3
Operational Considerations for Individual Counts of Mortality and Morbidity
Disaster-related mortality and morbidity can be measured using two primary approaches—individual counts and population estimates—both of which contribute to the comprehensive assessment of a disaster’s impact. This chapter discusses the many operational considerations related to individual counts in order to explore how these data can be collected and used in disaster management. Discussions of analytical approaches for conducting population estimates of disaster-related mortality and morbidity can be found in Chapter 4. This chapter begins by exploring the heterogeneity in death investigation and registration systems and how this, among other factors, affects the collection, reporting, and recording of individual mortality count data. The latter part of the chapter focuses on the current practices, tools, and systems for using individual mortality data and identifies potential best practices and opportunities for bringing these practices to scale. Because of the differences between disaster-related mortality and morbidity data for individual counts, the chapter handles these issues separately. Box 3-1 provides a brief overview of how mortality and morbidity can be attributed when there have been individual counts of mortality and morbidity as described in the framework in the prior chapter. Several examples of the assessment of coronavirus disease 2019 (COVID-19)-related mortality and morbidity are included in this chapter to highlight overlapping administrative and logistical challenges that persist regardless of disaster type.
The individual counting approach to estimating total reported mortality and morbidity is reliant on the capture of all relevant cases and the appropriate attribution and recording of each case. This process of capturing
and recording data on reported mortalities and morbidities involves a multitude of factors at the state or local level—policies and case definitions for individual attribution; the availability of evidence and guidance to support decision making, the structure of the state or local medicolegal death investigation system, the process of death registration, and the training and professional judgment of medical examiners, coroners, and other medical certifiers to perform this work accurately and consistently. No standard practices, policies, or systems exist for recording these data. Additionally, the range of known and unknown morbidities and their complex associations with the disaster exposure are vast, and the process of assessing morbidity is challenged further by a lack of understanding of how chronic conditions and their sequelae can be attributed directly or to some other degree in the context of a disaster. The additional consideration of how to capture indirect and partially attributable deaths adds further complexity. These categories of individual deaths are not likely to be referred to the medical examiner or coroner and are more likely to be recorded by other medical certifiers in clinical or residential settings, such as a hospital or nursing home, where evidence to connect the death to a disaster may not be considered or may be unavailable.
Additionally, as described in Chapter 2, there are other issues related to inequity and vulnerability, which further complicate the collection and use of reported mortality and morbidity data at an individual level. For example, not all individuals with a disaster-related morbidity will present themselves to health care providers, as the ability to access care is tied to broader social and environmental contexts. Likewise, these same underlying factors simultaneously heighten an individual’s risk of harm (e.g., pollution exposure or overcrowded housing) (McKibben, 2020). These associations complicate the collection of complete mortality and morbidity data and limit their actionability. Although this report will not discuss the integration and use of social determinants of health data into mortality and morbidity data to enhance their actionability for use in disaster management, Appendix D provides two high-level case studies, which examine how social determinants of health relate to mortality and mortality during and following disasters.
THE INVESTIGATION AND REGISTRATION OF DEATHS IN THE UNITED STATES
In the United States, individual mortality data are collected through a process that spans multiple medical, legal, and administrative systems: the nationwide network of state, local, tribal, and territorial (SLTT) medicolegal death investigation systems combined with state- and federal-level death registration systems. Understanding the challenges related to estimating disaster-related mortality using individual counting approaches requires an understanding of the process of registering a death. This begins when the certification of a death is performed by a medical certifier. The next step is for the death to be recorded in state and national death registration systems, which allows for state and federal mortality data to be compiled, analyzed, and disseminated. This section provides an overview of how these systems function and communicate to generate the individual-level mortality data used for estimating total reported mortality. Examining the function of these systems is essential to understanding the structural and administrative barriers that hinder the process of developing accurate individual counts.
Medicolegal Death Investigation Systems
The medicolegal death investigation system is responsible for investigating deaths and certifying the cause and manner of death for unnatural or unexplained deaths. This includes deaths due to homicide, suicide, unintentional injuries, and drug overdoses, among others. Those deaths processed via the medicolegal death investigation system account for 20 percent of all deaths (IOM, 2003). The medicolegal death investigation system has critical importance beyond the legal system and represents a great value to public health and research. Data collected in the system can be used to inform
epidemiological investigations, disease and injury prevention programs, and preparedness and response practices and planning. In the United States the medicolegal death investigation system consists of a patchwork of different types of systems at the state and local levels for investigating these deaths. No federal or standardized medicolegal death investigation system is in use across all states and territories. The United States has about 2,400 medical examiner and coroner (ME/C) jurisdictions nationwide (NSTC, 2016) (see descriptions of these professions below). Medicolegal death investigation systems may be centralized at the state level or decentralized at the county or district level and may involve a coroner system, a medical examiner system, or a combination of both (CDC, 2015) (see Figure 3-1). For instance, the state of Florida has a decentralized medical examiner system, where county medical examiners are responsible for reporting data to the state commission, which is responsible for setting policy. This is different from states such as Maryland, Rhode Island, and Virginia, which have statewide systems that report to the state’s chief medical examiner, who is responsible for policy setting. In Texas, the structure of the medicolegal system varies by county; some counties are served by the medical examiner’s office, while others assign coroner duties to a justice of the peace or sheriff.
Within this diverse patchwork of medicolegal death investigation systems, death investigations are performed by ME/Cs, who have vastly different levels of professional training and requirements for education and professional experiences, as set by state code. These qualifications vary from being a registered voter with a high school diploma and free of a felony conviction in some coroner systems to being a forensic pathologist with 4–6 years of postgraduate medical training and specialty board certification working in medical examiner systems as autopsy physicians and public health officers. Medical examiners are required to have a doctorate of medicine, and they have varying professional requirements, with some states requiring more specialized certifications than others. Medical examiners are typically pathologists or forensic pathologists or simply physicians of any medical specialty who serve at a county, district, or state level. Unlike medical examiners, coroners are elected or appointed into office and serve an individual county or locality. Coroners generally do not have a medical background, although they may receive some training in certain jurisdictions (IOM, 2003). Despite the essential skills and expertise that medical examiners bring to the medicolegal death investigation system, the number of professionals in the field is in decline and funding remains insufficient (IOM, 2003; NSTC, 2016).
Many studies have recommended the conversion of coroner-based systems to medical examiner systems where deaths are investigated by medical death investigators, autopsies are performed by forensic pathologists, and deaths are certified by physician medical examiners with expertise in
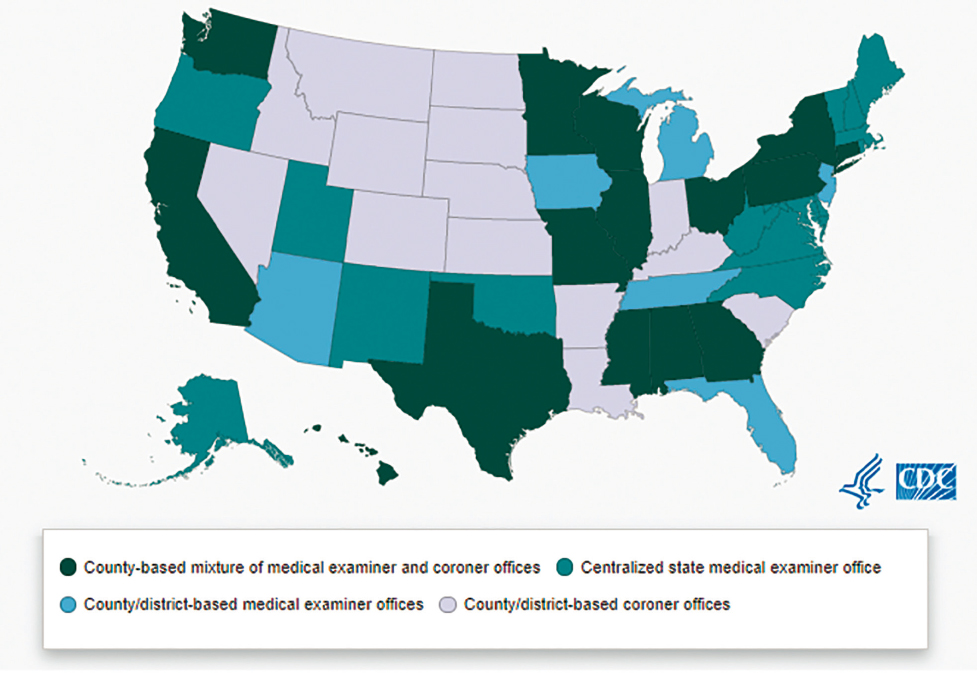
SOURCE: CDC, 2015.
identifying and documenting causes of death (IOM, 2003).1 A 2009 report by the National Research Council, Strengthening Forensic Science in the United States: A Path Forward, recommended that Congress should authorize and appropriate incentive funds to establish regional medical examiner offices. Such a program would bring baseline standards for expertise and uniformity in the certification and coding of deaths, professional excellence in determining the causes of death, and economies of scale in staffing, facilities, electronic case management systems, and supplies.
Other Medical Certifiers
The medical certifier is responsible for determining the cause and manner of death, making an assessment of whether a death is related to a disaster, and recording primary data on the death. The type of medical certifier responsible in a particular situation depends on the circumstances of the death (see Box 3-2) and can be not only a medical examiner or coroner, but also another medical certifier such as a justice of the peace, sheriff, sheriff-coroner, hospital physician, pathologist, nurse practitioner, or other licensed health professional or responsible party depending on the state (Ruiz et al., 2018). In order to accurately collect data on individual-level deaths, death certifiers need to be supported with appropriate training, standards, and functional systems for recording the death within state and federal vital statistics systems (see later section on Training).
___________________
1 A cause of death is the specific illness or injury that led to death. The manner of death is how that injury or illness led to the death. Natural deaths have internal physiological causes; the term “unnatural death” is often used by medical examiners and coroners to categorize a death that did not occur due to natural causes (Snohomish County, 2020).
Death Registration Systems in the United States
After a death is certified by a ME/C or other medical certifier, it must be registered at the state-level vital records office, creating a death record. It is at this point that the medicolegal death investigation systems and the death registration systems meet. The state-level death registration system takes in data entered from multiple sources at the local and county levels, such as information from the case management systems used by ME/Cs and information from other medical certifiers and funeral homes, in order to create death records in state-based electronic death registration systems (EDRSs). ME/C case management systems, which collect and store data for ME/Cs and are separate from the state EDRS, receive information from death scene investigations, toxicology reports, and autopsy reports. Physicians and other medical certifiers of death input data directly into the state-based EDRS, while funeral home systems provide the EDRS with demographic information on deaths.
The state-level death registration system in turn shares death record information with the National Center for Health Statistics (NCHS) through the National Vital Statistics System (NVSS). NVSS compiles national statistics on disaster-related mortality from information provided on death records; if the medical certifier has not recorded a disaster name and coded the death as disaster-related, then the death may not be reported as such (Horney, 2017; NVSS, 2017) (see Box 3-3). Therefore, the state and federal vital statistics offices play critical roles in the collection, recording, and
reporting of mortality data and are foundational to the accurate and timely assessment of individual mortality counts following large-scale disasters.
Ideally, this interactive network of independent ME/C, state, and national electronic mortality data systems would be interoperable and would facilitate rapid data sharing (see Figure 3-2). However, not all ME/C jurisdictions are equipped with electronic case management systems, nor have all states transitioned to fully electronic death registration systems (e.g., American Samoa, Connecticut, Guam, North Carolina, Northern Mariana Islands, Rhode Island, Virgin Islands, and West Virginia have not) (NAPHSIS, 2020a). Additionally, because ME/C case management systems are not interoperable with state EDRSs, ME/Cs have to preform duplicate data entry in each system, which creates an administrative burden on already overworked professionals. In a crisis, this time burden is even more of an issue and could affect data quality if ME/Cs do not enter sufficient descriptive data about deaths into the EDRS. Furthermore, the way in which these systems output disaster information varies widely, from basic line list to electronic transfer. The development of a national network of ME/C case management systems, which would require investment by the Centers for Disease Control and Prevention (CDC) and states, would address the chronic issues related to poor interoperability and minimum standards for data quality and collection. Such a network could feature electronic and interoperable systems between ME/C case management, state EDRS, and NVSS; standard coding practices for disaster-related deaths; and mechanisms for rapidly sharing data with communities to facilitate recovery and promote preparedness for future disasters.
Data Sharing Within and Between States and Territories
The ability to share mortality data across stakeholders within a state or locality is critical for the inclusion of these data in the public health response to and surveillance of a disaster. However, sharing data is not always simple, and barriers to sharing data have been noted within localities with decentralized medical examiner or coroner systems, where the vital records office functions separately from the public health department, or where plans are not in place to provide alternative methods of data sharing (e.g., daily mortality reports or access to preliminary death record data) (Horney, 2017). Some mechanisms do currently exist to facilitate data sharing across states and territories. The State and Territorial Exchange of Vital Events system, operated by the National Association for Public Health Statistics and Information Systems, provides a platform for secure inter-jurisdictional exchange of mortality data between state-level electronic death registration systems and the national system (NAPHSIS, 2020b).
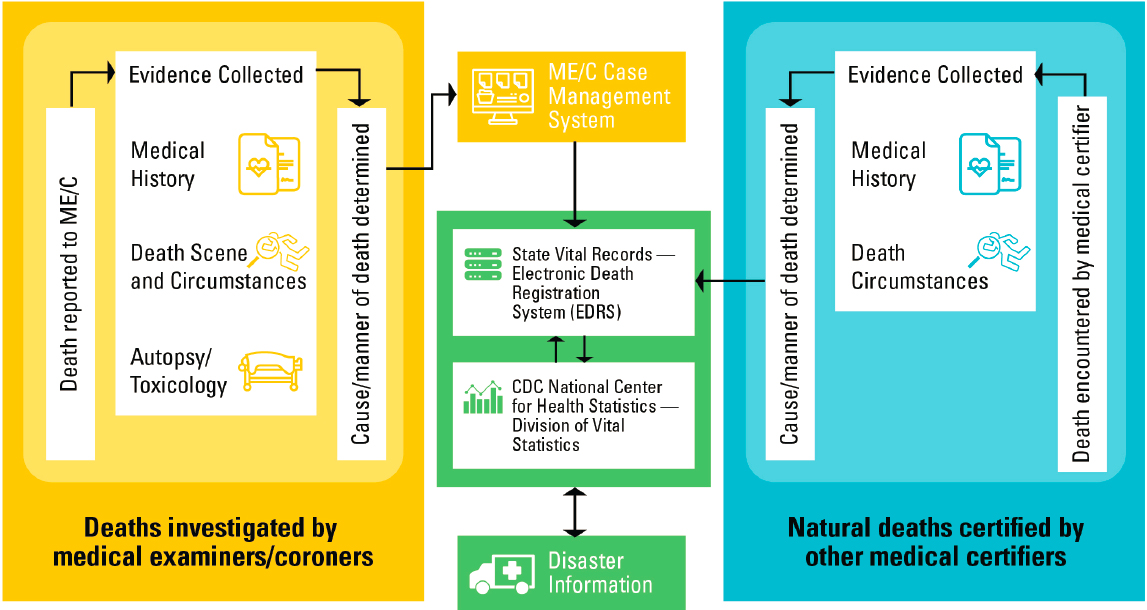
NOTE: CDC = Centers for Disease Control and Prevention; ME/C = medical examiner and coroner.
SOURCE: Adapted from FEMA, 2019.
Death Certificates Versus Death Records
In the age of paper-based reporting, the death certificate was considered to be the primary source of individual-level mortality data. However, with the advent of electronic death registration systems, the information collected in the death registration system, which is called the death record, is actually the primary source of individual mortality data. A portion of this death record is used to create the death certificate, which is used for legal purposes, and the other portion is a statistical record containing detailed medical and demographic data. The death record is sent to the federal level for automated medical coding and editing by NVSS for the creation of statistical files for state and federal use. NCHS does issue a national standard death certificate that complies with the International Classification of Diseases, Tenth Revision (ICD-10) standards to facilitate uniform data collection and reporting for statistical analysis. States are required to collect standard vital statistics data that are captured in the death record, and states may and do add additional data items for their own registration or statistical needs, such as opioid overdoses, maternal mortality, and smoking. The death record of the EDRS is now the source of the state death certificate and the statistical information used in mortality attribution at the local, state, and federal levels.
CHALLENGES WITH UNIFORM ATTRIBUTION ACROSS THESE SYSTEMS
Today, SLTT medicolegal systems and the state and federal death registration systems function in conjunction with one another, but originally these systems developed independently due to their historically different purposes. Death investigation systems and vital statistics registration systems in the United States evolved as state-level functions. Understanding the impact of the heterogeneity of medicolegal death investigation and death registration systems and the many different stakeholder roles is foundational to understanding the challenges related to operationalizing the collection, reporting, and recording of disaster-related mortality data. The structural consequences of this heterogeneity include poor interoperability and coordination among systems and stakeholders, variability in SLTT practices for attributing and collecting data on a death, and issues related to the completion of the death record in the state EDRSs. These major challenges contribute cumulatively to the under-reporting of disaster-related deaths and dramatic differences between states that would experience similar events.
Poor Interoperability and Coordination Among Systems and Stakeholders
Poor interoperability and limited coordination among systems and stakeholders present major challenges to the uniform attribution of disaster-related mortality across the nation. Medicolegal death investigation systems and vital statistics systems were not designed to capture information in a way that facilitates interoperability and data sharing within and across the SLTT and federal levels (Borfitz, 2019; Hanzlick, 2006; Noe, 2018). Furthermore, medical certifiers of death and those responsible for recording deaths have siloed professional roles and work within siloed systems despite multiple efforts to address these issues (ASPE, 2013).
Variability in SLTT Practices for Attributing and Recording Data on a Death
There exists no national uniform practice for attributing and recording disaster-related deaths, and substantial differences persist across SLTT practices for attributing and collecting data on a death. Variations in state and local practices on attributing and recording direct and indirect disaster-related deaths—particularly for natural deaths that are not sent to the ME/C for review—affect the collection of descriptive data on the death record. Table 3-1 illustrates the variation in disaster-related deaths attributed to four natural disasters across different state and federal entities and nongovernmental organizations between 2008 and 2013. Table 3-2 illustrates the extent of definitional variation in assessment practices for COVID-19 deaths across states and jurisdictions, which demonstrates the potential for variation in reported mortalities from state to state.
For example, there are policy differences at the administrative level regarding what counts as a disaster-related death. In some jurisdictions the death investigations systems have applied CDC’s uniform case definitions for direct and indirect disaster-related deaths, but many systems use different case definitions of varying stringency and specificity. Many jurisdictions do not count indirect deaths at all, and almost none purposefully count deaths that are partially attributable to a disaster, per the framework proposed by the committee in Chapter 2. ME/C systems typically have clearly defined legal requirements for which cases are reported as being disaster-related; however, inconsistencies among different states’ requirements affect the accuracy of national-level reporting. A literature review of medicolegal death scene investigations after natural disaster- and weather-related events found no consistent approach for attributing deaths to a disaster and significant variation in how death scene data collection tools were being used (Rocha et al., 2017).
TABLE 3-1 Variations in Reported Number of Deaths After Large-Scale Disaster Events
| Disaster Event | State Response Agencies | Red Cross | FEMA | NOAA–NWS | Vital Statistics |
|---|---|---|---|---|---|
| Hurricane Ike, TX (2008) | 74 | 38 | 104 | 20 | 4 |
| April 27 tornado, GA (2011) | 15 | 15 | 9 | 15 | 6 |
| Hurricane Sandy, NJ (2012) | 75 | 34 | 61 | 12 | 24 |
| May tornadoes, OK (2013) | 48 | 42 | 19 | 30 | 36 |
NOTE: FEMA = Federal Emergency Management Agency; NOAA–NWS = National Oceanic and Atmospheric Administration–National Weather Service; State response agencies = medical examiners and coroners and emergency operations centers; Vital Statistics = post-disaster review of death certificates in state-based vital statistics systems.
SOURCE: Noe, 2019.
NOTE: FEMA = Federal Emergency Management Agency; NOAA–NWS = National Oceanic and Atmospheric Administration–National Weather Service; State response agencies = medical examiners and coroners and emergency operations centers; Vital Statistics = post-disaster review of death certificates in state-based vital statistics systems.
SOURCE: Noe, 2019.
TABLE 3-2 Variations in Assessment Practices for COVID-19-Related Deaths by Jurisdiction, June 2020
| State/Jurisdiction | Criteria for Including Death as Attributable to COVID-19 |
|---|---|
| Centers for Disease Control and Prevention |
|
| Colorado |
|
| Iowa |
|
| State/Jurisdiction | Criteria for Including Death as Attributable to COVID-19 |
|---|---|
| Montana |
|
| Connecticut, Delaware, Ohio Pennsylvania |
|
SOURCES: Brown et al., 2020; CDC, 2020c; Iowa Board of Medicine, 2020; Montana DPHHS, 2020; Pennsylvania Department of Health, 2020.
Differences between New York City and Texas illustrate how variation in city- and state-level vital statistics systems affects mortality reporting. Both New York City and Texas have mandated electronic death registration systems. In New York City—one of only two U.S. cities to have an independent vital records jurisdiction—medical certifiers must start a death record within 24 hours of death, and the funeral home must complete the record (note that funeral directors do not play a role in determining cause of death and contributing factors) and register the death within 72 hours. The city’s centralized medical examiner office and rapid timeline for death registration are conducive to using death records for real-time mortality surveillance. In Texas, the death record must be registered within 10 days of death; the record is initiated by the funeral home, and then the designated medical certifier—depending on the county in question, this individual could be a coroner with little or no medical training—has 5 days to complete the medical portion of the death record.
Challenges Specific to the Completion of the Death Record
A host of challenges in capturing accurate individual-level mortality data relate specifically to issues concerning the completion of death records by ME/Cs and other medical certifiers and contribute to the under-reporting of disaster-related deaths in state and national databases. The consistency and quality of data captured on a death record are contingent on the consistency and quality of the data source. A lack of quality data limits the ability to assess individual mortality counts and, by extension, population estimates of mortality because state- and national-level mortality statistics are based solely on the information reported on the death record (NVSS, 2017).
Death Record Format
If the data entered into a death record by the certifier do not include the appropriate disaster-related terms (see Box 3-3), then NCHS cannot assign an ICD-10 code that attributes a death to a disaster.2 Prior research has noted that the quality of basic data recorded on death certificates is poor overall (Noe, 2018; NVSS, 2017) and that many death records in state EDRSs do not include clear, precisely defined terms for attributing a death directly or indirectly to a disaster.3 This can make it difficult for a medical certifier to record whether a disaster contributed to the death and to what degree. Evaluation studies have found that disaster-related deaths were under-reported on death certificates because they did not include key disaster terms to attribute a death as being related to a specific event (Issa et al., 2019; Kulkarni et al., 2015). Properly completing a death certificate is challenging for multiple reasons (Madsen and Begier, 2013), which are intensified in a disaster context (Madsen and Begier, 2013), and most death registration systems currently used across the country do not offer or require simple, precisely defined options for coding a death as directly, indirectly, or partially attributable to a specific disaster. See Figure 3-3 for a current example of the cause and manner of death entry fields in the District of Columbia EDRS.
___________________
2 “Brief History of Centers for Disease Control and Prevention Disaster-Related Mortality Activities.” Paper provided to the committee at the August 29, 2019, workshop in Washington, DC. Available by request from the Public Access Records Office by emailing PARO@nas.edu.
3Ibid.
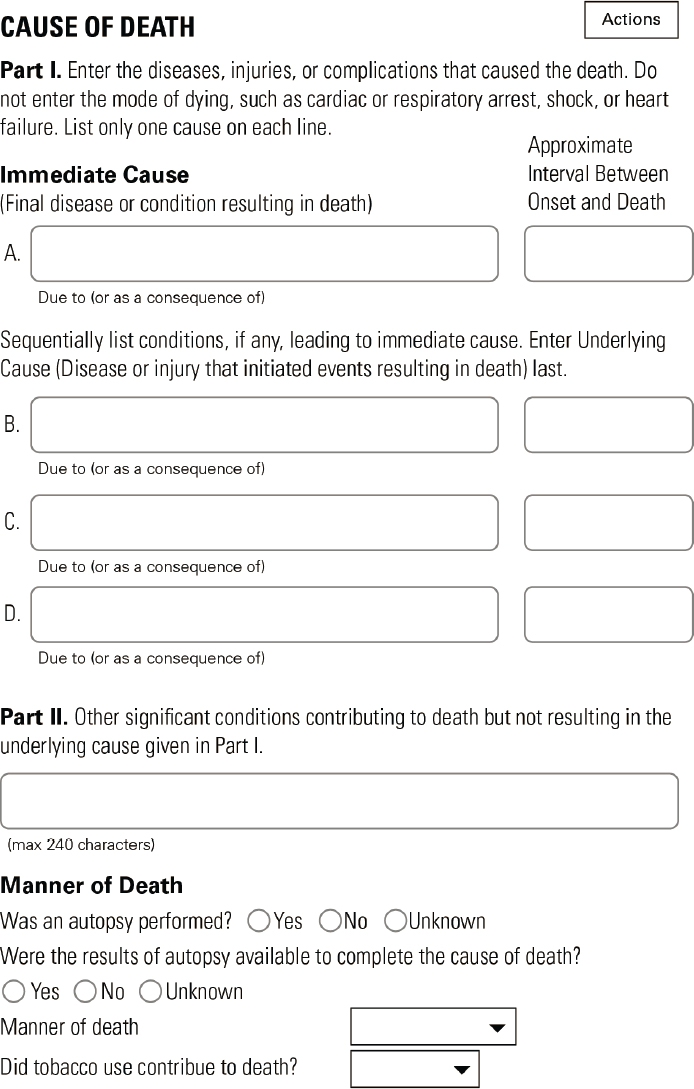
SOURCE: Personal communication, R. Anderson, NCHS, June 11, 2020.
Inadequate Training for Certifiers
In many cases, medical certifiers, such as medical personnel who typically treat living patients, are inadequately trained in determining the cause of death in ordinary circumstances (Madsen and Begier, 2013); the burden on inadequately trained certifiers is further intensified during a disaster context. Studies have found errors in attributing the cause or manner of death on about one-third of death records, largely due to physician inexperience and a lack of training in death registration (Brooks and Reed, 2015). As mentioned previously, no minimum professional qualification exists for medical certifiers, and many are unfamiliar with CDC’s uniform disaster mortality case definitions. Due to the lack of training and vastly different levels of professional qualification (Brooks and Reed, 2015), death certifiers may underappreciate the importance of including the disaster details or terms on death. Even if a death record entered into an EDRS does offer an option for disaster attribution, certifiers are generally not provided with clear case definitions or decision-making tools for distinguishing between directly and indirectly related deaths. Furthermore, ME/Cs may not have sufficient information from the death scene to attribute a death to the disaster (Bryant, 2003), and medical certifiers outside the medicolegal system frequently do not have access to descriptive health and personal data about the decedent that could be used to inform their completion of the death record. In many cases of “natural” death, the physician in the hospital is often asked to complete the death certificate without any knowledge or training in reporting disaster-related fatalities.
Philosophical Differences Among Certifiers
The diversity in medicolegal death investigation systems and the variability in what “counts” as a disaster-related death at a state and local level create an environment conducive to significant philosophical differences across the ME/C profession as to how to attribute the cause and manner of death. While most professionals agree that direct exposure to disaster-related environmental forces can contribute directly to morbidity and mortality, there is less consensus about how to codify the impact of indirect exposures on adverse health outcomes (Combs et al., 1999). For instance, some ME/Cs do not believe that certain types of deaths—such as natural deaths due to exacerbation of a chronic condition—should be attributed to a disaster.4 A study carried out at the annual meeting of the National Association of Medical Examiners (NAME) asked attendees to determine the relative contribution of a disaster to several deaths that had already been attributed by other medical examiners. Agreement with the previous
___________________
4Ibid.
attributions among the attendees ranged from 27 to 100 percent, with agreement less likely for cases of natural death or deaths due to indirect exposures linked to the disaster (Combs et al., 1999). The standardization of practices for attributing mortality and consensus of opinion among medical certifiers will address much of the variability in the completion of death records following disasters. The burden for adopting this improvement does not fall only on ME/Cs and other medical certifiers, but also on state registrars (Slavova et al., 2015), NCHS, and public health agencies that value access to robust disaster-related mortality data.
Conclusion 3-1: The heterogeneity of the nation’s systems of death investigation and registration prevents the accurate recording and reporting of disaster-related mortality data and impedes the meaningful analysis and use of these data to improve disaster management. Adoption of uniform practices for collecting, recording, and reporting mortality data is needed, as is improved vertical coordination across stakeholders and improved interoperability of electronic systems among medical certifiers, state vital records offices, and the national vital statistics system.
Conclusion 3-2: The collection and recording of disaster-related mortality data require the medicolegal workforce to value the need for these data and to have the capacity and capability to adopt standardized definitions, practices, and systems.
Federal Efforts to Improve the Quality of Mortality Data
Attempts have been made at a federal level to improve the quality of data collection and reporting and to evaluate the impact of these changes and investments on data quality. In 1986, CDC established the Medical Examiner and Coroner Information Sharing Program (MECISP) in order to improve the quality of death investigations nationwide through the standardization of policies and practices to facilitate communication among stakeholders, and to promote the sharing and use of death investigation data collected by ME/C offices (see Box 3-4).5 Since 1999, CDC has used the uniform disaster mortality case definitions that were developed by MECISP to categorize direct and indirect disaster-related deaths in a standardized manner (see Box 2-2 in Chapter 2) (Combs et al., 1999). The use of uniform case definitions and the inclusion of terms for the role of a disaster on death certificates would support certifiers in providing accurate information needed to improve state- and federal-level mortality statistics
___________________
5Ibid.
(Noe, 2018). However, the adoption of CDC’s uniform case definitions by SLTT death investigation systems remains limited.6
CDC engaged with the ME/C and vital statistics community and found that many are not aware of the case definitions and do not use them in their practice.7 To address this gap, CDC’s National Center for Environmental Health and NCHS released the Reference Guide for Certification of Deaths in the Event of a Natural, Human-Induced, or Chemical/Radiological Disaster (CDC, 2020b) in 2017. It provides guidance on the uniform case definitions and a step-by-step guide for attributing the cause of death and recording that information on the death certificate. CDC’s Disaster-Related Death Scene Investigation Toolkit (CDC, 2017) was also released in 2017 to help improve the quality of data collection at a death scene. In death scene investigations, ME/Cs or other death scene investigators gather information on how and why a death occurred. Death certifiers—which
___________________
6Ibid.
7Ibid.
may be ME/Cs, justices of the peace, or other responsible parties—use that information to determine the cause and manner of death and judge whether the death was related to a disaster. Standardizing the practices for collecting information during death scene investigations could provide death certifiers with more accurate information for determining a death’s disaster-relatedness and accurately reporting that information on the death certificate, which would improve the quality and utility of state and federal mortality statistics.8 However, whether and when to collect data at the scene remains a contentious topic among death scene investigators as this involves resources that their offices do not have, particularly in a disaster. CDC has also provided support for transitioning to and strengthening electronic death registration data systems for mortality data and piloting system improvements.9 In Oklahoma, CDC supported the implementation of an electronic flagging process within the state EDRS to capture data on tornado-attributed deaths (Issa et al., 2019), which is noted in this chapter as a best practice for individual-level disaster reporting.
The Public Health Emergency Preparedness (PHEP) cooperative agreement, which provides funding to strengthen SLTT public health departments, has provided stronger backing for CDC efforts to promote voluntary standardization efforts for mortality data collection and reporting. However, because of the heterogeneity of death investigation systems and the state-level control of death registration procedures, federal efforts to standardize these practices have not found much success.
Public Health Data Systems: COVID-19 Case Study
There are several differences between how morbidity and mortality are classified and reported during a pandemic versus other disasters, such as a fire, blizzard, or hurricane (see Appendix C for an analysis of different methods used during the COVID-19 pandemic). To begin with, the primary data source for morbidity and mortality during a pandemic comes not from vital statistics and the death registration system but rather from an entirely different data system, which is compiled by epidemiologists for public health purposes. Regardless of the presence of a pandemic or major infectious disease outbreak, each state maintains a list of notifiable diseases that require health care providers to report every individual case (i.e., morbidity) that meets the established definition of a notifiable condition to the local or state health department, which in turn maintains a database. Case definitions are established by public health authorities and typically include both the characteristic symptoms caused by the pathogen and a laboratory
___________________
8Ibid.
9Ibid.
test to confirm that an individual has either an active or previous infection with the pathogen of concern. The health department uses this list to identify individuals who may have been in contact with the known cases, test these contacts, and isolate those who are infected. These data are also used for surveillance—for example, to calculate the incidence of new cases and the prevalence of cases in the population. Because the purpose of this database is to manage the outbreak, the focus is on living cases; therefore, the number of deaths caused by the pandemic is based on tracking the survival of the known cases.
Novel pathogens that cause large-scale disasters, such as COVID-19 pose several challenges for counting cases and associated fatalities. Case definitions often include options for naming someone as a “probable” or “presumptive” case based on symptoms and a “confirmed” case only with a positive test, and these case definitions evolve as more is learned about the pathogen. At the peak of the COVID-19 outbreak in New York City, tests were not available in sufficient numbers, and as a result, many individuals with symptoms of COVID-19 were regarded as presumptive cases. While appropriate at the time, this decision resulted in the appearance of a sudden jump in COVID-19 cases and deaths in New York that did not reflect the epidemiological reality (Goodman and Rashbaum, 2020). Further fueling the inaccuracy of case counts is the fact that testing processes—and even case definitions (see Table 3-2)—have varied substantially from state to state. Additionally, when tests are conducted without a provider’s orders, such as with home tests and at freestanding testing sites, it is not clear how positive results collected via these activities are reflected in official public health databases.
Beyond the barriers associated with the collection of reported individual cases and deaths and mirrored by similar operational challenges associated with capturing morbidity data in other natural disasters, the early months of the COVID-19 pandemic have demonstrated ongoing reporting challenges. In order to be included in a public health database, the patient first must seek health care, then the health care provider must decide to order a diagnostic test, then the test must be available, and, in many cases, the patient must then go somewhere else to obtain the test. For many infectious diseases, providers often make treatment decisions empirically, based on symptoms alone, and so test samples are not collected or sent to a laboratory for confirmation. As a result, these unconfirmed cases are not included in initial public health case counts. Because COVID-19 can also be treated empirically—and because tests have been scarce and some health systems have been overwhelmed—relatively healthy people with COVID-19 symptoms have until recently been encouraged to stay home without testing, and thus they remain uncounted. For example, Holtgrave et al. (2020) found that during the height of the COVID-19 outbreak in New York State,
the proportion of those tested and diagnosed varied widely by race and ethnicity; only 6.5 percent of infected Hispanic adults were diagnosed compared to 11.7 percent and 10.1 percent of non-Hispanic Whites and Blacks respectively. As a result, the number of officially recorded COVID-19 cases in the United States almost certainly underestimates the true number of infections, perhaps dramatically. As testing capacity grew, so did the number of positive results, possibly catching up with actual cases and thus not reflecting a true rising incidence of new infections.
Because COVID-19 cases and deaths are likely to be undercounted by public health databases, vital statistics provide an important alternative source of mortality data for COVID-19. However, as discussed in Appendix C, vital statistics systems use different definitions and processes than public health surveillance systems. In early April 2020, NCHS issued guidance indicating that if COVID-19 played a role in a death, this condition should be specified on the death certificate either as the underlying cause of death, where warranted, or as probable or presumed if the circumstances were compelling within a reasonable degree of certainty, even if testing was not done (as it often was not, due to a lack of testing capacity) (CDC, 2020c). Consequently, vital statistics data, which are compiled from death record data, will include some deaths not included in public health case counts. However, as with other reporting for other disasters, some COVID-19 deaths will be missed in both public health case counts and on death records, and other deaths might be inaccurately attributed to COVID-19 on death records.
For instance, in April 2020 vital statistics reports indicated a large increase in individuals dying at home rather than in the hospital (Gillum et al., 2020), especially in New York City (CDC, 2020a; Hogan, 2020). One might infer that many of these in-home deaths were caused, directly or indirectly, by COVID-19, but most were never tested or reported and hence are not included in health department case counts. Some of these deaths might eventually appear in vital statistics reports, but most of these cases will never appear in public health case counts for COVID-19. In the other direction, there have been claims offered, without evidence, that doctors were coached to mark COVID-19 as the cause of death when certifying the death even when it was not in order to inflate the pandemic’s death toll per the vested interests of involved stakeholders (Rosenberg and Rutenberg, 2020). In response, some states do not include deaths in the official count without a mention of COVID-19 in the death record, even if the person had tested positive and was included in the public health surveillance database. In Colorado, this corresponds to a 24 percent reduction, because only 878 of 1,150 deaths (as of May 15, 2020) will be counted (Ingold and Paul, 2020).
Differences in Assessment of Mortality and Morbidity: Pandemics Versus Natural Disasters
Fundamentally, the collection and recording of individual-level mortality and morbidity for pandemics and other natural disasters are similar in terms of approaches that can be used. The major difference is the matter of temporality: hurricanes or wildfires occur over a period of days or weeks (although recovery can take much longer), while a pandemic can stretch into months or years. In all disasters, attributed mortality and morbidity counts and estimates change over time for two reasons: some long-term consequences take time to occur, and all data systems have lags, which vary over time. In pandemics, both of these factors apply, but there is an additional dynamic of ongoing infections. For instance, for the reasons discussed above COVID-19 deaths are sometimes seen as more reliable than case counts. However, deaths lag hospitalizations, the onset of symptoms, and the time of infection by 3 to 4 weeks. The daily number of COVID-19 deaths, therefore, is a lagging indicator of the efficacy of control efforts, and thus a poor guide for deciding whether certain infection control measures, such as social distancing measures, can be relaxed. Deaths may present as a lagging indicator in other types of disasters, such as from radiation exposure following a nuclear disaster, whereas direct deaths may take several weeks to present following the initial impact (CDC, 2018).
Conclusion 3-3: In pandemics and other disasters that evolve over time, trend data on the incidence of new cases are needed to assess the impact of control measures. In these settings care must be taken so that lags and reporting delays and changes in reporting systems do not obscure actual temporal changes.
OPPORTUNITIES TO FACILITATE THE CAPTURE AND REGISTRATION OF INDIVIDUAL DISASTER DEATHS
The ultimate aim of recording and reporting disaster-related deaths is to provide timely, accurate information to support communities affected by the disaster through the disaster lifecycle as well as to help communities be better prepared and resilient when faced with future events. Many entities across this enterprise are working diligently toward the aim of using individual mortality counts to protect the health and well-being of communities, but these efforts would benefit from greater collaboration and coordination across all systems and stakeholders to enable the network of state and federal death investigation and registration systems to function more effectively. At the outset, accurate and descriptive information to indicate, if present, the relationship of a death to a disasters—direct, indirect, or partially attributable to a disaster—needs to be entered into the death
record by the ME/C or medical certifier; these data must then be identified and then correctly coded by NCHS as a disaster-related death in the national databases. Ensuring that these systems function together is essential to improving mortality assessment and will require collaboration among all stakeholders involved with data collection and initial recording (e.g., death scene investigators, ME/Cs, medical certifiers) as well as those parties involved with the secondary recording and reporting of data, such as state and federal vital statistics offices. To work toward achieving this vision, the committee has identified several barriers and best practices in the areas of leadership, standardized attribution of disaster-related mortality, training of certifiers, stakeholder engagement, research, and systems interoperability.
Building Leadership
Above all, strong leadership will be needed to coordinate these efforts and shift the paradigm away from traditional, siloed thinking about death investigation and vital statistics systems. Support from leadership within the SLTT entities involved in death investigation and registration will be needed to develop and operationalize uniform approaches for assessing individual-level mortality. Furthermore, the purposeful inclusion of leaders and other stakeholders from these SLTT systems in the disaster management enterprise would be a step toward elevating the quality of disaster-related mortality data.
Conclusion 3-4: The implementation of an enterprise approach for improving the assessment of mortality and morbidity following large-scale disasters is essential to the implementation of systemic improvements involving multiple, siloed stakeholders. Leadership at all levels—federal, state, local, tribal, and territorial—will be responsible for championing change.
Standardizing Disaster-Related Mortality Attribution
Inconsistent processes for attributing disaster-related mortality is a key barrier that can be addressed by the adoption, in policy and in practice, of uniform case definitions for attributing disaster-related deaths and standardized methods for reporting those deaths across all professions and jurisdictions. Novel data systems developed specifically for this purpose are unlikely to be adopted and will add to the administrative burden of ME/Cs in particular. Therefore, using existing electronic reporting systems would offer greater benefit and be more likely to be supported by stakeholders. For instance, the ability of ME/C case management systems and state-based EDRSs to identify and collect information on individual disaster
deaths could be enhanced through the use of electronic alerts, automatic prompts, or dropdown boxes that would provide real-time support to the medical certifier in determining whether a death is related to the disaster and to what degree, per the framework developed by the committee (see Recommendation 2-1 in Chapter 2). These tools, which could be triggered to automatically appear following a Stafford Act disaster declaration or at the request of state or local leadership, would provide in-the-moment decision-making support to medical certifiers, including inserting descriptive terminology into the death record and allowing vital records staff to code and track flagged deaths (see Figure 3-4). For example, within the death record, the medical certifier could be asked whether the death is disaster related (Y/N), with definitions provided along with further Y/N prompts to indicate whether the death is direct, indirect, or partially attributable.
Beyond working to reduce inter-professional variation in the capture of direct deaths, which are most likely to be captured by ME/Cs as part of the death investigation system, such tools could provide value to other medical certifiers who are more likely to encounter indirect or partially attributable deaths within the clinical care environment. Furthermore, efforts to improve access to background health data by medical certifiers, such as electronic medical records, would assist medical certifiers in making more nuanced determinations concerning indirect and partially attributable disaster deaths.
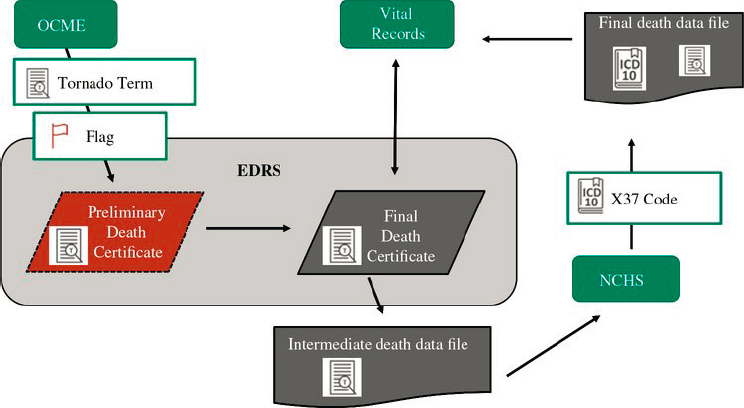
NOTE: EDRS = electronic death registration system; NCHS = National Center for Health Statistics; OCME = Office of the Chief Medical Examiner.
SOURCE: Issa et al., 2019. Reproduced with permission.
Training Medical Certifiers
As described in the previous section, certain medical certifiers, such as medical doctors and nurse practitioners, typically receive little or no formal and recurring training in how to appropriately enter data into the death record, are unfamiliar with the data field, and are unaware of how to indicate the degree of attribution within the data fields of the death record (Brooks and Reed, 2015). Medical examiners and coroners are more likely to be familiar with how to enter data into EDRSs, but due to their professional philosophy, administrative policy, or training on disaster-death attribution they often fail to complete the death record accurately. Errors and missing information in the death record are an immediate barrier to the accurate recording and reporting of disaster-related deaths. Consequently, vital statistics offices encounter difficulty in coding the causes of death accurately and completely. Addressing this issue will require medical certifiers to receive better training that is tailored to their profession and to have access to resources within death investigation and registration systems to support them in carrying out this work—for example, and as described in the section above, user-friendly interfaces for e-filing death records and access to electronic health records (EHRs). In some cases, mandatory training may be felt to be less effective due to the lack of immediate salience for trainees, particularly those medical certifiers who are unlikely to regularly complete death records. In addition to requiring mandatory training, data systems should be designed to be intuitive and integrated into routine, day-to-day systems so that just-in-time training is sufficient. In terms of death registration training, lessons may be learned from the widespread implementation of mandatory training for opioid prescribers.
The use of existing disaster-related mortality tools developed by CDC and other agencies should also be promoted among medical certifiers, vital statistics staff, and emergency management staff alike. Importantly, most direct disaster-related deaths will be certified by a medical examiner or coroner because they are unnatural deaths. However, indirect or partially disaster-related deaths may not fall under the auspices of the ME/C, highlighting the critical importance of training and building capacity among all medical certifiers, not just those of the medicolegal death investigation system (e.g., ME/Cs), about how to appropriately handle disaster-related deaths. A standard system that can query for associated causation would assist providers who are not routinely involved in death investigations. Furthermore, the auditing of death records during declared disasters could offer an opportunity to clarify or add information. Enhancing training and support for medical certifiers involved in the medicolegal death investigation and death registration systems will require consistent funding and support. Additional resources will also be needed by state and local agencies to support quality assurance and investigations.
Engaging Stakeholders
The coordination, communication, and integration of efforts among ME/C, vital statistics, public health and epidemiology, emergency medical services, and emergency management stakeholders are fundamental to aligning efforts and enhancing collaboration to realize better mortality statistics. Leaders, decision makers, and practitioners at all levels need to understand the value of accurately collecting and reporting vital statistics data. Bringing together stakeholders from across the death registration system—particularly from the local and state levels—into the disaster planning, mitigation, response, and after-action sessions of EMS and law enforcement would also help to improve stakeholder buy-in.
The inclusion of ME/Cs in public health and disaster planning provides an opportunity for all entities to determine what data are most essential for local and regional use, what resources are needed, and how they can work together in both routine and emergency situations to carry out common goals. Several states have already made efforts to enhance partnerships across these siloed entities. In Florida, for example, partnerships among the state vital records system, county medical examiners, funeral directors, and professional associations are supported by state-level coordination by the State Commission. In Oklahoma, vital records officials are actively engaged in the emergency response and the immediate recovery period in order to provide death certificates on the spot to people who need them to access support services and settle legal affairs such as insurance claims and wills. Additionally, some medicolegal death investigation systems are sufficiently robust, such as Virginia and New Mexico, to have an epidemiologist on staff to initiate and organize disaster-related data collection and databases. In other systems, ME/Cs would benefit from developing a relationship with SLTT epidemiologists in order to mobilize epidemiology resources in anticipation of disasters typical for the regions as well as for pandemics and smaller infectious disease outbreaks. These functioning professional relationships provide a foundation for further collaboration to benefit data collection, recording, and use following disasters.
The multitude of stakeholders involved and the varied contexts in which they perform their work makes the adoption of new uniform methods for collecting and recording individual mortality data challenging. However, gaining stakeholder buy-in is especially critical for capturing indirect and partially attributable deaths, which are the most variable in mortality counts from disasters and which require a common approach for attribution and categorization by certifiers. Best practices for engaging stakeholders from across the enterprise include improving the function of these systems to reduce redundancy in data entry and facilitate easier attribution of disaster-related mortality by medical certifiers as well as providing clear evidence of the value of collecting and recording these data
accurately and consistently. Access to training and the provision of active support by professional associations such as NAME and appropriate licensing boards and training by state registrars would also be beneficial, as these organizations play an important role in implementing change within these professions. There may be useful lessons that can be learned from the implementation of opioid death reporting systems (CDC, 2019).
Building an Evidence Base
Strengthening death investigation and registration systems has value beyond the collection of improved data for disaster-related deaths, but there is a lack of real-world evidence available to demonstrate the value of investing in these improvements. This lack can be addressed by conducting pilot projects and other real-world research to test modified practices and protocols for mortality reporting to improve the function of these systems and to increase stakeholders’ capacity to consistently capture disaster-related mortality. These pilot projects can be followed with evaluation components to highlight the value of merging mortality and morbidity data over the lifecycle of various disasters and to provide critical information to planners and responders. Academic centers, specifically schools of public health, could potentially be used to determine assessment strategies and expand disaster epidemiology research capacity (see Chapter 4) without overburdening state and local public health and emergency response agencies.
Improving System Standards and Interoperability
Mortality data in the United States largely sit in silos because systems were not designed to be interoperable and share information with each other (Borfitz, 2019). Improving interoperability among ME/C case management systems, other mortality records systems, and state- and federal-level electronic death registration systems would enable data to be collected and reported more rapidly, reliably, and accurately. For instance, ME/C case management systems often include rich data that are not entered into death records created in the EDRS due to the administrative burden on ME/Cs to enter these data twice. Furthermore, individuals affected by disasters do not always remain in the declared disaster area and often cross jurisdictional and state lines, further underscoring the necessity of interoperability systems and easy data sharing across stakeholders.
Immediate opportunities to address this barrier include facilitating the transition to fully electronic ME/C case management and death registration systems that are interoperable and also developing and piloting new methods for flagging, including dropdown boxes, additional prompting for descriptive information about disaster-relatedness within those systems,
and supporting in-the-moment decision making by medical certifiers as well as geocoding the place of death and place of residence. As mentioned previously, it is preferable to use and improve existing data systems rather than to develop novel systems. See Box 3-5 for examples of some of these efforts at the state level. Ultimately, mortality data need to be recorded and reported in a manner that can be fed back in meaningful ways to SLTT agencies and communities affected by disasters. As NVSS continues to strengthen and improve, there will be more opportunities to share data across and among states through better, more interoperable electronic data systems. Investing in the data infrastructure used for NVSS to collect, record, report, and use data on a daily basis will also strengthen disaster response capabilities. NCHS has worked with states to strengthen and improve the interoperability of their electronic death registration systems, and improving the quality of data captured on death records is a major priority for NCHS and NVSS. Vital statistics model law could be updated to incorporate data sharing and collection during disasters (e.g., standardized operation of electronic death records).
Technologies are also being developed to improve interoperability and support data sharing practices among ME/C systems, such as the Fast Healthcare Interoperability Resources standard for mortality reporting (Borfitz, 2019). An ideal integrated, interoperable system could provide immediate clinical decision support for death attribution, connectivity to
funeral homes, and a real-time feedback loop to vital statistics and electronic death registration systems, with reports flowing to state authorities and NCHS. Better data sharing between EHRs and the electronic death registration systems could streamline processes and provide additional information on deaths. Challenges and opportunities with respect to data sharing for population-level mortality and morbidity data will be explored in more detail in Chapter 4.
Continuity of Data Collection and Recording During Disasters
The difficulty of maintaining electronic data systems’ continuity during disasters is another barrier to the collection and reporting of individual-level mortality data. Flexible systems that are well tooled for day-to-day use are more effective than ad hoc systems or systems designed only for large-scale events. Research efforts should focus on evaluating continuity mechanisms for electronic systems so that these are robust enough for everyday use but also able to adapt and flex during a disaster. It is important to try to minimize the implementation of new procedures and practices during a crisis. For instance, Oklahoma has designed its electronic death registration system to be flexible for capturing information at large scale as well as for day-to-day use, for exercising the system, and for responding to smaller scale events (Baker, 2019). In Florida, surveillance systems are used continuously—not only deployed for disasters—and the system is flexible enough to expand beyond syndromic surveillance.
CONSIDERATIONS SPECIFIC TO THE COLLECTION OF MORBIDITY DATA
As described in Chapter 2, morbidity is a complex concept that covers a range of health outcomes from the physical to psychological, including cardiovascular, gastrointestinal, and respiratory diseases; physical injuries; and mental health outcomes. While a cause of death is sometimes difficult to determine, mortality itself is easier than morbidity to define. The collection and reporting of morbidity data, therefore, remains a persistent gap and the limited systems, tools, and practices associated with the collection of individual morbidity data cannot be evaluated to the same degree as mortality data. There are no standards or dedicated systems in place for the collection and recording of reported morbidities following disasters or for the use of data on morbidities. The collection of data about disaster-related morbidities in a uniform manner is challenging, given how broadly they are defined, the influence of pre-existing and co-morbid conditions on post-disaster health outcomes, the variation across disaster types, and
the difficulties associated with mining morbidity data from across a broad network of unique federal, SLTT, and health care systems.
Although they are certainly in need of improvement, the basic systems, mechanisms, and processes for the collection and recording of disaster-related mortality data already exist to some degree; this is not, however, the case for disaster-related morbidity data at the individual level. As with mortality, the variability in the capacities of SLTT health departments—and the fact that many are under-resourced—makes the creation of a standard system for collecting individual-level morbidity data especially difficult.
There are many possible data sources for tracking morbidities, particularly within the health care systems, which already generates individual-level morbidity data. These include hospital admissions data, EHRs, syndromic surveillance systems, records from disaster medical assistance teams, and data from sheltering operations (CDC, 2016) (see Box 3-6). However, these data are not necessarily captured in a manner that would allow for disaster attribution. There is also no consensus as to what information about morbidities that end users such as public health or emergency planners, health care systems, and SLTT and federal agencies need in order to respond better to disasters. As a result, there is also no consensus on which morbidities, indicators of morbidities, or data sources should be consistently tracked in common types of disasters (e.g., hurricanes, blizzards, tornadoes, pandemics/epidemics) (CDC, 2016).
Conclusion 3-5: Collecting morbidity data presents an additional challenge due to the large quantity of possible outcomes and data available across multiple unique systems. Understanding which data are of greatest value and how these data can be used to inform disaster management requires more research.
Conclusion 3-6: Standards for morbidity data are needed across different types of disasters. A standard dataset by disaster type would dramatically improve the uniform collection of morbidity data. This will improve the usability and actionability of these data.
The lack of data sharing and the inadequate interoperability of systems at all levels remain substantial barriers. EHRs, the most obvious source of electronic data on morbidities, and the systems that contain them are varied. Many of these systems lack the capacity to push important data to relevant parties in real time. For many, it is not yet possible using available EHR technology to aggregate and analyze large volumes of morbidity data to support real-time decision making. While traditional data sources such as hospital discharge data, EHRs, reportable disease systems, and others could be tapped to develop estimates of morbidity, these systems can be easily disrupted by the disaster, may fail to capture those individuals who do not present for care in a clinical setting, and are currently not suited to rapidly collecting and pushing out morbidity data to public health and disaster management stakeholders (Schnall et al., 2011). The experiences of first responders during the 2018 Camp Fire in Paradise, California, illustrate the need of localities to have access to shared morbidity data through interoperable systems. As described by officials in Paradise, the lack of rapid access to actionable data from the county level required Paradise responders to rely on local hospital data to guide their initial response and recovery efforts. Other county health departments have invested heavily in data systems that allow for greater collection and use of real-time mortality and morbidity data and have benefited from embracing greater collaboration between the public health and emergency management departments at a county level (see Box 3-7). However, investment in these data systems is dependent on available resources and is, therefore, not a realistic opportunity for all health departments. Additional investment is required from the federal level to implement systems that allow for greater interoperability and coordination and to use existing data systems for the collection of morbidity data following disasters.
Addressing these operational challenges to the collection of disaster-related morbidity data will be necessary in order to systematically and accurately capture the effects of disasters on health and to guide the implementation of changes in response and recovery to future disasters.
Standardizing data collection processes specific to morbidity after disasters can be built into the nation’s operational disaster response function, in a way that is similar to (but with different collection procedures) that proposed for mortality data collection. Various strategies could be considered to more effectively and systematically capture existing data on significant disaster-related morbidities. For example, applied machine learning techniques from EHRs could reveal trends in emergency department and acute care facility use that may provide a better profile of morbidity. The implementation of these strategies will require substantial investment in the development of procedures and best practices related to the types of morbidity data to be collected (see Chapter 2) and the processes for recording such data.
Additionally, the absence of established standards and guidance regarding what types of morbidity data should be collected provides an opportunity for research to be conducted to determine what types of morbidities and morbidity indicators are most essential for collection following large-scale disasters (see Chapter 4 for further discussion on the use of morbidity data to develop population estimates). As described in Chapters 1 and 2,
exclusively focusing on the collection of significant morbidities would likely fail to capture the data for less immediately critical but far more prevalent and costly morbidities related to the social determinants of health, such as respiratory diseases, mental health outcomes, and exacerbations of existing co-morbidities. See Appendix D for case studies describing the relationship between the social determinants of health and disaster-related morbidity and mortality. Defining which morbidity data to collect is a critical first step to building the capability within the system and stakeholders to collect and use these data. This foundation can then be developed further to facilitate the integration of data on social and environmental factors to better contextualize community vulnerabilities and programmatic targets for prevention and mitigation. Therefore, it will be necessary to invest in an ongoing process to develop, validate, and disseminate national standards for data collection concerning the key morbidities caused or exacerbated by specific types of disasters (see Recommendation 3-3).
Use of Electronic Health and Claims Data to Assess Morbidity: COVID-19 Case Study
The recent COVID-19 pandemic presents a potential model system for the recording and reporting of health data related to the virus, which could be replicated for morbidity data in future disasters. As noted in the section above on Public Health Data Systems, public health surveillance systems focus on cases (i.e., morbidity) rather than deaths. Nevertheless, much more needs to be known about the symptoms that these individuals exhibit, how many are hospitalized, and many other factors in order to comprehensively assess disaster-related morbidity. To address these issues, epidemiologists and health service researchers are using a variety of existing electronic data, such as claims data and EHRs. Accurately collecting, cleaning, and analyzing these data present enormous operational and analytical challenges for any type of large disaster. In the midst of a pandemic, these challenges need to be rapidly addressed due to an urgent need for these data to inform response.
Already, guidance has been developed concerning the use of COVID-19 health care claims data (Bohl and Roozeboom-Baker, 2020) and EHRs, which could be applied more broadly to other disaster-related mortalities and morbidities. It is important to consider a basic fact concerning these types of data: neither claims data nor EHR data were designed for the purposes of research. Claims data are designed for reimbursement purposes, and EHR data are designed for the recording of patient presentation, diagnosis, and treatment. Furthermore, as described earlier in this chapter, COVID-19 cases are likely widely under-reported, a deficit that will carry over to such data sources. However, the identification of many (but not
all) patients admitted with COVID-19 can still be captured through a careful examination of individual claims (either using the newly released ICD-10 code for COVID-19 or by examining respiratory conditions common to COVID-19 infection) for hospital inpatient and outpatient services, skilled nursing and long-term care, and professional services (Bohl and Roozeboom-Baker, 2020). The use of EHR data presents its own unique challenges. The process used to extract, clean, and check COVID-19-related EHR records is painstaking and requires careful fact checking beyond the use of commonly employed software that sorts this type of data (Robbins, 2020). Nevertheless, in the absence of a formal reporting process for morbidity data, analysis of the types of data described here—and the processes being developed around COVID-19 identification—can inform future disaster morbidity research.
USE OF INDIVIDUAL-LEVEL MORTALITY AND MORBIDITY DATA TO INFORM DISASTER MANAGEMENT
As discussed in Chapter 2, individual-level mortality and morbidity data have a wide range of uses, but the data’s primary value lies in preventing further health impacts of a disaster during response and recovery as well as in planning and mitigation to reduce the human impact of future disasters. These data have value for a broad range of stakeholders, including community members, public health practitioners, emergency management personnel, policy makers and political leadership, federal agencies such as FEMA, CDC, and the Department of Health and Human Services, and many others.
Barriers to and Best Practices for Use of Individual-Level Mortality and Morbidity Data
Data sharing and system interoperability within and across jurisdictions are major barriers to the operationalization of individual-level mortality data. Establishing data sharing agreements during interim periods between disasters as a best practice could address these barriers. In current practice, localities are often expected to share data with state and federal authorities without reciprocity. Instead, data sharing would benefit from the data flowing in a top-down as well as a bottom-up direction. A primary value of these data is to support local communities, so communities and local-level authorities should receive timely and actionable mortality data shared from the state and federal government systems.
Conclusion 3-7: Access to federal and state mortality and morbidity data is essential, but data access does not equate to actionability of
these data at the local level. If data are to be actionable, localities require the tools needed to read, analyze, and display data received from the federal or state level in a meaningful way as well as the expertise and capacity to use these data in decision making.
Research Priorities for Individual Mortality and Morbidity Counts
Several research gaps related to the use of individual mortality data need to be addressed in order to improve the quality of the data and to increase the understanding of which types of data are most valuable for various stakeholders at different points in the disaster lifecycle. A body of practical evidence demonstrates how these data could be used to inform practice and could be included in pilot projects with evaluative components. Cost-effectiveness research would also be useful in gaining buy-in from policy makers and other stakeholders for investment system improvements, practices for collecting and reporting individual-level mortality data, and training for medical certifiers.
RECOMMENDATIONS
REFERENCES
ASPE (Assistant Secretary for Planning and Evaluation). 2013. Assessing the status and prospects of state and local health department information technology infrastructure. https://aspe.hhs.gov/basic-report/assessing-status-and-prospects-state-and-local-health-department-information-technology-infrastructure (accessed June 11, 2020).
Bagwell, D. 2019. Session 4: Current capabilites in assessing and using morbidity and mortality data during the inter-disaster period. Presentation at the August 29, 2019, public meeting of the National Academies of Sciences, Engineering, and Medicine’s Committee on Best Practices in Assessing Mortality and Significant Morbidity Following Large-Scale Disasters, Washington, DC.
Baker, K. 2019. Session 5: Looking forward—best practices and tools for assessing and using morbidity and mortality data during a large-scale disaster in real time. Presentation at the August 30, 2019, public meeting of the National Academies of Sciences, Engineering, and Medicine’s Committee on Best Practices in Assessing Mortality and Significant Morbidity Following Large-Scale Disasters, Washington, DC.
Bohl, A., and M. Roozeboom-Baker. 2020. A COVID-19 primer: Analyzing health care claims, administrative data, and public use files. https://www.mathematica.org/ourpublications-and-findings/publications/a-covid-19-primer-analyzing-health-care-claimsadministrative-data-and-public-use-files (accessed June 5, 2020).
Borfitz, D. 2019. CDC creating a “ruckus” around mortality reporting. AITrends, July 5. https://www.aitrends.com/ai-world-government/cdc-creating-a-ruckus-around-mortality-reporting (accessed July 1, 2020).
Brooks, E. G., and K. D. Reed. 2015. Principles and pitfalls: A guide to death certification. Clinical Medicine & Research 13(2):74–82.
Brown, E., B. Reinhard, and R. Thebault. 2020. Which deaths count toward the COVID-19 death toll? It depends on the state. Washington Post, April 16.
Bryant, C. D. 2003. Handbook of death and dying. Thousand Oaks, CA: Sage Publications.
CDC (Centers for Disease Control and Prevention). 2015. Death investigation systems. https://www.cdc.gov/phlp/publications/coroner/death.html (accessed July 16, 2020).
CDC. 2016. A primer for understanding the principles and practices of disaster surveillance in the United States. Atlanta, GA: Centers for Disease Control and Prevention.
CDC. 2017. Death scene investigation after natural disaster or other weather-related events: A toolkit. https://www.cdc.gov/nceh/hsb/disaster/docs/DisasterDeathSceneToolkit-P.pdf (accessed July 1, 2020).
CDC. 2018. Determining deaths from a radiation emergency. https://www.cdc.gov/nceh/radiation/emergencies/determinedeaths.html (accessed July 31, 2020).
CDC. 2019. Enhanced state opioid overdose surveillance. https://www.cdc.gov/drugoverdose/foa/state-opioid-mm.html (accessed June 5, 2020).
CDC. 2020a. Preliminary estimate of excess mortality during the COVID-19 outbreak—New York City, March 11–May 2, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e5.htm (accessed June 5, 2020).
CDC. 2020b. Vital statistics reporting guidance. https://www.cdc.gov/nchs/nvss/reportingguidance.htm (accessed June 5, 2020).
CDC. 2020c. Guidance for certifying deaths due to Coronavirus Disease 2019 (COVID-19). https://www.cdc.gov/nchs/data/nvss/vsrg/vsrg03-508.pdf (accessed July 1, 2020).
Combs, D. L., L. E. Quenemoen, R. G. Parrish, and J. H. Davis. 1999. Assessing disaster-attributed mortality: Development and application of a definition and classification matrix. International Journal of Epidemiology 28(6):1124–1129.
Connecticut State Department of Public Health. 2020. Syndromic surveillance. https://portal.ct.gov/DPH/Epidemiology-and-Emerging-Infections/Syndromic-Surveillance (accessed July 17, 2020).
DeSalvo, K., and C. Petrin. 2017. From Katrina to wildfires: Leveraging technology in disaster response. https://www.healthaffairs.org/do/10.1377/hblog20171113.545312/full (accessed June 5, 2020).
FEMA (Federal Emergency Management Agency). 2019. Best practices for assessing mortlity and significant morbidity following large-scale disasters: Charge to the Committee. PowerPoint Presentation. Presented at the May 28, 2019, public meeting of the National Academies of Sciences, Engineering, and Medicine’s Committee on Assessing Mortality and Significant Morbidity Following Large-Scale Disasters. Washington, DC. http://webapp.nationalacademies.org/napar/projectview.aspx?key=51640#MeetingId11176 (accessed September 1, 2020).
Gillum, J., L. Song, and J. Kao. 2020. There’s been a spike in people dying at home in several cities. That suggests coronavirus deaths are higher than reported. https://www.propublica.org/article/theres-been-a-spike-in-people-dying-at-home-in-several-cities-that-suggests-coronavirus-deaths-are-higher-than-reported (accessed June 5, 2020).
Goodman, J. D., and W. K. Rashbaum. 2020. N.Y.C. death toll soars past 10,000 in revised virus count. The New York Times, April 14.
Hanzlick, R. 1997. The Centers for Disease Control and Prevention’s Medical Examiner/Coroner Information Sharing Program (MECISP). Journal of Forensic Science 42(3):531–532.
Hanzlick, R. 2006. Medical examiners, coroners, and public health: A review and update. Archives of Pathology and Laboratory Medicine 130(9):1274–1282.
Health Monitoring. 2020. What is EpiCenter? https://www.health-monitoring.com/syndromic-surveillance-epicenter (accessed July 17, 2020).
Hogan, G. 2020. Staggering surge of NYers dying in their homes suggests city is undercounting coronavirus fatalities. https://gothamist.com/news/surge-number-new-yorkers-dying-home-officials-suspect-undercount-covid-19-related-deaths (accessed June 5, 2020).
Holtgrave, D. R., M. A. Barranco, J. M. Tesoriero, D. S. Blog, and E. S. Rosenberg. 2020. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Annals of Epidemiology 48:9–14. https://doi.org/10.1016/j.annepidem.2020.06.010.
Horney, J. 2017. Disaster epidemiology: Methods and applications. New York: Academic Press.
Ingold, J., and J. Paul. 2020. Nearly a quarter of the people Colorado said died from coronavirus don’t have COVID-19 on their death certificate. Colorado Sun, May 15.
IOM (Institute of Medicine). 2003. Medicolegal death investigation system: Workshop summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/10792.
Iowa Board of Medicine. 2020. Guidelines for reporting and certifying COVID-19 deaths. https://medicalboard.iowa.gov/document/guidelines-reporting-and-certifying-covid-19-deaths (accessed June 4, 2020).
Issa, A. N., K. Baker, D. Pate, R. Law, T. Bayleyegn, and R. S. Noe. 2019. Evaluation of Oklahoma’s electronic death registration system and event fatality markers for disaster-related mortality surveillance—Oklahoma USA, May 2013. Prehospital and Disaster Medicine 34(2):125–131.
Jones, K. 2019. Session 2: Florida system for assessing post-disaster mortality and significant morbidity—case study. Presentation at the August 29, 2019, public meeting of the National Academies of Sciences, Engineering, and Medicine’s Committee on Best Practices for Assessing Mortality and Significant Morbidity Following Large-Scale Disasters, Washington, DC.
Kulkarni, P. A., R. S. Noe, and M. Warner. 2015. Sensitivity of disaster-related mortality surveillance after Hurricane Sandy—New Jersey, 2012–2013. Paper presented at the 2015 Annual Meeting of the Council of State and Territorial Epidemiologists, Boston, MA.
Louisiana Department of Health. 2020. LEERS electronic death registration—Information for physicians. http://ldh.la.gov/index.cfm/page/913 (accessed July 1, 2020).
Madsen, A., and E. Begier. 2013. Improving quality of cause-of-death reporting in New York City. Preventing Chronic Disease 10:E118.
McKibben, B. 2020. Racism, police violence, and the climate are not separate issues. The New Yorker. https://www.newyorker.com/news/annals-of-a-warming-planet/racism-police-violence-and-the-climate-are-not-separate-issues (accessed September 1, 2020).
Montana DPHHS (Department of Public Health and Human Services). 2020. Guidance for certifying COVID-19 deaths. https://dphhs.mt.gov/vitalrecords/certificationofcovid-19 (accessed June 4, 2020).
NAPHSIS (National Association for Public Health Statistics and Information Systems). 2020a. Jurisdictions. https://www.naphsis.org/systems (accessed June 8, 2020).
NAPHSIS. 2020b. State and Territorial Exchange of Vital Events (STEVE). https://www.naphsis.org/steve (accessed July 1, 2020).
New Jersey Department of Health. 2017. Meaningful use—syndromic surveillance. https://www.nj.gov/health/meaningfuluse/syndromic.shtml (accessed July 17, 2020).
Noe, R. 2018. Chapter 5—Applications: Disaster-related mortality surveillance: Challenges and considerations for local and state health departments. In J. A. Horney (ed.), Disaster epidemiology: Methods and applications. London: Academic Press. Pp. 55–63.
Noe, R. 2019. Session 3: Current capabilities in assessing and using morbidity and mortality data in real time during a large-scale disaster. Presentation at the August 29, 2019, public meeting of the National Academies of Sciences, Engineering, and Medicine’s Committee on Best Practices for Assessing Mortality and Significant Morbidity Following Large-Scale Disasters, Washington, DC.
NSTC (National Science and Technology Council). 2016. Strengthening the medicolegal-death-investigation system: Improving data systems. https://obamawhitehouse.archives.gov/sites/default/files/microsites/ostp/NSTC/strengthening_the_medicolegal_death_investigation_system_final.pdf (accessed July 3, 2020).
NVSS (National Vital Statistics System). 2017. Vital statistics reporting guidance: A reference guide for certification of deaths in the event of a natural, human-induced, or chemical/radiological disaster. https://www.cdc.gov/nchs/data/nvss/vsrg/vsrg01.pdf (accessed July 1, 2020).
Pennsylvania Department of Health. 2020. Additional guidance for coroners & medical examiners: Reporting of deaths attributed to COVID-19. https://www.health.pa.gov/topics/Documents/Reporting-Registries/SRN%202020-14%20Additional%20Guidance%20for%20Coroners%20and%20Medical%20Examiners%20-%20Reporting%20of%20Deaths%20Attributed%20to%20COVID-19.pdf (accessed July 1, 2020).
Robbins, R. 2020. Hospital records hold valuable COVID-19 data. Making it usable is time-consuming work. https://www.statnews.com/2020/05/27/mass-general-brigham-covid19-genetics-biobank (accessed June 5, 2020).
Rocha, L. A., C. Q. Fromknecht, S. D. Redman, J. E. Brady, S. E. Hodge, and R. S. Noe. 2017. Medicolegal death scene investigations after natural disaster- and weather-related events: A review of the literature. Academic Forensic Pathology 7(2):221–239.
Rosenberg, M., and J. Rutenberg. 2020. Fight over virus’s death toll opens grim new front in election battle. The New York Times, May 9.
Ruiz, L., B. M. Posey, M. A. Neuilly, M. K. Stohr, and C. Hemmens. 2018. Certifying death in the United States. Journal of Forensic Science 63(4):1138–1145.
Schnall, A. H., A. F. Wolkin, R. Noe, L. B. Hausman, P. Wiersma, K. Soetebier, and S. T. Cookson. 2011. Evaluation of a standardized morbidity surveillance form for use during disasters caused by natural hazards. Prehospital & Disaster Medicine 26(2):90–98.
Slavova, S., D. B. O’Brien, K. Creppage, D. Dao, A. Fondario, E. Haile, B. Hume, T. W. Largo, C. Nguyen, J. C. Sabel, D. Wright, and members of the Council of State and Territorial Epidemiologists Overdose Subcommittee. 2015. Drug overdose deaths: Let’s get specific. Public Health Reports 130(4):339–342.
Snohomish County. 2020. Cause and manner of death. https://snohomishcountywa.gov/806/Cause-Manner-of-Death (accessed July 31, 2020).
Ventura County Health Care Agency. 2017. Acceptance of meaningful use data. http://www.vchca.org/acceptance-of-meaningful-use-data#:~:text=Syndromic%20Surveillance%20Data%20Submission%3A,%3A%20805%2D981%2D5331 (accessed July 17, 2020).










































