Proceedings of a Workshop
WORKSHOP OVERVIEW1
Health literacy is the degree to which individuals have the capacity to obtain, communicate, process, and understand health information, services, and skills needed to make informed health decisions and take action (IOM, 2004). It is a critical skill for engaging in healthy behaviors to reduce disease risk and improve health outcomes across the continuum of cancer care. However, estimates suggest that more than one-third of the U.S. adult population has low health literacy, and nearly half of all patients with cancer have difficulty understanding information about their disease or treatment (Heckinger et al., 2004; Kutner et al., 2006). Low health literacy among patients with cancer is associated with poor health and treatment outcomes, including lower adherence to treatment protocols (Rust et al., 2015; Turkoglu et al., 2018), higher rates of missed appointments (Knolhoff et al., 2016), and an increased risk of hospitalization (Cartwright et al., 2017). Low health literacy can also impede informed decision making, especially as cancer care becomes increasingly complex and as patients and their families take more active roles in treatment decisions.
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop was prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of the individual presenters and participants, and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
To examine opportunities to improve communication across the cancer care continuum, the National Cancer Policy Forum collaborated with the Roundtable on Health Literacy to host a workshop, Health Literacy and Communication Strategies in Oncology, July 15–16, 2019, in Washington, DC. The workshop convened diverse participants, including patients, patient advocates, clinicians, and researchers, as well as representatives of health care organizations, academic medical centers, insurers, and federal agencies. The following topics were explored:
- Strategies to enhance communication among diverse populations with varying levels of health literacy and to promote culturally competent communication;
- Opportunities to improve patient–clinician communication across the cancer care continuum;
- Media and public health strategies to build public trust and convey accurate information about cancer;
- Research strategies to promote health literacy and communication;
- Opportunities for health care organizations and insurers to improve communication and support health literacy; and
- Stakeholder perspectives and priorities for communication and health literacy in oncology.
This workshop proceedings highlights suggestions from individual participants regarding ways to improve communication in cancer care and better support individuals across the range of health literacy abilities. These suggestions are discussed throughout the proceedings and are summarized in Box 1. Appendix A includes the Statement of Task for the workshop. The agenda is provided in Appendix B. Speakers’ presentations and the webcast have been archived online.2
HEALTH LITERACY AND COMMUNICATION
Many workshop speakers discussed the challenges of achieving effective communication in cancer care, and specifically the challenges in meeting the diverse health literacy needs of individuals and ensuring clinicians and public health practitioners engage in culturally competent communication. Karen Basen-Engquist, professor of behavioral science at the University of Texas MD Anderson Cancer Center, noted that the National Action Plan to Improve
___________________
2 See Health Literacy and Communications Strategies in Oncology: A Workshop at http://nationalacademies.org/hmd/Activities/Disease/NCPF/2019-JULY-15.aspx (accessed September 4, 2019).
Health Literacy outlines two key principles (ODPHP, 2010): (1) All people have the right to health information that enables them to make informed decisions, and (2) health services should be delivered in ways that are understandable to patients and that improve health, longevity, and quality of life.
She added that achieving these principles can be particularly challenging in oncology because of the complexity of cancer care. Michael Paasche-Orlow, professor of medicine at the Boston University School of Medicine, added that patients with cancer often face difficult decisions that are dependent on an individual’s clinical and social context. He noted that the key to promoting health literacy and communication is to identify strategies to empower patients and family members to help them make informed health decisions.
Leveraging Media for Cancer Education and Prevention
Elmer Huerta, director of the Cancer Preventorium at Medstar Washington Hospital Center’s Washington Cancer Institute, discussed media strategies to improve cancer education among Spanish-speaking populations. He described his formative experiences in a Peruvian hospital in the 1980s, where he observed that many patients had a limited understanding of their health but were well informed about activities such as sports or television programs with broad media coverage. This motivated him to develop and implement cancer prevention and early detection education programs through the use of broadly accessible media and to create clinics focused on disease prevention.
Huerta said that it is important to understand cancer epidemiology in context; the geographic distribution of cancer depends not only on tumor biology, but also on external factors such as the resources available in the community. “We should not concentrate only on the study of the tumor, but also on the person with the tumor,” Huerta said, adding that patients’ fears, poverty, fatalism, lack of insurance, false beliefs, and lack of information about cancer are just as important for disease etiology as genetic susceptibility. The challenge in addressing many of these factors is conveying the importance of cancer prevention. Thus, Huerta created a culturally relevant, media-based community program based on four principles: (1) consistent and predictable communication that occurs on a regular schedule; (2) comprehensive health education that addresses diverse health topics, not just cancer; (3) use of multiple media channels available to the community, including radio, Twitter, and Facebook; and (4) the building of community trust by ensuring that messages and programming are free from commercial interests.
To complement this media-based cancer education program, Huerta founded a clinic, the Cancer Preventorium, to provide chronic disease prevention, early detection, and patient education services. The Cancer Preventorium has two primary goals: to manage risk factors for chronic diseases, and to
identify and provide early treatment for asymptomatic conditions such as cancer, diabetes, and high blood pressure. Huerta noted that the preventorium model includes community outreach, the clinic itself, and a patient navigation program. He added that this model has been adopted by the National Cancer Institute (NCI) as part of the curriculum for the Cancer Prevention Fellowship Program.3
Since the Cancer Preventorium opened in July 1994, more than 37,000 people—30 percent men, 70 percent women, and approximately 95 percent foreign-born Hispanics—have been seen at the facility. Two-thirds of these patients have less than a high school level of education, and the majority do not have health insurance. For individuals who require follow-up care but lack health insurance, the Cancer Preventorium makes referrals to local community clinics for treatment. Huerta noted that the most common ways people learn about the Cancer Preventorium are through the radio or from friends and family. Approximately one-third of the clinic’s patients have no symptoms, and more than half present with symptoms they do not believe are related to cancer (see Figure 1). Huerta noted that approximately 90 percent of the clinic’s patients come for preventive care.
The Role of Culture in Cancer Care and Research
Marjorie Kagawa Singer, research professor at the University of California, Los Angeles, Fielding School of Public Health, discussed culturally informed clinical care, best practices for communicating with multicultural populations, and the importance of incorporating culture in health research. Kagawa Singer said that several factors could contribute to miscommunication, including low health literacy, anxiety about speaking with a doctor, differing expectations of communication etiquette, and language barriers. She stressed that miscommunication impedes progress in reducing health disparities (IOM, 2012).
Culture in Cancer Care and Communication
Kagawa Singer noted a major challenge in achieving effective communication among culturally diverse populations: the majority of health psychology researchers and participants in health psychology research are from WEIRD countries—Western, educated, industrialized, rich, and democratic. However,
___________________
3 See Course: Principles and Practice of Cancer Prevention and Control at https://cpfp.cancer.gov/summer-curriculum/course-principles-and-practices-cancer-prevention-and-control (accessed October 25, 2019).
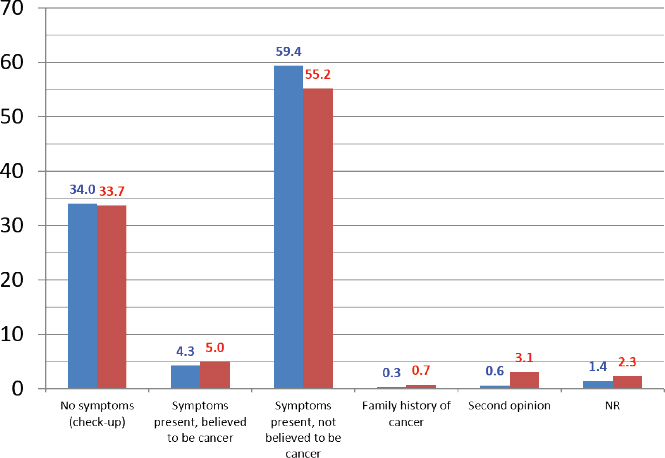
NOTES: This graph shows a total of 774 patients; 45.2 percent are male (blue) and 54.8 percent are female (red). NR = no reply.
SOURCE: Huerta presentation, July 15, 2019.
these WEIRD individuals represent only 12 percent of the world’s population (Henrich et al., 2010a,b). “For those of you who are researchers, every theory you use has likely been standardized on primarily non-Hispanic white populations, and that is not [representative of] the United States. . . . We are a multicultural society with a monocultural approach to health care that denies culture as a complex determinant for health disparities,” said Kagawa Singer. She noted that demographic trends in the United States will continue to exacerbate this challenge, as minority populations will soon constitute the largest share of the overall population (Colby and Ortman, 2014).
Kagawa Singer said that the health care community should recognize that there are fundamental differences in cultural constructs and should view cultural differences as assets and sources of strength for patients and their families. Many cultures emphasize interdependence, community welfare, and group consensus over individuality, and acknowledge that suffering is a fact of life. In contrast, cultural constructs in the United States often reflect independence, individualism, autonomy, and happiness. A major challenge in the delivery of culturally competent communication is reconfiguring the health care system and clinicians to respect these cultural differences and foster trust between clinicians and patients, even if they have distinct cultural values and
backgrounds that may initially conflict with the health care staff and agency structure. Kagawa Singer stated that integrating culture into health care helps the patient and family understand their situation and collaboratively create goals for care with their clinicians.
Ivis Sampayo, senior director of programs at SHARE,4 also described the benefits of integrating cultural competence in clinical care and cancer communication. She noted that her organization has the capability to help women who speak any of 19 languages; offers webinars and onsite programs in English, Spanish, and Japanese; provides outreach programs in English and Spanish; and has peer ambassadors to African American and Latino communities. She described LatinaSHARE’s novella program, a communication tool designed to overcome cultural and language barriers by presenting information on breast cancer detection, diagnosis, treatment, and survival using a fictional narrative in a culturally popular comic book format. Since the program’s development in 2010, approximately 150,000 copies of the novella have been distributed. Sampayo noted that, through the use of accessible media such as comic books, even children and teenagers can learn about cancer prevention and can help serve as educators for their families.
Culture in Cancer Research
Kagawa Singer discussed the application of culture in health research. She defined “culture” as a “dynamic, multilayered and multidimensional system comprised of shared beliefs, values, lifestyles, ecologic, social, political, and technical resources and constraints that dynamically changes and adapts to circumstances that its members use [it] to provide safety, security, and meaning for and of life” (Kagawa Singer et al., 2015). She noted that despite the central role of culture in explaining behavior, the construct of culture is woefully understudied, poorly defined, and rarely integrated beyond superficial steps in both research and practice. She said that culture is often operationalized in terms of ethnicity or language, but cautioned against this approach, because neither fully captures the construct and because these are unique constructs that need to be addressed individually in health research.
Instead, Kagawa Singer stressed the need for measurement frameworks that fully integrate salient aspects of each culture with health literacy. These frameworks enable clinicians and researchers to more accurately identify which aspects of culture may affect health outcomes. To address this need, the National Institutes of Health (NIH) Office of Behavioral and Social Sciences Research funded research to develop a cultural framework for health research
___________________
4 See the SHARE homepage at https://www.sharecancersupport.org (accessed October 25, 2019).
(Kagawa Singer et al., 2015). This framework calls for researchers to answer six questions before designing an intervention with culturally diverse populations:
- Is the rationale for the inclusion of culture clearly articulated in the problem statement?
- Has a definition of culture for the clinical or research objective(s) been articulated?
- Are select theoretical and cultural constructs known?
- Is there correspondence between salient theoretical and cultural constructs?
- Is there a conceptual framework that specifies how salient constructs affect the health issue of focus? (E.g., have independent variables, moderating effects, and mediating effects been identified?)
- Are there cross-culturally equivalent existing measures?
COMMUNICATION ACROSS THE CANCER CARE CONTINUUM
Many workshop participants discussed strategies and best practices to improve patient–clinician communication and meet patients’ health literacy needs across the continuum of cancer care.
Prevention and Screening
Cathy Meade, senior member in the Division of Population Science, Health Outcomes, and Behavior at the Moffitt Cancer Center, discussed the need for effective cancer prevention communication. She noted that almost half of cancer deaths are linked to preventable causes, including tobacco use, obesity, exposure to ultraviolet light, and vaccine-preventable infections (ACS, 2019). She added that prevention science has matured in recent decades, and the World Health Organization has described cancer prevention as the most cost-effective, long-term strategy for cancer control: “National policies and programs should be implemented to raise awareness, to reduce exposure to cancer risk factors and to ensure that people are provided with the information and support they need to adopt healthy lifestyles” (WHO, 2019).
Meade said the cancer community needs to convey the transformative potential of cancer prevention to the general public, noting that adopting a healthy lifestyle can reduce the risk of cancer and other chronic diseases, and improve treatment outcomes and prevent cancer recurrence. However, she said it can be challenging for many people to interpret and apply information about cancer prevention and risk reduction. Adding to the complexity of the challenge is the growing diversity of the U.S. population, which will require
improved emphasis on culture and literacy to inform and advance health equity (Collins and Blige, 2016; Meade, 2005).
Meade suggested that a significant obstacle to communication about cancer prevention is that members of the public may not understand what prevention entails. She described her experience conducting focus groups to develop patient materials about cancer. She found that many participants did not understand the term “prevention.” Meade recounted that one participant asked if prevention was like getting a checkup for a car, which reinforced to Meade the importance of likening cancer prevention activities to common and familiar points of reference. She said that striving for a shared understanding is the ultimate goal of cancer communication.
Meade said it is important to consider the development, delivery, and distribution of messages about cancer prevention. She said materials should be relatable, engaging, actionable, and written for the appropriate level of literacy (Meade et al., 2018). At the same time, messages need to be accurate and scientifically sound. Rigorous formative work—including focus groups, usability testing, and community–academic partnerships—can help to achieve these goals. Meade encouraged researchers to solicit and incorporate feedback on messages from the target audience. Other facets of effective health communication include good presentation, attention-capturing messaging, and the use of multiple modes of delivery to inform diverse members of the population about cancer prevention.
Meade proposed three strategies to achieve effective communication and promote health literacy for cancer prevention: (1) advocate at the national level for policies that enhance access, insurance coverage, and reimbursement for cancer prevention; (2) strengthen the evidence base for the role of health literacy through research that advances the engagement of marginalized, underrepresented, and underserved communities in cancer prevention; and (3) advocate for the creation of a national council or network that engages diverse stakeholders in establishing guidelines, procedures, and tools for communicating evidence-based information about cancer risk, prevention, detection, and treatment to patients, families, and communities.
Cancer Treatment
Anthony Back, professor of oncology at the University of Washington School of Medicine and co-director of the Cambia Palliative Care Center of Excellence, stressed that effective patient–clinician communication is critical, especially as cancer care becomes more complex. Back noted that NCI has identified six domains of patient-centered communication that affect health outcomes (see Figure 2): exchanging information, making decisions, fostering healing relationships, enabling patient self-management, managing
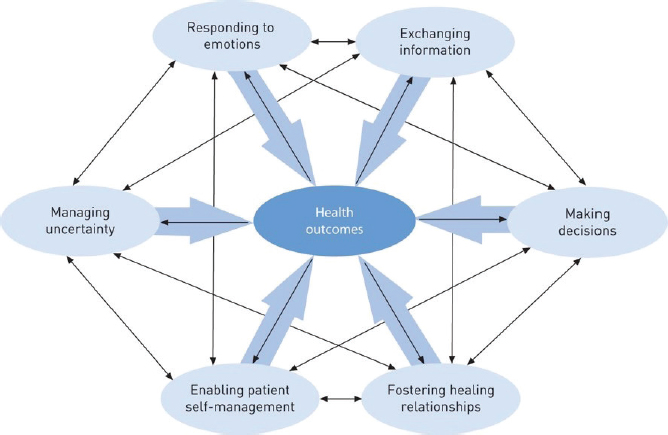
SOURCES: Back presentation, July 15, 2019; Epstein and Street, 2007.
uncertainty, and responding to emotions (Epstein and Street, 2007). Back suggested that all clinicians involved in caring for patients with cancer build skills in these domains.
Back noted that clinicians are often poor judges of their communication skills, with a misalignment between patients’ reporting of their clinicians’ communication abilities and clinicians’ self-reporting (Dickson et al., 2012) (see Figure 3). In a national physician survey, 99 percent of practicing physicians agreed that having conversations about advance care planning and goals of care are “important” or “very important,” but only 14 percent reported holding and documenting these conversations (PUR/C, 2016). Physicians reported various reasons for not holding these conversations, including a lack of formal training, inadequate time, and uncertainty about how to broach these challenging conversations with patients.
Back said that supporting communication competencies among clinicians is critical for achieving high-quality cancer care (Bernacki et al., 2019; Paladino et al., 2019): “Having these conversations improves patient outcomes,” said Back. He added that these conversations are associated with a higher likelihood of goal-concordant care, higher patient-rated care experiences, lower likelihood of aggressive care near the end of life, increased length of hospice care, and less depression and anxiety among bereaved family members (Curtis et al., 2018; Detering et al., 2010; Gade et al., 2008; Mack et al., 2010, 2012; Wright et al., 2008). Additionally, patients are more trusting of clinicians
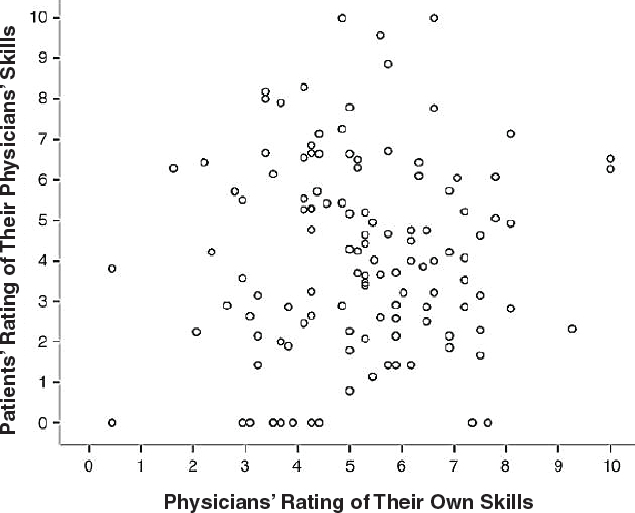
SOURCES: Back presentation, July 15, 2019; Dickson et al., 2012.
with strong communication skills, which improves patient care (Tulsky et al., 2011). “This is not about just being a nice doctor,” said Back. “It is really about a skill set that every oncology clinician should have.”
Back noted that communication is a learned skill (Langewitz et al., 1998) and that appropriate training can help clinicians be more empathetic, ask more questions, and actively recognize patients’ values (Back et al., 2007). What is missing, said Back, is the ability of every practicing clinician to receive such training. To address this, Back founded VitalTalk.org,5 a nonprofit organization that uses an evidence-based learning model to teach clinicians how to more effectively discuss serious illness with patients (Arnold et al., 2017). In 3 years, VitalTalk has trained more than 500 faculty members, who have subsequently held more than 600 workshops that enable clinicians to practice newly learned skills.
Back identified several strategies to improve clinician communication skills. First, develop better cognitive tools and protocols for communication that invite two-way, person-centered exchange (Back et al., 2009). One such
___________________
5 See the VitalTalk homepage at https://www.vitaltalk.org (accessed October 25, 2019).
tool is the REMAP framework, which teaches clinicians to reframe situations, expect emotions, map important values, align with patients and families, and plan treatment to uphold values (Childers et al., 2017). Additional strategies include promoting non-punitive learning cultures that reinforce deliberate, positive communication practice, and fostering peer learning to generate a network of informal mentoring.
Back emphasized that the tools to improve clinician communication are ready to scale, but policies are needed to support their implementation. He suggested widely disseminating evidence-based communication training programs and embedding clinician-educators within health systems to facilitate skills acquisition and maintenance (Back et al., 2019; Gilligan et al., 2017). He added that payers could create incentives for clinicians and health care organizations to build communication skills and that performance metrics could help to foster accountability (Back et al., 2019).
Mandi Pratt-Chapman, associate center director for patient-centered initiatives and health equity at The George Washington University Cancer Center, agreed that effective communication is essential for facilitating informed and shared decision making. Pratt-Chapman suggested using plain language and avoiding medical jargon (Schwartzberg et al., 2007). She also supported providing patients with specific advice, such as “increase your physical activity by five minutes three times a week,” rather than using ambiguous language, such as “get more exercise.” She added that using the teach-back method can help confirm that patients understand the information they receive.6 Pratt-Chapman also described the Institute for Healthcare Improvement’s Ask Me 3 technique,7 which helps focus patient–clinician conversations on identifying primary health concerns, discussing interventions to address them, and ensuring that patients understand the plans for their care.
Deborah Collyar, founder and president of Patient Advocates in Research, emphasized that all patients and families, no matter their level of education, experience shock when they receive a cancer diagnosis, which can impede effective communication. Collyar suggested that decision-making tools and templates be developed for clinicians to use during cancer care, particularly during enrollment for clinical trials. She added that the NCI Clinical Trials Network could employ an iterative process of designing and testing these materials, in partnership with patient communities.
___________________
6 In the teach-back method, clinicians ask patients to repeat medical information in their own words to ensure comprehension.
7 Additional information is available at http://www.ihi.org/resources/Pages/Tools/Ask-Me-3-Good-Questions-for-Your-Good-Health.aspx (accessed August 21, 2019).
Adolescents and Young Adults with Cancer
Gwendolyn Quinn, Livia Wan M.D. Professor of Obstetrics and Gynecology in the Department of Population Health and the Center for Medical Ethics at the New York University Grossman School of Medicine, discussed patient–clinician communication issues among adolescent and young adult cancer survivors. Every year, approximately 70,000 people ages 15 to 39—collectively referred to as adolescents and young adults (AYA)—are diagnosed with cancer (NCI, 2018). The AYA category also includes adult survivors of pediatric cancer, who often suffer lifelong effects from cancer and its treatment.8 Quinn noted that the AYA population has numerous psychosocial and health concerns after a cancer diagnosis, such as treatment side effects, finances, fertility, self-esteem, and career and education prospects.
Guidelines from several cancer advocacy and research organizations describe the importance of conveying information about reproductive health to adolescents and young adults with cancer (Coccia et al., 2018; Oktay et al., 2018). Quinn noted that reproductive health concerns in oncology extend beyond infertility and fertility preservation to include romantic partnering, friendships, body image, sexuality, sexual identity and orientation, contraception, and psychosexual adjustment. These concerns are relevant at various times throughout the continuum of cancer care (see Figure 4). However, cancer clinicians often do not broach these topics with AYA patients. In a national study of oncologists, Quinn and her colleagues found that the primary reasons oncologists do not talk about reproductive health or infertility with their AYA patients is that they do not have time and were not trained to do so (King et al., 2008a,b; Vadaparampil et al., 2007). She noted that clinicians were willing to accept responsibility for engaging AYA patients in conversations about reproductive health, but only if trained and empowered to do so (Quinn and Vadaparampil, 2009; Quinn et al., 2007, 2008).
The diverse developmental stages in AYA populations present an additional challenge in patient–clinician discussions about reproductive health. “The way you would talk about potential loss of fertility and sexual function to a 15-year-old who may never have had a sexual experience would be very different than how you would talk to a 35-year-old who has been in a partnered relationship for a time,” explained Quinn. As a result, it can be challenging for health care professionals to determine appropriate language and strategies to mitigate patients’ discomfort with the topic. Quinn noted that the heteronormativity of most patient education materials is also a concern when
___________________
8 The unique communication and health literacy needs of children were not a focus of this workshop, but discussions throughout this proceedings may help inform strategies for pediatric populations.
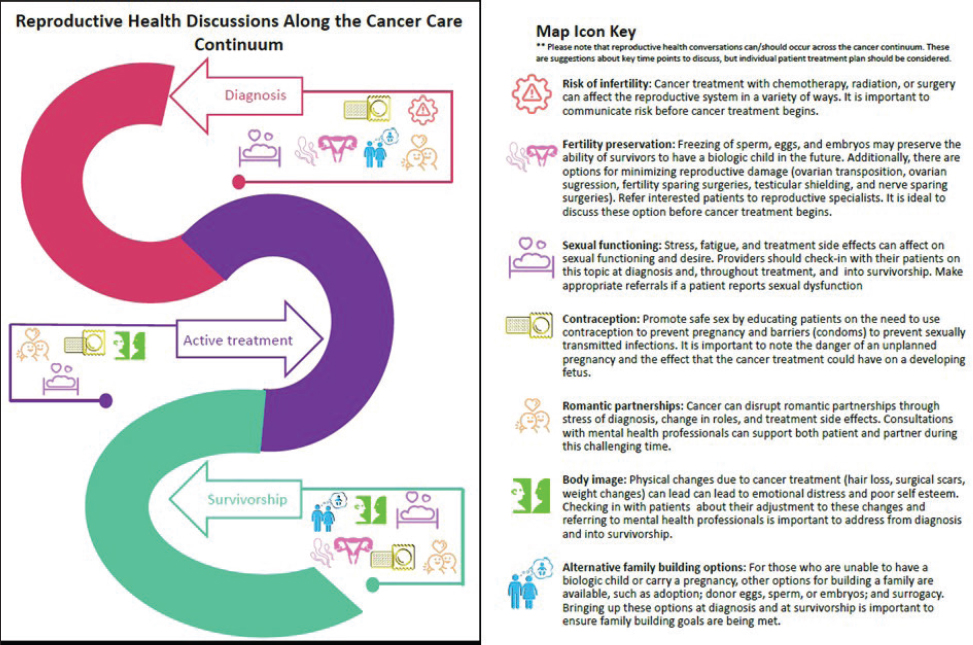
SOURCE: Quinn presentation, July 15, 2019.
discussing reproductive health with AYAs. In response, lesbian, gay, bisexual, and transgender patients with cancer are starting to create their own support and information networks.
To address patient–clinician communication challenges among AYA patients with cancer, Quinn suggested that institutional policies have a key role in establishing guidelines for appropriate communication. She suggested that health care organizations caring for AYA patients with cancer develop a readiness checklist that includes
- Referral pathways to reproductive specialists and mental health professionals,
- A documentation system,
- Communication training for clinicians,
- Psychological support for reproductive health services and access to financial support if reproductive health services are elected,
- Psychosocial support services, and
- Patient education materials.
Survivorship Care
Frank Penedo, associate director for cancer survivorship and translational behavioral sciences at the University of Miami Miller School of Medicine’s Sylvester Comprehensive Cancer Center, discussed challenges in communicating health information among the growing population of cancer survivors.9 He noted that as of 2019, there were more than 16.9 million Americans living with a history of cancer, a number projected to reach more than 26.1 million by 2040 (Bluethmann et al., 2016). Cancer survivors face ongoing chronic and debilitating health and psychosocial challenges, such as adverse effects from cancer and its treatment, comorbidities, functional limitations, and complex care needs, as well as life disruptions and financial burdens. Penedo said that approximately 30 percent of cancer survivors experience clinically elevated levels of psychological distress, particularly anxiety and depression (Mehnert et al., 2014).
Penedo noted that the report From Cancer Patient to Cancer Survivor: Lost in Transition found insufficient emphasis on the needs of cancer survivors (IOM, 2003, 2006; NASEM, 2017, 2018b). Penedo highlighted essential focus areas of high-quality survivorship care: addressing lifestyle factors and comorbidities, ensuring continuity of care, and conducting ongoing symptom monitoring and management. Penedo stressed that survivorship care plans
___________________
9 The term “cancer survivor” has been defined as “an individual affected by cancer, from the time of diagnosis through the balance of his or her life.” See https://cancercontrol.cancer.gov/ocs/statistics/definitions.html (accessed September 20, 2019).
(SCPs)10 are a key tool for ensuring effective patient–clinician communication in survivorship care. He noted that creating and discussing SCPs engages patients as active partners in their ongoing care. SCPs also promote continuity in the transition between oncology and primary care (IOM, 2006). According to guidelines from the American College of Surgeon’s Commission on Cancer, survivorship care plans should contain both a summary of the patient’s disease and treatment (e.g., clinicians’ contact information, diagnosis and stage, description of treatment, and description of ongoing toxicities) and a detailed plan for follow-up care (e.g., the need for ongoing therapy, schedule of upcoming visits and tests, symptoms of recurrence, and psychosocial concerns) (Mayer et al., 2014). Although the Commission on Cancer has recently revised their accreditation requirements to recommend but not require SCPs, Penedo said that these documents can help promote continuity of care by effectively communicating clinical care information that may otherwise not be available to the patient and the patient’s other clinicians.
Penedo discussed the importance of patient-centered communication in survivorship care, including responding to emotions, managing uncertainty, exchanging information, and enabling self-management (Economou and Reb, 2017) (see Table 1). He added that clinicians should incorporate patient-reported outcomes in their assessments, noting that patient-reported outcomes in survivorship care can enhance communication between patients and clinicians, facilitate shared decision making, and help patients assess their progress over time. Collyar agreed, adding that patient-reported outcomes can also help measure important aspects of patient experience that extend beyond disease symptomatology.
Penedo described the design and implementation of a program to monitor survivors’ patient-reported outcomes via the patient portal at the University of Miami Health System. Patients are asked to respond to questions that capture their experiences during and after care encounters. Many of the questions are based on the Patient-Reported Outcomes Measurement Information System,11 a set of short, well-validated, computerized questions that can be used to evaluate and monitor key domains, including pain, fatigue, physical functioning, and emotional well-being, as well as practical needs, such as transportation, child care, and nutrition. Some responses trigger automatic alerts to social work or nursing staff.
___________________
10 Survivorship care plans include a comprehensive summary of oncology care and a follow-up plan, and serve to facilitate communication between patients and their care teams after discharge from cancer treatment (IOM, 2006).
11 Additional information is available at http://www.healthmeasures.net/exploremeasurement-systems/promis (accessed August 12, 2019).
TABLE 1 Patient-Centered Communication Strategies for Cancer Survivors
| Function | Domains |
|---|---|
| Responding to emotions |
|
| Managing uncertainty |
|
| Exchanging information |
|
| Enabling self-management |
|
SOURCES: Penedo presentation, July 15, 2019; Economou and Reb, 2017.
Palliative and End-of-Life Care
Nina O’Connor, chief of palliative care for the University of Pennsylvania Health System and chief medical officer for Penn Medicine Hospice, defined “palliative care” as specialized medical care for patients with serious illnesses, such as cancer, that provides expert pain and symptom management, emotional support and assistance with coping, advance care planning, and end-of-life discussions (Ferrell et al., 2018). Palliative care is provided in partnership with the patient’s care team and is available any time during cancer care, regardless of the other treatments a patient receives (see Figure 5).
O’Connor noted that a key challenge in patient–clinician communication about palliative care is countering the inaccurate belief that palliative care is
| Function |
|---|
|
|
|
|
available only to patients who forego active treatment. Clinicians may also find it difficult to broach the topic of palliative care and advance care planning without training, because they fear it may take away a patient’s hope. However, “there are many ways we can teach health care providers to talk about palliative care while maintaining hope,” said O’Connor. She said that few clinicians have received formal training in discussing palliative care and advance care planning (Horowitz et al., 2014), and time pressures can create barriers to these discussions.
O’Connor added that there is a national workforce shortage of palliative and hospice care physicians (Lupu, 2010). O’Connor said that to help address this challenge, all oncology clinicians should be trained in basic palliative care

SOURCES: O’Connor presentation, July 15, 2019; Center to Advance Palliative Care.
skills, with select clinicians receiving additional training from palliative care specialists so they can serve as local resources. This would enable the limited pool of available palliative care specialists to consult on complex cases and train other clinicians. “Only through a model like this are we actually going to be able to meet all of the patients’ needs,” she said. O’Connor also spoke in favor of the Palliative Care and Hospice Education and Training Act12—a bill that has passed in the U.S. House of Representatives and is pending in the U.S. Senate—that would create training centers to expand the palliative care workforce. It would also fund research on best practices for palliative care and a public awareness campaign about palliative care.
To ensure that every University of Pennsylvania Health System patient with serious illness at has a conversation about advance care planning, O’Connor and her colleagues employ a strategy developed by Ariadne Labs and the Harvard T.H. Chan School of Public Health and tested at the Dana-Farber Cancer Institute.13 This strategy provides a set of tools to help clinicians, patients, and families engage in productive conversations about serious illness care. It also includes a 3-hour clinician training course and coaching for 1 additional month, as well as various system tools to assess program implementation. O’Connor stated that patients who have had these conversations at University of Pennsylvania Health System cancer centers have provided positive feedback. “Patients really want to have these conversations,” said O’Connor. “They are waiting for these conversations, and they feel much closer to their clinician when we have these conversations.”
___________________
12 See H.R. 1676—Palliative Care and Hospice Education and Training Act at https://www.congress.gov/bill/115th-congress/house-bill/1676 (accessed October 25, 2019).
13 See Serious Illness Care Program Study at https://www.ariadnelabs.org/wp-content/uploads/sites/2/2019/03/SI-DFCI-Outcomes-fact-sheet-2019-03-12c.pdf (accessed October 25, 2019).
COMMUNICATION STRATEGIES TO BUILD PUBLIC TRUST AND COUNTER INACCURATE INFORMATION
Many workshop participants discussed strategies for improving health literacy among the general public and building trust with the public health community. Workshop speakers also discussed the emergence of misinformation about cancer and the associated public health threat, and suggested opportunities for various stakeholders to counter inaccurate information.
Addressing Online Health Misinformation
Wen-Ying Sylvia Chou, program director in the Health Communication and Informatics Research Branch at NCI, defined “health misinformation” as “a health-related claim of fact that is currently false due to a lack of scientific evidence” (Chou et al., 2018). She said that addressing the high prevalence of false information on social media is key to engaging the public in effective communication about cancer. Although social media platforms can offer social support and an accessible venue for peer-to-peer sharing of health information, she said they can also serve as an echo chamber that enables the rapid spread of misinformation. Chou added that dissemination of misinformation is facilitated by the viral nature of social media, the vulnerability of patients and their families, low public trust in expertise, and the limited health literacy skills of individuals.
Chou discussed opportunities to assess and proactively address cancer-related health misinformation (Chou et al., 2018; Southwell et al., 2019). She said that the first step is to identify the consequences of exposure to misinformation, as well as the level of exposure that produces adverse effects. Next, she said, the cancer community needs to increase surveillance on health communication and misinformation. “We need to do a better job collecting longitudinal, spatial, and network information [and] thinking about not just explicit forms of misinformation, but implied and implicit misinformation.” She added that the public health community, in partnership with trusted community leaders, also needs to conduct outreach efforts to build public trust, raise awareness, and promote education about important health-related topics. Finally, she said, new interventions are needed that address and mitigate misinformation and that are respectful of the identities, emotions, and values of the intended audiences.
Chou described two NCI initiatives to promote research on public communication and strategies to address misinformation in cancer. The first is a funding opportunity to develop innovative approaches to studying cancer communication across the continuum of cancer care in the evolving media
environment.14 The second is a collaboration with the American Journal of Public Health to produce a special issue on health misinformation on social media,15 including articles characterizing misinformation, describing the health consequences of exposure to misinformation, and proposing strategies to mitigate the effects and limit the spread of misinformation. Chou noted that there are clear opportunities for health care organizations, community partners, and communication practitioners to assess and address misinformation about cancer and reduce its adverse effects on public health. She suggested that the public health community partner with social media platforms to promote the dissemination of accurate health information.
James Hamblin, writer and senior editor at The Atlantic, suggested that the public health community participate actively in social media to disseminate credible information and counter misinformation. “There are so many different platforms out there and so many different styles of communication. . . . [T]here is something for everyone,” he said. “It requires a little dedication and commitment to figuring out how that platform works, what your target audience is, and what you are trying to do, whether it is activate, inform, or just generally engage.” Hamblin noted that social media provides health care professionals and scientists the opportunity to reach large portions of the public, and to disseminate health information directly and in plain language so that messaging is relevant and broadly accessible.
Opportunities for Local and State Governments
Shalewa Noel-Thomas, chief of the Cancer and Chronic Disease Bureau at the District of Columbia (DC) Department of Health, noted three important health literacy concerns: health insurance benefits literacy, health care system literacy, and health behavior literacy. Health insurance benefits literacy enables patients to navigate insurance options, identify covered services, and understand their financial responsibilities for health care. Noel-Thomas noted that health insurance literacy can be challenging even for individuals with otherwise high levels of literacy. Health systems literacy requires understanding different types of care (e.g., primary care versus specialty care), how to access care, and how to navigate the health care system. Health behavior literacy considers health education and health promotion, and requires understanding
___________________
14 See Department of Health and Human Services: Part 1. Overview Information at https://grants.nih.gov/grants/guide/pa-files/par-16-249.html (accessed September 23, 2019).
15 See APHA Call for Proposals: Special Issues about Health Misinformation on Social Media at https://ajph.aphapublications.org/pb-assets/downloads/CFP_HealthMisinformation_Full.pdf (accessed September 23, 2019).
principles of disease management and the association between health behaviors and health outcomes.
Noel-Thomas described how the DC Department of Health approaches health education interventions for populations with varying levels of health literacy. For those with high health literacy, the department focuses on activities such as distributing brochures or engaging in mass media campaigns (e.g., an ongoing smoking cessation campaign that places advertisements on the sides of buses). For individuals with moderate health literacy, a more involved approach is needed, such as one-on-one counseling or health education classes. The DC Department of Health’s Thriving and Surviving workshop series, for example, includes seven weekly 2.5-hour sessions on self-management and communication skills led by cancer survivors or caregivers. For those with low health literacy, she said that more intensive services are warranted, including involvement of community health workers, as well as patient navigation for people diagnosed with cancer.
Noel-Thomas noted that she and her colleagues have assessed health literacy among local residents using mixed methods approaches that include web-based surveys and focus groups. These assessments found that DC residents’ health insurance coverage is among the highest in the nation and that residents have high self-efficacy for identifying a clinician to address a particular medical need.16 Participants were very active in chronic disease self-management, sought care at regular intervals, and were engaged in informed decision making. The evaluation also identified various challenges, such as long wait times for appointments. Respondents also reported fragmentation of care, particularly a lack of communication among clinicians. Navigating the health system was also difficult for many DC residents, and residents voiced frustration with the way health information was conveyed to them. Finally, residents reported low health literacy regarding their medications.
Noel-Thomas said that the recommendations from this evaluation included increasing the use of technology for clinician communication; using telehealth more extensively to reduce appointment wait times, particularly for specialty care; and increasing patient assistance programs, such as patient navigation. Other recommendations included reducing administrative barriers (e.g., the process for obtaining a referral) and providing a digital health management tool to enable patients to ask questions of their peers.
___________________
16 “Self-efficacy” refers to “an individual’s belief in his or her capacity to execute behaviors necessary to produce specific performance attainments.” See Teaching Tip Sheet: Self-Efficacy at https://www.apa.org/pi/aids/resources/education/self-efficacy (accessed September 24, 2019).
Conveying Accurate and Accessible Information to the Public
Richard Wender, chief cancer control officer at the American Cancer Society (ACS), spoke about ACS’s role in communicating accurate and accessible information about cancer. He noted that members of the public, as well as professional organizations, expect ACS to serve as a trusted source for information about cancer; to convene and provide leadership in the fields of cancer research and policy; to embrace health equity; and to meet the needs of patients, caregivers, and the general public. Wender said that ACS views its mission as a “360 degree effort” across a variety of activities and venues (e.g., online chat, call centers, personal guidance, and scientific articles) to meet the diverse needs of individuals and organizations. He added that Cancer.org, ACS’s website, is the most accessed cancer website in the world, logging approximately 120 million visits in 2018.
Wender stated that all information provided by ACS needs to be evidence based and comprehensive, and presented in a way that is easily understood. ACS is also attentive to acknowledging when there is insufficient evidence to make definitive statements. Everyone at the organization, he added, is responsible for providing information. He noted that ACS’s content development team includes two oncologists, nurses, and social workers, and also draws on subject matter experts throughout the organization. All of the organization’s materials for the public are available in both English and Spanish.
Wender said that ACS is very aware of its reputation as a trusted organization that has been in existence for more than 100 years. He stressed that the organization needs to re-earn that trust every day by communicating accurate, scientifically grounded information: “When you are facing marketing pressures and fundraising pressures, having that anchor of what we believe scientifically is truth is very important.” He noted that the organization is perceived by the public as a definitive source for cancer information, and multiple departments are involved in maintaining the accuracy of the information it disseminates. He added that there are substantial challenges to this responsibility, including challenges in addressing questions of causality in cancer etiology and in the use of ACS information in a variety of contexts (e.g., in controversial policy debates, lawsuits, or media coverage).
ACS responds to both national and local media inquiries daily, Wender noted, and the organization strives to engage experts throughout the organization rather than responding with prepared statements. “Anybody can read an official position on cancer.org, but our experts add value. They try to communicate with the media in ways that can be understood and synthesized,” Wender said. He noted that the organization will respond to almost any question on almost any topic, though he also understands that in the current media landscape, ACS’s efforts to convey science-based information may not
always be conveyed appropriately. “The reporter is not the one who writes the headlines, which often highlight where controversy is, and that is a challenge,” said Wender.
Community Engagement and Health Communication
Lisa Fitzpatrick, founder of Grapevine Health and lecturer at the Milken Institute School of Public Health at The George Washington University, started to think about opportunities to engage the public with effective health communication when she was asked by an audience member at a presentation how to find answers to health questions outside of clinician office visits. Years later, Fitzpatrick secured a small grant from The Commonwealth Fund to evaluate the potential for broadly disseminating accessible health information through digital media. The study found that mobile phone ownership was nearly ubiquitous, but few used digital health tools. However, there was interest, if such tools could be designed in an engaging way.
The study also found that participants were more trusting of health information received from family and friends than health information received from clinicians. Through a series of focus groups, she found that the primary driver for this mistrust is that clinicians speak in a manner that is not easily understood. She said that low trust in clinicians contributes to avoidance of the health care system, even among individuals who need medical care.
Fitzpatrick noted that another key lesson she has learned through her engagement with community members is that building trust requires showing up and engaging people where they live. “We cannot keep expecting them to come to us,” said Fitzpatrick, adding that people often find health care buildings cold and unfriendly and that staff can sometimes be disrespectful. By moving out of the clinic and engaging people where they live, she and her colleagues have identified and begun to counteract many common misconceptions about cancer. She said this community-based outreach is critical to building trust and improving the health of individuals and communities.
Fitzpatrick noted that it is crucial to train each person within a health organization on strategies to address the health literacy needs of patients and their families. This training needs to emphasize the importance of speaking in a language that community members can understand, with the goal of demystifying cancer treatment and research. Fitzpatrick also suggested that organizations assess barriers to the use of social media and consider opportunities to use social media to disseminate health messages. Health care organizations also need to ask for patient and community member input to build trusting relationships.
High-Quality Health Journalism
Ivan Oransky, vice president of the editorial department at Medscape, distinguished writer in residence at New York University’s Arthur L. Carter Journalism Institute, and co-founder of Retraction Watch, described the current state of health communication in news media. He stressed that health journalism is often undersupported in media outlets, which can contribute to oversimplified or inaccurate health news content. A study in 2008 that evaluated the content of 500 health-related news media items found that many did not meet several criteria for quality reporting (Schwitzer, 2008) (see Table 2). These deficiencies are important, he explained, because a large proportion of the population seeks health information from online media; in a 2010 poll surveying 1,066 adults, 88 percent reported looking for health information online (Harris Poll, 2010).
Oransky said that only 8 percent of health reporters have a background in biology, and as few as 3 percent are medical doctors (Viswanath et al., 2008). He added that many health reporters work at specialized media outlets, and few are well resourced. A small number of reporters are responsible for producing large volumes of content. Barriers to quality journalism include a lack of time and knowledge, competition for audience, complex terminology,
TABLE 2 Quality of Reporting in Health Journalism: Results from a Sample of 500 News Stories
| Quality Criteria (Did the Story Adequately . . . ?) | % Satisfactory |
|---|---|
| Discuss costs | 23% |
| Quantify benefits | 28% |
| Quantify harms | 33% |
| Discuss existing alternative options | 38% |
| Seek independent sources and explore conflicts of interests in sources | 56% |
| Avoid disease-mongering | 70% |
| Discuss quality of the evidence | 35% |
| Establish the true novelty of the approach | 85% |
| Discuss the availability of the new approach | 70% |
| Go beyond a news release | 65% |
SOURCES: Oransky presentation, July 15, 2019; Schwitzer G (2008) How Do US journalists cover treatments, tests, products, and procedures? An Evaluation of 500 Stories. PLoS Med 5(5): e95. https://doi.org/10.1371/journal.pmed.0050095.
difficulty in identifying and using reputable sources and independent experts, and editors who were not trained in critical appraisal of medical news and commercialism (Larsson et al., 2003).
Oransky noted that the prevalence of misleading health information can also be attributed in part to public relations communications within academic medical centers. For example, one study found that in a random sample of press releases from academic medical centers, 74 percent of the releases based solely on research conducted in test tubes or on animal models made explicit claims regarding relevance to human health (Woloshin et al., 2009). Of the 95 press releases about clinical research, 23 percent omitted the study size and 34 percent did not quantify effect size. Another study found that 40 percent of academic medical center press releases contained exaggerated advice, one-third contained exaggerated causal claims, and 36 percent contained exaggerated inferences to human health from animal research (Sumner et al., 2014). This study also found that exaggeration in press releases was strongly correlated with overstatement in resulting news stories.
To address these challenges in health journalism, Oransky suggested that reporters should produce fewer stories about single studies, and that health and medical journal editors make a concerted effort to publish and disseminate information about studies with null results, which are useful for advancing scientific progress but are often unreported and usually receive less news coverage. He also recommended that scientists review institutional press releases for accuracy and clarity, and that the health science community contact journalists when additional evidence is published that either supports or contradicts findings that have previously been reported in the news.
RESEARCH STRATEGIES
Many workshop participants discussed ongoing research in the fields of health literacy and communication in oncology, as well as avenues for future research, such as communication about cancer genetics, visual design strategies in messaging, and health insurance literacy.
National Cancer Institute’s Research Portfolio and Priorities for Future Research
April Oh, program director of the NCI Health Communication and Informatics Research Branch, said that addressing health literacy and its contributions to health disparities is a major NCI research priority. NCI’s priorities for health literacy research include assessing the effects of tailored and targeted communication, understanding the digital divide and its impact on health disparities, developing strategies for communicating uncertainty and
complex cancer information to diverse populations and those with limited health literacy, and applying mixed method approaches to investigate challenges associated with limited health literacy.
Oh noted that in 2016, NCI decided to integrate health literacy into funding announcements across the institute, rather than maintaining it as a separate program. This change reflects the understanding that health literacy cuts across a wide range of health issues and is fundamental to achieving health equity.
An internal review of NCI’s portfolio of health literacy research found that grant applications with aims related to health literacy primarily focused on the development or evaluation of interventions within particular racial or ethnic populations and addressed cancer screening, informed and shared decision making, or patient–clinician communication. Oh noted that achieving the goal of equity in health communication will require multilevel, multicomponent interventions that emphasize reach, effectiveness, adoption, implementation, and maintenance (Glasgow et al., 1999).
The research portfolio review also found that many of the NCI-funded health literacy projects addressed the intersection between health literacy and technology: between 2010 and 2013, the proportion of applications that considered technology increased from 58 percent to 78 percent. Oh noted that although access to mobile phones is now almost ubiquitous, there is still a divide in how people use information from the Internet (Robinson et al., 2015; van Deursen and van Dijk, 2019).
Oh noted that future NCI priorities for health literacy and communication research include
- Reducing communication inequalities, especially at the intersection of health literacy and digital health;
- Developing multilevel and multicomponent interventions;
- Evaluating participatory methods to develop health literacy interventions across patient, clinician, and organizational contexts;
- Examining health literacy in dissemination and implementation research and iterative approaches to understand behavior change; and
- Studying settings and contexts in which the research is occurring, to ensure that interventions are not unintentionally exacerbating health inequalities and disparities.
Oh urged investigators to work across disciplinary boundaries and consider implementation strategies for their interventions. “While you may not think of yourself as a dissemination or implementation scientist, you have a voice in that process,” she said. “We have to think about disseminating these interventions and tools . . . and about how to better design our interventions to be ready for implementation.”
Effective Communication About Cancer Genetics
Galen Joseph, professor in the Department of Anthropology, History, and Social Medicine at the University of California, San Francisco (UCSF); member of the Helen Diller Family Comprehensive Cancer Center; and affiliate faculty at the Center for Vulnerable Populations at Zuckerberg San Francisco General Hospital and Trauma Center, noted that genetics play an important role across the cancer continuum. However, there are ongoing challenges for integrating genetics in cancer care. One of these challenges is the under-representation of minority populations in genomic databases, which creates barriers to high-quality care for diverse populations (Smith et al., 2016). For example, genome-wide association studies have largely been conducted on individuals of European descent (Popejoy and Fullerton, 2016). As a result, genetic risk scores are less accurate for people of color in the United States. Underrepresentation of minorities also complicates the interpretation of test results for hereditary cancers. Many genetic variants that are more common in minority populations are missing from genomic databases, making it difficult to determine their associated risk. Joseph noted that expanding the diversity of genomic databases is a critical component of the research program funded by NIH called All of Us,17 as well as other NIH initiatives, including the Clinical Sequencing Evidence-Generating Research consortium (CSER).18 She noted that the funding announcement for CSER’s second phase includes a requirement that at least 60 percent of the population be composed of underrepresented groups (Amendola et al., 2018).
Another challenge for integrating genetics into cancer care is the low level of genomic literacy in the United States (Hurle et al., 2013), which is further complicated by the complexity and uncertainty of genomic information. She said this is true not only for patients, but also for clinicians, who increasingly need to interpret genetic testing results (Ha et al., 2018). “We know that we need to improve genomic literacy in order to realize the promise of genomic medicine,” said Joseph.
Joseph said that a study assessing the quality of communication in genetic counseling for patients at risk for hereditary breast and ovarian cancers in safety net clinics found a communication disconnect between genetic counselors and patients (Joseph et al., 2017). While counselors are trained in communication and think of themselves as skilled communicators, patients said they were confused by complex terminology and perceived that counselors provided too much information that was not always relevant for them. Moreover, patients reported that counselors unintentionally inhibited dialogue and
___________________
17 See the All of Us homepage at https://allofus.nih.gov (accessed October 25, 2019).
18 See the CSER homepage at https://cser-consortium.org (accessed October 25, 2019).
engagement by overloading them with information, but reported that there was insufficient information about recommendations for subsequent care.
To address the challenge of achieving effective communication among patients who have limited health literacy, Joseph and her colleagues developed an intervention based on four principles: (1) The clinician, not the patient, is responsible for effective communication; (2) All patients may benefit from plain language, known as the health literacy universal precautions;19 (3) Patient comprehension can—and should—be verified; and (4) Adapting content to meet the health literacy and numeracy needs of individual patients requires commitment, flexibility, and practice.
Working with genetic counselors who participated in the initial study, Joseph’s team developed and conducted a 4.5-hour training program on strategies to apply these four principles. The intervention also included a component on best practices for collaborating with interpreters to improve communication among genetic counselors and individuals who have limited English proficiency. Results from a pilot study demonstrated that genetic counselors successfully implemented these strategies and that patients were able to sufficiently understand the results and implications of their genetic tests (Joseph et al., 2019).
Joseph stressed that graduate education for genetic counselors should embed communication training and relationship building across all curricula. She added that clinicians should strive for clarity and conciseness when communicating complex health information, even if this simplification reduces precision.
Visual Design Strategies to Improve Cancer Communication
Allison Lazard, assistant professor in the Hussman School of Journalism and Media at the University of North Carolina at Chapel Hill and associate member of the Lineberger Comprehensive Cancer Center, said that cancer communication needs to be engaging and relevant for the intended audience: “We need to know what they think and feel, how they behave, and once we have an understanding of those [things], we can turn to the objective designs.” Lazard added that effectively conveying health information requires consideration and assessment of subjective user experiences through an iterative process of testing and refinement.
Lazard noted that individuals evaluate the quality of health information in the first few milliseconds of exposure, which suggests that messages are
___________________
19 See the AHRQ Health Literacy Universal Precautions Toolkit at https://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/index.html (accessed August 16, 2019) for an example of a universal precautions toolkit.
judged on their design rather than on their content (Lazard et al., 2016). She noted that the health communications literature often recommends the use of effective design, but often fails to identify the objective properties, principles, or strategies of effective design. Lazard proposed the following five principles for effective, clear, and patient-centered design:
- Image relevance: select images relevant to the intended audience. This can be accomplished through pilot testing that asks members of the intended audience to view potential images and identify those that resonate most with the proposed messaging (Lazard et al., 2017).
- Information cues: present information so it can be interpreted at a glance. Audiences prefer designs that present qualitative information supported by contextual cues, even if the simplification reduces precision (Byron et al., 2018; Lazard et al., 2019a).
- Visual hierarchy: use design to guide users’ attention. Design elements—such as large font size and redundant visuals—can be used to direct readers to the most salient information, while color shifts can be used to indicate the introduction of new topics (Lazard et al., 2019b) (see Figure 6).
- Social presence: elicit the feelings of a social experience. In the absence of face-to-face communication, design cues such as human imagery and chat functions can facilitate improved user attention, as well as the perceived trustworthiness and usefulness of the message.
- Mental models: understand the audience’s expectations for the message and interface. Designing effective health messages requires understanding and meeting users’ expectations and preferences for communication, even if they differ from those of the public health community.
The Role of Health Insurance Literacy in Reducing Patient Financial Burden
Mary Politi, professor in the Division of Public Health Sciences, Department of Surgery, Washington University School of Medicine in St. Louis, noted that selecting among health insurance plans requires advanced numeracy skills and comprehension of complex and unfamiliar concepts. However, lack of adequate insurance is associated with serious health and financial consequences; patients with inadequate coverage are more likely to avoid necessary care and to face large financial burdens associated with care (Smith et al., 2018; Tipirneni et al., 2018). Politi noted that patients with cancer are particularly vulnerable to these outcomes. The high costs of cancer care, including patients’ cost-sharing requirements for their care, are associated with missed medical appointments and rationing of prescriptions, even among
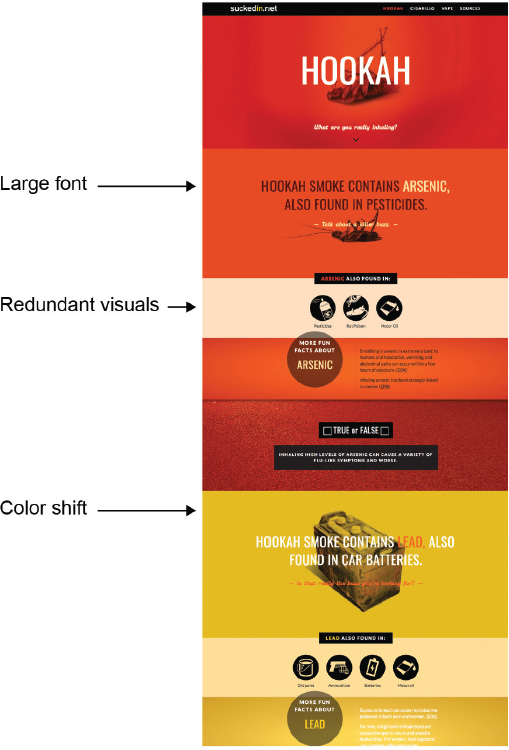
SOURCE: Lazard presentation, July 15, 2019.
patients who have private insurance (Bouberhan et al., 2019; Casilla-Lennon et al., 2018; Dusetzina et al., 2014; Nipp et al., 2016). Politi added that the high financial burden associated with cancer care extends beyond medical consequences; for example, patients with cancer who face high care costs report low quality of life and high levels of medical debt (Banegas et al., 2016; Kale and Carroll, 2016; Ramsey et al., 2013).
Politi said that one opportunity to mitigate financial burdens of care involves clinicians openly discussing treatment costs with patients. She said a survey found that 50 percent of patients reported a desire to discuss costs of
care with their clinicians (Bestvina et al., 2014). These conversations enable patients to make informed decisions about their care and can also help to lower costs with or without making treatment modifications, such as helping a patient enroll in co-pay assistance or switching to a generic medication (Zafar et al., 2015). Politi stressed that clinicians should be proactive in discussing costs of care with patients, rather than avoiding the conversation until financial distress motivates a patient to initiate this discussion. She added that improved clinician training on how to engage patients in these discussions is needed to facilitate and support these important conversations.
Politi described the development and implementation of a web-based, mobile-friendly tool to help patients choose between health insurance plans, called Improving Cancer Patients’ Insurance Choices (I Can PIC). This tool helps patients to (1) understand health insurance and how to use it to manage care, (2) talk to providers about care costs, and (3) identify resources to help offset care costs. The tool also includes a cost calculator that can estimate how much money an individual is likely to spend on their health insurance and care, given their age, gender, type of cancer, type of insurance, and health conditions. In an assessment of I Can PIC, patients who used the tool had more knowledge about health insurance and more confidence in their understanding of insurance terms than patients who did not use the tool. Users were also able to accurately describe complex trade-offs between insurance plans’ costs and coverage.
PROCEDURES, POLICIES, AND PROGRAMS TO ASSESS AND ADDRESS HEALTH LITERACY NEEDS
Many workshop participants described procedures, policies, and programs that health care organizations can employ to assess and address the health literacy needs of patients and their families.
Strategies for Health Care Organizations to Address Low Health Literacy
Urmimala Sarkar, professor of medicine in the Division of General Internal Medicine at UCSF and associate director of the UCSF Center for Vulnerable Populations, described the vision for a health-literate health care organization: it is one where everyone—members of the health care team, the patient, and family members—has the same information, which enables seamless communication and helps patients and clinicians engage in shared decision making.
Sarkar said current communication efforts fall short of this goal and used SCPs as an example of suboptimal communication in health care. She noted
that SCPs are intended to travel with patients after they complete cancer treatment because they contain critical information to guide their subsequent care. Sarkar noted that the effectiveness of SCPs has not been firmly established and their use is hindered by suboptimal implementation (Mendelsohn et al., 2016; Tevaarwerk and Sesto, 2018). Sarkar and her colleagues assessed whether the use of SCPs by health care organizations included the SCP elements recommended in the report From Cancer Patient to Cancer Survivor: Lost in Transition (IOM, 2006), and whether SCPs met patient usability standards, as measured by the Suitability Assessment of Materials.20 They collected 16 SCP documents from safety net hospitals, community hospitals, academic medical centers, and integrated care delivery systems in California and found that most of the plans did not include the recommended elements, and that their language was too complex for patient comprehension. Furthermore, only one SCP document exceeded the “adequate” rating for cultural appropriateness. She noted that SCPs are traditionally created to communicate care information to both patients and their primary care clinicians, but the information needs of these groups may be too disparate to be met with a single document. Sarkar concluded that as currently developed, SCPs are not an optimal strategy for communicating post-treatment information for survivorship care.
Sarkar suggested that health care organizations fundamentally redesign their SCPs, noting that the utility of the documents will evolve as interoperability of electronic health records (EHRs) is achieved. Sarkar described EHR interoperability as a “policy imperative” and stressed the importance of clinicians being able to directly view records from other health care organizations. She stressed that communication among primary care clinicians and oncologists should not be the responsibility of patients. “That is not to say that patients do not absolutely need to have a treatment summary, but the level of detail that is necessary for patients to have in their hands is not the same as what I need as the primary care physician,” said Sarkar. Sarkar said that to provide better survivorship care, primary care clinicians need to have access to their patients’ oncology records.
Patient Navigation Programs
Pratt-Chapman noted that 80 million Americans have trouble understanding and using health information, which can contribute to a lack of
___________________
20 The Suitability Assessment of Materials rates written materials across six domains: content, literacy demand, graphics, layout and type, learning stimulation and motivation, and cultural appropriateness. See SAM: Suitability Assessment of Materials for Evaluation of Health-Related Information for Adults at http://aspiruslibrary.org/literacy/SAM.pdf (accessed September 26, 2019) for additional information.
preventive care, reduced adherence to treatment regimens, increased hospitalization, lower health status, and higher mortality (Berkman et al., 2011). Pratt-Chapman stressed that patient navigation programs can be a key strategy for reducing the adverse effects of health literacy limitations, noting that navigators can help coordinate patients’ care, assess and address barriers to care, and promote healthy behaviors and effective coping strategies (NASEM, 2018a). She added that navigation services can help support patients’ health literacy and communication needs across the continuum of cancer care (Pratt-Chapman et al., 2015) (see Figure 7).
Pratt-Chapman said that patient navigation services should be targeted to address particular patient needs within an organization or community (Willis et al., 2013) and that navigation services need to be sensitive to the contextual barriers to effective care delivery. She proposed that navigation services and providers be tailored to meet specific health objectives: for example, she said that community health workers would be most appropriate to deliver health promotion interventions, while nurse navigators would be most appropriate to provide symptom management during active cancer care.
Pratt-Chapman said that it is often difficult to secure and sustain funding for patient navigation services, and she proposed several opportunities to make the business case for patient navigation and improving sustainability:
- Document the value of patient navigation, both for improving patient care and for reducing health care expenditures (Kline et al., 2019). She noted that metrics such as patient satisfaction, patient engagement, time to diagnosis and treatment, patient adherence, reduced acute encounters, greater efficiency, and cost savings can be used to demonstrate the value of navigation programs. Pratt-Chapman also noted that navigation can serve as a cost-saving measure under both value-based and fee-for-service reimbursement models. For example, patient navigators at the University of Alabama at Birmingham, a value-based system, saved $781.29 per navigated patient through reduced emergency department, intensive care unit, and unplanned hospital admissions (Kline et al., 2019). At the University of Pennsylvania Health System, which operates on a fee-for-service basis, patients with navigation support were 10 percent more likely to stay in the health system and receive multiple treatment modalities (Kline et al., 2019).
- Provide health systems with up-front investments and ongoing financial support for team-based cancer care. Pratt-Chapman noted that the Oncology Care Model,21 a demonstration project of the Centers
___________________
21 Additional information is available at https://innovation.cms.gov/initiatives/oncology-care (accessed August 16, 2019).
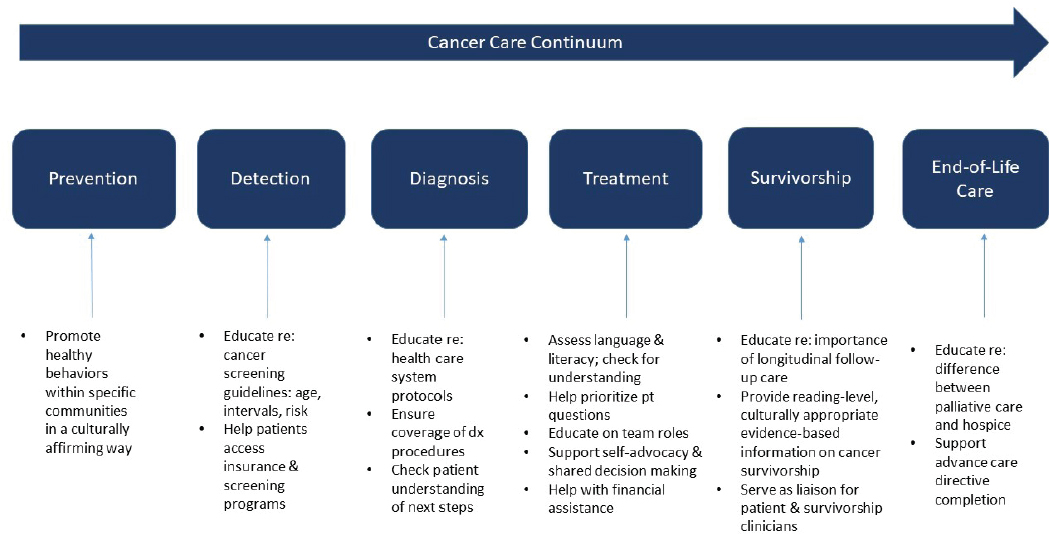
NOTES: While education on palliative care, hospice care, and advanced care planning are included in this diagram as a component of end-of-life care, they are important across the continuum of cancer care (IOM, 2013b). dx = diagnosis; pt = patient.
SOURCES: Pratt-Chapman presentation, July 16, 2019; Pratt-Chapman et al., 2015. Reprinted with permission from the Journal of Oncology Navigation & Survivorship. Pratt-Chapman, M, Willis A, and Masselink L. Core competencies for oncology patient navigators. Journal of Oncology Navigation & Survivorship. 2015;6:16–21. © Green Hill Healthcare.
- for Medicare & Medicaid Services, provides oncology practices with $160 per patient per month and requires the use of patient navigation. Although Pratt-Chapman questioned whether $160 per patient per month is sufficient, she supported the use of payment incentives for care coordination as a potentially viable model to support patient navigation. She added that the 2018 National Comprehensive Cancer Network Policy Summit working group also recommended coding mechanisms to reimburse team-based care and that several proposed congressional bills would facilitate team-based reimbursement under Medicare and Medicaid.
- Promote the use of flexible budgeting to correct misaligned incentives and enable all participants to share in the financial benefits of improving the quality and reducing the costs of care. She noted that with navigation services, there is often misalignment between those that fund and provide navigation services and those that financially benefit, and that navigation programs may increase a health care organization’s costs in the short term. Pratt-Chapman suggested that flexible budgeting could be used to reduce these barriers (Nichols and Taylor, 2018). Pratt-Chapman said the key is to use a trusted broker to share cost savings among all participants involved.
Supporting Patient Self-Management in Oncology
“Supporting patients and families in the very complex tasks of monitoring, communicating, and managing disease- and treatment-related symptoms is essential for quality cancer care,” said Heidi Donovan, professor of nursing and medicine at the University of Pittsburgh School of Nursing, co-director of the National Rehabilitation Research and Training Center on Family Support at the University of Pittsburgh, and director of the GynOnc Family CARE Center at Magee-Womens Hospital of the University of Pittsburgh Medical Center. She discussed the importance of supporting patients and families in engaging in self-management, defined as the tasks of illness-related work for patients with cancer and their families. “Self-management is the awareness and active participation by the person [and their family] in their recovery, recuperation, and rehabilitation to minimize the consequences of treatment and promote survival, health, and wellbeing” (Barlow et al., 2002). Donovan noted that effective self-management is not a knowledge-based skill that can be taught, but rather a behavior that requires ongoing support and resources from an interdisciplinary health care team. Core elements of self-management support in cancer care include increasing confidence to manage symptoms and illness, supporting self-monitoring, facilitating knowledge and uptake of health behaviors, and supporting the development of skills for communicating with a care team.
Donovan outlined three domains across which patients with cancer need to manage their disease: illness-related work, biographical work, and everyday life work (Corbin and Strauss, 1985). Illness-related work refers to tasks and knowledge about cancer and its treatment, such as maintaining treatment regimens, managing symptoms, and navigating transitions in care. Biographical work refers to tasks associated with maintaining a sense of identity during the course of a patient’s cancer diagnosis and treatment. It includes tasks such as coming to terms with a new normal, contextualizing cancer within a person’s life, and reframing a person’s identity. Everyday life work refers to the tasks of life that require attention even during cancer treatment, such as occupational work, maintaining relationships, emotional and psychological self-care, and health maintenance.
Donovan proposed several policy opportunities to promote effective self-management and support patients with cancer and their family members. She noted that informal caregivers provide an estimated 37 billion hours of care each year for patients with chronic illness,22 at an estimated economic value of $470 billion (Reinhard et al., 2015). This effort entails significant personal costs, and caregiving is associated with adverse psychological and physical health effects (Bell et al., 2019). To better support caregivers, Donovan suggested that the oncology community participate actively in policy initiatives to support families who care for their loved ones with cancer (Bell et al., 2019; NASEM, 2016). Within the clinical setting, she suggested that the oncology community encourage family caregiving by identifying and supporting family caregivers and involving them as integral members of the care team throughout the continuum of cancer care. She also suggested that caregivers could benefit from training to improve their health literacy, but acknowledged that it can be difficult to deliver caregiver education without adding to their burdens.
Donovan described a program, the GynOnc Family CARE Center, that she has implemented to support family caregivers at the University of Pittsburgh Medical Center’s Magee-Womens Hospital. The program identifies the primary caregiver for new patients, gathers basic information about that caregiver, and reaches out to them with emotional and informational support. An additional component of the program uses the National Comprehensive Cancer Network’s distress thermometer and problem list to identify the unmet needs of caregivers23 so they can be addressed by navigators with social care expertise and other staff members from the multidisciplinary clinical care team.
___________________
22 Donovan estimated that approximately 9 percent of family caregivers are taking care of patients with cancer.
23 Additional information is available at https://www.nccn.org/about/permissions/thermometer.aspx (accessed August 19, 2019).
Donovan also recommended that the oncology community advocate for policies and systems that promote multidisciplinary care teams in which each member is able to work at the full capacity of their training and licensure (IOM, 2010). Lastly, she suggested identifying and implementing models of care and payment that enable the health care team to support self-management across key transitions in the cancer care trajectory. This would shift the oncology paradigm from an acute care model to a chronic disease model and would incorporate lessons from areas such as diabetes education and management and cardiac rehabilitation. “The work of everyday life does not stop with cancer,” said Donovan, “so we need to design our health care system to better support families.”
Policies and Incentives for Health Insurers
Kim Parson, strategic consultant and leader of enterprise health literacy efforts at Humana, described her organization’s initiatives to support patients’ health literacy and promote effective communication in oncology. These initiatives include education about cancer prevention and screening, efforts to address the social determinants of health, and nurse outreach programs for patients with cancer. Parson said that a primary goal of Humana’s initiatives is to help patients navigate the health care system and reduce their administrative burdens.
Parson noted that Humana offers its members education about preventive screenings using direct mail, the Humana website and mobile applications, and primary care clinicians, health coaches, and personal nurses. These communication channels are selected based on patient preferences. Parson noted that communication about preventive care is delivered by all Humana staff. For example, when a member calls customer service, the representative will remind the caller if they have any pending screenings and will offer to transfer them to the scheduling department. Humana also incentivizes screening by providing gift cards for food and services as a reward for completion.
Parson described Humana’s efforts to proactively identify and address the social determinants of health of its members, noting that this is fundamental to achieving effective health care. She described the screening tools Humana uses to identify members who face challenges such as food insecurity or social isolation. When these screening tools identify a member in need of support, solutions are provided by a Humana Care program nurse who can offer referrals to resources such as food assistance.
Parson also described Humana’s cancer program, which aims to help patients with cancer optimize health outcomes and quality of life. Members undergoing active cancer treatment are identified through authorization requests, internal program referrals, and member calls. The program is
delivered by a team of oncology nurses, who provide support and education via telephone outreach. Phone calls are tailored to patients’ individual needs and provide education about the patient’s diagnosis, treatment, possible side effects, and nutritional needs. The nurses also provide assistance with patient navigation, including orienting patients to members of their care team and identifying the role that each member plays in patient care. Parson noted that, on average, Humana members with cancer spend 100 days in the program.
Parson noted that Humana is also working to improve patient experiences and health outcomes by coordinating cancer care delivery through its Oncology Model of Care program. In this program, Humana collaborates with oncology practices to build infrastructure for initiatives that support patients with cancer, including improving access to care; screening patients with cancer for depression and pain; better aligning care with patients’ values, preferences, and needs; and delivering patient and family education about different aspects of care.
STAKEHOLDER PERSPECTIVES AND PRIORITIES
Many workshop participants representing diverse backgrounds and roles in cancer care discussed opportunities for action to improve cancer communication and to better support the health literacy needs of patients and their families.
Potential Priorities in Research
Meade noted that during her 25-year tenure at a cancer center, she has learned that the cancer community needs to improve its strategies for disseminating information about cancer research and care. She added that it is important to include diverse perspectives in health research and to incorporate input from patients and the broader community. Darci Graves, special assistant to the director of the Office of Minority Health at the Centers for Medicare & Medicaid Services, agreed with the need for better communication between health researchers and the public. She implored the health care community to use available research to inform efforts in health literacy and to collaborate with diverse populations. Graves said that when conducting research, it is imperative to explain to community members why the data are needed and the purposes for which they will be used. Chou also spoke about the importance of community engagement and encouraged investigators to build multidisciplinary research teams that include patient representatives.
Potential Priorities in Clinical Care
Chou discussed her experiences as a caregiver for a loved one with cancer and how important it was for clinicians to listen to and elicit patients’ and their families’ values and preferences, and to identify patients’ concerns and information needs and tailor messages to address them. She said that improved training on listening is needed throughout health profession education. Chou added that clinical workflow routines should be modified to place the patient’s questions and concerns at the forefront of clinical encounters. She also suggested engaging experts on user-centered design to develop user-friendly educational materials and involving individuals who are skilled at patient communication on care teams.
Claire Saxton, senior director for education and outreach at Cancer Support Community, described a tool called Values Outcomes in Cancer Experience, which her organization developed to elicit patients’ values regarding their cancer care and to promote discussions about values among patients and family members. She noted that value is typically described as the relationship between health benefits and the financial costs of treatment, but in discussions of value with patients and caregivers, she said that families often describe their values in terms of quality of life and the quality of their relationships.
Saxton proposed convening members of advocacy organizations, industry partners, and health education specialists to develop a consistent language for discussing cancer care innovations. She said that patients and families often need to reconcile three different frameworks and terminologies of cancer care proposed by industry, clinicians, and patient advocacy groups. She noted that patients are often confused by the complexity of oncology care and stressed the importance of conveying a coherent framework for understanding the rapidly evolving landscape of cancer care.
Gwen Darien, executive vice president for patient advocacy and engagement at the National Patient Advocate Foundation, said that her experiences as a three-time cancer survivor and patient advocate have informed her perspectives on effective communication in cancer. She said that clinicians should use clear language—free from jargon—to promote an open dialogue. She added that supporting the health literacy needs of patients and their families is critical to achieving accessible, high-quality, affordable, and equitable health care. Rather than placing the burden on patients to learn how to effectively communicate with their clinicians, she said that the onus for communication should be on health care team members: “We do not need to give people words. We have to understand the words people are saying.”
Darien said that trust is a fundamental part of communication, and she emphasized that building trust should be central in any effort to improve communication and address patients’ health literacy needs. She stressed that trust is bidirectional: the patient needs to trust the clinician and the clinician
also needs to trust the patient. Kagawa Singer agreed that trust is a critical element of patient–clinician communication and stressed that listening with undivided attention promotes trust-building. “When any clinician listens to their patient in that way, the trust—the bond—is built and you can go forward as a team,” she said.
Graves, speaking from her perspectives as a cancer survivor and expert in health equity, emphasized that clinicians should tailor every interaction to meet the cultural and linguistic preferences of the patient and their family members. “Patient-centered care needs to be culturally and linguistically appropriate. We don’t need to do more—we just need to do better,” she said. Graves suggested that culturally and linguistically appropriate communication need to be embedded across the entire health care system. This fundamental change will require the active involvement and input of members of the community. “We are here to work with our communities to help them achieve their highest level of health.”
Robert Winn, associate vice chancellor for community-based practice at the University of Illinois at Chicago and director of the University of Illinois Cancer Center, agreed that community involvement is critical to advancing progress. He described an initiative in which he paired senior leaders of the cancer center with community leaders. Over the course of 1 year, community leaders mentored the cancer center leaders and voiced the issues that were important to community members. Collectively, these interactions helped develop better communication and outreach strategies. Winn added that health literacy is bidirectional; patients need to be conversant in the language of health, but health care systems also need to be conversant in the languages and concerns of the communities they serve.
WRAP-UP
Basen-Engquist summarized key messages from the workshop. She called for additional research to design and evaluate multilevel interventions to improve health literacy and patient–clinician communication. She noted that many participants spoke about the importance of building trust and strong partnerships between health care organizations and communities across the cancer care continuum. These efforts require effective communication between patients and clinicians, and within the clinical care team. Basen-Engquist also stressed the importance of team-based collaborative cancer care that fully engages patients and families and tailors information to meet their needs. “Once you become a patient, I think it’s really hard to stay in that mode where you’re one person alone making decisions. You rely on your network,” she said. Paasche-Orlow agreed that collaboration is essential for high-quality care. He concluded the workshop in rhyming verse: “health literacy across the continuum of cancer care, empower if you dare.”
REFERENCES
ACS (American Cancer Society). 2019. Cancer facts & figures 2019. Atlanta, GA: American Cancer Society.
Amendola, L. M., J. S. Berg, C. R. Horowitz, F. Angelo, J. T. Bensen, B. B. Biesecker, L. G. Biesecker, G. M. Cooper, K. East, K. Filipski, S. M. Fullerton, B. D. Gelb, K. A. B. Goddard, B. Hailu, R. Hart, K. Hassmiller-Lich, G. Joseph, E. E. Kenny, B. A. Koenig, S. Knight, P. Y. Kwok, K. L. Lewis, A. L. McGuire, M. E. Norton, J. Ou, D. W. Parsons, B. C. Powell, N. Risch, M. Robinson, C. Rini, S. Scollon, A. M. Slavotinek, D. L. Veenstra, M. P. Wasserstein, B. S. Wilfond, L. A. Hindorff, S. E. Plon, and G. P. Jarvik. 2018. The clinical sequencing evidence-generating research consortium: Integrating genomic sequencing in diverse and medically underserved populations. American Journal of Human Genetics 103(3):319–327.
Arnold, R. M., A. L. Back, W. F. Baile, K. A. Edwards, and J. A. Tulsky. 2017. The oncotalk/vitaltalk model. In Oxford textbook of communication in oncology and palliative care, 2nd ed., edited by D. W. Kissane, B. D. Bultz, P. N. Butow, C. L. Bylund, S. Noble, and S. Wilkinson. Oxford, UK: Oxford University Press.
Back, A. L., R. M. Arnold, W. F. Baile, K. A. Fryer-Edwards, S. C. Alexander, G. E. Barley, T. A. Gooley, and J. A. Tulsky. 2007. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Archives of Internal Medicine 167(5):453–460.
Back, A., R. Arnold, and J. Tulsky. 2009. Mastering communication with seriously ill patients: Balancing honesty with empathy and hope. Cambridge, UK: Cambridge University Press.
Back, A. L., E. K. Fromme, and D. E. Meier. 2019. Training clinicians with communication skills needed to match medical treatments to patient values. Journal of the American Geriatrics Society 67(S2):S435–S441.
Banegas, M. P., G. P. Guy, Jr., J. S. de Moor, D. U. Ekwueme, K. S. Virgo, E. E. Kent, S. Nutt, Z. Zheng, R. Rechis, and K. R. Yabroff. 2016. For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Affairs 35(1):54–61.
Barlow, J., C. Wright, J. Sheasby, A. Turner, and J. Hainsworth. 2002. Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling 48(2):177–187.
Bell, J. F., R. L. Whitney, and H. M. Young. 2019. Family caregiving in serious illness in the United States: Recommendations to support an invisible workforce. Journal of the American Geriatrics Society 67(S2):S451–S456.
Berkman, N. D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, and K. Crotty. 2011. Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine 155(2):97–107.
Bernacki, R., J. Paladino, B. A. Neville, M. Hutchings, J. Kavanagh, O. P. Geerse, J. Lakin, J. J. Sanders, K. Miller, S. Lipsitz, A. A. Gawande, and S. D. Block. 2019. Effect of the serious illness care program in outpatient oncology: A cluster randomized clinical trial effect of the serious illness care program in outpatient oncology. JAMA Internal Medicine 179(6):751–759.
Bestvina, C. M., L. L. Zullig, C. Rushing, F. Chino, G. P. Samsa, I. Altomare, J. Tulsky, P. Ubel, D. Schrag, J. Nicolla, A. P. Abernethy, J. Peppercorn, and S. Y. Zafar. 2014. Patient-oncologist cost communication, financial distress, and medication adherence. Journal of Oncology Practice 10(3):162–167.
Bluethmann, S. M., A. B. Mariotto, and J. H. Rowland. 2016. Anticipating the “Silver Tsunami”: prevalence trajectories and comoribidity burden among older cancer survivors in the United States. Cancer Epidemiology, Biomarkers, and Prevention 25:1029–1036.
Bouberhan, S., M. Shea, A. Kennedy, A. Erlinger, H. Stack-Dunnbier, M. K. Buss, L. Moss, K. Nolan, C. Awtrey, J. L. Dalrymple, L. Garrett, F. W. Liu, M. R. Hacker, and K. M. Esselen. 2019. Financial toxicity in gynecologic oncology. Gynecologic Oncology 154(1):8–12.
Byron, M. J., A. J. Lazard, E. Peters, H. Vu, A. Schmidt, and N. T. Brewer. 2018. Effective formats for communicating risks from cigarette smoke chemicals. Tobacco Regulatory Science 4(2):16–29.
Cartwright, L. A., L. Dumenci, J. B. Cassel, M. D. Thomson, and R. K. Matsuyama. 2017. Health literacy is an independent predictor of cancer patients’ hospitalizations. Health Literacy Research and Practice 1(4):e153–e162.
Casilla-Lennon, M. M., S. K. Choi, A. M. Deal, J. T. Bensen, G. Narang, P. Filippou, B. McCormick, R. Pruthi, E. Wallen, H. J. Tan, M. Woods, M. Nielsen, and A. Smith. 2018. Financial toxicity among patients with bladder cancer: Reasons for delay in care and effect on quality of life. Journal of Urology 199(5):1166–1173.
Childers, J. W., A. L. Back, J. A. Tulsky, and R. M. Arnold. 2017. Remap: A framework for goals of care conversations. Journal of Oncology Practice 13(10):e844–e850.
Chou, W. S., A. Oh, and W. M. P. Klein. 2018. Addressing health-related misinformation on social media. JAMA 320(23):2417–2418.
Coccia, P. F., A. S. Pappo, L. Beaupin, V. F. Borges, S. C. Borinstein, R. Chugh, and S. Dinner. 2018. Adolescent and young adult oncology, version 2.2018, NCCN clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network 16(1):66–97.
Colby, S. L., and J. M. Ortman. 2014. Projections of the size and composition of the U.S. population: 2014 to 2060. Washington, DC: U.S. Census Bureau.
Collins, P. H., and S. Blige. 2016. Intersectionality. Malden, MA: Polity Press.
Corbin, J., and A. Strauss. 1985. Managing chronic illness at home: Three lines of work. Qualitative Sociology 8(3):224–247.
Curtis, J. R., L. Downey, A. L. Back, E. L. Nielsen, S. Paul, A. Z. Lahdya, P. D. Treece, P. Armstrong, R. Peck, and R. A. Engelberg. 2018. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Internal Medicine 178(7):930–940.
Detering, K. M., A. D. Hancock, M. C. Reade, and W. Silvester. 2010. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ 340:c1345.
Dickson, R. P., R. A. Engelberg, A. L. Back, D. W. Ford, and J. R. Curtis. 2012. Internal medicine trainee self-assessments of end-of-life communication skills do not predict assessments of patients, families, or clinician-evaluators. Journal of Palliative Medicine 15(4):418–426.
Dusetzina, S. B., A. N. Winn, G. A. Abel, H. A. Huskamp, and N. L. Keating. 2014. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. Journal of Clinical Oncology 32(4):306–311.
Economou, D., and A. Reb. 2017. Communication concerns when transitioning to cancer survivorship care. Seminars in Oncology Nursing 33(5):526–535.
Epstein, R. M., and R. L. Street, Jr. 2007. Patient-centered communication in cancer care: Promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute.
Ferrell, B. R., M. L. Twaddle, A. Melnick, D. E. Meier. 2018. National consensus project clinical practice guidelines for quality palliative care guidelines. Journal of Palliative Medicine 21(12):1684–1689.
Gade, G., I. Venohr, D. Conner, K. McGrady, J. Beane, R. H. Richardson, M. P. Williams, M. Liberson, M. Blum, and R. Della Penna. 2008. Impact of an inpatient palliative care team: A randomized control trial. Journal of Palliative Medicine 11(2):180–190.
Gilligan, T., N. Coyle, R. M. Frankel, D. L. Berry, K. Bohlke, R. M. Epstein, E. Finlay, V. A. Jackson, C. S. Lathan, C. L. Loprinzi, L. H. Nguyen, C. Seigel, and W. F. Baile. 2017. Patient-clinician communication: American Society of Clinical Oncology consensus guideline. Journal of Clinical Oncology 35(31):3618–3632.
Glasgow, R. E., T. M. Vogt, and S. M. Boles. 1999. Evaluating the public health impact of health promotion interventions: The re-aim framework. American Journal of Public Health 89(9):1322–1327.
Ha, V. T. D., J. Frizzo-Barker, and P. Chow-White. 2018. Adopting clinical genomics: A systematic review of genomic literacy among physicians in cancer care. BMC Medical Genomics 11(1):18.
Harris Poll. 2010. “Cyberchondriacs” on the rise? Those who go online for healthcare information continues to increase. https://theharrispoll.com/the-latest-harris-poll-measuring-how-many-people-use-the-internet-to-look-for-information-about-health-topics-finds-that-the-numbers-continue-to-increase-the-harris-poll-first-used-the-word-cyberch (accessed October 25, 2019).
Heckinger, E. A., C. L. Bennett, T. Davis, and M. S. Wolf. 2004. Health literacy and cancer care: Do patients really understand. Journal of Clinical Oncology 22(14 Suppl):6045.
Henrich, J., S. J. Heine, and A. Norenzayan. 2010a. Most people are not weird. Nature 466:29.
Henrich, J., S. J. Heine, and A. Norenzayan. 2010b. The weirdest people in the world? Behavioral and Brain Sciences 33(2-3):61–83; discussion 83–135.
Horowitz, R., R. Gramling, and T. Quill. 2014. Palliative care education in U.S. medical schools. Medical Education 48(1):59–66.
Hurle, B., T. Citrin, J. F. Jenkins, K. A. Kaphingst, N. Lamb, J. E. Roseman, and V. L. Bonham. 2013. What does it mean to be genomically literate? National Human Genome Research Institute meeting report. Genetics in Medicine 15(8):658–663.
IOM (Institute of Medicine). 2003. Childhood cancer survivorship: Improving care and quality of life. Washington, DC: The National Academies Press.
IOM. 2004. Health literacy: A prescription to end confusion. Washington, DC: The National Academies Press.
IOM. 2006. From cancer patient to cancer survivor: Lost in transition. Washington, DC: The National Academies Press.
IOM. 2010. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
IOM. 2012. How far have we come in reducing health disparities? Progress since 2000: Workshop summary. Washington, DC: The National Academies Press.
Joseph, G., R. J. Pasick, D. Schillinger, J. Luce, C. Guerra, and J. K. Y. Cheng. 2017. Information mismatch: Cancer risk counseling with diverse underserved patients. Journal of Genetic Counseling 26(5):1090–1104.
Joseph, G., R. Lee, R. J. Pasick, C. Guerra, D. Schillinger, and S. Rubin. 2019. Effective communication in the era of precision medicine: A pilot intervention with low health literacy patients to improve genetic counseling communication. European Journal of Medical Genetics 62(5):357–367.
Kagawa Singer, M., W. Dressler, S. George, and W. Elwood. 2015. The cultural framework for health: An integrative approach for research and program design and evaluation. Bethesda, MD: National Institutes of Health.
Kale, H. P., and N. V. Carroll. 2016. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer 122(8):283–289.
King, L., G. P. Quinn, S. T. Vadaparampil, C. K. Gwede, C. A. Miree, C. Wilson, H. Clayton, and K. Perrin. 2008a. Oncology nurses’ perceptions of barriers to discussion of fertility preservation with patients with cancer. Clinical Journal of Oncology Nursing 12(3):467–476.
King, L., G. P. Quinn, S. T. Vadaparampil, C. A. Miree, C. Wilson, H. Clayton, and B. Zebrack. 2008b. Oncology social workers’ perceptions of barriers to discussing fertility preservation with cancer patients. Social Work in Health Care 47(4):479–501.
Kline, R. M., G. B. Rocque, E. A. Rohan, K. A. Blackley, C. A. Cantril, M. L. Pratt-Chapman, H. A. Burris, and L. N. Shulman. 2019. Patient navigation in cancer: The business case to support clinical needs. Journal of Oncology Practice 15(11):585–590. doi: 10.1200/JOP.19.00230.
Knolhoff, J. B., B. Djenic, C. H. Hsu, M. E. Bouton, and I. K. Komenaka. 2016. Missed appointments in a breast clinic: Patient-related factors. American Journal of the Medical Sciences 352(4):337–342.
Kutner, M., E. Greenburg, Y. Jin, and C. Paulsen. 2006. The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy. (NCES 2006-483). Washington, DC: U.S. Department of Education.
Langewitz, W. A., P. Eich, A. Kiss, and B. Wossmer. 1998. Improving communication skills—A randomized controlled behaviorally oriented intervention study for residents in internal medicine. Psychosomatic Medicine 60(3):268–276.
Larsson, A., A. D. Oxman, C. Carling, and J. Herrin. 2003. Medical messages in the media—Barriers and solutions to improving medical journalism. Health Expectations 6(4):323–331.
Lazard, A. J., I. Watkins, M. S. Mackert, B. Xie, K. K. Stephens, and H. Shalev. 2016. Design simplicity influences patient portal use: The role of aesthetic evaluations for technology acceptance. Journal of the American Medical Informatics Association 23:e157–e161.
Lazard, A. J., A. Schmidt, H. Vu, M. J. Byron, E. Peters, M. H. Boynton, and N. T. Brewer. 2017. Icons for health effects of cigarette smoke: A test of semiotic type. Journal of Behavioral Medicine 40(4):641–650.
Lazard, A. J., M. J. Byron, H. Vu, E. Peters, A. Schmidt, and N. T. Brewer. 2019a. Website designs for communicating about chemicals in cigarette smoke. Health Communication 34:333–342.
Lazard, A. J., J. Pikowski, L. Horrell, J. C. Ross, S. M. Noar, and E. L. Sutfin. 2019b. Adolescents’ and young adults’ aesthetics and functionality preferences for online tobacco education. Journal of Cancer Education.
Lupu, D. 2010. Estimate of current hospice and palliative medicine physician workforce shortage. Journal of Pain and Symptom Management 40(6):899–911.
Mack, J. W., J. C. Weeks, A. A. Wright, S. D. Block, and H. G. Prigerson. 2010. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. Journal of Clinical Oncology 28(7):1203–1208.
Mack, J. W., A. Cronin, N. L. Keating, N. Taback, H. A. Huskamp, J. L. Malin, C. C. Earle, and J. C. Weeks. 2012. Associations between end-of-life discussion characteristics and care received near death: A prospective cohort study. Journal of Clinical Oncology 30(35):4387–4395.
Mayer, D. K., L. Nekhlyudov, C. F. Snyder, J. K. Merrill, D. S. Wollins, and L. N. Shulman. 2014. American Society of Clinical Oncology clinical expert statement on cancer survivorship care planning. Journal of Oncology Practice 10(6):345–351.
Meade, C. D. 2005. Cancer, culture and literacy: Critical next steps in improving care for diverse populations. Cancer Control 12(Suppl 2):4–5.
Meade, C. D., S. M. Christy, and C. K. Gwede. 2018. Improving communications with older cancer patients. Geriatric Oncology 1–23.
Mehnert, A., E. Brahler, H. Faller, M. Harter, M. Keller, H. Schulz, K. Wegschedier, J. Weis, A. Boehncke, B. Hund, K. Reuter, M. Richard, S. Sehner, S. Sommerfeldt, C. Szalai, H. U. Wittchen, and U. Koch. 2014. Four-week prevalence of mental disorders in patients with cancer across major tumor entitites. Journal of Clinical Oncology 32(31):3540–3546.
Mendelsohn, M., J. E. Mortimer, L. Popplewell, L. L. Lai, E. Maghami, and D. Economou. 2016. Challenges in the implementation of survivorship care plans in an NCI-designated cancer center. Journal of Clinical Oncology 34(3 Suppl):68.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Families caring for an aging America. Washington, DC: The National Academies Press.
NASEM. 2017. Cancer care in low-resource areas: Cancer treatment, palliative care, and survivorship care: Proceedings of a workshop. Washington, DC: The National Academies Press.
NASEM. 2018a. Establishing effective patient navigation programs in oncology. Washington, DC: The National Academies Press.
NASEM. 2018b. Long-term survivorship care after cancer treatment: Proceedings of a workshop. Washington, DC: The National Academies Press.
NCI (National Cancer Institute). 2018. Adolescents and young adults with cancer. https://www.cancer.gov/types/aya (accessed September 20, 2019).
Nichols, L. M., and L. A. Taylor. 2018. Social determinants as public goods: A new approach to financing key investments in healthy communities. Health Affairs 37(8):1223–1230.
Nipp, R. D., L. L. Zullig, G. Samsa, J. M. Peppercorn, D. Schrag, D. H. Taylor, Jr., A. P. Abernethy, and S. Y. Zafar. 2016. Identifying cancer patients who alter care or lifestyle due to treatment-related financial distress. Psycho-Oncology 25(6):719–725.
ODPHP (Office of Disease Prevention and Health Promotion). 2010. National action plan to improve health literacy. Washington, DC: U.S. Department of Health and Human Services.
Oktay, K., B. E. Harvey, A. H. Partridge, G. P. Quinn, J. Reinecke, H. S. Taylor, W. H. Wallace, E. T. Wang, and A. W. Loren. 2018. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. Journal of Clinical Oncology 36(19):1994–2001.
Paladino, J., R. Bernacki, B. A. Neville, J. Kavanagh, S. P. Miranda, M. Palmor, J. Lakin, M. Desai, D. Lamas, J. J. Sanders, J. Gass, N. Henrich, S. Lipsitz, E. Fromme, A. A. Gawande, and S. D. Block. 2019. Evaluating an intervention to improve communication between oncology clinicians and patients with life-limiting cancer: A cluster randomized clinical trial of the serious illness care program. JAMA Oncology 5(6):801–809.
Popejoy, A. B., and S. M. Fullerton. 2016. Genomics is failing on diversity. Nature News 538(7624):161.
Pratt-Chapman, M., A. Willis, and L. Masselink. 2015. Core competencies for oncology patient navigators. Journal of Oncology Navigation and Survivorship 6(2):16–21.
PUR/C (PerryUndem Research/Communication). 2016. Physicians’ views toward advance care planning and end-of-life care conversations. https://www.johnahartford.org/images/uploads/resources/ConversationStopper_Poll_Memo.pdf (accessed October 31, 2019).
Quinn, G. P., and S. T. Vadaparampil. 2009. Fertility preservation and adolescent/young adult cancer patients: Physician communication challenges. Journal of Adolescent Health 44(4):394–400.
Quinn, G. P., S. T. Vadaparampil, C. K. Gwede, C. Miree, L. M. King, H. B. Clayton, C. Wilson, and P. Munster. 2007. Discussion of fertility preservation with newly diagnosed patients: Oncologists’ views. Journal of Cancer Survivorship 1(2):146–155.
Quinn, G. P., S. T. Vadaparampil, B. A. Bell-Ellison, C. K. Gwede, and T. L. Albrecht. 2008. Patient-physician communication barriers regarding fertility preservation among newly diagnosed cancer patients. Social Science & Medicine 66(3):784–789.
Ramsey, S., D. Blough, A. Kirchhoff, K. Kreizenbeck, C. Fedorenko, K. Snell, P. Newcomb, W. Hollingworth, and K. Overstreet. 2013. Washington state cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Affairs 32(6):1143–1152.
Reinhard, S., L. F. Feinberg, R. Choula, and A. Houser. 2015. Valuing the invaluable 2015 update. Washington, DC: AARP Public Policy Institute.
Robinson, L., S. R. Cotten, H. Ono, A. Quan-Haase, G. Mesch, W. Chen, J. Schulz, T. M. Hale, and M. J. Stern. 2015. Digital inequalities and why they matter. Information, Communication & Society 18(5):569–582.
Rust, C. F., C. Davis, and M. R. Moore. 2015. Medication adherence skills training for African-American breast cancer survivors: The effects on health literacy, medication adherence, and self-efficacy. Social Work in Health Care 54(1):33–46.
Schwartzberg, J. G., A. Cowett, J. VanGeest, and M. S. Wolf. 2007. Communication techniques for patients with low health literacy: A survey of physicians, nurses, and pharmacists. American Journal of Health Behavior 31(Suppl 1):S96–S104.
Schwitzer, G. 2008. How do US journalists cover treatments, tests, products, and procedures? An evaluation of 500 stories. PLOS Medicine 5(5):e95.
Smith, C. E., S. M. Fullerton, K. A. Dookeran, H. Hampel, A. Tin, N. M. Maruthur, J. C. Schisler, J. A. Henderson, K. L. Tucker, and J. M. Ordovás. 2016. Using genetic technologies to reduce, rather than widen, health disparities. Health Affairs 35(8):1367–1373.
Smith, K. T., D. Monti, N. Mir, E. Peters, R. Tipirneni, and M. C. Politi. 2018. Access is necessary but not sufficient: Factors influencing delay and avoidance of health care services. MDM Policy & Practice 3(1):2381468318760298.
Southwell, B. G., J. Niederdeppe, J. N. Cappella, A. Gaysynsky, D. E. Kelley, A. Oh, E. B. Peterson, and W. S. Chou. 2019. Misinformation as a misunderstood challenge to public health. American Journal of Preventive Medicine 57(2):282–285.
Sumner, P., S. Vivian-Griffiths, J. Boivin, A. Williams, C. A. Venetis, A. Davies, J. Ogden, L. Whelan, B. Hughes, B. Dalton, F. Boy, and C. D. Chambers. 2014. The association between exaggeration in health related science news and academic press releases: Retrospective observational study. BMJ 349:g7015.
Tevaarwerk, A. J., and M. E. Sesto. 2018. Continued challenges to the adoption and implementation of survivorship care plans. Journal of Oncology Practice 14(10):573–576.
Tipirneni, R., M. C. Politi, J. T. Kullgren, E. C. Kieffer, S. D. Goold, and A. M. Scherer. 2018. Association between health insurance literacy and avoidance of health care services owing to cost. JAMA Network Open 1(7):e184796.
Tulsky, J. A., R. M. Arnold, S. C. Alexander, M. K. Olsen, A. S. Jeffreys, K. L. Rodriguez, C. S. Skinner, D. Farrell, A. P. Abernethy, and K. I. Pollak. 2011. Enhancing communication between oncologists and patients with a computer-based training program: A randomized trial. Annals of Internal Medicine 155(9):593–601.
Turkoglu, A. R., H. Demirci, S. Coban, M. Guzelsoy, E. Toprak, M. M. Aydos, D. A. Ture, and Y. Ustundag. 2018. Evaluation of the relationship between compliance with the follow-up and treatment protocol and health literacy in bladder tumor patients. Aging Male 22(4):266–271.
Vadaparampil, S. T., H. Clayton, G. P. Quinn, L. M. King, M. Nieder, and C. Wilson. 2007. Pediatric oncology nurses’ attitudes related to discussing fertility preservation with pediatric cancer patients and their families. Journal of Pediatric Oncology Nursing 24(5):255–263.
van Deursen, A. J., and J. A. van Dijk. 2019. The first-level digital divide shifts from inequalities in physical access to inequalities in material access. New Media & Society 21(2):354–375.
Viswanath, K., K. D. Blake, H. I. Meissner, N. G. Saiontz, C. Mull, C. S. Freeman, B. Hesse, and R. T. Croyle. 2008. Occupational practices and the making of health news: A national survey of US health and medical science journalists. Journal of Health Communications 13(8):759–777.
WHO (World Health Organization). 2019. Cancer prevention. Geneva, Switzerland: World Health Organization. https://www.who.int/cancer/prevention/en (accessed August 21, 2019).
Willis, A., E. Reed, M. Pratt-Chapman, H. Kapp, E. Hatcher, V. Vaitones, S. Collins, J. Bires, and E. Washington. 2013. Development of a framework for patient navigation: Delineating roles across navigator types. Journal of Oncology Navigation and Survivorship 4(6):20–26.
Woloshin, S., L. M. Schwartz, S. L. Casella, A. T. Kennedy, and R. J. Larson. 2009. Press releases by academic medical centers: Not so academic? Annals of Internal Medicine 150(9):613–618.
Wright, A. A., B. Zhang, A. Ray, J. W. Mack, E. Trice, T. Balboni, S. L. Mitchell, V. A. Jackson, S. D. Block, P. K. Maciejewski, and H. G. Prigerson. 2008. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300(14):1665–1673.
Zafar, S. Y., F. Chino, P. A. Ubel, C. Rushing, G. Samsa, I. Altomare, J. Nicolla, D. Schrag, J. A. Tulsky, A. P. Abernethy, and J. M. Peppercorn. 2015. The utility of cost discussions between patients with cancer and oncologists. American Journal of Managed Care 21(9):607–615.


















































