2
The Process for Identifying Candidate Leading Health Indicators
At its April 19, 2019, public information-gathering virtual meeting with the Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2030 (SAC) co-chairs and the co-chairs of the objectives and data subcommittees, the National Academies committee learned that the SAC intended for the Leading Health Indicator (LHI) selection criteria to be applied to all of the Healthy People 2030 (HP2030) core objectives. The SAC developed two sets of criteria to be applied sequentially. In Phase 1, four criteria would be applied to rank the objectives (see Table 2-1). In Phase 2, the subset ranked highly in Phase 1 would undergo an iterative process of being assessed against four additional criteria for the set of LHIs. The iterative process would involve multiple considerations related to the Phase 2 criteria, which would mean that decision makers could add or remove some objectives from LHI consideration based on discussions about those considerations. In its report on the criteria for LHI selection, the National Academies committee recommended using the HP2030 Framework itself as Phase 0 in LHI selection (see Table 2-1).
The committee did not undertake a process that ranked each of the 355 draft core objectives for HP2030 on the LHI criteria. That is because the HP2030 objectives had not been finalized at the time the committee began its work and were not expected to be completed until much later. Thus, instead of obtaining a list of LHI candidates based on evaluating and rating each of the 355 draft core objectives, the committee used two approaches that integrated all LHI selection criteria (see Table 2-1) and the core objective selection criteria (see Box 2-1).
| Phase 0 (recommended in NASEM, 2019c; themes and subthemes drawn from the HP2030 Framework developed by the Secretary’s Advisory Committee) | Phase 1 (developed by the Secretary’s Advisory Committee) | Phase 2 (developed by the Secretary’s Advisory Committee; edited for brevity below) |
|---|---|---|
| Alignment with the HP2030 Framework: Themes and Subthemes (the description in Figure 1-1) |
Apply the following criteria to the individual LHI candidates:
|
Apply the following criteria to the set of LHIs:
|
Closing Gaps
|
||
Cultivating Healthier Environments
|
||
Increasing Knowledge and Action
|
||
Health and Well-Being Across the Lifespan
|
||
This chapter provides an overview of the process undertaken by the committee to review and weigh the available evidence to inform the selection of a set of candidate LHIs. The committee’s present work builds on the first report on criteria for LHI selection (see Box 2-2 for the report’s findings and recommendations).1
This report proposes LHIs—and where appropriate, new topics and objectives related to LHIs for which there were no extant draft core objectives—that reflect the intent of all components of the HP2030 Framework and criteria for core objective selection. It identifies areas where measures appropriate to serve as LHIs are available for making international comparisons. Lastly, it applies the LHI selection criteria described earlier.
The committee reviewed a large group of well-validated measure sets as described next. It then (1) drew on those existing sources to identify priority candidates for LHIs (i.e., the top-down procedure; see Chapter 3) and (2) applied a systematic approach to selecting from among the current draft core objectives by comparing them to the results of (1) (i.e., the bottom-up procedure, described in Chapter 4).
___________________
1 The entire report is available for free download at https://www.nap.edu/25531 (accessed August 20, 2019).
MEASUREMENT LITERATURE REVIEWED
To prepare for the procedure that would yield a list of LHI contenders, the committee reviewed compilation of indicators prepared by study staff that were drawn from more than a dozen well-known and validated sets, including several that focused specifically on measures of health equity, or rather, measures of the factors that influence health equity. A brief overview of reviewed sets is provided in Table 2-2; note that this overlaps
| Reference Sets of Indicators | ||||||
|---|---|---|---|---|---|---|
| Broad Topic or Domain for Which the Indicator Set Includes One or More Indicators | AHR | AHRQ Older Americans 2016 | BARHII | CDC Winnable Battles | CHR | HHS HP2020 |
| Length of Life | X | X | X | |||
| Quality of Life | X | X | X | |||
| Tobacco | X | X | X | X | X | |
| Nutrition, Physical Activity, Obesity | X | X | X | X | X | |
| Alcohol/Substance Use | X | X | X | X | ||
| Sexual Health | X | X | ||||
| Access to Care | X | X | X | X | X | |
| Quality of Care | X | X | X | X | ||
| Education | X | X | X | X | ||
| Employment | X | X | X | |||
| Income | X | X | X | X | ||
| Family/Social Support/Civic Engagement | X | X | X | |||
| Community Safety | X | X | X | X | X | |
| Environmental Quality | X | X | X | X | X | |
| Housing, Transit | X | X | X | |||
| Cost of Care/Medical Expenditures | X | |||||
NOTES: The entries in this table are updated from the prepublication version of this report to more accurately reflect the content of these resources.
AHR = America’s Health Rankings; AHRQ = Agency for Healthcare Research and Quality; BARHII = Bay Area Regional Health Inequities Indicators; CDC = Centers for Disease Control and Prevention; CHR = County Health Rankings; HHS HP2020 = Healthy People 2020
with but does not include all the measurement efforts presented at the May 28, 2019, information-gathering meeting (see agenda in Appendix B). The committee also reviewed measure sets or measurement efforts that focus primarily on tackling root causes of health disparities and advancing health equity, including the Bay Area Regional Health Inequities Indicators (BARHII), the HOPE Index, the National Equity Atlas, and the Prevention Institute Health Equity Indicators (BARHII, 2015; PolicyLink and USC PERE, 2018; Prevention Institute, 2015; Wong Croal et al., 2018).
| HUD Healthy Communities Index | IOM HP2020 | OECD Health at a Glance | OECD Social at a Glance | Prevention Institute Health Equity Indicators | IOM Vital Signs Report | WHO 100 Health Core | WIN |
|---|---|---|---|---|---|---|---|
| X | X | X | X | X | X | X | |
| X | X | X | X | X | X | X | |
| X | X | X | X | X | X | X | |
| X | X | X | X | X | X | ||
| X | X | X | X | X | X | X | |
| X | X | X | X | ||||
| X | X | X | X | X | X | ||
| X | X | X | X | X | |||
| X | X | X | X | ||||
| X | X | X | X | ||||
| X | X | X | X | X | |||
| X | X | X | X | X | |||
| X | X | X | X | X | X | ||
| X | X | X | X | X | |||
| X | X | X | X | ||||
| X | X | ||||||
LHIs; HUD HCI = Department of Housing and Urban Development Healthy Communities Index; IOM HP2020 = 2011 IOM report on the HP2020 Leading Health Indicators; OECD = Organisation for Economic Co-operation and Development; Vital Signs = 2015 IOM Vital Signs report; WHO 100 Core = World Health Organization 100 Core Measures; WIN = Well-being in the Nation.
In addition to the key sets of metrics already listed here, and the information presented at the May 2019 meeting, the committee also reviewed some of the literature on measurement of health equity and the factors that shape it, and on well-being—two concepts that are central to the HP2030 Framework.
CONSIDERATIONS RELATED TO HEALTH EQUITY
The committee’s thinking about measures to monitor equity was informed by the following list of Braveman’s criteria:
- Indicators “must meet standard scientific and ethical criteria” (e.g., quality data and local knowledge).
- “[D]ifferences in the indicators between better- and worse-off groups should be relatively likely to reflect avoidable, unfair gaps in important conditions that could be narrowed through policy changes in any sector that influences health and not just health care.”
- Appropriately disaggregated data “on the indicators is accessible for monitoring over time at the desired geographic level.”
- “[I]ndicators must occur frequently enough in the groups to be monitored to permit reliable estimates of differences between the groups.”
- [T]he range of indicators should include indicators of “health status, major determinants of health apart from health care, and key aspects of health care (e.g., financing, quality).” (Braveman, 1998, pp. 19–20)
The concept of health equity is related to health disparity and health differences. It is useful to briefly review these terms. Health differences refer to variations in rates of morbidity or mortality between two or more groups. There is no implication of any kind of causal reason for these variations. They are empirically observed differences. Health disparities, however, refer to health differences that are based on or originate in social disadvantages. A recent National Academies study defined health equity as “the state in which everyone has the opportunity to attain full health potential and no one is disadvantaged from achieving this potential because of social position or any other socially defined circumstance” (NASEM, 2017, p. 1). Braveman and colleagues offer the following definition that elaborates on socially defined circumstances:
Health equity means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerless-
ness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care. (Braveman et al., 2017, p. 2)
“[Ac]hieve health equity” is both part of a foundational principle and one of the five overarching goals of the HP2030 Framework.2 Moreover, the framework’s first foundational principle is “Health and well-being of all people and communities are essential to a thriving, equitable society.” The committee interprets this framing (i.e., “all people and communities,” and “equitable society”) as reflecting a concern with the conditions that ensure “fair and just opportunity to be as healthy as possible” (Braveman et al., 2017). This suggests the importance not only of monitoring health data disaggregated by different demographic groups but also of monitoring the social and structural inequities that affect health.
The committee notes that the literature contains roughly four broad categories of measures relevant to health equity:
- Traditional measures of health outcomes and health states (e.g., infant mortality rate, prevalence of diabetes) that are simply disaggregated by race, ethnicity, or other subpopulation; these shed light on disparities in health status and outcomes, but do not reveal causal pathways related to fairness or justice.
- Measures of disparities in health care (e.g., colorectal screening, diagnosis, survival) that reveal some of the structural and systemic factors that shape the delivery, access, quality, and other aspects of care that contribute to unjustly disparate health outcomes (IOM, 2003; Mays et al., 2007).
- Measures drawn from other sectors that shed light on factors that shape health outcomes (e.g., housing cost burden, access to transit or miles driven alone).
- Measures that may themselves be shaped by underlying structural social inequities (e.g., segregation, redlining, unfair lending practices, bias in hiring), assessed by such measures as the Everyday Discrimination Scale and the Index of Dissimilarity (Shah et al., 2014).3
___________________
2 See https://www.healthypeople.gov/2020/About-Healthy-People/DevelopmentHealthy-People-2030/Framework (accessed February 12, 2019).
3 For example, see the Boston Behavioral Risk Factor Surveillance System measure of “residence in public housing, subsidized housing, or neither” as a measure of inequities in the conditions that shape health and well-being, specifically, exposures to asthma triggers (see Shah et al., 2014). To compensate for the fact that the BRFSS sample “lacks power to conduct subgroup analyses in smaller neighborhoods,” the Boston Public Health Commission “generates neighborhood and subgroup estimates by combining survey data from several years” (Shah et al., 2014, p. 2).
The committee noted that the first category—disaggregating key health indicators by race, ethnicity, and other demographics—has historically been a part of the Healthy People objectives and LHIs, but the committee agreed that in addition to continuing to providing disaggregated data for each LHI, the more robust focus on health equity reflected in the HP2030 Framework requires the addition of measures more explicitly linked with social equity and the creation of social, environmental, and economic conditions required for equitable health outcomes.
CONSIDERATIONS RELATED TO THE CONCEPT OF WELL-BEING
The World Health Organization (WHO) discusses well-being as existing “in two dimensions, subjective and objective. It comprises an individual’s experience of their life as well as a comparison of life circumstances with social norms and values” (WHO, 2012). Well-being and health are seen as interactive concepts whereby health influences overall well-being, and wellbeing affects future health (WHO, 2012). The well-being construct was first introduced in the Healthy People initiative as part of HP2020, in the goal “Improve health-related quality of life and well-being for all individuals” (HealthyPeople.gov, 2019). The HP2020 website states the following:
Promoting well-being emphasizes a person’s physical, mental, and social resources and enhances protective factors and conditions that foster health. Instead of the traditional view of prevention as only avoiding or minimizing illness and risk factors, well-being also focuses on disease resistance, resilience, and self-management.
The SAC expanded the definition of well-being beyond the individual to acknowledge that it is an attribute of communities or society more broadly, and is shaped by a wide array of factors. The SAC’s brief on “health and well-being” described the concept of well-being “as both a determinant and an outcome of health and reflects aspects of life that include physical, mental, emotional, social, financial, occupational, intellectual, and spiritual” factors (SAC, 2018b). The SAC further notes that health and well-being are mutually reinforcing, and importantly for communication and for appealing to stakeholders in other sectors, it asserts that well-being may be a “more motivating and unifying pursuit” than health (SAC, 2018b). The brief proposes that in the context of HP2030, “health and well-being can be defined as how people think, feel, and function” and also that there are “reciprocal influences between individual and societal health and well-being.”
The Centers for Disease Control and Prevention (CDC) provides additional extensive discussion of well-being as part of its Health Related
Quality of Life (HRQOL) program. CDC describes measurement of well-being as including one’s view of one’s living conditions, “global judgments of life satisfaction from depression to joy,” and “judging life positively and feeling good” (CDC, 2018).
The committee reviewed the draft core objectives for a measure of well-being, and finding none, it endeavored to identify and vet at least one to propose as an LHI. The committee has recommended a measure that is aligned with international measurement efforts (see below).
FIVE STEPS TO SELECT CANDIDATE LEADING HEALTH INDICATORS
Overview
The committee undertook two separate approaches resulting in five total steps in its effort to identify a slate of LHI candidates to recommend to the Department of Health and Human Services (HHS) (see Figure 2-1).
The terms top-down and bottom-up are intended to reflect the committee’s consideration about the combination of approaches needed to identify a good working list of LHI candidates. “Top-down” refers to
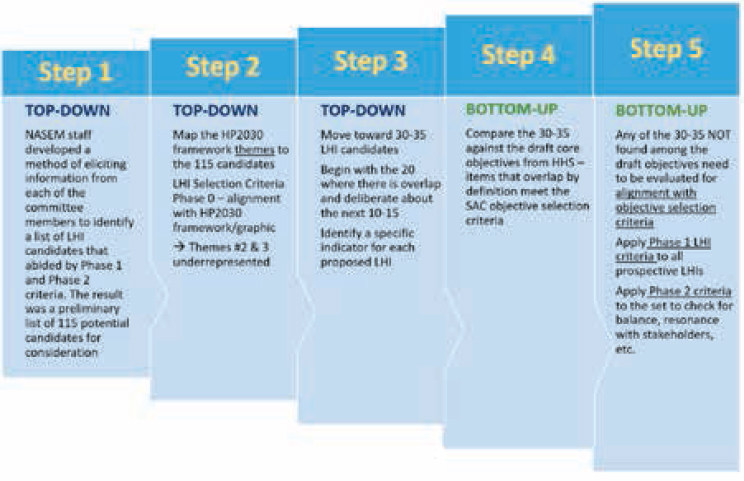
bringing the committee’s combined expertise and judgment to bear on the selection of candidate LHIs, and “bottom-up” refers to the work of comparing the large number of existing draft HP2030 core objectives to the results of the top-down process to help identify LHI candidates. This step helped identify areas of overlap and gaps. The committee applied the objective selection criteria to committee-proposed LHI candidates not found on the HHS list of draft objectives to ensure that proposed measures qualified (see Box 2-1 for the objective selection criteria). Additionally, the final slate recommended to HHS would also need to adhere to the three categories of LHI selection criteria discussed in the first report (see Table 2-1). The committee also noted the importance of finding LHI measures useful to deploy at the state and local level, and LHI measures useful for making international comparisons.
The Top-Down Procedure
Committee members developed a list of potential indicators derived from more than a dozen sets of health metrics (see Table 2-2) that they identified as relevant to achieving the goal of selecting LHIs for HP2030. Using the curated list of resources as their primary reference, members were asked to identify candidates for consideration through the three-step top-down procedure (see Figure 2-1): (1) eliciting a set of 15 preferred priority indicators from each individual committee member; (2) mapping the resulting 115 candidates to the themes in the HP2030 Framework graphic; and (3) narrowing down the list of LHI candidates to 34—through a consensus process.
The Bottom-Up Procedure
There were roughly two steps for the bottom-up procedure: (1) approximately comparing the candidates resulting from the top-down procedure against the draft core objectives provided by HHS, and (2) applying the objective selection criteria to any items that were not found among current core objectives.
Reviewing the Evidence for Proposed LHIs
The committee considered the evidence for potential LHIs (and the objectives associated with them) at multiple points during the process. Evidence base is one of the criteria for selecting core objectives (see Box 2-1), and it specifies that the objective should have “a known evidence base, and identified evidence-based interventions to improve outcomes.” The criterion calls for applying the evidence rating
scale developed for HP2020: rigorous (4), strong (3), moderate (2), and weak (1).4 Level 4 evidence is described as emerging from recommendations of the U.S. Preventive Services Task Force, the Community Preventive Services Task Force, or systematic reviews published in peer-reviewed journals. Level 3, or “strong” evidence, rests on nonsystematic reviews published by the federal government and nonsystematic reviews published in peer-reviewed journals. Level 2, seen as “moderate” evidence, emerges from journal articles of individual studies, published intervention research, and published pilot studies. Level 1, regarded as “weak,” lists intervention evaluations or “studies without peer review that have evidence of effectiveness, feasibility, reach, sustainability, and transferability” (HHS, n.d.).
The committee recognizes the tension inherent in broadening the framework of considerations of health and well-being at the same time that HP2030 seeks to promote and adhere to high standards of evidence for intervention effectiveness. Measuring well-being implies drawing from a wider range of indicators, including some from outside the health sector, hence the potential for a wider range of types of interventions and evidence. It is the committee’s view that in seeking LHIs that best represent high-level priorities for the nation, it will be important to maintain accommodation of levels of evidence appropriate to the domain, time frame, and type of intervention with respect to what constitutes evidence adequacy when drawing from work conducted in other sectors. This view resonates with the HP2020 publication Evidence-Based Clinical and Public Health: Generating and Applying the Evidence, which discusses the “limitations of the traditional hierarchy of evidence” and “the need for contextual information” (SAC, 2010, p. 11).
The evidence associated with potential LHIs is as varied as the LHIs themselves: some imply health care system interventions (e.g., contraceptives, HIV), others require “connecting the dots” to health outcomes (e.g., fourth grade reading proficiency), and others are endpoints to multiple pathways for intervention (e.g., life expectancy, infant mortality). This reality calls for articulating a different, broader, mental model for the relationship between LHIs and their evidence. LHIs are intended to move the dialogue and galvanize action by stakeholders; therefore, some indicators may not be supported by evidence that meets the criteria for “rigorous,” but the perfect ought not to be the enemy of the good—less than perfect evidence may be warranted when there is a highly compelling reason to track a certain LHI. Moreover, the HP2030 effort centers well-being along with health and health equity, but markers of
___________________
4 See HHS, n.d., or https://www.healthypeople.gov/2020/tools-resources/Evidence-Based-Resources (accessed May 5, 2019).
well-being do not necessarily have the same links to an evidence base that health measures do. The LHIs the committee proposes are supported either by evidence that specific interventions will improve outcomes or by evidence that the LHI is itself a marker of better health or well-being.














