Proceedings of a Workshop
INTRODUCTION1
Behavioral health and substance use disorders (SUDs) affect approximately 20 percent of the U.S. population (NIMH, 2017). Of those with an SUD, approximately 60 percent also have a mental health disorder (Center for Behavioral Health Statistics and Quality, 2015). Together, these disorders account for a substantial burden of disability, have been associated with an increased risk of morbidity and mortality from other chronic illnesses, and can be risk factors for incarceration, homelessness, and death by suicide. In addition, they can compromise a person’s ability to seek out and afford health care and adhere to treatment recommendations (Roberts et al., 2015; WHO, 2015).
Despite the high rates of comorbidity of physical and behavioral health conditions (which include mental health and substance-related and addictive disorders) integrating services for these conditions into the American health care system has proved challenging. Part of the explanation lies in a historical legacy of discrimination and stigma that made people reluctant to seek help and also led to segregated and inhumane services for those suffering from mental health or substance use disorders (Storholm et al., 2017). Health
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop was prepared by the rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
insurance programs also often provided limited coverage of services for these disorders compared to services for other conditions (Storholm et al., 2017).
Individuals with mental health conditions face numerous barriers to receiving quality care: in 2018, only 43.3 percent of U.S. adults with mental illness received treatment (NAMI, 2019). Research has found that the most common reason for not seeking care is an inability to pay for services (Novak et al., 2019). In addition, fear of discrimination in housing, employment, military service, and other arenas can deter people from seeking or continuing care (Mojtabai et al., 2014). Nearly 90 million Americans live in areas with a shortage of mental health professionals, a situation exacerbated by a lack of adequate training (AAPA, 2016). Additionally, many professionals do not have the support to identify mental health and substance use disorders (MHSUDs) and then appropriately manage care through direct services, referral, and collaboration (AAPA, 2016). Often, evidence-based psychosocial interventions are not available as a part of routine clinical care due to issues related to access to quality care, workforce training, insurance coverage, or fragmentation of care (Priester et al., 2016).
To provide a structured environment and neutral venue to discuss data, policies, practices, and systems that affect the diagnosis and provision of care for MHSUDs, the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine (the National Academies) created the Forum on Mental Health and Substance Use Disorders. The forum activities are expected to advance the discussion and generate potential ideas on ways to address many of the most persistent problems in delivering mental health and substance use services. The inaugural workshop, held October 15–16, 2019, in Washington, DC, explored the key policy challenges and opportunities that impede efforts to improve care for those individuals with MHSUDs.
The first session set the stage for the ensuing discussions by acknowledging the critical importance of person-centered care, shared decision making, and patient and family engagement in treating MHSUDs. The second session focused on identifying essential components of care for people with MHSUDs. During lunch, participants engaged in group discussions on the topics of the first two sessions. Building on those discussions, the third session examined opportunities to translate knowledge into practice and monitor implementation of evidence-based practices. The workshop’s first day concluded with a brief summary of the luncheon discussions and lessons learned and key messages from the session presentations.
The second day began with a session exploring ways in which data can be leveraged to improve care delivery and patient outcomes for people with MHSUDs. The final session examined the challenges and opportunities related to developing the workforce to provide high-quality care for MHSUDs. Each
of the five sessions included a discussion period in which audience participants could pose questions to the speakers.
This Proceedings of a Workshop summarizes the presentations and discussions. A broad range of views was presented. Box 1 provides a summary of suggestions for potential actions from individual workshop participants. The workshop agenda and Statement of Task are in Appendixes A and B, respectively. The speakers’ presentations (as a PDF and video files) are archived online.2
PROMOTING PERSON-CENTERED CARE, SHARED DECISION MAKING, AND PATIENT AND FAMILY ENGAGEMENT
The workshop opened with Michael Weaver, the executive director of the International Association of Peer Supporters, welcoming the workshop participants. Weaver explained that the first session would set the stage by focusing on the importance of promoting person-centered care, patient and family engagement, and shared decision making.
Flipping the Script: Advancing Patient-Centered Care and Supported Decision Making
Keris Jän Myrick, the chief of peer services at the Los Angeles County Department of Mental Health, began the session by pointing out that the focus of mental health care tends to be on the mental illness and reducing symptoms, rather than the various aspects of patients’ lives that those symptoms disrupt. What would happen, she asked, if that script was flipped and mental health care was delivered in the context of wellness, well-being, and an individual’s meaningful roles in life rather than using illness as the care model target? Myrick encountered one example of that flipped script in Trieste, Italy, where mental health centers are open 24 hours per day and the emphasis is on keeping people connected with their community, family, friends, social activities, and meaning and purpose (Mezzina, 2014). “All of these things they are able to carry out because of their deep investment in their values and principles,” she said.
Those values and principles translate into warmly welcoming everyone who comes through the doors of the mental health center and “meeting people where they are” with regard to their mental health status. The health centers’ care model focuses on inclusion, participation in the community, and helping
___________________
2 For additional information, see http://www.nationalacademies.org/hmd/Activities/MentalHealth/MentalHealthSubstanceUseDisorderForum/2019-OCT-15.aspx (accessed January 14, 2020).
people to stay in their homes even when they are in crisis. Staff, she noted, work hard at building resilience in the context of relationship, community, and meaning and purpose in life.
Myrick added that an important aspect of “flipping the script” is to tap into the power of peer support for both individuals receiving care and their parents, family, and other caregivers. Myrick noted that the Substance Abuse and Mental Health Services Administration (SAMHSA) has produced several briefs that discuss peer support as part of mental health and substance use care.3 She also pointed out that the National Alliance on Mental Illness
___________________
3 SAMHSA’s peer support briefs are available at https://www.samhsa.gov/brss-tacs/recovery-support-tools/peers (accessed November 1, 2019).
(NAMI) has created a guidebook for mental health caregivers to help them understand what they can do on their own and who in the mental health care system should provide specific aspects of care.4
Returning to the earlier example of the health center in Trieste, Myrick explained that mental health and substance use care relies on supported decision making, in contrast to shared decision making, with the individuals seeking care identifying the supporters who will help them in their decision making. This approach to care maximizes an individual’s autonomy, explained Myrick. She noted that the American Bar Association developed a guide to help individuals, families, and lawyers determine how to best provide supported decision making. The PRACTICAL Toolkit (ABA, 2016) states the following:
- Presume guardianship is not needed
- Reason: Clearly identify the reasons for concern
- Ask if a triggering concern may be caused by temporary or reversible conditions
- Community: Determine if concerns can be addressed by connecting the person to family or community resources
- Team: Ask the person if they already have a team to help make decisions
- Identify abilities: Identify areas of strengths and limitations in decision making
- Challenges: Screen for and address any potential challenges presented by supporters
- Appoint a legal supporter or surrogate consistent with the person’s values and preferences
- Limit any guardianship petition or order to only what is necessary
In addition, Temple University’s Collaborative on Community Inclusion developed tools to help people think about self-directed care, which is another way to increase autonomy. “The more one feels empowered and in charge of their care or their support or whatever their needs are in their life, the more able they are to be fully engaged in the community,” said Myrick. She noted that self-directed care is starting to make inroads in mental health care in the United States, though she was not sure if the same was true for substance use care. In Myrick’s opinion, this allows us to examine how we fund care and do so in a way that maximizes people’s autonomy.
___________________
4 The NAMI guidebook is available at https://www.nami.org/About-NAMI/Publications-Reports/Guides/Circle-of-Care-Guidebook/CircleOfCareReport.pdf?utm_source=direct&utm_campaign=circleofcare (accessed November 1, 2019).
In closing, Myrick said that flipping the script and truly innovating will require doing things differently, which will include thinking about how to provide care from a humanistic view and considering the values, culture, language, and principles of the individual needing care.
Trauma-Informed Care and the Ryan White Model of Delivery
Building on the opening discussion of supportive care, Edward Machtinger, the director of the Center to Advance Trauma-Informed Health Care and Women’s HIV Program at the University of California, San Francisco (UCSF), explained that trauma-informed health care5 is a powerful and essential tool to effectively address MHSUDs. “Understanding the impact of trauma on health demystifies why so many patients struggle with substance use and mental illness in the first place and why these conditions are often so refractory to supposedly effective therapies. This understanding explains why some patients can seem chaotic, defensive, or demanding,” he added. Understanding the impact of trauma can also explain why the experiences of health care providers and systems of care can often mirror patients’ trauma experiences.
Trauma-informed care, explained Machtinger, has three tenets. The first tenet states that the occurrence of substance use and mental illness correlates strongly with individual, family, and community-level trauma. Trauma is defined as an event, series of events, or set of circumstances that are experienced by an individual as physically or emotionally harmful or threatening and that have lasting adverse effects. The impact of trauma on adult health and well-being, he noted, is well documented and startling. The Adverse Childhood Experiences (ACEs) study,6 for example, found that high rates of ACEs were strong predictors in a dose-dependent manner of the major causes of adult morbidity, mortality, and disability (Felitti et al., 1998). Individuals who reported four or more ACE categories had 1.6 times the rate of obesity compared to those with no ACEs, as well as more than 2 times the rate of smoking, 3 times the rate of depression, 6 times the rate of attempting suicide, 7 times the rate of alcoholism, and 10 times the rate of intravenous drug use (Felitti et al., 1998). Similarly, adult trauma and the consequences of trauma, such as posttraumatic stress disorder (PTSD), have also been shown to have dose-dependent relationships with many of the same conditions. The Philadelphia Urban ACE study looked at the additive impact of community-level traumas by assessing the impact of five types of community-level adverse
___________________
5 For more information, see https://www.traumainformedcare.chcs.org (accessed February 7, 2020).
6 For more information, see https://www.ajpmonline.org/article/S0749-3797(98)00017-8/abstract (accessed December 2, 2019).
events, such as experiencing racism, experiencing bullying, witnessing violence, being in foster care, and living in an unsafe neighborhood (Cronholm et al., 2015; Wade et al., 2016). Individuals who experienced three or more of these community-level traumas in childhood were more than twice as likely as those with no community-level ACEs to smoke as an adult and to be depressed, three times more likely to have a substance use problem, and four times as likely to have a sexually transmitted disease. ACEs are not the sole driver of substance use and mental illness; “nonetheless, to understand and effectively treat substance use disorder and mental illness, I have found it incredibly helpful to see these conditions, like HIV, as primarily a symptom of a much larger and more insidious reality of individual, family, and community-level trauma,” said Machtinger.
Machtinger explained that the second tenet of trauma-informed health care is that while trauma makes people more vulnerable to substance use and mental illness, it also acts as an obstacle to effective treatment of those same conditions. The evidence for this tenet is strongest in co-occurring SUD and PTSD, which is associated with poorer recruitment and retention in treatment programs, treatment outcomes, and treatment adherence, and shorter periods of abstinence post-treatment compared to SUD alone (Roberts et al., 2015).
The third tenet is that clinics and environments of care often mirror the trauma experienced by patients. For example, staff and health care providers often feel overwhelmed and unsupported, and as a result, they can sometimes be dismissive and rigid with patients. In turn, patients who have a history of being coerced by an intimate partner or experiencing discrimination or incarceration often feel unwelcome or unsafe in such situations, said Machtinger. “In this way, our clinics can actually be trauma-inducing for patients, pushing them away from the care that they so desperately need,” said Machtinger. These trauma-inducing environments can also contribute to burnout among staff and health care providers, many of whom have histories of trauma themselves. “For us to sustain a movement of healing for substance use disorder and mental illness, we have to take this burnout seriously and adopt trauma-informed practices that support team-based care, reflective supervision, and self-care,” he noted.
Ultimately, understanding the impact of trauma on health and behavior helps health care clinicians be more patient and compassionate and enables them to form trusting connections with patients that are foundational for effective care of people with MHSUDs. “It is from that foundation of a trusting connection that we can provide or link patients to the care that they want and need,” said Machtinger. To be successful in helping individuals with MHSUDs, Machtinger stressed that there needs to be a delivery platform for trauma-informed care that facilitates integrated, interdisciplinary primary and behavioral health care, as well as partnerships with peers and community organizations that support self-care and access to specialty care.
According to Machtinger, the national Ryan White HIV/AIDS Program,7 administered by the Health Resources and Services Administration (HRSA), has been uniquely effective at creating exactly that type of platform for delivering care to individuals with HIV/AIDS. “It is a model that we should all know about and build upon to be successful in overcoming our country’s opioid epidemic and to effectively address other forms of substance use disorder and mental illness,” he said. Machtinger encouraged the use of examples of effective care to guide the development of care delivery approaches for people with MHSUDs. He cautioned that not doing so risks setting the bar for success too low and thus adapting to a health care system that is profoundly insufficient for the needs of patients.
As an example of what effective care can look like in the context of MHSUDs, Machtinger told the story of Pebbles, a 42-year-old woman who had recently entered a residential treatment program for heroin and crack cocaine use and been referred to the UCSF clinic for primary medical care (see Box 2).
Machtinger said the reason he and the clinic staff were able to deliver what was ultimately effective care comes down to three components: (1) the values that guide the clinic staff, (2) provider-level interventions over which staff have some control, and (3) systems-level interventions that required structural change (see Table 1).
The values that informed Pebbles’s care—and that enabled her to stay engaged despite her shame for her drug use and endangering her grandchild—are aligned with the six core values of trauma-informed care, which begins with safety. “She did not think we were going to punish her or stop loving her because of her behavior,” said Machtinger. The next value, trustworthiness and transparency, allowed her to share her feelings and fears. The value of collaboration minimized power differentials between her and clinic staff. Peer support was provided by individuals with shared experiences and she was empowered to recognize her inner strength and resiliency. Lastly, clinic staff had been trained in the value of cultural humility and responsiveness to implicit biases and the realities of historical and intergenerational trauma.
Machtinger explained how UCSF has gone through a deliberate 2-year process to become a trauma-informed clinic. He noted that in terms of clinician-level interventions, “all of our staff and providers understand the impact of trauma on health and behavior.” In addition, all health care providers must be waiver eligible to prescribe buprenorphine and understand that it is imperative to screen for other co-occurring SUDs and mental health conditions. Staff also received training to employ motivational interviewing to help patients achieve their individual goals.
___________________
7 Additional information is available at https://hab.hrsa.gov/about-ryan-white-hivaids-program/about-ryan-white-hivaids-program (accessed November 8, 2019).
TABLE 1 The Characteristics of Effective Trauma-Informed Care
| Values | Provider-Level Interventions | Systems-Level Interventions |
|---|---|---|
| Safety | Understand impact of trauma on health | Interdisciplinary team-based care |
| Trustworthiness and transparency | See most substance use as self-medication | Peers and community/peer organizations integrated into care |
| Collaboration | Compassion, patient | 30–45-minute visit lengths; long-term relationships |
| Peer support | Prescribe buprenorphine | Integrated behavioral health services (e.g., groups, medication-assisted treatment) |
| Empowerment | Screen and refer for other addictions and mental illness | Partner agencies in community |
| Cultural humility and responsiveness | Motivational interviewing | Leadership support and funding for comprehensive care |
SOURCE: As presented by Edward Machtinger, October 15, 2019.
In terms of systems-level interventions, one crucial factor in the clinic’s success with individuals like Pebbles is that it exists within the larger Ryan White HIV/AIDS care system, Machtinger explained. That system requires and funds the clinic to provide interdisciplinary team-based care that allowed Machtinger, along with the clinic’s social worker, therapist, and medication-assisted treatment (MAT) counselor, to provide care to Pebbles. Other systems-level interventions include
- integrating peers and community/peer organizations into care;
- enabling longer clinic visits and long-term relationships that facilitate trust;
- integrating behavioral health services, including a MAT program and group therapy for trauma and substance use, into primary care;
- establishing partnerships with community-informed residential treatment centers; and
- providing leadership and funding to facilitate this model of care.
Machtinger credits SAMHSA with taking the lead on trauma-informed care nationally and shared that he finds it inspirational that a federal agency can drive an entirely new field. SAMHSA has developed practical guidance for trauma-informed health care in terms of “four Rs,” which states that trauma-informed care
- Realizes the widespread impact of trauma and understands effective paths for recovery;
- Recognizes signs and symptoms of trauma in clients, families, staff, and others involved;
- Responds by integrating understanding and response to trauma in interactions, care, and policy; and
- Seeks to actively resist re-traumatization.
SAMHSA, UCSF, and others have produced models and toolkits to help guide the establishment of trauma-informed practices and clinics (see Figure 1), and the field is now trying to understand how to best package the interventions for which there is evidence supporting their effectiveness.
Machtinger noted that before the Ryan White model of HIV care emerged in the 1990s, the U.S. health care system was struggling with the ongoing AIDS epidemic. Early AIDS patients, as with most people with SUD and mental illness, were from highly marginalized populations, and they faced a stigmatizing and often uniformly fatal illness. At the time, clinicians did not have the expertise or tools to effectively fix the problem in front of them. Most care, explained Machtinger, was provided in hospitals at the end
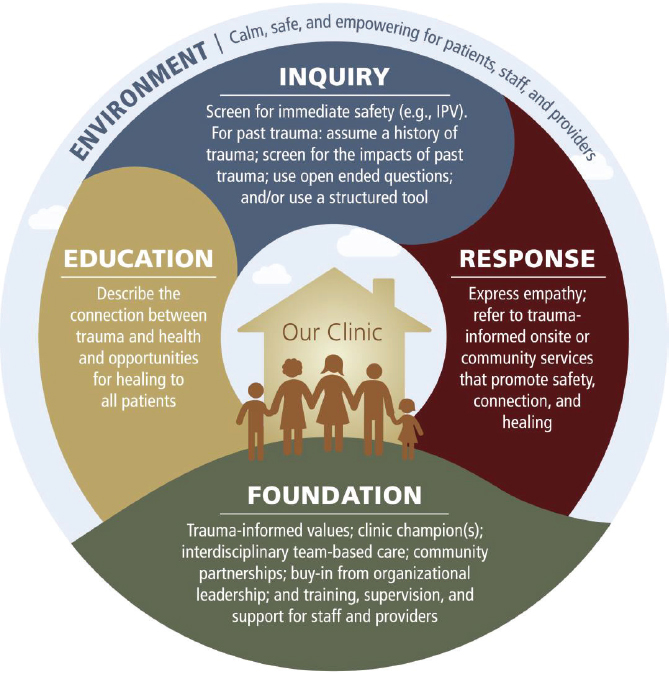
NOTE: IPV = interpersonal violence.
SOURCES: As presented by Edward Machtinger, October 15, 2019; Machtinger et al., 2019.
of life, and there was limited understanding of how to integrate HIV care into primary care.
The Ryan White Care System8 currently serves more than half of the people diagnosed with HIV/AIDS, or almost 600,000 people, and after 30 years of operation, it has become the nation’s safety net for people living with HIV. “The revolutionary power of Ryan White comes from how it funds outpatient treatment and care,” said Machtinger. “It specifically supports
___________________
8 For more information, see https://hab.hrsa.gov/about-ryan-white-hivaids-program/about-ryan-white-hivaids-program (accessed December 4, 2019).
integrated team-based primary care with an emphasis on wraparound services, such as social work, case management, therapy, and medication adherence.” This system requires clinics to integrate individuals living with HIV into the decision-making process for how care services are delivered and drives the integration of community-based organizations (CBOs) and peers into onsite care delivery through a structure of shared funding between CBOs and primary care clinics. “Despite Ryan White serving predominantly low-income patients, it has far better outcomes than clinics that have private insurance,” he noted. Machtinger estimated that if this model were extrapolated to the opioid epidemic, it would cost about $100 billion over 10 years, which he said is a fraction of what the opioid epidemic is costing the nation.9
In closing, Machtinger pointed out that trauma-informed care provides values and provider-level guidance, while the Ryan White model provides the crucial systems-level platform. “The combination of this platform and these values is necessary and possible for addressing our substance use epidemic,” said Machtinger. As a warning, he implored the workshop participants to be wary of being “mesmerized by purely biomedical solutions to problems that are fundamentally relational. The Ryan White system of AIDS care was at its best when new, effective biomedical treatments were integrated into a system that saw people as people and did everything they could to help them survive,” he said. “That combination was the best care this country has ever provided, and we have a rare opportunity right now to realize that model of care for substance use and mental illness,” concluded Machtinger.
Creating Hope Through Person-Directed Care, Decision Negotiation, and Collaboration
Lisa St. George, the director of recovery practices at RI International, finds that she works in a field full of hope and possibility—an attitude that she tries to inspire in the people that she and her colleagues serve. “It is of such importance that the people that we work with know and understand that everything can change for them,” said St. George. While acknowledging that every person will have a unique journey of recovery, she pointed out that every single person has the possibility of achieving a full recovery.
Recovery, explained St. George, does not mean people will never have a symptom of their illness again, that they no longer need to take medication if they have a mental health challenge, or that they will not battle addiction every day of their lives. Rather, recovery means that they do all of those things
___________________
9 A 2017 study estimated that the opioid epidemic is costing the United States more than $500 billion per year (Council of Economic Advisors, 2017).
while living a full and complete life. She noted that many health care clinicians believe they do not know how to inspire hope, but in her opinion, that does not take much training or a massive change to the way they work. She added that inspiring hope requires looking through the lens of what is possible for people rather than what is not possible. That change in focus can inspire hope even when people are struggling in their worst moments, stated St. George.
In the past, hospitals had limited visiting hours that had the effect of isolating patients from their loved ones and friends—the very behavior that those in recovery are asked to avoid. “We want people to be among those that give them comfort and support,” said St. George. In the same way, patients were often told what to do rather than being asked to be full participants in planning their care. “Person-centered care does not occur if the individual is not present,” St. George noted. Nor does it occur, she added, if the individual does not have an equal voice among all those who are involved in formulating and carrying out a care plan.
According to St. George, the key to achieving true person-centered care is collaboration through negotiation, which involves three key components:
- Identifying negotiation and collaboration guidelines,
- Assuming that all partners on a care team—including the individual—have valuable and valid knowledge, and
- Ensuring that all voices are heard and respected.
Compromises and trial runs are an acceptable part of the collaborative care through negotiation process, St. George noted, but everyone must stay in the discussion even in difficult areas where reaching an agreement may be a challenge. In addition, when the individual being served wants to do something different than what the rest of the team wants, that individual should still receive support.
St. George explained that within the context of the collaborative care negotiation team, everyone takes strategic risks and individuals and team members grow to trust one another. When a person is a full participant in their care planning, everyone ends up sharing the weight of the resulting plan, and when a person makes choices about what they want, they gain self-confidence. This self-confidence, in turn, moves people toward their strengths and away from helplessness and helps them realize they are effective decision makers and that they can learn from errors. The end result is that people stay engaged and invested in their well-being. Peer supporters are trained to work in this self-directed, self-guided, and negotiated manner. “They work that way because they are perfectly equal with the people that they are serving, and they work from a knowledge base of ‘I have been through that and I understand what you are going through,’” she said. Peer supporters, she explained, do not direct
the work that people do with them, and they support thoughtful risk when people want to try something new.
St. George shared that 100 percent of the individuals served by RI International’s peer transition teams report that they are satisfied with the process and outcomes they achieve. In addition, the RI International peer transition teams program has demonstrated the ability to reduce both the number of people hospitalized (from 159 to 30) and the number of times an individual requires hospitalization (from 202 to 40) (Optum, 2015). St. George noted that one health system has seen a 58 percent increase in individuals served over a 5-year period by a program that includes peer support, resulting in a 32 percent reduction in hospitalizations and $12.1 million in cumulative savings over those 5 years (Optum, 2015). This program also led to a 33 percent reduction in Involuntary Treatment Act admissions, an additional $10.3 million in savings, and a 32 percent reduction in 30-day readmission rates and $1.1 million in cumulative savings over the 5-year period (Optum, 2015).
Discussion
In the discussion session following the speaker presentations, Kenneth Stoller from Johns Hopkins University asked St. George to reflect on the possibility that patients’ lack of hope might result from clinicians not appreciating how people can improve if granted access to comprehensive treatment, which could include trauma-informed care. She replied that a big part of the problem is that most patients see their primary care physician, who has 15 minutes to assess what they need and will likely miss a large piece of what is happening. In St. George’s view, this is why community treatment is important, as it creates the opportunity for health care providers and peer supporters, for example, to spend more time with people and come to understand what the patient truly needs in order to fully engage with their treatment.
Stoller also asked Machtinger if trauma-informed care can be packaged for office-based practices providing primary care. Machtinger said this was indeed possible and noted that SAMHSA has published federal guidance for delivering trauma-informed care in behavioral health settings. In addition, he noted, there has been a national effort to publish guidance for trauma-informed primary care that should result in the National Council for Behavioral Health doing so.10 This latter guide and accompanying materials can serve as a prescriptive toolkit to help clinics transition from trauma-inducing environments to trauma-responsive environments, Machtinger explained.
___________________
10 Additional information is available at https://www.thenationalcouncil.org/consulting-areas-of-expertise/trauma-informed-primary-care (accessed November 11, 2019).
Andrew Pomerantz, the national mental health director for integrated services in the U.S. Department of Veterans Affairs (VA) Office of Mental Health and Suicide Prevention and an associate professor of psychiatry at the Geisel School of Medicine at Dartmouth asked the panelists if they had seen any of the cost savings resulting from delivering trauma-informed and recovery-oriented care reinvested in expanding that type of care. St. George replied that she would like to think that those who invest in funding that type of care would reinvest that way, but in truth, she has no idea what funders do with those savings. “Investing that money back into the system of care, into peer support, and into recovery-focused services is vital to make those savings be of use to us rather than going into funders’ pockets,” said St. George.
Machtinger added that cost savings in medicine are unequally distributed, so increased spending for primary care and behavioral health, for example, will translate into savings from lower emergency department (ED) use and fewer hospital admissions. At the same time, he said, primary care and behavioral health are often held accountable for increased spending without considering the broader cost savings created by increased expenditures in both sectors. “That is why I feel so strongly that we need to have a more structured national response to substance use and mental illness that really looks at this holistically and does not rely on innumerable valiant but fragmented efforts throughout the country to accomplish what we really see as shared goals,” he said. The only place that he sees such a holistic approach in action is in the VA.
Myrick referenced legislation proposed in California that would have approved a process for peer providers to be state certified. Though peer certification has been shown to provide a return on investment in the form of reduced hospitalizations, longer tenure in the community, and people being able to leave the public support system and return to work, the concern was the cost of setting up the program. The governor ultimately vetoed the bill. As someone with a business background, Myrick said she was interested in how best to argue for supporting these programs that demonstrate value and savings.
Tisha Wiley from the National Institute on Drug Abuse noted that each of the speakers had stressed the importance of building on family relationships to support a family member’s recovery, which for her raised the question of how the panelists manage some of the tensions inherent in providing patient-centered care and supporting families that have also suffered traumas created by their family member’s drug use. For example, Pebbles’s grandchild experienced several traumas and likely requires support and care related to her own individual traumas. Machtinger replied that the most troubling aspect of Pebbles’s case was that Pebbles, whom everyone loved, had hurt Lily through her behavior. “The single most important thing we can do to help protect children from abuse is to take care of their mothers and fathers, help them
to end their drug use, help them not die, help them stay out of prison,” said Machtinger.
Karen Drexler from the VA asked Machtinger if he and his team considered contingency management,11 also called “motivational incentives,” as a treatment for Pebbles’s drug use to reinforce abstinence and engage her quickly and effectively. Such incentives, Drexler explained, are typically delivered as a reward for negative urine tests. Machtinger said he and his team use contingency management informally with a gift card program to incentivize actions that help patients survive, such as going to get needed care. He added, however, that he intended to learn more about this approach as a potential tool for his program.
IDENTIFYING ESSENTIAL COMPONENTS OF CARE BY DEFINING WHAT MINIMALLY ADEQUATE CARE WOULD BE ACROSS DIVERSE CARE SETTINGS
Susan Essock, the Edna L. Edison Professor of Psychiatry, Emerita, at Columbia University, stated the charge for the second session: given that research has outlined what the optimal interventions are for MHSUDs, the panelists were asked to identify the essential components of care for different disorders and ways to monitor whether effective care is being provided.
The Veterans Affairs Integrated Care Experience
Andrew Pomerantz began his presentation by reviewing the lessons learned from systematic research on translating evidence into practice:
- Screening alone is at best inadequate to improve care;
- A collaborative care model improves outcomes with limited initial cost;
- Health psychology improves outcomes for many conditions;
- Colocation of mental health and substance use services in primary care settings is necessary but not sufficient for improving care;
- Measurement-based care improves clinical outcomes at the same or lower cost as traditional care; and
- Peer support improves engagement in treatment, leads to better outcomes, and saves money.
___________________
11 For more information, see https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/evidence-based-approaches-to-drug-addiction-treatment/behavioral-0 (accessed December 2, 2019).
Pomerantz noted that he is currently leading the VA’s effort to implement a congressionally mandated program to integrate mental health peer specialists into primary care. Even though he had the funding to pay for the peer specialists, management at some of the 15 VA facilities where he started this program were resistant because they believed their facilities needed another clinician, not a peer. “People still see peer support as a luxury,” Pomerantz pointed out.
In Pomerantz’s view, it is most important to focus on what brings patients to the clinic for treatment. In fact, he said, people who come for help most often fail to return for follow-up treatment because they are not getting what they need from treatment. “We tend to be the only specialty that does not start with a patient’s chief complaint as the problem to be addressed,” said Pomerantz, “but if we start with what seems to be the main problem, we help a large number of patients.”
Based on his experience and that of others in the field, Pomerantz felt that many stakeholders oppose moving mental health care into primary care as part of the Patient-Centered Medical Home (a model where treatment is coordinated through a patient’s primary care physician) (Croghan and Brown, 2010). Yet, evidence is growing that providing integrated care and providing team-based care is essential for providing the best care for individuals with MHSUDs. He explained that this is why the VA is working hard to integrate mental health care and primary care in the Patient Aligned Care Teams that are the VA’s version of the patient-centered medical home.
Pomerantz noted that VA integrated care has two key components. The first is co-located collaborative care that embeds a mental health clinician in the medical home team to provide consultative advice, problem-focused assessment, and brief interventions, typically delivered in up to four to six 30-minute visits. The medical home provides population-based care for mental illness, SUDs, and health-related behavior change using evidence-based treatments that the VA adapted and tested for use in the primary care setting.
The second component, care management, uses the collaborative care model12 that relies on telephone-based patient follow-up methods to track symptoms, help patients with medication adherence, and connect the consulting psychiatrists with the primary care provider. One benefit of this model is that it eliminates the 1- to 2-hour extensive initial evaluation that drives many patients away from treatment; instead, it focuses on the problem at hand and is combined with proactive follow-up. Pomerantz pointed out that across VA clinics nationally, patients have an average of two to three appointments to receive evidence-based brief interventions developed specifically for primary
___________________
12 Additional information is available at https://www.psychiatry.org/psychiatrists/practice/professional-interests/integrated-care/learn (accessed November 11, 2019).
care. Patient-reported outcome measures guide initial assessments and ongoing treatment decisions. However, one issue for consulting mental health professionals is that they do not currently receive workload credit for spending time helping the primary care physician determine their patients’ next steps. Pomerantz noted that he is working on addressing this issue.
Pomerantz explained that the facilities that have implemented this model have realized clinical outcomes that are as good, or better, than those from specialty mental health care. Other positive outcomes for VA facilities that have implemented the integrated care model include
- Improved identification and treatment in the primary care population;
- Improved engagement and continuation of care if referred to more intensive levels of treatment;
- Reduced demand for specialized mental health care;
- High patient and provider satisfaction;
- Increased likelihood of guideline-concordant care;
- Improved use of antidepressants by primary care providers;
- Reduced no-shows; and
- Significant cost savings, by both shifting more mental health care to primary care and reducing no-shows and non-engagement rates.13
Pomerantz noted that there are challenges with this model, however, including reimbursement issues, unmet training needs, maintaining advanced clinical access, developing the evidence base for the brief interventions, and the need to consistently show that this approach results in cost savings while improving people’s lives. Pomerantz also identified the need to change the culture that makes it difficult to adopt team-based care. The bottom line, said Pomerantz, is that many, if not most, patients can be adequately treated by doing only a few things differently (see Box 3).
Going forward, Pomerantz suggested expanding telehealth and mobile technology to reach more individuals and mobile technology to provide clinician-directed and supportive care that helps the patient manage their own care. He noted that there are innovations under way to use the collaborative care model for opiate use disorder, for example, and to address more complicated illnesses in primary care by providing additional mental health resources to primary care—rather than adding primary care to mental health clinics.
___________________
13 For more information, see https://www.hsrd.research.va.gov/impacts/pc-mhi.cfm (accessed January 8, 2020).
Can We Provide Necessary Care for Substance Use and Mental Health Disorders in the United States?
Access to treatment for MHSUDs is among the greatest health care disparities in the United States, said Shelly F. Greenfield, the Kristine M. Trustey Endowed Chair of Psychiatry and the chief academic officer at McLean Hospital and a professor of psychiatry at Harvard Medical School. This disparity exists despite the high prevalence of these disorders, the current dual public health crises of opioid deaths and suicide, and the availability of evidence-based treatments. It has developed, in Greenfield’s view, due to three factors:
- A chronic lack of a coordinated and integrated treatment infrastructure,
- A lack of a trained multi-disciplinary treatment workforce, and
- A longstanding stigma associated with these disorders.
According to Greenfield, addressing this problem will require a multilevel, linked, and integrated health system and a trained workforce that can deliver the multiple necessary components of care. Greenfield noted that, according to data from the National Survey on Drug Use and Health,14 57.8 million Americans had a mental health and/or substance use disorder in 2018. Approximately 19.3 million people aged 18 years and older had an SUD, 47.6 million Americans 18 years and older had a mental illness, and 9.2 million people 18 years and older had both an SUD and a mental illness (SAMHSA, 2019). Moreover, among people with an SUD aged 12 years and older or 18 years and older, nearly 90 and 57 percent, respectively, did not receive treatment (SAMHSA, 2019). Greenfield noted that of the 30.3 million Americans who had diabetes in 2015, more than three-quarters were diagnosed—compared to the situation for SUD and mental illness, where just more than 10 percent and 43 percent of patients, respectively, received treatment in 2018 (SAMHSA, 2019).
Greenfield pointed out that overcoming the technical challenges related to putting men on the moon in 1969 was accomplished more readily than harnessing the political will to build the needed infrastructure and capacity to solve this profound health care disparity in the United States. She referred to the tripartite model of innovation and change in public health and health care, developed in the 1980s and 1990s as something that could bring about needed changes (Richmond and Kotelchuck, 1991). According to this model, Greenfield explained, innovation and change can occur when there is a knowledge base with evidence of effective treatments, a social strategy that prioritizes policies to act on that knowledge base, and the political will to make change happen.
One example of the lack of political will, said Greenfield, is apparent in the fact that while the Institute of Medicine (IOM)15 issued Broadening the Base of Treatment for Alcohol Problems (IOM, 1990) as a blueprint for combining a comprehensive continuum of treatment that combined community and specialized treatment to improve alcohol use treatment, little has been done to follow that blueprint. One possible result of inaction has been a nearly
___________________
14 Available at https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.htm (accessed January 9, 2020).
15 As of March 2016, the Health and Medicine division of the National Academies of Sciences, Engineering, and Medicine continues the consensus studies and convening activities previously carried out by the IOM. The IOM name is used to refer to publications issued prior to July 2015.
50 percent increase in 12-month prevalence of alcohol use disorders in the United States since 1990 (Grant et al., 2017) despite many excellent models of comprehensive continuum of treatment (Modesto-Lowe and Boornazian, 2000; Rehm et al., 2016; Rivara et al., 2000).
“Why does this not get done?” asked Greenfield. She observed that at the practitioner level, the reasons include lack of time, inadequate or no training, no reimbursement, no idea of where to send patients for services, and not knowing that patients are treatable. “The reasons are the same today as they were 10 years ago and 20 years ago,” she noted. At the systems level, the reasons include the lack of reimbursement, absence of linkages to services, inadequate institutional or workforce capacity, and stigma in health care organizations, among health care providers, and in the community, said Greenfield. She pointed out that one result of not building the infrastructure and workforce to effectively treat MHSUDs is that the country has been unable to respond promptly to the opioid epidemic.
In 2019, the National Academies released Medications for Opioid Use Disorder Save Lives (NASEM, 2019b). The report presented research indicating that the three evidence-based treatments available for opioid use disorder (OUD) save lives, prevent relapses, reduce criminal activity and infectious disease transmission, increase retention in treatment, and increase social functioning. Such treatments are also completely underutilized, which is particularly galling, noted Greenfield, in the face of the deaths occurring from opioid use.
What the nation lacks, said Greenfield, is a coordinated, integrated treatment infrastructure, with linkages between the necessary components of care, and a trained workforce to cover all areas of the treatment infrastructure. She argued that strategies to address these deficiencies can be based on lessons learned from the experience of high-performing health plans with treatment initiation and engagement for substance and alcohol use disorders. Other lessons can be drawn from the World Health Organization’s (WHO’s) Service Organization Pyramid for integrating and linking the necessary components of care (see Figure 2).
Researchers have used the WHO pyramid to argue that three interlinked services or platforms of care—self-care and informal health care, primary care, and specialty care—are needed to meet all mental health needs. “Each platform is an essential component of care, as are the linkages among them,” said Greenfield. She added that “in the United States, we have at various times focused on one platform or another platform, but we have not focused on all of these platforms simultaneously, and the linkages between them.”
WHO defines self-care as including wellness practices, mindfulness, yoga, exercise, and activities designed to relieve stress, while the informal care system includes individuals such as peers, traditional healers, family associations, faith-based counselors, and recovery coaches. The informal care system also
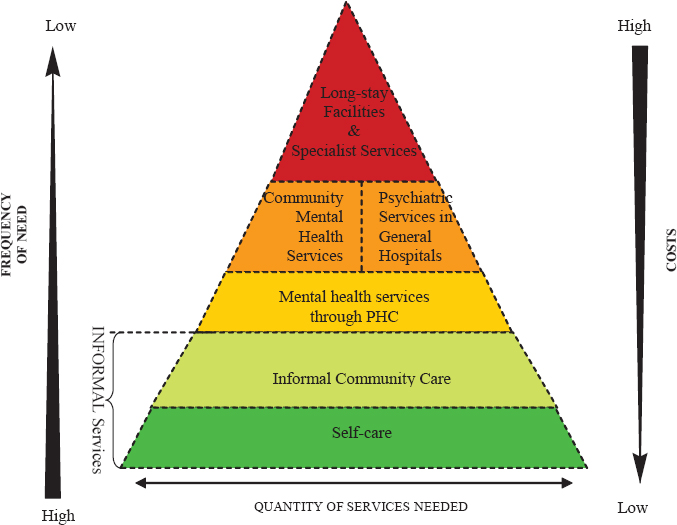
NOTE: PHC = primary health care.
SOURCES: As presented by Shelly F. Greenfield, October 15, 2019; WHO, 2003.
includes activities that build mental health literacy throughout the community to enable better recognition of the signs and symptoms of these disorders and awareness about effective treatment options.
The primary health care system is the fundamental and first component of care in the formal health care system, noted Greenfield. In her opinion, primary health care is often more accessible, affordable, and acceptable for individuals, families, and communities than specialty care, and it is a place where mental health and SUD services are most likely to be integrated with other medical issues an individual might be facing. Primary care is also likely to be where collaborative and stepped approaches to care occur, she explained.
Specialty care, noted Greenfield, is where psychiatry and addiction services are located. These include general hospital psychiatry units that are well staffed with trained providers, specialty mental health and addiction programs, community mental health centers and addiction treatment programs, opioid treatment programs, and residential treatment centers that combine hospital- and outpatient-based care.
“Every single one of these platforms is necessary to provide care, and linkages between and among them are necessary,” said Greenfield. Without those linkages, she added, the system does not work.
As one example of policy changes and necessary linkages among components of care for MHSUDs, Greenfield noted the lessons learned from a conference at McLean Hospital that convened state and local government officials, treatment experts, law enforcement officials, and representatives of community-based agencies from the 10 states most heavily affected by opioid overdoses (see Figure 3).
Greenfield also referenced a 2019 study that examined best practices for treating, initiating, and engaging people for SUD and OUD treatment among 400 health plans. The study found that, with respect to initiation and engagement, high-performing plans were associated with higher rates of outpatient services, intensive outpatient services, and partial hospitalization16 (O’Brien et al., 2019). The study also identified three common themes among plans with higher rates of engagement and initiation of treatment:
- The care model was focused on care coordination, including physical, mental, behavioral, and SUD-specific services.
- Benefit design required no prior authorization for outpatient treatment and medication for OUD and included coverage for at least two MAT options and naloxone; Medicaid plans had no out-of-pocket costs for covered services.
- There was open communication among health care providers and beneficiaries, including the availability of secure electronic messaging and outreach teams trained to communicate effectively.
In addition, the study identified barriers to treatment, initiation, and engagement and a number of potential solutions to address those barriers (see Table 2). The last barrier—that plan members have competing needs such as housing and child care—is one potential explanation for high-performing health plans have fewer female beneficiaries seeking treatment, as females are more likely to have these roles and responsibilities, said Greenfield.
___________________
16 Partial hospitalization refers to an intense, structured treatment setting for individuals who have difficulty maintaining current daily routines or would otherwise require inpatient behavioral health care (O’Brien et al., 2019).
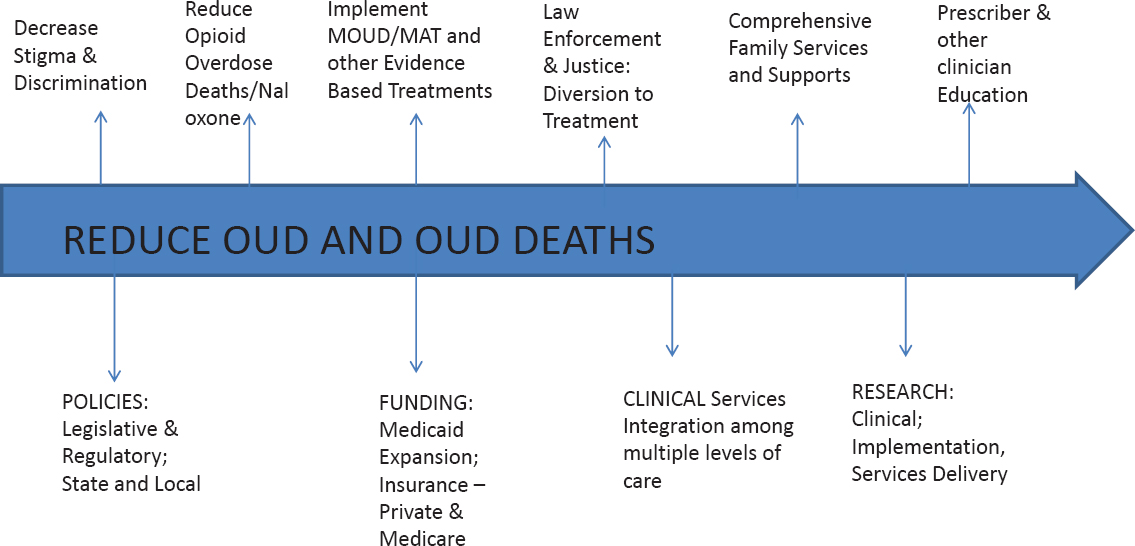
NOTE: MAT = medication-assisted treatment; MOUD = medications for opioid use disorder; OUD = opioid use disorder.
SOURCE: As presented by Shelly F. Greenfield, October 15, 2019.
| Barriers | Potential Solutions |
|---|---|
|
|
SOURCES: As presented by Shelly F. Greenfield, October 15, 2019; O’Brien et al., 2019.
Building on these lessons learned, Greenfield suggested a number of strategies to deliver the necessary components of mental health and SUD care, including
- Incentivize the workforce to see patients in multiple settings for screening, assessment, referral, and treatment;
- Build capacity through training;
- Provide access to levels of care in all the necessary delivery platforms;
- Acknowledge multiple co-occurring disorders, and build in mechanisms and incentives for identification and treatment;
- Use technology to address wide gaps in care and in training;
- Model and assess outcomes across multiple sectors prospectively and longitudinally;
- Address the stigma barrier by society and clinicians, as well as self-stigma; and
- Restructure payment systems to achieve these goals.
Greenfield stressed that in the area of payment reforms, it will be necessary to incentivize physicians and other health care providers by increasing individual provider payments for needed services, including screening, assessment, and diagnosis, smoking cessation treatment, and prescribing MAT. According to Greenfield, restructuring and reforming the health care payment system (including making changes in Medicare and Medicaid programs to support these goals) would incentivize them to achieve desired outcomes—as would creating a stable, reliable, and predictable funding base to support a coherent system of care. Greenfield also recommended requiring training at all levels of provider education. This would involve training on MHSUDs for nurses, psychologists, social workers, pharmacists, physician assistants, and other professionals involved in an integrated system of care. She emphasized that it will be necessary to push all available policy levers at the same time in order to make real progress.
In closing, Greenfield said the opioid crisis has been superimposed on longstanding failures to provide necessary treatment for SUDs and other mental health disorders in the United States. Moreover, the response to the crisis demonstrates the need for linked, multi-level formal and informal service delivery platforms and supports from other service sectors. She noted that evidence-based treatments are possible at each level of treatment delivery platforms but all are necessary, interrelated, and linked components of care. Ultimately, effective solutions require a multi-level, integrated health system, a workforce trained to provide treatment, and a combination of state and federal policies to address payment and training barriers, concluded Greenfield.
Considering Essential Components of Care While Maintaining a Focus on Behavioral Health Equity
Ruth Shim, the Luke and Grace Kim Professor in Cultural Psychiatry at the University of California, Davis, School of Medicine, began her presentation by recounting an observation she made when she was a psychiatry resident and split her time between Emory University Hospital—a well-resourced institution in Atlanta’s suburbs—and Grady Memorial Hospital in downtown Atlanta. She observed that the predominantly white patients admitted to Emory with a serious mental illness would get better when provided with inpatient therapy, while the predominantly African American patients admitted to Grady with a serious mental illness would not improve even though they received the same
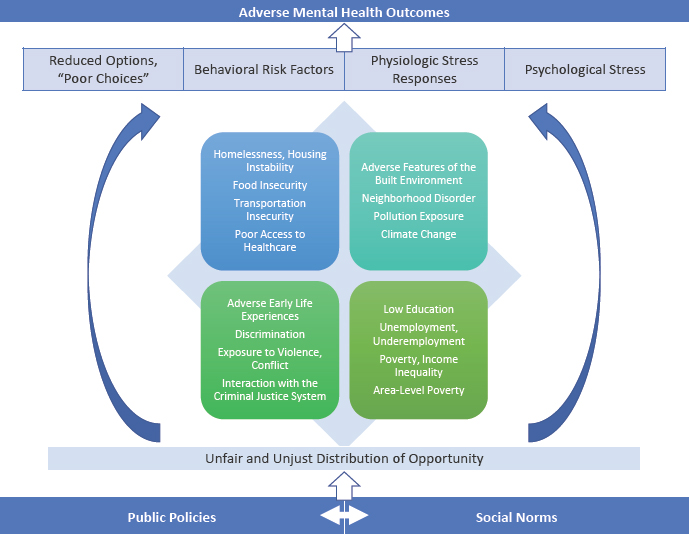
SOURCE: As presented by Ruth Shim, October 15, 2019.
interventions. After considering a number of possible reasons for the differences in outcomes, Shim realized that the root cause came down to the two patient populations’ experiences with the social determinants of health (see Figure 4).
Citing WHO, she defined the social determinants of health, mental health, and behavioral health as “those factors that impact upon health and well-being: the circumstances into which we are born, grow up, live, work, and age—including the health system. These circumstances are shaped by the distribution of money, power, and resources at global, national, and local levels, which are themselves influenced by policy choices.” In other words, said Shim, “the factors by which we live are often shaped by the decisions that we as a society make about who gets resources and who does not.”
Shim clarified that there is a difference between health disparities and health inequities. Health disparities are differences in health status among distinct segments of the population, including differences that occur by gender, race or ethnicity, education or income, disability, or various geographic localities. Health inequities are disparities in health that are a result of systemic, avoidable, and unjust social and economic policies and practices that create
barriers to opportunity. “So when we think about all of the disparities that we have been talking about that affect substance use disorders, that affect mental health, that affect all of our health outcomes, are these actually disparities, or are they inequities?” asked Shim. According to Shim, the differences in mental health and mental illness outcomes are inequities, not disparities.
Shim pointed out that the U.S. Surgeon General issued a report in 2001 highlighting that racial and ethnic minority groups have less access to care and availability of care, receive generally poorer-quality mental health services, and experience a greater disability burden from unmet mental health needs. At the heart of this issue, said Shim, lies the concept of social justice, which the political philosopher John Rawls defined as “assuring the protection of equal access of liberties, rights and opportunities, as well as taking care of the least advantaged members of society” (Rawls, 1971). Shim also stressed the importance of understanding the concept of structural racism, a system in which public policies, institutional practices, cultural representations, and other norms work in various often reinforcing ways to perpetuate inequity between racial groups (Bonilla-Silva, 1997). Structural racism, she explained, identifies dimensions of our history and culture that have allowed privileges associated with “whiteness” and disadvantages associated with “color” to endure and adapt over time. Most importantly, said Shim, structural racism is not something that a few people or institutions choose to practice; rather, it has been a feature of the social, economic, and political systems in which everyone exists. In other words, even if all interpersonal discrimination was eliminated from society, inequities in health outcomes would still persist because of how deeply structural racism is entrenched in U.S. society.
Providing historical context, Shim explained that the Social Security Act of 1935, which allowed generations of people to build wealth in the United States, is an example of structural racism in that it excluded agricultural and domestic workers—the majority of whom were African Americans living in the South. The war on drugs, residential segregation resulting from redlining and other practices, and current immigration policies are other examples of structural racism (Bailey et al., 2017; Gee and Ford, 2011). So, too, is the lack of a national health care system, which Shim claimed came about because of a historical decision by physicians and the American Medical Association to push back against efforts to provide all people access to health care. The end result, she said, is that the percentage of people without adequate health insurance coverage varies markedly according to race (see Figure 5).
Shim emphasized that racism and discrimination substantially affect health and mental health. She called attention to data that support the association of racism and discrimination with poor mental health across a variety of outcomes and mental health conditions, including PTSD, major depressive disorder, generalized anxiety disorder, and alcohol use disorder (Paradies et
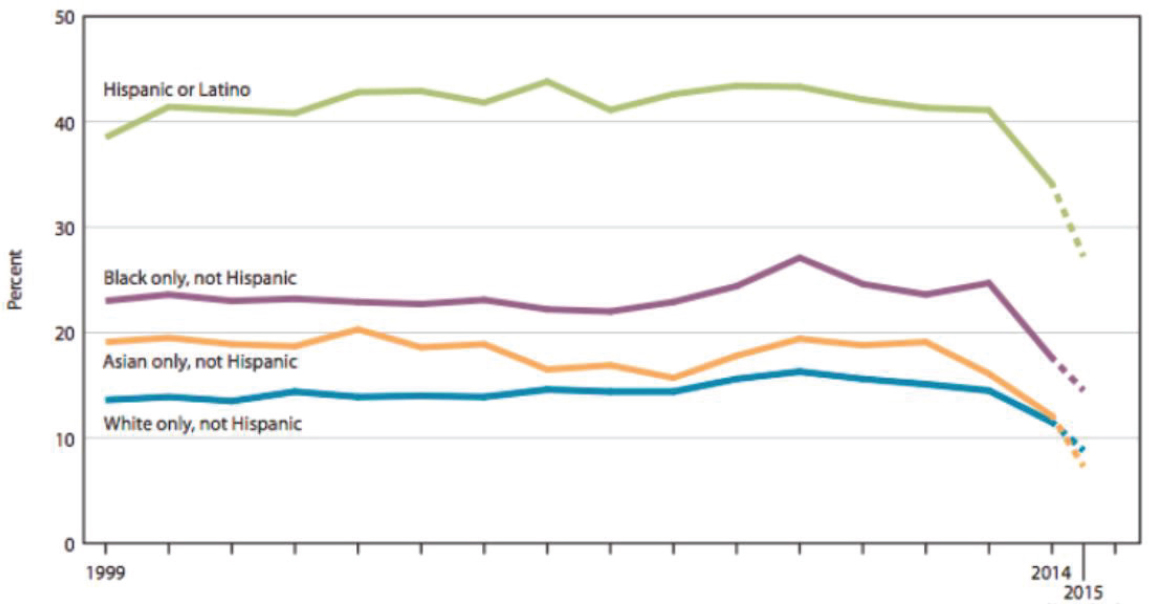
SOURCES: As presented by Ruth Shim, October 15, 2019; NCHS, 2016.
al., 2015). Shim also referenced a 2017 study, which found that 32 percent of African Americans and 20 percent of Latinx report they have been discriminated against when going to a doctor or health clinic (Harvard T.H. Chan School of Public Health et al., 2017) (see Figure 6). “We talk about designing systems that people want to go to, but I think that if you are discriminated against when you go to seek care, you would not necessarily want to return to that type of setting,” said Shim.
Shim also discussed the concept of intersectionality—that there are multiple identities people share within themselves that build on each other—as it relates to MHSUDs (Crenshaw, 1991). Failing to address a person’s multiple identities, she said, means that not all of their needs are being addressed.
Shim described how focusing on social care can be an effective way to address poor outcomes in health, mental health, and SUDs (NASEM, 2019a). Countries with a higher percentage of gross domestic product spent on social care programs (including education, retirement, housing, employment, disability benefits and food security) have longer life expectancies, she said—a finding that also holds true for individual U.S. states (Bradley et al., 2016).
In closing, Shim suggested that the goal should be equity, not equality. Moreover, when defining essential components of care, it is important to appropriately consider the needs of the specific target population.
Implementation Science and Care for Mental Health and Substance Use Disorders
“Why do large health care systems implement change?” asked Mary Durham, the retired director of Kaiser Permanente’s Center for Health Research. She noted that this is an important question to ask when considering what essential components of care look like in a capitated system.17 Durham stated that capitation has limitations but also allows for greater flexibility in choosing programs and benefits for individuals through clinical care. She pointed out that given that capitated care relies on an evidence base, ineffective and unsafe choices can be eliminated as part of the basis for defining essential components of care for MHSUDs.
Durham explained that large health systems implement change for a number of reasons, including the need to grow market share. This often requires determining which services will be attractive for employers to offer to their employees and negotiating where services are to be delivered and the technologies used to deliver care. Similarly, health systems change as part
___________________
17 Capitation is a type of payment in which a health care service provider is paid a fixed amount per patient for a prescribed period of time by an insurer or physician association.
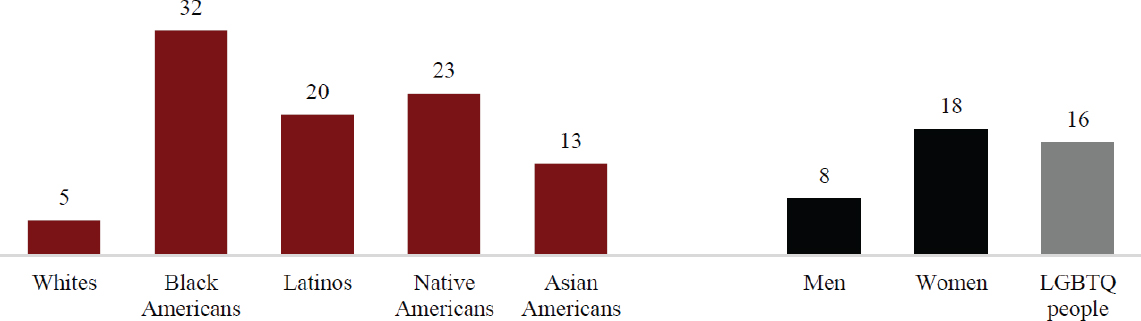
NOTE: LGBTQ = lesbian, gay, bisexual, transgender, queer/questioning.
SOURCES: As presented by Ruth Shim, October 15, 2019; Harvard T.H. Chan School of Public Health et al., 2017.
of their drive to obtain a five-star rating from the National Committee for Quality Assurance, which is based in part on behavioral health measures and important for the financial stability of large health care organizations, Durham observed.
She also pointed out that systems implement change related and in response to regulations and lawsuits, Medicaid expansion, new medical evidence, and a vocal clinical champion for change. She noted that state regulations can provide opportunities to include measurement as part of the data required in health care system reporting. Additionally, real or threatened lawsuits can provide opportunities to raise awareness about the social determinants of health, said Durham. She added that, with this awareness, researchers can examine the impact of an investment in the social determinants of health on an individual’s health and safety.
Durham noted that important drivers of organizational change include the need to save money and address labor shortages. Durham commented that a desire for long- versus short-term return on investment will affect whether some health care organizations will implement evidence-based programs. For example, medical homes are presumed to improve care coordination and cut costs, but the degree to which they gain traction will depend on whether the systems implementing them will realize a fairly quick return on investment.
According to Durham, labor shortages can also impact whether large health systems implement change. Health care systems may not have a choice given an absence of primary care providers, or they may be required to use other providers to fill those roles. She noted that primary care has been redesigned many times in an attempt to improve care delivery and produce cost savings. Information system implementation can also drive change, as systems must respond to changing evidence and technologies. Perhaps the most forceful driver of change, in Durham’s opinion, is a clinical champion; she has seen examples of these champions—health care providers, chief executive officers, or board members—creating change by demonstrating unexpected evidence.
Durham noted the importance of evaluation: bright ideas without solid and specific evidence of effectiveness and a strong return on investment will not be acceptable in practice to health care plans. Additionally, health systems may need to critically reevaluate common frameworks and models to meet the needs of the current population.
In conclusion, Durham cautioned that unsettled health care policies due to fluctuating politics can also impede change, due to regulatory or legal uncertainty and changes in federal funding. However, factors such as progress in technology, artificial intelligence, addressing the social determinants of health, and financial incentives for quality measures represent promising advancements that could contribute to health systems change.
Discussion
In the discussion session following the speakers’ presentations, Missy Rand from the National Association of State Mental Health Program Directors asked Pomerantz if there are specific screening tools he has used consistently that look at mental health screening, substance use screening, and suicidality. Pomerantz responded that good mental health care requires a clinical pathway to address a positive screen and not just screen for the sake of complying with an accreditation requirement or getting paid. Toward that end, and with the increasing focus on suicide prevention, the VA has instituted a multi-step suicide screening process18 that Pomerantz noted eventually led to a more comprehensive suicide risk and safety planning evaluation.
Abigail Wydra from the U.S. Department of Health and Human Services’ Office of Inspector General asked Greenfield if she could describe what successful linkages look like. Greenfield replied that practitioners voice frustration with not being able to move people to and from the levels of care they need. For example, her primary care colleagues see patients with profound MHSUDs that they were never trained to address, and yet they have trouble finding psychiatric care or community-based care for these patients. Similarly, an inpatient psychiatric care facility may have trouble referring patients to community-based care. This is a solvable, human-made problem, said Greenfield, but it will require finding ways within Medicare and Medicaid to incentivize creating those linkages. Greenfield suggested that the first step would be to adequately pay providers who treat MHSUDs. Essock added that it is important to find ways to design a system that will incentivize spending on effective treatment approaches that generate good clinical outcomes, and this requires building relationships that instill hope and trust.
Stephanie Guerra with the VA Office of Research and Development asked the panelists if there are intentional strategies to ensure programs can be sustainable over the long term, once initial funding has ended. Pomerantz replied that this is a challenge because much of the payoff occurs over the long term, even though many programs can demonstrate some short-term success. Durham commented on the importance of having clinical champions, who can tout those short-term clinical successes, and regulations that set minimum standards. Shim agreed that regulations and policies are needed to support long-term implementation of effective programs.
Michael Freed from the National Institute of Mental Health asked the panelists for their thoughts on evidence standards that might inform funding and adopting interventions. Greenfield replied that the problem is not a lack
___________________
18 For more information, see https://www.healthquality.va.gov/guidelines/MH/srb/VADODCP_suiciderisk_full.pdf (accessed December 3, 2019).
of evidence-based treatments. In fact, she applauded the work the research community has done on the efficacy and effectiveness in clinical trials for both behavioral and pharmacotherapeutic treatments for MHSUDs. In her opinion, the problem is a lack of multiple integrated and linked platforms of care to deliver those interventions. Pomerantz added that evidence-based medicine is only part of the equation; the other part is the individual person being treated. Pomerantz recalled when he had a patient with PTSD and tried to treat him with cognitive processing therapy. That did not work for him, but he began to heal when he was given dentures. According to Pomerantz, the dentures made him more socially acceptable, and that had a significant impact on his mental health and well-being.
Dawn Wiest from the Camden Coalition of Healthcare Providers and the National Center for Complex Health and Social Needs asked the panelists for ideas on how to reconcile the fragmentation in research and within delivery systems to create a dialogue around scalable evidence. Pomerantz’s idea was to expand studies to look at outcomes beyond health and cost and find ways of evaluating the effect of an intervention on presenteeism and absenteeism, family members, and other non–health care outcomes. Greenfield agreed with that idea and added the suggestion to hold convenings that bring together people from different systems to learn from one another and create a system that combines the evidence base and the implementation of that evidence base in the real world.
PROMISING STRATEGIES TO TRANSLATE KNOWLEDGE INTO PRACTICE AND MONITOR IMPLEMENTATION
Opening the workshop’s third session, moderator Anita Everett, the director of the Center for Mental Health Services at SAMHSA, noted that her agency has addressed the challenge of improving care for individuals with MHSUDs by breaking it down into three components:
- The “front door problem,” which focuses on the problem of increasing access to care;
- The “black box” of what happens in the treatment setting; and
- The “exit strategy,” or how the system deals with individuals in terms of whether they need episodic or ongoing treatment.
The focus of this workshop panel, explained Everett, is on the black box component, or the overly variable system of care in the United States. “What people get in that box, whether it is primary care, specialty care, or even more intensive residential style care, is extremely variable across our country. One of
the reasons for that variability has to do with the way that we implement or do not implement those kinds of services,” said Everett.
Harnessing Implementation Science to Realize the Promise of Evidence-Based Practice
Rinad Beidas, an associate professor of psychiatry and medical ethics and health policy at the University of Pennsylvania Perelman School of Medicine and the director of the Penn Implementation Science Center at the University of Pennsylvania’s Leonard Davis Institute of Health Economics, began her presentation with a personal story to illustrate why she believes implementation science can be a valuable tool for transforming health and mental health. She described that while doing her clinical training to become a psychologist, she began to observe a troubling pattern of clinicians in the community not using evidence-based practices, such as cognitive behavioral therapy, to treat children with mental health issues. The result was that these children were not improving. This realization, she explained, changed her career trajectory and sent her down the path of focusing on implementation science as a potential solution to this problem.
Beidas explained that it takes approximately 17 years for 14 percent of research to make its way into practice (Balas and Boren, 2000; Morris et al., 2011). “I think we can all agree that is unacceptable,” said Beidas, which is one reason she believes in the importance of applying implementation science to mental health and substance use treatment. Implementation science, she explained, is about making sure that people are receiving care and treatment approaches that have been demonstrated to work in the community to move the needle in health and mental health. Beidas explained that implementation science is the scientific study of methods to promote systematic uptake of proven clinical treatments, practices, and organizational and management interventions into routine practice, and hence to improve health (Eccles et al., 2012; Grimshaw et al., 2012). At its core, she noted, implementation science is about clinician behavior change within organizational constraints. Contextual differences across sites and organizations can provide important lessons going forward, observed Beidas. Importantly, Beidas noted, implementation science only deals with evidence-based interventions. “We want some evidence for what we are trying to implement or scale up,” she said.
As an example of ways in which she has applied concepts of implementation science, Beidas described some of the work in Philadelphia’s large public mental health system, which treats more than 150,000 individuals per year, including 30,000 children and families (Beidas et al., 2016b). Starting in 2007, the newly appointed commissioner of the city’s Department of Behavioral Health and Intellectual Disability Services began a number of efforts to transform the sys-
tem to one of recovery by implementing evidence-based practices—particularly cognitive therapy, prolonged exposure, trauma-informed cognitive behavioral therapy, dialectical behavior therapy, and parent–child interaction therapy—in the city’s public mental health system. After a few years, Beidas explained, the commissioner noticed that there were common challenges implementing these evidence-based practices. In response, he convened a public academic task force in 2013, the Evidence-Based Practice and Innovation Center, to serve as the centralized infrastructure to support the implementation of evidence-based practices (Powell et al., 2016). The task forced developed five key components to support implementation of evidence-based practices (see Figure 7).
The first component involved educating clinicians on evidence-based practice and providing them with ongoing support aligned with recommendations from leading treatment developers, said Beidas. The second component relied on a unique situation in Philadelphia—a single-payer system for all Medicaid services falling under the umbrella of community behavioral health—that enabled the city to encourage health care providers to use evidence-based guidelines in contracts for service. A third component involved hosting events that highlighted evidence-based practice champions and individuals who had benefited from those practices. As these practices diffused through the system, organizations acquired the designation as evidence-based practice agencies, which led to enhanced rates for delivering such practices, noted Beidas.
To observe what happens when a large health care system, such as Philadelphia’s, implements a centralized infrastructure to support evidence-based practice, Beidas and her colleagues launched a 5-year prospective mixed-methods observational study of the 29 agencies that serve more than 80 percent of the children and families receiving outpatient mental health services. Nineteen agencies, with 130 therapists, agreed to participate, with others joining in subsequent years. One of the first questions the team examined was whether clinical or organizational characteristics played a role in determining how well evidence-based practices were adopted. The data showed that organizational
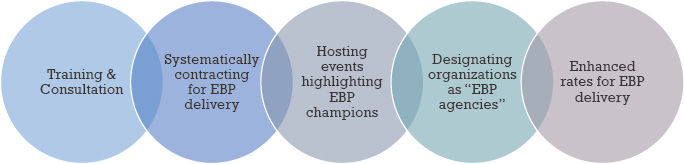
NOTE: EBP = evidence-based practice.
SOURCES: As presented by Rinad Beidas, October 15, 2019; Powell et al., 2016.
factors explained more of the variance in the use of evidence-based practices, while therapist factors explained more of the variance for non-evidence-based practices (Beidas et al., 2015). These results, noted Beidas, suggest the importance of targeting organizational factors when thinking about implementation approaches and clinician factors when thinking about changing patterns of existing clinician behavior.
Beidas explained that over the course of 5 years, the use of cognitive behavioral therapy increased 6 percent, and for each additional evidence-based practice initiative the clinicians participated in, self-reported use of cognitive behavioral therapy techniques increased by 3 percent. While these numbers seem small, Beidas said that a 6 percent change in a very large system that treats 30,000 children and families can be meaningful. She added that a proficient organizational culture at baseline predicted a steeper increase in the use of cognitive behavioral therapy (Beidas et al., 2019a,b) and that she and her team have yet to look at patient outcomes to see if these practice changes were making a difference in patients’ lives. She felt that creating a centralized infrastructure that can foster change was a promising outcome.
Beidas explained that her team then examined qualitative data to understand the barriers and facilitators to the implementation process from a range of stakeholders, including the system’s treatment developers, system leaders, and agency administrators who were involved in the implementation initiative (Beidas et al., 2016b). What they learned was that coordination, communication, and collaboration were major facilitators of success. At the same time, the team also identified three barriers to implementation:
- The chilling fiscal environment in community mental health and substance use treatment delivery (Stewart et al., 2016);
- Staff turnover of 24 percent per year (Beidas et al., 2016a), creating the need for training models that allow for continuously bringing in new staff; and
- A new workforce model that is shifting from using salaried therapists in favor of independent contractors (Beidas et al., 2016c), which is a trend seen nationally.
In terms of the last barrier, a subsequent study on attitudes toward and knowledge about evidence-based practices in this new workforce suggest that there are fewer positive attitudes and less knowledge and use of evidence-based practice among independent contractors. In Beidas’s opinion from qualitative data, the issue is that administrators are less likely to send their contractors to trainings because they see them as being a more transient workforce.
One lesson from this work, observed Beidas, is that agencies are necessarily more worried about keeping their clinics open, staying compliant with
regulations, and retaining their workforces than implementing new practices. “Evidence-based practice is like self-actualization; everybody thinks it is important, and yet there are some real infrastructural challenges to be thinking about,” said Beidas. Another important lesson is that systems were able to iterate their approach to implementation in response to the ongoing evaluation of their efforts. For example, noted Beidas, the latest contracts for service require agencies to have more salaried therapists on staff.
Additionally, in Beidas’s view, clinicians work in a challenging context, so any new program must make it easier, not harder, for them to do the right thing. “I think sometimes that our evidence-based practices make it harder on them,” observed Beidas.
Beidas noted that implementation efforts must go beyond training and consider interventions to address organizational factors. Evidence-based practices will not be a panacea for addressing infrastructural challenges that require greater investments in the community health system. Beidas concluded that implementation science is important because it allows us to understand how to transform the quality of care and improve the lives of children and families.
Using Evidence to Support Healthier Families and Better Lives
Bruce Chorpita, a professor of psychology and the director of the Child FIRST (Focus on Innovation and Redesign in Systems and Treatment) program at the University of California, Los Angeles, began his remarks by emphasizing that the overarching goal of health system reform is not to implement evidence-based practices, though he acknowledged it is an important strategy. Rather, he explained, the goal is to make people’s lives better, to build systems that transform lives and make stronger, healthier communities.
Chorpita noted that in his area of expertise (youth mental health) there is a strong research base that includes 1,118 randomized controlled trials over the past 50 years. However, he pointed out, even after all of that research and more than 20 years of implementation, most youths still receive no or low-quality care (Garland et al., 2001; Gyani et al., 2014; Zima et al., 2005). For Chorpita, this is due to the way in which evidence is packaged that makes it difficult for clinicians to use it in the systems in which they work.
Chorpita pointed out that there are more than 770 evidence-based practices for youth mental health and substance use problems—which may be too many. Chorpita explained that when he and his colleagues tried implementing 50 of these practices in Los Angeles County, with a population of approximately 13–14 million people, the outcome was not positive (Bernstein et al., 2015a,b; Chorpita et al., 2011; Park et al., 2018; Southam-Gerow et al., 2010). Chorpita said that most of the interventions were not implemented and that his team repeatedly observed that evidence-based practices have lower effect sizes when
put into practice in the community than when tested under controlled conditions. Chorpita noted that some of this difference may be because, although clinicians may be required to use a practice, they may not do so effectively.
In Chorpita’s view, this finding suggests that the problem is how knowledge and evidence is designed. He explained that what is needed is a dynamic design that can respond to measurement and feedback from the individual and the community, as well as strategic intelligence. “What is happening around you is important to know,” said Chorpita. He mentioned copious evidence in the literature that supervision and consultation, which he considers strategic intelligence, are important services to improve quality and professional development.
To better understand the available data, over the past two decades, Chorpita and his team have coded more than 2,400 treatments for hundreds of features, allowing them to identify 30–40 common elements among effective treatments. Chorpita noted that this helps to reduce and filter information to inform people at the point of care. They then developed a methodology for discovering the common practices for treatments for specific problems and contexts. The result is what Chorpita referred to as “an instant meta-analysis knowledge product” that represents the distillation of raw knowledge from research papers and the knowledge summaries contained in numerous review articles into a form the practicing clinician can access and read quickly to get the information needed at the moment it is needed to best treat an individual patient. Treatment manuals, said Chorpita, are examples of knowledge products. “The takeaway point here is that we need to think about how we are designing and packaging knowledge. We’re going to continue to do science, [and] we’re going to continue to discover what works, what makes things better. We need to think about how to package that effectively,” he said.
Chorpita emphasized that supplying knowledge does not necessarily lead to its strategic use (Graham et al., 2006; Park et al., 2018; Tsai et al., 2019; Young et al., 2007). The reason, he explained, is that knowledge is packaged in an action cycle that does not always start from a place of first identifying the problem before selecting the evidence in support of a solution. “You might think that people would identify the problem they are going to work on before they pick the intervention they are going to use, but that is not the case,” he said. For example, people are using evidence-based treatments for problems that children do not have, which is, in a certain sense, not unexpected given the mandate to use such treatments.
Chorpita explained that the action cycle does not happen on its own, as he and his colleagues determined in a study that looked at the benefits of adding supervision to the process. Preliminary findings have shown that without supervision, people select an evidence-based intervention only 7 percent of the time. With supervision, people identify the problem collaboratively and select a solution—usually an evidence-based treatment.
Chorpita suggested one approach to expanding the implementation of evidence-based practices is to consider providing incentives to industry to entice it to join in this effort and bring with it all the health information systems, literature databases, messaging and visualization technologies, and learning management systems it has developed. “These technologies can be leveraged, coordinated, and arranged to do the things we want them to do in children’s mental health and substance use,” said Chorpita. Currently, he added, lettuce production is more advanced and evidence based than the delivery of mental health care to the nation’s children.
Chorpita discussed some of the work he and his colleagues conducted over a 20-year period in Hawaii. The team implemented a fully coordinated system, which tripled the average effect size of clinical and functional outcomes across all youth in Hawaii’s mental health system in that time (Daleiden et al., 2006). Moreover, Chorpita described how a fully coordinated system enabled clinicians to produce results that were better than usual care and were even better than standard evidence-based treatments implemented by their developers (Weisz et al., 2012). Chorpita and his colleagues obtained similar results working in Los Angeles County (Chorpita et al., 2017), where the fully coordinated system has become the nation’s largest for youth mental health. This practice model, which has trained more than 4,000 care providers and served more than 250,000 youths in just that county, is the only model being used today by every one of the 95 agencies to adopt it over the past 7 years (Mennen et al., 2018; Rodriguez et al., 2018).
Chorpita also pointed to results from the Child and Health Development Institute of Connecticut, which, while they had yet to be peer reviewed at the time of the workshop, did show that a fully coordinated system is outperforming all other cognitive behavioral therapies, other evidence-based treatments, and usual care in the state. Chorpita added that the results indicate that children of color responded disproportionately better than did white children.
Referencing his opening remarks, Chorpita concluded by emphasizing that big change is needed, and this will require taking steps to create a system that better translates knowledge into action. “We will never know as little as we know now, because we’re still discovering things every day, and we know more now than we ever did in history,” he said, “so the problem of knowing everything and not knowing what to do with it is only going to get worse.”
Medication-Assisted Treatment and Substance Use Disorder Treatment in Primary Care Settings: A Focus on Community Health Centers
Marwan Haddad is the medical director of the Center for Key Populations at Community Health Center, Inc. Founded in 1972, the center is one of the largest federally qualified health centers in the nation. The center has 15 clinics,
treats 100,000 patients per year, and serves as a patient-centered medical home.19 Haddad identified the center’s three foundational pillars as (1) clinical excellence, (2) research and development, and (3) training the next generation of clinicians. The organization’s Weitzman Institute functions as the research, education, and training arm. Haddad also noted that the center is the first of its kind that focuses on the key groups that experience health disparities secondary to stigma and discrimination, including people who use drugs; lesbian, gay, bisexual, and transgender populations; the homeless; the recently incarcerated; and sex workers. A cohort of experts in the center train and educate primary care providers across the organization so that they are able to integrate care for these populations as a part of their routine medical care responsibilities.
Haddad pointed out that the Weitzman Extension for Community Health Outcomes (ECHO) program20 provides specialty support for primary care providers seeking to gain expertise in managing certain complex illnesses and conditions (Arora et al., 2010), and Community Health Center, Inc., is the first federally qualified health center to operate its own Project ECHO clinics. ECHO, explained Haddad, is a model of training and consultation in which primary care providers participate in video conferences with a multidisciplinary faculty of experts who consult on cases. The idea is that over time, the primary care providers become experts in their own right, creating a force multiplier that allows providers to treat their patient locally. The ECHO program, started in 2012, focused initially on HIV and hepatitis C and has expanded over time to multiple other disciplines, including MAT for OUD in 2013. To date, 126 practices nationwide have participated in the ECHO MAT program.21
Haddad observed that over the past couple of years, many health centers around the country have received grant funding to establish MAT programs but struggled to figure out how to either implement and initiate or scale up such programs. In response, Haddad and his colleagues developed a set of learning series and webinars, virtual and in-person trainings, and site visits with ongoing coaching and consultation for these agencies. From the moment the Weitzman Institute began offering this technical assistance program for MAT for SUD, it has received interest from health care providers in every state across the nation, explained Haddad.
Working with Community Health Center, Inc., clinics, as well as other health centers across the nation, Haddad has seen a number of different MAT
___________________
19 For more information, see https://www.centerforkeypopulations.com (accessed April 23, 2020).
20 For more information, see https://echo.unm.edu (accessed December 3, 2019).
21 For more information, see https://echo.unm.edu/teleecho-programs/mat (accessed April 23, 2020).
models being adopted. Haddad pointed out that his center’s primary option is the integrated primary care model that inducts, stabilizes, and maintains its MAT patients who are seen alongside any other patient. Other popular models include an integrated MAT clinic model, where prescribers have times and days set aside for MAT patients; the co-located model, in which MAT is prescribed in a clinic separate from primary care but prescribers could be primary care providers; the hub-and-spoke model, in which an expert hub provides inductions and a health center handles stabilization; and telemedicine models, which are starting to be deployed to deliver behavioral health and substance use treatments.
Haddad identified a number of common challenges for MAT programs in primary care:
- Obtaining buy-in to the program from both clinical staff and administration;
- The financial cost and securing reimbursement in the context of the 15-minute clinical visit and the use of nonclinical staff, such as case managers and coordinators;
- Inadequate training and expertise on addiction, harm reduction, and treating addiction as a chronic disease;
- Too little time and support in the face of competing priorities;
- The inability to use information technology efficiently to look at quality measures and engage in quality improvement activities;
- Not knowing how to deal with polysubstance use, which is linked to a lack of understanding and training on addiction and SUD;
- Fear of diversion (the idea that patients will try to deceive providers); and
- The confusion as to whether providers have a health care or law enforcement responsibility.
Presenting data and statistics goes a long way toward getting buy-in, said Haddad, as does finding clinical champions who can lead the way at their organizations. One way to address the financing problem, he suggested, is to identify approaches to maximizing billing potentials, such as billing for registered nurse time as part of a care team. Encouraging more training can be done by promoting and paying for any training a health care provider needs on an ongoing basis. So, too, can working with a Project ECHO mentor who can support the provider and hiring providers and staff that already have training in addiction. “You have to conduct agency-wide and discipline-specific trainings over and over again, especially around true harm reduction,” said Haddad.
Haddad suggested taking a team-based approach with the prescriber at the center of a team that includes nursing, behavioral health, and care coor-
dinators. Under this approach, for example, patients are required to follow up with a team member to obtain a voucher that enables them to receive prescriptions at the pharmacy.
Haddad also explained that Community Health Center, Inc., has implemented a buprenorphine dashboard that will help with quality improvement initiatives. Dealing with polysubstance use requires training and involving behavioral health professionals as true partners in a patient’s care in the primary care setting. Haddad noted that his center has established a number of strategies to limit diversion and tampering with samples, including using urine cups with temperature gauges and requiring patients to designate a pharmacy.
Haddad pointed out that the center has prescribed buprenorphine to nearly 2,700 patients since 2007, with about 2,200 of those prescriptions written since the ECHO MAT program was implemented in 2013. Haddad also shared that, according to a preliminary data analysis from more than 1,500 patients, buprenorphine treatment retention rates were approximately 55 percent in the first year, slowly dropping to between 46 and 29 percent of patients retained over the next 9 years, which demonstrates good retention rates for a real-world primary care setting like their large federally qualified health center. He noted that most studies typically only report buprenorphine retention rates over a 6- to 12-month period. Haddad added that they were not able to account for patients becoming incarcerated, moving, or changing to a different treatment program, which would likely explain some of the drop in retention rates.
Haddad emphasized that an additional benefit of providing MAT in the primary care setting is that it allows individuals to be engaged in primary care alongside substance use care. As a result, screenings for hepatitis C, HIV, syphilis, depression, and breast, cervical, and colon cancer all increase between the first MAT prescription and the last one.
In closing, Haddad presented a list of larger structural and societal barriers that he believes need to be addressed to combat the opioid and drug use epidemics and some potential solutions (see Table 3).
Integrating Primary Care and Behavioral Health Services in Coordinated Community Systems
Steven Melek, a principal and a consulting actuary for Milliman Consulting, shared the experience of integrating primary care and behavioral health services in Colorado. He noted that between 2015 and 2019, Colorado received $65 million from the Center for Medicare & Medicaid Innovation (CMMI) to implement and test an innovation plan to integrate physical and behavioral health care in more than 400 primary care practices and commu-
| Barriers | Potential Solutions |
|---|---|
|
|
SOURCE: As presented by Marwan Haddad, October 15, 2019.
nity mental health centers with approximately 1,600 primary care clinicians.22 Each practice, he noted, could do so in its own way, using team-based care, collaborative care, telephone psychology consults, and other approaches suitable for use in the urban, rural, or frontier regions of the state.
Melek explained that Colorado’s all-payers claims database was an important resource for the project: it provided detailed membership and claims data
___________________
22 For more information, see https://www.colorado.gov/pacific/healthinnovation/what-sim (accessed June 26, 2020).
for inpatient facilities, outpatient facilities, professional services, ancillary services, and prescriptions—essentially all health care costs per person. In addition, each record was attributed to each patient’s primary care provider, which allowed the assessment team to identify each practice’s pool of patients and follow how health care costs and use for those patients varied over time. The analysis team used these data to prepare reports for the practices that gave the primary care providers a picture of what their patients were doing outside the clinic, such as when they were using the ED and whether they were filling their prescriptions or being readmitted to the hospital. These reports also included the costs associated with those activities occurring outside of the practice.
Melek noted that the CMMI grant came with three requirements: (1) the project would produce a positive return on investment, (2) the effort would be sustainable once the grant ended, and (3) it would be scalable beyond Colorado. CMMI also wanted the practice reports to include annual member out-of-pocket spending per attributed member and the allowed cost per member per month for the attributed population. These were key metrics for the practices to be able to see and compare how they were doing with other practices, said Melek. The figures were also adjusted for risk scores, as calculated by the Milliman Advanced Risk Adjuster,23 so that each practice could see how its patients compared to those of other practices. Other metrics CMMI wanted in the practice reports were ED use rates, admissions, and readmissions for both physical and behavioral health issues and follow-ups after hospitalization for a mental health problem. “We thought there were good metrics, but we did not think these metrics gave the practices enough information,” said Melek.
To address that issue, he and his team included cost and use in the quarterly practice reports that incorporated information such as per member per month cost by service category (e.g., ambulances, emergency services, hospice, home health care, inpatient/outpatient hospitals, skilled nursing facilities), ED costs, specialty physician and primary care physician use, and both medical and psychotropic prescriptions. The practices could then use these reports to track their performance over time, review which types of services were experiencing increasing or decreasing costs, and compare individual practice results to those of mixed primary care, pediatric, and internal medicine practice results. The reports also included risk scores by business line and were able to inform cost projections, cost savings, and return on investment. Melek emphasized that the goal of this project was to increase certain cost categories and decrease others, with the end goal of bending the health care cost curve and saving money.
___________________
23 Additional information is available at http://www.milliman.com/mara (accessed November 15, 2019).
Melek and his team calculated separate returns on investment for commercial, Medicaid, and Medicare payers at the request of the practices and also included fee-for-service Medicare and Medicare Advantage plans. There were certain adjustments to the data, such as excluding patients with more than $250,000 of health care expenditures in 1 year and only including patients with at least 6 months of eligibility. According to Melek, the expectations were that there would be reductions in costs associated with inpatient behavioral and physical care, ED and ambulance use, skilled nursing facility use, and increased spending on primary and specialty medical profession services, behavioral services, diagnostic testing, and prescriptions. Preliminary draft projections showed that the program would save $17 million in the first year, $42 million in the second year, and $67 million in the third year. Broken down by patient, the goal was to save about $1.90 per member per month by making integrated care available to 80 percent of all people living in Colorado.
Melek noted that practices did not receive a great deal of money—no more than $5,000 each—but they did receive practice transformation support, actuarial reporting, and support in the field through public health agencies. Some practices received infrastructure support, such as laying cable in frontier areas so they could access high-speed Internet. Melek noted that practices were added to the program in cohorts.
Melek shared that for the first cohort of 100, primary care practices and the community mental health centers combined saved $47 million in the first year and $114 million in the second year. The results from the second cohort were not as positive, which Melek attributed to the fact that the practices selected for the first cohort were well prepared and ready to transition to an integrated care system, whereas subsequent cohorts needed more help transforming their practices. Nonetheless, preliminary data showed that the second cohort saved $16 million in the first year despite a nearly $28 million increase in spending for Medicaid patients, which likely reflects the elevated level of need for this patient group. He also noted that the program was unable to break even with the pediatric population, while the community mental health centers saved $25 million over 2 years.
Contributors to the positive return on investment included reductions in inpatient hospital admissions and ED use. While prescription drug costs increased, Melek noted that that was deemed acceptable because it indicated patients were complying with treatment plans. Readmission rates fell, producing a significant cost savings. According to Melek, in the end, the project was unable to spend the entire $65 million grant and still produced a combined projected savings through 2015 of $178.6 million, or approximately 4.5 percent of projected health care costs for the state. “That is in line with what effective and integrative programs have done in the last decade, and we are very pleased
that we can report results like that,” said Melek. In closing, Melek pointed out that Colorado has received an extension to conduct one more analysis in the spring of 2020, and the hope is that the results will be even better.
Discussion
Howard Goldman of the University of Maryland School of Medicine opened the discussion session by noting that the presentations in this session highlighted the importance of considering both the content of an intervention and the context in which it is delivered. He referred to earlier work that he and his colleagues had conducted, which surprisingly found that changing context might be necessary but was not sufficient (Goldman et al., 2002). However, changing the organization and financing of mental health services systems created an infrastructure that made it possible to implement high-quality services. In Goldman’s view, it is that balance between context and delivering high-quality services that will be key to moving forward. Beidas commented that all of these pieces are interrelated; infrastructure, organizational culture, and having trained clinicians all act as enablers of delivering high-quality services. “No one thing is going to be the silver bullet to transform mental health care,” said Beidas.
Both Melek and Haddad, responding to a question about early adopters of change, noted the importance of preparing an organization and its health care providers to make change before starting a transformation initiative. To Melek, this is why the first cohort in Colorado did so well right from the start, while the second cohort did not perform as well in its first year. Haddad said he has also seen that early adopter clinics had already primed themselves for change and were ready to hit the ground running.
Stoller, referring to the suggestions to liberalize buprenorphine prescribing and eliminate waiver trainings, noted that there has recently been an increase in waiver trainings. According to Stoller, there are approximately 76,000 waivered practitioners in the United States (SAMHSA, 2019) who, in theory, could treat more than 4 million people—or about twice as many people with OUD. In his opioid treatment program, about 28 percent of the patients are misusing buprenorphine, which he said is a reason to be cautious about instituting a new policy at a desperate moment that might have unintended consequences. Haddad noted that at least some of the requirements for prescribing buprenorphine or methadone do create barriers to care.
LUNCHEON DISCUSSIONS
Over lunch, workshop participants gathered and discussed the first two sessions. At the end of the first day, St. George and Greenfield provided a brief summary of the luncheon discussions (see Box 4).
KEY LEARNINGS FROM DAY ONE OF THE WORKSHOP
To conclude the first day of the workshop, participants were invited to comment on lessons they learned from the earlier sessions. Machtinger shared that he was impressed by the speakers’ emphasis on the importance of interdisciplinary team-based care—built largely on a nursing and social work model—that allows for connection as a means of delivering treatments that people want and need. He added that the difficulty is in how to shift away from the current health care system of 15-minute appointments, which conspires against that exact model of care.
Pomerantz noted the VA has found that investing more in low-cost care leads to big savings in high-cost care, but he is not sure this is the right investment to make. He explained that connecting more people to primary care can also lead to more people coming into the system who need a higher level of care and more intensive team-based services. “By increasing that engagement, are we increasing the amount of money being spent on mental health?” he asked. If so, that would not be a bad thing, as long as the goal is less about saving health plan dollars and more about saving the cost to society from untreated mental illness or SUDs.
St. George expressed concern that community mental health centers will become crowded and uncomfortable places to go over time. She added that in the past, she often felt that she had to recover from appointments for her mental health, because the environment was so stigmatizing compared to other health care environments. Stoller agreed with her concern, noting that sometimes conditions within contractual agreements can contribute to unwelcoming conditions in hospitals and clinics.
To summarize the discussions of the workshop’s first day, Margarita Alegría, a professor in the Departments of Medicine and Psychiatry at Harvard Medical School and the co-chair of the workshop planning committee, shared her takeaways from the day’s sessions:
- The importance of building delivery platforms that provide a continuum of care, recognizing that doing so will require making up for decades of underinvestment in the mental health care system;
- The critical role that interpersonal relationships play in delivering effective care and how frustrated and disappointed people are at a lack of improvements in this area—possibly due to emphasizing productivity rather than on getting to know and care about a patient;
- The potential to use new levers to transform the system, such as using employer benefits to emphasize greater access to and quality of mental health and substance use care;
- The significance of building a proficient organizational culture for implementation, including the importance of communication, coordination, and collaboration;
- The need to advance modular designs for evidence-based practices; and
- The importance of including the voices of people with lived experiences in developing programs, funding initiatives, and policies.
In closing the first day, Alegría noted that despite the challenges discussed during the workshop’s sessions, she felt optimistic that the field is starting to develop solutions for informed action.
USING DATA TO IMPROVE CARE SERVICE DELIVERY AND PATIENT OUTCOMES
To open the second day of the workshop, the session highlighted innovative practices to facilitate and optimize data collection, integration, and use. Alegría explained that this session would examine how to effectively use data to provide the most beneficial services.
Examining the Opioid Epidemic Using Linked Data in Massachusetts
Dana Bernson, the director of special analytic programs and public health sciences at the Massachusetts Department of Public Health, noted that the opioid epidemic in Massachusetts has followed the same trajectory as seen across the nation (see Figure 8).
The rate of opioid deaths, driven primarily by prescription opioids, remained fairly stable from 2000 to 2010, described Bernson, but deaths started rising in 2010, driven by an influx of heroin, which is less expensive.24 Bernson noted that the current fentanyl-driven third wave of the crisis, where overdose deaths have grown exponentially since 2015, has caused opioid-related overdose deaths in Massachusetts to reach twice the national average. “This is surprising because Massachusetts in usually at the top of every list of good health outcomes,” said Bernson. “This is not a place we are used to being.” She added that the number of nonfatal opioid-related incidents to which emergency medical services responded more than doubled between 2013 and 2015.25
Bernson explained that the Massachusetts Department of Public Health has more than 300 mostly unlinked, completely siloed data systems with little interoperability. Moreover, those systems were reporting data that were at least 1 year behind the on-the-ground situation. As a result, estimates of the extent of the crisis relied heavily on statistical modeling. Previously, data were largely accessed through static, online reports, with little opportunity for people outside of the department to study and explore the data and little idea of who was using the data, she explained. Bernson pointed out that “all of this meant that we had a limited ability to answer complex public health questions.”
It was in that context in 2015 that Massachusetts’s governor Charlie Baker signed legislation (known as “Chapter 55”) that eliminated some of the barriers to data sharing and created a sense of urgency around data sharing and access problems, explained Bernson. She noted that the legislation required the Department of Public Health to collect data across state government and answer seven questions posed by the legislature—all within 1 year and without additional funding. Bernson and her colleagues approached the problem by breaking it down into three domains—differing legal requirements, data considerations, and information technology architecture—that they needed to tackle simultaneously. She noted that they needed to find compliance solutions that were applicable across these three domains.
Bernson pointed out that one unusual step her team took was to develop data agreements that went above and beyond legal requirements as a way
___________________
24 For more information, see mass.gov/dph (accessed April 23, 2020).
25 For more information, see mass.gov/dph (accessed April 23, 2020).
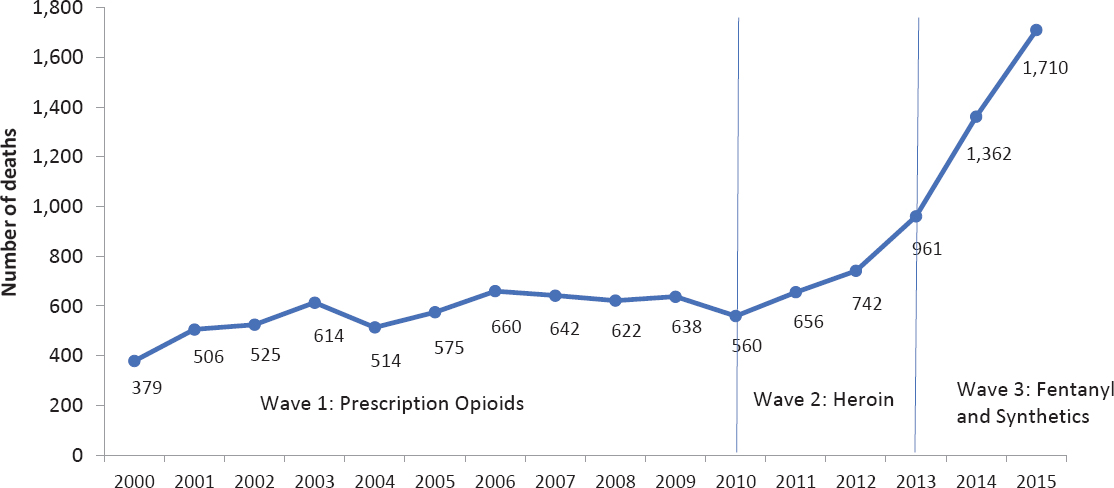
SOURCES: As presented by Dana Bernson, October 16, 2019; Massachusetts Department of Public Health: mass.gov/dph (accessed January 14, 2020).
to get quick buy-in to the process from the agencies that would be providing the data. “We did not have a lot of time to do this, so we really had to make agencies that would be providing data feel as comfortable as possible with us holding their data,” explained Bernson. She noted that data security entailed hand-delivering data on encrypted hard drives and encrypting the data throughout the input and storage process. She and her colleagues also created a complicated data linkage process that splits files, so that identifiers and analytic data are never stored within the same file, creating an environment where analysts could not see individual-level data, only aggregate de-identified data. Temporary work files were also deleted at the end of a session. All data operations are fully audited, she added.
The health department’s team managed to meet its deadline, provide data on opioid overdoses, and answer the seven questions. The team decided to conduct four additional analyses to highlight the importance of using linked data to understand the epidemic, which led to the program being reauthorized and expanded to allow the department to approve more than 20 projects with external collaborators. “We knew we had more data than we had capacity to analyze in-house in the department,” said Bernson, “so we invited people to come in and give us a hand.”
Today, the Massachusetts Department of Public Health’s data system pulls together traditional public health datasets, all-payer medical claims data, and hospitalization data, as well as data provided by public safety, criminal justice, and other state agencies. Bernson noted that the all-payer claims database covers about 98 percent of the state’s population, which enables the system to provide accurate analysis of the problem as a percentage of that population—complete with demographic information and the ability to compare different populations in the state.
Once again, the state legislature was impressed with the results of the project, and in 2017, it permanently authorized establishing a public health data warehouse, which created the opportunity to use data-driven public health methods to analyze state population health trends for the first time. Bernson pointed out that the legislature’s actions resulted from an iterative process of proving the health department’s trustworthiness when it came to handling data.
Going forward, Bernson’s team is expanding the data warehouse to address not only the opioid crisis but other important public health issues, including disparities in maternal and child health care. The health department is also adding data to look at the intersection of infectious diseases and the opioid epidemic and data on the social determinants of health to better understand pressing issues, such as food insecurity and housing instability in the state.
In terms of what the data reveal about the opioid crisis in Massachusetts, Bernson said key findings were that the prevalence of OUD was 4.6 percent
among people 11 years or older in 2015 and that the number of individuals with OUD is likely increasing, particularly among young people (Barocas et al., 2018). The data also revealed that the proportion of this population dying from opioid-related overdoses has nearly doubled between 2011 and 2015. Bernson emphasized that understanding the size of the population at risk for opioid-related harms helps the health department allocate resources and appropriately plan and implement prevention, treatment, and recovery services.
Another important finding that Bernson shared was that few individuals who had a nonfatal overdose received MAT for their OUD, though for those that did, the risk of death was cut in half (Larochelle et al., 2018). As a result, clinicians are now receiving funding to provide MAT, and the health department is working with the state’s medical schools to change the curriculum to emphasize the value of MAT for OUD. The state has also created a commission to study the impact and outcomes of MAT.
Bernson shared that the data indicate the rate of opioid-related overdose deaths in the state is 120 times higher among individuals released from incarceration, with most of those deaths within the first month of release (Joudrey et al., 2019). This finding led to legislation that requires 7 of the state’s 14 county jails and a few department of corrections facilities to provide medications for OUD. In closing, Bernson pointed out that the state’s rate of opioid overdose deaths has significantly stabilized. “We are hopeful that some of it is because of recent policy changes that were a result of some of this work,” observed Bernson. She added that “I think it is a great way to highlight how we can actually see data directly relate to policy change and outcomes.”
Advances in Mental Health Measurement
Robert Gibbons, the Blum-Riese Professor of Biostatistics in the Departments of Medicine and Public Health Sciences and the director for the Center for Health Statistics at the University of Chicago, opened his presentation by pointing out that a new approach to screening and measurement of mental health disorders, SUDs, and suicidality can dramatically increase the precision of measurement, eliminate the clinician’s burden of measurement, and decrease the burden to a particular individual. Given the power of the Internet and today’s computers, it would be possible, Gibbons added, to screen the entire U.S. population in a single day using a mere 300 servers.
Measurement is the process of obtaining the magnitude of a quantity relative to an agreed-upon standard, which is not always available, explained Gibbons. In contrast to the physical sciences, where we know the truth (e.g., a true concentration in an analytical chemistry experiment), in mental health our interest is in unobservable or “latent” variables, which require us
to infer truth from a series of manifest symptoms. To obtain valid and reliable measurements researchers must ask many more questions of patients than is feasible or desirable. Gibbons noted that complex diseases, such as depression or anxiety, are inherently multi-dimensional, requiring the use of more complicated measurement models than are typically used in educational measurement. To reduce patient burden, we can use computerized adaptive testing (CAT). CAT, which determines what question to ask based on the answer to the preceding questions, rather than having every individual answer every question in an assessment tool. The items can thus vary in content and number from person to person. Gibbons noted that the paradigm shift is from traditional fixed length tests that fix the items and allow measurement precision to vary to adaptive tests that fix the precision of measurement and allow the items to vary.
Gibbons described how he and his collaborators developed the CAT-mental health (CAT-MH) suite of nearly 15 computerized adaptive tests based on multi-dimensional item response theory. As one example, the depression test in the CAT-MH allows for extracting information from 400 items meant to assess depression symptoms using an average of 10 adaptively administered items, while maintaining a correlation of r = 0.95 with the 400-item test score (Gibbons and deGruy, 2019; Gibbons and Hedeker, 1992; Gibbons et al., 2007; Graham et al., 2019). This is a paradigm shift from previous attempts to create a fixed-length tool that can apply to many people, such as the Patient Health Questionnaire-9 for depression severity. “As such, we can dramatically increase precision while eliminating clinician burden and minimizing subject burden,” said Gibbons. A similar suite has extended this technology to the assessment of children, with modules for both children and their parents (Gibbons et al., 2019), he added.
Gibbons detailed the advantages of adaptive testing:
- Adaptive tests provide constant precision of measurement throughout the entire severity continuum for any measured disorder.
- Items are targeted to a patient’s specific level of severity at that point in time.
- Adaptive tests ask different questions upon repeat administration, eliminating response bias produced by repeatedly asking the same questions.
- The CAT-MH has been validated against structured clinical diagnostic interviews, so it can also provide diagnostic profiles for a large number of disorders and suicide risk.
- The CAT-MH can be used for both screening and measurement.
- Adaptive tests are ideal for longitudinal assessments essential for measurement-based care.
- Adaptive tests estimate not only the severity of a disorder but the uncertainty in that severity score and measure all patients to the same level of precision.
- Adaptive tests can also characterize the critical threshold for various treatment options.
- The CAT-MH is scalable to any size population via a Health Information Portability and Accountability Act secure cloud-based platform. Patients can be screened, measured, and monitored in or out of the clinic.
- The CAT-MH can be fully integrated into the electronic health record, and Gibbons’s team has developed clinical workflows for integrated behavioral health and primary care practices and clinics.
Gibbons and his collaborators have also developed the first computerized adaptive diagnostic scale, which takes 36 seconds to administer and achieves a sensitivity and specificity nearly matching that of an hour-long, face-to-face diagnostic interview (Gibbons et al., 2013). As an example, his team administers this test to perinatal women every week during pregnancy and the postpartum period to determine the earliest onset of perinatal depression. They then administer an instrument with more dimensional measures to characterize the nature of the disorder. This test has also been used to assess treatment response to patients using deep brain stimulation to treat their depression at home (Sani et al., 2017).
Gibbons’s team has also used this approach to screen 1,000 individuals who came to the University of Chicago’s ED for a non-psychiatric issue. According to Gibbons, approximately 22 percent screened positive for major depressive disorder, with 7 percent in the moderate to severe range and in need of immediate treatment and 3 percent at serious risk of attempting suicide. None of the latter were identified by ED staff, said Gibbons. Importantly, he said, individuals with scores in the moderate to severe range had a threefold increase in ED visits over the next year and a fourfold increase in hospitalizations. “These are super utilizers, and it took us 2 minutes to figure out who they were,” said Gibbons. He noted that a Spanish version of the test produces similar results in Latinx populations.
Gibbons explained that CAT-MH assessments have been validated and are now used to measure depression, anxiety, mania and hypomania, suicidality, PTSD, substance use, and psychosis in adults. In one application, for example, CAT-MH was used to screen a freshman class of 6,000 students at the University of California, Los Angeles, and it found that 4 percent were at serious suicide risk. Students with mild to moderate depression and anxiety who were not suicidal were referred to Internet-based cognitive behavioral therapy and a peer counseling network. More severely ill students were sent to the ED, student health, or the Department of Psychiatry depending on the
time of day they remotely took the tests. Suicidal students were immediately contacted by a suicide hotline and triaged to treatment. The Chicago team is also validating the CAT-MH for assessing borderline personality disorder, functional impairment, quality of life, and functional status and well-being in cancer patients and survivors. For perinatal applications, CAT-MH has been validated and is in use for diagnosing depression, anxiety, mania, and hypomania, while in children, it has been validated and is in use for diagnosing depression, anxiety, mania and hypomania, attention-deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, and suicidality. The instrument is also being validated for autism spectrum disorder in children.
In closing, Gibbons listed a few example applications of CAT:
- Screening 1.8 million Los Angeles residents to develop a registry of 100,000 patients,
- Surveying the state of Indiana for SUD,
- Perinatal depression screening and follow-up at the NorthShore University HealthSystem, and
- Large-scale national survey of prevalence of mental illness and SUD in the U.S. adult population.
He concluded his presentation by noting that “we spend billions of dollars on biological measurement, yet we validate those using Stone Age clinical measurements. We can do so much better.”
Achieving Population Well-Being Through Mental Health Integration and Team-Based Care
Brenda Reiss-Brennan, the former director of mental health integration at Intermountain Healthcare and now the chief clinical science officer at Alluceo, opened her remarks by sharing that Intermountain participated in the surgeon general’s first meeting on integrating primary care and mental health in 2000. She pointed out that it was at that same time that Intermountain began developing the first care process models for depression, suicidality, substance use, and diabetes. Reiss-Brennan noted that through her work, she aims to normalize mental health as a growing health priority that affects a significant proportion of adults and carries with it a significant cost: annual costs are estimated to reach $280 billion by 2020, which makes it the costliest medical condition in the United States (SAMHSA, 2014).
Citing a definition offered by David Satcher when he was the U.S. Surgeon General, Reiss-Brennan said “mental health is a state of successful performance of mental and physical functioning, resulting in productive activities, fulfilling relationships with others, and the ability to adapt to change and cope with
adversity” (HHS, 1999). Team-based mental health integration, she added, focuses on prevention and access by normalizing mental and behavioral health care as routine medical care through unified connected team interactions.
Reiss-Brennan explained that when she first started working at Intermountain, she convinced management that they did not need a new approach to address mental health. She argued instead that the goal should be to treat it as a chronic disease that could be mapped onto all other chronic diseases. In this way, approximately two-thirds of patients could be cared for routinely in primary care, with the remainder requiring additional assistance and education or referral to specialty care.
To implement this approach, Reiss-Brennan explained, she and her colleagues examined the lived experiences of people trying to care for patients and family members suffering with mental health and social issues in the context of primary care. In clinics without team-based care and support, clinicians felt forced to address these issues in isolation, while patients also felt isolated and alone with their problems—perhaps getting medications but little help dealing with their depression or other MHSUDs, described Reiss-Brennan. This was not the case for clinics with high-performing teams, however, where patients reported being treated as a whole person by a team to which they felt connected and on the same page with in terms of their condition and treatment.
Building high-performing teams takes a great deal of effort on the part of everyone involved to facilitate this process, Reiss-Brennan and her team developed a playbook that defines the roles of every team member. “When everybody knows everybody else’s role, you get high-performing teams,” she explained. Beyond the playbook, she noted there are five factors essential to integrating and normalizing mental health as part of primary care:
- Leadership and culture, with champions establishing a core value of accountable and cooperative relationships;
- Clinical workflow that engages patients and families on the team and matches their complexity and need to the right level of support;
- Information systems, including electronic health records, enterprise data warehouses, registries, and dashboards to support team communication and outcome tracking;
- Financing and operations that can project, budget, and sustain team full-time equivalents to measure return on investment; and
- Identifying community partners who can help engage the population in sustaining wellness.
Reiss-Brennan noted that Intermountain is standardizing a clinical operational team relational process that incorporates mental health as a comple-
mentary component of wellness and healing. “We have taken clinical decision making and organized it in a way to understand complexity, not just conditions,” she explained. She added that the process looks to identify “the combined effects of mild, moderate, and high complexity so that you can really allocate the right level of team resources and use the strengths of the patients and families to provide some of the support that we need.”
Intermountain’s data systems enabled Reiss-Brennan and her colleagues to explore the impact of high-performing teams that acculturated the five key components on cost, use, and patient experience. Reiss-Brennan noted that between 2003 and 2013, 113,000 members received care from one of Intermountain’s 27 high-performing teams.26 These members were screened for depression; a positive screen activated the depression care process model that helped patients self-manage their condition and avoid ED use and hospitalization. Reiss-Brennan shared that the cost of providing team-based care was $22.19 per year and total savings from use of these teams equaled $115 per patient per year (Reiss-Brennan et al., 2016). She recounted that when Intermountain’s chief financial officer saw these results, the first question was why there were only 27 integrated care teams, given the return on investment. The answer, she said, is that implementation is difficult and requires intensive human resources.
Reiss-Brennan’s team found that integrating mental and physical health through primary care teams resulted in better clinical outcomes and lower costs. For example, the cost of ED visits was 23 percent lower, while hospital admissions fell 10.6 percent, primary care encounters were reduced by 7 percent, and payments to health care providers dropped 3.3 percent (Reiss-Brennan et al., 2016). Nearly twice as many members were screened for depression compared to those seen in traditional practice management medical practices, and more than five times as many members had documented self-care plans. She noted that once the results of this study were published, there was rapid adoption and routinization of integrated mental and physical health in the context of primary care across the Intermountain system.
In closing, Reiss-Brennan described some of the lessons she has learned:
- Lead with passion;
- Embrace complexity;
- Understand risk;
- Understand where a project is heading;
- Do not fear bringing patients, families, and other people into the conversation; and
- Develop meaningful innovations that make people’s lives different and better and that leave clinicians feeling good about what they are doing.
___________________
26 For more information, see https://intermountainhealthcare.org (accessed April 23, 2020).
Reiss-Brennan stressed that any innovations should show strategic value over time, and demonstrating that requires good measurement and data systems. In her final remark, Reiss-Brennan reminded workshop attendees that “normalizing mental health is all of our business.”
Adapting a Data Infrastructure to Address the Opioid Epidemic in Camden, New Jersey
Dawn Wiest, the co-director for data and quality improvement at the Camden Coalition of Healthcare Providers, explained that the coalition has worked together with its hospital partners, primary care providers, behavioral health providers, and social services providers in Camden, and increasingly throughout southern New Jersey, to build a model of care for people who have complex health and social needs. This practice, referred to as “health care hotspotting,” evolved in response to clinical observations and internal data analysis showing that the highest need patients had the most frequent emergency room visits and hospital admissions, with 1 percent of the patients accounting for 30 percent of hospital costs in Camden.
To put the coalition’s work in context, Wiest explained that approximately 30 percent of the city’s residents live below the poverty line and 57 percent are covered by Medicaid (Wiest et al., 2019). The median household income in Camden in 2019 was $26,000, compared to $76,000 for all of New Jersey (Wiest et al., 2019). Wiest further explained that the coalition’s primary form of intervention, the Camden Core Model,27 identifies patients who would most benefit from a wraparound care management intervention. The model engages patients in care planning beginning at the hospital and provides them with community-based care management after discharge from the hospital that includes home visits and medicine reconciliation and accompaniment to primary care and specialist visits within 7 days of hospital discharge (Noonan and Craig, 2019).
Wiest described the elements of a framework in which the coalition operates, known as the COACH model28:
- Connect tasks with vision and priorities,
- Observe the normal routine,
- Assume a coaching style,
- Create a care plan, and
- Highlight progress with data.
___________________
27 Additional information is available at https://camdenhealth.org/care-interventions/camden-core-model (accessed November 18, 2019).
28 For more information, see https://camdenhealth.org/the-coach-model (accessed December 3, 2019).
The tenets of care include using motivational interviewing, providing trauma-informed care, and developing authentic healing relationships that are patient centered, strength based, and focused on harm reduction, with accompaniment serving as a foundational aspect of the coalition’s work. Wiest explained that “accompaniment—being able to work with a person to build their confidence and ability to navigate complex systems on their own—has become important because many of the people we work with have to engage multiple systems … that often serve to re-traumatize people.”
Wiest noted that when the coalition started working with this high-need population, it became clear that while the medical issue is extremely important, these individuals face many more relevant areas of need, such as food, housing, and transportation (see Figure 9). Wiest explained that patients themselves often listed their medical issue as their second or third most pressing problem, with issues such as reconnecting with family, finding a job, and obtaining identification being more important. “Our model of care is built on figuring out how to work with people in the community to connect people to the services that they need so that they can build that life or rebuild that life that they see as being important to them,” said Wiest.
In describing the data structure that is integral to the coalition’s work, Wiest identified the system’s three most important components as (1) a real-time, vendor-managed health information exchange; (2) a user-customizable,
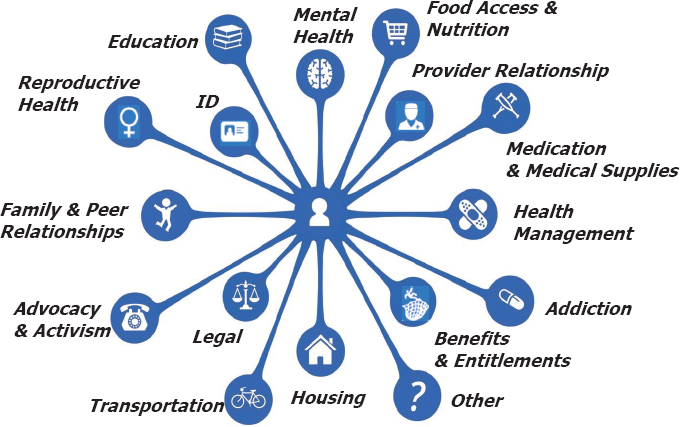
SOURCE: As presented by Dawn Wiest, October 16, 2019.
vendor-hosted internal performance and care tracking system that also uses data to identify areas for quality improvement; and (3) a homegrown database for research, evaluation, and quality improvement and longitudinal analysis of outcomes. Wiest added that this database includes administrative data from an all-payer claims database, the criminal justice system, and social services partners.
Wiest and her colleagues have been working closely with Camden’s partners to draw more attention to the issue of untreated SUD in the context of the opioid epidemic. They have been advocating for policy change at the state level and have helped health care providers in the city redesign their workflows to bring patients into their office within 7 days after hospital discharge and to better identify patients who are at risk for substance use or complications related to it. An important component is the 7-Day Pledge initiative started in 2014 to address barriers to timely follow-up in primary care. Thirteen practices in the city, including sole practitioners, federally qualified health centers, and health-system-affiliated practices pledged to open appointment slots for patients recently discharged from the hospital. Evaluation of this initiative found that patients who connected with primary care within the 7 days had fewer 30- and 90-day readmissions compared to similar patients with a later or no primary care appointment (Wiest et al., 2019).
The coalition also found that 50 percent of Camden Core Model patients had an active SUD, with 21 percent using opioids at the time of engagement with the model (Rentas et al., 2019). Analysis of patient data provides a picture of a patient’s trajectory across multiple systems and enables the coalition team to identify whether a person was housed or living on the street, for example, and to identify opportunities for health care providers, the police, and other agencies to intervene in a way that would have changed the trajectory of the person’s life. Coalition staff are now working on ways that will allow clinicians to use their health information exchange system to see when they have a patient coming in who is at risk of opioid use and potential overdose.
Discussion
In the discussion session following the speakers’ presentations, Mallory Rapalyea from the Coalition for Disability Health Equity asked how the CAT-MH instrument adjusts for cultural differences. Gibbons replied that using a technology called “differential item functioning,” he can compare the results from different subpopulations (after 500–1,000 individuals in a sub-population have been assessed) and determine which 5–10 percent of the items are culturally biased and no longer good discriminators. He noted that his team has recently developed a version of CAT-MH for criminal justice populations.
Gisela Rots from the Education Development Center commented on the importance of considering the social determinants of health when thinking
about integrating prevention efforts into primary care, which she said seems like a good opportunity for a positive return on investment as well as treating wellness more generally beyond a focus on mental health disorders. Her question for the panelists was how her organization can work with theirs to make the case for including prevention in system change efforts. Bernson replied that the Massachusetts Department of Public Health has been trying to focus further upstream on prevention and noted that it is harder to collect data pertinent to prevention. She added that intervening early is a form of prevention, and the data her department collects do enable identification of populations most at risk and can therefore inform early intervention. Reiss-Brennan said her organization has saved money by going upstream to proactively identify chronic diseases and treat them early. She added that data are providing leads that enable clinical staff to reach out to patients in their homes, before they reach the clinic. “There is so much that patients and families can do in their homes to begin to start thinking about their wellness and their care,” said Reiss-Brennan.
Wiest commented that the Camden Coalition is now working with the local school system to develop an algorithm to better identify students who are at risk for homelessness or currently homeless. Gibbons noted the importance of moving from a passive data collection process to a more active one. For example, perinatal depression is the only form of a mental health disorder that has a narrow period of onset. “We know when it happens, so let us proactively measure pregnant women every week to see when is the earliest time that we can identify it and then be able to treat it before it gets bad,” said Gibbons. His team is working with the state of California to assess the entire community college system, where 20 percent of the students are estimated to be homeless.29 “We can get prospective measurements in terms of their mental health and their well-being and be able to intervene before they become suicidal,” said Gibbons.
Responding to a question from Guerra as to whether she has had interactions with other state public health departments, Bernson replied that she not only talks to other state health departments almost every week but has been a vocal advocate for developing and using this type of data system. In fact, Massachusetts is now part of a multi-state grant with Kentucky, New York, and Ohio to help those states create a similar system. She also shares the data use agreements her team had developed to guide other state health departments.
Colleen Barry from Johns Hopkins University asked Reiss-Brennan how one can take the lessons learned from her work at Intermountain—a unique delivery system—and use them to inform individual primary care providers within the community or smaller systems that are not as well equipped
___________________
29 For more information, see https://www.latimes.com/local/education/higher-ed/la-polca-community-college-homeless-students-20190307-story.html (accessed April 23, 2020).
to create care teams and make them work. Reiss-Brennan replied that her team has been able to build out the five key components in communities in Kentucky and Mississippi. While these systems may not be able to do everything Intermountain does, they are asked to think about culture change and identify the tasks they can accomplish. She noted that other systems have made this approach work, so the real challenge is to identify what is missing at a policy level to build those five key components for individual practitioners and small clinics.
Barry also asked Reiss-Brennan if there were lessons from Intermountain’s work on mental health that could be related to treating SUDs in primary care. Reiss-Brennan responded that Intermountain treats SUDs as one of its chronic diseases, and so it screens patients for substance use and social determinants. However, even though Intermountain has a care process model for SUDs, it has been difficult to integrate with care for depression and anxiety, for example, because of the stigma associated with SUD. While the system’s primary care providers have taken on mental health care as part of normal care and are champions for that work, they are at a loss when it comes to dealing with SUD. “I think the beginning part is to get an expert on the team that is actually able to coach them and train them and build their confidence about substance use,” observed Reiss-Brennan.
Captain Michael Colston from the U.S. Department of Defense (DoD) commented that DoD, even with its enormous databases, cannot find a good measuring point for suicide and mental health, and asked Gibbons about CAT implementation. Gibbons replied that he and collaborator Cheryl King at the University of Michigan built a crosswalk among bullying, PTSD, symptoms of depression, anxiety, and mania and mapped those onto suicidality for children and adolescents in pediatric EDs. For adults, they used the existing CAT-MH 1,008-item bank for depression, anxiety, and mania to identify 100 items that are precursors to the emergence of suicidality. When combined with an additional 11 items for which they had data on passive and active suicidality, the instrument could pick up suicidality in people who are yet to become suicidal or realize that they are suicidal and then take preventive steps.
Gibbons explained that for the DoD’s Wingman Project, the CAT suicide measure has been used to identify those individuals who may be reluctant to talk about suicidal thoughts and behavior but are willing to share feelings about hopelessness, helplessness, and anhedonia30—all precursors of suicide. “I think that kind of covering of the continuum and being able to measure people just as precisely at the low ends of the clinical scale as in the high ends of this clinical scale are going to help in terms of our ability to predict future suicidal behavior,” said Gibbons.
___________________
30 Anhedonia is defined as the inability to feel pleasure.
Karen Drexler from the VA asked if the CAT has been integrated into the Cerner electronic health record. Gibbons said that they have developed an application programming interface that has been used to integrate the CAT-MH into several electronic record systems and integration to Cerner is under way. He noted that integrating the CAT into the Epic electronic health record system takes 2 weeks of major effort; to make that experience easier, his team has designed transportable workflows, a manual, and a video that walks users through how to use the CAT in the primary care workflow.
Reiss-Brennan commented that Intermountain has changed its thinking about suicide prevention. “We are hearing from the community and from people working on [suicide] that it is not going to be solved in the medical setting and that it is a community problem, a social health problem, and a public health problem,” she said. Addressing the suicide epidemic will require education and building awareness throughout the entire population about what is happening, what its causes are, and what can be done in the community to prevent suicide, she added.
Pomerantz, referring to the one-sixth of Intermountain’s primary care patients who need specialty mental health services, asked Reiss-Brennan how the health system keeps those individuals connected to primary care given that they are also at the highest risk for negative health outcomes beyond their mental illness. Reiss-Brennan replied that those individuals receive their services from specialists who work within the extended primary care team. She emphasized that Intermountain is concerned about all chronic illnesses, so along with mental health specialists, there are endocrinologists, cardiologists, and other specialists working at the highest scope of their licenses contributing to the primary care team approach. There are some individuals who, after consulting with the entire team (including the care manager), are transitioned to the appropriate inpatient setting until they are stabilized—at which point, they can return to primary care. The key, said Reiss-Brennan, is embracing the complexity with which some patients present and using the same team-based approach to address that complexity.
DEVELOPING THE WORKFORCE FOR INTEGRATED CARE
To start the workshop’s final session, Thomas Engels, the acting administrator at HRSA, noted the essential role of the workforce in addressing the needs of individuals living with mental health or substance use disorders, whether in a primary care or specialty behavioral health setting. “Clearly, you cannot have access to care and you cannot implement best practices without an adequately trained and available workforce,” said Engels.
Looking at today’s behavioral health workforce, the critical question, said Engels, is whether the nation has a sufficient supply where it is needed.
He pointed out that addressing the supply and distribution of the workforce, particularly in underserved communities, is part of HRSA’s core mission, and doing so will require being creative with how the workforce is deployed and used. Focusing on recruitment and retention will be important to meeting workforce demands, as will incorporating more peers and community health workers and fully embracing telemedicine.
The State of the Nation’s Behavioral Health Workforce
Michelle Washko, the director of the National Center for Health Workforce Analysis at HRSA, shared that approximately 18 percent of the adult U.S. population suffered from a mental health disorder, and an estimated 1.8 million people misused opioids in 2016 (SAMHSA, 2017). She noted that beyond the direct toll on individuals and families, mental illness and SUDs are well-established drivers of disability, mortality, and health care cost. “Behavioral and mental well-being is essential to overall health, yet serious challenges exist in providing behavioral health care services to the U.S. population at large,” said Washko.
Addressing the size, location, composition, capacity, and quality of the behavioral health services workforce is increasingly important to improving overall population health, said Washko, with sufficiency and maldistribution complicating the behavioral health landscape. Those two factors, she said, constrain access to essential care and treatment for millions of individuals.
The behavioral health workforce is a diverse group of health care and health support occupations, but Washko explained that currently there is no consensus as to who is included. Psychologists, psychiatrists, clinical social workers, marriage and family therapists, and other professionals with advanced degrees are considered core mental health professionals. There are, however, other occupations that provide care for those seeking behavioral health prevention or maintenance services, including peer providers and community health workers, and they have varying levels of education and training.
It was within this complex workforce context that the 21st Century Cures Act31 mandated that HRSA, in consultation with SAMHSA, produce workforce projections for select behavioral health occupations. Published in 2018, these projections32 include psychiatrists, psychologists, several types of counselors and therapists, social workers, and select primary care providers. The key finding of this analysis was that barring major shifts in the use of behavioral
___________________
31 For more information, see https://www.fda.gov/regulatory-information/selected-amendments-fdc-act/21st-century-cures-act (accessed December 3, 2019).
32 For more information, see https://bhw.hrsa.gov/health-workforce-analysis/research/projections/behavioral-health-workforce-projections (accessed December 4, 2019).
health services, there will be shortages of workers for several of these occupations by 2030, including adult psychiatrists, addiction counselors, and mental health and school counselors. As Washko stated, all indicators are pointing toward increasing use of behavioral health services in the future.
While workforce shortages are an obvious concern, maldistribution is the more critical issue, according to Washko. As part of the 21st Century Cures Act analysis, her team found severe maldistribution trends for several behavioral health occupations. “Unfortunately, this is not uncommon for health care occupations,” said Washko, “and it is perhaps more a factor of complex socioeconomic determinants that push and pull an individual to live and work in a given geographic area.” As a result, she said, building, redistributing, and reshaping the behavioral health workforce must be aligned with other efforts to address the social determinants of health and improve overall delivery of mental health and SUD services. Toward that end, the behavioral health field must move toward improved coordination and integration with not only primary care but specialty emergency and rehabilitation care settings. At the same time, she added, the nation must push for continual improvement of workforce quality by encouraging the development of cutting-edge curricula, trainings for work in various specialty settings, and unique treatments for specific populations, such as the prison and homeless populations.
Assessing and Expanding the Clinical Workforce for Treating Substance Use Disorder in Colorado
Colorado, like most states in the nation, is experiencing an epidemic of SUD, said Steve Holloway, the branch chief of the Colorado Department of Public Health and Environment’s Health Access Branch. While Colorado has a reputation for a healthy population, the state has higher rates of substance use, suicide, and poor access to behavioral health services than the national average. He noted that although Colorado has been a leader in the recreational use of cannabis, recent data suggest that legalizing recreational cannabis did not have a positive or negative relationship to the escalation of the opioid epidemic (Flexon et al., 2019).
In response to the opioid epidemic, the Colorado legislature convened a committee in 2018 to examine various policy options to deal with opioid misuse and other SUDs, ranging from changing Medicaid reimbursement to enabling safe injection sites. Holloway explained that legislation resulting from this study required his agency to improve the assessment of the state’s SUD workforce, expand practice incentives for health care providers, and add a scholarship program to its existing loan repayment program—the single largest state-based loan repayment program in the country, with more than $10.6 million per year available—for certified addiction counselors. He noted
that the state has about $3 million in private funding in addition to state appropriations.
Holloway described a number of challenges to assessing the workforce. In Holloway’s view, the quality of the data is not high and the data change quickly. In Colorado, for example, his team has detected a change of as much as 2.5 percent per month in the state’s workforce datasets—which means that a dataset that is accurate today will be off by about one-third in 12 months. Holloway also pointed out that much of the available data are segregated in narrow purpose-built data systems and that commercial solutions tend to be limited in scope, expensive, and unable to be shared with partners. Colorado’s approach has been to aggregate data with a purpose-built solution. “We looked across multiple datasets to try and answer the question of who the providers are, what places they are providing that care, and what health plans are paying for those services,” said Holloway. According to Holloway, the resulting system will be able to accommodate up to 25 million information samples per year. Through a complex process of disaggregation and reassembly, the data in the Colorado system are now being queried and analyzed to assess the workforce at specific time points. The data can also be distributed through secure user interfaces that enable partners to benefit from this work.
A key challenge in working with the existing federal system of modeling SUD workforce demand, said Holloway, is that it assumes that demand is similar regardless of age or gender. In addition, health care provider information is often dependent on datasets that are less reliable in terms of identifying a provider’s location and use service areas defined by civil boundaries, which may or may not represent how people actually receive care. In addition, the current model does not represent regional variation or reliably stratify relative need. To address these shortcomings, Holloway and his collaborators first surveyed the approximately 17,600 health care providers with active licenses who met the definition of core SUD and mental health professionals. They also determined the average SUD encounter per provider per year for the nearly 13,000 providers who were actively practicing in the SUD treatment field (Bauer and Groneberg, 2016; Kanuganti et al., 2016; McGrail, 2012). Holloway explained that these data were useful for assessing the difference between those who were engaged in SUD treatment full time versus part time and between professions such as psychiatric nurse practitioners and physician assistants (Bauer and Groneberg, 2016; Kanuganti et al., 2016; McGrail, 2012).
Holloway described the process his team used to determine health care demand. Drawing on data from the National Survey on Drug Use and Health (which are stratified by age, sex, and specific SUD), the team applied a presumed prevalence rate to every census block group in the state. This rate was then converted into an encounter demand to measure how local capacity matches that demand by using the enhanced two-step floating catchment
area technique.33 The results of the initial analysis revealed “that only the top decile [of providers] is able to provide a minimum of eight encounters per person with an SUD,” said Holloway. He added that the number of minimum encounters may sound familiar to workshop participants, given that “some have suggested [it] is the minimally adequate treatment34 for a person with SUD.” A finer-grained analysis at the city level also reveals maldistribution issues that allows Holloway’s department to make discrete decisions about resource allocations and how to apply practice incentives.
In terms of identifying providers to receive incentives, Holloway explained that he and his colleagues look for providers who have demonstrated a commitment to meeting the needs of poorly served populations and graduated from a Colorado training program, because clinicians tend to practice in the state in which they were trained. They also look for prior experience working in rural or low-income communities, evidence that a provider has a commitment to learning about the needs of underserved populations, and letters of support from employers that address how retainable they think the provider will be. Holloway pointed out that Spanish language skills are a bonus that adds to both retention characteristics and a commitment to the state’s Spanish-speaking population. All of this information is designed to provide a predictor of how likely a provider will keep working in underserved areas once the loan repayment contract is fulfilled. Holloway noted that the program funded 73 new awards in its first year. These health care providers are predicted to engage in nearly 153,000 encounters over the 3-year contract.
In closing, Holloway explained that going forward, his group plans to advise policy makers and academic programs on training and workforce needs affecting the state and collaborate with state Medicaid and human services agencies on allocation of public resources, program coordination, mobile MAT, and network sufficiency assessments. The team plans to further develop the scholarship model to increase training capacity to respond to service demands and support community-initiated strategies to respond to treatment needs through philanthropic and federal grant making.
Nurse Care Manager Model for Office-Based Addiction Treatment
Colleen LaBelle, who oversees Office-Based Addiction Services at the Boston Medical Center, provided her perspective on the nurse care manager model for office-based addiction treatment. She explained that it began at
___________________
33 The two-step floating catchment area method was developed to measure spatial accessibility to primary care physicians.
34 For more information, see AHCPR (1993); APA (1998, 2000, 2002, 2004); and NCQA (1997).
the Boston Medical Center in 2003 with a pilot program designed to introduce office-based MAT to a primary care workforce that did not understand addiction. LaBelle stated that the program uses registered nurses working to the scope of their license to serve as the point of care providing complex care management in an outpatient practice.
LaBelle explained that when Massachusetts saw how effective this pilot program was at getting patients into and retaining them in treatment (Alford et al., 2011), it funded community health centers across the state to adopt this program with training and technical assistance from LaBelle and her colleagues. At first, not many health centers were interested, which LaBelle attributed to the stigma attached to SUDs. Over time, though, as the opioid epidemic became more problematic, the state increased funding and more health centers adopted the program.
Analyzing data from the 12-month period between July 1, 2016, and June 30, 2017, LaBelle’s team found that the nurse care manager program decreased hospitalizations, ED visits, and nights spent in detox (see Figure 10). The data also showed that this program improved patients’ lives and brought them back into the workforce. Between 2007 and 2019, state-funded sites have treated more than 20,600 patients (Alford et al., 2011).
LaBelle explained that initially, the program focused on training nurses using one-on-one encounters, day-long trainings, shadowing, and additional offsite trainings. Since then, the program has started training others, including medical assistants and health care providers by request. LaBelle noted that when her team contacted the 1,600 health care providers for whom it had provided buprenorphine waiver training, 30 percent requested additional assistance and education. This finding, in LaBelle’s view, argues against eliminating the waiver requirement because it shows how important training and education are for properly prescribing and treating SUD with MAT.
LaBelle noted that disparities in care are still an issue. “There are still ways in which our patients are not getting the services they need,” she said. “They are not being able to access the treatment when and where they want it and with the providers they [want]. We need to think differently.” For LaBelle, thinking differently means relying on nurses who are engaged in treating individuals with SUDs and take ownership in caring for them in community settings. “They are not only part of the team, they are an integral piece of the team,” said LaBelle.
The nurse care manager program leverages technology to reach out to those who would benefit from MAT and addiction treatment. The program’s website,35 for example, had 22,000 visitors in its first year of existence (starting in July 2018). The website contains free, easy-to-use clinical tools for health
___________________
35 For more information, see www.bmcobat.org (accessed November 19, 2019).
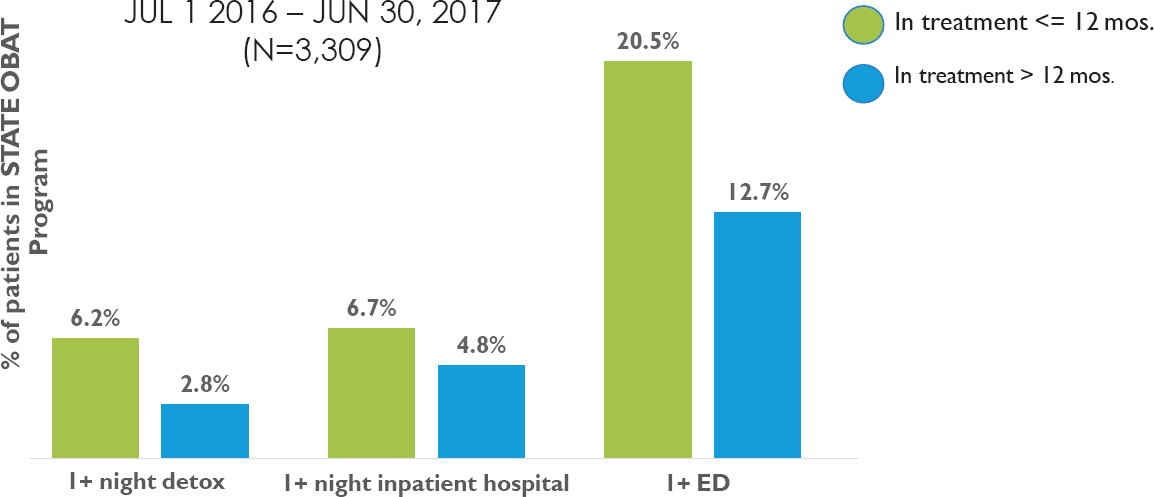
NOTE: ED = emergency department; OBAT = office-based addiction treatment.
SOURCES: As presented by Colleen LaBelle, October 16, 2019; Alford et al., 2011.
care providers and clinical algorithms that will eventually be interactive to help providers decide on the appropriate treatment plan for a given individual. The program is also taking video conferencing to another level, making live chats with nurses and recovery coaches available whenever a patient might need one. The website also includes virtual trainings for providers on a new long-acting injectable form of buprenorphine, walking providers through the logistical barriers and increasing patient options, explained LaBelle. The program uses Project ECHO tools that Haddad spoke about in his earlier presentation.
When considering how to address workforce shortages, LaBelle believes that nurse practitioners and physician assistants will be a big part of the solution, particularly given the trend of fewer physicians entering into and remaining in primary care, especially in community health centers and rural areas. She noted there have been legislative efforts to try to standardize nurse practitioners’ ability to practice independently, as this further creates barriers to treatment. LaBelle added that this is a huge barrier for rural areas and community health centers, and the IOM has recommended (IOM, 2011) leveraging nurses and allowing them to work to the scope of their practice in all settings. Community health centers, she added, can be the “secret sauce” for meeting the needs of patients in their communities, but only if they are provided with adequate support and resources to meet the demand for services. Community centers are often plagued by high staff turnover, inadequate salary and benefits, burnout, stigma, limited educational resources, and barriers to insurance coverage. LaBelle suggested addressing these barriers by
- Providing treatment on demand;
- Requiring comparable reimbursement for substance use services and reimbursing regardless of practice setting;
- Building off existing successful examples, such as the Ryan White Model;
- Adding services based on uncovered needs, resources, and disease impact;
- Supporting growth and value job satisfaction;
- Increasing use of telehealth and virtual visits for behavioral health care;
- Integrating behavioral health, medical, and specialty groups;
- Using recovery coaches and peer navigators;
- Allowing doctors of pharmacy to prescribe buprenorphine under the Drug Addiction Treatment Act of 2000; and
- Removing copays, prior authorizations, and all restrictions to MAT.
From LaBelle’s experience with this program, she has learned that trainers and trainees are more engaged, efficient, and effective when training adjusts to the changing workforce and meets their needs, skill set, and
availability. Online training resources can also be adopted to a variety of formats and learning styles. She also found that ongoing support was essential to staff retention.
To continue developing the workforce for integrated care, LaBelle supports allowing all providers to work to the scope of their practice, having treatment on demand wherever patients present, using community health centers, telehealth, nurses, and pharmacists to expand treatment, educating and engaging champions, and removing all barriers to care.
Social Work Workforce: Spanning Multi-Focused Care Delivery Systems
The VA, which serves more than 9 million enrollees, is the largest employer of master’s-degree-holding social workers in the United States, explained Laura Taylor, the national director for social work at the VA. The VA also trains approximately 1,500 social workers per year at the graduate level, supporting nearly 1,000 of them with stipends.36 Taylor explained that social work at the VA focuses on helping veterans, as well as their families and caregivers, resolve psychosocial, emotional, and economic barriers to health and well-being. It is also woven into the fabric of VA health care, providing services in all clinical programs across the continuum of care. All social workers at the VA receive training on using what is known as a “person-in-environment perspective,” which highlights the importance of understanding an individual and their behavior in the environmental contexts in which they live, work, and play.
Taylor referenced a 2019 National Academies report, Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health (NASEM, 2019a). The report emphasized the importance of making sure that health care providers are sensitive to and inclusive of social needs within the care they deliver.
According to Taylor, of the 15,000-plus social workers working in the VA, fewer than 1,000 are new graduates, with the remainder licensed independent providers. In the 2018 fiscal year, VA social workers cared for more than 1.4 million veterans.37 “We do not see every single veteran that comes through our doors, but we certainly are embedded in those teams and available for veterans who are experiencing some of the concerns, conditions, social determinants of health that have been talked about thus far,” said Taylor. Approximately 6,000 social workers are involved specifically in the VA’s homeless programs, and another 3,500–4,000 are working in a mental
___________________
36 For more information, see https://www.socialwork.va.gov (accessed February 7, 2020).
37 For more information, see https://www.socialwork.va.gov (accessed February 7, 2020).
health capacity.38 She noted that the VA is working to expand its workforce that provides caregiver support from around 500 social workers to 1,200 in the coming months.39
For Taylor, this is an exciting time at the VA because the system is moving toward having all of its health care providers embrace a person-centered, recovery-oriented approach to the care they deliver. As she explained, social workers are trained (and bound through their professional code of ethics) to approach people through a holistic view in order to assess and work with people at the individual level and within their communities. The final tenet and guiding principle for social workers, said Taylor, is respecting a person’s right to self-determination. “As a licensed social worker, we are bound to find out what a person chooses for themselves and then to try to help support them and understand the consequences of the choices that they make and really respect that. This means at times we are at odds with others on our embedded teams of which we are a member,” said Taylor.
Social workers at the VA exercise a range of clinical skills, starting with identifying high-risk veterans who may experience adverse health outcomes related to social determinants of health or other barriers to care. They also complete a clinical assessment of a veteran’s biopsychosocial situation, including MHSUDs, and screen for a variety of mental health conditions, including PTSD and suicide risk. VA social workers also develop veteran-centered goals and interventions relevant to any identified needs, deficits, and problems and then collaborate or coordinate services with community programs to strengthen or improve the continuity of care for that veteran. The Patient Aligned Care Team (Primary Care) social work practice model, explained Taylor, assesses veterans in six domains: (1) access to care, (2) economics, (3) housing, (4) psychological and cognitive status, (5) social support, and (6) functional status. The social worker assigns an acuity rating for each domain.
Taylor described research she and her colleagues conducted to gain a better understanding of the role that social determinants of health play in suicide attempts (Blosnich et al., 2019). In Veterans Integrated Service Network 4,40 which covers the entire state of Pennsylvania and parts of Delaware and southern New Jersey, they looked at nearly 300,000 veterans with at least one inpatient or outpatient visit in fiscal year 2016 and used multiple logistic regression to adjust for sociodemographic characteristics and medical comorbidity. The social determinant deficits they examined include violence, housing instability, employment/financial problems, legal problems, social/
___________________
38 For more information, see https://www.socialwork.va.gov (accessed February 7, 2020).
39 For more information, see https://www.socialwork.va.gov (accessed February 7, 2020).
40 For more information, see https://www.visn4.va.gov (accessed February 7, 2020).
family problems, lack of access to care/transportation, and non-specific psychosocial needs. Taylor explained they found that each individual dose of a social determinant deficit, even after adjusting for medical comorbidity, produced a significant dose-dependent response with documented suicide attempts. A person with just one social determinant deficit was 4.63 times more likely to have a suicidal ideation than a person with no deficit, and this risk increased with each additional adverse social determinant (Blosnich et al., 2019).
In closing, Taylor emphasized that mental health and social needs should not be considered separately but instead need to be recognized as dimensions of health and wellness that the health care system and delivery systems need to think about together—particularly regarding suicide prevention. Taylor added that given their whole-health approach to care, social workers are uniquely qualified to address these aspects of care and are vital members of health care delivery and integrated care teams. “We have to expand our traditional health care delivery model to include behavioral health and the social determinants of health,” she concluded.
Discussion
During the discussion session following the speaker presentations, Kathy Pham from the American College of Clinical Pharmacy commented that pharmacists, like registered nurses, routinely practice in team-based care and want to be part of improving care for people with MHSUDs. She asked LaBelle whether her team learned any lessons that would be useful to other professions as they leverage their knowledge and expertise to improve access to better care. LaBelle suggested having everyone on a care team look at the services each member provides, from clinicians to paraprofessionals, and determine whether they are practicing at or below the scope of their licenses. In that way, she said, it is possible to better leverage the available skills and bring in other workers to handle tasks such as billing for services. This approach not only better allocates resources but gives health care providers a better sense of satisfaction because they can better engage with patients without worrying as much about the boxes they have to check and forms they need to complete.
Pham then asked Holloway if his work has identified other barriers to care for OUD aside from workforce development and training. He responded that one barrier in Colorado relates to population distribution: the urban core surrounding Denver is highly populated while the rest of the state is largely rural and frontier. Some counties, he noted, have fewer than 1,000 residents, so MAT at a stationary site outside of the urban core is unlikely to be successful. However, mobile care can make it difficult to maintain patient anonymity. Additionally, in his opinion, nobody in urban areas wants a treatment facility in their neighborhood.
Matthew Tierney from the American Psychiatric Nurses Association and the UCSF School of Nursing and Office of Population Health asked the panelists if they knew of any evidence that workforce attitudes, beliefs, and perceptions about behavioral health problems are social determinants of health. Taylor replied that she did not know of any research on that subject but that this was an interesting question that needs to be answered. LaBelle said that in the early stages of her state’s expansion of the nurse care manager model, there were a few clinics in which there were attitude problems: some staff members did not want to treat patients with SUDs. Now, her program has new staff spend time with the nurses as they see patients, which allows the new staff members to see the value of this approach.
Holloway noted that he and his colleagues are conducting a claims analysis to look at where a patient receives care for their SUD relative to where they live, and stratified by income and race, to see if there is a difference in patients’ preferences of where to go for care. If this analysis finds that a certain population is bypassing the nearest source of care, his team can start to ask questions about the cultural competency, training, and transportation access at that facility. “That could tell us something important about how we resource the safety net,” said Holloway.
Weaver noted that peer support is not a profession according to the U.S. Department of Labor, which ruled in 2018 that peer supporters were not significantly different than community health workers. His organization was told that to become a formally identified profession, there must be at least 25,000 individuals in the United States in that profession. He asked the panelists where they obtain their data on how many employees they have in different professional categories. Taylor responded that the VA generates that data internally. She added that from the social work perspective, peer specialists are highly valued members of the care team who can reach and connect with people in a way that is meaningful when the rest of care team cannot. Washko’s advice to Weaver was to have everyone who identifies as a peer support professional state that as their occupation on surveys, such as the American Community Survey.41 Using the same terminology regularly triggers the U.S. Census Bureau coders to determine that they have sufficient numbers of individuals in an occupation, which helps to make the argument that there is a distinct profession. She added that she has gone through this process for direct care aides, home health aides, and certified nursing assistants.
Responding to a question posed by Andrew Kessler from the International Certification & Reciprocity Consortium, LaBelle concluded the discussion period by noting that there are parts of the health care system that are now
___________________
41 For more information, see https://www.census.gov/programs-surveys/acs (accessed December 3, 2019).
seeing individuals with SUDs and have no idea what to do to provide care and treatment. In particular, she has seen this in skilled nursing facilities, long-term care facilities, and home care. For example, skilled nursing facilities are struggling with how to care for a 20-year-old with an SUD with an 80-year-old patient in the next bed. “We have not put the resources there and people do not know what to do,” said LaBelle. Home health care is another area, she said, where things can get out of hand if the workforce is not appropriately trained.
In closing, Alexander Ross, the senior behavioral health advisor in the Office of Planning, Analysis and Evaluation at HRSA, encouraged the workshop attendees to reflect on the key themes raised during the workshop sessions and to continue to address the challenges in caring for those facing MHSUDs. He thanked the moderators, speakers, and staff for their contributions and adjourned the workshop.
REFERENCES
AAPA (American Academy of Physician Assistants). 2016. PAs are frontline providers for patients with mental health conditions. https://www.aapa.org/wp-content/uploads/2016/12/PAs_and_Mental_Health.pdf (accessed February 7, 2020).
ABA (American Bar Association). 2016. Practical tool for lawyers: Steps in supporting decision-making. https://www.americanbar.org/content/dam/aba/administrative/law_aging/PRACTICALGuide.pdf (accessed February 7, 2020).
AHCPR (Agency for Health Care Policy and Research). 1993. Depression Guideline Panel, Vol 2: Treatment of major depression, clinical practice guideline, No 5. Rockville, MD: Agency for Health Care Policy and Research, U.S. Public Health Service, U.S. Department of Health and Human Services.
Alford, D. P., C. T. LaBelle, N. Kretsch, A. Bergeron, M. Winter, M. Botticelli, and J. H. Samet. 2011. Collaborative care of opioid-addicted patients in primary care using buprenorphine: Five-year experience. Archives of Internal Medicine 171(5):425–431.
APA (American Psychiatric Association). 1998. Practice guideline for treatment of patients with panic disorder. Washington, DC: American Psychiatric Association.
APA. 2000. Practice guideline for the treatment of patients with major depressive disorder (revision). American Journal of Psychiatry 157(4 Suppl):1–45.
APA. 2002. Practice guideline for the treatment of patients with bipolar disorder (2nd ed.). Washington, DC: American Psychiatric Association Press.
APA. 2004. Practice guideline for treatment of patients with schizophrenia (2nd ed.). Washington, DC: American Psychiatric Association Press.
Arora, S., S. Kalishman, K. Thornton, D. Dion, G. Murata, P. Deming, B. Parish, J. Brown, M. Komaromy, K. Colleran, A. Bankhurst, J. Katzman, M. Harkins, L. Curet, E. Cosgrove, and W. Pak. 2010. Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: Disruptive innovation in specialty care. Hepatology 52(3):1124–1133.
Bailey, Z. D., N. Krieger, M. Agenor, J. Graves, N. Linos, and M. T. Bassett. 2017. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 389(10077):1453–1463.
Balas, E. A., and S. A. Boren. 2000. Managing clinical knowledge for health care improvement. Yearbook of Medical Informatics (1):65–70.
Barocas, J. A., L. F. White, J. Wang, A. Y. Walley, M. R. LaRochelle, D. Bernson, T. Land, J. R. Morgan, J. H. Samet, and B. P. Linas. 2018. Estimated prevalence of opioid use disorder in Massachusetts, 2011–2015: A capture-recapture analysis. American Journal of Public Health 108(12):1675–1681.
Bauer, J., and D. A. Groneberg. 2016. Measuring spatial accessibility of health care providers—introduction of a variable distance decay function within the floating catchment area (FCA) method. PLoS One 11(7):e0159148.
Beidas, R. S., S. Marcus, G. A. Aarons, K. E. Hoagwood, S. Schoenwald, A. C. Evans, M. O. Hurford, T. Hadley, F. K. Barg, L. M. Walsh, D. R. Adams, and D. S. Mandell. 2015. Predictors of community therapists’ use of therapy techniques in a large public mental health system. JAMA Pediatrics 169(4):374–382.
Beidas, R. S., S. Marcus, C. B. Wolk, B. Powell, G. A. Aarons, A. C. Evans, M. O. Hurford, T. Hadley, D. R. Adams, L. M. Walsh, S. Babbar, F. Barg, and D. S. Mandell. 2016a. A prospective examination of clinician and supervisor turnover within the context of implementation of evidence-based practices in a publicly-funded mental health system. Administration and Policy in Mental Health 43(5):640–649.
Beidas, R. S., R. E. Stewart, D. R. Adams, T. Fernandez, S. Lustbader, B. J. Powell, G. A. Aarons, K. E. Hoagwood, A. C. Evans, M. O. Hurford, R. Rubin, T. Hadley, D. S. Mandell, and F. K. Barg. 2016b. A multi-level examination of stakeholder perspectives of implementation of evidence-based practices in a large urban publicly-funded mental health system. Administration and Policy in Mental Health 43(6):893–908.
Beidas, R. S., R. E. Stewart, C. Benjamin Wolk, D. R. Adams, S. C. Marcus, A. C. Evans, Jr., K. Jackson, G. Neimark, M. O. Hurford, J. Erney, R. Rubin, T. R. Hadley, F. K. Barg, and D. S. Mandell. 2016c. Independent contractors in public mental health clinics: Implications for use of evidence-based practices. Psychiatric Services 67(7):710–717.
Beidas, R. S., N. J. Williams, E. M. Becker-Haimes, G. A. Aarons, F. K. Barg, A. C. Evans, K. Jackson, D. Jones, T. Hadley, K. Hoagwood, S. C. Marcus, G. Neimark, R. M. Rubin, S. K. Schoenwald, D. R. Adams, L. M. Walsh, K. Zentgraf, and D. S. Mandell. 2019a. Correction to: A repeated cross-sectional study of clinicians’ use of psychotherapy techniques during 5 years of a system-wide effort to implement evidence-based practices in Philadelphia. Implementation Science 14(1):89.
Beidas, R. S., N. J. Williams, E. M. Becker-Haimes, G. A. Aarons, F. K. Barg, A. C. Evans, K. Jackson, D. Jones, T. Hadley, K. Hoagwood, S. C. Marcus, G. Neimark, R. M. Rubin, S. K. Schoenwald, D. R. Adams, L. M. Walsh, K. Zentgraf, and D. S. Mandell. 2019b. A repeated cross-sectional study of clinicians’ use of psychotherapy techniques during 5 years of a system-wide effort to implement evidence-based practices in Philadelphia. Implementation Science 14(1):67.
Bernstein, A., B. F. Chorpita, E. L. Daleiden, C. K. Ebesutani, and A. Rosenblatt. 2015a. Building an evidence-informed service array: Considering evidence-based programs as well as their practice elements. Journal of Consulting and Clinical Psychology 83(6):1085–1096.
Bernstein, A., B. F. Chorpita, A. Rosenblatt, K. D. Becker, E. L. Daleiden, and C. K. Ebesutani. 2015b. Fit of evidence-based treatment components to youths served by wraparound process: A relevance mapping analysis. Journal of Clinical Child and Adolescent Psychology 44(1):44–57.
Blosnich, J. R., A. E. Montgomery, M. E. Dichter, A. J. Gordon, D. Kavalieratos, L. Taylor, B. Ketterer, and R. M. Bossarte. 2019. Social determinants and military veterans’ suicide ideation and attempt: A cross-sectional analysis of electronic health record data. Journal of General Internal Medicine 34(11):1–9.
Bonilla-Silva, E. 1997. Rethinking racism: Toward a structural interpretation. American Sociological Review 62(3):465–480.
Bradley, E. H., M. Canavan, E. Rogan, K. Talbert-Slagle, C. Ndumele, L. Taylor, and L. A. Curry. 2016. Variation in health outcomes: The role of spending on social services, public health, and health care, 2000–09. Health Affairs 35(5):760–768.
Center for Behavioral Health Statistics and Quality. 2015. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf (accessed March 10, 2020).
Chorpita, B. F., A. Bernstein, and E. L. Daleiden. 2011. Empirically guided coordination of multiple evidence-based treatments: An illustration of relevance mapping in children’s mental health services. Journal of Consulting and Clinical Psychology 79(4):470–480.
Chorpita, B. F., E. L. Daleiden, A. L. Park, A. M. Ward, M. C. Levy, T. Cromley, A. W. Chiu, A. M. Letamendi, K. H. Tsai, and J. L. Krull. 2017. Child STEPs in California: A cluster randomized effectiveness trial comparing modular treatment with community implemented treatment for youth with anxiety, depression, conduct problems, or traumatic stress. Journal of Consulting and Clinical Psychology 85(1):13–25.
Council of Economic Advisors. 2017. The underestimated cost of the opioid crisis. Executive Office of the President of the United States, Council of Economic Advisors.
Crenshaw, K. 1991. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review 43(6):1241–1299.
Croghan, T. W., and J. D. Brown. 2010. Integrating mental health treatment into the patient centered medical home. AHRQ Publication No. 10-0084-EF. Agency for Healthcare Research and Quality. https://pcmh.ahrq.gov/sites/default/files/attachments/Integrating%20Mental%20Health%20and%20Substance%20Use%20Treatment%20in%20the%20PCMH.pdf (accessed March 10, 2020).
Cronholm, P. F., C. M. Forke, R. Wade, M. H. Bair-Merritt, M. Davis, M. Harkins-Schwarz, L. M. Pachter, and J. A. Fein. 2015. Adverse childhood experiences: Expanding the concept of adversity. American Journal of Preventive Medicine 49(3):354–361.
Daleiden, E. L., B. F. Chorpita, C. Donkervoet, A. M. Arensdorf, and M. Brogan. 2006. Getting better at getting them better: Health outcomes and evidence-based practice within a system of care. Journal of the American Academy of Child and Adolescent Psychiatry 45(6):749–756.
Eccles, M. P., J. M. Grimshaw, P. Shekelle, H. J. Schünemann, and S. Woolf. 2012. Developing clinical practice guidelines: Target audiences, identifying topics for guidelines, guideline group composition and functioning and conflicts of interest. Implementation Science 7(1):60.
Felitti, V. J., R. F. Anda, D. Nordenberg, D. F. Williamson, A. M. Spitz, V. Edwards, M. P. Koss, and J. S. Marks. 1998. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 14(4):245–258.
Flexon, J. L., L. Stolzenberg, and S. J. D’Alessio. 2019. The effect of cannabis laws on opioid use. International Journal of Drug Policy 74:152–159.
Garland, A. F., R. L. Hough, K. M. McCabe, M. A. Y. Yeh, P. A. Wood, and G. A. Aarons. 2001. Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry 40(4):409–418.
Gee, G. C., and C. L. Ford. 2011. Structural racism and health inequities: Old issues, new directions. Du Bois Review 8(1):115–132.
Gibbons, R. D., and F. V. deGruy. 2019. Without wasting a word: Extreme improvements in efficiency and accuracy using computerized adaptive testing for mental health disorders (CAT-MH). Current Psychiatry Report 21(8):67.
Gibbons, R. D., and D. R. Hedeker. 1992. Full-information item bi-factor analysis. Psychometrika 57(3):423–436.
Gibbons, R. D., R. D. Bock, D. Hedeker, D. J. Weiss, E. Segawa, D. K. Bhaumik, D. J. Kupfer, E. Frank, V. J. Grochocinski, and A. Stover. 2007. Full-information item bifactor analysis of graded response data. Applied Psychological Measurement 31(1):4–19.
Gibbons, R. D., G. Hooker, M. D. Finkelman, D. J. Weiss, P. A. Pilkonis, E. Frank, T. Moore, and D. J. Kupfer. 2013. The computerized adaptive diagnostic test for major depressive disorder (CAD-MDD): A screening tool for depression. Journal of Clinical Psychiatry 74(7):669–674.
Gibbons, R. D., D. J. Kupfer, E. Frank, B. B. Lahey, B. A. George-Milford, C. L. Biernesser, G. Porta, T. L. Moore, J. B. Kim, and D. A. Brent. 2019. Computerized adaptive tests for rapid and accurate assessment of psychopathology dimensions in youth. Journal of the American Academy of Child and Adolescent Psychiatry. doi: 10.1016/j. jaac.2019.08.009. [Epub ahead of print].
Goldman, H. H., J. P. Morrissey, R. A. Rosenheck, J. Cocozza, M. Blasinsky, F. Randolph, and the ACCESS National Evaluation Team. 2002. Lessons from the evaluation of the access program. Psychiatric Services 53(8):967–969.
Graham, A. K., A. Minc, E. Staab, D. G. Beiser, R. D. Gibbons, and N. Laiteerapong. 2019. Validation of the computerized adaptive test for mental health in primary care. Annals of Family Medicine 17(1):23–30.
Graham, I. D., J. Logan, M. B. Harrison, S. E. Straus, J. Tetroe, W. Caswell, and N. Robinson. 2006. Lost in knowledge translation: Time for a map? Journal of Continuing Education in the Health Professions 26(1):13–24.
Grant, B. F., S. P. Chou, T. D. Saha, R. P. Pickering, B. T. Kerridge, W. J. Ruan, B. Huang, J. Jung, H. Zhang, A. Fan, and D. S. Hasin. 2017. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 74(9):911–923.
Grimshaw, J. M., M. P. Eccles, J. N. Lavis, S. J. Hill, and J. E. Squires. 2012. Knowledge translation of research findings. Implementation Science 7(1):50.
Gyani, A., R. Shafran, P. Myles, and S. Rose. 2014. The gap between science and practice: How therapists make their clinical decisions. Behavior Therapy 45(2):199–211.
Harvard T.H. Chan School of Public Health, Robert Wood Johnson Foundation, and National Public Radio. 2017. Discrimination in America: Final summary. Princeton, NJ: Robert Wood Johnson Foundation.
HHS (U.S. Department of Health and Human Services). 1999. Mental health: A report of the surgeon general. Rockville, MD: U.S. Public Health Service, U.S. Department of Health and Human Services.
IOM (Institute of Medicine). 1990. Broadening the base of treatment for alcohol problems. Washington, DC: National Academy Press.
IOM. 2011. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
Kanuganti, S., A. K. Sarkar, and A. P. Singh. 2016. Evaluation of access to health care in rural areas using enhanced two-step floating catchment area (E2SFCA) method. Journal of Transport Geography 56:45–52.
Larochelle, M. R., D. Bernson, T. Land, T. J. Stopka, N. Wang, Z. Xuan, S. M. Bagley, J. M. Liebschutz, and A. Y. Walley. 2018. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Annals of Internal Medicine 169(3):137–145.
Machtinger, E. L., K. B. Davis, L. S. Kimberg, N. Khanna, Y. P. Cuca, C. Dawson-Rose, M. Shumway, J. Campbell, A. Lewis-O’Connor, M. Blake, A. Blanch, and B. McCaw. 2019. From treatment to healing: Inquiry and response to recent and past trauma in adult health care. Women’s Health Issues 29(2):97–102.
McGrail, M. R. 2012. Spatial accessibility of primary health care utilising the two step floating catchment area method: An assessment of recent improvements. International Journal of Health Geographics 11(1):50.
Mennen, F. E., J. Cederbaum, B. F. Chorpita, K. Becker, O. Lopez, and M. Sela-Amit. 2018. The large-scale implementation of evidence-informed practice into a specialized MSW curriculum. Journal of Social Work Education 54(Suppl 1):S56–S64.
Mezzina, R. 2014. Community mental health care in Trieste and beyond: An “open door–no restraint” system of care for recovery and citizenship. The Journal of Nervous and Mental Disease 202(6):440–445.
Modesto-Lowe, V., and A. Boornazian. 2000. Screening and brief intervention in the management of early problem drinkers. Disease Management and Health Outcomes 8(3):129–137.
Mojtabai, R., L.-Y. Chen, C. N. Kaufmann, and R. M. Crum. 2014. Comparing barriers to mental health treatment and substance use disorder treatment among individuals with comorbid major depression and substance use disorders. Journal of Substance Abuse Treatment 46(2):268–273.
Morris, Z. S., S. Wooding, and J. Grant. 2011. The answer is 17 years, what is the question: Understanding time lags in translational research. Journal of the Royal Society of Medicine 104(12):510–520.
NAMI (National Alliance on Mental Illness). 2019. Mental health by the numbers. https://www.nami.org/learn-more/mental-health-by-the-numbers (accessed March 20, 2020).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2019a. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press.
NASEM. 2019b. Medications for opioid use disorder save lives. Washington, DC: The National Academies Press.
NCHS (National Center for Health Statistics). 2016. Health, United States, 2015: With special feature on racial and ethnic health disparities. Hyattsville, MD: National Center for Health Statistics.
NCQA (National Committee for Quality Assurance) (Ed.). 1997. HEDIS 3.0: Narrative: What’s in it and why it matters. Washington, DC: National Committee for Quality Assurance.
NIMH (National Institute of Mental Health). 2017. Mental illness. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml (accessed February 7, 2020).
Noonan, K., and K. Craig. 2019. From siloed systems to ecosystem: The evolution of the Camden Coalition’s complex care model. Camden, NJ: Camden Coalition of Healthcare Providers.
Novak, P., K. A. Feder, M. M. Ali, and J. Chen. 2019. Behavioral health treatment utilization among individuals with co-occurring opioid use disorder and mental illness: Evidence from a national survey. Journal of Substance Abuse Treatment 98:47–52.
O’Brien, P., E. Crable, C. Fullerton, and L. Hughley. 2019. Best practices and barriers to engaging people with substance use disorders in treatment. Greenwood Village, CO: Truven Health Analytics.
Optum. 2015. Pierce County Regional Support Network (RSN). https://www.optum.com/content/dam/optum/resources/whitePapers/BSPUB0119S003JV_PierceCty-WR.pdf (accessed February 7, 2020).
Paradies, Y., J. Ben, N. Denson, A. Elias, N. Priest, A. Pieterse, A. Gupta, M. Kelaher, and G. Gee. 2015. Racism as a determinant of health: A systematic review and meta-analysis. PLoS One 10(9):e0138511.
Park, A. L., K. H. Tsai, K. Guan, and B. F. Chorpita. 2018. Unintended consequences of evidence-based treatment policy reform: Is implementation the goal or the strategy for higher quality care? Administration and Policy in Mental Health 45(4):649–660.
Powell, B. J., R. S. Beidas, R. M. Rubin, R. E. Stewart, C. B. Wolk, S. L. Matlin, S. Weaver, M. O. Hurford, A. C. Evans, T. R. Hadley, and D. S. Mandell. 2016. Applying the policy ecology framework to Philadelphia’s behavioral health transformation efforts. Administration and Policy in Mental Health 43(6):909–926.
Priester, M. A., T. Browne, A. Iachini, S. Clone, D. DeHart, and K. D. Seay. 2016. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: An integrative literature review. Journal of Substance Abuse Treatment 61:47–59.
Rawls, J. 1971. A theory of justice. Cambridge, MA: Harvard University Press.
Rehm, J., P. Anderson, J. Manthey, K. D. Shield, P. Struzzo, M. Wojnar, and A. Gual. 2016. Alcohol use disorders in primary health care: What do we know and where do we go? Alcohol and Alcoholism 51(4):422–427.
Reiss-Brennan, B., K. D. Brunisholz, C. Dredge, P. Briot, K. Grazier, A. Wilcox, L. Savitz, and B. James. 2016. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 316(8):826–834.
Rentas, K. G., L. Buckley, D. Wiest, and C. A. Bruno. 2019. Characteristics and behavioral health needs of patients with patterns of high hospital use: Implications for primary care providers. BMC Health Services Research 19(1):81.
Richmond, J. B., and M. Kotelchuck. 1991. Co-ordination and development of strategies and policy for public health promotion in the United States. In Oxford textbook of public health, edited by W. W. Holland, R. Detels, and G. Knox. Oxford, UK: Oxford Medical Publications. Pp. 441–454.
Rivara, F. P., S. Tollefson, E. Tesh, and L. M. Gentilello. 2000. Screening trauma patients for alcohol problems: Are insurance companies barriers? Journal of Trauma 48(1):115–118.
Roberts, N. P., P. A. Roberts, N. Jones, and J. I. Bisson. 2015. Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review 38:25–38.
Rodriguez, A., A. S. Lau, B. Wright, J. Regan, and L. Brookman-Frazee. 2018. Mixed-method analysis of program leader perspectives on the sustainment of multiple child evidence-based practices in a system-driven implementation. Implementation Science 13(1):44.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2014. Projections of national expenditures for treatment of mental and substance use disorders, 2010–2020. HHS Publication No. SMA-14-4883.
SAMHSA. 2017. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. HHS publication No. SMA 17-5044, NSDUH series H-52. Paper read at Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
SAMHSA. 2019. Mental health services administration: Practitioner and program data. https://www.samhsa.gov/medication-assisted-treatment/training-materials-resources/practitioner-program-data (accessed February 7, 2020).
Sani, S., J. Busnello, R. Kochanski, Y. Cohen, and R. D. Gibbons. 2017. High-frequency measurement of depressive severity in a patient treated for severe treatment-resistant depression with deep-brain stimulation. Translational Psychiatry 7(8):e1207.
Southam-Gerow, M. A., J. R. Weisz, B. C. Chu, B. D. McLeod, E. B. Gordis, and J. K. Connor-Smith. 2010. Does cognitive behavioral therapy for youth anxiety outperform usual care in community clinics? An initial effectiveness test. Journal of the American Academy of Child and Adolescent Psychiatry 49(10):1043–1052.
Stewart, R. E., D. R. Adams, D. S. Mandell, T. R. Hadley, A. C. Evans, R. Rubin, J. Erney, G. Neimark, M. O. Hurford, and R. S. Beidas. 2016. The perfect storm: Collision of the business of mental health and the implementation of evidence-based practices. Psychiatric Services 67(2):159–161.
Storholm, E. D., A. J. Ober, S. B. Hunter, K. M. Becker, P. O. Iyiewuare, C. Pham, and K. E. Watkins. 2017. Barriers to integrating the continuum of care for opioid and alcohol use disorders in primary care: A qualitative longitudinal study. Journal of Substance Abuse Treatment 83:45–54.
Tsai, K. H., A. L. Moskowitz, R. E. Lynch, E. Daleiden, C. Mueller, J. L. Krull, and B. F. Chorpita. 2019. Do treatment plans matter? Moving from recommendations to action. Journal of Clinical Child and Adolescent Psychology 48(Suppl 1):S72–S78.
Wade, R., Jr., P. F. Cronholm, J. A. Fein, C. M. Forke, M. B. Davis, M. Harkins-Schwarz, L. M. Pachter, and M. H. Bair-Merritt. 2016. Household and community-level adverse childhood experiences and adult health outcomes in a diverse urban population. Child Abuse and Neglect 52:135–145.
Weisz, J. R., B. F. Chorpita, L. A. Palinkas, S. K. Schoenwald, J. Miranda, S. K. Bearman, E. L. Daleiden, A. M. Ugueto, A. Ho, J. Martin, J. Gray, A. Alleyne, D. A. Langer, M. A. Southam-Gerow, and R. D. Gibbons. 2012. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry 69(3):274–282.
WHO (World Health Organization). 2003. Organization of services for mental health. Geneva, Switzerland: World Health Organization.
WHO. 2015. Meeting report on excess mortality in persons with severe mental disorders. https://www.who.int/mental_health/evidence/excess_mortality_meeting_report.pdf (accessed February 7, 2020).
Wiest, D., Q. Yang, C. Wilson, and N. Dravid. 2019. Outcomes of a citywide campaign to reduce Medicaid hospital readmissions with connection to primary care within 7 days of hospital discharge. JAMA Network Open 2(1):e187369.
Young, J., E. L. Daleiden, B. F. Chorpita, J. Schiffman, and C. W. Mueller. 2007. Assessing stability between treatment planning documents in a system of care. Administration and Policy in Mental Health 34(6):530–539.
Zima, B. T., M. S. Hurlburt, P. Knapp, H. Ladd, L. Tang, N. Duan, P. Wallace, A. Rosenblatt, J. Landsverk, and K. B. Wells. 2005. Quality of publicly-funded outpatient specialty mental health care for common childhood psychiatric disorders in California. Journal of the American Academy of Child and Adolescent Psychiatry 44(2):130–144.


























































































