Summary
Social isolation (the objective state of having few social relationships or infrequent social contact with others) and loneliness (a subjective feeling of being isolated) are serious yet underappreciated public health risks that affect a significant portion of the older adult population. Approximately one-quarter (24 percent) of community-dwelling Americans aged 65 and older are considered to be socially isolated, and a significant proportion of adults in the United States report feeling lonely (35 percent of adults aged 45 and older and 43 percent of adults aged 60 and older). While there are challenges in measuring social isolation and loneliness precisely, there is strong evidence that many older adults are socially isolated or lonely in ways that puts their health at risk. For example:
- Social isolation has been associated with a significantly increased risk of premature mortality from all causes;
- Social isolation has been associated with an approximately 50 percent increased risk of developing dementia;
- Loneliness among heart failure patients has been associated with a nearly four times increased risk of death, 68 percent increased risk of hospitalization, and 57 percent increased risk of emergency department visits; and
- Poor social relationships (characterized by social isolation or loneliness) have been associated with a 29 percent increased risk of incident coronary heart disease and a 32 percent increased risk of stroke.
Understanding the full scope and complexity of the influence of social relationships on health is challenging. In addition to the absolute number or extent of social relationships, the quality of such relationships is also an important factor in their impact on health. Two aspects of social relationships, social isolation and loneliness, have become increasingly prominent in the scientific literature. While both social isolation and loneliness can affect health throughout the life course, this report focuses on the health impacts of social isolation and loneliness among adults aged 50 and older. Of note, it is incorrect to assume that all older adults are isolated or lonely or that aging, independent of other factors, causes social isolation and loneliness. Rather, older adults are at increased risk for social isolation and loneliness because they are more likely to face predisposing factors such as living alone, the loss of family or friends, chronic illness, and sensory impairments. Over a life course, social isolation and loneliness may be episodic or chronic, depending on an individual’s circumstances and perceptions.
Many approaches have been taken to improve social connections for individuals who are socially isolated or lonely, but opportunities to intervene may be most challenging for those who are at highest risk. For example, people who do not have consistent interactions with others (e.g., have unstable housing, do not belong to any social or religious groups, or do not have significant personal relationships) may never be identified in their own communities. However, nearly all persons 50 years of age or older interact with the health care system in some way. Therefore, this report focuses on the role of the health care system as a key and relatively untapped partner in efforts to identify, prevent, and mitigate the adverse health impacts of social isolation and loneliness in older adults.
STUDY CONTEXT AND CHARGE
A systematic and rigorous science of social relationships and their consequences, especially in terms of health, emerged in the latter part of the 20th century as part of a broader recognition of the role of social determinants of health. By the beginning of the 21st century, several aspects of social relationships were being studied systematically in research and had been identified as potential influences on human health. Only recently have the adverse health effects of social isolation and loneliness received public attention nationally and internationally. For example, in January 2018, Theresa May, the prime minister of the United Kingdom, established and appointed a Minister of Loneliness to develop policies for both measuring and reducing loneliness.
With support from the AARP Foundation, the National Academies of Sciences, Engineering, and Medicine (the National Academies) formed the Committee on the Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults in fall 2018. The committee’s charge essentially consisted of
two parts. First, the committee was charged with summarizing the evidence for how social isolation and loneliness affect health and quality of life in adults aged 50 and older, particularly among low-income, underserved, and vulnerable subpopulations (groups the committee refer to as “at-risk” populations). Second, the committee was charged with identifying and recommending opportunities specifically for clinical settings of health care to help reduce the incidence and adverse health impacts of social isolation and loneliness (such as clinical tools and methodologies, professional education, and public awareness) and to examine avenues for the dissemination of information targeted to health care practitioners.1
While this report focuses on the role of the health care system, the committee emphasizes that the health care system alone cannot solve all of the challenges of social isolation and loneliness; rather, the health care system needs to connect with the broader public health and social care communities. Furthermore, the committee recognizes that in the larger context of addressing social isolation and loneliness, the most effective interventions may not require the participation of the health care system. However, this does not mean that the health care system should not strive to help improve the health and well-being of those who suffer the adverse health impacts of social isolation and loneliness. In fact, health care providers may be in the best position to identify individuals who are at highest risk for social isolation or loneliness—individuals for whom the health care system may be their only point of contact with their broader community. In this way, the health care system can help those individuals to connect with the most appropriate care, either inside or outside the health care system. Therefore, the health care system has the potential to be a critical component of a much larger solution.
DEFINING ASPECTS OF SOCIAL RELATIONSHIPS
The broad, interdisciplinary scientific fields that together form the modern science of social relationships have used a variety of terms—social isolation, social connection, social networks, social support, social relationships, loneliness, and so forth—to refer to related situations. There are important distinctions among these terms in what they describe or measure, but they are often erroneously used interchangeably. An individual can be isolated and not feel lonely, or can feel lonely even if he or she is not isolated. Social isolation and loneliness represent distinct phenomena. Social isolation typically refers to the objective lack of (or limited) social contact with others and is marked by a person having few social network ties, having infrequent social contact, or, potentially, living alone.
___________________
1 The complete Statement of Task is presented in Chapter 1 of this report.
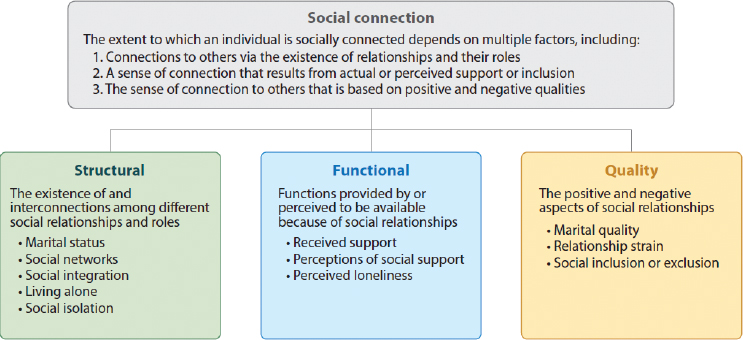
SOURCE: Holt-Lunstad, 2018a. Reproduced with permission from the Annual Review of Psychology, Volume 69 © 2018 by Annual Reviews, http://www.annualreviews.org (accessed March 13, 2020).
Loneliness, by contrast, refers to the perception of social isolation or the subjective feeling of being lonely. Although those who lack social contact may feel lonely, social isolation and loneliness often are not significantly correlated. Thus, it is important to distinguish between the two states.
The term “social relationships” is arguably the most common way of referring to the connections and intersections among human beings, and it derives from and is employed in broader common usage. In 1979 Berkman and Syme documented the strong association between social relationships and all-cause mortality and, hence, life expectancy, using the terms “social networks” and “social integration” to denote a broad pattern of social relationships (with both individuals and groups). Additionally, there has been much research on the concept of social support, the actual or perceived availability of resources from others. Over the past several decades there has been a new focus on loneliness as a risk factor for health. While each of these terms have been linked to important health outcomes, they are not highly correlated, suggesting that they may influence health through different mechanisms. Thus, the term “social connection” has been proposed to encompass the different conceptual and measurement approaches (see Figure S-1). Social isolation is reflected in Figure S-1 as a structural indicator of social connection while loneliness is functional indicator.
The literature concerning social isolation and loneliness uses all of these terms. To describe the evidence base as accurately as possible, when the evidence does not differentiate among or combines several related terms, this report uses
the term “social connection” to refer to the various structural, functional, and quality aspects of social relationships. This report uses the specific terms “social isolation,” “loneliness,” or other terms when the data are specific to these terms.2
GOALS AND RECOMMENDATIONS
The committee formulated its recommendations in accordance with five goals, each of which addresses an aspect of enhancing the role of the health care system in addressing the health impacts of social isolation and loneliness in older adults (see Box S-1). While not all of the recommendations are explicitly directed to clinicians or clinical settings of care, the committee identified recommendations that would be most helpful to reach the ultimate goal of developing and improving clinical interventions to mitigate the negative health impacts of social isolation and loneliness. Furthermore, the committee emphasizes that the preservation of an individual’s own decisions regarding his or her life is essential as a guiding principle for all interventions. The following sections discuss the overall goals and recommendations of this report, all of which apply to interventions in health care settings for adults aged 50 and older.
___________________
2 While social integration can describe high social connection, low scores on measures of social integration (e.g., on the Berkman–Syme Social Network Index) are frequently used as an indication of social isolation. Thus, the term “social isolation” will also be used to represent these data.
Goal 1: Develop a More Robust Evidence Base
While a substantial and growing body of evidence demonstrates the health impacts of social isolation and loneliness, the evidence base for interventions for specific populations or settings is less robust. Recommendations are provided for meeting the goal of developing a more robust evidence base on effective assessment, prevention, and intervention strategies.
Social Isolation, Loneliness, and Mortality
Social isolation and loneliness are as prevalent and play as large a role in today’s society as many other well-established risk factors for health, yet limited resources and attention have been committed to better understanding social isolation and loneliness and their individual and collective impacts on health. More than four decades of research has produced robust evidence that lacking social connection—and, particularly, scoring high on measures of social isolation—is associated with a significantly increased risk for premature mortality from all causes. Furthermore, there is some evidence that the magnitude of the effect of social connection on risk for mortality may be comparable to or greater than other well-established risk factors that are widely recognized and acted on by the public health and health care systems.
While there is evidence that loneliness is associated with mortality, the existing evidence does not yet approach the cumulative weight of evidence for the association between social isolation and mortality. More research is needed to establish the strength and robustness of the predictive association of loneliness with mortality in relation to social isolation and to clarify how social isolation and loneliness relate to and operate with each other.
RECOMMENDATION 2-1: Major funders of health research, including the government (e.g., the National Institutes of Health, the Center for Medicare & Medicaid Innovation, and the Patient-Centered Outcomes Research Institute), foundations, and large health plans should fund research on social isolation and loneliness at levels that reflect their associations with mortality.3
Risk Factors and Health Impacts
The relationships among risk factors, social isolation or loneliness, and health impacts can be reciprocal in that not only can being socially isolated or lonely have an impact on health, but the resultant health conditions can increase an
___________________
3 The committee’s recommendations are numbered according to the chapter of the main report in which they appear. Thus, Recommendation 2-1 is the first recommendation in Chapter 2.
individual’s likelihood of experiencing social isolation or loneliness. Furthermore, some factors may increase the risk for social isolation and loneliness (and ultimately, result in negative health impacts) while other factors may provide protective benefits. Substantial evidence indicates that social isolation, loneliness, and other indicators of social connection have associations with major forms of physical, cognitive, and psychological morbidity; health-related behaviors; and health-related quality of life. However, the evidence for specific impacts in the at-risk populations is sparse.
Beyond these associations, the mechanisms by which social connection, or lack thereof, affects the development and course of disease have been elucidated by a growing evidence base. Strong evidence links social isolation, loneliness, and other indicators of social connection to changes in biological and behavioral responses which may in turn influence health risk. Thus, current evidence supports plausible biological and behavioral mechanisms that explain how social isolation and loneliness ultimately influence health outcomes.
The committee identified the increased funding of basic research as key to developing a more robust evidence base on effective assessment, prevention, and intervention strategies for social isolation and loneliness (Goal 1). Specifically, the committee concluded that identifying, prioritizing, and developing ways to translate scientific knowledge about the impacts of social isolation and loneliness on health into effective and efficient clinical and public health interventions first requires a better understanding of how social isolation and loneliness are connected with each other and how they impact health. This includes understanding the mechanisms through which social isolation and loneliness affect health, the risk factors for social isolation and loneliness, and the factors that affect those relationships.
RECOMMENDATION 3-1: Major funders of health research, including the government (e.g., the National Institutes of Health, the Center for Medicare & Medicaid Innovation, and the Patient-Centered Outcomes Research Institute), foundations, and large health plans should fund research to improve the basic scientific understanding of the links between social connection and health, including the study of risk factors and mechanisms.
The Current Evidence Base for Interventions
The overall quality of the evidence for specific clinical and public health interventions for social isolation and loneliness in older adults is mixed. In part, this is due to the heterogeneity of older people themselves and the underlying causes of their isolation or loneliness. While there is some evidence for promising approaches, the committee concludes that researchers are only beginning to understand which specific approaches work best for which populations and which risk factors. In particular, the committee emphasizes that different intervention
approaches may be needed for social isolation versus loneliness. Furthermore, in the case of technological interventions, many gaps in understanding remain, particularly related to possible unintended harms and ethical concerns as well as the impact of current trends, such as the use of social media on future generations of older adults.
The committee identified three major aspects of the evidence base for effective clinical and public health interventions that need to be addressed in order to determine best practices and approaches: quality, funding, and research gaps. That is, the overall quality of the evidence base needs to be improved, adequate funding of research will be required, and research on major gaps in the current evidence base needs to be prioritized. Therefore, the committee makes the following recommendations:
RECOMMENDATION 9-3: Funders should prioritize research that builds a scientific foundation for clinical and public health interventions that reduce the health and medical impacts of social isolation and loneliness based on standard theoretical frameworks. Researchers and health care providers and systems that study interventions for social isolation or loneliness should consider the following key elements in the design and evaluation of any intervention in order to enhance the ability to compare across studies:
- A theoretical framework that drives particular approaches
- Appropriate choice of measure
- A specific target population
- Scalability
- Sustainability
- Ways to encourage data sharing
RECOMMENDATION 9-4: Major funders of health research, including the government (e.g., the National Institutes of Health, the Center for Medicare & Medicaid Innovation, and the Patient-Centered Outcomes Research Institute), foundations, and large health plans should fund research on interventions in clinical settings to identify, prevent, and mitigate the effects of social isolation and loneliness in older adults.
RECOMMENDATION 9-5: Those who fund, develop, and operate programs to assess, prevent, and intervene in social isolation and loneliness should prioritize research on the following major gaps in the evidence base:
- Tailored interventions based on a public health framework of primary, secondary, and tertiary prevention. In particular, researchers should examine improved measures to identify individuals who may be at
-
high risk for social isolation or loneliness and primary interventions in order to target such individuals.
- Trends among current younger adults as they age (e.g., use of technology, economic trends) to gain knowledge that informs future approaches to addressing social isolation and loneliness.
- Flexibility in funding to allow for the pilot testing and evaluation of innovative funding mechanisms for interventions.
- Approaches for assessments of and interventions among understudied groups of older adults (e.g., low income, lesbian, gay, bisexual, and transgender) and those who face unique barriers to health.
RECOMMENDATION 9-6: System designers as well as those who are developing and deploying technology in interventions should ensure that technological innovations related to social isolation and loneliness are properly assessed and tested so as to understand their full range of benefits and potential adverse consequences in order to prevent harm, and they should work to understand and take into account contextual issues, such as broadband access and having sufficient knowledge and support for using the technology.
Goal 2: Translate Current Research into Health Care Practices
Older adults are high-volume and high-frequency users of the health care system. Targeting the major social and behavioral risk factors for health offers a way to improve population health and even reduce health disparities. Health care delivery systems are exploring the feasibility and impact of using practice-based strategies to identify and address the social determinants of health, including social isolation and loneliness. Many intervention efforts for social isolation and loneliness focus only on community-based organizations, but given the evidence for the broad-reaching impacts of social isolation and loneliness on the health of older adults and the emerging evidence for their impacts on health care utilization, the committee concluded that the health care system is well poised to develop methods for beginning to identify social isolation and loneliness in health care settings. By first identifying those at highest risk, clinicians and health care researchers may be able to use these findings to better target meaningful clinical and public health interventions to individual patients as well as to high-need populations served by a practice or health care system. Furthermore, this will support a step-wise approach to care that includes the identification of individuals at risk, the provision of education, and ultimately, intervention.
RECOMMENDATION 7-1: Health care providers and practices should periodically perform an assessment using one or more validated tools to identify older adults experiencing social isolation and loneliness in order to
initiate potential preventive interventions after having identified individuals who are at an elevated risk due to life events (e.g., loss of a significant relationship, geographic move, relevant health conditions).
- In the case of older adults who are currently socially isolated or lonely (or at an elevated risk for social isolation or loneliness), health care providers should discuss the adverse health outcomes associated with social isolation and loneliness with these older adults and their legally appointed representatives. Providers should make appropriate efforts to connect isolated or lonely older adults with needed social care.
- For older adults who are currently socially isolated or lonely, health care providers should attempt to determine the underlying causes and use evidence-based practices tailored to appropriately address those causes (e.g., hearing loss, mobility limitations).
A variety of established research tools can be used to measure social isolation and loneliness, each with its own strengths and weaknesses. Despite the limits of the evidence base concerning how best to implement these tools in clinical settings, the committee concluded that an important aspect of selecting a tool for use in clinical settings is standardization. This means that within a specific health care system or organization, all clinicians should use the same tool or set of tools; they should use only validated tools and refrain from using only parts of existing tools or creating new, unvalidated tools. While the committee recognizes that some variation in choice of appropriate tools may be necessary for assessing certain specific populations or health conditions, it emphasizes that the chosen measurement tool needs to match the research question. (That is, if assessing for loneliness, for instance, the tool needs to be validated specifically for the measurement of loneliness, as opposed to other indicators of social connection.) In spite of limitations to existing tools, their use is necessary to address social isolation and loneliness more fully in clinical settings. More effort is needed to update existing tools and to develop and validate better tools that can fully capture the experience of social isolation and loneliness among today’s older adults.
Additional research is needed to evaluate the ethical implications and unintended consequences of clinical assessments and also to determine specific implementation details, including
- who should receive the assessment,
- who should conduct the assessment,
- the ideal frequency of assessment for different subpopulations, and
- the appropriate interventions, referrals, and follow-up care.
Many initiatives to address social isolation and loneliness in clinical settings are being undertaken by individuals without formal research training.
Linking clinicians and others who are implementing new interventions with formally trained researchers early on in the design of the intervention can help to ensure robust research design, and thereby improve the evidence concerning the use of validated tools in clinical settings.
RECOMMENDATION 7-2: Health care systems should create opportunities for clinicians to partner with researchers to evaluate the application of currently available evidence-based tools to assess social isolation and loneliness in clinical settings, including testing and applications for specific populations.
Finally, the committee concludes that assessment data need to be included in clear locations in the electronic health record.
RECOMMENDATION 7-3: The committee endorses the recommendation of previous National Academies reports that social isolation should be included in the electronic health record or medical record.
Research will be needed to determine how to best integrate information from a patient’s assessments into his or her health record in order to make determinations about future care and the identification of risk.
Goals 3 and 4: Improve Awareness and Strengthen Ongoing Education and Training
Educating and training the health care workforce about addressing social isolation and loneliness will require a broad approach similar to educating the workforce to address the social determinants of health. Workforce development is needed within formal degree and postgraduate programs for health professionals, in training programs for direct care workers and community members, and in lifelong learning opportunities. It will be necessary to educate and train all members of the health care workforce, including professionals, direct care workers, community health workers, volunteers, family caregivers, and members of the larger community, such as police officers and mail carriers, who provide a broad array of services to or regularly interact with older adults.4
Improving Overall Awareness
Based on the significant evidence base concerning the health and medical impacts of social isolation and loneliness, the committee concluded that, as with
___________________
4 This report focuses on the education and training of health care workers, particularly health care professionals and direct care workers.
other public health issues of the same magnitude, a critical step toward preventing, mitigating, or eliminating negative health impacts will be to improve awareness among the general public and, specifically for this report, among the health care workforce itself.
RECOMMENDATION 8-1: The U.S. Department of Health and Human Services should advocate for including measures of social isolation and loneliness in major large-scale health strategies (e.g., Healthy People) and surveys (e.g., National Health Interview Survey).
RECOMMENDATION 8-2: Health and aging organizations, relevant government agencies, and consumer-facing organizations should create public awareness and education campaigns that highlight the health impacts of social isolation and loneliness in adults.
- Health care systems, associations representing all types of health care workers (e.g., American Medical Association, American Nurses Association, American Psychological Association, National Association of Social Workers, American Geriatrics Society, American Association for Geriatric Psychiatry, organizations representing direct care workers); health-related organizations (e.g., American Heart Association); consumer-facing, health-related organizations (e.g., AARP); aging professional associations (e.g., American Society on Aging, Gerontological Society of America); aging services organizations (e.g., area agencies on aging, state departments on aging); and organizations working with at-risk older adults (e.g., National Hispanic Council on Aging) should actively communicate information about the health impacts of social isolation and loneliness through print and digital media.
- Organizations representing health plans and providers should include consumer-friendly information about the health impacts of social isolation and loneliness in their repository of patient resources (e.g., where the organization provides information about the self-management of various chronic diseases).
Strengthening Education and Training
While research-based evidence is not yet available to support curricular content on specific interventions for social isolation and loneliness in older adults, enough is known about the health impacts to warrant broad curricular recommendations for all health professions and careers. Education is needed about the prevalence of social isolation and loneliness in older adults, the health outcomes and risk factors for social isolation and loneliness, and how to assess
for these problems. Health professionals also need to learn how to work directly with older adults and their significant others to support and encourage ways to prevent or reduce social isolation and loneliness, including how to make and follow-up on referrals to appropriate community-based services. This will include learning to work with direct care workers, community health workers, family caregivers, and other community members as part of a team-based approach to helping older adults. Health care professionals also need to learn how to work with community partners to develop, implement, and evaluate programs for preventing or mitigating social isolation and loneliness in older adults. Competency in each of these areas will become increasingly important as systems of care are developed for preventing, assessing, and treating the negative health impacts of social isolation and loneliness in older adults. Therefore, as a first step, the committee makes the following recommendations:
RECOMMENDATION 8-3: Health professions schools and colleges as well as direct care worker training programs should include education and training related to social isolation and loneliness in their curricula, optimally as interprofessional team-based learning experiences.
- Health education and training programs should include information on clinical approaches to assessing and intervening when an older adult is at risk for social isolation and loneliness.
- As evidence on effective interventions develops, health education and training programs should provide education on integrating care related to social isolation and loneliness into clinical practice and as part of discharge planning, care coordination, and transitional care planning with community organizations.
RECOMMENDATION 8-4: Health professional associations should incorporate information about the health and medical impacts of social isolation and loneliness on older adults in their advocacy, practice, and education initiatives.
- Health professional associations should include social isolation and loneliness in conference programming, webinars, toolkits, clinical guidelines, and advocacy priorities.
RECOMMENDATION 8-5: Health professional associations, membership organizations, academic institutions, health insurers, researchers, developers of education and training programs, and other actors in the public and private sectors should support, develop, and test different educational and training approaches related to the health and medical impacts of social isolation and loneliness in older adults across different segments of the
health care workforce (including health care professionals and direct care workers) in order to determine the most effective ways to enhance competencies. In addition to initial clinical education, these approaches should apply to professional education, continuing education modules, online learning, and other forms of lifelong learning.
Depending on the complexity of the knowledge to be disseminated or the evidence-based practices to be implemented, a variety of teaching strategies can be considered. As the evidence for interventions evolves, the educational and training opportunities need to expand to include new and updated evidence-based practices for preventing, assessing, and treating the negative health impacts of social isolation and loneliness.
Goal 5: Strengthen Ties Between the Health Care System and Community-Based Networks and Resources
Like other social determinants of health, social isolation and loneliness are community-wide problems and some solutions will require coordinated solutions between the health care system and community-based social care providers. National, state, and local coalitions of public and private health care leaders, including minority-based community organizations, need to work collectively to develop strategies to address social isolation and loneliness in older adults.
RECOMMENDATION 9-1: Health care providers, organizations, and systems should partner with social service providers, including those serving vulnerable communities, in order to create effective team-based care (which includes services such as transportation and housing support) and to promote the use of tailored community-based services to address social isolation and loneliness in older adults.
Many health care organizations (e.g., hospitals) are required under federal law to submit community benefit reports. Efforts by such entities to partner with social service providers could be used as an example of their community benefit. The 2019 National Academies consensus study report Integrating Social Care into the Delivery of Health Care cites the provision of transportation vouchers and the investment in community ride-sharing programs as examples of activities that can improve the integration of care. Such services could allow individuals to travel to health care appointments and to overcome individual transportation-related barriers to being more integrated into local community events, both of which could help to reduce social isolation and loneliness.
A variety of stakeholders, both within and outside of the formal health care system, are testing new approaches to preventing, identifying, and intervening in social isolation or loneliness for older adults. The committee concluded that as
new evidence develops, a centralized sharing of resources and best practices would benefit all stakeholders.
RECOMMENDATION 9-2: Given the public health impact of social isolation and loneliness, the U.S. Department of Health and Human Services should establish and fund a national resource center to centralize evidence, resources, training, and best practices on social isolation and loneliness, including those for older adults and for diverse and at-risk populations.
DISSEMINATION AND IMPLEMENTATION
The dissemination and implementation of evidence into regular and effective use is complex because of the multiplicity and varying capacities of health care systems and providers and the diversity of the target audiences. However, such efforts are imperative in order to improve quality of care, outcomes, and population health. Two main challenges exist for the dissemination and implementation of evidence related to the social isolation and loneliness of older adults. First, better dissemination is needed of the evidence of the health impacts. Second, the best practices of implementation science need to be used in order to ensure that health care systems and providers are able to more quickly adopt evidence-based practices. This will be particularly important as the evidence base on the effectiveness of specific interventions improves.
This page intentionally left blank.
















