Proceedings of a Workshop
INTRODUCTION1
Behavioral health conditions (which include mental health and substance use disorders [MHSUDs]) affect approximately 20 percent of Americans (NIMH, 2017). Of those with a substance use disorder (SUD), approximately 60 percent also have a mental health disorder (CBHSQ, 2015). Together, these disorders account for a substantial burden of disability, have been associated with an increased risk of morbidity and mortality from other chronic illnesses, and can be risk factors for incarceration, homelessness, and death by suicide. In addition, they can compromise a person’s ability to seek out and afford health care and adhere to care recommendations (Roberts et al., 2015; WHO, 2015).
Despite the high rates of comorbidity of physical and behavioral health conditions, integrating services for these conditions into the American health care system has proved challenging. As many as 80 percent of patients with behavioral health conditions seek treatment in emergency rooms and primary care clinics, and between 60 and 70 percent of them are discharged without receiving behavioral health care services (Klein and Hostetter, 2014). More than two-thirds of primary care providers report that they are unable to con-
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop was prepared by the rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
nect patients with behavioral health providers because of a shortage of mental health providers and health insurance barriers (Alliance for Health Policy, 2017; Cunningham, 2009). Part of the explanation for the lack of access to care lies in a historical legacy of discrimination and stigma that makes people reluctant to seek help and also led to segregated and inhumane services for those facing MHSUDs (Storholm et al., 2017). Moreover, health insurance programs often provide limited coverage of services for these disorders compared to services for other conditions, so there has been little or no financial incentive to bring behavioral health care into the primary care setting. However, even when services are covered, inadequate reimbursement or network adequacy may still limit access (Klein and Hostetter, 2014). While the majority of mental health services are currently delivered in primary care settings, the implementation of integrated care models shown to support delivery of evidence-based mental health services in primary care has been limited to demonstration programs with funding from time-limited grants (McGinty and Daumit, 2020).
In an effort to understanding the challenges and opportunities of providing essential components of care for people with MHSUDs in primary care settings, the National Academies of Sciences, Engineering, and Medicine’s Forum on Mental Health and Substance Use Disorders planned a 1-day, in-person workshop in Washington, DC. Given restrictions placed on travel and large public gatherings as a result of the coronavirus disease 2019 (COVID-19) pandemic, the workshop (originally scheduled for June 3) was converted into a virtual workshop with three webinars held on June 3, July 29, and August 26, 2020, that addressed the following:
- Efforts to define essential components of care for people with MHSUDs in the primary care setting for three illustrative conditions (depression, alcohol use disorder, and opioid use disorder [OUD]);
- Opportunities to build the health care workforce and delivery models that incorporate those essential components of care; and
- Financial incentives and payment structures to support the implementation of those care models, including value-based payment strategies and practice-level incentives.
A paper commissioned by the Think Bigger Do Good Policy Series2 provided an overarching framework for the workshop (McGinty and Daumit, 2020). This paper was authored by the first webinar’s two speakers, Beth McGinty, associate professor, associate chair for research and practice, co-director of the Center for Mental Health and Addiction Policy Research,
___________________
2 The Think Bigger Do Good Policy Series is a partnership of the Scattergood Foundation, Peg’s Foundation, Patrick P. Lee Foundation, and Peter & Elizabeth Tower Foundation.
and associate director of the ALACRITY Center for Health and Longevity in Mental Illness at the Johns Hopkins Bloomberg School of Public Health, and Gail Daumit, Samsung Professor of Medicine, vice chair for clinical and translational research, and director of the ALACRITY Center.
Howard Goldman, professor of psychiatry at the University of Maryland at Baltimore School of Medicine and forum co-chair, opened the first virtual workshop, explaining that the paper was the product of a collaboration among the Think Bigger Do Good Policy Series, the National Academies, and the journal Psychiatric Services. “We have illustrated the kind of collaboration we can do within the behavioral health field, and it is now incumbent on us to do a better job in integrating behavioral health and general medical care,” said Goldman. Adding that this is not a new topic, Goldman shared that he wrote a background paper on the subject for the Institute of Medicine (IOM)3 about 40 years ago. At the time, the focus was on diagnosis and referral from general medicine to specialty care because, as he explained, “no one at that time thought that general medicine would really pay much attention to implementing evidence-based practices.”
Colleen Barry, the Fred and Julie Soper Professor and chair of the Department of Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health, co-director of the Johns Hopkins Center for Mental Health and Addiction Policy, and forum co-chair, noted in her introductory remarks that this workshop was taking place while the nation was confronting two public health crises—the COVID-19 pandemic and the aftermath of the brutal murder of George Floyd—both with profound implications for mental health and well-being. “It is clear that persistent racism and income and health inequities are themselves public health crises with profound implications for mental health,” said Barry. “As we dive into a discussion of how to improve care for mental illness and addiction, we can all be motivated by the fact that the crises surrounding us today make the topics we are discussing all the more pressing and important.” Barry also remarked that researchers were documenting worsening mental health and substance use in the context of the pandemic, underscoring the importance of this workshop.
Overview of the Proceedings
As noted above, the virtual workshop unfolded over three webinars. The first webinar in the series explored the landscape of models of care, such
___________________
3 As of March 2016, the Health and Medicine division of the National Academies of Sciences, Engineering, and Medicine continues the consensus studies and convening activities previously carried out by the Institute of Medicine (IOM). The IOM is used to refer to publications issued prior to July 2015.
as accountable care organizations (ACOs), patient-centered medical homes (PCMHs), and collaborative care arrangements, and how essential components of care for MHSUDs might be induced for those care models. The webinar also addressed policy issues related to implementing these models and the essential components of care.
The second webinar highlighted the essential components of care for three key conditions—depression, alcohol use disorder, and OUD—in primary care settings. The speakers also described key factors that support or impede implementation of these essential components.
The third webinar examined ways to improve the workforce to support providing the essential components of care. It also focused on addressing financing, payment, practice, and systems-level issues, policies, and incentives to support providing these components.
This Proceedings of a Workshop summarizes the presentations and discussions of the 3 days of virtual sessions. A broad range of views was offered. Box 1 provides a summary of suggestions for potential actions from individual workshop participants. Appendixes A and B contain the workshop Statement of Task and the workshop agenda, respectively. The workshop speakers’ presentations (as PDF and audio files) have been archived online.4
MODELS OF CARE FOR PEOPLE WITH MHSUDs
Daumit began her remarks by framing the problem confronting the care of people with MHSUDs. She noted that MHSUDs, also known as “behavioral health conditions,” are significantly undertreated in the United States. In fact, she said, although nearly 20 percent of U.S. adults experience a behavioral health issue every year, in 2018 only 43.3 percent of adults with mental illness received any mental health treatment, and only 11 percent with an SUD received addiction treatment (NAMI, 2019). Moreover, mental illness and SUDs are highly comorbid with one another—one in five U.S. adults with mental illness also experience an SUD (NIDA, 2010)—and with common physical health conditions, such as cardiovascular and metabolic diseases. HIV infection and chronic liver disease are common comorbidities with SUDs (SAMHSA, 2020).
Despite the high prevalence of comorbidity, physical illnesses are frequently undertreated in people with behavioral health conditions. This suboptimal care for people with behavioral health conditions has major health implications, Daumit explained. Depression is a leading cause of
___________________
4 For more information, see http://www.nationalacademies.org/hmd/Activities/MentalHealth/MentalHealthSubstanceUseDisorderForum/2019-OCT-15.aspx (accessed October 6, 2020).
disability, both in the United States and worldwide, and people with serious mental illnesses, such as schizophrenia, bipolar disorder, and major depressive disorder, die at least 10 years prematurely relative to the overall population, mostly as a result of cardiovascular disease and other medical conditions (Bodenheimer et al., 2002). Notwithstanding the high burden of behavioral health conditions and their comorbidities, the U.S. mental health and addiction treatment systems have historically operated outside of the general medical system. This fragmentation, said Daumit, is an important driver of undertreatment.
Developing implementation models for integrating general medical care and behavioral health care—what is known as “integrated care”5—has been a priority in the clinical and health policy communities for decades, explained Daumit. Although the majority of mental health services are delivered in primary care settings (Coyne et al., 1994; Katon and Schulberg, 1992; Regier et al., 1993; Schulberg et al., 1995), Daumit stressed that integrated care models shown to be effective in clinical trials have not been widely implemented outside of demonstration programs or other time-limited mechanisms. “We have unrealized opportunities to address mental illness and SUDs in primary care settings,” she said.
As Daumit pointed out, the majority of integrated care interventions shown in clinical trials to improve treatment delivery and patient outcomes implement variations of the collaborative care model,6 which is based on Wagner’s chronic care model (Wagner et al., 1996). That model (see Figure 1) defines essential elements of health systems, particularly team-based care, that encourage high-quality chronic disease care. It encompasses elements of community resources and policies from within the health system, self-management support, delivery system redesign, decision support, and clinical information systems. “These elements facilitate productive interactions between activated patients and a proactive clinical team to improve health outcomes,” explained Daumit.
Daumit explained that the collaborative care model was developed by researchers at Group Health and the University of Washington to focus on improving care in the primary care setting for individuals with depression. In collaborative care, primary care physicians work with a care manager and consulting psychiatrist to proactively identify, treat, and monitor people with behavioral health conditions.
___________________
5 According to the World Health Organization, integrated care is defined as “the organization and management of health services so that people get the care they need, when they need it, in ways that are user-friendly, achieve the desired results and provide value for money” (Waddington et al., 2008).
6 Collaborative care refers specifically to the blending of mental and physical health care in order to provide patient-centered, comprehensive, accountable care (Insel, 2015; Katon et al., 1995).
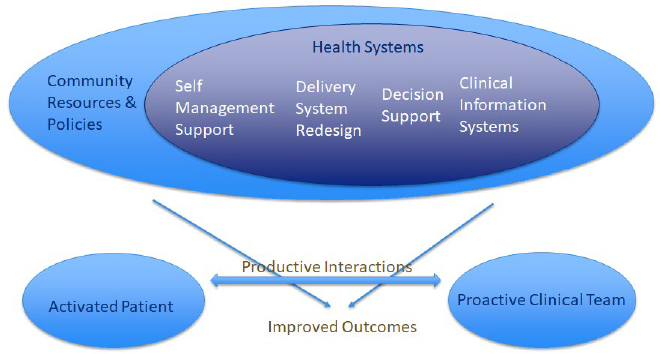
SOURCES: As presented by Gail Daumit, June 3, 2020; adapted from Wagner, E. H., B. T. Austin, and M. Von Korff. 1996. Organizing care for patients with chronic illness. The Milbank Quarterly 74(4):511–544. Reprinted with permission from the Milbank Memorial Fund.
Daumit pointed out that the core tenets of the collaborative care model include population-based care, measurement-based care, and stepped care (see Table 1). She noted that population-based care differs from care in which clinicians see one patient after another individually and focus only on the patient in front of them rather than the broader population of people with a certain condition.
TABLE 1 Core Tenets of the Collaborative Care Model
| Core Tenets of the Collaborative Care Model | Description |
|---|---|
| Population-based care |
|
| Measurement-based care |
|
| Stepped care |
|
SOURCES: As presented by Gail Daumit, June 3, 2020; adapted from McGinty and Daumit, 2020.
In measurement-based care, the Patient Health Questionnaire major depressive disorder module (PHQ-9), for example, could serve to both diagnose depression and identify those individuals who are not improving with treatment. In terms of stepped care, failure to intensify treatment is common for patients with depression who are treated in primary care, explained Daumit (Pence et al., 2012; Unützer and Park, 2012).
As Daumit explained, there is a large and conclusive body of evidence from randomized controlled trials supporting the beneficial effects of collaborative care, in terms of both access to care and patient outcomes, for patients with depression in the primary care setting (Bao et al., 2015; Ginsburg et al., 2018; Simon, 2006). Evidence also suggests that collaborative care could benefit individuals with anxiety (Archer et al., 2012; Curth et al., 2019), bipolar disorder (Reilly et al., 2013), schizophrenia (Baker et al., 2019; Neville, 2015), SUDs (Jeffries et al., 2013; Wiktorowicz et al., 2019), and comorbid health conditions (Camacho et al., 2018; Coventry et al., 2015).
Daumit explained that the main issue with implementing the collaborative care model is that it is complex and requires team members from multiple specialties. She noted several simpler models of integrative care, such as the Screening, Brief Intervention, and Referral to Treatment (SBIRT) model (Agerwala and McCance-Katz, 2012; SAMHSA, 2013) and the consultation-liaison model (Gillies et al., 2015; Meadows et al., 2007; Muskin, 2017).
Daumit pointed out that the SBIRT model has been used predominantly for treating alcohol use disorder and other SUDs. The model applies a validated screening process to identify patients and stratify them by level of risk. Daumit noted that low-risk patients might receive brief behavioral therapy for an SUD and a motivational enhancement intervention designed to help them change their behavior, while high-risk patients would receive a referral for specialty treatment. SBIRT has been tested primarily in primary care and emergency department (ED) settings, and the resulting small body of research has produced mixed results. Daumit noted that one high-quality trial found no effects on alcohol or substance use after a 6-month follow-up (Drake et al., 2009). However, she added, a recent systematic review did find that brief interventions delivered in primary care or ED settings can reduce alcohol consumption and improve alcohol consumption behaviors (Driessen and Zhang, 2017).
Daumit defined consultation-liaison models as those where processes exist for the primary care provider to consult with a behavioral health specialist. She explained that some studies suggest this approach can improve depression outcomes and reduce the length of general medical inpatient hospitalizations among those with mental illness. She cautioned, however, that “we need more data on these kinds of integrated care models to know how they really work.”
Key Elements of Integrated Care
McGinty shifted the focus to the key elements of integrated care: process-of-care and structural elements (see Table 2). McGinty explained that the process-of-care elements include proactively and systematically identifying patients and connecting them to evidence-based treatments. Proactivity, she pointed out, is a hallmark of Wagner’s chronic care model and stands in contrast to traditional medical practice, which historically responds to a patient’s needs as they appear during an exam. She noted the importance of the structural elements that are needed to implement the process-of-care elements.
Policies to Support Integrated Care
Pivoting to a discussion of policies to support integrated care, McGinty explained that most policy actions so far have focused on financing mechanisms. She emphasized that a major barrier to scaling integrated care is the lack of insurance reimbursement mechanisms for the key process-of-care and structural elements, such as care management. She pointed out the three main approaches to addressing this barrier: Centers for Medicare & Medicaid Services (CMS) behavioral integration codes, primary care medical home reimbursement strategies, and ACOs.
TABLE 2 Key Elements of Integrated Care
| Key Elements of Integrated Care | |
|---|---|
| Process-of-Care Elements | Structural Elements |
|
|
SOURCES: As presented by Beth McGinty, June 3, 2020; adapted from McGinty and Daumit, 2020.
CMS behavioral health integration billing codes, introduced in 2017, are per-person, per-month billing codes adopted by Medicare, some commercial payers, and some state Medicaid plans (Carlo et al., 2018, 2020). General medical providers can use four of these codes, three of which are for care management and care coordination services delivered specifically within a collaborative care model and the fourth is for care management and behavioral health care management services delivered in any type of integrated care model. McGinty referred to a study that examined uptake of these billing codes, which found that only 0.1 percent of Medicare beneficiaries with MHSUDs had a behavioral health integration billing code indicating they received one of these integration services (Carlo et al., 2019; Cross et al., 2019). Of that 0.1 percent, 75 percent of the billing codes were for general behavioral health integration services rather than a collaborative care service. Subsequent qualitative work aimed at exploring the reasons why uptake of billing codes for integrated care is so low found that many practices lack the structural elements needed to provide the services to use the codes, particularly for the collaborative care codes that require a practice to have a consulting psychiatrist and a behavioral health care manager.
Turning to PCMHs, McGinty noted that they are focused on improving primary care more broadly rather than focusing explicitly on behavioral health integration. She did note, however, that PCMHs are also based on Wagner’s chronic care model, which has been used increasingly to integrate behavioral health into primary care. Some PCMH programs have used a relatively modest per-member, per-month payment of $20–$200 per beneficiary to cover care management or other previously nonbillable process-of-care services. McGinty emphasized that two federal demonstration projects—the Comprehensive Primary Care Program (Peikes et al., 2018) and the Multi-Payer Advanced Primary Care Demonstration Program (Leung et al., 2019)—failed to lead to high uptake of evidence-based behavioral integration practices.
McGinty noted that ACOs, the third approach to support integrated care, are like PCMHs in that they are not focused specifically on behavioral health integration. However, ACOs can incentivize behavioral health integration through shared savings, and potentially losses, in two-sided risk arrangements tied to achieving quality of care and health care spending targets. Despite the proliferation of ACOs in the United States, McGinty noted that the available evidence reveals that ACOs have had some small but not clinically meaningful effects on care for people with MHSUDs (Busch et al., 2016; Gordon, 2016; O’Donnell et al., 2013). One reason for this limited impact, she explained, is that behavioral health specialists are often excluded from ACO networks. In addition, ACO payment incentives have emphasized metrics for general medical conditions and not behavioral health.
McGinty explained three major lessons learned from these various attempts to use policy to incentivize integrating primary care and behavioral
health care. First, multi-payer financing arrangements are important for supporting both process-of-care and structural elements of integrated care models. Behavioral health integration billing codes have so far focused on process-of-care elements, but frontline providers report that they cannot implement those elements because they do not have the structural elements in place.
Second, McGinty noted, primary care has to be accountable for the health of the whole person. “We have historically held primary care physicians responsible for general medical conditions and behavioral health specialists responsible for behavioral health conditions, and that does not incentivize truly meaningful collaboration and care integration around improving the health of the whole person,” said McGinty. ACOs, because they have incentives to improve “whole-person” health, could be part of the answer if policies more effectively addressed some of the barriers discussed above, such as the failure to appropriately align payment incentives with behavioral health performance metrics.
Third, policy barriers that are antithetical to integrating care still exist, such as multiple state Medicaid programs prohibiting clinicians from billing for a general medical service and a behavioral health service for the same person on the same day, said McGinty. While the 21st Century Cures Act7 clarified that federal law does not prohibit same-day billing, several states still maintain that prohibition. McGinty noted that behavioral health carve-outs, where behavioral health benefits are administered by a separate organization than general medical benefits are, are a major policy issue in today’s behavioral health policy dialogue. Some providers and insurers have cited this separation of benefit management as a barrier to integrated care, though evidence supporting that is limited. One study examined the effects of carving in behavioral health benefits in the Illinois Medicaid program and found that doing so decreased the cost of behavioral health care without changing use (Xiang et al., 2019). McGinty warned that the study, however, failed to answer key questions about the degree to which that carve-in prompted care integration processes and improvements in quality of care or health outcomes for people with behavioral health conditions.
McGinty explained that various condition-specific policy barriers exist as well. For example, federal regulations require primary care providers to obtain a special waiver from the federal government to prescribe buprenorphine for OUD. Primary care providers are also prohibited from prescribing methadone.
Ultimately, in McGinty’s view, financing policies are likely to be necessary but not sufficient to truly prompt adoption of complex, effective integrated care models. She sees a strong need for additional policy activity regarding
___________________
7 For more information, see Public Law 114-255. See https://www.congress.gov/bill/114th-congress/house-bill/34 (accessed August 25, 2020).
the behavioral health workforce. Primary care clinicians often cite a shortage of behavioral health workers as a barrier to implementing integrated care. Options to address this issue range from traditional health care workforce policies to adopting better reimbursement policies for telemedicine to deliver behavioral health services. McGinty shared her hope that the rapidly evolving telemedicine landscape prompted by the COVID-19 pandemic will provide some important lessons. She emphasized that meaningfully addressing the behavioral health workforce problem will require reimbursing behavioral health services at a sufficiently high rate to incentivize clinicians to choose challenging behavioral health careers.
As a final comment, McGinty noted that the adverse social determinants of health—including poverty, unemployment, housing instability, and involvement with the criminal justice system—are overrepresented among people with behavioral health problems. These factors also contribute to many of the barriers to care and poor health outcomes that individuals with MHSUDs experience. McGinty pointed to the range of policy options available to address the social determinants, particularly large-scale social safety net policies that target groups that include but are not limited to those with behavioral health issues. “I would also highlight the need to think about models that integrate not only general medical and behavioral health care but also social services,” said McGinty. Accountable health communities,8 which extend the ACO model into the community, may offer some lessons about the types of policies that can incentivize that type of three-way integration.
Panel Reactions and Discussion
Ruth Shim, the Luke & Grace Kim Professor in Cultural Psychiatry and associate professor in the Department of Psychiatry and Behavioral Sciences at the University of California, Davis, said that she was struck by McGinty’s final comments about the social determinants of health and the importance of figuring out how to integrate these and the social determinants of mental health into the work on integrating behavioral health care into primary care. “I feel that we are gaining traction in that space,” said Shim. “I think that in
___________________
8 According to CMS, the Accountable Health Communities Model is based on emerging evidence that addressing health-related social needs through enhanced clinical–community linkages can improve health outcomes and reduce costs. Unmet health-related social needs, such as food insecurity and inadequate or unstable housing, may increase the risk of developing chronic conditions, reduce an individual’s ability to manage these conditions, increase health care costs, and lead to avoidable health care use. For more information, see https://innovation.cms.gov/innovation-models/ahcm (accessed October 26, 2020).
the past several years, there has been movement to incorporate more work around social determinants of health and bringing all of that into the world of integrated behavioral health care.”
Barry agreed with Shim and added that historical legacies are still slowing progress on integrating primary care and behavioral health care. “It is discouraging, frankly, and we need to figure out how to move the ball,” said Barry, “but we need, as Beth and Gail have nicely done, to diagnose the problems first.”
For Barry, the reason behavioral health issues are treated differently than general medical issues comes down to economics, institutional policies, or stigma. Barry noted her concern that the financial strains health care systems are experiencing as a result of the COVID-19 pandemic will lead to strong incentives to cut costs. She fears that such pressures will limit integration efforts, given the inherent slowness of health care institutions to evolve. Barry added that she sees little progress in lowering the stigma associated with behavioral health issues.
Deidra Roach, medical project officer in the Division of Treatment and Recovery Research at the National Institute on Alcohol Abuse and Alcoholism (NIAAA), agreed that advancing integration efforts will depend on economics, institutional policy, and stigma and also require community participation. “I think [community participation] is a factor that has been largely overlooked in our planning of integrated care and that could make a significant difference in what our progress will be going forward,” said Roach. Noting the important role research will play, Roach strongly recommended that researchers use a community-based participatory model to take advantage of the wisdom of those living in the community, which may help resolve some of the existing structural issues.
Goldman asked the speakers to describe their key qualitative ingredients of integrated care, including the difficult-to-measure constructs, such as communication or teamwork. Daumit said that she believes these qualitative aspects of integrated care are both important and difficult to measure and pointed to the key qualitative ingredients of integrated care listed in the McGinty and Daumit paper:
- The belief of primary care clinicians and other people in a practice about the importance of population health, the goal of improving whole-person health, and shared values around these ideas;
- The implementation climate;
- How supportive leadership is of integrated care and evidence-based practice around collaborative care; and
- Whether clinicians have the self-efficacy to deliver integrated care (McGinty and Daumit, 2020).
Shim asked the speakers to comment on the cultural shifts needed to facilitate care integration and how to achieve them. Daumit said that organizational culture is incredibly important, and she posed questions to ask about that culture. “What is leadership thinking? What are all the different levels of clinicians and staff thinking, and what are the explicit and implicit incentives, formal and informal, that are contributing to that culture and climate?” In her opinion, the shift from differentiating physical health and mental health toward shared responsibility to the whole person will require medical training to end the practice of placing each discipline in separate silos. In addition, leadership will need to emphasize to all levels of the organization that new evidence-based practices are important to learn and implement. Finally, she said, financial incentives should support the cultural shifts toward integration.
Regarding the major barriers that the workforce itself poses to integration, McGinty said that she thinks of workforce issues as falling into one of two categories: the shortage of behavioral health workers and gaps in competencies among the current workforce. She noted that she addressed certain strategies for overcoming workforce shortages in her presentation, particularly the need to pay adequately for behavioral health services in order to create competitive financial packages for these clinicians at all levels, including nurse practitioners and physician assistants.
McGinty added that a silver lining of the COVID-19 pandemic is the expanded use of telehealth. While telehealth will not increase the number of behavioral health providers, it does allow them to extend their geographic reach into underserved regions of the country. Maximizing telehealth, though, will require policies designed to address the digital divide. To address the clinician training issue, McGinty said that it is important to ensure that accreditation policies require general medical providers to receive some training in delivering mental health care, and vice versa, and also that all clinicians receive training in team-based care.
Roach commented that one of the most troubling observations is that when key elements of collaborative care are implemented in real-world settings, the benefits for individuals with depression have been minimal (Solberg et al., 2013). McGinty said that understanding why that is true is the million-dollar question. After all, multiple rigorous clinical trials have found that collaborative care-based models can be effective at improving depression symptoms and improving outcomes for people with SUDs. Nevertheless, evaluation of the Depression Improvement Across Minnesota, Offering a New Direction Initiative9—a statewide effort to implement depression care in primary care settings (Solberg et al., 2013)—showed that while it expanded the
___________________
9 For more information, see https://aims.uw.edu/depression-improvement-across-minnesota-offering-new-direction-diamond (accessed August 25, 2020).
delivery of depression care in the primary care setting, there were no effects on patient outcomes in terms of improving depression symptoms or remission (ICSI, 2014). McGinty noted that this was the case even though the initiative included a care management tracking system and payment designs to cover both process-of-care and structural elements along with intensive training for leaders, frontline providers, and staff.
This discouraging result has researchers trying to determine which key elements of the collaborative care model are not being translated from clinical trials to real-world contexts. Daumit mentioned one possibility, which has yet to be tested empirically: treatment intensification was not occurring in the real-world setting to the degree that it took place in the experimental setting. Daumit added that she hopes efforts to improve primary care, which has its own issues, will incorporate behavioral health priorities.
Goldman, posing a final question before inviting questions from webinar participants, asked McGinty about any downsides to the carve-in arrangements she mentioned in her presentation. There could be, she acknowledged, particularly because no strong evidence shows that such arrangements are good for behavioral integration. “It makes intuitive sense on many levels, but it has not, at this point, been empirically demonstrated,” she said. One place where carve-outs work well, she noted, is for specific specialty services, such as psychiatric rehabilitation or intensive outpatient care that may not have clear parallels on the general medical services side. Daumit agreed that a well-run carve-in could benefit behavioral health care integration, but she worries that when budgets and services are cut, behavioral health services will be the first to go.
Question and Answer Session with the Webinar Participants
A webinar participant asked the panelists to comment on the role of training primary care providers regarding stigmatization of people with MHSUDs. This participant noted that they had heard primary care providers say that they do not want their practices to be places where “those people” come for care. Daumit replied that there may be a need to better screen those who are admitted to medical school in addition to providing better training. “I think that once people go into their practices and health care organizations, the organizational culture cannot tolerate anything like this anymore,” said Daumit. “I think we need to recognize consumers with mental illness and substance use problems as a population [for which there are significant] disparities that deserves all the same interventions to break down stigma as other minority and disabled populations have had over the years.”
McGinty noted that anti-bias training for clinicians can be effective in reducing race-related biases, and the same type of training is needed for stigma
surrounding MHSUDs. McGinty referred to a national study of primary care physicians and their attitudes about people with OUD (Kennedy-Hendricks et al., 2020; McGinty et al., 2020) that she and her colleagues completed recently. The study revealed that primary care physicians endorse the medical model of OUD and do not believe that SUDs in general are a moral failing and the individual’s fault. At the same time, they hold other quite stigmatizing attitudes toward people with OUD. “They are very unwilling to have a person with opioid use disorder, even a person who is on stable treatment with guideline-concordant medication, as a neighbor or marry[ing] into their family,” said McGinty. “They do not want a clinic that provides buprenorphine or methadone in the neighborhood where they live.” Addressing these attitudes requires anti-bias training, she added.
In Shim’s view, the issue goes beyond stigma and is a case of systemic structural discrimination against people with serious mental illness and SUDs. “I appreciate Gail’s comment that we have to do a better job of evaluating the workforce and making sure that the people that we bring into the profession do not harbor discriminatory beliefs toward people with serious mental illness and SUDs,” said Shim. Roach added that anti-bias training needs to begin at the earliest stage in the education of providers, even well before medical school, because these attitudes become ingrained at an early age and are difficult to reverse after that. McGinty remarked that it is important to recognize that anti-bias training and anti-stigma training alone are likely not enough. Rather, she said, they need to be paired with policy and system-level changes that empower clinicians to work with people with behavioral health disorders in a way that is effective for all people.
There were multiple questions from the webinar participants regarding CMS behavioral billing codes. One question was whether Medicaid Section 1115 waivers10 could be used to promote adoption by and provide technical assistance to primary care practices. McGinty responded that she was not aware of any states doing that, but this does seem to be a potential use. “I do think there is definitely a role for technical assistance around use of these codes and support in helping to get some of the structures in place to help practices bill these codes,” she said, adding that technical assistance alone will not address
___________________
10 Section 1115 of the Social Security Act gives the Secretary of Health and Human Services authority to approve experimental, pilot, or demonstration projects that the secretary finds to be likely to assist in promoting the objectives of the Medicaid program. Section 1115 demonstration projects present an opportunity for states to institute reforms that go beyond routine medical care and focus on evidence-based interventions that drive better health outcomes and quality of life improvements. For more information, see https://www.medicaid.gov/medicaid/section-1115-demonstrations/about-section-1115-demonstrations/index.html (accessed June 23, 2020).
staffing elements of care. Goldman noted that the Advancing Integrated Mental Health Solutions (AIMS) Center at the University of Washington has provided technical assistance on both the conduct of collaborative of care and some of the policy issues discussed during the webinar. It also has a collaborative care implementation guide available for downloading.11
The final question focused on whether there is evidence that any of the many approaches to integrating behavioral and physical health are more effective. Daumit responded that multiple clinical trials offer evidence that the collaborative care model of integrating behavioral health into primary care is effective for depression and anxiety. Much less evidence exists, she said, regarding efforts to bring physical health care services into behavioral health care settings.
Closing Remarks of the First Webinar
In closing, Roach observed that although the participants could not be together physically, she still felt the energy of a committed community. “We believe that energy is transforming health care in the U.S.,” said Roach, “such that in the foreseeable future it will consistently reflect the reality that optimal physical health is only possible when there is optimal mental health and vice versa.”
ESSENTIAL COMPONENTS OF CARE FOR THREE MHSUD CONDITIONS IN PRIMARY CARE SETTINGS
Goldman introduced the second webinar by explaining that the day’s panelists would elaborate on their understanding of the essential components of care for three illustrative conditions: depression, alcohol use disorder, and OUD. The panelists were also charged with highlighting crosscutting components of care and possible differences among those conditions. Goldman encouraged the panelists to explore the issues important to prevention, screening, case identification, and treatment in primary care settings, including those with limited resources.
Exploring the Essential Components of Care for Alcohol Use Disorder in Primary Care Settings
Richard Saitz, professor and chair of the Department of Community Health Sciences at the Boston University School of Medicine and School of Public Health, began his remarks with an anecdote reflecting the challenge of
___________________
11 For more information, https://aims.uw.edu/collaborative-care/implementation-guide (accessed November 23, 2020).
caring for individuals with alcohol use disorder in primary care. He explained that in 2015, he and a colleague came across a paper in a major medical journal that validated a screening tool for alcohol and other drug use disorders (Tiet et al., 2015). His colleague wrote a letter to the journal pointing out that this tool, while useful for identifying these disorders, would not identify the full spectrum of unhealthy alcohol use. When the letter was published (McNeely and Saitz, 2015), the editor added a note that acknowledged that the field of drug use and screening would benefit from clarity in terminology—distinguishing between substance use and an SUD—and added, “However, in practice, it can be very challenging to distinguish between substance use and an SUD.”
Saitz was stunned by the response. “I was really shocked that an editor of a major medical journal would admit and write down that it would be hard to tell the difference between substance use and SUD,” he said. “It is almost like saying that you could not tell the difference between high cholesterol and myocardial infarction or an elevated glucose [level] and a diagnosis of diabetes.” In fact, Saitz pointed out, alcohol use disorder and the spectrum of unhealthy alcohol use taken together are similar to the spectrum of elevated cholesterol or glucose levels and their respective progression to heart disease and diabetes. He described that the spectrum of alcohol use begins at abstinence; proceeds to low-risk use, risky use, at-risk use, and hazardous use; and culminates in alcohol use disorder. As consumption increases, so do the associated consequences, Saitz added.
Saitz described what he considered the essential components of care: identify the disorder, discuss the diagnosis and treatments with the patient, treat the disorder, and refer the individual for services and specialized care. “These are similar components of care across many conditions, medical, psychiatric, and otherwise,” he said. Saitz pointed out that for alcohol use disorder, one single question—how many times in the past year have you had five or more drinks in 1 day for a man or four for a woman—is a simple, validated screening test (Smith et al., 2009).
Saitz explained that the next step is to identify any consequences of excessive use to determine if the individual has an alcohol use disorder. The 11 criteria in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (APA, 2013) serve that function. In terms of discussing this diagnosis and possible treatments with the individual, Saitz said that there is no difference between how the primary care physician should address alcohol use disorder or a condition such as hypertension. Saitz noted that while some individuals may deny they have an alcohol use disorder and not want to treat it, this is similar to how some people with hypertension deny they have a problem because they are not feeling any symptoms.
In Saitz’s view, the SBIRT model has shortcomings because it only includes a brief intervention and then referral and does not include treating
alcohol use disorder as an essential component of care. “Although I am an addiction specialist as well as a primary care physician, I will say that treatment for alcohol use disorder is not really that complicated,” noted Saitz. There are four available medications, he explained, and primary care providers can monitor response simply by asking about drinking, any side effects, and the patient’s challenges and successes. If an individual requires more comprehensive care than the clinician can offer with repeated counseling and medication, the clinician will refer the patient for specialized treatment in the same way as for a patient who was not responding to high blood pressure treatments.
The task ahead, said Saitz, is to convince the primary care clinical community that addressing alcohol use disorder is not very different from identifying and treating hypertension or diabetes. Saitz added that while there are comorbidities associated with alcohol use disorder, primary care providers are accustomed to addressing multimorbidities. While acknowledging that primary care providers are already stretched for time, Saitz noted that he has never heard a primary care physician say they do not have enough time to treat hypertension or diabetes. In fact, he added, it is more difficult to get someone to take insulin for diabetes than it is to prescribe daily naltrexone for alcohol use disorder. In closing, Saitz suggested convincing primary care providers that alcohol use disorder is their responsibility so that they take on that role and address the stigma and systems that act as barriers to care.
The Case for Integrating MHSUDs into Primary Care
Sarah Wakeman, medical director for the Substance Use Disorders Initiative, program director of the Addiction Medicine Fellowship at Massachusetts General Hospital, and assistant professor of medicine at Harvard University, began her remarks by pointing out that when making a case to primary care providers about treating SUDs, it is critical to understand what the patient wants. Wakeman noted that it is irrelevant, for example, if she believes that a person should make changes related to their drug or alcohol use. Rather, it only matters if the patient believes their life is going to be better if they do so. She added that it does not matter that she thinks all primary care doctors should be treating alcohol and drug use disorders. “The point is, why might primary care doctors think that this is in their purview and as important as treating diabetes or hypertension?” she asked.
The answer, she said, ties into the three devastating public health crises affecting the nation: the drug overdose crisis, the COVID-19 pandemic, and the epidemic of racism. She noted that addiction medicine is a field closely tied to racism, given that the nation’s drug policy has its roots in racism. She explained that people of color experience discrimination under every com-
ponent of U.S. drug policy and at every stage of the criminal justice system. “If we are going to talk about racism, we have to talk about drug policy, and part of that is about identifying and treating those who do have [an] SUD as having a medical condition,” explained Wakeman.
She then explained that the second reason primary care should include alcohol and substance use treatment in its purview is that treatment in primary care is feasible, effective, and rewarding. It is much more difficult, for example, to safely manage anticoagulation or insulin titration, heart failure, and many other issues that primary care is adept at treating. In Wakeman’s experience, primary care providers say they do not have the time or skillset to treat alcohol and drug use disorders for two reasons. First, treatment is not taught in medical school. Second, because of this, primary care has been given a pass on thinking of these disorders as medical conditions that should be addressed as part of what is normally considered general medical care.
As Wakeman observed, multiple studies have shown that these disorders can be effectively treated in primary care with outcomes that are as good as in specialty care settings. She cited one study that examined buprenorphine treatment in primary care, with or without adjunctive psychosocial addiction treatments, such as cognitive behavioral therapy (Fiellin et al., 2014), and found no difference in study completion, opioid use, or cocaine use between primary care medication management with or without adjunctive psychosocial intervention. The fact is, said Wakeman, primary care providers can manage these conditions, and that is often where patients want to receive treatment—by the doctors and care teams they trust.
Wakeman pointed out that one important task for primary care “is to reframe the way we think about care for people who use substances and the ways that we inadvertently harm people in our health care system who use alcohol and drugs.” As an example, she explained that if a person came into the hospital experiencing a myocardial infarction and recurrent chest pain, they would not be discharged against medical advice. “And yet if a person with an SUD is in the hospital and is having ongoing substance use, often the response is this punitive one of kicking people out of care or forcing them out of care,” said Wakeman.
She observed that while the medical profession talks about the harm that alcohol and drug use does to people’s health, many of the health consequences of substance use are related to health system policies and approaches. Drug users, for example, do not get infective endocarditis from heroin but rather as a result of contaminated drug supplies and a punitive drug policy approach that forces people to use heroin in secrecy and in unsanitary conditions—without access to safer injection equipment or supervised injection sites. In addition, the health care system often treats people who use drugs and alcohol differ-
ently than other patients in terms of security, visitor policies, and the length of time they are allowed to stay in the hospital. Wakeman noted that “in those ways, the health outcomes and health harms of someone’s substance use are more related to our approaches, to discrimination and stigma, than to the actual substance itself.”
For Wakeman, developing a system of care that treats SUDs and delivers effective medical care to all patients who use substances requires thinking about what patient-centered and patient-guided care really mean. As with any other disorder, the patient’s needs, wants, and preferences should be what the primary care system focuses on first, not what providers think is the most important need. Wakeman explained that she and her primary care colleagues take the approach that caring for those with an SUD is both the right thing to do and the smart thing to do if the goal is to take better care of populations, keep people out of the hospital, reduce health care costs, and keep patients healthy.
Wakeman observed that one reason providers tend to blame patients for their substance use issues is that these providers can feel helpless and do not know what to do. The remedy to this problem is to provide clinicians with tools they need to be able to successfully treat these patients. Wakeman noted that one approach is to use addiction champions—doctors, nurses, behavioral health providers, and recovery coaches—who themselves have had experience with an SUD. Addiction champions are valuable members of multidisciplinary teams and can deliver a multidisciplinary care model, much like what is used to care for patients with HIV or diabetes.
Wakeman stressed that it will be important to study different care models to determine what aspects are effective and which are not and to inform the primary care community about the results of those studies. She and her colleagues, for example, looked at practices with or without integrated SUD care and found that individuals with SUDs who received care in a practice without integrated services had more ED visits and a higher number of total inpatient bed days (Wakeman et al., 2019).
Wakeman added that while data are important, narrative and patient stories can be valuable in terms of spreading hope and giving people—patients and their health care teams—a tangible reminder that an SUD is a highly treatable condition with a good prognosis. “I do not think the first thing many of our providers think, when they hear about someone who is injecting heroin or fentanyl, is ‘wow, that is incredibly treatable,’” said Wakeman, “and yet it is.” Many people, she said, will achieve remission and go on to live healthy lives, and helping an individual get to that place is incredibly rewarding to providers. She added that embedding recovery coaches in the system has been one powerful way to consistently remind people of that message of hope.
In closing, Wakeman shared a quotation from one of her institution’s 14 recovery coaches:
I am a woman in long-term recovery from opioid use disorder. Facing early trauma and adversity at a young age, I struggled with a severe opioid use disorder for 17 years and had almost given up hope. I began to have multiple critical infections as a result of my use and luckily was finally introduced to a medication to treat my opioid use disorder. Without the treatment of buprenorphine, I would never have been able to build the foundation of my recovery supports [that] I now stand on 6+ years later. I am incredibly proud to say I have a leadership role at a major medical center working to help patients such as myself with substance use disorder. I am also a mom to the most amazing little boy, a wife to an amazing husband, and a homeowner. Without that initial treatment of buprenorphine, I know none of these things would have been possible.
Implementing Collaborative Care Treatment for Depression
Lydia Chwastiak, professor in the Department of Psychiatry and Behavioral Sciences and co-director of the Northwest Mental Health Technology Transfer Center at the University of Washington, opened her remarks by noting that the majority of integrated care interventions that have been shown in clinical trials to improve depression outcomes have been some variation of collaborative care. In fact, she said, evidence from more than 80 randomized controlled trials supports the effectiveness of collaborative care for improving depression and anxiety outcomes (Archer et al., 2012). The first large, multi-site trial to demonstrate its effectiveness in treating depression was the Improving Mood–Promoting Access to Collaborative Treatment (IMPACT) trial, which involved 2,000 participants at 8 health care organizations (Unützer et al., 2002).
Chwastiak explained that collaborative care is derived from the chronic care model, and it has five core principles that provide the foundation for effective implementation (see Figure 2).
Chwastiak noted that the primary care provider is a critical member of the collaborative care team and continues to prescribe and monitor all medications. In addition, collaborative care adds two members to the primary care team that treats depression. The first is a behavioral health care manager, often a social worker, who is integrated into the primary care team. The care manager has two sets of tasks: general care management, such as tracking and coordinating care and conducting systematic follow-up, and providing evidence-based brief behavioral interventions for depression or anxiety. The second new team member is a psychiatric consultant who is typically not in the primary care clinic and does not see patients directly but does spend 2–3
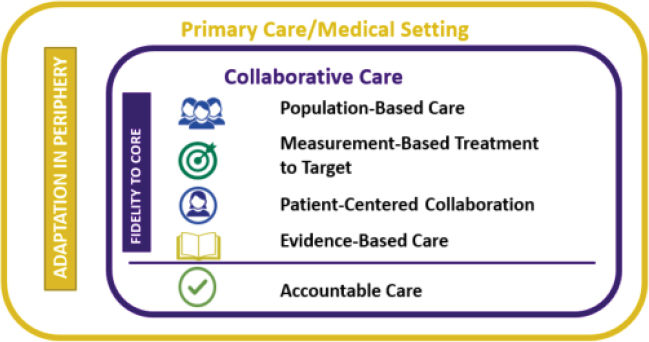
SOURCES: As presented by Lydia Chwastiak, July 29, 2020; used with permission from the University of Washington AIMS Center, 2020.
hours per week working with the care team, including taking part in a structured weekly caseload review meeting with the care manager.
Chwastiak noted that studies have shown that collaborative care is not only significantly more effective than usual care but also associated with a shorter time to depression remission (Garrison et al., 2016). For example, data from a large, statewide collaborative care implementation project in Minnesota, conducted over 5 years with more than 7,300 individuals with depression, showed that the mean time to remission of symptoms was 86 days for those who received collaborative care. In contrast, it was 614 days, or seven times longer, for those who received usual primary care (Garrison et al., 2016). She noted that a typical course of treatment in collaborative care is 6–12 months, and between 50 and 75 percent of the individuals in treatment will require at least one change of treatment during that time. Collaborative care’s use of measurement-based care and “treatment-to-target” facilitate timely treatment adjustments that are critical to reducing time to response. Chwastiak noted that treatment-to-target in this context involves defining a measurable target for treatment—such as a PHQ-9 score of less than 5 for depression remission—and then monitoring the desired outcome at clinical visits with regular review to iteratively adjust treatment.
Chwastiak explained that measurement-based care and treatment-to-target are only as effective as the actual depression treatment provided, which is why the use of evidence-based treatments is the fourth core element of collaborative care. Collaborative care uses both guideline-adherent medications for depression and brief psychotherapy interventions that fit a treatment schedule
of 30-minute visits every other week. She noted that structured, manualized treatments, such as problem-solving therapy and behavioral activation, are most feasible for this context.
Chwastiak pointed out that the final element of collaborative care, accountable care, means that collaborative care increases access to care and, in doing so, provides care to more patients and minimizes the time between identification and care. Collaborative care is accountable care because it (1) includes a systematic approach to identifying individuals who would benefit from care, and (2) incorporates a strategy of continuous quality improvement in terms of both treatment of individual patients and evaluation of program performance. Chwastiak stressed that collaborative care, like any evidence-based intervention, needs to be adapted to the specific setting in which it is implemented, but while every implementing organization makes some changes to the model, the core principles must be retained for effective implementation.
In her organization’s experience, said Chwastiak, adequate staffing with trained employees who have dedicated time for their roles in collaborative care is essential for effective implementation of the model, as is effectively using a registry. Financing mechanisms also have played a critical role in sustaining the program in organizations around the country. Chwastiak explained that process-of-care elements that facilitate implementation of collaborative care include standardized screening and referral workflows, training teams and providing them with ongoing support, and operationalized accountability through audits and feedback.
Chwastiak pointed out some barriers to implementing the care model that her team has experienced: difficulties hiring a care manager or identifying a psychiatric consultant because of workforce shortages. She noted that telepsychiatry has proven to be an effective tool for extending the reach of psychiatric expertise and engaging a consulting psychiatrist for a collaborative care program. Currently, for example, through the Mental Health Integration Program, psychiatrists based at the University of Washington act as consulting psychiatrists for collaborative care programs in more than 100 community health centers across Washington State. There is also evidence that the role of the care manager on the collaborative care team can be conducted virtually and be effective. Chwastiak observed that telepsychiatry is increasingly important as the COVID-19 pandemic continues to impact the nation.
Recent research, said Chwastiak, has focused on developing and adapting models to comanage multiple conditions, such as depression and diabetes (Ali et al., 2020; Chwastiak et al., 2017). She added that these models need to also address social determinants of health systematically.
In closing, Chwastiak remarked that the 2017 CMS billing codes for collaborative care have represented a major advance for implementing this model. She pointed out that in her experience, uptake of these codes was
slow initially but has increased as Medicaid programs and some private payers adopted the codes.
Sustaining Successful Interventions in Primary Care Practices
Frank deGruy, the Woodward Chisholm Chair and professor of family medicine at the University of Colorado School of Medicine, often thinks about successful primary care–based interventions for mental health problems and the reasons those interventions cannot sustain themselves after a successful demonstration. In deGruy’s experience, clinicians adopt a successful intervention and then tend to gradually drift back to pre-intervention workflows within 6 months to 1 year in the face of all the other responsibilities primary care providers have to fulfill. In fact, embedded behavioral care clinicians and embedded care managers are, in practice, primary care clinicians. “They get pulled into all of the other noisy, dirty problems that are more important at that moment and have great difficulty staying focused on the original problem for which they might have been hired into the practice,” said deGruy. To illustrate that point, he noted that of the 2,900 practices that implemented the Comprehensive Primary Care Plus model (CPC+) starting in 2017, more than 95 percent achieved some behavioral health integration by 2019, but only 700 of those practices looked anything like the collaborative care model despite it being the only model offered during the program’s first 3 years.12
DeGruy explained that the dominant integrated care model implemented over the past 15 years, integrated behavioral health in primary care (IBH-PC), embeds a care manager and a behavioral health clinician—usually a psychologist or social worker with or without a psychiatrist or psychiatric nurse practitioner—in the primary care clinic. He added that evaluating whether this type of integrated care is effective for addressing depression, anxiety disorders, SUDs, and alcohol use disorder is difficult because the IBH-PC model is not disease specific. “You are looking at integrated care as the active ingredient, applied differently in different practices to different conditions, according to that site’s most pressing problems or according to the patient’s most pressing problems,” explained deGruy.
In terms of the evidence base for integrated primary and behavioral health care, deGruy pointed to the results of Advancing Care Together, a Colorado-
___________________
12 CPC+ is a national advanced PCMH model that aims to strengthen primary care through regionally based multi-payer payment reform and care delivery transformation. CPC+ includes two primary care practice tracks with incrementally advanced care delivery requirements and payment options to meet the diverse needs of primary care practices in the United States. For more information, see https://innovation.cms.gov/innovation-models/comprehensive-primary-care-plus (accessed August 12, 2020).
wide trial of an integrated primary care and behavioral health model (Green and Cifuentes, 2015). He noted that the Agency for Healthcare Research and Quality’s Integration Academy13 maintains a research collection that focuses on evidence that supports various models for various conditions in various clinics. The Integration Academy also provides playbooks, guides for professional practice, assessment measures, and resources for treating OUD and other SUDs.
Based on his observations of integration efforts, both successful and less so, deGruy offered four suggestions about ways to study and assess whether an integration model is successful. First, it is critical to fully understand the work of primary care clinicians and reconceptualize interventions according to a revised understanding of the workflow in a primary care setting. “If we wish to develop sustainable interventions that fit into their workflow, I think dealing with disease-specific interventions is not likely to ever get us there,” said deGruy. DeGruy also suggested no longer running controlled clinical trials on these interventions. In his view, such trials are best deployed when an intervention can be standardized for a well-defined target population in which the context (comorbid conditions and family, social, and environmental factors that affect that population) is in effect irrelevant. “That does not describe usual primary care,” he said.
Third, deGruy asserted that disease-specific outcome measures are at best insufficient and at worst inappropriate and “crushingly burdensome.” In deGruy’s view, primary care’s demonstrated value to individuals and populations lies not in its ability to produce improvements in disease-specific outcomes but in overall health and longevity.
His final recommendation was to fully commit to garnering the needed resources to “actually develop and stabilize a sustainable model in primary care.” Primary care practices are stretched to the limit already and do not have the margin to plan and implement a workflow change, fit that into their other workflows, and then realize sufficient revenue from that added set of tasks to keep it as a first priority, said deGruy. “We have to quit trying to get quality on the cheap,” explained deGruy. In his opinion, the previous speakers had each described enormously successful interventions that will work in primary care but only if sufficient resources are allocated to keep those interventions as priorities in practice in the face of all the other demands being made of primary care. “As long as we expect primary care to contend with the tsunami of demands and expectations that keep pouring over the transom of what else needs to be done there, these are not going to be sustainable interventions,” he warned in closing.
___________________
13 For more information, see https://integrationacademy.ahrq.gov (accessed August 12, 2020).
Panel Reactions and Discussion
Goldman opened the panel discussion by pointing out that he did not understand how IBH-PC or other integration models will overcome the difficulties deGruy identified in terms of implementation fidelity and financial sustainability, to which deGruy replied that there are several possible mechanisms by which a primary care practice can be financially sustainable with additional care managers and behavioral health clinicians. One approach is to increase billing through the increased productivity that occurs when there is a behavioral health clinician available to deal with complex behavioral issues. In fact, he said, he has observed team-based care that is efficient enough to cover the cost of the team members who may not be able to bill for their services. He noted, too, that when primary care practices are left to their own devices, they settle into what he called the “first generation of integrated hybrid models,” in which the embedded behavioral health clinicians take on whatever conditions with which patients present.
Responding to Goldman and deGruy’s comments, Chwastiak said that a criticism of the collaborative care model is that it is too complex for many organizations to implement. Yet, all integrated care models face some similar implementation challenges, such as workforce shortages of behavioral health care providers—which is particularly problematic for rural and frontier communities. Chwastiak noted that CMS billing codes for collaborative care have increased programs’ financial sustainability and led to increasing adoption of the model nationally. In Chwastiak’s view, the administrative requirements for using the CMS billing codes are modest but can be burdensome for small practices. She was careful to point out, however, that for all practices, there is a large clinical and administrative burden when services are only reimbursed by one payer, such as Medicare. Clinic staff then have to sort out what services can be billed to Medicaid and private insurance.
Commenting on the idea of stretching a model versus drifting from model fidelity, Chwastiak explained that many providers and clinics have been very creative in trying to flex the collaborative care model to fit the particular setting and patient population, but it is critical that programs maintain the four core components. Goldman noted that when he and his colleagues analyzed implementation results from the original IMPACT study,14 he was impressed with the robustness of the comprehensive care model in a wide array of primary care settings, including the U.S. Department of Veterans Affairs (VA), Kaiser Permanente, and private and multigroup practices.
Goldman then asked Chwastiak to talk about the type of adaptations that have to be made to address deGruy’s suggestion to move away from a
___________________
14 For more information, see https://aims.uw.edu/keyword-tagging/impact-trial (accessed August 25, 2020).
disease-specific model. She replied that it depends on the context in which the implementation will occur, the disorders that will be treated, and the composition of the care team. As an example, she explained that when she and her colleagues moved from treating depression to co-managing depression and diabetes, they found a completely different workflow in diabetes specialty clinics that required adaptations to the intervention. The key, she said, was to learn from the work on implementation science that has been done over the past decade or more to understand how to flexibly adapt the program while maintaining the core elements of the evidence-based intervention. In turn, deGruy seconded Chwastiak’s comment about implementation science and said that he believes that will be the way forward as far as adapting comprehensive care to work in regular primary care settings.
Pivoting to a new topic, Goldman asked Wakeman what her institution is doing about policies that reflect racism and structural racism associated with SUDs and alcohol use disorder. Wakeman replied that there are two parts to that question: how to change the outright discrimination and stigma people who have an SUD experience when they come into the health care system and how to address structural racism. Though these two are interwoven, she said, they have slightly different answers. Wakeman pointed out that in the ED, the key has been to identify peer champions—other ED personnel—who can lead efforts to catalyze change and address discrimination and stigma against people with SUDs.
Wakeman described how one idea for catalyzing change came from a resident who had studied behavioral economics. This resident developed a social media campaign called “Get Waivered” in which the ED chair invited staff to obtain a waiver to prescribe buprenorphine and were paid for their time doing so. In addition, those who took advantage of this offer were celebrated on social media and in faculty newsletters, and they earned an opioid recovery champion badge to wear with their hospital identification. “It was a way of making this work valued and recognizing people for what they were doing,” said Wakeman.
Another approach adopted by Wakeman’s institution was to start every faculty meeting with outcome stories for people the ED staff had seen weeks or months earlier. This enabled ED staff to better understand the positive impact their actions were having on the lives of people they treated, something that they rarely hear. “Now, 95 percent of our emergency medicine attendings are waivered to prescribe buprenorphine, and we now have 24/7 access in the emergency department,” said Wakeman.
She cautioned that addressing the bigger question of structural racism is much more difficult given how embedded it is throughout society and the health care system. One piece of the solution is to use data to identify where racism exists in all components of the care system, including addiction referrals, retention, and engagement. Wakeman added that for too long, people
have talked about race as a risk factor, when the real risk factor is racism and living in a racist society. Another aspect of the solution is to hire, retain, and promote Black and Latinx leaders in addiction medicine, starting early in the educational pipeline, to create an environment that is welcoming to Black people, Indigenous people, and other people of color.
Wakeman shared that in her experience, people will leave the hospital prematurely because they feel they are being treated poorly or have competing priorities that the health care system has not recognized. She and her colleagues have found that people being treated for an SUD come to believe they are being treated differently than others in the hospital or that being hospitalized feels like being incarcerated, something many patients with an SUD have experienced. Often, she said, health care providers believe they are doing something good and protecting patients from trying to access drugs while they are in the hospital, rather than seeing that those actions are actually hurting their patients.
Goldman then asked Saitz to talk more about the decision to treat someone in the primary care setting or refer them to a specialty clinic. Saitz replied that this is not an either/or situation. “Of course we need to do some disease-specific things because there are specific treatments that improve disease-specific outcomes, and, in doing so, they often translate into overall better health as perceived by the patient,” he said. Some of the specific treatments for alcohol use disorder—oral naltrexone and acamprosate—are not difficult for a primary care physician to learn and prescribe. Moreover, the brief counseling that goes along with these pharmaceutical treatments does not differ from the counseling that is given with high blood pressure medication. In the case of heavy drinking, counseling would include asking people if they are continuing to drink heavily, and if so, why, and what challenges they are facing in cutting back on their alcohol consumption. If they have had some successes, counseling would include congratulating them.
Saitz pointed out that every primary care clinician makes referral decisions based on their own expertise and experience. For example, a clinician might have expertise in treating cardiac disease and have a high threshold to refer a patient to a specialist, but that same clinician may feel uncomfortable treating someone with diabetes and refer them to a specialist right away. The same can be true with alcohol use disorder and OUD.
One factor that goes into whether to make a referral or not, added Saitz, is the satisfaction providers get from caring successfully for their patients. A survey he and his colleagues conducted two decades ago asked primary care doctors and some nurse practitioners if they were satisfied caring for people with diabetes, high blood pressure, alcohol use disorder, and SUDs. The results showed that the respondents were least satisfied caring for patients with SUDs, moderately but still not so well satisfied taking care of patients with alcohol use disorder, and very satisfied taking care of patients with high blood pres-
sure. It is unclear why this was the case, given that some of the most satisfied primary care clinicians he has met over the past decade have been those that began prescribing buprenorphine for OUD. “I have had people come up to me surprised at how happy and excited they were taking care of patients with opioid use disorder, and they would have never predicted that,” said Saitz.
Question and Answer Session with Webinar Participants
The first two questions asked for ideas on how to make care more patient-centered and focus on what patients want so they feel heard and respected. Saitz responded that when presenting a diagnosis, the clinician should talk to the patient to find out how the diagnosis is impacting their life. In the case of alcohol dependence, the patient might identify the consequences related to their drinking. The clinician might then turn the discussion to what the patient might want to change, using motivational interviewing techniques that help the patient feel listened to and respected (Morgenstern et al., 2012). He noted that emerging evidence suggests that many people can perceive and experience improvement in important outcomes (Kuerbis et al., 2014; Tucker et al., 2020) while continuing to consume alcohol. “They can reduce their drinking substantially to the point where they are satisfied that they have achieved a good outcome, that they feel good, that their health-related quality of life is better,” said Saitz. Chwastiak added that focusing on patient preferences and their perceptions of potential benefit from treatment is also important for treatment of depression.
The next question was directed to Wakeman, requesting a comment on what can be done to better educate medical students and residents in primary care about drug and alcohol use disorders. Wakeman replied that evidence-based treatments for these conditions need to be part of medical education, which is currently not the case. Some students may receive 1–2 hours of instruction on addiction-related content, but they are not getting weeks of both book and experiential learning or exposure to clinical care for these disorders in their clinical rotations. In addition, she said, faculty need to be mentoring students and trainees to show them that addiction medicine is a rewarding and meaningful specialty. Such a message of hope and positivity can help counteract the nihilism and pessimism about treating these disorders that trainees may get from only seeing end-stage patients in the emergency room. Wakeman noted that students want those positive messages, especially those who are passionate about social justice and view drug and alcohol addiction as a social justice issue.
The panelists were asked to comment on whether they saw signs indicating that insurers are becoming more focused on value-based care and if that might help promote models such as integrated care and collaborative
care. In reply, deGruy said that he believes value-based care is likely to be the mechanism that fits most comfortably with what primary care is attempting to become. What will be important, he said, is to listen to and respond to a patient’s values and desires while avoiding a negative impact on quality measures if what the patient desires is not considered optimal care. For example, a smoker with end-stage lung disease may not want to quit smoking but merely stay alive long enough to see his daughter graduate from law school. “I think it is important that we continue to adjust our complexity scores and our patient-centered scores so that that kind of value gets recognized,” he said.
Chwastiak noted that, in her experience, value-based care for depression has been a primary driver for the uptake of the collaborative care model, beginning when primary care organizations sought strategies to integrate behavioral health services in order to become PCHMs. This has accelerated as many states have integrated care as part of statewide Medicaid transformation initiatives and health care systems looked for models that can improve outcomes. She remarked that one strategy she and her colleagues have used to engage primary care providers in integrated care is to describe the impact that behavioral health disorders have on medical outcomes and the potential for improved outcomes with effective treatment of behavioral health conditions. Diabetes care teams, for example, have found their patients can achieve better control of their disease when they receive treatment for depression or SUDs. Responding to questions about the roles of peers, harm reduction, and methadone, Wakeman stated that peers are invaluable and essential nonclinical members of the care team. The role of a recovery coach, for example, is intentionally separate from a clinical role. Being able to provide a shared lived experience and support in addressing barriers and engaging with a person’s goals is invaluable for making care person-directed and person-centered. She noted that insurance companies pay for one or two of her institution’s coaches because they believe the coaches provide value within the complex landscape that these patients must navigate.
Harm reduction, Wakeman emphasized, has to be a part of every aspect of care. She pointed out, however, that although harm reduction is a central consideration for other chronic conditions, it seems to be juxtaposed against treatment. “It is as if you have treatment on one hand and harm reduction on the other, and those two are not mutually exclusive,” said Wakeman. “In fact, good treatment and harm reduction are one and the same.” The goal, she added, is to respect the dignity, autonomy, and humanity of people who use drugs and let them guide treatment based on their goals, recognizing that many still want to use drugs. In that case, the goal of care should be to point the person to safer ways of using and reduce the negative consequences. She pointed out that harm reduction is not simply a bridge to treatment and the goal should not be to keep people alive until they get to treatment. Rather,
she said, it should be to help people live their best life in their best health in whatever way that means to them.
Wakeman noted that methadone is an incredibly effective treatment for OUD (NASEM, 2019), and yet it is incredibly regulated and only available through opioid treatment programs (OTPs). She believes that many more people would benefit from methadone treatment if it were offered in a setting they wanted to access, such as a primary care clinic. In other words, the OUD treatment system should be modernized to offer the right treatment for the right person in the setting that they choose. “Patients should be able to get care where they want to get care and where they feel comfortable and with a provider team that they feel comfortable with,” Wakeman explained. “They should not be told that they have to go to this separate, nonequal system, or to a certain site, and have a piece of their care carved away.”
Saitz added that it is possible to connect with OPTs in a way that coordinates and integrates care, but it takes a huge effort to do so. The better answer, which he said Wakeman was describing, was to integrate methadone care and treatment into primary care so that those clinicians can prescribe it in the primary care setting. This is how methadone is prescribed in most other countries, he noted.
Another participant question focused on ways that specialist behavioral health practices can reach out to and build partnerships with primary care practices. Chwastiak responded that in Washington State, as part of Medicaid transformation activities, behavioral health organizations have received a great deal of support and training around how to partner with a primary care organization to integrate care bidirectionally and been financially incentivized to engage in such partnerships. She stressed the importance of leadership buy-in and the promotion of integration. Next, deGruy added that his organization has established rotations in primary care for psychiatry residents and an addiction medicine fellowship in family medicine.
A webinar participant asked if stigma and discrimination explained the difficulty of integrating behavioral health care into primary care. Saitz replied that stigma is a huge reason, reflected in the federal agencies that deal with MHSUDs separately from the rest of health care. He sees the movement to integrate behavioral health into primary care as a way of pushing back on that institutional stigma and making it clear that behavioral health is a part of primary care delivery. Goldman added that the newest frontier is recognizing the fundamental nature of behavioral health in overall health and the need to address social determinants of health.
Panelists were also asked to speak to the concept of flattening hierarchies in the treatment team as it relates to improving patient care and employee satisfaction and whether it was possible to change the way care teams operate to achieve better goals. Wakeman replied that this is difficult because the
hierarchy is so deeply embedded in every aspect of care. At her institution, for example, all care teams have intentionally been interdisciplinary, interprofessional, and interdepartmental. She noted that having multiple perspectives and multiple voices about a patient is important to realizing the best care. Saitz said that his organization addresses issues related to hierarchy by designating individuals who may be lower on that hierarchy to lead the team.
The session ended with a final question about the ways in which the essential components of care and integrated care can help providers do a better job of supporting people in the community who are suffering from the devastation wrought by the COVID-19 pandemic. In reply, deGruy stated that acute problems arise all the time, and the care teams are equipped to deal with those as much as chronic disorders. “It is just a matter of constituting your team so that it is competent to deal with the range of problems that occur in ordinary primary care,” said deGruy.
IMPLEMENTATION OF ESSENTIAL COMPONENTS OF CARE IN PRIMARY CARE SETTINGS
W. Perry Dickinson, professor in the Department of Family Medicine and director of the Practice Innovation Program at the University of Colorado and moderator for the second session, opened by noting that primary care practices and clinicians have often struggled to achieve optimal implementation of the essential components of care as a result of several factors, such as the diversity and complexity of patient issues, the systemic disincentives for practices to identify and treat behavioral health issues, workforce and training deficiencies, and uneven or absent payment for behavioral health services. This session, he noted, would further explore models of care and lessons learned regarding integrating behavioral health into primary care settings, including key factors that support or impede implementation of the essential components of care, approaches to addressing the key barriers to implementation, implementation differences that may exist for various types of practices and different demographics, the varying levels of resources that serve different age groups, and how different approaches may be necessary for caring for children.
Implementing the Essential Components of Care in Primary Pediatric Practices
David Keller, professor and vice chair of clinical strategy and transformation in the Department of Pediatrics at the University of Colorado School of Medicine and Children’s Hospital Colorado, addressed how to provide integrated, comprehensive care for children in a pediatric primary care setting.
As every clinician who cares for children knows, mental health problems are common, though different, among children and youth, said Keller. Among mental health disorders, attention-deficit hyperactive disorder, behavior problems, anxiety, and depression are the most common diagnoses for children (CDC, 2020), and Keller noted that in his experience they are frequently a factor in pediatric primary care practices’ visits. Access to treatment varies by age, condition, and socioeconomic status.
Depression becomes a major problem as adolescence begins, but it is not uncommon at earlier ages (see Figure 3). Before adolescence, Keller has seen anxiety and other behavioral disorders frequently presenting to pediatric primary care. Keller noted that psychotropic medications prescribed for children by primary care physicians are often the first line of treatment.
As Keller noted, and as detailed in the 2004 National Research Council and IOM report Children’s Health, the Nation’s Wealth (NRC and IOM, 2004), the goal of caring for children is to maximize their upward trajectory and to improve their health to the point where they become the most successful adults they can be. Achieving that goal, said Keller, involves work across a range of areas, including biology, behavior, and the social and physical environments, all of which are handled through the kaleidoscope of services and policies that affect children throughout their lives. Keller highlighted the importance of understanding the 5Ds of how children differ from adults in behavioral health care (see Box 2).
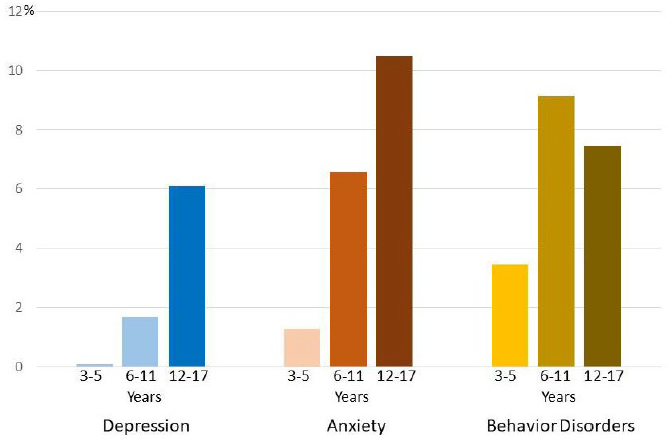
SOURCES: As presented by David Keller, July 29, 2020; CDC, 2020.
According to Keller, looking through the lens of the 5Ds affects how integrated care occurs for children. He offered the development of the maternal and child health system as an example. Such a system, Keller explained, has to consider the issue of mothers who are opioid dependent during pregnancy and may be delivering children who have, or are at risk for, neonatal abstinence syndrome. The Center for Medicare & Medicaid Innovation (CMMI) recently issued the Maternal Opioid Misuse model of care,15 which provides developmental support through early intervention to make sure an affected child develops properly. The model accounts for the fact that maternal opioid use often exists in the context of complex family and broader social systems, and it is critical to engage social services in the care team.
Keller pointed out that mother and child are often dealing with multiple diagnoses, not only OUD, and face socioeconomic factors that affect the way
___________________
15 For more information, see https://innovation.cms.gov/innovation-models/maternal-opioid-misuse-model (accessed August 13, 2020).
they receive care. Race is a factor, explained Keller, as is living in a rural environment, where it can be difficult to pull together the teams needed to address OUD. In addition, payment models are complex, and infant care is most often reimbursed on a fee-for-service basis and is completely disconnected from value-based care that the mother may be receiving. “We need to take these factors into consideration as we design systems going forward,” said Keller.
Treating depression in school-aged children is particularly challenging, noted Keller, at least in part because there are no effective screening tools for them. The Health Resources and Services Administration (HRSA) recently funded the Pediatric Mental Health Care Access Program16 that is now being piloted in 21 states and the District of Columbia. This program makes a child psychiatry consultant available to primary care clinicians who are trying to manage children with depression in their practices. This program is helping to create developmentally appropriate screening tools, therapies, and medications that can be used to help manage children with depression. In addition, much of the depression in children is trauma-related and comorbid with anxiety.
Although SBIRT has been modified to be appropriate for adolescents with SUDs, it is not widely used in practice. Confidentiality is tricky, said Keller, with regulations varying by state, as is dealing with stigma and the complicated relationship between adolescents and family. Navigating the need for family engagement to help manage SUDs with the developing adolescent need for independence is something that requires additional training and thought when creating teams capable of working well with adolescents. An SUD in adolescents is usually characterized more by bingeing than chronic use, which affects how screening tools are developed, and the substances used vary depending on where a child lives. Payment can also be a problem when the adolescent is not ready to disclose they have an SUD but the parents will receive the bill.
In closing, Keller reinforced the idea that children are not little adults and reiterated the importance of looking at whatever system is in place or being developed through the lens of the 5Ds. “We need to think about child development. We need to think about dependency. We need to think about the different epidemiology. We need to think about the way demographics factor into this, and we need to think about how the dollars will accrue,” said Keller. “Integration requires a broad team, and we also need to think how we make that team work across health systems, social services, education, and juvenile justice to really benefit children.”
___________________
16 For more information, see https://mchb.hrsa.gov/training/pgm-pmhca.asp (accessed August 25, 2020).
Successful Strategies for Implementing Alcohol SBIRT into Adult Primary Care
Stacy Sterling, research scientist at the Kaiser Permanente Northern California Division of Research, discussed the key factors involved in implementing alcohol SBIRT in her large, diverse organization. Kaiser’s approach, she noted, was informed by a study the organization conducted that examined different ways of delivering SBIRT (Mertens et al., 2015) and found it was particularly effective to have medical assistants screen for unhealthy alcohol use as part of their regular screening for blood pressure, tobacco use, and exercise when first settling a patient into the exam room. Physicians would then deliver a brief intervention and advice and refer to specialty treatment as needed. This model was introduced in July 2013 to serve all of Kaiser Permanente of Northern California’s adult primary care patients through approximately 2,500 primary care providers. Kaiser had conducted more than 12.4 million screenings and delivered almost 800,000 brief interventions as of May 2020 (Palzes et al., 2020; Sterling et al., 2020).
In describing some of the key factors for this model’s successful implementation, Sterling noted that leadership support has been critical. Both the executive medical director and the head of adult primary care recorded videos for physician trainings, emphasizing the importance of the work and encouraging primary care providers to participate. This messaging was important because alcohol and drug use disorders are rarely top priorities for busy providers. “The message also carried more weight coming from fellow physicians rather than researchers,” she said.
Sterling explained that SBIRT implementation involved stakeholders from primary care, addiction medicine, psychiatry, and research throughout the entire process. An implementation facilitator, particularly at the beginning of the initiative, provided the clinical teams with coaching and technical assistance. Every medical center had a team comprising a primary care provider and a chemical dependency clinician counterpart to serve as the resident SBIRT experts, and clinicians at each medical center received what she called a “matchmaking e-mail” to introduce staff to the members of the local SBIRT team and encourage collaboration. Teams were brought together regularly by conference call to share successes and troubleshoot failures.
She described how SBIRT tools were embedded in the electronic health record (EHR), including reminders for the medical assistant to complete NIAAA’s single-item screening tool for each patient, tailored to patient age and gender. This tool, Sterling explained, asks how many times in the past 3 months an individual has had five or more drinks containing alcohol in 1 day for men or four or more drinks in 1 day for women. Two follow-up questions query the patient about how often they drink during 1 week and how many
drinks they have in 1 day when they have an alcoholic beverage. The EHR calculates average weekly consumption from these responses, which can trigger a best practice alert to the provider that presents the screening results and provides decision support and further assessment tools to use if they believe their patients might be at risk for an alcohol use disorder.
Sterling further explained that using a train-the-trainer model, based on work by Saitz and colleague Dan Alford, the alcohol champions at each medical center trained their fellow primary care physicians on the brief intervention and referral process, and nurse managers trained medical assistants on the screening process (Alford et al., 2008). The training emphasized normalizing discussions about alcohol use as part of overall health and well-being as a means of reducing the stigma of having these conversations. Clinicians also received regular feedback on screening and intervention performance.
Sterling described how provider trainings included concrete scripts that they could use or adapt to discuss alcohol use and emphasize the tie between drinking and any health problems patients present. This approach, she noted, shifts the emphasis from alcohol use per se in isolation to how it affects patients’ overall health and well-being. Sterling said that such training for medical assistants acknowledges how conversations about alcohol use can be awkward and provides them with specific ways of dealing with patients getting angry or refusing to answer. Medical assistants undergo extensive practice sessions in which they rehearse asking the screening questions correctly. “We know from the literature that how questions are asked can really affect people’s willingness to disclose alcohol use and the accuracy and validity of their answers,” Sterling explained. In addition, every primary care exam room displayed posters that normalize asking patients about drinking and illustrate standard drink sizes17 as a way to get everyone on the same page about consumption amounts.
In closing, Sterling noted that monthly performance feedback reports generated for providers and medical assistants are sent to managers and physician leaders to create healthy competition and spur performance improvements. When these reports are presented unblinded in meetings, alcohol champions can use them to talk to low- and high-performing care team members about their work.
___________________
17 According to the National Institute on Alcohol Abuse and Alcoholism, a standard drink is any drink that contains about 14 grams of pure alcohol (about 0.6 fluid ounces or 1.2 tablespoons). To view standard equivalents for different types of beverages, see https://pubs.niaaa.nih.gov/publications/practitioner/PocketGuide/pocket_guide2.htm (accessed August 28, 2020).
Integrating Primary Care and Behavioral Health
Speaking from the perspective of a clinical provider working in a community health center setting, Suzanne Snyder, director of behavioral health at ACCESS Community Health Network,18 described how her Chicago-area federally qualified health center (FQHC) has been working toward integrating behavioral health into primary care for approximately 20 years. This effort, she added, started with behavioral health clinicians joining her organization’s Ryan White HIV program wraparound care teams. This historical fact is important, she said, because it means that collaborative care is in her organization’s DNA.
Patient engagement, population health management, and accounting for social determinants of health are key to the integrated model developed by ACCESS (Hoge et al., 2014). Regarding integrated behavioral health, ACCESS’s services include universal screening for depression, SBIRT, care coordination, integrated medication-assisted treatment (MAT), and psychiatry and therapy services.
Snyder noted that behavioral health in primary care promotes Triple Aim goals, often by addressing previously unidentified and unmet patient needs. However, it is the Triple Aim’s third goal—improving the patient’s experience—that most informs her advocacy for integration. “There is a long history of stigma, lack of health parity, and siloing in mental health and substance use care,” she observed, and “I believe that integrated behavioral health care at its best provides patients an alternative experience, a health care experience that assures the patient that every door is the right door to begin to holistically address their health care needs.” She acknowledged that the saying “every door is the right door” is aspirational, but striving to make it a reality is the guiding principle for integration work at ACCESS. Snyder added that it is critical for primary care providers to address patients’ mental health and substance use concerns, which can include breaking down environmental barriers and attending to social determinants that affect care. She stressed that it is also important to help patients move toward positive health behavior changes.
Over the course of her integration work, it became clear that trauma-informed, patient-centered collaborative care is a critical element of integrated care. “We know and have learned through mistakes that this is foundational,” said Snyder. She explained that several years ago, ACCESS launched an all-systems rollout of universal depression screening without sufficient input or training across the organization or preparing patients for the screening. Learning from those mistakes, ACCESS began universal SBIRT screening with a more trauma-informed approach. To prepare patients, for example, ACCESS launched an anti-stigma campaign called We Ask Because We Care. This mes-
___________________
18 For more information, see https://www.achn.net (accessed August 25, 2020).
saging is conveyed consistently in exam rooms and through written handouts to normalize screening for both patients and care teams. For providers and care coordinators, her team provided training in motivational interviewing and patient-centered educational tools. She explained that when ACCESS started SBIRT, it carefully defined roles and workflows, and it launched each health center individually, allowing her team to make weekly visits to a clinic and make adjustments along the way. “No surprise, the provider response was much more positive,” she said of the revised launch.
Snyder said that patient-centered collaborative principles and meeting patients where they are guided the organization as it grew its MAT services. Today, MAT is available at 14 of ACCESS’s health centers, with plans to expand this service throughout its system so that patients can receive care in their own communities and from familiar care teams. She explained that when preparing a clinic to start delivering MAT services, she and her colleagues train the entire health center team on what “meeting patients where they are” entails, focusing on harm reduction and overdose prevention, addressing implicit biases, and providing access to treatment at the point of care and at a time when patients are ready to receive treatment.
Snyder remarked that having established quality metrics to track progress is important when adopting evidence-based practice tools. ACCESS uses the PHQ-9 for managing depression in primary care (Moore et al., 2012) and developed documentation and workflows that are led by behavioral health in collaboration with chronic disease and maternal and child health clinics. ACCESS has also learned to leverage its EHR to transparently tie treatments and responses to quality metrics.
Snyder shared that integration is ever evolving and clinical needs change, sometimes quickly, which is why the organization has continued to make adjustments to the way it operates. For example, in response to the COVID-19 pandemic, some of ACCESS’s providers have asked to change the adult depression screening workflow to make the PHQ-4 (which addresses both depression and anxiety), as well as the standard PHQ-2, available as an option for initial screening, because more patients are presenting with symptoms of anxiety. “Because of the shared responsibility for depression management across disciplines, we were able to make this change easily and see it as an organization[al] first step to addressing the mental health needs that the COVID-19 pandemic has laid bare and exacerbated,” said Snyder.
In closing, Snyder emphasized that while it is critically important to understand the components of integrated care, it is also important to accept that there will be persistent challenges that should be anticipated and addressed whenever taking new steps in integration. Snyder pointed out that these challenges include
- existing provider and resource shortages along the continuum;
- sharing patient health information, particularly regarding SUD care;
- developing reimbursement systems that more fully support integration, care coordination, and community supports for patients;
- bridging differences between care models and clinical paradigms;
- requiring time to implement a change and the timing to do it; and
- managing the effects on clinicians of caring for patients with new and different vicarious trauma loads.
Breaking Down Silos to Improve Integrated Care
The webinar’s final speaker, Laura K. Murray, senior scientist in the Department of Mental Health at the Johns Hopkins Bloomberg School of Public Health, discussed the Common Elements Treatment Approach (CETA) as a means of breaking down silos to improve integrated care (see Figure 4). She opened her remarks by reminding everyone that all humans have comorbidity in some form. As a result, comorbidity is the norm for patients who present with mental, emotional, or behavioral health problems. “As clinicians, we rarely ever see or hear of an individual with just depression or just trauma or just substance use,” said Murray.
Despite this, the current approach to providing services is siloed, Murray explained. Even in the mental health field itself, it is common to teach provid-

SOURCES: As presented by Laura Murray, July 29, 2020; provided by CETA, www.cetaglobal.org (accessed August 28, 2020).
ers different types of evidence-based therapies for one disorder rather than the range of disorders. Murray said that this means that mental and behavioral health specialists need to train an estimated 8–10 different evidence-based treatments to serve the comorbidities in a population. In addition, by focusing on one disorder and not treating the whole patient, clinicians will miss making referrals and patients may have to engage in long, ongoing, sequential care for each individual problem. “This is challenging at best, often impossible, and most certainly costly and unsustainable,” said Murray.
CETA, a modular, multi-problem program, is one solution for breaking down silos in the field of behavioral, emotional, and mental health. It addresses depression, violence, trauma, aggression, risky behaviors, and other aspects of behavioral health as a whole and is customized for each individual. Murray emphasized that CETA is not a new treatment, just a different approach to providing evidence-based treatments. As she explained it, she and her colleagues teach providers and counselors to combine elements in different ways to address possible comorbidities. These elements include therapeutic approaches, such as cognitive processing therapy, cognitive behavioral therapy, parenting skills, problem management plus, and trauma-focused cognitive behavioral therapy. Given CETA’s design, it also has the flexibility to move into stepped care models, where someone might need only one or two elements.
Several studies have shown that the CETA approach outperforms usual treatments (Bolton et al., 2014; Kane et al., 2020; Murray et al., 2014, 2018, 2020). “So [it is] not much of a surprise [that] when we treat the whole individual and we address all of their problems, we can usually be more effective,” said Murray. In one study, conducted in Zambia, she and her colleagues looked at interpersonal violence and alcohol use (Murray et al., 2020). By combining therapies for mental health issues with those aimed at reducing substance use, this approach was able to maintain reductions in alcohol use and interpersonal violence at 24 months after treatment. She noted that in low-resource countries, her team is training lay providers to deliver CETA therapies.
Murray noted that many organizations have difficulties breaking down silos. “We still have a deeply embedded siloed care approach in our care settings, and in funding, and until we de-silo this, we are going to have many [ongoing] challenges,” she said. “We have to try to move from treating just one thing to looking to the person as a whole.”
In closing, she pointed out the need to change licensing and reimbursement requirements so that both training and implementing evidence-based care is mandated. Many trainees, she said, leave their programs without being trained in any evidence-based treatments, and yet they are still licensed. What that means, she said, is that “if someone is on an integrated team but they have only been trained to treat depression or substance use, that is a huge loss.”
Panel Reactions and Discussion
Dickinson asked the panelists to talk about the types of team members that are necessary to implement the integrated services they discussed in their presentations and the type of training behavioral health professionals need to adapt their roles in primary care practices. Snyder responded that behavioral health clinicians, primary care providers, and, most importantly, care coordinators are key to her organization’s efforts. Care coordinators, she noted, are mostly registered nurses, with some licensed clinical professional counselors and licensed clinical social workers. Other important team members are medical assistants and community health specialists with lived experiences who can do some of the educating and reaching out to patients, as well as senior leadership and quality control people who can handle the data analytics needed for quality improvement. Regarding training for behavioral health consultants, Snyder thought it important that they have an interest in and dedication to learning about chronic disease processes so that they can understand how to engage other members of the care team and patients and families. She also emphasized the importance of training everyone on the team in trauma-informed care.
Keller remarked that while it is great to have an extensive team, he did not want to leave the impression that integrated care cannot be successful with a much smaller team. He recounted working in environments where his team included one part-time licensed clinical social worker, some medical assistants, and a few nurses and nurse practitioners. “I do not think our medical assistants, for example, thought of themselves as behavioral health providers,” said Keller, “but by the time we were through with them, they were providing the essential elements of behavioral health care.” What this speaks to, he added, is the need to incorporate this type of training into programs more broadly. Toward that end, his institution has developed a 1-year fellowship to teach newly trained Ph.D. psychologists in integrated behavioral health. This enables the fellows to work in a primary care setting and learn how to work with children to prevent minor behavioral health problems from becoming major problems. Keller pointed out that he would like to see preventive mental health care become part of the child health spectrum of care. Along those lines, Sterling remarked that her institution has had success including clinical health educators on their care teams to work on preventive mental health care.
Dickinson asked Murray if CETA, which her team has deployed predominantly in low- and middle-income countries, would work in the United States. Murray replied that she and her colleagues have introduced CETA in Washington State and underserved communities in the Chicago area. She also noted that other transdiagnostic models are being studied in this country. The key is to train the providers to figure out which elements of an approach they need for their practices and then ensure they are using evidence-based care and measurement-based care.
Sterling, whose work has focused on supporting large practices in an integrated health system, said that it is important to make things as easy as possible for the clinicians, and she suggested embedding tools in the EHR and providing specific scripts for providers and medical assistants. The goal, Sterling explained, is to ease the fear that many clinicians have when they start engaging in integrated care and help them realize that they are not going to have to spend a great deal of time asking every patient about their behavioral health needs and engaging every patient in in-depth treatment.
Snyder added that one of the turning points with SBIRT for her organization was to ensure that their community health specialists, who do the brief interventions, received feedback on their performance and training on how to report their findings so that the clinician who follows them will know exactly what the patient needs and wants. This, in turn, leads to effective communication throughout the team using the EHR, which helps with adoption. The other tactic her organization uses is pilot studies, either based geographically or with a small segment of a population, allowing Snyder and her team to learn what works and does not work without overwhelming clinical staff. Dickinson noted that in his experience, there can be significant technological barriers related to the EHR when working with primary care physicians from one system and behavioral health professions outside of that system, who often have a different type of recordkeeping system.
Dickinson asked Keller for some key lessons he has learned as to how to best support practices as they implement integrated care. The most important one, replied Keller, is having facilitators who meet practices where they are and listen nonjudgmentally to where the practice is and where it wants to go. It is also beneficial if the facilitator can help the practice incorporate the voice of the patient into its work. He noted that many providers do not want to tackle that, but once they hear from patients that they want to be involved in their care and have a voice, they work to incorporate that approach into their practices.
Keller reminded everyone of the need to be cognizant of the multiple demands currently being placed on primary care staff, particularly given the COVID-19 pandemic. “We are all suffering from change fatigue, so you have to have some skill at working with your practices on managing the change fatigue that is going to happen as you move through these different processes,” said Keller.
Sterling remarked that in her organization’s SBIRT effort, medical assistants were the linchpin in terms of screening, and it was important to make sure they were recognized and respected for their efforts and the key role they play. The facilitators also tried to tap into the medical assistants’ inherent desire to help people improve their health and well-being and to represent their patients’ needs and wants. Dickinson noted that he has found that in
practices that are resistant to change, a little encouragement from leadership and the medical assistants, who are closer to the patient perspective, can move a practice forward.
Murray, speaking to the problem of the hierarchy in hospitals and clinics, said that they are among the worst organizations in terms of creating an environment of emotional safety given the divide that exists based on, as she put it, “how many letters you have after your name.” While the business world is moving away from that type of hierarchy, that movement has not yet reached health care, said Murray. In her experience, one effect of that is that some team members become reluctant to speak up and voice concerns about how the system is treating patients.
Dickinson then asked the panelists to provide any recommendations for policy makers who are looking to encourage implementing integrated models of care. Murray said that she wants to see training changed to break down silos. She noted that when people go through school, they are trained to specialize in silos, and, as a result, they lose the ability to look at the patient as a whole and think about how diabetes, for example, is affecting a person’s behavior and mental health. “That is a big shift we need to make in our education programs and then in our supervision,” she said, adding that licensing requirements should also be changed to reflect the need for a broader educational focus.
One place where silos are particularly entrenched is the divide between pediatrics and adult medicine. In the real world, Murray said, many parents want to be seen by the same clinicians as their children and do not want to be referred out of the practice. She acknowledged that this change will be difficult, but it needs to start happening and both funders and licensing boards need to get behind these efforts of integration. Keller noted that there have been interesting and successful pilot programs designed to combine adult and child services. The challenge is to scale these pilots to a statewide or national level. Keller added that one of the great mistakes the federal government made was to break up the U.S. Department of Health, Education, and Welfare because for children, health, education, and welfare are intimately connected.
Snyder remarked that she often has patients apologizing for asking for care related to issues of mental health, substance use, and social determinants. “When that stops happening,” she said, “then we know we are getting somewhere as providers and patients.” She also noted that payment policies need to change, given the importance of where the money goes.
Sterling commented that she has the advantage of working in a capitated system,19 which encourages integration to an extent. Nonetheless, she sees
___________________
19 A capitated system is defined as a health care plan that pays a flat fee for each enrolled person, whether or not that person seeks care.
attitudinal barriers and disciplinary foci as a stronger force at keeping silos in place. “Even though we are an integrated system and, theoretically, we have carved in addiction medicine and psychiatry, we still have those barriers among the different clinicians,” explained Sterling.
Question and Answer Session with Webinar Participants
A webinar participant asked Snyder to speak more about implementing SBIRT in an FQHC setting and particularly about the selection process for those designated to deliver the intervention itself. Snyder said that this has been a learning process, and when she and her team first launched their universal depression screening, they found they still had a disturbingly low rate of depression. The team is now adding community health specialists and medical assistants who can conduct the screening, at which point the primary care provider can decide to handle the brief intervention themselves or have the community health specialists or medical assistants do it, depending on the workflow. Snyder explained that her team is now piloting this approach at six sites, and early results are encouraging. In addition, the team is working on having the community health specialists who do SBIRT cross-train with the community health specialists who support MAT as a means of broadening the training these specialists receive. Snyder added that her group currently has an external trainer working with the community health specialists on motivational interviewing.
Dickinson noted that he has been involved in two different waves of SBIRT implementation in Colorado. In the first wave, primary care practices would embrace this model, but the barrier was knowing whom to refer patients to for MAT. The second wave includes trying to support practices in learning how to do MAT themselves to the degree possible. This approach is just getting started, he said, but he believes it will be much more successful.
Another participant asked Keller if there are elements of care that can be helpful for getting a child with mental health issues into treatment when the family is resistant. Keller replied that this is where having an integrated primary care practice is helpful because providers can talk with families, continue the conversation, and build the trust needed to convince parents of their child’s need for treatment. “The beauty of primary care,” he added, is that “its fundamental value is relationship, and everything after that is built off of that foundation.”
Sterling noted that her organization completed a successful adolescent SBIRT trial that included alcohol and drug use, depression, anxiety, and stress. They found that having a warm handoff and introduction to a friendly and welcoming behavioral health clinician in the pediatric primary care clinic worked well at easing the trepidation teens often feel about talking to a coun-
selor. This approach was much more effective, Sterling pointed out, in getting adolescents to initiate treatment. Keller added that a benefit of working in an integrated practice is that families have often met the psychologists and social workers in non-crisis situations. In fact, his organization has a program where a psychologist or social worker will stop by one of the well visits and offer families some behavioral support without telling them their child has a problem. Sterling stressed that every well-child or well-teen visit should include an emotional as well as physical checkup, which would help normalize behavioral health care as an important part of health care. Dickinson agreed that this would help people realize that the behavioral health care professional is just as much a part of the team as other clinicians.
Snyder said that her organization often sends its new behavioral health care professionals to its obstetrics clinics for an afternoon to accompany the provider and talk about perinatal depression and perinatal mood disorder. Often, those conversations end up identifying someone the patient knows who is having trouble after a pregnancy. Her team encourages the person to get their neighbor or friend to come into the clinic.
Keller said that his institution trains all of its behavioral health staff as HealthySteps20 providers. HealthySteps is an evidence-based program for preventive behavioral health care for children. He noted that some state Medicaid agencies will pay for this program. Keller also answered a question about how the COVID-19 pandemic was affecting how behavioral health integration was working in his system. The biggest effect, he responded, has been developing and rapidly implementing telehealth, given its ability to enable multiple team members to consult with a patient without violating social distancing requirements. He noted that another benefit of telehealth is that children with autism spectrum disorders, for example, prefer virtual care.
Sterling noted that at the time of the webinar, Kaiser was in the middle of a surge of infections, and staff had already figured out a seamless way to do handoffs via videoconferencing. She added that video technology provides the opportunity to bring in interpreters virtually when needed. In addition, more people are putting their evidence-based continuing education trainings online, making them more accessible to more professionals. Murray’s hope is that this trend continues, because it can ensure that all behavioral health professionals receive training in evidence-based care, which is not the case today.
A webinar participant asked the speakers about financing strategies that help break down silos. Keller responded that he was fortunate to help develop the Children’s Behavioral Health Initiative in Massachusetts. This program, started 10 years ago, brought together funding from a variety of sources through the state Medicaid system that was used to provide a statewide system
___________________
20 For more information, see https://www.healthysteps.org (accessed August 25, 2020).
of wraparound services. This initiative, said Keller, was able to demonstrate that it could decrease the number of children in crisis who were ending up in the ED. Colorado, he lamented, has not been as successful at developing this type of system, to which Dickinson commented that working in Colorado is difficult because there are so many different payers and no single, large health plan, making it complicated to navigate across Medicare, Medicaid, and multiple payers. Progress occurs in one area, but unless all payers are onboard, progress stops. Given that this happens all over the country, it will take the country moving to an all-payer system to make true progress on the payment front.
The panel was asked to speak to the opportunities for integrating behavioral health and medical care in the corrections settings. Dickinson is involved in a fledgling project with Colorado prisons to work on screening and treatment for mental and behavioral health problems and SUDs. Prisons, he said, are hungry for help in this area, but, unfortunately, the pandemic’s effect on the state budget is temporarily cutting off funding for what was going to be a multiyear program.
Snyder said that one of her team’s successes has been collaborating with other agencies that work in the Cook County jail’s discharge area. They are able to schedule appointments for people coming out of the mental health hospital at the jail, which is one of the biggest mental health providers in Illinois. As people are discharged, FQHCs in the region have a system where they are scheduled for a next-day appointment at these centers. This is particularly critical, she said, for patients going into substance use programs. ACCESS is also working with safety departments in the Chicago suburbs on court diversion for MAT and partnering with social agencies to fund housing and medical care for people in MAT or with chronic mental illness.
Closing Remarks of the Second Webinar
Roach said that while a virtual event cannot replace a face-to-face experience, she and her fellow committee members still felt a strong sense of connection to everyone who participated. She said that in light of the mounting evidence of rapidly escalating rates of anxiety, depression, and substance use, conversations such as these are more critically important than ever, as they are shaping the values, policies, and ensuing actions that will determine how we emerge from the current converging public health crises. “Your partnership and willingness to engage in transformative dialogue reassures us that one day in the foreseeable future, the design of U.S. health care systems will consistently reflect the reality that optimal physical health is only possible where there is optimal mental health and vice versa,” concluded Roach.
IMPROVING THE WORKFORCE TO SUPPORT PROVIDING ESSENTIAL COMPONENTS OF CARE
In his remarks to open the third webinar, Alexander Ross, senior behavioral health advisor in HRSA’s Office of Planning, Evaluation, and Analysis, explained that one of the key elements critical to integrating mental health and substance use treatment into primary care is a well-trained workforce. Ross pointed out that the first session of this webinar would explore the role of workforce training in meeting expectations around essential components of care for people with MHSUDs in primary care settings. He noted that the speakers in the webinar’s first session would illustrate how the field can effectively train clinicians to provide the essential elements of care discussed in the preceding webinars.
Developing the Workforce to Support Health Centers
Colleen LaBelle, program director of the State Technical Assistance Treatment Expansion Office-Based Opioid Treatment with Buprenorphine21 and a member of the Boston University School of Medicine’s Clinical Addiction Research and Education Unit, began her remarks by noting that she and her colleagues at the Boston Medical Center launched a pilot program in 2003 in which nurse care managers play the lead role in delivering buprenorphine in primary care practices to individuals with SUDs. They soon expanded the pilot to include 14 community health centers across Massachusetts, and, as a result of its success, in 2007 the state Department of Public Health funded her team to provide Office-Based Addiction Treatment (OBAT) training and technical assistance to the state’s primary care providers (Alford et al., 2011).
LaBelle pointed out that by 2015 the state’s OBAT program was treating more than 15,000 individuals for SUDs, and by 2020 OBAT training and technical assistance efforts were reaching more than 2,500 members of the addiction treatment workforce annually. Today, more than 40 FQHCs in Massachusetts use this model to deliver multidisciplinary wraparound care for complex patient needs relating to SUDs. “Our health centers have been the engine to treat substance use across Massachusetts,” said LaBelle.
Initially, LaBelle explained, FQHCs were reimbursed for the nurse’s salary, but the state has transitioned to unit-based reimbursement. She noted that as FQHCs integrated behavioral health into their models of care, the OBAT model has fit well into the context of treating patients with complex needs and enabling them to access services in real time. Nurses, the primary focus for training and technical support, are paired with prescribers to both train and support them in their SUD care. This approach has enabled her team to build a statewide
___________________
21 For more information, see https://www.bmcobat.org (accessed September 11, 2020).
network, expanding access to providers and facilities and increasing providers’ comfort level in treating people with SUDs. LaBelle and her colleagues have also worked to involve pharmacists and professionals from other disciplines in caring for individuals with all types of SUD, not just opioid addiction.
LaBelle noted that one key to maintaining the workforce at FQHCs, which have a high rate of personnel turnover, has been to train a facility’s entire staff using webinar series and online courses that award continuing education credits. This technology-based approach has enabled the program to rapidly integrate training specific to the COVID-19 pandemic into its offerings. In fact, said LaBelle, there has been an exponential increase in training and technical support provided since the pandemic began. Between March 1 and August 20, 2020, she and her colleagues have conducted more than 100 live online trainings and at least 100 online drop-in sessions for more than 3,000 participants. Her team has trained more than 12,000 registered nurses, physicians, nurse practitioners, social workers, physician assistants, and others between January 1, 2019, and July 31, 2020. “More and more providers seem to be getting engaged using technology, which is exciting,” said LaBelle.
LaBelle described how trainings in the COVID-19 era now include how to care for patients remotely during the pandemic, what type of tools providers need to do so, and how to engage recovery coaches and support their work. “We developed [virtual] drop-in sites where recovery coaches get together twice a week, which has been invaluable to that workforce,” said LaBelle. The OBAT training and technical support team can assist recovery coaches in their work via these sites.
LaBelle would like to see regional training and technical assistance centers of excellence established for community health centers and their staff. Doing so, she predicted, would extend the reach of this successful approach. “We could provide evidence-based resources and treatments, we could support the nurses and multidisciplinary workforce, and [we could] have online repositories of resources, apps, and algorithms,” said LaBelle. All of these resources would be directed at treating the whole person, she said in closing.
The Role of Peer-Support Services in Delivering Collaborative Care to Treat MHSUDs
Phyllis Foxworth, vice president of advocacy for the Depression and Bipolar Support Alliance22 (DBSA), noted in her introduction that her organization was founded 35 years ago with the idea that peers supporting peers could be a key component of an individual’s health and wellness plan. The resulting movement, as she called it, has led to the integration of peer-support services
___________________
22 For more information, see https://www.dbsalliance.org (accessed September 11, 2020).
delivered by a certified peer-support specialist as an adjunct to clinical care teams. “This protocol has been proven to improve health outcomes for people living with behavioral health conditions,” said Foxworth.
Foxworth explained that a peer support worker is someone with the lived experience of recovery from a mental health condition, an SUD, or both. Peer support workers, who are credentialed by their experiences in their own recovery journey, support others experiencing similar challenges by providing nonclinical, strength-based support. Foxworth noted that peer support workers can be referred to as “peer specialists,” “peer recovery coaches,” “peer advocates,” and “peer recovery support specialists,” depending on the setting in which they practice. Those settings include peer-run organizations, recovery community centers, recovery residences, drug courts, hospital EDs, and behavioral health and primary care. Regardless of their title or place of work, peer support workers inspire hope that people can and do recover. “They walk with people on their recovery journeys, they dispel myths about what it means to have a mental health or substance use disorder, they provide self-education, and they link people to tools and resources,” said Foxworth. Peer support, she added, offers a level of acceptance, understanding, and validation not found in many other professional relationships.
Foxworth presented an example of how her organization is using peer support services to improve health outcomes in seniors. The demonstration project she discussed, a collaborative care model that integrates primary care and mental health care, was conducted in partnership with Facey Medical Group in Mission Hills, California, and the AIMS Center at the University of Washington. The goal of this ongoing project is to improve overall health by treating both physical and mental health using one-on-one, community-based peer support. Success, said Foxworth, will be measured by the individual demonstrating continued engagement with the primary care team, improving PHQ-9 scores, and identifying a health and wellness goal.
Foxworth explained that the initiative begins with the primary care provider, who screens all Medicare Advantage patients using the PHQ-9. Foxworth said that a score of 10 or higher triggers a protocol to contact behavioral health services staff located in the same building. A therapist responds immediately, coming to the exam room to perform an initial assessment and introducing the DBSA Senior Strength program. If the person agrees to enroll, within the next 48 hours, the care coordinator introduces them to the peer specialist they will work with and arranges a location and time convenient for them to have their visits. “This is not at the clinic; it is at the location convenient to the person they’re working with,” explained Foxworth.
Importantly, she said, these visits are not wellness check-ins or companion calls. Rather, each visit begins with the peer specialist asking the individual to do a self-assessment using the PHQ-9. The results provide a place for starting
the conversation for that visit. The peer specialist then uses decisional balancing worksheets and motivational interviewing techniques to assist the person in identifying their own wellness goals and support them in working toward those goals. The peer specialists, added Foxworth, have monthly meetings with clinical staff to discuss their cases, and patients continue to see their primary care provider.
Explaining that the COVID-19 pandemic has forced adaptations to the program, Foxworth noted that referrals now come from behavioral health professionals rather than from the initial visit with a primary care provider, and the peer support specialist visits with the individual by phone or video. Foxworth commented that establishing a clearly defined role among all the partners has been a major factor in the program’s success. DBSA recruits and supervises the peer specialist and develops and implements the peer support services program. DBSA also tracks the results in the AIMS Center’s Care Management Tracking System. Facey Medical Center has been responsible for training the primary care physicians on how to use the program. The AIMS Center conducts bimonthly coaching calls in addition to providing training on and access to its clinical trials management system. Unpublished preliminary results from 2 years into the 3-year demonstration show that the peers who graduated from the program have reduced their PHQ-9 scores by 57 percent.
Concluding her remarks, Foxworth noted the importance of using individuals who are certified paraprofessionals when implementing a peer support program as an adjunct to the clinical care team. She said that 48 states and the VA have established credentialing requirements for peer support specialists. Most states require completing and passing a peer specialist or recovery coach course and completing an apprenticeship of as many as 2,000 hours (GAO, 2018). All states require continuing education to maintain credentialing. “At DBSA, we believe it takes skill, talent, and dedication to provide peer support services, and when delivered by credentialed paraprofessionals, the potential for positive outcomes is great,” concluded Foxworth.
Behavioral Health Workforce to Optimize Medication Outcomes
Carla Cobb, founder of Capita Consulting, opened her remarks by noting that people with MHSUDs often have co-occuring medical conditions that contribute to them dying years younger than their peers, often as a result of nonoptimal treatment (Walker et al., 2015). This outcome is compounded by a national shortage of health care providers, she added. Cobb pointed out that data from the Kaiser Family Foundation show that the United States has approximately 27 percent of the psychiatrists needed to meet the demand (KFF, 2019), with even larger shortages in some regions (see Figure 5). The United States will have a shortage of approximately 11,000 addiction counselors by 2030 (HRSA, 2019).
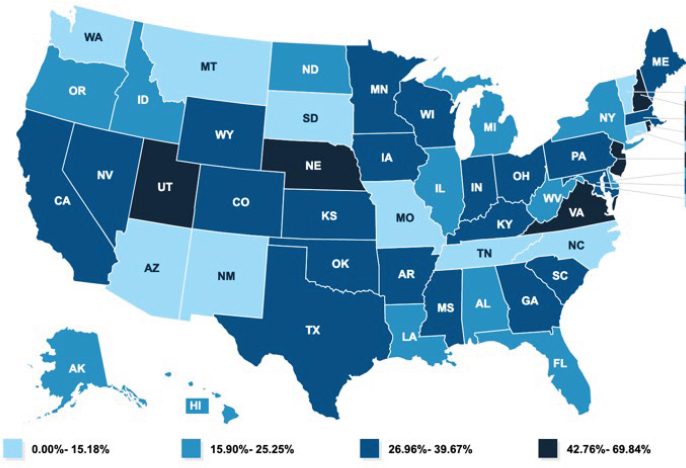
SOURCES: As presented by Carla Cobb, August 26, 2020; KFF, 2019.
In 2017, the National Council for Behavioral Health and the Medical Director Institute proposed a number of solutions to this shortage (NCBH, 2017), including a call to make efficient use of other types of underused health care professionals with specialty training in mental health, such as board-certified psychiatric pharmacists. Cobb explained that these pharmacists have completed 1 or 2 years of residency training in which they learned an evidence-based process of care known as “comprehensive medication management” (CMM in Primary Care Research Team, 2018). This process focuses on identifying, treating, and resolving drug therapy problems, most often for people with complex medication regimens or those who are not meeting therapeutic goals. Cobb explained that psychiatric and other types of clinical pharmacists are working on teams at FQHCs, in the VA system, and with Project ECHO,23 providing direct patient care and education to interprofessional teams. Some Project ECHO teams, for example, include a psychiatric pharmacist who works with the team to help teach and support primary care providers caring for people with MHSUDs, often in rural areas.
Cobb discussed how this care model fits with the key elements of integrated behavioral health that McGinty and Daumit described in the first
___________________
23 Project ECHO is a collaborative model of medical education and care management that empowers clinicians everywhere to provide better care to more people, right where they live. For more information, see https://echo.unm.edu/about-echo (accessed September 3, 2020).
webinar. “When you look at team-based care in the primary care setting, pharmacists can serve as an important part of that team,” said Cobb. “They participate in treatment team meetings, they review patient registries, and they contribute to case reviews with their teams.” For example, if the treatment team decides to start someone on buprenorphine for OUD, the pharmacist may help by providing patient education, ensuring that the patient can actually get the medication, troubleshooting side effects, and monitoring for medication adherence. A patient might have failed antidepressant treatment, in which case the psychiatric pharmacist would try to identify the reasons for failure, such as side effects, drug interactions, and patient preference, while also looking at treatment guidelines to help guide next steps. “These are people who in the past may have been referred out for care to a psychiatrist, but now we realize that it is better to provide that care right there in their own doctor’s office with the help of the integrated behavioral health team,” explained Cobb. Being part of a multidisciplinary team is a key component of this approach, she added.
As another example, Cobb noted that FQHC clients discharged from an inpatient stay for an alcohol use disorder have a joint appointment with the behavioral health provider and a psychiatric pharmacist before meeting with their primary care physician. Together, the behavioral health provider and psychiatric pharmacist review the individual’s psychosocial and medication history and examine different options for medications to treat alcohol use disorder if that is something the patient might desire. The team then makes recommendations for the primary care physician to consider when seeing the individual.
In closing, Cobb commented that the United States needs to improve access to care and outcomes for people with MHSUDs. “We need to make sure that every patient has access to appropriate, safe, and effective medications to improve their chances of success and to decrease mortality rates,” said Cobb. She cautioned, though, against simply creating a team and hoping that the members figure out how to work together. “To make the team as efficient as possible, the team has to sit down and talk through who is the best team member to do each part of the work in taking care of patients and to establish workflows,” said Cobb. “I believe that we can help address the workforce shortage by providing a team-based approach to care and making sure that we use every member of the team to the top of their training.”
Digital Enhancement of the Primary Care Workforce
Steven Ondersma, professor in the Division of Public Health at Michigan State University, focused his remarks on ways in which technology can play an important role in addressing workforce issues in primary care. He first noted that any discussion of integrating treatment for alcohol use, opioid use, or
depression into primary care has to first take stock of the treatment gap (see Figure 6). Data from the Substance Abuse and Mental Health Services Administration show that the majority of people do not receive care for MHSUDs. Moreover, the majority of those who do not receive care—particularly for SUDs—are not seeking care and do not believe they need it (McCance-Katz, 2018). “This underlines the importance of addressing these issues in primary care,” said Ondersma, “but it also means that we cannot just think in terms of providing services. We have to think in terms of proactively reaching out and identifying people who are at risk, whether or not they present themselves as somebody at risk, and secondly about motivating them to make changes and to take advantage of available services.”
One approach Ondersma shared is to have primary care clinicians provide these services using an approach known as SBI (Screening and Brief Intervention) or SBIRT. While there are successful models of screening individuals and offering brief interventions in primary care, he explained, the literature is full of examples showing that doing so is more difficult than anticipated. Time, for example, is an issue given how many other responsibilities are being added to the workload of primary care providers. A study from 2003 showed that performing all the U.S. Preventive Services Task Force A- and B-rated24 activities for each patient would take an average primary care provider an additional 4.4 hours per working day (Yarnall et al., 2003).
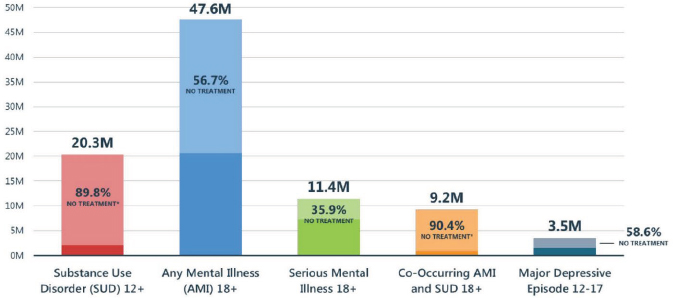
* No treatment for substance use disorder is defined as not receiving treatment at any location, such as a hospital (inpatient), rehabilitation facility (inpatient or outpatient), mental health center, emergency room, private doctor’s office, self-help group, or prison/jail.
SOURCES: As presented by Steven Ondersma, August 26, 2020; https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/Assistant-Secretary-nsduh2018_presentation.pdf (accessed September 4, 2020).
___________________
24 For more information, see https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-and-b-recommendations (accessed September 11, 2020).
A second issue, said Ondersma, is the amount of training required to give primary care clinicians the skills to screen their patients for MHSUDs. This need is further complicated by the fact that training does not always produce sustained changes in their behaviors (van Beurden et al., 2012). Ondersma added that an additional challenge is that primary care providers vary in the extent to which they are comfortable directly addressing MHSUDs, with the end result being that most at-risk adults do not receive even brief advice to change (McKnight-Eily et al., 2020).
Ondersma and his colleagues have sought to address these issues by taking advantage of a practice’s waiting room as a window of opportunity to provide SBIs using either the individual’s own smartphone or technology provided by the practice. The app generates a report for the primary care team. In fact, said Ondersma, his team and others have shown in a number of trials that these approaches have had a significant impact on substance use behavior (Martino et al., 2018; Ondersma et al., 2014; Ramsey et al., 2019; Yonkers et al., 2020). His team has also shown that this technology-based approach was equal to, and more cost-effective than, treatment as usual (Martino et al., 2018; Olmstead et al., 2019). Ondersma noted that an ongoing implementation trial has shown that more than 90 percent of patients successfully used an SBI app with little assistance while waiting for their appointment. Moreover, patients are highly satisfied with this electronic SBI process (Loree et al., 2019; Ondersma et al., 2015).
Ondersma said that such findings raise the possibility that technology could dramatically reduce training needs and the workload of primary care staff. As an example, he pointed to the app-generated report that could flag key behavioral health risks and prompt primary care staff to address them. “Technology may be a way to let us zero in and prioritize in a way that is more sustainable for primary care teams,” Ondersma concluded. However, he cautioned that unintended consequences could create more problems.
Supporting a Workforce for the Provision of the Essential Components of Care
Parinda Khatri, chief clinical officer at Cherokee Health Systems, explained that blending behavioral health and primary care has been at the core of her organization’s mission since the early 1980s and is an integral part of its care model. She shared that Cherokee Health has also been using telehealth for 20 years, primarily as a means of enhancing access to care. Khatri noted that because it is a challenge to get trained providers to come to the mountainous areas of Tennessee and work with the underserved, her organization has been “growing its own workforce for the past 40 years.”
Primary care teams at Cherokee Health include a behaviorist—typically a licensed behavioral health provider—a psychiatrist, and a community health coordinator. The organization also relies on peer wellness coaches and certified peer recovery specialists who stay in close contact with their clients. Khatri said that the care teams are structured so that patients feel that they are in one space and that everything is organized around them. She added that primary care at Cherokee Health is enhanced by behavioral health support and that patients also have access to a continuum of specialty mental health services. Khatri noted, too, that patients often travel 2–3 hours to a facility, making it important that every clinic in the system offers a broad scope of services. Toward that end, Cherokee Health has training partnerships that include residencies in family medicine, psychiatry, psychology, nursing, social work, nutrition, pharmacy, and public health, while also providing training to health care providers from other systems who want to learn about its model of care.
Khatri explained that everyone trained at Cherokee Health learns to conduct behavioral health assessments and provide treatment, including for MHSUDs, which she called a game changer for the system. For example, every pharmacist trained at Cherokee Health participates in the addiction medicine clinic and the intensive outpatient program for alcohol and drug use. “I can tell you, it opens their eyes,” said Khatri. “They are seeing the soft underbelly of people who have experienced trauma and who are struggling to make it through each day.” The result, she added, is that trainees gain empathy and understanding that changes the way they practice.
Khatri explained that training at Cherokee Health also stresses the “4Cs of primary care”—contact accessibility, coordinated care, comprehensive care, and continuity of care (Starfield, 2001)—and the importance of team-based care and attending to contextual, cultural, and social factors. Training includes shadowing multiple providers and attending clinical meetings in disciplines outside of a trainee’s primary area of interest, as well as team-based multidisciplinary teaching, immersion in the culture of integrated care, and population health analytics. Every trainee also learns the common elements for assessing and treating depression and SUDs, including screening and management protocols, motivational interviewing, trauma-informed care, and medication management.
On a final note, Khatri said that Cherokee Health has started including a developmental psychologist in every well-child check for mothers seen in the obstetrics clinic who were addicted to opiates or other substances. Such intersectionality, she said, provides a wonderful opportunity for trainees to see how behavioral health care can be integrated into primary care settings of all types.
Panel Reactions and Discussion
Session moderator Ross opened the session by asking the panelists to discuss what the field should emphasize regarding training in order to advance integrated care. LaBelle replied that training and supporting people so that every team member can work to the scope of their practice has huge value, as does reimbursing them for the services they provide at the same level that specialty care is reimbursed. In other words, registered nurses, peer recovery coaches, social workers, pharmacists, and other members of the team should all be reimbursed for their services. Cobb noted that pharmacists are often part of the primary team in some settings but only when additional funding to support them is available. Medicare, for example, does not reimburse for pharmacist services. She explained that in Montana, Medicaid has started paying for services provided by a clinical pharmacist working in a medical office, which has been helpful. At the same time, due to limited resources, there are not many psychiatric pharmacists being trained in the context of integrated primary care, with most being trained in hospitals, she said.
Khatri views future training initiatives as paying greater attention to telehealth, and not just for those providers who are interested in it, and clinical informatics and the types of data that need to be shared within a team. She believes that knowledge about clinical informatics and the ability to practice via telehealth will shape financing in the future. Ross added that teaching benchmarking and how to feed that information to the team is an exciting area of promise.
Ross asked Foxworth if she sees peer supporters playing as important a role in treating OUD or alcohol use disorder as they can in depression care management. Foxworth explained that her organization has been a pioneer in creating peer specialist coursework, and DBSA has a contract with the VA to train all of its peer apprentices. She added that it does not matter if training encompasses SUDs or mental health conditions. She explained that “at the end of the day, what the peer specialist is doing is using their unique lived experience and knowledge of living with a mental health or substance use disorder and bringing that knowledge of how to thrive and live” to the individual facing those challenges.
Responding to a question about the future role of technology, Ondersma replied that he sees its applications expanding to address multiple factors, such as substance use and mental health issues during pregnancy and postpartum. “There are so many other behavioral risks for which we can use technology to reach out, identify, provide some motivation, and then try to make sure that the primary care team has the information it needs,” said Ondersma. He also said that developers continue to make technology more personalized, using natural language capabilities and feedback from clinical trials, so that nobody comes to the technology with an interest or perspective that cannot be under-
stood. In addition, Ondersma said that systems will become better at parsing information and providing it to clinicians in ways they find most helpful and that will lead to better outcomes for patients. The idea, highlighted Ondersma, is to deploy user-centric techniques to put information into a focused and actionable form that empowers clinicians to do their jobs better rather than feel more overwhelmed by information.
Khatri noted that Cherokee Health, as a safety net system, has a patient population that is highly variable in terms of digital literacy and Internet access. As a result, it has had to create access points at its clinics for telehealth appointments and make adjustments for those who cannot do a 30-minute telehealth session. One approach has been to engage in interactive texting, and Cherokee Health has also hired digital health literacy coaches to help clients set up e-mail accounts and learn how to log in to and use the health system’s patient portal.
LaBelle pointed to the ways that training has changed during the COVID-19 pandemic. Instead of all-day, in-person sessions, she noted, training is now done in 1- to 4-hour online blocks with more interactive and case-based modules. The key, she said, is to be creative in thinking about how to use chat functions and other online features to enhance training. LaBelle then asked Cobb why pharmacists are not getting trained to obtain a waiver to prescribe buprenorphine. The main reason, said Cobb, is that pharmacists are not allowed to obtain that waiver, and while they may have collaborative practice agreements allowing them to prescribe medications under the supervision of a physician, buprenorphine is excluded from that provision. She noted that national pharmacy organizations are lobbying to change those regulations.
When Ross asked Ondersma if the information from his app could be incorporated into a clinical decision-support system as a next step in creating baseline standards of care, Ondersma replied that this is an important avenue for future work. Currently, he and his colleagues are working on a project funded by the Centers for Disease Control and Prevention to implement electronic screening and a brief intervention for alcohol use among women throughout the Henry Ford Health System.25 Part of this project does include using clinical decision support in the Epic EHR to provide physicians with quick tips on how to proceed when there is a positive score on the assessment. “It is important to take these results and put them into the medical record where we can track them and where we can implement specific procedures that are standardized across these behaviors,” said Ondersma. He added that his team is studying ways to ensure that physicians are not burdened with too many alerts from the EHR.
___________________
25 For more information, see https://www.henryford.com (accessed September 11, 2020).
Question and Answer Session with Webinar Participants
The first question asked the panelists to discuss the importance of seeing patients in person in primary care and whether integration is more difficult when that is not possible. Khatri replied that going virtual does make providing care more difficult, given that proximity with other team members is such a key part of the integrated primary care model. Her system has switched to a schedule that reduces the density of people in the clinic and uses a digital platform to bring teams together, but clinical staff are still adjusting to this new way of practicing medicine. “I do not think they are at the point where it is easy,” said Khatri. “You have to be absolutely intentional and realize that we have to continue to communicate and collaborate.”
Foxworth explained that the intent of the peer model is to meet patients where they are, so rather than have patients come to the clinic, peer specialists support them in their community at a place of their choosing. She noted that in March, her team had to contact its peer support specialists and tell them that they could no longer meet in person with their clients; rather, they had to work virtually, such as via phone. What was lost in the transition, however, was the weekly and semimonthly huddles with clinicians to talk about their clients. “What we have learned, especially in our monthly coaching calls, is that there is no such thing as too much communication,” said Foxworth. In addition to monthly video conferences that bring everyone together, peer support specialists are encouraged to use e-mail whenever they have a question for the clinical staff.
In terms of adapting to the new realities of the COVID-19 pandemic, Ondersma said that his team had to figure out a way to provide patients with a link to the app that they could access on their own devices. “We are doing it differently in different clinics, but there are all kinds of ways that we have been able to adjust it so that patients have been able to make use of the technology before they are seen,” Ondersma explained. At one obstetrics clinic, women arrive and scan a bar code at the clinic door with a smartphone. They return to their cars and complete the assessment that has been opened on their device. With respect to smartphone ownership and comfort with technology, Ondersma noted that age is a better predictor of familiarity and comfort with technology than income.
A webinar participant asked how LaBelle’s and Khatri’s models incorporate the social determinants of health, and LaBelle said that they are critical: “If you do not address people’s housing and food insecurities, you might as well just go home, because the rest does not work,” said LaBelle. In Massachusetts, she explained, the Bureau of Substance Addiction Services26 funds care manag-
___________________
26 For more information, see https://www.mass.gov/orgs/bureau-of-substance-addiction-services (accessed September 11, 2020).
ers, peer navigators, and peer recovery coaches to help with support services. In addition, her program uses the Tool for Health & Resilience in Vulnerable Environments27 to assess and decide how to best meet an individual’s needs with regard to social determinants. Doing so, said LaBelle, is often the most important service her program provides.
Cherokee Health has community health coordinators who, in Khatri’s view, are “geniuses at being able to connect people with resources, such as food, clothing, and shelter, as well as getting medical equipment and supplies that people need.” She noted that before the pandemic, a large part of the community health coordinators’ workload was going to people’s homes, appointments, and even court dates. Cherokee Health has food pantries in all of its clinics, several busses, a mobile clinic, and community partners that help meet patients’ needs, including bringing truckloads of fruits and vegetables to clinics that are located in food deserts.
Foxworth said that she has been humbled and honored to see the success of peer support specialists in providing strategies for self-empowerment and achieving self-determined lives. She noted that when a patient works with someone who has walked the same walk as they have and is able to give them hope and inspiration, it can make a huge difference in alleviating some of the social determinants of health. “They realize what kind of life they want, and they are getting the support and strategies to attain that life,” said Foxworth.
In response to a question about limitations on the number of patients that health care providers can care for, LaBelle noted that there are limitations due to federal requirements and mandates. LaBelle pointed out, however, that in her view, if everyone in primary care was treating people with MHSUDs, there would be no problem meeting demand. For example, in her experience, this is not a barrier to providing care in the community health centers in Massachusetts, said LaBelle, because the staff are invested in this work as a result of the positive results they have seen in their patients.
A webinar participant asked Cobb about policy actions that could help increase the number of clinical pharmacists trained to engage in integrated behavioral health or resources that can help families who want to access pharmacist team members. Cobb replied that two of the biggest barriers to including clinical pharmacists on the care team are reimbursement and training. Currently, she noted, some 30,000 board-certified clinical pharmacists in the United States work in outpatient settings (BPS, 2019). To gain access to a pharmacist, she recommended contacting an FQHC or community health center, which is where the largest number of clinical pharmacists work outside of the VA system. Cobb said that it was her understanding that the Indian
___________________
27 For more information, see https://www.preventioninstitute.org/tools/thrive-tool-health-resilience-vulnerable-environments (accessed September 11, 2020).
Health Service28 also has a robust clinical pharmacy program. She said that she would like to see telehealth used to increase access to the limited number of psychiatric pharmacy specialists and a regulatory change that would allow psychiatric pharmacists to serve as the psychiatric specialist on a team. Today, the collaborative care model billing code cannot be used for psychiatric pharmacists unless there is a partner psychiatrist or psychiatric nurse practitioner on the team.
A webinar participant with a family member in a state hospital due to severe mental illness and an SUD described the difficulty in getting care for their loved one. The participant questioned the role of the primary care sector in providing care for someone with such severe health challenges. Khatri responded by noting that the question speaks to the challenge of navigating the U.S. health system and how financing silos create problems for families seeking care for their loved ones. In fact, she noted, being a health care professional does not make it any easier to find care for a loved one with a serious MHSUD. Her advice for the participant was to connect with an advocacy group, such as the National Alliance on Mental Illness,29 to see what resources are available to help navigate the system. Typically, Khatri added, every state has a mental health association to which all community mental health centers belong. LaBelle noted that Section 42 of the Code of Federal Regulations30 has not made it easier to access care for a loved one with an SUD, but she added that changes are coming. She stressed the importance of having responsible family members at the table to ensure access to needed services.
The next question focused on the role of family members on the integrated care team. Foxworth said that is a complicated question because, while it has been proven that those individuals who have support from family members have better recovery outcomes, that has to be balanced against patient preferences. “There could be reasons why the patient does not want their family involved,” she said. That can be painful for family members when they see ways in which they can help, but they have to accept that their loved one has their pathway to recovery and the family members have their own journey to recovery, and those might be very separate journeys. Khatri added that Tennessee, Maryland, and a number of other states have a certified peer position called a “family support specialist,” who is typically a parent with a child who has been diagnosed with an MHSUD, and they go through training
___________________
28 For more information, see https://www.ihs.gov (accessed September 11, 2020).
29 For more information, see https://www.nami.org/Home (accessed September 11, 2020).
30 42 CFR Part 2 serves to protect patient records created by federally assisted programs for the treatment of SUDs. For more information, see https://www.hhs.gov/about/news/2020/07/13/fact-sheet-samhsa-42-cfr-part-2-revised-rule.html (accessed September 4, 2020).
to essentially serve as navigators. Her hope is that this role will be expanded and enhanced, because it has been quite useful, particularly when working with children.
Cobb, responding to a request for advice on building strong primary care–based integrated clinical teams, said that bidirectional education is key. Many behavioral health providers, she explained, are not used to working in fast-paced primary care clinics, and many primary care physicians are not used to working with other members of a team. It is also important to develop criteria for when other team members are called on to care for a particular patient. For example, she explained, not all patients need to see a clinical pharmacist.
Cobb added that communication and using a single medical record is also important, as is developing protocols for how team members communicate with one another and workflows for incorporating other team members into the care process. Many people, for instance, have never worked with a clinical pharmacist and do not understand how that is different from working with a community pharmacist. She added that teaching nurses and physicians how to do a warm handoff can help them explain to their patients the role of any new team member in their care.
A webinar participant asked a question about what level of certification and training is appropriate for peer specialists. Foxworth noted that every state has its own requirements and regulations. At a minimum, she said, every state requires that peer specialists take a course, but there are no uniform requirements around course contents. Some courses provide training on how to use tools such as motivational interviewing and decisional balanced worksheets, while others are more about peer empowerment and finding one’s voice. As a result, one barrier for the profession is achieving standardization on minimum requirements for peer support specialists and recovery coaches so that credentials issued in one state will be valid in another. Foxworth replied to a question about where to find courses to become a peer specialist or peer navigator by recommending that people start with their state department of mental health to find out what the requirements are to become a peer support specialist or recovery coach. She noted that some states refer to those positions by other names, such as “certified support recovery coach.”
A webinar participant asked LaBelle why registered nurses are the basis for the model she and her colleagues developed. She replied that in 2003, when she started doing this work, there was a limited knowledge base about treating SUDs. Her approach was to follow the HIV model, which had nurses work to the scope of their practice and left treating more complex patients to providers, who then did not have to deal with social determinants and other behavioral health issues. She noted that of the 13 registered nurses caring for 900 patients in one region, 6 are in school to become psychiatric nurse
practitioners, which speaks to their commitment and her organization’s ability to support them in their profession. In addition, many of those nurses have become certified addiction nurses.
To close the session, in response to a question about what defines a learning health system and how it relates to the workforce, Khatri explained that a learning health system is one that teaches, educates, and is invested in building a workforce. “That becomes a compass to guide you in everything that you do,” she said.
ADDRESSING FINANCING, PAYMENT, PRACTICE, AND SYSTEMS-LEVEL ISSUES, POLICIES, AND INCENTIVES TO SUPPORT PROVISION OF ESSENTIAL COMPONENTS OF CARE
To start the final session of the webinar, Richard Frank, professor of health economics in the Department of Health Care Policy at Harvard Medical School, said that a long-held belief has been that some simple policy fixes would go a long way to promoting the integration of behavioral health and other types of medical care into primary care. The final session, he said, would focus on what is needed beyond those simple fixes to advance the goal of integration.
Can Primary Care Afford Behavioral Health?
Robert Phillips, Jr., executive director of The Center for Professionalism & Value in Health Care, began his presentation by noting that when he finished his residency training in 1998, he and his cohort of trainees were not allowed to put a mental health diagnosis down as part of their billing because doing so would invalidate the entire billing. As a result, said Phillips, “you had a whole generation of family physicians who were acculturated to not actively diagnos[e] mental health, even though we treated it on a regular basis.” Today, mental health remains integral to the family medicine curriculum and is a requirement of residency training.
Phillips explained that when he moved into a community-based residency training program, there were three integrated psychologists, a doctor of pharmacy (Pharm.D.), and a Pharm.D. education program, all of which are gone now because of a payment model that would not support those positions. “We have had to develop alternative ways of making sure that our trainees are getting exposure to not just psychological care but how psychologists address care and can be a partner,” said Phillips.
Data from the National Health Interview Survey reveal that almost half
of all people only receive primary care, regardless of whether they self-reported better mental health or poor mental health on the survey (Petterson et al., 2014). For those with a worse mental health score, approximately 5 percent will get care only in a mental health setting, and about 14 percent will get care in both a primary care and a mental health setting. Similarly, 65 percent of elderly patient visits for depression were in primary care (Harman et al., 2006). “There are many people with mental health issues being cared for in primary care alone, and not nearly enough overlap, particularly for those with severe mental illness,” said Phillips. “As the last panel was very clear about, it would be so much better if behavioral health and substance use disorder care were integrated.”
Phillips noted that about 10 percent of the graduates of family medicine training programs not only have buprenorphine waivers 3 years later but also report actively caring for people with OUD. He added that those 50–60 graduates per year serve as one of the largest workforces caring for mothers with SUDs, both prenatally and postnatally (St. Louis et al., 2020).
Three years ago, said Phillips, Sanjay Basu and his colleagues used a simulation model to determine if integrated behavioral health care could be financially viable (Basu et al., 2017). These investigators looked at two different models of care:
- Collaborative care, in which primary care manages in-person care and pharmacotherapy, with registered nurses or a master’s level behaviorist providing follow-up care by phone; and
- Primary care behaviorist, in which a Ph.D. psychologist or licensed clinical social worker is embedded at the primary care site to provide in-person care.
This simulation showed that the first model was viable, as previous speakers pointed out, but the second model was not financially viable outside of an FQHC.
Similarly, Brenda Reiss-Brennan and her colleagues at Intermountain Healthcare conducted a retrospective cohort study comparing an integrated behavioral health model with usual practice and found that while the integrated model resulted in fewer ED visits and hospitalizations and better quality of care, the practices received less reimbursement (Reiss-Brennan et al., 2016). A commentary accompanying that paper said that while the integrated model was the right thing to do, the cost-benefit accrues to the employer or insurer, not to the practice that bears the expense of providing integrated care (Schwenk, 2016).
The bottom line, said Phillips, is that in a fee-for-service environment, the models of integrated care that work so well—and which the last panel
described—are not financially viable for the majority of the population cared for outside of the safety net. “We need to find payment models that will support the integration of behaviorists and opioid use disorder therapies into primary care more robustly,” concluded Phillips.
Delivery System Considerations for Integrating Addiction and Mental Health Treatment into Primary Care Settings
“Despite some important examples, such as prescribing antidepressants or screening for alcohol problems, we know that integrated mental health and substance use treatment in primary care is still not the norm,” explained Sharon Reif, senior scientist and deputy director of the Institute for Behavioral Health at the Brandeis University Heller School for Social Policy and Management. In her view, one reason for this is that systemic change requires a system-focused framework, rather than the “adoption of innovations” framework that highlights how an innovation’s relative advantage and complexity can drive an individual or single entity, such as a primary care practice, to integrate care (Plsek, 2003; Wisdom et al., 2014).
A systems focus highlights essential aspects of innovation adoption beyond the individual program or setting, Reif explained. It requires a resource system that provides financial, regulatory, management, and oversight support for change agents or champions who contribute specialized expertise and can advance the cause of adoption (Greenhalgh et al., 2004). A systems focus also pays attention to the “outer context,” such as national efforts to address opioid addiction, which can affect whether the innovation is feasible or sustainable at that time. Reif noted that delivery and payment systems can facilitate a move toward integrated care, and, in doing so, they can also address systemic barriers. As an example, she said that the development and support of integrated care models at the system level highlights their value to the delivery system as a whole, which can also reduce stigma.
Reif noted that the availability of system-wide training, technical assistance, or expert report models can address barriers within primary care settings, such as a lack of knowledge or confidence about screening for and treating MHSUDs, by providing support and reassurance, particularly during the early phases of adoption. She stated that funding and incentives are essential “carrots” or “sticks” to encourage primary care practices to adopt integrated care and that supporting the infrastructure needed for integrated care can reduce silos and encourage collaboration and holistic care. She explained that “one can consider, for instance, how many innovative models started under Medicaid Section 1115 waivers, which address financing and delivery system changes together.” Reif added that an advantage systems have, compared to individual practices, is that they can wield greater power to address concerns about regulatory and financial issues.
Reif emphasized that system-level change requires both delivery and payment system reform, which together determine access to care, quality of care, and ultimately health equity (see Figure 7).
“These systems are intertwined, and effective change must address both,” said Reif. A delivery system may provide access to integrated care, for example, but if the payer does not allow same-day visits, it reduces access. In the same way, providers must be paid sustainably for delivering these services or they will not offer truly integrated care. In addition, said Reif, quality of care always remains at the forefront, and delivery systems can set goals and incentives to encourage high-quality integrated care. However, the quality metrics and data used in the separate primary care and specialty systems may not remain the same for integrated care systems.
Reif listed several broad facilitators of change important for delivery systems. Champions are necessary for adoption of any innovation across systems and payers. This is particularly true for MHSUDs, where stigma persists at all levels, and champions can raise awareness, serve as role models for adoption, share knowledge, and celebrate successes. Delivery-level champions must engage with practice-level champions to ensure that change diffuses in all settings, added Reif.
Flexibility during the adoption process is key as well, said Reif. “We know that there is tremendous variation across practices and settings, not just in their organization but also in their knowledge level, willingness, and capacity
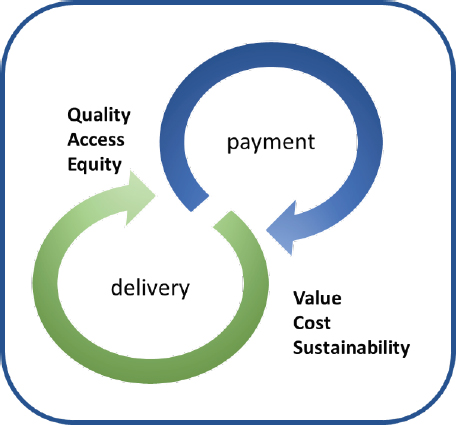
SOURCE: As presented by Sharon Reif, August 26, 2020.
to implement integrated care approaches,” she noted. “By creating systems that allow flexibility during implementation, the likelihood of success may improve.” Flexibility also highlights building on what has already worked within the setting of good practices, increasing the likelihood of provider buy-in or stakeholder engagement for the next stage of adoption.
While many interventions are implemented successfully, not all are durable or sustainable. In integrated care, for example, reimbursement issues and funding for non-billable infrastructure, such as care managers, are a primary reason innovations are not sustained, Reif explained. At the same time, the fragmented nature of health care means that the influence of any one payer or health care system may be insufficient to get any given primary care practice to adopt an intervention. Multisystem approaches, she said, would increase influence and the likelihood of successful change. Such an approach should include systems such as social services or specialty care, each of which requires relationships with the integrated care setting and an understanding of how these other care systems work and how to engage patients in need.
One concern with delivery system approaches, explained Reif, is that they can include system-level interventions imposed from the top down and may not diffuse to direct care providers or be incorporated fully into a practice. A practice, for example, might only offer referrals for buprenorphine therapy versus actually inducing and maintaining patients itself.
Looking to external factors, Reif explained that a significant barrier to change is the sheer number of initiatives and requirements that have already overloaded many practices. External context also includes the social determinants of health, and Reif noted that specialty care, more often than primary care, engages social services, housing, and other systems to address social determinants. “That said, delivery systems could be significant drivers of innovations, such as integrated care, if the resources, knowledge providers, and external contexts are all considered and engaged, along with payment systems and the need for sustainability,” concluded Reif.
Medicare and Medicaid Opportunities and Challenges for Integrating Behavioral Health Care in General Medical Settings
Kirsten Beronio, director of policy and regulatory affairs at the National Association for Behavioral Healthcare, explained that her remarks would focus on two components of the integration models that previous speakers had described that are considered to be critical but are often difficult to finance: case management or care coordination activities and consultations with a behavioral health specialist. She also noted that while Medicare, in 2017, implemented behavioral health integration billing codes designed to support
the collaborative care model, provider uptake of those codes has been low (Carlo et al., 2019; Cross et al., 2019).
One issue with the codes, said Beronio, is that certain processes and structures have to be in place to bill for these services, and the cost of implementing those processes and structures is rarely reimbursed. When those implementation costs are covered (e.g., with discretionary grants) it is not in a way that ensures ongoing support through mainstream financing mechanisms, said Beronio. Another possible issue, she explained, is that payment for the behavioral health specialist has to flow through the primary care provider, creating an administrative burden for the primary care provider and a disincentive for the behavioral health specialist. Beronio said that a more recent Medicare action to create interprofessional consult billing codes31 does present an opportunity for obtaining coverage for the consultation part of these integrated care models. Beronio noted that this may be a more flexible way to support that critical component of integration models and overcome some of the obstacles to integrating care.
Medicare’s expanded coverage of telehealth prompted by the COVID-19 pandemic32 is another development that Beronio believes holds promise for integration, though she noted that CMS may not continue this policy for all telehealth services once the pandemic ends. Beronio also noted that the 2018 Substance Use-Disorder Prevention That Promotes Opioid Recovery and Treatment for Patients and Communities Act33 now allows Medicare to pay for telehealth services for SUD treatment and comorbid mental health conditions provided to an individual while at home. Medicare’s new OTP benefit,34 which became effective in January 2020 and covers methadone clinic services, is another opportunity for integrating care, said Beronio. Her hope is that this new bundled payment will help broaden the availability of OTPs for Medicare and Medicaid beneficiaries and for those covered by private insurance. Beronio also noted that OTPs can be the hubs in a hub-and-spoke model as in Vermont and support provision of treatment for OUD in more mainstream settings including primary care offices.
___________________
31 For more information, see https://www.aappublications.org/news/2019/01/04/coding010419 (accessed September 14, 2020).
32 For more information, see https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html (accessed September 14, 2020).
33 For more information, see https://www.congress.gov/bill/115th-congress/house-bill/6 (accessed September 5, 2020).
34 For more information, see https://www.cms.gov/Center/Provider-Type/Opioid-Treatment-Program-Center (accessed September 14, 2020).
Beronio said that CMS, as part of its new physician fee schedule,35 is finalizing a new payment in Medicare for MAT in EDs. While this is not a collaborative care model exactly, she noted, it is aimed at integrating specialty care into more mainstream settings. There is some evidence, added Beronio, that this can be helpful for engaging people in the ED, connecting them with follow-up care, and improving outcomes (D’Onofrio et al., 2015).
Beronio explained that Medicaid generally does not allow for reimbursement of consultations when the beneficiary is not physically present for the service. This policy creates a significant obstacle to paying for consulting with a specialist. While CMS has clarified that the cost of that consultation can be incorporated into the payment for a primary care encounter, the rates for those encounters are already low, so trying to pay for more services with those rates is not going to change much, said Beronio. She noted that the November 2018 State Medicaid Director letter contains a table that maps different components of the collaborative care model to specific Medicaid benefits (CMS, 2018).
Recently, CMS approved a Section 1115 demonstration for Rhode Island that allows the state to continue implementing a program similar to the Massachusetts Child Psychiatry Access Project36 (Straus and Sarvet, 2014), whereby a team of behavioral health specialists and care managers can help support multiple pediatricians and improve access to behavioral health care. Rhode Island’s program, initially funded by a grant from CMMI, allows the state to pay specialists directly instead of through the primary care physician. Beronio noted that HRSA has a grant program—the Pediatric Mental Health Care Access Program37—that also supports this type of approach, enabling a team of behavioral health specialists to support pediatricians in providing access to behavioral health care.
Beronio highlighted the importance of tying together increased coverage benefits through Medicare and Medicaid with a more flexible approach to federal funding that can help pay for some of the up-front implementation costs. She also noted the importance of existing Medicaid benefits covering case management, care coordination, and health homes.
In closing, she listed three overarching barriers to implementing integrated care:
- Implementation costs, regarding staffing, training, billing, and workflow changes, as well as technology for consultation and remote services;
___________________
35 For more information, see https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched (accessed September 14, 2020).
36 For more information, see https://www.mcpap.com (accessed September 5, 2020).
37 For more information, see https://mchb.hrsa.gov/training/projects.asp?program=34 (accessed September 5, 2020).
- Workforce challenges, including limited availability of behavioral health care providers, participation in payer programs, and a reluctance to screen and engage in MHSUD treatment; and
- A lack of awareness of opportunities and coordination of financing available through Medicare, Medicaid, private insurance, and grant funding.
The Addiction Recovery Medical Home Model
In the webinar’s final presentation, David Smith, chief executive officer and founder of Third Horizon Strategies and founder of the Alliance for Addiction Payment Reform, said that one focus of his organization’s work has been to follow how money moves from taxpayers, employers, or consumers to payers, managers, provider groups, and doctors and how that ultimately affects patient care. Smith noted that the highly fragmented way in which money moves through the system automatically creates disincentives to take the actions that have been shown to promote better health outcomes.
Smith explained that he came to work in the SUD field as a result of having his father, younger brother, and younger sister all die from opioid overdoses. He said that he watched their journeys in and out of recovery, in and out of rehab, and in and out of group settings, each time supposedly “cured” of their addictions. “With stunning realization, I came to find out they were not, in fact, cured, but that there was a disruption in their recovery and it ultimately led to their fatal event,” said Smith. About 3 years ago, he and a colleague started looking at ways to reconfigure the flow of money at the payer level to better align incentives and organize the delivery system to offer the types of models that the speakers had discussed over the course of the workshop. Smith clarified that two concepts were at the core of this effort: that society has started to view addiction as a chronic disease, not a moral failing, and that the delivery system was not providing what it was being paid for (i.e., successful, long-term recovery).
Over an 8-month period, Smith and his colleagues developed the Addiction Recovery Medical Home Alternative Payment Model.38 The model was originally designed to be a thought exercise, but publishing it (Polak et al., 2018) triggered phone calls from health plans, state governments, and others who were excited by its potential. Since then, the Alliance for Addiction Payment Reform has worked with a wide range of payers, health systems, advocacy organizations, and others to further develop the model. Smith said
___________________
38 For more information, see https://www.incentivizerecovery.org (accessed September 11, 2020).
that he is most enthusiastic about a partnership with the Washington State Health Care Authority to help it respond to a CMS grant that would implement the model statewide. His organization has also announced a number of pilot programs in which health systems are working to implement this model of addiction treatment.
Smith explained that the model has five foundational elements—a multifaceted payment model, quality metrics, an integrated treatment and recovery network, a care recovery team, and a treatment and recovery plan—and is based on 10 guiding principles (see Box 3).
Smith explained that the payment model adopts elements of episodes of care and bundled payments to reward performance based on recovery-linked process measures and emerging quality measures. He further explained that risk-bearing providers or providers in pay-for-performance arrangements have three mechanisms through which they assume risk, earn bonus payments, and achieve a nontraditional payment adjustment from the model: episodes of integrated care, a quality achievement payment, and a performance bonus. In closing, Smith pointed out that the model looks different in different markets, but each implementation of the model has generally adhered to the principles listed above.
Panel Reactions and Discussion
Frank opened the discussion by asking the panelists to talk about what they would do to bring to a national scale the integrated delivery models that the workshop discussed over this and the previous two webinars. Beronio replied that being flexible about how an integration model is implemented is critical, as in not limiting implementation of a model to treating a specific disease and being overly focused on fidelity to a particular model. Given that consultations and case management are essential components of care for many different conditions, Beronio said that it should be possible to consider integrating services and taking a team-based approach to care for an entire patient population, or at least the subset with serious chronic conditions. Doing so, she offered, might make it more feasible to finance some of those services. As an example, she suggested that since the interprofessional consult code is not tied to behavioral health, it can be applied to other services, such as diabetes management or a cardiologist consult. Expanding telehealth to enable access to specialists will also be important, said Beronio, particularly for systems serving rural areas. Her final suggestions were for Medicaid to be more flexible in how it reimburses for case management and for payers to provide resources to implement these models and train staff.
Phillips noted that primary care tends to treat the whole person and is often dealing with not just mental health issues but an array of other chronic or acute health conditions. This requires balancing the needs of each of those conditions and maximizing therapeutic value, for both a particular visit and
the relationship over time. He cited the Vermont Blueprint for Health,39 which operated under a Medicare waiver and created community resources for behavioral health, social services, and other services that small practices could draw on but would otherwise not be able to afford to deliver. Phillips also noted that the payment models and support systems for FQHCs enable them to have the richest mix of PCMH components. “I think we have existing models, but they just have not been translated for primary care writ large,” said Phillips. “I think that is the next opportunity.”
Reif, agreeing with Beronio and Phillips, emphasized the need for collaboration across systems, expertise, and payers. She noted that the Washington State hub-and-spoke model,40 in which the expert is the hub for six treatment networks that include MHSUDs, is organized in part by the state’s substance use system, which is paying for nurse care managers and some of the infrastructure needs. Reif added that given most Washington State residents with OUD are on Medicaid, the networks can engage with state Medicaid decision makers to try to address some of the regulatory barriers to implementing integrated care models.
Smith commented that one challenge to scale any of these models on a national level is that regulatory and cultural conditions differ from community to community—the same factors that often befuddle large companies when they try to expand overseas. At the same time, said Smith, there is more than enough money, technology, science, clinical know-how, and evidence to address the challenges that have been raised. “We know many of the answers, but we get in our own way, economically, sociologically, and politically,” said Smith.
Smith then remarked that people do difficult things when they are in pain, and the pain in health care tends to be economic for many of the stakeholders in this $4 billion industry. His approach has been to quantify that pain for providers and payers, identify a more ideal way to organize the financial and delivery systems to alleviate it, and then create consensus at the community level that acknowledges the idiosyncrasies of those communities so they can try to advance this work.
Frank commented that a focus on billing codes and fee-for-service may not be the most productive direction to take and that the mental health and addiction treatment communities should focus more on alternative payment systems. He asked the panelists to talk about the alternative payment models they view as most promising. Phillips said that primary care is where half of
___________________
39 For more information, see https://blueprintforhealth.vermont.gov (accessed September 11, 2020).
40 For more information, see https://www.hca.wa.gov/about-hca/behavioral-health-recovery/washington-state-hub-and-spoke-project (accessed September 11, 2020).
all care happens, but Medicare and other payers devote a small percentage of their total spending to it. Alternative payment models that continue that policy of disproportionately low spending on primary care are not going to create space for the rest of mental health, behavioral health, and even oral health to become integrated into primary care. “I do not think there is a way to get around that,” said Phillips. “You have to put more resources in and put them in in a way that supports integration and enables those other professions to be embedded in the same space.” He agreed with Smith’s point that the money exists to finance primary care at a higher level, and as Rhode Island and Delaware have demonstrated, it does not take a huge amount of money to do better. In Phillips’s opinion, the CPC+ and Primary Care First41 models are promising in that regard.
Reif said that it is difficult to consider financing options such as bundled payments and those types of approaches with a long-term view, which is what is needed when talking about recovery from an SUD or with a chronic model. As a result, she does not have a favorite alternative payment model other than it cannot be fee for service. Reif also commented that value-based payments and incentives and associating payments with quality are good ideas conceptually but difficult to realize in practice without making changes across the entire system. The incentives, she added, also have to be bigger, to get practices to change.
Smith said that he lives by the edict of “you get what you pay for,” and, in his opinion, that applies to the billing codes and fee-for-service structures. He agreed with Phillips that the CPC+ model is attractive, as are the next-generation ACO model42 and some of the permutations of the Bundled Payments for Care Improvement Advanced model.43 These models have demonstrated good results, said Smith, but they have not been scaled or lifted the burden of care, which he blames on the field not pushing itself hard to make them work better. “If we do not challenge ourselves to reorganize the system in a way that is more integrated, more inclusive, better coordinated, and more patient centric, we are going to continue what we have,” said Smith.
Smith noted that he has been hearing chief executive officers stand up at conferences and talk about the incredible things they are doing with value-based care, but their financial statement reveals that it represents 5 percent of their total income. “Five percent is not enough to move an institution to
___________________
41 For more information, see https://innovation.cms.gov/innovation-models/primary-care-first-model-options (accessed September 5, 2020).
42 For more information, see https://innovation.cms.gov/innovation-models/next-generation-aco-model (accessed September 5, 2020).
43 For more information, see https://innovation.cms.gov/innovation-models/bpci-advanced/participant-resources (accessed September 5, 2020).
reorganize itself in the right way,” said Smith. “Behavioral health has to have a seat at the table and be part of the value chain or we will leave a major efficiency gap in patients’ whole health,” he emphasized.
Beronio said that she did not have a particular model to cite and instead noted that any alternative payment approach should include multiple payers as a means of reducing the administrative burden that practices and systems shoulder to manage different funding streams and requirements. Beronio also noted the need for better metrics for integration that would be required to make value-based payments and the importance of raising reimbursement rates for behavioral health care and integrated primary care. She recounted that when Virginia implemented its Section 1115 demonstration to increase access to SUD treatment, it increased reimbursement rates, and suddenly more providers participated in Medicaid. Beronio added that Medicaid is currently overseeing a demonstration program44 in which it is funding 15 states to implement strategies to increase the capacity of their state Medicaid programs to provide beneficiaries with access to MHSUD treatment, including by closely examining and potentially increasing reimbursement rates for MHSUD treatment and assessing how that affects participation in Medicaid programs.
Frank commented that most of the discussion throughout the day centered on “pull” incentives, such as paying more or paying differently, and he asked the panelists to talk about what the field should be “pushing on” in terms of what types of services or infrastructure should be reimbursed to encourage integrated care. Smith said that the financial straits that states are in today and will be in for the next couple of years create an important opening for dialogue on restructuring health care to be more integrated. States are going to be looking for demonstrable savings, and, as Smith noted, a tremendous amount of evidence and science shows how the nature of certain interventions and certain combinations of people, processes, and technology can shift and change health outcomes and lower the economic burden on states. “There is a huge opportunity to prosecute a case for behavioral health,” said Smith. He also pointed out the incredible FQHC infrastructure in this country that has largely been sidelined for years but that could be expanded to improve care in parts of the country in which mental health care has been undersupported. Reif added that it is important to create pathways that would drive people to integrated care or at least collaborative care.
Beronio, agreeing with her colleagues, acknowledged that payers are increasingly recognizing the importance of focusing on people with behavioral health conditions because these patients are major drivers of cost and
___________________
44 For more information, see https://www.cms.gov/newsroom/press-releases/cms-commits-50-million-assist-states-substance-use-disorder-treatment-and-recovery (accessed October 2, 2020).
part of the small segment of patients who account for the majority of health care spending in this country. “If you look at overall spending on behavioral health, it is very low as a percentage, but if you look at the medical spending for this population, it is disproportionate,” said Beronio. In her opinion, payers should drive their providers and networks to screen patients for MHSUDs and facilitate access to treatment. Part of that effort is making it easier for providers to access a behavioral health specialist and providing the funds to enable that change in practice, including funding to cover the cost of finding and developing an arrangement with a behavioral health care specialist to provide consultations, hiring personnel to help with care coordination and case management, determining how best to modify the provider’s practice to implement an integration model, and training personnel on the model and how to bill for the new services. In her view, policy makers often believe that if they make a change to add coverage for something, it will get done—but it is not that simple. “We need to recognize the implementation cost and time that have to be invested into making these kinds of changes but also recognize that those are necessary investments, because if you do not address behavioral health issues, they will come back up,” said Beronio.
Phillips remarked that he and his primary care colleagues screen all their patients for depression and that he can prescribe pharmacotherapy, initial counseling, and even some initial cognitive behavioral therapy. However, until Virginia puts more money into its state Mental Health Access Program, if he wants to get a patient into counseling, he will continue to pull out an Excel spreadsheet and give the patient a list of at least five providers who take their insurance and offer a particular therapeutic modality. “My hope is that at least one of those five might be able to take them,” said Phillips. He explained that Virginia currently has a program where he can arrange to have a care coordinator take over the process of getting his patient into therapy. He noted that without an easy way to refer patients, providers are reluctant to screen.
Question and Answer Session with Webinar Participants
Referring to LaBelle’s presentation, a webinar participant asked about what can be learned from the nurse-led community health center model’s successful scaling and sustainability at the state level. Reif replied that what she likes about that model is that it includes training and technical assistance for all levels of staff engaged in the care process. The model’s developers have also been working with state officials to iron out some of the reimbursement issues that speakers in this session outlined. Another strong feature of that model, which has been sustained since 2003, is that there is an infrastructure of people who are helping to continually improve the model based on lessons learned from the successes of other models.
Responding to a question as to whether there was a business case that can be presented to payers and provider organizations to support peer integration in the primary care sector, Phillips responded that there have been studies45 showing there are overall savings with integrated care—demonstrating a business case—and he cannot understand what the barriers are to adopting these models. Smith suggested that the evidence that these models improve care and reduce costs is certainly strong enough, but it is still important to determine who captures that value. Only then will it be possible to identify ways of reorganizing or reconstituting a payment structure to shift rewards so that value is captured more fairly.
Reif, responding to a question about nonfinancial incentives, said that those could include providing technical assistance, placing care managers in a health system, and even handing out certificates of achievement or placing stars next to a provider's name in the local directory. Beronio noted that she has seen that having a behavioral health care manager can help alleviate some of the pressures on primary care providers. She also suggested showing providers that working with people with MHSUDs does improve patients’ lives as a means of reinforcing the positive benefits of participating in integrated care.
A webinar participant asked Beronio if she sees the new CMS/CMMI demonstrations for community health care and rural transportation as an opportunity to include behavioral health integration or increase reimbursements to primary care providers. Beronio said that she had not studied that demonstration initiative closely but that CMMI often provides up-front funding for some implementation costs that she had highlighted as presenting barriers to implementing integration models. One issue is that federal agencies often prohibit use of grant funding for “administrative costs,” which can limit the degree to which those grants can help address the types of barriers she talked about in her presentation. CMMI grants do, however, tend to focus on care coordination, she added, which could help support implementation of integration models.
Phillips responded to a question about whether behavioral health carve-outs pose a challenge to integration in the context of Medicaid by stating that “what the carve-outs did is put the burden of delivering most of the mental health care on me without any payment for it and [leave] the patients largely with having to call and get connected to someone they have no natural connection to, no relationship with, who is focused solely on that issue.” Phillips added that “the carve-outs were devastating, and I think they made care harder in most cases for us.” He noted, too, that “we felt quite cheated by it because we were still caring for the people’s mental health issues but were not allowed to even put the diagnosis code down.”
___________________
45 For more information, see https://aims.uw.edu/collaborative-care/building-business-case-cost-effectiveness-studies-collaborative-care (accessed October 6, 2020).
Smith said that he believes it is incredible that in 2020, just under half the states still have some type of carve-out in their Medicaid programs for behavioral health or long-term services and supports even though the evidence does not support this in terms of achieving integration and collaboration. In Smith’s view, as long as behavioral health is treated as something separate that is paid for through a separate funding stream or a different entity, taxpayer dollars will be left on the table and there will never be enough money to meet the demand for services.
CLOSING REMARKS
To conclude the session, Frank noted that all the day’s discussions focused on what has been done to the behavioral health field, and he wanted the webinar attendees to think about what the behavioral health provider system needs to do in terms of accountability and changing the culture of primary care to include behavioral health. “I think work on accountability and culture are important to move the ball forward,” said Frank.
Roach, offering remarks to close the virtual workshop, recounted speaking about the workshop with a friend who is a retired mental health and addiction professional. Her friend said that her colleagues talked about integrating primary care, mental health, and addiction services 40 years ago. What her friend did not say but implied was, “What makes you think all your talking is going to translate into meaningful action this time around? What is your X factor?” Roach said that one of her X factors was everyone who participated in the workshop and the collective enthusiasm, experience, and wisdom they brought to these discussions. To her, this suggests that there is now a critical mass of people with the requisite knowledge, skills, and motivation to make meaningful and lasting changes in the nation’s health care systems.
Roach’s other X factor is this particular moment in time and the urgent need for transformative change in the nation’s health care delivery system in the setting of today’s multiple converging public health crises. “It is hard to imagine how we could possibly overcome these crises and move forward as a society in the absence of profound changes in our systems of health care delivery,” said Roach. “The times are compelling us to act in ways that we have never acted before and [they] will continue to do so for some time to come. I believe, based on the energy and insights that all of our speakers and all of our audience members brought to these discussions, that we are more than well prepared to meet the challenge.”
Roach concluded the virtual workshop, noting that
Our fondest hope is that all of us will continue these powerful and transformative conversations well beyond this workshop in keeping with our surer understanding that optimal mental health is foundational to optimal
physical health, and encouraged by our faith that by working together across differences and professional disciplines, across disparities and resources and other would-be barriers, we can transform the delivery of health services in the United States in ways that will strengthen our communities and families for generations to come.
REFERENCES
Agerwala, S. M., and E. F. McCance-Katz. 2012. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs 44(4):307–317.
Alford, D. P., J. M. Richardson, S. E. Chapman, C. E. Dubé, R. W. Schadt, and R. Saitz. 2008. A web-based Alcohol Clinical Training (ACT) curriculum: Is in-person faculty development necessary to affect teaching? BMC Medical Education 8:11. https://doi.org/10.1186/1472-6920-8-11.
Alford, D. P., C. T. LaBelle, N. Kretsch, A. Bergeron, M. Winter, M. Botticelli, and J. H. Samet. 2011. Collaborative care of opioid-addicted patients in primary care using buprenorphine: Five-year experience. Archives of Internal Medicine 171(5):425–431.
Ali, M. K., L. Chwastiak, S. Poongothai, K. Emmert-Fees, S. A. Patel, R. M. Anjana, R. Sagar, R. Shankar, G. R. Sridhar, M. Kosuri, A. R. Sosale, B. Sosale, D. Rao, N. Tandon, K. Narayan, V. Mohan, and INDEPENDENT Study Group. 2020. Effect of a collaborative care model on depressive symptoms and glycated hemoglobin, blood pressure, and serum cholesterol among patients with depression and diabetes in India: The INDEPENDENT randomized clinical trial. JAMA 324(7):651–662. https://doi.org/10.1001/jama.2020.11747.
Alliance for Health Policy. 2017. Chapter 8—Mental health and substance abuse. http://www.allhealthpolicy.org/sourcebook/mental-health-and-substance-abuse (accessed August 10, 2020).
APA (American Psychiatric Association). 2013. Substance-related and addictive disorders. In Diagnostic and statistical manual of mental disorders, 5th ed.https://doi.org/10.1176/appi.books.9780890425596.dsm05.
Archer, J., P. Bower, S. Gilbody, K. Lovell, D. Richards, L. Gask, C. Dickens, and P. Coventry. 2012. Collaborative care for depression and anxiety problems. Cochrane Database of Systematic Reviews 10:CD006525.
Baker, E., R. Gwernan-Jones, N. Britten, M. Cox, C. McCabe, A. Retzer, L. Gill, H. Plappert, S. Reilly, V. Pinfold, L. Gask, R. Byng, and M. Birchwood. 2019. Refining a model of collaborative care for people with a diagnosis of bipolar, schizophrenia or other psychoses in England: A qualitative formative evaluation. BMC Psychiatry 19(1):7.
Bao, Y., B. G. Druss, H.-Y. Jung, Y.-F. Chan, and J. Unützer. 2015. Unpacking collaborative care for depression: Examining two essential tasks for implementation. Psychiatric Services 67(4):418–424.
Basu, S., B. E. Landon, J. W. Williams, Jr., A. Bitton, Z. Song, and R. S. Phillips. 2017. Behavioral health integration into primary care: A microsimulation of financial implications for practices. Journal of General Internal Medicine 32(12):1330–1341.
Bodenheimer, T., E. H. Wagner, and K. Grumbach. 2002. Improving primary care for patients with chronic illness. JAMA 288(14):1775–1779.
Bolton, P., C. Lee, E. E. Haroz, L. Murray, S. Dorsey, C. Robinson, A. M. Ugueto, and J. Bass. 2014. A transdiagnostic community-based mental health treatment for comorbid disorders: Development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Medicine 11(11):e1001757.
BPS (Board of Pharmacy Specialties). 2019. Annual Report.https://board-of-pharmacy-specialties.dcatalog.com/v/2019-Annual-Report (accessed October 2, 2020).
Busch, A. B., H. A. Huskamp, and J. M. McWilliams. 2016. Early efforts by Medicare accountable care organizations have limited effect on mental illness care and management. Health Affairs 35(7):1247–1256.
Camacho, E. M., L. M. Davies, M. Hann, N. Small, P. Bower, C. Chew-Graham, C. Baguely, L. Gask, C. M. Dickens, K. Lovell, W. Waheed, C. J. Gibbons, and P. Coventry. 2018. Long-term clinical and cost-effectiveness of collaborative care (versus usual care) for people with mental–physical multimorbidity: Cluster-randomised trial. The British Journal of Psychiatry 213(2):456–463.
Carlo, A. D., J. Unützer, A. D. H. Ratzliff, and J. M. Cerimele. 2018. Financing for collaborative care—A narrative review. Current Treatment Options in Psychiatry 5(3):334–344.
Carlo, A. D., A. Corage Baden, R. L. McCarty, and A. D. H. Ratzliff. 2019. Early health system experiences with collaborative care (COCM) billing codes: A qualitative study of leadership and support staff. Journal of General Internal Medicine 34(10):2150–2158.
Carlo, A. D., L. Drake, A. D. H. Ratzliff, D. Chang, and J. Unützer. 2020. Sustaining the collaborative care model (COCM): Billing newly available COCM CPT codes in an academic primary care system. Psychiatric Services. https://doi.org/10.1176/appi.ps.201900581.
CBHSQ (Center for Behavioral Health Statistics and Quality). 2015. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. HHS Publication No. SMA 15-4927, NSDUH Series H-50 SAMHSA. https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf (accessed October 26, 2020).
CDC (Centers for Disease Control and Prevention). 2020. Data and statistics on children’s mental health. https://www.cdc.gov/childrensmentalhealth/data.html (accessed October 2, 2020).
Chwastiak, L. A., S. L. Jackson, J. Russo, P. DeKeyser, M. Kiefer, B. Belyeu, K. Mertens, L. Chew, and E. Lin. 2017. A collaborative care team to integrate behavioral health care and treatment of poorly-controlled type 2 diabetes in an urban safety net primary care clinic. General Hospital Psychiatry 44:10–15. https://doi.org/10.1016/j.genhosppsych.2016.10.005.
CMM in Primary Care Research Team. 2018. The patient care process for delivering comprehensive medication management (CMM). Lenexa, KS: American College of Clinical Pharmacy.
CMS (Centers for Medicare & Medicaid Services). 2018. Opportunities to design innovative service delivery systems for adults with a serious mental illness or children with a serious emotional disturbance. SMD #18-011, Centers for Medicare & Medicaid Services. https://www.medicaid.gov/federal-policy-guidance/downloads/smd18011.pdf (accessed October 26, 2020).
Coventry, P., K. Lovell, C. Dickens, P. Bower, C. Chew-Graham, D. McElvenny, M. Hann, A. Cherrington, C. Garrett, C. J. Gibbons, C. Baguley, K. Roughley, I. Adeyemi, D. Reeves, W. Waheed, and L. Gask. 2015. Integrated primary care for patients with mental and physical multimorbidity: Cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. British Medical Journal 350:h638.
Coyne, J. C., S. Fechner-Bates, and T. L. Schwenk. 1994. Prevalence, nature, and comorbidity of depressive disorders in primary care. General Hospital Psychiatry 16(4):267–276.
Cross, D. A., X. Qin, P. Huckfeldt, S. Jarosek, H. Parsons, and E. Golberstein. 2019. Use of Medicare’s behavioral health integration service codes in the first two years: An observational study. Journal of General Internal Medicine. https://doi.org/10.1007/s11606-019-05579-2.
Cunningham, P. J. 2009. Beyond parity: Primary care physicians’ perspectives on access to mental health care. Health Affairs 28(Suppl 1):w490–w501.
Curth, N. K., U. Brinck-Claussen, K. B. Jørgensen, S. Rosendal, C. Hjorthøj, M. Nordentoft, and L. F. Eplov. 2019. Collaborative care vs. consultation liaison for depression and anxiety disorders in general practice: Study protocol for two randomized controlled trials (the Danish Collabri Flex trials). Trials 20(1):607.
D’Onofrio, G., P. G. O’Connor, M. V. Pantalon, M. C. Chawarski, S. H. Busch, P. H. Owens, S. L. Bernstein, and D. A. Fiellin. 2015. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. JAMA 313(16):1636–1644.
Drake, R. E., J. S. Skinner, G. R. Bond, and H. H. Goldman. 2009. Social Security and mental illness: Reducing disability with supported employment. Health Affairs 28(3):761–770.
Driessen, J., and Y. Zhang. 2017. Trends in the inclusion of mental health providers in Medicare shared savings program ACOs. Psychiatric Services 68(3):303–305.
Fiellin, D. A., R. S. Schottenfeld, C. J. Cutter, B. A. Moore, D. T. Barry, and P. G. O’Connor. 2014. Primary care–based buprenorphine taper vs. maintenance therapy for prescription opioid dependence: A randomized clinical trial. JAMA Internal Medicine 174(12):1947–1954.
GAO (U.S. Government Accountability Office). 2018. Report to congressional committees mental health leading practices state programs to certify peer support specialists. https://www.gao.gov/assets/700/695435.pdf (accessed October 2, 2020).
Garrison, G. M., K. B. Angstman, S. S. O’Connor, M. D. Williams, and T. W. Lineberry. 2016. Time to remission for depression with collaborative care management (CCM) in primary care. Journal of the American Board of Family Medicine 29(1):10–17.
Gillies, D., P. Buykx, A. G. Parker, and S. E. Hetrick. 2015. Consultation liaison in primary care for people with mental disorders. Cochrane Database of Systematic Reviews 2015(9):CD007193.
Ginsburg, A. D., P. S. Stadem, C. R. Takala, P. E. Croarkin, A. B. Mattson, M. L. Billings, R. M. Brennan, and J. E. Huxsahl. 2018. An examination of screening tools for collaborative care of adolescent depression. Journal of Clinical Psychiatry 79(4).
Gordon, S. Y. 2016. Integrating behavioral health into accountable care organizations: Challenges, successes, and failures at the federal and state levels. Alexandria, VA: National Association of State Mental Health Program Directors.
Green, L. A., and M. Cifuentes. 2015. Advancing care together by integrating primary care and behavioral health. The Journal of the American Board of Family Medicine 28(Suppl 1):S1.
Greenhalgh, T., G. Robert, F. Macfarlane, P. Bate, and O. Kyriakidou. 2004. Diffusion of innovations in service organizations: Systematic review and recommendations. The Milbank Quarterly 82(4):581–629.
Harman, J. S., P. J. Veazie, and J. M. Lyness. 2006. Primary care physician office visits for depression by older Americans. Journal of General Internal Medicine 21(9):926–930.
Hoge, M. A., J. A. Morris, M. Laraia, A. Pomerantz, and T. Farley. 2014. Core competencies for integrated behavioral health and primary care. Washington, DC: SAMHSA-HRSA Center for Integrated Solutions.
HRSA (Health Resources and Services Administration). 2019. Behavioral health workforce projections, 2017–2030. Rockville, MD: Health Resources and Services Administration.
ICSI (Institute for Clinical Systems Improvement). 2014. The DIAMOND program: Treatment for patients with depression in primary care. Bloomington, MN: Institute for Clinical Systems Improvement.
Insel, T. 2015. Collaborative care. In Post by Former NIMH Director Thomas Insel. Bethesda, MD: National Institute of Mental Health.
Jeffries, V., A. Slaunwhite, N. Wallace, M. Menear, J. Arndt, J. Dotchin, K. GermAnn, and S. Sapergia. 2013. Collaborative care for mental health and substance use issues in primary health care. Ottawa, Ontario: Mental Health Commission of Canada.
Kane, J. C., A. Sharma, L. K. Murray, G. Chander, T. Kanguya, M. E. Lasater, S. Skavenski, R. Paul, J. Mayeya, C. Kmett Danielson, J. Chipungu, C. Chitambi, and M. J. Vinikoor. 2020. Common elements treatment approach (CETA) for unhealthy alcohol use among persons with HIV in Zambia: Study protocol of the ZCAP randomized controlled trial. Addictive Behaviors Reports 12:100278.
Katon, W., and H. Schulberg. 1992. Epidemiology of depression in primary care. General Hospital Psychiatry 14(4):237–247.
Katon, W., M. Von Korff, E. Lin, E. Walker, G. E. Simon, T. Bush, P. Robinson, and J. Russo. 1995. Collaborative management to achieve treatment guidelines: Impact on depression in primary care. JAMA 273(13):1026–1031.
Kennedy-Hendricks, A., C. L. Barry, E. Stone, M. A. Bachhuber, and E. E. McGinty. 2020. Comparing perspectives on medication treatment for opioid use disorder between national samples of primary care trainee physicians and attending physicians. Drug and Alcohol Dependence 216:108217. https://doi.org/10.1016/j.drugalcdep.2020.108217.
KFF (Kaiser Family Foundation). 2019. Mental health care health professional shortage areas (HPSAS). https://www.kff.org/other/state-indicator/mental-health-care-health-professional-shortage-areas-hpsas/?activeTab=map¤tTimeframe=0&selectedDistributions=percent-of-need-met&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (accessed September 3, 2020).
Klein, S., and M. Hostetter. 2014. In focus: Integrating behavioral health and primary care. New York: The Commonwealth Fund.
Kuerbis, A., S. Armeli, F. Muench, and J. Morgenstern. 2014. Profiles of confidence and commitment to change as predictors of moderated drinking: A person-centered approach. Psychology of Addictive Behaviors 28(4):1065–1076.
Leung, M., C. Beadles, M. Romaire, and M. Gulledge. 2019. Multi-payer advanced primary care practice demonstration on quality of care. American Journal of Managed Care 25(9):444–449.
Loree, A. M., K. A. Yonkers, S. J. Ondersma, K. Gilstad-Hayden, and S. Martino. 2019. Comparing satisfaction, alliance and intervention components in electronically delivered and in-person brief interventions for substance use among childbearing-aged women. Journal of Substance Abuse Treatment 99:1–7.
Martino, S., S. J. Ondersma, A. Forray, T. A. Olmstead, K. Gilstad-Hayden, H. B. Howell, T. Kershaw, and K. A. Yonkers. 2018. A randomized controlled trial of screening and brief interventions for substance misuse in reproductive health. American Journal of Obstetrics and Gynecology 218(3):322.e1–322.e12.
McCance-Katz, E. F. 2018. The National Survey on Drug Use and Health: 2018. Rockville, MD: Substance Abuse and Mental Health Services Administration.
McGinty, E. E., and G. L. Daumit. 2020. Integrating mental health and addiction treatment into general medical care: The role of policy. Psychiatric Services. https://doi.org/10.1176/appi.ps.202000183.
McGinty, E. E., E. M. Stone, A. Kennedy-Hendricks, M. A. Bachhuber, and C. L. Barry. 2020. Medication for opioid use disorder: A national survey of primary care physicians. Annals of Internal Medicine 173(2):160–162.
McKnight-Eily, L. R., C. A. Okoro, K. Turay, C. Acero, and D. Hungerford. 2020. Screening for alcohol use and brief counseling of adults—13 states and the District of Columbia, 2017. Morbidity and Mortality Weekly Report 69(10):265–270.
McNeely, J., and R. Saitz. 2015. Appropriate screening for substance use disorder. JAMA Internal Medicine 175(12):1997–1998.
Meadows, G. N., C. A. Harvey, L. Joubert, D. Barton, and G. Bedi. 2007. Best practices: The consultation-liaison in primary-care psychiatry program: A structured approach to long-term collaboration. Psychiatric Services 58(8):1036–1038.
Mertens, J. R., F. W. Chi, C. M. Weisner, D. D. Satre, T. B. Ross, S. Allen, D. Pating, C. I. Campbell, Y. W. Lu, and S. A. Sterling. 2015. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: The ADVISe cluster randomized controlled implementation trial. Addiction Science & Clinical Practice 10:26.
Moore, M., S. Ali, B. Stuart, G. M. Leydon, J. Ovens, C. Goodall, and T. Kendrick. 2012. Depression management in primary care: An observational study of management changes related to PHQ-9 score for depression monitoring. British Journal of General Practice 62(599):e451–e457.
Morgenstern, J., A. Kuerbis, P. Amrhein, L. Hail, K. Lynch, and J. R. McKay. 2012. Motivational interviewing: A pilot test of active ingredients and mechanisms of change. Psychology of Addictive Behaviors 26(4):859–869.
Murray, L. K., S. Dorsey, E. Haroz, C. Lee, M. M. Alsiary, A. Haydary, W. M. Weiss, and P. Bolton. 2014. A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cognitive and Behavioral Practice 21(2):111–123.
Murray, L. K., B. J. Hall, S. Dorsey, A. M. Ugueto, E. S. Puffer, A. Sim, A. Ismael, J. Bass, C. Akiba, L. Lucid, J. Harrison, A. Erikson, and P. A. Bolton. 2018. An evaluation of a common elements treatment approach for youth in Somali refugee camps. Global Mental Health (Cambridge, England) 5:e16.
Murray, L. K., J. C. Kane, N. Glass, S. Skavenski van Wyk, F. Melendez, R. Paul, C. Kmett Danielson, S. M. Murray, J. Mayeya, F. Simenda, and P. Bolton. 2020. Effectiveness of the common elements treatment approach (CETA) in reducing intimate partner violence and hazardous alcohol use in Zambia (Vatu): A randomized controlled trial. PLoS Medicine 17(4):e1003056.
Muskin, P. R. 2017. A “new” model for consultation-liaison psychiatry. Focus (American Psychiatric Publishing) 15(4):7s–8s.
NAMI (National Alliance on Mental Illness). 2019. Mental health by the numbers. https://www.nami.org/mhstats (accessed June 18, 2020).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2019. Medications for opioid use disorder save lives. Washington, DC: The National Academies Press. https://doi.org/10.17226/25310.
NCBH (National Council for Behavioral Health). 2017. The psychiatric shortage: Causes and solutions. Washington, DC: National Council for Behavioral Health.
Neville, C. 2015. Collaborative care approaches for people with severe mental illness. Clinical Nurse Specialist 29(3).
NIDA (National Institute on Drug Abuse). 2010. Comorbidity: Addiction and other mental illnesses. Rockville, MD: National Institute on Drug Abuse.
NIMH (National Institute of Mental Health). 2017. Mental illness. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml (accessed August 10, 2020).
NRC and IOM (National Research Council and Institute of Medicine). 2004. Children’s health, the nation’s wealth: Assessing and improving child health. Washington, DC: The National Academies Press.
O’Donnell, A. N., B. C. Williams, D. Eisenberg, and A. M. Kilbourne. 2013. Mental health in ACOs: Missed opportunities and low-hanging fruit. American Journal of Managed Care 19(3):180–184.
Olmstead, T. A., K. A. Yonkers, S. J. Ondersma, A. Forray, K. Gilstad-Hayden, and S. Martino. 2019. Cost-effectiveness of electronic- and clinician-delivered screening, brief intervention and referral to treatment for women in reproductive health centers. Addiction 114(9):1659–1669.
Ondersma, S. J., D. S. Svikis, L. R. Thacker, J. R. Beatty, and N. Lockhart. 2014. Computer-delivered screening and brief intervention (e-SBI) for postpartum drug use: A randomized trial. Journal of Substance Abuse Treatment 46(1):52–59.
Ondersma, S. J., J. R. Beatty, D. S. Svikis, R. C. Strickler, G. K. Tzilos, G. Chang, G. W. Divine, A. R. Taylor, and R. J. Sokol. 2015. Computer-delivered screening and brief intervention for alcohol use in pregnancy: A pilot randomized trial. Alcoholism, Clinical and Experimental Research 39(7):1219–1226.
Palzes, V. A., C. Weisner, F. W. Chi, A. H. Kline-Simon, D. D. Satre, M. E. Hirschtritt, M. Ghadiali, and S. Sterling. 2020. The Kaiser Permanente Northern California Adult Alcohol Registry, an electronic health records-based registry of patients with alcohol problems: Development and implementation. JMIR Medical Informatics 8(7):e19081. doi: 10.2196/19081.
Peikes, D., G. Anglin, S. Dale, E. F. Taylor, A. O’Malley, A. Ghosh, K. Swankoski, J. Crosson, R. Keith, A. Mutti, S. Hoag, P. Singh, H. Tu, T. Grannemann, M. Finucane, A. Zutshi, L. Vollmer, and R. Brown. 2018. Evaluation of the comprehensive primary care initiative: Fourth annual report. Princeton, NJ: Mathematica Policy Research.
Pence, B. W., J. K. O’Donnell, and B. N. Gaynes. 2012. The depression treatment cascade in primary care: A public health perspective. Current Psychiatry Reports 14(4):328–335.
Petterson, S., B. F. Miller, J. C. Payne-Murphy, and R. L. Phillips. 2014. Mental health treatment in the primary care setting: Patterns and pathways. Family, Systems & Health 32(2):157–166.
Plsek, P. 2003. Complexity and the adoption of innovation in health care. Paper presented at Accelerating Quality Improvement in Health Care Strategies to Speed the Diffusion of Evidence-Based Innovations, Washington, DC.
Polak, A. M., D. Smith, G. William, and F. de Brantes. 2018. The addiction recovery medical home as an alternative payment model. In Health Affairs Blog. Bethesda, MD: Health Affairs.
Ramsey, A. T., J. M. Satterfield, D. R. Gerke, and E. K. Proctor. 2019. Technology-based alcohol interventions in primary care: Systematic review. Journal of Medical Internet Research 21(4):e10859.
Regier, D. A., W. E. Narrow, D. S. Rae, R. W. Manderscheid, B. Z. Locke, and F. K. Goodwin. 1993. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry 50(2):85–94.
Reilly, S., C. Planner, L. Gask, M. Hann, S. Knowles, B. Druss, and H. Lester. 2013. Collaborative care approaches for people with severe mental illness. Cochrane Database of Systematic Reviews (11):CD009531.
Reiss-Brennan, B., K. D. Brunisholz, C. Dredge, P. Briot, K. Grazier, A. Wilcox, L. Savitz, and B. James. 2016. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 316(8):826–834.
Roberts, N. P., P. S. Roberts, N. Jones, and J. I. Bisson. 2015. Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review 38:25–38.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2013. Systems-level implementation of screening, brief intervention, and referral to treatment. Rockville, MD: Substance Abuse and Mental Health Services Administration.
SAMHSA. 2020. Common comorbidities. https://www.samhsa.gov/medication-assisted-treatment/treatment/common-comorbidities (accessed August 10, 2020).
Schulberg, H. C., M. J. Madonia, M. R. Block, J. L. Coulehan, C. P. Scott, E. Rodriguez, and A. Black. 1995. Major depression in primary care practice: Clinical characteristics and treatment implications. Psychosomatics 36(2):129–137.
Schwenk, T. L. 2016. Integrated behavioral and primary care: What is the real cost? JAMA 316(8):822–823.
Simon, G. 2006. Collaborative care for depression. BMJ 332(7536):249–250.
Smith, P. C., S. M. Schmidt, D. Allensworth-Davies, and R. Saitz. 2009. Primary care validation of a single-question alcohol screening test. Journal of General Internal Medicine 24(7):783–788.
Solberg, L. I., A. L. Crain, N. Jaeckels, K. A. Ohnsorg, K. L. Margolis, A. Beck, R. R. Whitebird, R. C. Rossom, B. F. Crabtree, and A. H. Van de Ven. 2013. The DIAMOND initiative: Implementing collaborative care for depression in 75 primary care clinics. Implementation Science 8:135.
St. Louis, J., A. R. Eden, Z. J. Morgan, T. W. Barreto, L. E. Peterson, and R. L. Phillips. 2020. Maternity care and buprenorphine prescribing in new family physicians. The Annals of Family Medicine (2):156–158. https://doi.org/10.1370/afm.2504.
Starfield, B. 2001. New paradigms for quality in primary care. The British Journal of General Practice: The Journal of the Royal College of General Practitioners 51(465):303–309.
Sterling, S. A., V. A. Palzes, Y. Lu, A. H. Kline-Simon, S. Parthasarathy, T. Ross, J. Elson, C. Weisner, C. Maxim, and F. W. Chi. 2020. Associations between medical conditions and alcohol consumption levels in an adult primary care population. JAMA Network Open 3(5):e204687. doi: 10.1001/jamanetworkopen.2020.4687.
Stille, C., R. M. Turchi, R. Antonelli, M. D. Cabana, T. L. Cheng, D. Laraque, and J. Perrin. 2010. The family-centered medical home: Specific considerations for child health research and policy. Academic Pediatrics 10(4):211–217.
Storholm, E. D., A. J. Ober, B. J. Hunter, K. M. Becker, P. O. Iyiewuare, C. Pham, and K. E. Watkins. 2017. Barriers to integrating the continuum of care for opioid and alcohol use disorders in primary care: A qualitative longitudinal study. Journal of Substance Abuse Treatment 83:45–54.
Straus, J. H., and B. Sarvet. 2014. Behavioral health care for children: The Massachusetts Child Psychiatry Access Project. Health Affairs 33(12):2153–2161.
Tiet, Q. Q., Y. E. Leyva, R. H. Moos, S. M. Frayne, L. Osterberg, and B. Smith. 2015. Screen of drug use: Diagnostic accuracy of a new brief tool for primary care. JAMA Internal Medicine 175(8):1371–1377.
Tucker, J. A., J. Cheong, T. G. James, S. Jung, and S. D. Chandler. 2020. Preresolution drinking problem severity profiles associated with stable moderation outcomes of natural recovery attempts. Alcoholism: Clinical and Experimental Research 44(3):738–745.
Unützer, J., and M. Park. 2012. Strategies to improve the management of depression in primary care. Primary Care: Clinics in Office Practice 39(2):415–431.
Unützer, J., W. Katon, C. M. Callahan, J. Williams, J. W. E. Hunkeler, L. Harpole, M. Hoffing, R. D. Della Penna, P. H. Noël, E. H. B. Lin, P. A. Areán, M. T. Hegel, L. Tang, T. R. Belin, S. Oishi, and C. Langston. 2002. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA 288(22):2836–2845.
van Beurden, I., P. Anderson, R. P. Akkermans, R. P. Grol, M. Wensing, and M. G. Laurant. 2012. Involvement of general practitioners in managing alcohol problems: A randomized controlled trial of a tailored improvement programme. Addiction 107(9):1601–1611.
Waddington, C., D. Egger, and WHO Working Group on Service Delivery. 2008. Integrated health services—What and why? Geneva, Switzerland: World Health Organization.
Wagner, E. H., B. T. Austin, and M. Von Korff. 1996. Organizing care for patients with chronic illness. Milbank Quarterly 74(4):511–544.
Wakeman, S. E., N. A. Rigotti, Y. Chang, G. E. Herman, A. Erwin, S. Regan, and J. P. Metlay. 2019. Effect of integrating substance use disorder treatment into primary care on inpatient and emergency department utilization. Journal of General Internal Medicine 34(6):871–877.
Walker, E. R., R. E. McGee, and B. G. Druss. 2015. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 72:334–341.
WHO (World Health Organization). 2015. Meeting report on excess mortality in persons with severe mental disorders. Geneva, Switzerland: World Health Organization.
Wiktorowicz, M., A. Abdulle, K. Di Pierdomenico, and S. A. Boamah. 2019. Models of concurrent disorder service: Policy, coordination, and access to care. Frontiers in Psychiatry 10:61.
Wisdom, J. P., K. H. B. Chor, K. E. Hoagwood, and S. M. Horwitz. 2014. Innovation adoption: A review of theories and constructs. Administration and Policy in Mental Health and Mental Health Services Research 41(4):480–502.
Xiang, X., R. Owen, F. Langi, K. Yamaki, D. Mitchell, T. Heller, A. Karmarkar, D. French, and N. Jordan. 2019. Impacts of an integrated Medicaid managed care program for adults with behavioral health conditions: The experience of Illinois. Administration and Policy in Mental Health 46(1):44–53.
Yarnall, K. S., K. I. Pollak, T. Østbye, K. M. Krause, and J. L. Michener. 2003. Primary care: Is there enough time for prevention? American Journal of Public Health 93(4):635–641.
Yonkers, K. A., J. I. Dailey, K. Gilstad-Hayden, S. J. Ondersma, A. Forray, T. A. Olmstead, and S. Martino. 2020. Abstinence outcomes among women in reproductive health centers administered clinician or electronic brief interventions. Journal of Substance Abuse Treatment 113:107995.




























































































