Prevention and Control Act of 1970—as well as Section 3 of the Narcotic Addiction Treatment Act of 1974. Following from this legislation, methadone for OUD is allowed only for providers who have a separate DEA registration to dispense it for maintenance or detoxification (DEA, 2006).
Some have argued that this segregation of methadone treatment for OUD from primary care is out of step with the current crisis and leads
___________________
6 Andrew Talal, Professor of Medicine, University of Buffalo, personal communication, May 6, 2019, and Gregory Lucas, Associate Professor of Medicine, Johns Hopkins University School of Medicine, personal communication, August 5, 2019.
7 Gregory Lucas, Associate Professor of Medicine, Johns Hopkins University School of Medicine, personal communication, August 5, 2019.
to poorer outcomes for patients (Samet et al., 2018). In 1995, the Institute of Medicine noted in a consensus study that regulations surrounding methadone treatment for OUD
foster situations where addicts cannot obtain a treatment program tailored to their individual circumstances, physicians are unable to exercise professional judgment in treating individual patients, programs are isolated from mainstream medical care (thus depriving patients of important ancillary services), and significant economic costs are incurred in assuring compliance with regulatory requirements—costs that are shared by programs, insurers, patients, and taxpayers. (IOM, 1995, p. 31)
The 1995 study further suggested that regulations surrounding methadone should be altered to “shift responsibility for treatment decisions from regulators to clinicians” (IOM, 1995, p. 221). While diversion of methadone—and buprenorphine—has been posed as a negative consequence of increased access, the National Institute on Drug Abuse has noted that the majority of diversion is for self-medication and to reduce cravings from other opioids, not for euphoric purposes (NIDA, 2018d). As former reports (IOM, 1995) and articles (Samet et al., 2018) have suggested, training providers on the use of methadone for OUD is paramount to ensuring that patient care is maximized and negative consequences are minimized. As mentioned, the Controlled Substances Act currently allows methadone to be prescribed for the treatment of OUD only within specially licensed and regulated facilities (opioid treatment programs), but not in office-based medical practices (FSMB, 2013). This is despite the fact that evidence suggests methadone can be effectively provided in office-based settings with high treatment retention (Fiellin et al., 2001), and that methadone is prescribed in office-based settings in several other countries. Access to methadone in primary care may be especially useful in rural areas, where opioid treatment programs may be limited (Samet et al., 2018).
Seven of the 11 programs interviewed reported some concern with the professional workforce for providing integrated OUD and infectious disease treatment. This included, most commonly, an issue with education. Several program informants believed there were simply not enough high-quality mechanisms for providers to be trained on integrated OUD and infectious disease care to meet the needs of patient populations. Programs also expressed a concern about the lack of billing and reimbursement mechanisms for training and their inability to bill for the hours of the non-physician workforce crucial to providing integrated care (e.g., case managers or peer-support specialists). In addition, programs stated that there are few incentives for providers to move to and practice in rural areas where the need is the greatest. Finally, several informants mentioned that state licensure rules prevented their programs from billing and obtaining rev-
enue for certain kinds of care, such as a rule that prohibits billing behavioral health services unless they are provided by a licensed clinical social worker, as opposed to other professional licenses. Data from SAMHSA (2018a) support these kinds of licensure requirements as a barrier to integrated care.
Regarding training, some have argued for additional OUD education in medical schools or residency programs, which could be coupled with infectious disease training that already exists (Dwarakanath, 2019; Haffajee et al., 2018; Ram and Chisolm, 2016; Ratycz et al., 2018; Wakeman and Barnett, 2018). This could include training on prescribing MOUD and or the Screening, Brief Intervention, and Referral to Treatment (SBIRT) program (Madras et al., 2009) as a prerequisite for medical, residency, nursing, or PA training program accreditation, thereby increasing provider confidence. Typically, accrediting bodies (such as the Liaison Committee on Medical Education for medical schools or the Accreditation Council for Graduate Medical Education for residency programs) list a general set of competencies or standards that training programs must meet; for medical schools, increased education toward pressing societal problems, such as the dual epidemics of OUD and infectious diseases, could be put forth as a curricular criterion for training programs across the country. Currently, medical schools do not devote a significant portion of training to SUD in general, with respect to evidence-based treatment, harm reduction, and stigma reduction (Finkelstein et al., 2011). Yet, inserting new curricula into an already filled medical education may be difficult. This has led others to argue for embedding SUD treatment into the regular curricula via case studies where substance use is a component of the overall patient profile, including patients with infectious diseases (Lembke and Humphreys, 2018). Regarding graduate medical education, HRSA has begun to provide funding for addiction medicine fellowship programs (ACAAM, 2019), though such programs are not available at all academic medical centers. Nonetheless, training alone may not be a sufficient incentive for newer health professionals to begin prescribing MOUD. As an example, when not using the DEA number of their supervising physician or hospital, a resident must pay a first-time application fee of $731 and a 3-year renewal fee of $551 to the DEA to obtain their own prescribing number (DEA, 2019). This may pose a financial barrier.
Finally, MOUD training coupled with infectious disease care could be encouraged and supported for continuing medical education once providers are practicing (Haffajee et al., 2018), offering opportunities for continual exposure to best care practices across a clinician’s career. Training on these topics is currently available, including on harm-reduction practices in primary care (ASAM, 2019), MOUD (PCSS, 2019c), and integrated care for patients with OUD and infectious diseases (Sax, 2019).
With respect to the lack of a trained workforce specifically in rural areas, several novel models have been proposed. One is to allow patients
the opportunity to take buprenorphine from home (often called “home induction”) without immediate provider supervision, thereby reducing the number of necessary visits to a provider’s office. Evidence is emerging—though studies are not of exceptional quality—that few adverse outcomes are associated with patients taking buprenorphine from home (Cunningham et al., 2011; Lee et al., 2009, 2014; Martin et al., 2018; Sohler et al., 2010). While more research is needed on the efficacy of home-based treatment, this represents a promising avenue for patients who lack transportation in rural areas or do not have easy access to a waivered provider. Another is to increase telemedicine access such that providers can interact with a greater number of patients across rural areas, providing MOUD or infectious disease care via local pharmacies. An expert interviewed for this study8 provided a proof-of-concept study on hepatitis C virus (HCV) treatment for people who take methadone in both rural and urban areas (PCORI, 2019). The results suggest that telemedicine treatment for HCV to patients receiving methadone at an opioid treatment program was successful (Buffalo State, 2019). Given the historical dissociation between methadone treatment for OUD and medical care (including infectious disease care) (Merrill, 2003), this model may represent a promising avenue for further integrating these services in the hundreds of opioid treatment programs throughout the United States. Indeed, this may be increasingly relevant, as opioid treatment programs are opening more frequently in rural areas (Vestal, 2018). Nevertheless, stable reimbursement mechanisms for telemedicine services remain elusive (Buffalo State, 2019). HRSA has the Substance Abuse Treatment Telehealth Network Grant Program, but it does not include a specific focus on integrating OUD and infectious disease care (HRSA, 2019d). Other training models, such as the National Network of STD Clinical Prevention Training Centers funded by CDC, demonstrate how government-funded training can be distributed throughout rural regions of the country (CDC, 2019g). A similar model could be instituted for training on OUD and infectious disease integration.
An additional proposed solution is to expand hub-and-spoke models, as have been instituted in several states to address opioid use (Williams and Bisaga, 2016): a primary hub for a larger geographic region serves as the intake point for new patients, connecting them with initial MOUD treatment and determining the best placement for further treatment. Then, when patients are stable on MOUD, they are transferred to “spoke” care (primary care staffed by, for instance, nurse–counselor teams and buprenorphine prescribers). The goal is to move from more specialty care
___________________
8 Andrew Talal, Professor of Medicine, University of Buffalo, personal communication, May 6, 2019.
(hubs) to less intensive care (spokes) (Brooklyn and Sigmon, 2017) that can treat a wide variety of illnesses, including infectious diseases. Another mechanism to address rural workforce shortage is to institute widely advertised loan forgiveness programs focused specifically on treating OUD and infectious diseases in underserved areas. As of 2019, HRSA had such a program to combat the opioid epidemic in rural communities, although it does not explicitly address the need to treat co-occurring infectious diseases (HRSA, 2019c).
Findings
- There is an inadequate number of providers—including health professionals, social workers, peer-support specialists, therapists, and counselors—capable of treating infectious diseases and opioid use disorder in an integrated way (including medications and ancillary services for both) relative to the population struggling with these concurrent epidemics.
- The workforce shortage is especially notable in rural areas.
- Despite treating thousands of patients with opioid use disorder and concurrent infectious diseases, opioid treatment programs (where methadone is dispensed) do not frequently provide infectious disease care in this setting.
- Though in the early stages, telemedicine is being studied and used in order to provide integrated services for opioid use disorder and infectious diseases.
Conclusions
- A more robust provider workforce must be developed from those already in practice and those currently in training.
- Incentives must be made available for providers to treat patients in rural areas, where services are otherwise difficult to access.
- Integrating infectious disease testing and treatment in opioid treatment programs throughout the United States represents an opportunity to integrate care for many patients already seeking opioid use disorder treatment.
- Telemedicine and other approaches that increase access to care represent promising opportunities to integrate services for opioid use disorder and infectious diseases.
Recommendation 3-5: In addition to the Opioid Workface Expansion Program for behavioral health trainees, the Health Resources and Services Administration should fund high-quality,
clinically relevant training on the care and management of co-occurring opioid use disorder (OUD) and infectious diseases for clinicians working in a wide variety of settings (e.g., primary care clinics, infectious disease care settings, and other settings that treat people with OUD and related infectious diseases).
Recommendation 3-6: The Health Resources and Services Administration should devote additional resources toward—and more widely promote—programs that incentivize providers (including psychiatrists, health service psychologists, licensed clinical social workers, psychiatric nurse specialists, marriage and family therapists, and licensed professional counselors) to work in rural areas where opioid and infectious disease outbreaks are most likely to occur (one such program is the National Health Service Corps Rural Community Loan Repayment Program, in coordination with the Rural Communities Opioid Response Program within the Federal Office of Rural Health Policy).
Recommendation 3-7: The Health Resources and Services Administration should widen the scope of its Substance Abuse Treatment Telehealth Network Grant Program to support telemedicine approaches for integrating both opioid use disorder and infectious disease services, particularly in rural areas.
Recommendation 3-8: The Department of Health and Human Services should explore policy incentives for providers and clinics to provide a wider array of evidence-based medications for opioid use disorder and to institute universal, opt-out testing and connection to treatment for infectious diseases, especially at methadone-based opioid treatment programs.
Recommendation 3-9: Congress should amend Section 303 of the Controlled Substances Act to permit providers to deliver methadone treatment for opioid use disorder in primary care settings.
Recommendation 3-10: The Diversion Control Division of the Drug Enforcement Administration should waive the fee associated with gaining a registration number for health professionals (i.e., medical residents, physician assistants, and qualified nurses) in their residencies or soon after their training is finished to incentivize them to gain buprenorphine prescribing authority early in their careers.
Recommendation 3-11: To better integrate training on opioid use disorder (OUD) and infectious diseases in health professions training:
- The Liaison Committee on Medical Education (LCME) should assure that medical students receive practical, clinically relevant, harm-reduction-focused, case-management-based training on OUD and infectious disease assessment, management, and treatment in response to LCME’s curricular content standard 7.5 (societal problems).
- The Accreditation Council for Graduate Medical Education should, among its common program requirements, require that residents and fellows receive practical, clinically relevant, harm-reduction-focused, case-management-based training on OUD and infectious diseases.
- The accreditation bodies for nursing education should assure that students receive practical, clinically relevant, harm-reduction-focused, case-management-based training on OUD and infectious disease assessment, management, and treatment through their curricular, programmatic, or competency criteria.
- The Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) should assure that students receive practical, clinically relevant, harm-reduction-focused, case-management-based training on OUD and infectious disease assessment, management, and treatment in response to ARC-PA’s program curriculum standard number B2.08 (social and behavioral sciences).
Recommendation 3-12: State medical boards (and equivalent licensing bodies for other health professionals) should encourage providers to take continuing education focused on harm reduction in fulfilling their continuing education requirements.
STIGMA
Behaviors or conditions that are socially discrediting can be stigmatizing such that individuals are “labeled, set apart and linked to undesirable characteristics that leads them to experience status loss and discrimination” (Link and Phelan, 2001). Individuals with OUD and some infectious diseases such as HIV and viral hepatitis, often experience stigma related to their condition(s) (NASEM, 2016a,b, 2019). Stigma can occur at any of the following five levels: (1) intrapersonal, (2) interpersonal, (3) community,
(4) organizational/institutional, and (5) governmental/structural (Cook et al., 2014; Heijnders and Van Der Meij, 2006; Rao et al., 2019). Internalized stigma associated with shame, guilt, and fear of negative effects (Kelly and Westerhoff, 2010), and perceived stigma by others that individuals are dangerous, unpredictable, and to be blamed for their own condition (Yang et al., 2017) may deter individuals from seeking health care or providers from delivering care (Van Boekel et al., 2013). Despite the fact that stigma deters access to systems of care for diagnosis, treatment, and successful health outcomes (Katz et al., 2013; Rueda et al., 2016; Van Boekel et al., 2013; Yang et al., 2017), “stigma reduction is not a routine part of the way in which health services are delivered or evaluated” (Nyblade et al., 2019).
Seven informants from the 11 programs interviewed commented on the role that stigma plays as a barrier for individuals seeking care and in shaping care delivery. There were several key aspects about stigma that were repeated across programs. The first was that stigma in general may prevent patients from seeking treatment (especially those who inject drugs) and prevent organizations from delivering treatment. Another was the stigma associated with infectious diseases, and the additional stigma that patients may encounter if they are positive for HIV or viral hepatitis while continuing to use drugs.
A third issue cited across several programs was provider stigma, and the need to instill compassionate, patient-centered care in providers.
Provider stigma toward individuals with OUD has been noted in the literature as a problem that can hinder care delivery and quality (Kennedy-Hendricks et al., 2016; NASEM, 2019; Olsen and Sharfstein, 2014). Though the issue is complex, there is evidence that stigma against persons who use drugs—or those already seeking treatment through MOUD—may limit the care (Kepple et al., 2019). Four of the interviewed programs mentioned the importance of providing “culturally competent care,” or that this type of care was at the core of their mission. It is possible that more widespread use of care protocols—such as SBIRT—may assist providers in treating patients in an unbiased manner (Babor et al., 2007).
Related to provider stigma is the problem of stigmatizing language used by health professionals (e.g., “addicts” rather than person-centered language like “individuals with SUD”) (Kelly et al., 2016). Recommendations for improving terminology related to substance use and SUD have been made by the White House Office of National Drug Control Policy (Botticelli, 2017). Professional associations have also called for reducing stigma by improving language related to SUD (AMA, 2018; Goldsmith, 2016). The committee heard from one clinician informant that the language used in the treatment field continues to be stigmatizing. In this clinician’s view, the term “medication-assisted treatment” (MAT) perpetuates stigma by conveying medication as secondary to other kinds of treatment: “I think we need to eliminate the term ‘medication-assisted treatment’; it’s treatment or it’s medication. The medication is the focus.”9 Another term used in the field, “induction,” was also viewed as a stigmatizing term compared to simply “starting treatment.” The clinician reported that providers in clinical settings are often concerned about having to “induct individuals” on medication: “As I try to convince more settings to integrate, there’s this fear of starting. I think the term induction has been a tremendous negative. We don’t induct individuals on . . . medication; we start people on medication.”10 “Opioid substitution therapy” is an additional term that may perpetuate stigma, implying that patients seeking MOUD are simply substituting one addiction or one opioid with another (Samet and Fiellin, 2015).
Stigma has been a perennial issue with respect to OUD (Kennedy-Hendricks et al., 2017; Vigilant, 2004), infectious diseases (Alonzo and Reynolds, 1995), and SUD more generally (Link et al., 1997). Interviewed programs proposed a number of solutions for reducing stigma and increasing patient-centered care. A number of informants noted that because many of their clients have stigmatized health needs, they strive to counter the stigma by consistently working to make sure the environment
___________________
9 Michael Fingerhood, Associate Professor, Johns Hopkins University Bloomberg School of Public Health, personal communication, June 28, 2019.
10 Michael Fingerhood, Associate Professor, Johns Hopkins University Bloomberg School of Public Health, personal communication, June 28, 2019.
is stigma free and that their policies promote a welcoming, nonjudgmental care environment. Additionally, several programs mentioned structuring their models of care to reduce the stigma associated with OUD and infectious diseases. Primary care clinics, in particular, reported that integrating OUD treatment within primary care services resulted in less stigmatization. One reason is that, in an integrated clinic, patients may be visiting for any number of reasons, including SUD or infectious diseases or simply a primary care checkup.
Early research suggests that educational interventions to reduce self-stigma (i.e., stigma that patients feel about themselves) (NASEM, 2016b), general public stigma, and provider stigma can be effective. These tactics include group-based acceptance and commitment therapy, motivational interviewing/voluntary counseling, communication of positive stories of people with SUD, and contact-based training (Avery et al., 2019; Chidrawi et al., 2016; Feyissa et al., 2019; Livingston et al., 2012). Beyond intrapersonal, interpersonal, and community-level interventions to reduce stigma, interventions that work within systems of care and institutions are crucial to reduce stigma and support health outcomes. Feyissa and colleagues (2019) state that targeted training for popular opinion leaders within systems of care can reduce health care workers’ stigmatization of people living with HIV and improve compliance with universal precautions. As demonstrated at the interpersonal and community levels, showcasing positive stories of those who are successfully recovering from SUD can also help improve health professionals’ attitudes toward patients seeking treatment and reinforce the notion that treatment works (Rao et al., 2009). Additionally, education efforts that incorporate critical self-reflection and contact with stigmatized patients has been shown to reduce stigma among psychiatry residents and medical students (Ballon and Skinner, 2008; Bland et al., 2001; Meng et al., 2007; Silins et al., 2007). It has been suggested that large-scale, government efforts to eliminate stigma are possible (NASEM, 2016b). Indeed, Bahora and colleagues (2008) demonstrated a significant decrease in social distance toward cocaine and alcohol dependence among police officers who received interactive and instructive crisis intervention skills training.
Health system structural approaches may also be effective. For example, the Health Policy Project has developed approaches to implement antidiscrimination policies and prevent infectious diseases by distributing injection equipment supplies and supporting other prevention efforts (HPP, 2011). The way in which physical spaces are designed can also increase, or mitigate, the stigma that patients experience (Sullivan, 2012). Physical changes can lower the stigma experience and the risk of unwanted exposure (Bil, 2016). For instance, a pharmacy in Zambia historically had two separate windows where medications could be picked up—one for people living with HIV and the other for remaining patients—thereby
inducing a stigmatizing and “othering” experience. Now all medications are picked up at the same window in this pharmacy (Topp et al., 2012).
During discussions with program informants the committee learned that some programs dealt with the issue of provider stigma during the early stages of integration. A number of informants also commented on the need to educate not just physicians, but also nurses, pharmacists, front-desk staff, and others to counter stigmatizing attitudes among all health professionals. Indeed, the literature supports this point, suggesting that clinical and nonclinical staff would benefit from stigma-reduction interventions (Nyblade et al., 2019). In addition, studies have found that it is important to emphasize that empowerment is key for both patients and health care providers in reducing stigma (Batey et al., 2016), to utilize technology for increased engagement with care (Nyblade et al., 2018), and to target existing policies that inadvertently increase stigma.
Findings
- Stigma surrounding opioid use disorder, substance use disorder, and infectious diseases is pervasive in many corners of society, including in medical care and behavioral health systems.
- Stigma and the lack of culturally competent care are likely key reasons that patients do not seek treatment, do not remain in treatment, or do not maintain strong social support systems (such as family or community ties).
- Research exists that can provide insight into scalable, sustainable interventions to reduce stigma broadly, and more specifically, among people who use drugs themselves (i.e., self-stigma), the general public, and health professionals.
Conclusions
- To effectively treat opioid use disorder and concurrent infectious diseases at scale, stigma must be significantly reduced in medical settings among medical professionals at all levels, among people who use drugs, and among the public more generally.
- Individuals struggling with opioid use disorder must be made to feel that they can seek nonjudgmental, compassionate, patient-centered, and culturally competent treatment.
Recommendation 3-13: The Substance Abuse and Mental Health Services Administration should support implementation of multi-level, sustainable, evidence-based, and measurable intervention strategies aimed at reducing stigma in clinical set
tings against people who use drugs, people who inject drugs, and people undergoing treatment with medications for opioid use disorder or who have infectious diseases. Such efforts should be targeted toward a range of health professionals (e.g., counselors, prescribing health professionals, front-desk staff, and others) across geographic regions of the United States, and the evaluations and results from these interventions should be made publicly available.
PAYMENT AND FINANCING LIMITATIONS
Eight of the programs interviewed commented on the difficulty in finding sustainable, long-term sources of funding for services they were providing or aimed to provide. This was especially true for harmreduction services (including syringe service programs), telemedicine, case management, and peer-recovery counselors.
There is a robust literature describing effectiveness and cost-effectiveness of syringe service programs in preventing new cases of infectious diseases among people who inject drugs. A systematic review found consistent effects across 15 studies, with decreases in HIV and HCV incidence and prevalence (Abdul-Quader et al., 2013). Other studies have found similar effects (Des Jarlais et al., 2005), and still others have observed that syringe service programs are cost-effective, saving dollars in the long run by preventing new cases of infectious diseases (Belani and Muennig, 2008; Nguyen et al., 2014). Despite this evidence, federal funding for syringe services has been minimal or inconsistent (Showalter, 2018). In 2016, Congress passed legislation allowing HHS to fund syringe service programs, reversing a decades-long prohibition against using federal funds to support syringe service programs.11 However, the law came with several caveats. First, the funds could not be used for syringes or syringes themselves or for cookers, only for ancillary costs associated with the service (e.g., staff salaries, quality assurance, other supplies, testing kits for viral hepatitis and HIV, or syringe disposal equipment). While syringes and other paraphernalia are relatively inexpensive, they are the very tools that are directly responsible for reducing the transmission of blood-borne infections and are often the reason patients first visit a syringe service program. Notably, however, costs for equipment that is not allowable with federal funding can range between 11 and 28 percent
___________________
11 Early evidence demonstrated that syringe service programs that received state or local funding were able to offer more services, including HIV testing and counseling, and distribute more syringes than programs not receiving public funds (Des Jarlais et al., 2004). More recent evidence supports these findings (Bramson et al., 2015).
of the total annual costs to operate a syringe service program. This suggests that allowing federal funding for this equipment may incentivize more syringe service programs to open, or would assist currently operating programs with their ongoing expenses (Teshale et al., 2019). If the ban on federal funding remains, on the other hand, it is expected that syringe service programs will not be able to offer additional services (e.g., testing for infectious diseases), as a large percentage of their budget will be devoted to purchasing injection equipment. This is especially so for syringe service programs located in states where no state or local funding is available (Bramson et al., 2015). Second, the programs were required to provide evidence that the surrounding region was “experiencing or at risk for significant increases in hepatitis infections or an HIV outbreak due to injection drug use” (CDC, 2019a). In general, the policy landscape around syringe services has changed somewhat rapidly in recent years, creating legal, policy, and funding confusion for these programs (Jones,
2019). Lifting the prohibition on funding equipment and increasing overall federal and state funding is vital to scaling up a robust network of syringe service programs. It should also be mentioned that states can independently fund syringe service programs (including the provision of injection equipment), and that state funding has been shown to increase the number of services that syringe service programs can offer (e.g., testing for infectious diseases onsite) (Bramson et al., 2015). Syringe service programs have the potential to serve as a low-threshold access point for a wide range of health and social services for people who inject drugs, but spatial access to them remains limited: as of 2019, there were fewer than 400 syringe service programs nationwide, and a number of states have none (amfAR, 2019).
Several programs also mentioned that case management services were difficult to fund, despite the great need for effective case management for patients with comorbid OUD and infectious diseases. The Ryan White
program allows for wraparound services (including case management and transportation reimbursement) for people living with HIV, services that have been shown to be effective in increasing care retention and viral suppression (Kay et al., 2018). Programs interviewed mentioned that similar services for those with OUD or other infectious diseases besides HIV would provide significant benefits to patients (in addition to continuity in insurance coverage, as is described further with respect to Medicaid in the criminal justice section later in this report).
Similarly, programs that incorporated peer addiction recovery counselors or specialists also mentioned difficulties in sustaining funding for these positions. This is in line with published literature: Englander and colleagues (2019) created a list of recommendations for sustaining these positions, mentioning that peer services are frequently not billable. Hence, other funding mechanisms are required.
More generally, programs mentioned that they frequently had to create a patchwork of funding and build the financial case for integration to provide integrated OUD and infectious disease services. Some community health center programs received funding under HRSA’s Health Center Program, such as Federally Qualified Health Centers (FQHCs),12 some programs received Ryan White funding that was used to provide OUD services, and others received a mix of grant funding to provide other ancillary services. A 2019 study showed that lack of resources, staff, or funding were primary reasons why programs elected not to provide MOUD in their clinics (Kepple et al., 2019). Nevertheless, there are government programs available for assistance. SAMHSA, for instance, provides technical assistance and funding opportunities (SAMHSA, 2019b) for programs and communities to address OUD prevention, treatment, and recovery (SAMHSA, 2019h), as well as for the integration of primary and behavioral health care (though this funding opportunity does not specifically address the interplay between OUD and infectious diseases) (SAMHSA, 2019f). There may be other government-sponsored mechanisms for programs to sustain their services. In the SUPPORT Act of 2018, Congress called upon CMS and the Center for Medicare & Medicaid Innovation (CMMI) to test new models of funding for programs to deliver MOUD; similar efforts could be made to test models of funding for integrated care between OUD and infectious diseases. In addition, there are many published models of funding at the state level—such as bundled payment models that provide comprehensive services for patients with OUD—that
___________________
12 FQHCs are designated community health centers that operate as part of the Health Center Program administered by the Bureau of Primary Health Care within the Health Resources and Services Administration. The Health Center Program provides grants to FQHCs under Section 330 of the Public Health Service Act (42 U.S.C. § 254b) (GAO, 2018).
could be scaled up and incorporated with infectious disease care or propagated to other states (Gueronniere, 2019; O’Brien et al., 2019). This could be accomplished, for instance, through the use of Section 1115 authority to institute experimental, pilot, or demonstration projects to test and evaluate changes to state Medicaid programs (NCSL, 2017). Each of the aforementioned models may hold promise for restructuring financing systems to better integrate services for OUD and infectious diseases.
Informants for this study—and the committee—drew parallels between the current opioid crisis and the HIV crisis in the late 20th century. In 1989, the year before the CARE Act was passed, the number of reported cases of HIV had reached 100,000. In its first year, the CARE Act provided $220.5 million in funding for community-based care and treatment services, managed by HRSA (HHS, 2019a). The CARE Act is viewed today as a crucial piece of legislation for reducing the burden of HIV/AIDS on the public’s health (HRSA, 2019a; Sood et al., 2014). The program provides easier access to medication, and as of 2017, 85.9 percent of patients receiving its support were virally suppressed, compared to the national average of 59.8 percent (HRSA, 2019a).
In 2018, more than 2 million people had OUD, 808,000 people used heroin, and tens of thousands were killed as a result of opioid overdose (HHS, 2019d; NIDA, 2019). The mortality rate from opioids is now higher than that of HIV at its peak, despite the fact that effective medications exist to treat OUD and none existed early in the HIV epidemic (Berger, 2019). Indeed, there is drop-off at every level of the opioid care cascade. Many patients cannot access treatment, many that access treatment are not retained, and many who are retained in treatment undergo relapse or overdose (Williams et al., 2017). This drop-off in effectiveness may be due in large part to the lack of services available at every stage in care. Importantly, the types of services provided by Ryan White funding for people living with HIV—including wraparound services and those that address other social determinants of health—were mentioned by interviewed programs as being difficult to fund for patients with OUD who were not also living with HIV. Programs mentioned that the same level of funding attention is required for OUD as was provided in the early years of the HIV epidemic.
Findings
- Syringe service programs are effective in reducing the transmission of infectious diseases and engaging patients in care, yet there are federal restrictions on funding for injection equipment.
- Funding to pay for integrated services is insufficient or difficult for some programs to find and obtain. Often, programs have to
-
use a patchwork of funding to deliver integrated opioid use disorder and infectious disease services.
- The opioid care cascade model, as has been currently proposed in Williams et al. (2019), consists of metrics for assessing and ameliorating opioid use disorder through prevention, identification, treatment, and recovery.
- The Substance Abuse and Mental Health Services Administration is a source of technical advice on integration, offering resources about the ways in which programs can be coordinated/integrated, including from a payments and finances perspective.
- When a similar public crisis caused by HIV was identified, it was necessary and transformative for the Department of Health and Human Services to fund gaps in care through the Ryan White Comprehensive AIDS Resources Emergency Act.
Conclusions
- Syringe service programs are a crucial element in reducing the spread of infectious diseases and increasing connection to care for opioid use disorder.
- Stable, easily accessible sources of funding are needed to ensure fully integrated services for opioid use disorder and infectious diseases (and primary care and substance use disorder more generally).
- Much like the human immunodeficiency virus care cascade model, the opioid care cascade model could be an effective framework for the government in assessing how to reduce the harm associated with opioid use disorder.
- The Substance Abuse and Mental Health Services Administration is well positioned to provide both the funding and technical assistance needed for programs to integrate services for opioid use disorder and infectious diseases.
- By harmonizing funds with evidence-based preventive and therapeutic services, the Ryan White Comprehensive AIDS Resources Emergency Act not only funded but also shaped the national response to the HIV epidemic and sharply reduced HIV-related mortality.
Recommendation 3-14: Congress should ensure that federal funds can be used to purchase injection equipment at syringe service programs.
Recommendation 3-15: The Substance Abuse and Mental Health Services Administration should support programs attempting to implement quality care through integrated services (e.g., from
colocated services to fully integrated) through grants that provide technical assistance on implementation of integration strategies, while also collecting data to form an evidence base about the best strategies for future integration.
Recommendation 3-16: The Substance Abuse and Mental Health Services Administration and the Health Resources and Services Administration and other government funders should require that organizations receiving funding for opioid use disorder (OUD) and infectious disease services submit information on a regular basis with data related to the opioid care cascade model and their plans for using the care cascade model to prevent, identify, treat, and promote recovery for patients with OUD.
Recommendation 3-17: Congress should authorize and appropriate funding for the Health Resources and Services Administration to comprehensively address the needs of low-income uninsured or under-insured individuals with co-occurring opioid use disorder and infectious diseases. Such an effort should encompass a full range of services—including integration of prevention and treatment services—as well as services that address the social determinants of health (e.g., housing and transportation). Furthermore, the effort should develop clear metrics of success and require participating organizations to report these metrics as a condition for participation. The committee recognizes that policy makers will need to wrestle with program specifics such as the specific services to be covered, coordination with other federal programs, program standards, and eligibility levels.
SAME-DAY BILLING RESTRICTIONS
Reimbursement regulations at the state level were mentioned as a barrier for five programs interviewed for this study. Some states prohibit an organization from billing for both behavioral and physical health care visits on the same day, referred to as “same-day billing” (SAMHSA, 2018a). For programs seeking to provide integrated care between OUD and infectious diseases in the same facility, this restriction poses a difficulty (Bachrach et al., 2014). For some programs, the most viable option may be to provide behavioral health services without seeking reimbursement, or to ask that the patient return on a different day (Miller et al., 2013).
The federal government does not prohibit same-day billing; rather, state Medicaid reimbursement rules dictate whether this practice is allowed.
As of 2019, 13 states had same-day billing restrictions (Henderson, 2019). Increasingly, states are modifying these rules to allow for same-day billing (Brown and McGinnis, 2014). For example, Florida’s Medicaid reimburses providers for up to three medical encounters per day (physical, dental, and behavioral health); Washington State allows multiple providers to bill on the same day for the same patient, or the same provider to bill on the same day for unrelated diagnoses (Houy and Bailit, 2015).
Although interdisciplinary treatment may encourage the best patient outcomes, medical visits are often billed at a higher rate and are therefore prioritized in states with same-day billing restrictions (Monson et al., 2012). This poses a financial-sustainability problem for programs seeking to integrate care, as they may only be able to seek reimbursement for a fraction of the care provided.
In addition, same-day billing restrictions may have unequal effects across different populations. Low-income individuals and racial/ethnic minorities are less likely to have secure transportation or the ability to skip work for an additional appointment, and are more likely to be covered by Medicaid (Syed et al., 2013). They may be less likely to make a second appointment on a different day if needed, preventing full continuity of care and integration between behavioral and physical health.
As mentioned, states are revising same-day billing regulations. Still, because state-level changes are happening relatively quickly, it is important that practitioners are made aware of the changes so they may provide the most effective integrated care possible (Roby and Jones, 2016). At the federal level, CMS often provides guidance or information to state
Medicaid programs through several mechanisms, including regulations, state Medicaid director letters, state health official letters, FAQs, and informational bulletins. In response to the interrelatedness of the opioid and infectious disease epidemics, CMS could encourage states to remove same-day billing restrictions. It could accomplish this through informational bulletins, as bulletins do not “establish new policy or issue new guidance” but rather “share information, address operational and technical issues, and highlight initiatives or related efforts” (CMS, 2019a).
Finding
- Some state Medicaid administrators prohibit a medical care organization from billing for both behavioral and physical health care visits on the same day.
Conclusion
- The restriction on same-day billing is a barrier to providers seeking to integrate care, as it means that patients either need to come back on a separate day or the provider must provide services without seeking reimbursement.
Recommendation 3-18: State Medicaid administrators should revise their billing policies to allow for more than one service in a given day (e.g., allow for one physical and one behavioral visit per day; allow multiple providers to bill on the same day
for the same patient; or allow the same provider to bill on the same day for different diagnoses, such as opioid use disorder and infectious diseases).
Recommendation 3-19: The Centers for Medicare & Medicaid Services should issue an Information Bulletin to state Medicaid programs, sharing information about how states have removed same-day billing restrictions and highlighting the importance of removing these restrictions for providing integrated care.
LIMITS ON HARM-REDUCTION SERVICES
As mentioned in the Introduction, the committee focused on harmreduction strategies when interviewing programs and developing recommendations. According to the Harm Reduction Coalition, a not-for-profit organization focused on reducing the stigma surrounding substance use, “harm reduction is a set of practical strategies and ideas aimed at reducing negative consequences associated with drug use. Harm reduction is also a movement for social justice built on a belief in, and respect for, the rights of people who use drugs” (HRC, 2019). Harm reduction is at the center of integration between OUD and infectious disease services, aiming to reduce the danger associated with OUD and new infections. Practices aligned with this include clean syringes rather than used, widespread distribution of naloxone to people who use drugs (and to the family members of individuals with OUD), pre-exposure prophylaxis, Good Samaritan laws, tapered use of substances, low-barrier entry to treatment programs, and maintenance in treatment despite continued used of illicit substances (Ball, 2007; Hawk et al., 2015; Marlatt, 1996; Van Den Berg et al., 2007). Harm-reduction practices related to OUD that have the greatest evidentiary support are syringe service programs, MOUD, overdose prevention efforts, and drug prevention programs for adolescents and young adults (Marlatt and Witkiewitz, 2010). A harm-reduction approach to providing care to persons who use drugs includes respecting patients’ decisions; setting realistic expectations and accepting any positive change to improve health; tailoring support and care to patients’ needs; and providing services without judging, stigmatizing, or requiring abstinence (Hawk et al., 2015).
The committee asked each of the programs about their practices and experiences with harm reduction, which revealed several themes related to harm reduction and integrated OUD and infectious disease services. The first is the importance of providing avenues for small steps toward health and well-being. As one program mentioned, decreasing heroin use from several times per week to once per week represents a significant reduction in the harm associated with continued use and the risk of contracting an infectious disease.
A second theme was the need for low-threshold entry into treatment and low-threshold maintenance in treatment. Several programs used the phrase “meeting patients where they’re at” to specify that treatment programs needed to be flexible to the individual needs of a patient. This could mean an easy access point for patients to begin buprenorphine at home, rather
than having to come into a clinic. In addition, programs mentioned that it was essential to maintain patients in treatment programs even if they were continuing to use; viewing continued drug use as a “failure,” for instance, would only provide opportunities for further stigmatization and harm (e.g., lack of OUD care leading to contracting HIV or viral hepatitis).
A third theme was the importance of state and regional support for syringe service programs, a strategy that has proved effective in preventing new infectious diseases for several decades (NRC, 1995). The evidence of syringe service programs’ effectiveness is well known, and the cost of equipment to syringe service programs can be high (Teshale et al., 2019). Several programs mentioned that state regulations or city ordinances prevented them from supplying clean syringes to patients to reduce the incidence of infectious diseases. This point was especially important in light of how syringe service programs can lead to treatment: several programs stated that local syringe services were frequently the entry point for patients to get tested for infectious diseases or to start MOUD. Insofar as syringe service programs can be the avenue for reduced use of injectable drugs and for safer sexual behaviors, they may reduce the risk of contracting infectious diseases. These programs have increased in number in the past several decades and have provided a convenient and accessible avenue for patients to access other kinds of testing and treatment (Des Jarlais et al., 2009, 2015; Eckhardt et al., 2018; Hagan et al., 1995; Islam et al., 2012; Rich et al., 2004). Still, according to 2019 data from the North American Syringe Exchange Network—which tracks syringe service programs who self-report their services—10 states had no programs, and another 9 had only one or two (amfAR, 2019). This is despite the fact that modeling studies demonstrate syringe service programs can significantly reduce the incidence of infectious diseases (Gonsalves and Crawford, 2018). Notably, congressional appropriations acts have placed a restriction on using federal funds to purchase syringes (Consolidated Appropriations Act of 2019, Pub. L. No. 1116-6), which can be expensive for individual syringe service programs (Teshale et al., 2019).
A final theme relevant for integrating OUD and infectious disease services was the importance of having a workforce that valued and believed in harm-reduction principles. Several programs stated that a culture shift was required in the workforce to continue to “meet patients where they’re at” and provide treatment even if patients continue to use illicit substances.
Findings
- Harm-reduction principles are aligned with a nonjudgmental, patient-centered approach that does not require abstinence and builds on small steps toward health and well-being.
- Programs interviewed for this study—as well as a preponderance of findings from the literature—support evidence-based harm reduction as an effective practice in preventing infectious diseases and increasing engagement in medical care, especially when such services have a low barrier to entry.
- The goals of harm reduction and medications of opioid use disorder are consistent and complementary with one another: to reduce the overall harm associated with drug use and prevent infectious diseases.
- Harm-reduction services are not universally supported at the federal, state, and local levels, including funding and support for syringe service programs.
Conclusions
- The effectiveness of harm-reduction strategies is well supported by evidence but is not widespread in substance use disorder care. This poses a problem in the effort to mitigate the burden of infectious diseases and opioid use disorder on patients and health systems.
- Organizations that deliver care for opioid use disorder and infectious diseases could improve patient outcomes by offering low-threshold services and treatments and adopting a harm-reduction approach.
Recommendation 3-20: Individual clinics, health care programs, and providers should incorporate harm-reduction strategies into both infectious diseases and opioid use disorder care, such as by linking patients to syringe service programs, distributing naloxone, adopting a harm-reduction philosophy focused on patient-centered care, prescribing pre-exposure prophylaxis, and providing safe drug use and safe-sex education.
Recommendation 3-21: States should lift the remaining bans on evidence-based syringe services, offering syringe services at publicly funded health departments and allowing for independently operated syringe service programs.
Recommendation 3-22: The Substance Abuse and Mental Health Services Administration should make available grants for researchers from a broad set of disciplines (medicine, nursing, epidemiology, behavioral science, health policy, and implementation science) to conduct research on the integration of opioid use disorder and infectious disease care under a harmreduction lens.
DISCONNECT BETWEEN THE HEALTH AND CRIMINAL JUSTICE SYSTEMS
More than 200,000 active heroin users pass through the correctional system annually (McKenzie et al., 2009), and in 2010 nearly 85 percent of incarcerated individuals had a history of (or current) SUD, were arrested while under the influence, committed an offense to obtain drugs, or were incarcerated for a drug-related crime (Califano, 2010). Rates of HIV and viral hepatitis are considerably higher in correctional facilities than among the general public (Baillargeon et al., 2017; Rich et al., 2014). Moreover, those in the criminal justice system with OUD have poorer overall health, greater frequency of sexually transmitted infections, and viral hepatitis and HIV at higher rates than those without OUD (Winkelman et al., 2018). This evidence suggests that the need to integrate OUD and infectious disease care is especially high in the criminal justice system and that there is a great opportunity to reach a large number of patients with comorbid illness through such integration.
Most persons in the criminal justice system are not offered SUD treatment; for OUD, most patients are not offered buprenorphine, methadone, or naltrexone (Chandler et al., 2009; Springer et al., 2011; Volkow et al.,
2014). Upon release, many patients relapse quickly, and overdose is a primary cause of death in the subsequent 2 weeks (Binswanger et al., 2013). Risk of poor health outcomes for infectious diseases are also high directly following release: Although individuals living with HIV who are involved in the criminal justice system can achieve viral suppression prior to release, it is often lost within 3 months afterward (Meyer et al., 2014; Springer et al., 2004; Stephenson et al., 2005). This can occur even when discharge planning, case management, and other social services are in place (Teixeira et al., 2015), though some evidence suggests that MOUD in conjunction with HIV medications can produce positive outcomes for recently released patients (Springer et al., 2010).
While testing and treatment of HIV in correctional facilities has increased in the past several decades, it is not altogether common that correctional facilities have adopted universal opt-out screening for infectious diseases (Morris et al., 2017; NASEM, 2017); a lack of political will and the high cost of effective HCV treatment are barriers to screening in these facilities (Spaulding et al., 2017). This is despite the fact that HCV treatment during incarceration has been shown to be feasible and cost-effective (Assoumou et al., 2019; He et al., 2016). In addition, while there are effective vaccines for hepatitis A virus and hepatitis B virus,
they are not universally provided across correctional facilities in the United States (Sequera et al., 2015). Entry into the criminal justice system itself is strongly correlated with increased HIV and HCV acquisition among people who inject drugs (81 percent and 62 percent increased risk, respectively) (Stone et al., 2018).
Eight programs mentioned various aspects of the criminal justice system as barriers to providing high-quality, integrated care for OUD and infectious diseases. Specifically, programs mentioned that (1) a lack of open communication between stakeholders (e.g., law enforcement, correctional facilities, public health practitioners, treatment clinics) inhibits patient-centered care and coordination, (2) there is generally inadequate treatment within correctional facilities, and (3) that the transition out of criminal justice settings represents a critical period for reaching patients and providing care.
There has been a movement in the direction of greater coordination between public health and the criminal justice system in recent years, and recommendations for reform (AMA, 2019). Police, courts, and correctional systems can improve access to treatment (Clifasefi et al., 2017) and growing use of naloxone by law enforcement officers and Good Samaritan laws represent steps toward integrating public health with the criminal justice system (Davis et al., 2014; Tanaka, 2019). Treatment as an alternative to arrests has been tried with success in some jurisdictions, such as in Seattle (Clifasefi et al., 2017). Informants from the Plumas County Public Health Agency attributed a cross-county coalition of stakeholders (including law enforcement officials) as a major driver of their success in integrating responses to OUD and infectious diseases.
Still, the lack of treatment options within correctional facilities represents a barrier to achieving a sustained response to the correlated incidence of OUD and infectious diseases. It is not common practice throughout the United States to provide MOUD in correctional facilities (Beletsky et al., 2015), though access is increasing with recent legal challenges (Nicholas, 2019). A small study in Rhode Island demonstrated the benefit of MOUD in correctional facilities. Following a state policy change, incarcerated individuals in the state are able continue to receive such medications if they were taking them prior to incarceration. In addition, incarcerated individuals are able to initiate medications when needed. The study tracked the impact of this policy, finding a 60 percent reduction in overdose deaths among formerly incarcerated individuals in the subsequent 6 months and a 12 percent reduction in overdose deaths across the state for the following year (Green et al., 2018). Given the high risk of overdose death following release (Binswanger et al., 2013; Ranapurwala et al., 2018), policies that improve continuity of treatment for incarcerated individuals are likely to reduce overdose mortality. The Pew Charitable
Trusts has conducted recent research on health care delivery in criminal justice settings, reviewing data that show a $4.29 return on every dollar spent in jails and prisons to treat SUD (Urahn et al., 2018).
Because viral suppression is critical to reduce HIV transmission, it is important to note that there is evidence for a reduction in relapse and overdose (Lee et al., 2016) and improved HIV viral suppression (Springer et al., 2012, 2018) when persons are offered MOUD before release from prison or jail (Kinlock et al., 2008; Lee et al., 2016).
Other states have taken similar steps to improve the connection between the public health and criminal justice systems. The Denver Health Medical Center, for instance, partnered with city and county jails to both start and maintain patients on MOUD while incarcerated. SAMHSA has developed a toolkit for health care organizations to develop partnerships with the intent of integrating services (SAMHSA, 2015b). In addition, reentry services are available, allowing recently released individuals to maintain their medications and access case management services. This effort is funded by a state tax on marijuana sales, a federal grant (State Targeted Response to the Opioid Crisis), and state general funds (Connolly, 2019). Other states have implemented measures to increase access to naltrexone for recently released individuals or fund prison-based social workers to coordinate care upon release (Connolly, 2019). Following lawsuits brought by inmates in Massachusetts, state prisons and jails will now provide buprenorphine to newly incarcerated individuals who were already taking it and for those going through opioid withdrawal (Westervelt, 2019). Counties and cities typically operate and fund jails, though states may also contribute funding, and some states finance both prisons and jails (Urahn et al., 2018). Because of this, the cost of mandates for treating patients within jails falls upon these local jurisdictions and states, which may not have the funds available (Urahn et al., 2017a, 2018), thereby reducing the incentive to screen individuals entering the system. This is especially true for medications for HCV and HIV, given the high prevalence of these diseases in correctional settings and therefore the high costs associated with treatment (Urahn et al., 2017a). Indeed, spending at the state level for correctional facilities typically ranks third, behind Medicaid and education (NRC, 2014). Because persons in jails or prisons are not eligible for coverage by Medicaid, many correctional facilities fund treatments for individuals in criminal justice settings through state block grants or direct appropriations at the state level (SAMHSA, 2019i). A number of states and jurisdictions have implemented programs to offer MOUD in prisons or jails or for individuals after release (SAMHSA, 2019i). These models are precedents for delivering treatment in these settings. The SUPPORT for Patients and Communities Act of 2018 authorizes HHS to provide grants to state agencies to carry out SUD preven-
tion, treatment, and evidence-based programs (including with MOUD); establish grant funding for comprehensive opioid recovery centers; prevent overdoses; coordinate communities of recovery; and fund surveillance and education regarding infections associated with opioid use (Pub. L. No. 115-271). Eligible grantees could consider using these funds for improved treatment access in correctional facilities, linkage to care following the transition out of correctional facilities, or better integration of care for OUD and infectious diseases.
As several programs mentioned, the transition out of incarceration represents a crucial period for intervention to better treat both OUD and infectious diseases. Recently released people face issues of housing insecurity, under-employment, food insecurity, lack of community or family ties, and chronic illness (Freudenberg et al., 2005). In addition, they are at increased risk for opioid overdose and mortality, especially in the first 2 weeks following release (Binswanger et al., 2013; Ranapurwala et al., 2018). Medications for OUD are effective at increasing the time to relapse and decreasing the chances of relapse following release from correctional facilities (Urahn et al., 2018), and those who have received medications in jail are less likely to return to jail and will spend a longer time in the community before recidivism (Urahn et al., 2018). Many jails contract directly with vendors to provide health care. In this context, it is notable that a recent Pew study documented that a minority of correctional facilities request any MOUD services from the health care providers they contract with, or if they do, tend to offer them only to pregnant women (Urahn et al., 2018). As of 2016, only 13 state departments of corrections provided MOUD upon release (Urahn et al., 2017b). In 2017, 30 out of 5,100 U.S. prisons and jails offered methadone or buprenorphine (SAMHSA, 2019i).
The Bronx Transitions Clinic (BTC) and the Transitions Clinic Network (an umbrella organization coordinating information between many transition clinics) were both interviewed for this study. Data from these clinics illustrate both the promise and difficulty in coordinating care for recently released individuals. One 2019 Connecticut study found that formerly incarcerated individuals being cared for in a transitions clinic were less likely to return to prison for a parole or probation violation and were incarcerated for less time than a matched control group (Wang et al., 2019).
Still, access to care does not guarantee positive outcomes. In the Bronx, of 135 patients recently released from prison, fewer than half were retained in care at 6 months. This was especially true for those with opioid dependence (Fox et al., 2014). HIV patients had generally positive outcomes and higher retention in care, which the authors attribute to the more robust wraparound services through state and federal programs. Another study from the BTC found that chronic HCV infections were common, but went untreated and uncured, pri-
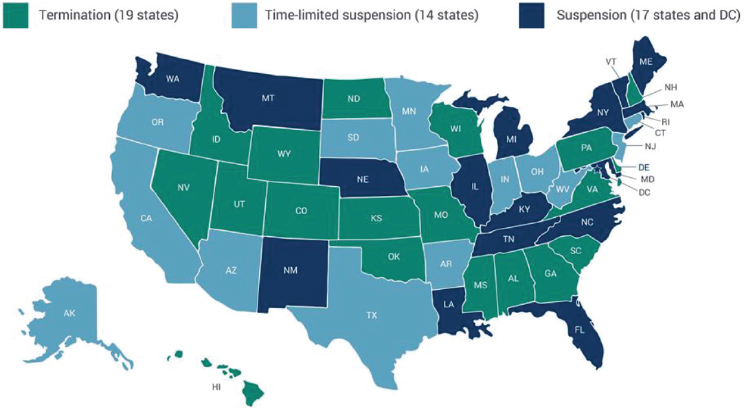
NOTES: Colorado and Hawaii recently passed laws to suspend rather than terminate Medicaid enrollment and are in the process of implementing the law. Some states specify that suspension policies apply to specific prisons and jails.
SOURCES: MACPAC, 2018a.
marily because patients were not retained in care (Hawks et al., 2016). These data suggest that primary care services are necessary but not sufficient to ensure effective reintegration and management of chronic diseases, such as OUD.
One additional barrier to preventing a seamless transition out of correctional settings—and maintaining suppressed viral load for infectious diseases—is continuity of insurance coverage. State policies on the continuation of Medicaid in and out of correctional settings vary, as shown in Figure 3-1. Most states suspend Medicaid while an individual is incarcerated, varying in time from 30 days to the full length of the sentence. Coordination is required between the corrections and state Medicaid systems to ensure that newly incarcerated individuals are suspended from Medicaid and that newly released individuals’ coverage can be reinstated (MACPAC, 2018a; Ryan et al., 2016). As one program mentioned, this coordination can be difficult to achieve because incarcerated individuals may be released with little notice. In addition, many state Medicaid programs—and state-regulated private insurers—do not cover all three medications approved for OUD, thereby limiting patients’ access to these medications entering and exiting criminal justice settings (SAMHSA, 2019d).
Several states have taken steps to improve continuation of coverage for formerly incarcerated individuals. In Ohio, for instance, peer navigators assist those who are incarcerated with enrolling in Medicaid upon release; Illinois has a similar program. Connecticut, on the other hand, uses a short eligibility form to simplify the process by which formerly incarcerated individuals can access Medicaid coverage, and 60 percent of those who are incarcerated are enrolled in Medicaid before release (MACPAC, 2018a; Ryan et al., 2016).
Findings
- A vast majority of incarcerated individuals have some connection with substance use disorder (SUD): they have a history of (or current) SUD, were arrested while under the influence, committed an offense to obtain drugs, or were incarcerated for a drug-related crime.
- Rates of infectious diseases (including human immunodeficiency virus and viral hepatitis) are higher in correctional facilities than in the general public and higher still for incarcerated individuals with opioid use disorder.
- There is often a lack of communication between law enforcement, correctional facilities, and treatment programs regarding patients/inmates substance use disorder.
- Evidence-based treatment for substance use disorder in correctional facilities is generally nonexistent or inadequate. The same is often true for some infectious diseases, particularly hepatitis C virus. There are mechanisms by which states have begun to provide treatment for opioid use disorder and infectious diseases in criminal justice settings.
- The transition out of criminal justice settings is the time when users are most likely to overdose on opioids.
- States vary in their policies for continuation of Medicaid coverage following time spent in a correctional facility.
Conclusions
- Historically, substance use in the United States has been treated as a criminal justice issue rather than a public health or medical issue, which has inhibited effective, patient-centered care.
- The lack of communication between health professionals/systems and the criminal justice system inhibits patient-centered care and coordination.
- The lack of treatment within correctional facilities for opioid use disorder increases the chances that patients will continue to use drugs upon release, and therefore increases the risk of infectious diseases. Lack of treatment for infectious diseases in correctional facilities causes harm to patients and increases the risk of infection for others.
- Special attention must be paid to the period just before release from correctional facilities, and care must be lined up at this stage to prevent overdose and promote recovery.
- Discontinuity of Medicaid coverage is likely to cause financial hardship among patients who do not realize they have become unenrolled, which may limit their access to treatment for opioid use disorder and infectious diseases.
Recommendation 3-23: Through federal grant funding, state block grants or direct appropriations, states should fund—and correctional facilities should offer—evidence-based screening and treatments for opioid use disorder and co-occurring infectious diseases.
Recommendation 3-24: Clinics and organizations that treat opioid use disorder and infectious diseases should coordinate with law enforcement and correctional facilities to better track and maintain records of patients entering and exiting the criminal justice system.
Recommendation 3-25: Through federal grant funding, state block grants or direct appropriations, states should fund high-quality, evidence-based reentry services for prisons and jails, including medications for opioid use disorder and infectious diseases, as well as linkage to care in the community and harmreduction services following release (e.g., naloxone to reduce the risk of fatal overdose).
Recommendation 3-26: State Medicaid administrators should adjust policies to ensure that individuals previously enrolled in Medicaid before entering the criminal justice system are automatically re-enrolled at the time they are released.
































































