4
Respiratory Risks and User Requirements for the Public
Nontraditional respirator user populations—that is, workers who perform duties outside of a formal respiratory protection program or members of the public—face situation-specific risks that may require respiratory protection despite the absence of a formal respiratory protection program. In a session moderated by planning committee member John Balmes of the University of California, San Francisco, three workshop speakers discussed the risks encountered by members of the public among these user groups and examined how situation-specific needs and respiratory risks align with existing recommendations, guidance, and standards.
NON-OCCUPATIONAL RESPIRATOR USE AT U.S. EMBASSIES AND CONSULATES
Claire Huson, an industrial hygienist at the Department of State, said that the Department of State has more than 270 diplomatic posts around the world. The Department of State promotes peace and stability in areas of vital national interest and provides services for U.S. citizens and government employees traveling abroad, including providing passports and visas to foreigners seeking to visit the United States. When abroad, U.S. government employees and their families living in areas with high levels of air pollution often require respiratory protection outside of their workplaces—for example, when commuting to work or school. This population’s use of respiratory protection is voluntary, but the decision whether to use respiratory protection is often made with input from the Department of State. Because members of this population may influence others through their
decisions and practices regarding respirator protection use, Huson said, it is important to the Department of State that members of this population set a good example in terms of using respiratory protective devices (RPDs). For instance, U.S. employees and their families may influence the behaviors of locally engaged staff at embassies and consulates, locally employed staff and their family members, and residents of host nations.
Respiratory Protection Use Scenarios
Severe air pollution is the primary reason that families overseas choose to wear some form of respiratory protection, Huson said. Severe pollution affects more than half of the Department of State posts around the world. The average PM2.51 level in those settings is worse than the areas with the worst pollution in the United States, and in some settings the average PM2.5 level is as much as three times higher than the most polluted areas of the United States. Additionally, families may choose to use respiratory protection due to vegetative fires, volcanic eruptions, and pandemic influenza. For instance, Huson said that in 2019 wildfires in Australia had an impact on the air quality at the Department of State posts in that country, sharing two photographs of a city landscape to illustrate the severity of pollution in certain settings. In the first image air pollution has made it impossible to see the city landscape in the photograph. At the time the photograph was taken, the Air Quality Index (AQI) was 370, which falls under the Environmental Protection Agency’s (EPA’s) designation of hazardous. In the second photograph, which was taken on the following day, the city landscape is visible, and the air appears to be much clearer. However, at the time the second photograph was taken, the AQI was 154, which falls under EPA’s designation of unhealthy. Huson said that Department of State employees often report that while they were aware of air quality issues in their host countries prior to moving, they were surprised by the amount of air pollution once they arrived. Some U.S. government employees have become extremely concerned and are eager to find ways to protect themselves and their families. For example, many people overseas use a variety of negative-pressure-type air-purifying respirators for particulate filtration is common. Huson said that the Department of State discourages purchasing cloth facial coverings from sidewalk vendors. If travelers decide to seek out an RPD, then the Department of State advises them on which respiratory protections
___________________
1 The Environmental Protection Agency has developed ambient air quality trends for particle pollution, also called particulate matter (PM). PM2.5 describes fine inhalable particles with diameters that are generally 2.5 micrometers and smaller. More information about PM2.5 trends is available from https://www.epa.gov/air-trends/particulate-matter-pm25-trends (accessed September 15, 2020).
might work best. They also advise people to consider whether they may be putting themselves at risk by wearing respirators (e.g., through risks associated with pre-existing medical conditions).
The Department of State’s Considerations for Recommending Respiratory Protective Devices
Ideally, air-purifying particulate respiratory devices should offer consistent and effective protection, Huson said. She explained that, in addition to guidance on whether the use of a facial covering is medically acceptable for individuals, the Department of State offers guidance on filtration quality, fit, and proper use. Other considerations for air pollution respiratory devices include comfort, portability, availability in sizes that fit children, the use of ear loops versus head straps, cleanability, and cost. She added that many aspects of the currently available information about respiratory devices can cause confusion, such as devices marked as “not for industrial use,” “HEPA [high-efficiency particulate air]-type,” or “shows conformance to U.S. standards in testing.” Additionally, there may be confusion about persons with beards wearing respiratory devices. The Department of State recommends that travelers find reusable respirators approved by the National Institute for Occupational Safety and Health (NIOSH). If none is available, it advises travelers to seek other hallmarks of quality. Huson said that travelers often find lightweight, portable cloth facial coverings, which Huson and her colleagues refer to as “air pollution masks.” These facial coverings are desirable for many travelers because they are lightweight, low profile, reusable, and somewhat cleanable. However, none of these air pollution masks is NIOSH-approved. Huson added that should such a pollution mask attain NIOSH approval, it would be encouraging for those deployed overseas seeking protection from air pollution. She explained that her office is only comfortable recommending NIOSH-certified RPDs. She reported that one of her colleagues has located an elastomeric, low-profile N95 respirator and has encouraged travelers to use it; however, they have not yet received feedback on this device.
Health Indications, Pre-Existing Conditions, and Respirator Use
Huson said that for the Department of State, the first considerations for respirator use are an individual’s health indications and pre-existing conditions, including physiological effects such as pulmonary concerns, cardiac issues, claustrophobia, anxiety, hyperventilation, and heat stress risks, which can be exacerbated when using a respirator. Potential contraindications that make wearing a mask inadvisable include severe pulmonary disease, severe cardiac disease, uncontrolled hypertension, claustrophobia,
and facial abnormalities that prevent good fit. There are additional concerns regarding respiratory protection for children. Children are not merely “little adults,” she noted. Children may benefit from respirators, but they may also face greater risks associated with them. For example, sensitive individuals—such as children with asthma—may have the greatest need for respiratory protection, but use of a respirator may pose the biggest challenge with respect to medical provider concurrence.
Huson said the Department of State’s medical staff need clear, consistent, evidence-based guidance to inform their decisions and assist them in making recommendations to medical professionals and parents. She specifically mentioned a need for more research to address liability concerns and to create a risk-benefit analysis of respirator use. Furthermore, the department requires guidance for identifying the appropriate respirator types for various challenging situations (e.g., lower-resistance models, carbon dioxide) and for offering specific advice for populations that are especially sensitive to air pollution. Differentiated approaches may be required for routine use and emergency situations. Where individuals are entering settings with chronic air pollution, Huson said, they need to be prepared in advance. People need to be able to distinguish between the warning signs of problems caused by respirators and those caused by exposure hazards. Finally, Huson emphasized the need to highlight and prioritize other exposure reduction strategies.
Leak Checking Air Pollution Masks
Huson said that to address issues regarding the fit of employees’ air pollution masks, the Department of State conducts “leak checks” by having people put on their chosen device and performing a leak challenge test. She said that this procedure is not as rigorous of a fit test as those conducted according to the standards of the Occupational Safety and Health Administration (OSHA). However, the Department of State has found high device failure rates when using this leak-check method, even for devices that people considered to be of high quality (see Figure 4-1). She noted that this can be upsetting for people who believed they had been wearing a high-quality device in outdoor environments with severe air pollution but found out that it had not afforded them the protection they expected.
Respiratory Protection Devices: Considerations and Potential Ways Forward
Huson formatted her presentation around the use of RPDs among Department of State employees and their families who are posted abroad. The major considerations are whether respiratory protection is even needed
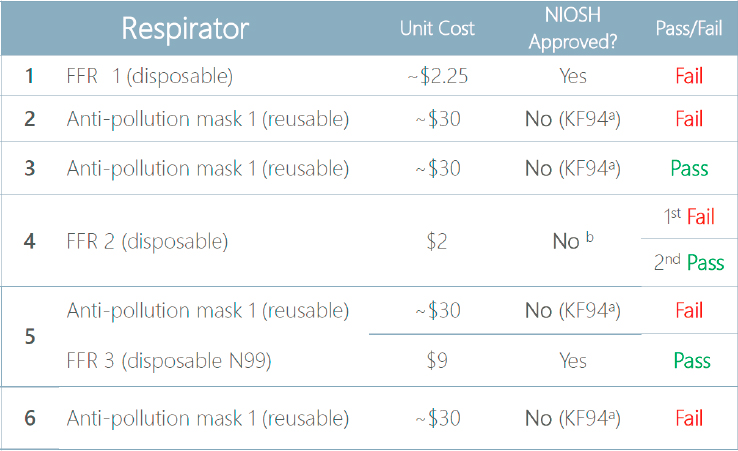
NOTE: FFR = filtering facepiece respirator; NIOSH = National Institute for Occupational Safety and Health. a Korean standard, 94% efficient. b U.S. brand.
SOURCE: Huson presentation, August 5, 2020.
for this population and, if so, when it is needed and what the mechanism should be for triggering the use of RPDs.
Regarding the first consideration, Huson suggested that RPDs will likely be necessary in light of the 2019 decision by the California Occupational Safety and Health Administration (Cal/OSHA) to establish an emergency regulation on protection from wildfire smoke to address the concerns regarding workers’ exposure to smoke, ash, and poor air quality. Huson said that conditions abroad are often worse than California’s established threshold AQI for PM2.5 of 151 for 1 hour or longer.2 Further needs include a more detailed understanding of medical indications and contraindications for using RPDs and for a more consistent vocabulary for
___________________
2 Under Cal/OSHA’s emergency regulation on protection from wildfire smoke, if the AQI for PM2.5 exceeds 151, employers are required to allow for voluntary respiratory protection, following all applicable OSHA guidelines. More information about Cal/OSHA’s emergency regulation on protection from wildfire smoke is available from https://www.dir.ca.gov/dosh/doshreg/Protection-from-Wildfire-Smoke/Wildfire-smoke-emergency-standard.html (accessed August 14, 2020) and in Chapter 3.
explaining the issues around RPD selection and use. Additionally, a greater variety of sizes or an improvement in universal fit of RPDs is needed; the affordability and availability of the devices are key concerns as well. Huson said out that air pollution masks are somewhat expensive—costing approximately $50 per year—and that any necessary replacement parts must be readily available. To improve the clarity and detail of information provided to consumers about RPDs and other devices like air pollution masks, she suggested adopting a protection-factor system and conveying information about breathing resistance from the RPD itself. User acceptance, Huson said, is determined by factors such as aesthetics, comfort, and convenience; these considerations are critical for developing persuasive messaging that convinces people to use RPDs. The devices should feature an adequate filter, Huson said, with appropriate fit and seal every time they are worn, and would benefit from an easy-to-conduct seal check procedure. Huson specified that these devices must be available in sizes that also fit children and various facial features, with sizes that are consistent to accommodate online ordering. These devices, she added, should be also be cleanable and last for at least 6 months of regular use. Huson said all of these design and use considerations contribute to preventing the false sense of protection that many of these overseas employees have regarding the effectiveness of their devices. Huson closed by remarking that the ideal scenario would be to entirely eliminate the use of RPDs by eradicating the exposure hazards that make them necessary.
RESPIRATORY PROTECTION IN CHILDREN AND ADULTS
In her presentation, Stephanie Holm, the co-director of the Western States Pediatric Environmental Health Specialty Unit, explored considerations related to respiratory protection in children. She opened by explaining why protecting the respiratory health of children should be at the forefront of the discussion of respiratory protection for the general public. Children tend to be more vulnerable to respiratory hazards than adults because children often spend more time outdoors and more time exercising, which increases their breathing rate and can cause them to take in more airborne pollutants. Even when children are not exercising, their physiological characteristics make them more vulnerable to respiratory hazards. For instance, due to their higher rate of ventilation per kilogram of body weight, children breathe in a greater volume of air and thus a greater volume of airborne irritants than adults. Additionally, Holm said, changes that occur during developmental windows in early childhood can have lifelong effects. For example, evidence suggests that children with lower lung function become adolescents and adults with lower lung function.
Mask Filtration and Leakage
Discussions about the use of masks and respirators for individual respiratory protection, such as during wildfire smoke events, should focus on protection for the wearer, Holm said. Filtration and leakage are two primary considerations. Filtration refers to the proportion of particles that pass through the material of the mask or respirator and the decrease in particles after moving through the material. Leakage refers to the number of particles that can pass around the mask or respirator. Holm provided an overview of some of the characteristics of and evidence for cloth and medical masks.
Cloth Masks
Cloth masks have increasingly become a topic of interest because of their potential to decrease transmission of infectious droplets. However, Holm said, when they have been tested for use against particulate pollution, studies have found them to have a broad range of filtration properties depending on the category and type of fabric. Thus, the original source or application of a fabric (i.e., a t-shirt, hijab, scarf, or sweatshirt) is not indicative of the filtration characteristics of that material because most fabrics are not designed to optimize filtration characteristics, Holm said. Notably, cloth masks made with certain fabrics have been found to “pool particles” in such a way that it creates higher PM2.5 concentrations inside the mask (Shakya et al., 2017). In other cases—for example, for bandanas and some commercially available cloth masks—the decrease in exposure is as low as 10 percent due to poor filtration and leakage, which is a small and highly unpredictable decrease (Bowen, 2010; Oberg and Brosseau, 2008; Rengasamy et al., 2010; Shakya et al., 2017). For that reason, even though cloth masks are currently recommended for decreasing the droplet transmission of viruses, they should not be relied on to decrease exposure in the case of particulate pollution, Holm said.
Medical Masks
Medical masks, or surgical masks, are designed to prevent surgeons from contaminating the surgical field with droplets, not specifically for respiratory protection, Holm said. However, because these masks are somewhat regulated, they may offer some degree of respiratory protection. Multiple studies have tested medical and surgical masks specifically for filtration by looking at the characteristics of the materials, which have been found to filter 60–80 percent of particles (Jung et al., 2014; Langrish et al., 2009; Oberg and Brosseau, 2008). That range is wide because filtration is
not the intended purpose of these materials, she explained. Because medical masks do not fit tightly over the face like a respirator, these masks allow for substantial leakage around the mask perimeter. In NIOSH testing, the mean decreases in particulate exposure were between 15 and 40 percent (Oberg and Brosseau, 2008). Other groups have found average decreases in exposure of between 33 and 60 percent (Bowen, 2010; Duling et al., 2007; Grinshpun et al., 2009). Holm said, the only study that has tested medical masks specifically in children (a small sample of 11) found that medical masks decreased children’s exposure by 66 percent or more, which is similar to the findings for adults (van der Sande et al., 2008). Notably, the researchers in that study helped the children secure their masks tightly to their faces, which likely helped to ensure a good seal. This suggests that children could be expected to get roughly similar protection from medical masks as adults as long as the mask is well fitting, Holm said.
Filtering Facepiece Respirator Use by the General Public
Next, Holm discussed the general public’s use of filtering facepiece respirators (FFRs). A major consideration is that when these respirators are used by the general public—unlike in an occupational setting—they are not fit tested. No regulatory body is currently tasked with making decisions or certifications of respirators for the general public. In 2007 a NIOSH study found that without fit testing, the 95th percentile value for the class of FFR was a reduction in exposure of 70 percent or more (Duling et al., 2007). Holm said that some products would meet the criterion for occupational use even without fit testing (meaning that they achieve a protection factor of 10, or a 90 percent reduction in exposure in 95 percent of users). This suggests that in the future, Holm said, there could be products certified for the general public that have more stringent requirements for how much reduction of an exposure is required in the absence of fit testing.
Furthermore, Holm said, data suggest that some respiratory protection for the public user is possible when using respirators without the implementation of a respiratory protection program. Historically, respiratory protection programs have been key for ensuring respiratory protection in occupational settings. Holm said that although it is difficult to envision how a respiratory protection program could be implemented for the general public, it is important to acknowledge that some protection is still available to the public even in the absence of such programs. Several studies have found beneficial health effects for adults who wear N95 respirators in the presence of particulate pollution. These effects include having less airway inflammation (Guan et al., 2018), lower systolic blood pressure (Langrish et al., 2009), and fewer symptoms and improved short-term indicators of cardiovascular health among adults with cardiovascular disease (Langrish
et al., 2012). Holm said, only two studies have evaluated the use of N95 respirators among children. The aforementioned study evaluated the use of N953 respirators among 11 Dutch children ages 5–11 and found a decrease in exposure of 92–97 percent (van der Sande et al., 2008). Holm reiterated that children were given assistance in donning and securing their respirators in this study. Another study of 106 children in Singapore found that it was possible to achieve a quantitative mask fit with an N95 respirator designed for children (Goh et al., 2019). Additionally, Holm said, 3M has reported that it has propriety data on the use of N95 respirators among children. It has reported that (1) many children fall on the NIOSH adult grid for face size, (2) when using an adult small respirator most children’s exposure is reduced by greater than 80 percent, and (3) potential further reductions in exposure will be possible with a respirator designed specifically for children. While these claims are based on unpublished proprietary data, Holm suggested that regulatory standards for respirators for children could facilitate further reductions in exposure.
Public Concerns About Mask and Respirator Use
Holm highlighted some common concerns raised about the use of masks and respirators among the general public. Many people are concerned that the use of respiratory protection by the general public, specifically by children, could create a false sense of security and promote riskier behavioral choices. Holm said this concern highlights the need for clear communication to help people understand that (1) masks and respirators reduce—but do not eliminate—pollution or particulate exposure, (2) devices provide the best protection when they are used correctly, and (3) these devices should only be considered in the context of other preparedness options. For example, Holm said, preparation for wildfires should include plans to improve the quality of indoor air.
Safety is another area of concern related to the use of masks and respirators by the general public. Holm said that most safety research has evaluated the use of these devices among adults and generally has found subjective physical changes, including the experiences of discomfort, heat around the face, and anxiety. However, physiological parameters such as heart rate, respiratory rate, and blood pressure change only slightly, if at all, and typically stay within normal ranges for healthy adults. One study of 10 young men found a slight increase in facial temperature and a slight increase in respiratory rate (Jones, 1991). Another study of adults found no physiological changes after adults spent 1 hour on a treadmill wearing
___________________
3 In this study, researchers used NFP2 respirators, which are the European equivalent of N95 respirators.
respirators with different pressure drops (Roberge et al., 2013). A study that evaluated 10 health care workers found no physiologic changes after 1 hour on a treadmill in subjects wearing an N95 respirator versus subjects not wearing one (Roberge et al., 2010). A study evaluating 10 nurses found no change in blood pressure or SpO24 after wearing an N95 respirator for 12 hours, although PCO25 did increase slightly (Rebmann et al., 2013). In an evaluation of the use of respirators in a general population cohort that included individuals with mild respiratory disease, some subjects reported mild discomfort, but heart rate, respiratory rate, and spirometry were found to be within normal adult ranges (Bansal et al., 2009; Harber et al., 2009). Another study assessed the effects of respirator use among children while reading and while exercising on a treadmill for 3 minutes (Goh et al., 2019). The only difference found when children wore N95 respirators compared to when they did not is that they had slightly higher end-tidal carbon dioxide (CO2), which is used as a marker of metabolic work. While the end-tidal CO2 among those wearing N95 respirators was slightly higher, the ranges of those wearing N95 respirators overlapped with those not wearing N95 respirators. Holm added that data on the effects of respirators on pregnant people are mixed but that the use of an N95 respirator by pregnant women has not been found to have an effect on fetal heartrate (Roberge et al., 2014).
Holm said that these data suggest that respirator use is safe, both for the general public and for children. However, she cautioned that certain children should not use face coverings. These include young children under the age of 2,6 children who are unable to remove a face covering on their own, children who have difficulty breathing while wearing a face covering, and children for whom the only available face covering is a possible choking or strangulation hazard. Additionally, Holm said, respirators should generally be used only by individuals who would be able to effectively communicate if they experience a problem while wearing a respirator. Holm said that while feeling hot or uncomfortable is normal, if an individual wearing a respirator has trouble breathing, he or she should take off the respirator. Holm reiterated that there are benefits that can be realized by
___________________
4 SpO2 is a measurement of how much oxygen your blood is carrying as a percentage of the maximum it could carry.
5 PCO2 is the partial pressure of carbon dioxide that is the measure of carbon dioxide within arterial or venous blood.
6 Centers for Disease Control and Prevention (CDC) recommendations advise against the use of masks by children under the age of 2 or anyone who has trouble breathing, is unconscious, incapacitated, or otherwise unable to remove the mask without assistance. More information about CDC recommendations for wearing masks is available from https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html (accessed August 20, 2020).
the use of RPDs by the general public, even in the absence of a respiratory protective program, and that the perfect should not be the enemy of the good. She maintained that the public should be offered available devices with clarity about the amount of protection the devices provide so that individuals can make their own decisions.
IMPROVING MASKS WORN BY THE GENERAL PUBLIC
Mark Nicas, an emeritus adjunct professor at the University of California, Berkeley, focused on ways to improve the masks worn by the general public and offered four recommendations to do so. He explained that any face covering worn for the purpose of reducing the wearer’s pollutant exposure—including NIOSH-approved N95 FFRs, surgical masks, cloth masks, or bandanas—is a form of respiratory protection. However, certain face coverings—including bandanas, cloth masks, and most surgical masks—do not qualify as “respirators” within the domain of occupational hygiene and in terms of compliance with OSHA standards because those face coverings permit excessive pollutant penetration and are not tested and certified by NIOSH. Nicas compared the appearance and function of NIOSH-approved N95 FFRs with that of a conventional cloth mask. NIOSH-approved N95 FFRs have two straps that wrap around the user’s head to secure the device, while cloth masks typically rely on ear loops, which provide a less snug fit. He said that these two devices also offer very different levels of protection for the wearer. A well-fitting N95 FFR might allow 5 percent particle penetration, while a cloth mask may permit 50 percent particle penetration. Bandanas permit nearly 100 percent particle penetration. He remarked that during his presentation he would primarily focus on the use of cloth masks by the public, but that the ideas discussed pertain to other RPDs as well.
Increasing the Production of N95 Filtering Facepiece Respirators
Nicas’s first suggestion was to substantially increase the manufacturing of N95 FFRs so that these devices will be available to the general public without causing shortages in workplace settings. The rationale is that N95 FFRs are far superior to cloth masks in terms of respiratory protection for the wearer. Particulate pollutants are a key concern for the public and are related both to wildfire smoke and infectious viruses, as are concerns related to exposure to gaseous pollutants. Cloth masks can only remove some particulates; by contrast, FFRs more efficiently remove these particulate pollutants, and some FFRs incorporate sorbents that can remove certain gases and vapors. Small wildfire smoke particles are less than 2.5 microns in diameter, and a virus carried by particles emitted from
the respiratory tract may be up to 10 microns in diameter. Particles smaller than 10 microns can penetrate down to the end air sacs in the lungs. Nicas explained that the penetration of pollutant particles into a mask without an exhalation valve may occur in two ways: through the filter itself and through gaps around the mask perimeter. Masks with exhalation valves (see Chapter 6 for image reference) may provide a third route for particle penetration through a poorly sealed exhalation valve. Different filter materials allow particles to penetrate to different degrees—that is, different filter materials remove particles with different efficiencies. The various materials used to make cloth masks have varying filtering capacities, he added. For instance, some cloth filter materials may be greater than 99 percent efficient in removing 10-micron particles but only 25 percent efficient in removing 1-micron particles. Such a filter material would be suitable for filtering pollen grains, but not for filtering wildfire smoke.
For any mask, determining overall filter efficiency requires testing the filter against a range of particle sizes, Nicas said. However, this type of testing has been conducted for only a few cloth masks. Furthermore, different masks will fit the same individual’s face differently, and the same mask will fit different individuals’ faces differently. Nicas said achieving a good mask fit is comparable to finding a well-fitting shoe. Nicas explained that an individual who wears a size 9 shoe cannot expect all size 9 shoes to fit equally well, and the shoe that best fits such an individual will not necessarily be the shoe that best fits all individuals who wear size 9 shoes. Furthermore, the looser the fit of any mask, the more gaps exist around the mask perimeter. In turn, more unfiltered air will enter that mask through these gaps. Nicas said that whenever large openings can be seen on the sides of a cloth mask, the wearer is likely experiencing significant inward air leakage. A mask with two head straps is likely to fit more snugly than a mask with ear loops. The fit of a mask to a person’s face can be quantitatively measured by quantifying the filter penetration, which involves measuring the degree of unfiltered inward air leakage permitted by a cloth mask while simultaneously accounting for the degree of test particle penetration through the filter. Again, he added, this type of testing has seldom been conducted on cloth masks.
Formulating Standard Protocols for Cloth Mask Testing
Nicas’s second recommendation to improve masks worn by the general public was for a government agency or a professional or academic group to oversee the formulation of standard protocols for testing filter efficiency and fit, including exhalation valve leakage, of cloth masks. If a government agency tested the masks—or funded a group to do the testing—then the results could be posted publicly so that consumers could compare mask
performance, he said. While NIOSH might be the government agency with the most appropriate technical expertise, the evaluation of masks for the general public is outside of NIOSH’s mandate. The Food and Drug Administration (FDA) may be the appropriate agency to carry out such testing in terms of agency purview, he suggested.
Nicas explained that, according to OSHA standards, workers must first pass a “fit test” to ensure that the fit of the respirator is adequate before they are assigned an N95 FFR for use. In fit testing, the N95 FFR wearer is exposed to a challenge aerosol. The N95 FFR filter is very efficient in removing the challenge particles, so if too much of the challenge aerosol is detected inside the N95 FFR, it is concluded that the mask perimeter leakage is excessive. Nicas said that most cloth masks would not pass the fit tests that are used to test the fit of N95 FFRs due to both the looser fit of typical cloth masks and the lower filter efficiency against challenge particles of most cloth masks. In addition to fit testing, OSHA standards require a seal check whenever a successfully fitted N95 FFR is donned. Upon donning an N95 FFR, the wearer is supposed to do a quick seal check of the N95 FFR for excessive air leakage around the perimeter. Nicas expressed concern that the current method of conducting seal checks of FFRs is not reliable and said that it would be useful to offer wearers a more reliable method.
Devising Fit- and Seal-Checking Procedures for Snugly Fitting Cloth Masks
Nicas’s third recommendation was for a government agency or professional or academic group to devise both fit-testing and seal-checking procedures specific for snugly fitting cloth masks for use by the public, such as those equipped with head straps. The materials and equipment involved in such procedures would need to be both easy to use and inexpensive so that the procedures could be employed by the general public.
Studying Levels of Carbon Dioxide Gas Inhaled with Different Types of Masks
Nicas’s final recommendation addressed the concern of some wearers of cloth masks, surgical masks, and N95 FFRs regarding their exposure to exhaled CO2 gas. Exhaled air contains between 40,000 parts per million (ppm) and 50,000 ppm of CO2 gas. Because exhaled gas can be trapped in the air volume between a mask and the wearer’s face (i.e., “dead space”), it may be pulled back into the lungs upon the next inhalation. CO2 concentrations between 40,000 ppm and 50,000 ppm can cause dizziness, headache, and breathing difficulty, but the air inhaled by mask wearers is
likely to have much lower CO2 levels than this, Nicas said—typically about 10-fold lower than the 40,000–50,000 ppm range. Generally speaking, the amount of CO2 gas inhaled by a mask wearer will depend on the volume of the mask’s dead space and the air volume inhaled per breath, which in turn depends on the wearer’s work rate.
Nicas offered rough estimates of typical amounts of CO2 gas inhaled by wearers of cloth masks. A cloth mask’s dead space has a volume of roughly 100 mL, and the volume inhaled per breath during light exercise, such as walking, is roughly 1,200 mL. For an ambient concentration of CO2 gas of 400 ppm and a CO2 gas concentration of 45,000 ppm in exhaled air, the CO2 gas level would be 4,100 ppm in the inhaled air volume. A concentration of CO2 gas of 4,100 ppm in inhaled air is not dangerous, he said, although such levels of CO2 gas could cause some physiological effects and a decrease in cognitive performance. He added that the final determination of such effects would need to be made by qualified medical physiology experts. However, he noted that tens of millions of people across southeast Asia, China, Japan, and Korea have routinely worn cloth masks and surgical masks for years and that millions of workers in the United States have routinely worn respirators for the past several decades. Thus, he suggested that side effects would probably already have been observed in those populations if inhaling 4,100 ppm of CO2 gas caused serious side effects for the wearer.
Given these considerations, Nicas’s final recommendation was for a government agency or professional or academic group to conduct a laboratory study to measure the CO2 gas levels inhaled when wearing various types of cloth masks and inhaling various volumes per breath. Such tests could be conducted in a test chamber by placing a mask on a breathing mannequin, he suggested. The CO2 gas levels could be controlled at a range of 40,000–50,000 ppm for exhaled air and 400 ppm for the chamber air. A measure of CO2 gas levels in the total inhaled air volume could then be evaluated by medical experts to determine whether the inhaled CO2 gas would result in health effects of concern.
DISCUSSION
Leak Testing
Balmes said that several participants asked for additional information on the Department of State’s leak test. Huson replied many people were using the Bitrex fit test kit for N95 masks or testing for air and smoke on N99 respirators. The Department of State offers the choice of which challenge agent they would like to use. A challenge agent or scent is used to determine whether a respirator is leaking or improperly fitting. If the
individual wearing the respirator can smell the released agent, then that respirator is leaking, she said.7
Wildfire Smoke
Balmes shared a participant’s question regarding wildfire smoke and asked whether gases are a concern in addition to fine PM. Balmes responded that according to the presentation by Joe Domitrovich of the U.S. Forest Service, wildland firefighters do have a risk of gas exposure. However, the primary concern in areas downwind of a fire is PM2.5 and not gases.
Public Fit Testing
A participant commented that the public will not have access to fit testing unless the municipality pays for it and suggested that the public should have access to a central stock of RPDs at the local level. Balmes said that even if the municipality pays for public fit testing, it is doubtful whether it would take place. This underscores the need to increase the production of N95s and possibly surgical medical masks to make them more broadly available to the public, rather than making them exclusively available to frontline workers.
Improving the Fit of Disposable Masks for Public Wearers
Balmes asked whether medical tape should be used to secure disposable masks for a better fit and reduced leakage. Holm said, “Anything you can do to improve the fit is going to be helpful.” She noted that problems arise when the filtration characteristics of the mask material are unknown. For instance, the filtration properties of an N95 or a surgical mask are relatively well known, and securing these will likely decrease one’s particulate exposure. However, it is much more difficult to predict the impact of securing a cloth mask with medical tape because the filtration characteristics of the cloth are unknown. Holm also said that any action that could potentially irritate the skin is difficult to maintain for long periods of time; for instance, some health care workers experience skin irritation from the pressure of an N95 worn day after day. Holm said that better solutions are needed for the general public if they are to avoid resorting to ad hoc measures such as securing cloth masks with medical tape.
___________________
7 More information about challenge fit tests can be found at https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134AppA (accessed October 9, 2020).
A participant asked whether FFRs that are designed to be attached to the face via adhesive may be a viable option for members of the public to use as a barrier face covering. Another participant, who works for the National Personal Protective Technology Laboratory (NPPTL), said that NIOSH has approved respirators with adhesive seals but that these types of devices do not necessarily provide a better fit than those with straps.
N95s with Exhalation Valves
Balmes reported several questions regarding whether N95s with exhalation valves provide adequate protection. Nicas said that N95s with exhalation valves are not supposed to leak for the wearer. There is always a little leakage, but the exhalation valve leakage is assessed during NIOSH-approval testing and must be below a specified level. He added that the main issue is whether N95s with exhalation valves act as effective source control in reducing the amount of the virus exhaled by an infected wearer. Nicas listed three potential pathways for the release of exhaled air from the wearer: (1) unfiltered air coming from around the edges of cloth masks, (2) filtered air coming through the mask media itself, and (3) unfiltered air coming out an exhalation valve. He said he was not aware of any quantitative studies that have apportioned the percentage or volume of air coming from each of those pathways, however. Nicas added that during a NIOSH study of a fit test on an N95 used during light exercise, there was an observation that the exhalation valve was not activated, at least according to a visual inspection. This suggested that there is not much air coming through the exhalation valve during light exercise and that substantial force would have to be exerted to activate the exhalation valve. Nicas said that his impression is that the amount of unfiltered air coming out of an N95 respirator exhalation valve is not substantial enough to merit not using the device. However, he said that if individuals are concerned about N95 facepieces with exhalation valves, they should not use them. Importantly, a participant said, more complete data are still needed regarding the infectious dose of the virus and the size of particles that people need to be protected from. Access to such data would allow for a greater understanding of how source control strategies, such as masks or face shields, can best be used to protect the public.
KN95 Standards
Balmes relayed a participant question about whether the widely available ear-loop KN95s are effective or whether these offer a false sense of security for the wearer. Holm replied that it is difficult to know, but more certainty is possible with regulated devices, and she is, therefore, more
confident in recommending NIOSH-certified devices. She added that many of these devices are currently entering the United States through atypical routes. For instance, people are ordering devices online from many different countries and manufacturers. She said that in theory the KN95 certification standard is a good standard, but when devices enter the country through atypical pathways it is more difficult to ascertain the true level of protection that these devices offer the wearer.
Maryann D’Alessandro, the director of NPPTL at NIOSH, said that NIOSH has evaluated many KN95s and found that about half of those tested have not met the requirements of the KN95 standard. FDA issued an emergency use authorization for KN95s, which identifies those KN95s that do perform to filtration efficiency requirements that are similar to the NIOSH requirements for use in health care settings. NIOSH has published results from respirator assessments that have been performed as part of its coronavirus 2019 disease (COVID-19) response, she added.8 Richard Metzler, a retired senior scientist at NPPTL at NIOSH, said that a couple of years ago he researched the Chinese GB-2626 standard and found that it was essentially a combination of European standards and NIOSH standards. He noted that, per the data D’Alessandro presented, there may be issues with the conformity assessment (CA) program, or distributors may be counterfeiting or inappropriately labeling those respirators that do not actually meet the standards.
Nicas added that all the KN95s he has seen have had ear loops and that the use of ear loops implies that these KN95s would likely have more face perimeter leakage than a NIOSH-approved N95 face filtered respirator with head straps. He acknowledged that he has not seen quantitative fit-testing data comparing the face perimeter leakage of these two devices, but he said that he presumes KN95s with ear loops are not the equivalent of NIOSH-approved N95s. Kojola said that KN95s have been used in many health care facilities in New York state and New Jersey and that reports from representatives and staff from the health care unions indicate that these have been provided without fit testing. He stated that devices with ear loops generally do not pass fit-testing requirements and that needed fit testing is not taking place. Jim Johnson, a consultant for JSJ & Associates, said that preliminary data indicate that a device with ear loops could have a measured fit factor level between 6 and 10, which does not approach the 100 needed to receive OSHA approval for the strap requirement.
___________________
8 More information about respirator assessments to support the COVID-19 response is available from https://www.cdc.gov/niosh/npptl/respirators/testing/NonNIOSHresults.html (accessed September 16, 2020).
User Seal Checks
Balmes suggested that it would be helpful to have data on the efficacy of using only a seal check to fit test a respirator. He noted that during the H1N1 influenza pandemic, FDA required manufacturers to conduct a study before marketing respirators for influenza to the public, which involved an anthropometric balanced group of people who had never worn a respirator before. Participants were asked to perform a seal check and then were quantitative fit tested. Balmes, who performed this study for a manufacturer, said the respirator “failed miserably.” However, he said, 3M also did the study, and their respirator passed. Balmes suggested that manufacturers require encouragement to design respirators with a user seal check that would provide assurance that the respirator actually provides an effective fit. Nicas asked about the pass fit factor used in the seal check studies conducted during the 2009 H1N1 influenza pandemic. He said that the only 3M study of which he is aware was published in the mid-1990s and used a pass fit factor of 10 for the quantitative fit testing to indicate a good fit, as opposed to the OSHA standard, which requires a criterion of 100. Nicas said that in that study, the seal check seemed effective because the criterion for adequacy was lowered.
Use of N95 Respirators by the Public
A participant commented that the N95 respirator requires fit testing to be effective and asked whether individuals wearing non-fit-tested N95s might have a false sense of security that could result in reduced social distancing. Nicas replied there is only a false sense of security when a person does not understand the limitations of a device, which underscores the importance of clearly communicating and providing information about a device’s capabilities. Referring to Holm’s data showing that non-fit-tested N95s can still reduce particulate exposure, Nicas said a non-fit-tested N95 filtering face respirator reduces a wearer’s exposure by approximately 75 percent. While this may not be the 95–99 percent reduction in exposure that a fit-tested N95 respirator is meant to provide, Nicas contended that a 75 percent reduction is likely of benefit.
Fit-Test Adapter Equipment
A participant asked whether NIOSH approves fit-test adapter equipment as part of its approval process or whether any approving agency approves fit-test adapters. The participant reported that the fit-test adapter for a particular elastomeric mask, which is marketed for use while welding, is attached on the sides of the mask near the user’s cheeks. Typically, the fit-test adapter is centered on the mask. A representative from NPPTL explained that NIOSH does not approve the fit-testing adapter because the
requirement to complete individual fit testing is an OSHA requirement, and OSHA-accepted methods must be employed in the testing. The representative added that fit testing should always be conducted using all required personal protective equipment (PPE) that a worker is required to wear because the equipment may interface with the performance of the respirator.
Cloth Masks
Balmes relayed a participant question regarding the efficacy of the three-layer cloth masks that were recommended by the Centers for Disease Control and Prevention. Holm was unable to address the question because of a lack of data but noted that the limited number of studies assessing different types of cloth masks suggest that the filtration characteristics of fabric vary widely. However, Holm continued, without knowing the specifics about the fabric being used, it is nearly impossible to predict how much protection such a cloth mask actually provides. Balmes added that additional layers are likely to improve filtration but are also likely to increase resistance to breathing and thus decrease comfort.
Counterfeit Respirators
Planning committee member Robert Harrison of the University of California, San Francisco, asked about laws prohibiting the sale of counterfeit respirators in the United States and whether that would fall within the purview of FDA’s Consumer Product Safety Commission or other regulatory agencies. D’Alessandro answered that with the current COVID-19 response there are indeed rules in place across many federal agencies. Agencies including the Department of Homeland Security and FDA’s Office of Criminal Investigations are involved in looking into counterfeit respirators and are working to get these products off the market. Metzler added that years ago NIOSH contacted the Federal Bureau of Investigation and the Department of State regarding a nonconforming product that the supplier was making false declarations about. At the time the issue was not pertinent enough for those agencies to address, but, given the current COVID-19 pandemic, that is no longer the case. A participant asked how those seeking to purchase NIOSH-approved products can avoid counterfeit products. An NPPTL representative answered that NIOSH works hard to remove counterfeit and substandard products from the market.9
___________________
9 More information about NIOSH’s assessment of counterfeit and substandard products is available from https://www.cdc.gov/niosh/npptl/respirators/testing/default.html (accessed September 14, 2020) and https://www.cdc.gov/niosh/npptl/usernotices/counterfeitResp.html (accessed September 14, 2020).
Balmes asked D’Alessandro to comment on manufacturer labeling of devices as N95s even if they have not been NIOSH-approved. D’Alessandro said that the term “N95” currently has no regulation associated with it and is not currently trademarked, although NIOSH is in the process of doing so. In terms of meeting requirements for filtration and breathing resistance, the term “N95” can be meaningless if a device has not been NIOSH approved, she added.
REFLECTIONS FROM DAY 1
The Need for a National Strategy for Respiratory Protection
Balmes said that in any given situation it is necessary to identify the respiratory hazards and risks at hand and to ensure that respiratory protective gear is up to the task of protecting against the hazards and risks identified via a CA process. Balmes said that a national strategy that is able to address emerging risks, such as COVID-19, would help to ensure respiratory protection for the public. Such a strategy should include clear and simple messaging to improve awareness and educate the public about respiratory protection. While offering RPDs to the public outside of a respiratory protection program may be beneficial, Balmes said, it is antithetical to the current regulatory frameworks used to ensure respiratory protection for occupational users. Issues related to RPD sizing (e.g., child sizes), fit testing, and a lack of training on fit testing and use will further complicate the necessary considerations related to providing RPDs outside of respiratory protection programs. Harrison added that it appears that innovative research will be needed to improve our understanding of hazard assessment and respiratory protection to nontraditional users of RPDs. These populations, Harrison said, are in urgent need of new and innovative forms of PPE that are adaptive to their unique needs. Nontraditional users of RPDs may not be familiar with the terminologies used within the respiratory health disciplines. Thus, Harrison added, it must be ensured that clear guidance can be successfully delivered to the end user of RPDs. Additionally, it may be necessary to consider in advance how the various regulations of agencies, such as NIOSH, OSHA, and FDA, will apply to the use of RPDs by these nontraditional user populations.
Addressing the Needs and Concerns of Nontraditional Workers and Their Employers
Workshop planning committee member Melissa McDiarmid, a professor of medicine, epidemiology, and public health at the University of Maryland School of Medicine, said that the COVID-19 pandemic has highlighted
the need to offer respiratory protection in settings where workers typically do not wear respirators (e.g., long-term care). Even employers that have a comprehensive health and safety program may be unaware that respiratory protection needs to be included. Regarding this concern, Harrison suggested research that engages employers and frontline workers—and particularly workers who are not in formal employment relationships—will help to inform understanding of their perceptions, needs, and recommendations, whether it is under the auspices of “research to practice” or applied research. In his opinion, he said, this responsibility could fall within the purview of a federal agency such as NIOSH in partnership with academic researchers, frontline groups, worker education programs, unions, worker centers, and community-based organizations. Balmes added that less representation by unions in the labor force in the United States, has led, in part, to a devaluation of occupational health and safety as a component of public health, and in that respect, it may be helpful if an agency focused on occupational safety and health, such as NIOSH, had greater visibility among employers.
Planning committee member Daniel Shipp, who is retired from the International Safety Equipment Association, remarked that NIOSH is not a regulatory agency and so there are limitations to its scope and authority. NIOSH can set standards for respiratory protection, for example, and it can approve respirators. However, other agencies must determine when NIOSH-approved respirators should be used, when hazard assessments should be conducted, the need for fit testing, and other related issues. He added that currently no overarching health and safety agency in the United States has regulatory authority that can be extended to the public or to the multiple uses of cloth masks; even OSHA’s scope is limited to certain workplaces. McDiarmid remarked that employers have some obligation to recognize respiratory hazards, even in segments of the worker population that have not traditionally been thought of as needing a formal respiratory protection program. She suggested that part of a research agenda could prioritize the examination of both employer and employee hazard recognition. McDiarmid wondered how to translate that research into practice—for example, with some type of pre-regulatory or regulatory structures. Johnson added that the COVID-19 pandemic has shifted the prioritization of PPE and RPDs as defenses against respiratory hazards and that going forward it may be necessary to reevaluate the role of, research on, and training for the use of PPE.
Harmonizing Regulation with the Needs of Nontraditional Workers and the Public
Balmes said that the rigor of an OSHA-compliant respiratory protection program cannot be reproduced for the general public. For instance,
it will not be feasible to offer fit testing to the public, and the education about respiratory protection provided to the public will differ from that provided within occupational settings. McDiarmid added that while misinformation about respirators may pose a hazard to the public, especially during the COVID-19 pandemic, there is likely a greater hazard in the unavailability of RPDs. To address future respiratory protection needs of the public, she added, new kinds of respirators may be needed. Such respirators may include large sealing surfaces so that fit testing may not be required. Harrison pointed out that the authority to make recommendations related to respiratory protection for the public generally rests with state and local governments. This was true in California until Cal/OSHA established the emergency regulation on protection from wildfire smoke. He raised the question of whether the mission and responsibility of an agency such as NIOSH could be expanded to cover the public use of PPE. Balmes added that in California, the public is bombarded with various messages about wildfire smoke and respiratory protection and that efforts are under way to harmonize the messaging from county public health officials, the Department of State, NIOSH, and EPA representatives.






















