1
Introduction
In the hours, days, weeks, and months following a disaster, coming to terms with the event’s impact on human life is critical for affected communities, responders, and those watching the aftermath unfold from afar. Assessments of disaster-related mortality and morbidity ascribe a quantitative value to a traumatic event, and these assessments hold deep emotional, societal, financial, and logistical value. These data can assist a community in memorializing what has been lost; inform and justify the scale of a response; determine access to resources; and strengthen mitigation and response practices to save lives in the future. Furthermore, as climate change alters the frequency and severity of many natural disasters and the map of global vulnerability shifts and expands, these data can provide an accounting of the financial and societal costs of failure to prevent or mitigate the effects of climate change. These data are imperative for long-range planning related to large-scale infrastructure projects and even for addressing questions of where to build and whether to rebuild in the context of our changing world. Accurately quantifying mortality and morbidity caused by disasters is foundational to protecting the public’s health and well-being in myriad ways. However, the practices, systems, and stakeholders that exist across the nation to support these essential efforts are less coordinated, robust, and reliable than they should be. These systematic inadequacies—both simple and complex—hamper the nation’s capability to respond more effectively in moments of crisis and limit the ability to proactively and economically mitigate the effects of the next disaster. This report describes the importance of accurately assessing mortality and morbidity data and the diverse uses of these data. In addition to reviewing the current landscape
of practices and methods used in the field and highlighting existing barriers and challenges, the report provides stakeholders with a blueprint for action to enhance the collection, reporting, and use of accurate information on the mortality and morbidity of major disasters.
STUDY BACKGROUND AND SCOPE
Following the October 2018 passage of the Federal Aviation Administration Reauthorization Act, which contained the Disaster Recovery Reform Act, the Federal Emergency Management Agency (FEMA) tasked the National Academies of Sciences, Engineering, and Medicine (the National Academies) to carry out a consensus study of best practices for conducting mortality and morbidity assessments following large-scale disasters. The Statement of Task (see Box 1-1) developed by FEMA charged the consensus study committee with reviewing and describing the current state of the field of assessing disaster-related mortality and morbidity. This includes examining current practices and methods for collecting, recording, sharing, and using data across state, local, tribal, and territorial (SLTT) stakeholders and evaluating best practices and areas for future resource investment.
The Statement of Task directs the committee to focus on large-scale disasters1—natural or manmade—as defined in the Robert T. Stafford Disaster Relief and Emergency Assistance Act (Stafford Act) (see Box 1-2). The Statement of Task also makes clear that in-depth exploration or recommendations that are directly related to syndromic surveillance, long-term surveillance of health impacts related to disasters, or the surveillance of emergency responders are outside the scope of the committee’s work.
The concepts of mortality and morbidity are used heavily throughout the report. The term “mortality” is widely used to mean a death or deaths that occur regardless of cause. The term “morbidity” generally means a disease(s) or injury(ies) of varying degree of severity. At the end of this chapter, there is a section titled Terminology Choices and Key Concepts, where more context is provided for the various terms and concepts used throughout this report. These include an explanation of the term “significant morbidity,” per the language used in the Statement of Task, as well as a discussion of the vocabulary used for the attribution of both mortality and morbidity to a disaster, among others.
___________________
1 The Stafford Act declaration in response to the ongoing coronavirus pandemic resulted in the inclusion of the pandemic in the committee’s deliberation and report. See Appendix C for a paper developed independently by two committee members on the assessment of coronavirus mortality.
Inclusion of COVID-19
Despite the original request for the committee to focus its deliberations on disasters other than infectious disease-related disasters, the emergence of the coronavirus disease 2019 (COVID-19) pandemic and subsequent issuance of a Stafford Act declaration in March 2020 for all states ultimately led to the selective inclusion of COVID-19 in the report. In the weeks following the emergence and initial spread of COVID-19, before transmission was widespread domestically, the committee did not consider the outbreak to be within the scope of the report. However, as the number of cases increased within the borders of the United States, it became clear that the administrative, logistical, and methodological challenges illustrated in the early attempts of assessing COVID-19-related mortality and morbidity mirrored many of the same issues found in other large-scale
disasters. Following the Stafford Act declaration, the committee requested confirmation from the study sponsor that discussions of COVID-19 could be included in the report. FEMA provided its approval for the inclusion in May 2020. The committee chose to include a few illustrative examples throughout the report from the COVID-19 pandemic regarding mortality and morbidity assessment to highlight overlapping logistical and methodological barriers with other large-scale disasters. In short, the committee believes that experiences from COVID-19 illustrate the same need for coordination across stakeholders and consistent policies and systems to accurately identify and report cases as in other natural disasters. The pandemic also provides clear and timely examples of the uses of different methods for assessing morbidity and mortality, which help to illustrate their comparative strengths and weaknesses for different purposes.
At the same time, the widespread transmission of COVID-19 in the United States occurred toward the end of the committee’s deliberation period and the committee did not have sufficient opportunity to consider the full implications of COVID-19 (a pandemic that remained very active and evolving even at the time of the report’s final editing) and also did not wish for the contentious issues surrounding COVID-19 to overtake the core messages of the report. As a result, the committee has included in Appendix C a separate thought piece, which was independently authored by two committee members, on early experiences of assessing COVID-19 mortality and morbidity. This paper provides additional real-time context and support for the report’s core recommendations by highlighting overlapping methodological, administrative, and logistical challenges with other disasters and unique features of the pandemic—and a more focused analysis of morbidity and mortality estimation challenges in this public health emergency than what is provided in the main body of the report.
Inclusion of Social Determinants of Health
An in-depth focus on the socio-environmental dimensions of health and how these factors function to heighten vulnerabilities to disasters (e.g., association between secondary exposures, such as contaminated water supplies post-disaster; pre-existing economic disparities; and exacerbation of gastrointestinal illnesses) (CDC, 2005; Furey et al., 2007; Marinova-Petkova et al., 2019; Nigro et al., 2011; Yee et al., 2007) was determined to be outside the scope of this study. For this reason, this report does not provide a detailed analysis of these issues or dedicated recommendations on strategies for integrating social determinants of health information into mortality and morbidity data systems or how these data, once collected, could inform the actions of the disaster management enterprise. The committee, however, feels strongly that the lack of such in-depth discussion is purely a reflection of the limited scope of the study’s charge and not
a reflection of the fundamental importance of these issues. In particular, while research documenting stark disparities in the impacts of disasters on underserved and historically disadvantaged communities is relatively robust, dedicated research on how to mitigate or eliminate these disparities is sparse and much needed. For instance, there would be tremendous value in strengthening the knowledge base regarding the role of community resilience in mitigating disaster-related impacts including mortality and morbidity. Considerations related to the intersection of the social determinants of health and mortality and morbidity assessment will be highlighted at various points throughout the report as a reminder of the critical importance of these issues (see especially Chapter 2). Additionally, a short supplemental paper drafted by staff, which includes two case studies on the contributory roles of the social determinants of health on community vulnerabilities to adverse health outcomes following disasters, has been included at the end of this report (see Appendix D).
Report Approach and Methodology
This report explores a broad range of issues relevant to the assessment of mortality and morbidity following large-scale disasters, with a specific focus on those disasters defined by the Stafford Act. To address the study’s Statement of Task (see Box 1-1), the National Academies appointed a 15-member committee with a broad range of academic and professional expertise, including public health policy, planning, and ethics; epidemiological and statistical research methods and analysis; and SLTT disaster response and fatality management. The committee deliberated from May 2019 to June 2020 and during this time the committee held five in-person meetings.
Committee’s Approach
Regarding the committee’s approach, this study was brought before the committee due the extreme discrepancies in mortality estimates following Hurricane Maria in Puerto Rico in 2017. While this tragedy emotionally underpinned the committee’s deliberations, the committee chose not to endorse a specific methodological approach or a particular singular way of assigning a “death toll” for all disasters. Instead, the committee interpreted the Statement of Task as asking, “What are the appropriate methods for tackling the problem of estimation and attribution?” and “How can these data be used to save lives and prevent suffering?” As such, the committee approached this study as an opportunity to provide stakeholders with an actionable roadmap that addresses persistent administrative, methodological, logistical, and organizational barriers to the effective assessment of disaster-related mortality and morbidity. Early in the deliberative process,
it became evident that overcoming these barriers and achieving lasting change across multiple systems is reliant on the coordinated commitment of multiple entities. The committee’s call for an enterprise approach to overcome persistent fragmentation in stakeholder responsibilities and systems ultimately forms the foundation for the report’s final chapter, which lays out the recommendations as components of a broader plan. These recommendations seek to (1) provide a strong framework for conceptualizing mortality and morbidity assessment; (2) guide the appropriate selection and use of various estimation approaches; (3) strengthen data collection and reporting systems to enhance the quality and comparability of data; and (4) provide SLTT stakeholders with the actionable data, tools, resources, and training needed to use mortality and morbidity data to save lives.
Additionally, to further enhance the applicability of the report for all hazards, the committee sought to emphasize the similarity of challenges across disasters of all types and scales in the collection, recording, and use of mortality and morbidity data. Therefore, while the report’s recommendations are focused directly on major disasters as defined in the Stafford Act and are referred to in this report as “large-scale disasters,” the report’s conclusions and recommendations can be read and adopted more broadly. Chapter 5 includes further discussion on the broader applicability of the committee’s recommendations.
Report Methodology
The work of the committee was informed by several different mechanisms and activities—six public sessions, two webinars, two site visits, two public comment sessions, electronic public comments, and a literature review. The committee hosted multiple types of open-to-the-public, information-gathering sessions. In August 2019, the committee convened a 2-day, in-person public workshop that brought together stakeholders to discuss their experiences and perspectives on assessing disaster-related mortality and morbidity as well as related policy and practice considerations. This workshop included a public comment session. The third committee meeting held in October 2019 included four additional open sessions and were hosted during site visits in Butte County and Sacramento, California. During these October 2019 sessions, the committee engaged with city officials in the city of Paradise, representatives of the county public health office in Butte County, and the medical examiner of Sacramento County (see Appendix B for the public workshop and meeting agendas). In addition to these in-person events, the committee hosted two public webinars in February 2020, which featured researchers who use a variety of statistical approaches to develop population estimates in their respective fields. Public comments were formally solicited during the first and second in-person meetings of the
committee in May and June 2019, respectively, and written comments from the public were accepted electronically for the entirety of the deliberative process. These public information-gathering sessions and the deliberations of the committee were supplemented by peer-reviewed and grey literature.
At the onset of deliberations, the committee worked in collaboration with the National Academies Research Center to develop and carry out a comprehensive review of the literature to support its work and provide additional evidence to inform the report’s conclusions and recommendations. This primary review concentrated on journals in a series of databases, including Embase, Medline, PAIS, ProQuest, PubMed, PsycInfo, Scopus, SocINDEX, and Worldcat, among others, and concentrated on articles published between 1980 and 2019. The committee chose to focus its efforts on research related to disasters in the United States but did not automatically eliminate literature involving international disasters (e.g., 2004 Indian Ocean tsunami). A more detailed accounting of the search parameters for the primary literature review can be found in Appendix A. The intent of the committee’s review of the literature on population estimation methods (see Chapter 4) was not to review every possible method and select a universal standard, but to explore the most relevant—and rigorous—methods that have been used, identify the benefits, shortcomings, and requirements for these methods, and, ultimately, develop a research agenda. The articles identified were reviewed for relevance to the Statement of Task and were made available to the committee, staff, and science writer. In addition to the primary comprehensive literature review, the committee drew from two supplemental papers drafted by members of the committee and staff (see Appendixes C and D) to provide additional supporting material for the report.
Guiding Precepts for an Effective Data System for Assessing Mortality and Morbidity
After reviewing the current landscape of practices for assessing mortality and morbidity following large-scale disasters, the committee established a set of guiding precepts to aid in developing its recommendations. The precepts describe the key qualities and philosophies of a responsive system for the collection and use of mortality and morbidity data that enables proactive decision making by stakeholders. These precepts, which follow, and their implications are incorporated throughout the report.
Collect and use data for community health protection as an essential component across all phases of disaster management
The fundamental responsibilities of emergency management and public health—at every level and capacity—are to protect human health, support
recovery, and prevent similar consequences from occurring in the future. High-quality mortality and morbidity data can improve preparedness, mitigation, response, and recovery capabilities if they are widely accessible, appropriately analyzed, and used effectively. Efforts to improve the timeliness and accuracy of mortality and morbidity data should be underpinned by the broader ethos of saving lives, protecting health, and preparing for future disasters.
Incorporate both individual counts and population estimates to better understand a disaster’s true effect
The two primary approaches for assessing disaster-related mortality and morbidity, individual counts and population estimates, have important and complementary values. The committee seeks to balance the two approaches in contributing to a comprehensive picture of a disaster’s true effect. These estimation approaches have different uses, advantages, and drawbacks, but both are critical for accurately and comprehensively assessing and describing a disaster’s impact on human health and for developing and improving approaches to limit the future consequences of disasters.
Leverage morbidity data and mortality data to support response, recovery, mitigation, and preparedness
Focusing exclusively on disaster-related mortality—the traditional outcome of interest—is shortsighted. Using morbidity data—both during the crisis and in the inter-disaster period—to evaluate and guide disaster management efforts provides greater opportunities for reducing future mortality outcomes and increasing the resilience of the community.
Build on and use existing systems, capacities, and methodologies
Efforts to drive systems-level improvements benefit from using existing capabilities and capacities as well as identifying shared goals and existing resources to support stakeholders across fields and disciplines. Failure to strengthen the broader system for collecting, recording, and reporting mortality and morbidity data weakens the ability of the nation to respond effectively to changing health threats. Changes that occur only in siloes or at certain levels will be insufficient to optimize the use of mortality and morbidity data.
Commit to the continuous improvement of systems over time
Access to valuable individual counts and population estimates of morbidity and mortality is foundational to understanding a disaster’s impact. The specific data needs, appropriate tools, effective practices, and key stakeholders evolve over time, and thus systems need to respond by evolving in parallel. Adopting a systems-level learning approach can provide a
foundation for continuously improving the integrity and interpretation of mortality and morbidity data, thus enabling greater protection of human life.
Adopt an enterprise approach to activate stakeholders and systems in times of crisis and during the inter-disaster period
Effectively collecting and using mortality and morbidity data requires collaboration across the disparate institutions and organizations that are directly and indirectly involved in disaster response, recovery, mitigation, and preparedness. An enterprise approach across the disaster management enterprise would unite stakeholders under common goals and mitigate the complexity of operationalizing improved practices and methods.
Support the resilience and strength of historically disadvantaged populations by using data to understand, mitigate, and eliminate inequalities in disaster impacts
Mortality and morbidity data can offer valuable contextual information about population-specific vulnerabilities and provide evidence for targeted mitigation and preparedness efforts to protect and improve the resilience of these populations.
VALUE AND MEANINGFUL USE OF MORTALITY AND MORBIDITY DATA IN DISASTER MANAGEMENT
The overarching aims of quantifying mortality and morbidity following a disaster are to facilitate actions that save lives, to protect health, and to prepare for the future (CDC, 2016). To achieve these aims, accurate data must be effectively communicated to a broad range of stakeholders that spans emergency management, government agencies, health systems, the general public, policy makers and political leadership, and other public- and private-sector stakeholders (see Chapter 2). The value of these data shifts across stakeholders, across the disaster management cycle, and over time (see Figure 1-1). Value is also determined by the type and quality of the data collected, how and when data are captured, and how these data are analyzed. Although mortality and morbidity data hold value for a variety of reasons, the primary focus of this report is how these data can be used to improve future health outcomes in large-scale disasters.
Two strands of work emerge following a disaster: one is driven by the need for immediate information on mortality, morbidity, and other relevant contextual data to facilitate response and recovery efforts, while the other seeks to better understand what happened during the response and recovery and how mitigation and prevention efforts can be informed and improved with better data. Quantifying the public health impacts of
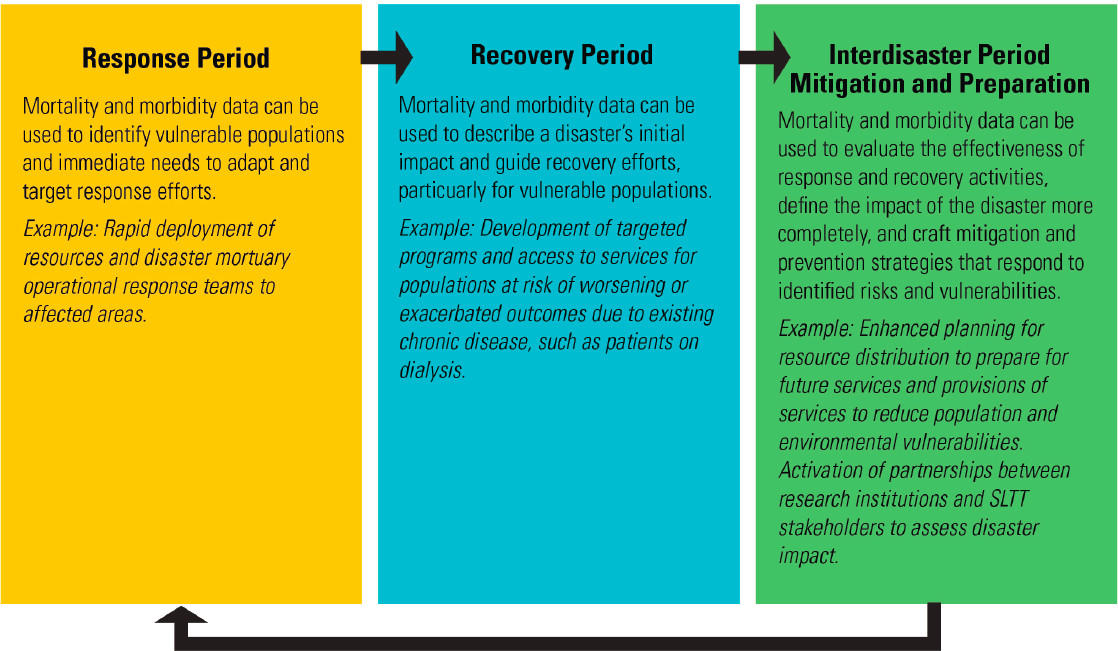
disasters is important not only for informing immediate response efforts, but also for offering insights into the effectiveness of policies and interventions to strengthen future response and recovery efforts (Khan et al., 2014). Understanding the potential impact of a threat is essential for preparation, planning, mitigation, and response.
Modeling based on morbidity and mortality data can also help elucidate a particular future or past threat and provide an estimate of the likely impact the threat will have or had on a given population. When compared to baseline data, these analyses can help determine whether there is sufficient local-level capacity to manage that threat and whether federal resources may be required. These different approaches—individual counts and population estimates—used for estimating disaster-related mortality and morbidity as well as the practical uses for these data and relevant barriers will be discussed in greater detail in Chapters 3 and 4.
CURRENT ISSUES IN MORTALITY AND MORBIDITY ASSESSMENT
Despite the importance of mortality and morbidity data in protecting human life, the nation lacks the capacity to assess disaster-related mortality and morbidity in a standardized way across states, tribal nations, territories, and localities. Additional challenges that hinder the collection, reporting, and recording of accurate mortality and morbidity data include (1) an inconsistent adoption of uniform definitions for disaster-related mortality, (2) a lack of standards for defining and quantifying disaster-related morbidity, and (3) a lack of capacity and support for the medicolegal system to accurately collect and record the data. Furthermore, the valuable data that are already being collected about disaster-related mortality and morbidity are not being used effectively; the organizations that collect and use these data function in professional silos with insufficient capacity and inadequate tools to effectively analyze and use the data. These challenges and others identified by the committee will be discussed in subsequent chapters.
What Counts as a Disaster-Related Death or Morbidity?
A major barrier to accurately assessing the mortality and morbidity associated with a disaster is the lack of consensus concerning the key concepts and definitions across the extensive network of systems and stakeholders involved in collecting, reporting, and using mortality and morbidity data. Most fundamentally, there is no agreement about what counts as a disaster-related death or morbidity, there are no standard practices or uniformly adopted case definitions for attributing different degrees of disaster-relatedness to a death, and there are no established standards or data systems
for attributing and collecting data on disaster-related morbidities. This enterprise-wide lack of uniformity and consistency in standards and practices for assessing mortality and morbidity undermines the accuracy of the data that are collected and squanders valuable data that are not collected at all. It also undercuts the ability to gain insights from comparing the impacts of a disaster—or of similar disasters—across settings and over time.
Disaster-Related Death
According to the Centers for Disease Control and Prevention (CDC), disaster-related mortality is routinely underestimated nationwide.2 A primary reason is that critical information indicating that a death is associated with a disaster is often omitted from a decedent’s official death record. In many cases, reports of the total deaths due to a disaster are based exclusively on counts of individual death records. If those death records lack detail about association to a recent disaster, the estimates will predictably underestimate the true toll. Chapter 3 describes current practices for collecting and recording data in the death record. Relying only on counts of individual death records has further disadvantages as well. For instance, this approach routinely excludes individuals who died of myocardial infarction, stroke, diabetic ketoacidosis, inability to obtain dialysis, disaster-related infections, and many other physical and mental health conditions that might not have arisen in the absence of the disaster. Such deaths are every bit as real and every bit as important as direct deaths counted by examining death certificates; however, these deaths are most effectively captured and described by using population-based estimation methods (see Chapter 4). Obvious mismatches between mortality as presented by individual counts versus population estimates can ignite controversy and confusion—as was most recently seen following Hurricane Maria in Puerto Rico in 2017 (see Box 1-3)—in addition to perpetuating inaccurate perceptions of a disaster’s true effect.
Disaster-Related Morbidities
Morbidity is an exceptionally complex and broad term that encompasses a vast range of short- and long-term health outcomes from the physical to psychological, including cardiovascular, gastrointestinal, and respiratory diseases; physical injuries; and mental health outcomes. Mortality is easier, comparatively, to define. Disaster-related morbidity is no
___________________
2 “Brief History of Centers for Disease Control and Prevention Disaster-Related Mortality Activities.” Paper provided to the committee at the August 29, 2019, workshop in Washington, DC. Available by request from the Public Access Records Office by emailing PARO@nas.edu.
less broad than all-cause morbidity and includes infectious diseases exacerbated by extreme socio-environmental conditions, such as population displacement, overcrowding, lack of access to clean water (Kouadio et al., 2012), chronic diseases brought on by stress or aggravated by disaster conditions (Miller and Arquilla, 2008), and chronic conditions that become acute (Mokdad et al., 2005). In addition to physical morbidities, intense exposure to stressors is associated with mental health sequelae such as suicide attempts and substance abuse (McFarlane and Williams, 2012). The relationship between disasters and morbidities of all types has increasingly become a research subject of interest, particularly as our understanding of the causal links among the social determinants of health, disasters, and morbidities has developed (see Appendix D).
Collecting data about disaster-related morbidities, specifically, presents its own set of challenges, given the broad scope of morbidities that can be tied, to some degree, to a disaster and the conditions it creates; the influence
of pre-existing and co-morbid conditions; variation in the landscape of morbidities across disaster types; and the logistical challenges associated with mining morbidity data from across a broad network of unique federal, SLTT, and health care systems. As with disaster-related mortalities, there is no established standard for what counts as a disaster-related morbidity or what data or indicators should be consistently tracked across common types of disasters (e.g., hurricanes, blizzards, tornadoes, pandemics/epidemics) to provide actionable information to end users such as public health and emergency planners, health care systems, and SLTT and federal agencies. As with all data, different data types provide different opportunities for use. The COVID-19 pandemic has demonstrated how the availability of multiple methods for assessing mortality and morbidity can create confusion and make these numbers susceptible to manipulation or the appearance thereof.
Defining which morbidity data are of value to the disaster management enterprise and developing standards for the data systems that generate these data are critical first steps to building the capability to collect and use these data effectively (see Chapters 3 and 4). A discussion of how the committee chose to define significant morbidity as it relates to a disaster can be found later in this chapter.
Federal Efforts and Guidance to Improve the Assessment of Mortality and Morbidity
Wide variation persists in what counts as a disaster-related death across counties, states, and the federal government (see Table 3-2 for federal and state criteria for attributing deaths to COVID-19). Some federal and professional guidance exists for medical certifiers certifying individual deaths attributable to a disaster, but this guidance has not been consistently adopted across jurisdictions to harmonize the variation in case definitions and inconsistencies in data collection and reporting practices. Along with the lack of a universal, methodologically sound framework for understanding disaster-related mortality and morbidity, these factors (and others) limit the ability to intervene to reduce the health impacts of future disasters (Combs et al., 1999). Furthermore, the variability in the ways that disaster-related mortality and morbidity are reported in different jurisdictions can even obfuscate the impact of an event that has already happened.
Over the past few decades, CDC and partners have worked to improve data collection and reporting practices at state and local levels by developing standard case definitions and tools to support stakeholders—primarily medicolegal death investigation professionals (see Chapter 3)—in the attribution of disaster-related mortality. In 1999, CDC published uniform disaster mortality case definitions for attributing direct and indirect deaths
to a disaster3 (Combs et al., 1999) (see Box 1-4). These have been used to categorize deaths after the fact in retrospective studies of large-scale disasters (Brunkard et al., 2008; CDC, 2004, 2006; Ragan et al., 2008). To bolster national awareness about the importance of attributing deaths to a disaster, CDC has also developed guidance to support professionals working in the medicolegal system in completing death certificates with accurate information. This guidance includes A Reference Guide for Certification of Deaths in the Event of a Natural, Human-Induced, or Chemical/Radiological Disaster (NCHS, 2017) and instructions for completing the cause of death section on a death certificate. The guide is based on CDC’s uniform disaster mortality case definitions and offers a flow chart for making determinations about attribution; it also includes examples of common causes of direct disaster-related death and common circumstances leading to indirect disaster-related deaths. To address challenges in gathering death-scene data, CDC’s Death Scene Investigation After Natural Disaster or Other Weather-Related Events toolkit supports investigators by providing a common framework for collecting and documenting consistent disaster-related death-scene information (CDC, 2017). Additional tools piloted and supported by CDC are discussed in Chapter 3.
Despite these federal efforts, the adoption of these uniform case definitions, data recording practices, and reporting methods remains inconsistent among SLTT-level stakeholders, who are primarily responsible for collecting and recording disaster-related mortality and morbidity data. A multitude of different terms, interpretations of policy, and professional practices for recording attribution across SLTT medicolegal systems are used to categorize and describe the degree of association between an individual- or population-level health outcome and exposure to a disaster. Fatality management templates and protocols to support uniform standards and practices for medical examiners, coroners, and other medical certifiers have been developed by various states and by professional associations (e.g., the National Association of Medical Examiners), but adherence to these standards is voluntary. Furthermore, many of the templates and protocols do not provide specific guidance about which data points for disaster-related mortality are important to collect or about how they should be recorded within information systems to benefit emergency management and public health. These inconsistencies in data recording make it difficult to compare data across localities and states and also limit the effective use of these data (see Chapter 3).
___________________
3 “Brief History of Centers for Disease Control and Prevention Disaster-Related Mortality Activities.” Paper provided to the committee at the August 29, 2019, workshop in Washington, DC. Available by request from the Public Access Records Office by emailing PARO@nas.edu.
Public Health Emergency Preparedness and Response Cooperative Agreement Requirements for Mortality and Morbidity Data
CDC’s Public Health Emergency Preparedness (PHEP) cooperative agreement outlines the responsibility of SLTT public health agencies to aggregate and analyze mortality and morbidity data after any disaster as an essential public health capability. All 50 states, 4 major metropolitan areas, and 8 territories are recipients of the PHEP cooperative agreement. The CDC tools mentioned above have now been included in the updated CDC Public Health Emergency Preparedness and Response Capabilities of the PHEP cooperative agreement (CDC, 2018, 2020). Despite commitment from certain federal and SLTT agencies and the requirements of the PHEP agreement, CDC guidance and standards have not yet been widely adopted in practice nationwide (Noe, 2019).
Stakeholders
The responsibilities for collecting, recording, and reporting mortality and morbidity data are distributed across many different stakeholders and entities—some of which have competing interests and conflicting policies—at the local, state, regional, and federal levels. Different agencies and organizations are accountable for different components of this complex process and have responsibility for different pieces of data following large-scale disasters (see Box 1-5 for a list of the stakeholders involved). Three critical federal players are CDC, FEMA, and the Office of the Assistant Secretary for Preparedness and Response in the Department of Health and Human Services. Other important stakeholders are hospital and health
systems, health care providers, nursing homes, social support cultural centers, care systems for end-stage renal disease, epidemiologists, morgues and medical examiners, state and local governments, and communities. The major users of mortality and morbidity data are widely dispersed across the general public, political leadership, the private sector, and the public sector. However, these stakeholders’ responsibilities are commonly siloed, and the integration of disaster epidemiology into disaster management and policy making remains limited (Malilay et al., 2014). For example, despite the critical importance of the medicolegal system in collecting essential data for disaster management, this group of stakeholders is rarely engaged in emergency management and public health planning for disasters.
TERMINOLOGY CHOICES AND KEY CONCEPTS
From the outset, it is important to clarify the terminology choices made by the committee and explain how these distinctions support improved assessment of mortality and morbidity following large-scale disasters. The concepts will be discussed in greater detail in future chapters.
Terminology for Estimating Impact
Multiple terms have been used to denote the presence and degree of a relationship between a death or injury and a disaster (e.g., key affected populations, excess deaths from violent causes, disaster-attributed mortality, incident morbidity). These terms are often conflated, resulting in misunderstandings about estimated impacts and poor comparability of mortality and morbidity assessments over time and across disasters. Additional challenges relate to characterizing what is being assessed and the context in which it is being assessed. These issues lead to further confusion over how to measure total mortality and morbidity and how these data can be best used by policy makers and other stakeholders.
Throughout the report, the committee has adopted a set of uniform terms to describe quantitative indicators of disaster impact and the methods and data used to develop them. Chapter 2 provides more detail on these terms and the committee’s rationale, but a brief summary is provided here to facilitate the reader’s entry into the report. First, the terms individual count (i.e., estimates derived from individual death records) and population estimate (i.e., estimates derived from population-based estimation methods) are used throughout the report to refer to the two main approaches for estimating a disaster’s impact on mortality and morbidity. These two approaches can be used to describe essential information about mortality and morbidity and encompass distinct methodologies and tools. Additional terms used in the report include
- Direct mortality and morbidity: those killed or injured directly by the disaster;
- Indirect mortality and morbidity: those killed or injured indirectly as a result of the disaster; and
- Partially attributable mortality and morbidity: those killed or injured in part or possibly as a result of the disaster.
These terms were selected for use in the report based on several foundational concepts explored further in Chapter 2. First and most significantly, disasters are complex events with multifactorial health consequences, and there can be more than one appropriate approach to answering the question “How many deaths and severe morbidities were caused by this disaster?”
No single, standardized methodological approach to assessing disaster-related mortality and morbidity can be applied universally to generate a singular estimate that sufficiently describes a disaster’s impact. However, while there is no standard method for generating mortality or morbidity estimates, best practices among the available methodologies can now be specified for both individual counts and population estimates, as can the appropriate circumstances for their uses. Gaining a comprehensive understanding of a disaster’s impact on human health requires more than one method of assessment.
The second foundational concept is that quantitative assessments of disaster impact represent an estimation of impact at a distinct point of time, within a specific context, and based on particular assumptions. Estimates of total mortality and morbidity—both individual counts and population estimates—are not static and can change over time as additional data are gathered or updated, as additional mortality or morbidity occurs, or as the assumptions for characterizing the estimate evolve.
The third concept is that each approach is valuable and imprecise in different ways and has different appropriate uses. Individual counts rely on administrative data, such as death records, to estimate the number of reported deaths in a certain geographical area at a defined point in time and are valuable for an initial understanding of the immediate impact of disasters or causes of death (e.g., carbon monoxide poisonings from improper generator use in the home). However, this method can be undermined by inaccuracies in the ways that data are recorded and reported; individual counts also fail to count certain individuals, such as those who die of natural causes during a disaster but would not have died but for the disaster (see Chapter 3). Population-based estimation methods are crucial for capturing a full understanding of the impacts of a disaster on health and mortality and for illustrating population-level trends and associations (e.g., an increase in myocardial infarctions following Hurricane Sandy in New Jersey) (Swerdel et al., 2014). These methods may incorporate less precise information on cause of death and in some applications (e.g., estimates of “excess” deaths) cannot distinguish which individuals would have survived in the absence of the disaster from those who would have died during the period regardless (see Chapter 4). The complex nature of disasters and the multiple pathways through which they affect human health make it difficult to quantify the impact of a specific disaster on human health with precision. Together, however, the two approaches can provide both timely information and a far more comprehensive picture of the health and mortality impacts of a disaster.
Finally, and especially in pandemics, is the matter of temporality. Disasters such as hurricanes or wildfires occur over a period of days or weeks (although recovery can take months or years). Attributed mortality and
morbidity counts and estimates change over time for two reasons: some long-term consequences take time to occur, and all data systems have lags that vary over time. In pandemics both of these factors apply, but there is an additional dynamic: the continued infection of new cases, which reflects efforts to control the pandemic through social distancing and other methods. For instance, for the reasons discussed above, COVID-19 deaths are sometimes seen as more reliable than case counts. But deaths lag hospitalizations, the onset of symptoms, and the time of infection by 3 to 4 weeks. The daily number of deaths, therefore, is a seriously lagging indicator of the efficacy of control efforts, and thus a poor guide for deciding whether, say, social distancing measures can be relaxed.
Defining Significant Morbidity
The qualification of significant morbidity, rather than all degrees and types of disaster-related morbidity, was specifically noted in the committee’s Statement of Task, but the term was not explicitly defined by the study sponsor. Further discussions with FEMA during the committee’s first meeting provided some clarity concerning this term and, per FEMA’s guidance, limited the committee’s deliberations to very serious morbidities, both physical and mental. Because no standard practices or systems to collect disaster-related morbidity data exist at a national level (see Chapter 4), no standard definition for describing what counts as significant disaster-related morbidity exists in the literature. However, this term has been used previously to describe a serious risk of immediate hospitalization or risk to life due to the restriction of critical bodily functions for specific diseases and conditions, such as end-stage liver disease (Brown et al., 2016) and chronic obstructive pulmonary disease (Cushen et al., 2017). The term significant is highly subjective, and significant morbidity could realistically encompass a wide range of physical and mental injuries that are deemed significant in different ways by different stakeholders. In the absence of a widely accepted scientific or operational definition for significant morbidity and based on the guidance of the sponsor, this report will approach significant morbidity from the context described above—injuries or illnesses that place an individual at high risk of hospitalization or imminent death, such as acute cardiovascular events or the worsening of a chronic condition such as kidney disease.
While this report will focus on practices for assessing significant morbidity as it is described above, readers should approach the report with the understanding that the recommendations are applicable to the assessment of morbidity at all levels. Throughout the report text, the committee will use the term morbidity to refer to significant morbidity per the above context unless otherwise stated. A discussion of the many uses for disaster-related
morbidity data can be found in Chapter 2; a discussion of challenges and opportunities for improving the assessment of disaster-related morbidity can be found in Chapters 3 and 4.
Finally, the inherent complexity of morbidity, the variation of morbidities across disasters, and the current lack of standards and infrastructure for systematically assessing morbidity following disasters indicates that what counts as significant morbidity is likely less important than the question of what should be counted. It is beyond the committee’s capacity to develop an evidence-based set of standards and indicators to frame the future collection of morbidity data, as considerable investment in research will need to occur to develop the body of research to support such a job. However, the committee stresses that the identification of key morbidities across common disaster types could add value to early efforts to capture disaster-related morbidity data in a systematic manner by SLTT and federal stakeholders. See Chapter 3 for a discussion of potential key morbidities that could be targeted by data collection efforts and how these individual counts could be used by SLTT entities and Chapter 4 for information about survey methods for collecting these data and analytical approaches for developing population estimates of morbidity.
ORGANIZATION OF THIS REPORT
This report seeks to provide federal and SLTT stakeholders with actionable guidance for improving the assessment of mortality and significant morbidity of disasters. Although the committee’s charge focused primarily on major disasters as defined by the Stafford Act, the report’s recommendations are largely applicable to other disasters and emergencies. Each chapter includes highlighted conclusions that provide evidence for the report’s recommendations, which are laid out in the final chapter of the report. In Chapter 2 the committee explores the importance of and various uses for mortality and morbidity data. The chapter also lays out the committee’s framework approaches for conceptualizing disaster-related mortality and morbidity estimates and describes a recommended set of standard definitions. Chapter 3 provides an overview of the diversity in the nation’s death investigation systems and explores the current landscape of individual-level mortality and morbidity data collection, recording, and use across this network. In that chapter the committee also identifies barriers to the collection, reporting, and use of individual counts and provides a set of best practices for the implementation of individual counting methods for assessing mortality and morbidity from disasters. Chapter 4 reviews analytical methods used to develop population estimates of mortality and morbidity from disasters and provides recommendations on operational practices. Chapter 5 provides a summary of the report’s major conclusions
and recommendations and sets forth a suggested plan of action for use by relevant stakeholders. Several appendixes with supplemental material selected by the committee can be found at the end of the report. Appendix A includes the committee’s preliminary literature review search strategy and Appendix B contains a record of all of the public sessions hosted by the committee over the course of its deliberations. Appendix C includes a companion piece developed independently by two members of the committee about the assessment of mortality and morbidity from the COVID-19 pandemic. Appendix D contains two supplemental case studies on how the social determinants of health can affect the assessment of mortality and morbidity. Appendix E contains the committee and staff biographies.
REFERENCES
Bacon, J. 2017. Why Puerto Rico faces a monumental recovery effort. USA Today. https://www.usatoday.com/story/news/nation/2017/09/26/why-puerto-rico-faces-monumentalrecovery-effort/703515001 (accessed June 22, 2020).
Brown, C. L., B. G. Hammill, L. G. Qualls, L. H. Curtis, and A. J. Muir. 2016. Significant morbidity and mortality among hospitalized end-stage liver disease patients in Medicare. Journal of Pain and Symptom Management 52(3):412–419.
Brunkard, J., G. Namulanda, and R. Ratard. 2008. Hurricane Katrina deaths, Louisiana, 2005. Disaster Medicine and Public Health Preparedness 2(4):215–223.
CDC (Centers for Disease Control and Prevention). 2004. Preliminary medical examiner reports of mortality associated with Hurricane Charley—Florida, 2004. Morbidity and Mortality Weekly Report 53(36):835–837.
CDC. 2005. Vibrio illnesses after Hurricane Katrina—multiple states, August–September 2005. Morbidity and Mortality Weekly Report 54(37):928–931.
CDC. 2006. Mortality associated with Hurricane Katrina—Florida and Alabama, August–October 2005. Morbidity and Mortality Weekly Report 55(9):239–242.
CDC. 2016. A primer for understanding the principles and practices of disaster surveillance in the United States. Atlanta, GA: Centers for Disease Control and Prevention.
CDC. 2017. Death scene investigation after natural disaster or other weather-related events. Atlanta, GA: Centers for Disease Control and Prevention. https://www.cdc.gov/nceh/hsb/disaster/docs/DisasterDeathSceneToolkit-P.pdf (accessed June 26, 2020).
CDC. 2018. Public health emergency preparedness and response capabilities. https://www.cdc.gov/cpr/readiness/capabilities-change.htm (accessed June 26, 2020).
CDC. 2020. Public Health Emergency Preparedness (PHEP) cooperative agreement. https://www.cdc.gov/cpr/readiness/phep.htm#:~:text=Eight%20U.S.%20territories%20and%20freely,%2C%20and%20Republic%20of%20Palau (accessed June 4, 2020).
Combs, D. L., L. E. Quenemoen, R. G. Parrish, and J. H. Davis. 1999. Assessing disaster-attributed mortality: Development and application of a definition and classification matrix. International Journal of Epidemiology 28(6):1124–1129.
CRS (Congressional Research Service). 2017. Stafford Act declarations 1953–2016: Trends, analyses, and implications for Congress. CRS report no. R42702. https://crsreports.congress.gov/product/pdf/R/R42702 (accessed June 25, 2020).
Cushen, B., R. Morgan, and R. Summer. 2017. Chronic obstructive pulmonary disease. In S. R. Quah (ed.), International encyclopedia of public health, 2nd ed. Cambridge, MA: Academic Press. Pp. 28–35.
Furey, J. S., H. Fredrickson, C. Foote, and M. Richmond. 2007. Post-Katrina fecal contamination in Violet Marsh near New Orleans. International Journal of Environmental Research and Public Health 4(2):84–92.
Khan, Y., B. Schwartz, and I. Johnson. 2014. Surveillance and epidemiology in natural disasters: A novel framework and assessment of reliability. PLOS Currents doi: 10.1371/currents.dis.6773eb9d5e64b733ab490f78de346003.
Kishore, N., D. Marqués, A. Mahmud, M. V. Kiang, I. Rodriguez, A. Fuller, P. Ebner, C. Sorensen, F. Racy, J. Lemery, L. Maas, J. Leaning, R. A. Irizarry, S. Balsari, and C. O. Buckee. 2018. Mortality in Puerto Rico after Hurricane Maria. New England Journal of Medicine 379(2):162–170.
Kouadio, I. K., S. Aljunid, T. Kamigaki, K. Hammad, and H. Oshitani. 2012. Infectious diseases following natural disasters: Prevention and control measures. Expert Review of Anti-Infective Therapy 10(1):95–104.
Liu, E. C. 2008. Would an influenza pandemic qualify as a major disaster under the Stafford Act? Congressional Research Service report to Congress. https://digital.library.unt.edu/ark:/67531/metadc627007/m1/1/high_res_d/RL34724_2008Oct20.pdf (accessed June 25, 2020).
Malilay, J., M. Heumann, D. Perrotta, A. F. Wolkin, A. H. Schnall, M. N. Podgornik, M. A. Cruz, J. A. Horney, D. Zane, R. Roisman, J. R. Greenspan, D. Thoroughman, H. A. Anderson, E. V. Wells, and E. F. Simms. 2014. The role of applied epidemiology methods in the disaster management cycle. American Journal of Public Health 104(11):2092–2102.
Marinova-Petkova, A., I. Guendel, J. P. Strysko, L. L. Ekpo, R. Galloway, J. Yoder, A. Kahler, A. Artus, A. R. Hoffmaster, W. A. Bower, H. Walke, B. R. Ellis, T. Hunte-Ceasar, E. M. Ellis, and I. J. Schafer. 2019. First reported human cases of leptospirosis in the United States Virgin Islands in the aftermath of Hurricanes Irma and Maria, September–November 2017. Open Forum Infectious Diseases 6(7):ofz261.
McFarlane, A. C., and R. Williams. 2012. Mental health services required after disasters: Learning from the lasting effects of disasters. Depression Research and Treatment 970194.
Milken Institute School of Public Health. 2018. Ascertainment of the estimated excess mortality from Hurricane María in Puerto Rico. Washington, DC: The George Washington University. https://publichealth.gwu.edu/sites/default/files/downloads/projects/PRstudy/Acertainment%20of%20the%20Estimated%20Excess%20Mortality%20from%20Hurricane%20Maria%20in%20Puerto%20Rico.pdf (accessed June 26, 2020).
Miller, A. C., and B. Arquilla. 2008. Chronic diseases and natural hazards: Impact of disasters on diabetic, renal, and cardiac patients. Prehospital and Disaster Medicine 23(2):185–194.
Mokdad, A. H., G. A. Mensah, S. F. Posner, E. Reed, E. J. Simoes, M. M. Engelgau, and Chronic Diseases and Vulnerable Populations in Natural Disasters Working Group. 2005. When chronic conditions become acute: Prevention and control of chronic diseases and adverse health outcomes during natural disasters. Preventing Chronic Disease 2(Spec No):A04.
NCHS (National Center for Health Statistics). 2017. A reference guide for certification of deaths in the event of a natural, human-induced, or chemical/radiological disaster. Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/data/nvss/vsrg/vsrg01.pdf (accessed June 26, 2020).
Nigro, O. D., A. Hou, G. Vithanage, R. S. Fujioka, and G. F. Steward. 2011. Temporal and spatial variability in culturable pathogenic Vibrio spp. in Lake Pontchartrain, Louisiana, following Hurricanes Katrina and Rita. Applied and Environmental Biology 77(15):5384–5393.
Noe, R. 2019. Session 3: Current capabilities in assessing and using morbidity and mortality data in real-time during a large-scale disaster. Presentation at the August 29, 2019, public meeting of the National Academies of Sciences, Engineering, and Medicine’s Committee on Best Practices for Assessing Mortality and Significant Morbidity Following Large-Scale Disasters, Washington, DC.
Ragan, P., J. Schulte, S. J. Nelson, and K. T. Jones. 2008. Mortality surveillance: 2004 to 2005 Florida hurricane-related deaths. The American Journal of Forensic Medicine and Pathology 29(2):148–153.
Swerdel, J. N., T. M. Janevic, N. M. Cosgrove, J. B. Kostis, and the Myocardial Infarction Data Acquisition System Study Group. 2014. The effect of Hurricane Sandy on cardiovascular events in New Jersey. Journal of the American Heart Association 3(6):e001354.
Yee, E. L., H. Palacio, R. L. Atmar, U. Shah, C. Kilborn, M. Faul, T. E. Gavagan, R. D. Feigin, J. Versalovic, F. H. Neill, A. L. Panlilio, M. Miller, J. Spahr, and R. I. Glass. 2007. Widespread outbreak of norovirus gastroenteritis among evacuees of Hurricane Katrina residing in a large “megashelter” in Houston, Texas: Lessons learned for prevention. Clinical Infectious Diseases 44(8):1032–1039.


























