7
Addressing Research and Communication Gaps
The challenges of ensuring respiratory protection for nontraditional workers and the public through regulation have been further complicated by gaps in research and communication. As mentioned in earlier chapters, a key component to getting individuals to use appropriate respiratory protective devices (RPDs) will be educating workers, employers, and the general public about the different types of RPDs available. In a session moderated by planning committee member Tener Veenema of the Johns Hopkins University School of Nursing, three speakers discussed the public understanding of respiratory protection, explored the human factors and systems engineering perspective on RPDs, and described concerns relating to the use of respirators by the general public.
PUBLIC COMMUNICATION ABOUT RESPIRATORY PROTECTION
Rachael Jones, an associate professor at The University of Utah, provided an overview of the types of public communication strategies that could help to educate the general public about the benefits of the proper use of respiratory protection. She remarked that the coronavirus disease 2019 (COVID-19) pandemic has highlighted a gap in knowledge about the perception and knowledge of respiratory protection among both the general public and among people who do not routinely wear respirators in occupational settings. Additionally, the contexts in which people are willing to wear respirators are not well understood. Jones said in certain areas of the United States, there have been high rates of compliance and interest in wearing face coverings in response to the COVID-19 pandemic, but the
experiences regarding respirator compliance in communities has varied. Much remains unknown about the motivating factors that have influenced people’s attitudes about wearing face coverings and respirators. These motivating factors, Jones said, may be interpreted partly as a political response to the COVID-19 pandemic, but they may also be interpreted as a reflection of various personal values or perceptions. Many people are willing to wear face coverings and respirators in the context of wildfires or pandemics. However, she added, less is known about the general public’s willingness to use face coverings and respirators while in their homes, working on projects, or in other non-occupational contexts. Jones suggested that better characterizing this user group would contribute substantially to addressing this research gap and advancing efforts to target messages and designs that facilitate the use of respiratory protection.
Research on respirator design could support efforts to effectively communicate and educate nontraditional users of RPDs about respiratory protection, Jones said. For instance, there has been public concern about the presence of and risks associated with exhalation valves on respirators amid the COVID-19 pandemic. Jones suggested this public concern could be addressed in a relatively straightforward way by conducting the necessary research and communicating the findings through clear public messaging.
Communication strategies are also needed to address misperceptions and misinformation about respiratory protection that have emerged in the context of the COVID-19 pandemic, Jones said. For example, videos that circulated online raised concerns among the public about trapping carbon dioxide in the facepieces of respirators. These concerns, Jones said, could be addressed relatively straightforwardly with evidence providing a reasonable explanation for the presence of carbon dioxide in facepieces. However, this explanation and the associated evidence would need to be communicated to the public in a clear and appropriate way. Similarly, news reports during the early stages of the pandemic raised concern about the chemical content of respirators that could potentially affect the wearer. Jones said that regardless of the validity of such claims, they can affect public perceptions and provide a reason to fear respirators.
Better public communication is also needed about respirator fit and the potential consequences of ill-fitting respirators, Jones said. However, research is ongoing into how to increase the number of individuals who will be able to achieve proper respirator fit, Jones added. Research will need to be complemented by effective communication strategies about the importance of a properly fit respirator, Jones explained. People also need to be aware of health conditions that can affect a person’s ability to effectively and comfortably wear a respirator, she said.
Jones added that research- and evidence-informed communication strategies are needed to encourage the use of respirators and the adoption and
implementation of respiratory protection programs in the workplace, particularly among smaller organizations. The Occupational Safety and Health Administration (OSHA) standards for respiratory protection programs are complicated and may be challenging for small organizations to implement, particularly if they do not already have other kinds of occupational health and safety programs in place, Jones said. Research could be conducted to investigate how to best to communicate about respiratory protection programs, how to implement them efficiently, and how to evaluate them. This research, Jones said, could then be used to inform guidance on the effective use of workplace respiratory protection among small employers or employers that do not have established health and safety programs.
A HUMAN FACTORS AND SYSTEMS ENGINEERING PERSPECTIVE ON RESPIRATORY PROTECTIVE DEVICES
Ayse Gurses, a professor at the Johns Hopkins University School of Medicine, offered a human factors and systems engineering perspective on issues related to the use of RPDs by nontraditional users. She described the role of human factors engineering in the design and use of RPDs, framed RPDs as a part of a larger sociotechnical safety-critical work system, and suggested avenues for future research on RPDs from a human factors engineering perspective. According to the International Ergonomics Association, human factors and ergonomics (HFE) is “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system and the profession that applies theory, principles, data, and methods to design in order to optimize human well-being and overall system performance.”1 HFE can be applied to systems, technologies, or tools, such as N95 respirators. Some HFE scientists, Gurses said, are concerned with ensuring that patients and health care workers remain safe, as the safety of these groups is critical for optimization of system performance in health care settings. For instance, the Armstrong Institute for Patient Safety and Quality is dedicated to improving the way that people—health care professionals, patients, and families—interact with care systems so that the systems are safer, high performing, and patient-centered.2 Their projects include, for example, work done to address Ebola, she said.
Gurses identified three specializations in the field of HFE and described how they may relate to the issues of RPDs: (1) physiological ergonomics, (2) cognitive ergonomics, and (3) macroergonomics, also called organiza-
___________________
1 More information about HFE and the International Ergonomics Association is available from https://iea.cc/what-is-ergonomics (accessed August 31, 2020).
2 More information about the Armstrong Institute for Patient Safety and Quality is available from www.hopkinsmedicine.org/armstrong/humanfactors (accessed August 31, 2020).
tional ergonomics (Gurses et al., 2012). Physical ergonomics may help to address the issues of RPD fit, comfort, and ease of use. Cognitive ergonomics may help address the issues of RPD packaging and labeling, manufacturer instructions for use, colors and textures used in RPDs, and RPD training. Macroergonomics may help address issues related to the use of RPDs within a specific context or “work system,” Gurses said. Macroergonomics addresses entire systems by considering the relevant timing constraints, safety climates, and teamwork. Macroergonomics also accounts for training and adaptive capacity—that is, whether workers’ training encourages them to merely follow directions or empowers them to adapt to changes in the workplace to maintain their safety while completing their work. Macroergonomics also uses participatory ergonomics to design interventions in a manner that increases acceptance of those interventions.
Respiratory Protection Devices as a Component of the Sociotechnical Work System
Gurses said that nontraditional users of RPD vary in terms of physical characteristics, anthropometric characteristics, cognitive characteristics, knowledge, skills, attitudes, and user behaviors as well as in terms of age, preferences, degree of trust, culture, comfort, perceived workload, and perceived ease of use, usefulness, and feasibility. These factors, Gurses said, influence user behaviors that, in turn, affect compliance or noncompliance. As Jones noted in her presentation, little is known about these user populations or why some populations are more motivated to use face coverings or respirators than others. Research on these issues may help to elucidate the cultures, preferences, biases, and factors of comfort that contribute to the use behaviors of these different groups. This could contribute to better managing the respiratory health and improving the compliance of these groups within user populations, she said.
Gurses presented a model from a systems engineering initiative for patient safety (see Figure 7-1). This model was created to address patient safety, but it could also be used to consider the safety of health care work systems or even home safety. The work system component of the model represents individuals conducting tasks. This work system model indicates that there are many complex interactions occurring among technology and tools, persons, tasks, environments, and organizations. RPDs fit within the designation of technology and tools, and understanding their context among the other work system factors could inform strategies to design RPDs, develop instructions for their use, and develop training about RPDs.
In the field of respiratory protection, the term “hazard” is often used to refer to an exposure hazard, Gurses said. However, in HFE, hazards include any factors that may lead to noncompliance. For instance, if a work system
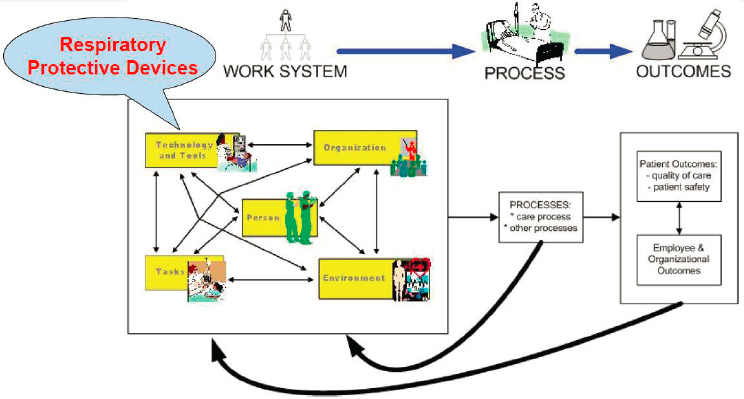
SOURCES: Gurses presentation, August 5, 2020; Carayon et al., 2006.
does not have N95s, then it will be impossible for workers to comply. Less extreme examples of “hazards” include poorly fitting RPDs or any other factor that is a hazard to compliance with a safety program. In addition to considering exposure hazards, Gurses said, it is necessary to consider hazards in the work, home, or public system that impede users from complying with intended use and protocols.
The sociotechnical work system is a highly dynamic system, Gurses said. This system exists in “safety critical” work or living environments. In HFE, task–technology fit is a key consideration for safety critical work or living environments. The safety-prone approach focuses on work as imagined. This approach sets out to design every factor of systems in the “correct” way to ensure safety among the system participants. In HFE, the safety-tool approach acknowledges that safety critical environments are highly dynamic, nonlinear, and unpredictable. This approach presumes that it is not possible to account for every possible hazard through design. For instance, face coverings or masks are designed to be worn in a particular way to ensure their proper function, yet “in the wild” masks are worn in myriad ways that diminish their function, Gurses said. The approaches in safety literature focus on work-as-done and educating system participants, thus providing them with tools to ensure their own safety. This approach is intended to ensure that when safety factors change unexpectedly, system participants will be resilient and able to develop solutions to preserve system safety. HFE methods and approaches must be used to study work and living environments and engineer resilience using a combination of the
safety-prone and safety-tool approaches, Gurses said. She emphasized that resilience is key in this model. When unexpected events occur, resilient systems empower individuals to react in a safe manner. For instance, Gurses and her colleagues published a paper on their findings that workers in a cardiovascular operating room had begun taping labels on their new smart intravenous pumps to clearly mark the names of the drugs being dispensed (Pennathur et al., 2013). This demonstrates an oversight on the part of engineers who did not fully consider the needs of the users of these products and also illustrates the resilience of workers who recognized a safety need and adapted. Similar types of studies and design approaches should be considered in the development of RPDs, she said.
Human Factors Engineering Approaches and Respiratory Protective Devices
Gurses said that there are many approaches of HFE that may be relevant to the use of RPDs. Conceptual approaches to HFE of relevance include systems approaches, naturalistic decision making, distributed cognition, reliance engineering, high reliability, organizational learning, and implementation science. Methodological approaches include task analysis and cognitive task analysis; work system analysis, including in-depth understanding of the context of use; human-centered design; usability evaluation, including formative and summative evaluations; proactive risk analysis, including failure mode and effects analyses and what-if analyses; and participatory ergonomics and design. Gurses said that naturalistic decision making has to do with how people make decisions in real settings. For example, researchers may study how people choose which personal protective equipment (PPE) or gowns or gloves to use when under time pressure in real settings and team environments. This approach was developed through the study of firefighting. She added that implementation science is a key approach for issues related to RPDs. Even if the perfect RPD could be developed, proper implementation would be necessary to account for the variation in tasks that require RPDs to be used and in the types of RPD users. Cognitive task analysis is used to evaluate why individuals make certain decisions, such as why a person may don a mask incorrectly, she said. This form of analysis may be used to investigate whether the person is unaware of the correct way to don the mask or perhaps has chosen to don it incorrectly for some reason. This kind of analysis is valuable for designing better training and instructional materials, Gurses said. Finally, she noted that numerous areas of study within the domain of human-centered design may be of value to those working on the challenges of RPDs.
Creating a Research Strategy to Improve Use and Safety of Respiratory Protective Devices
Gurses proposed that a comprehensive, interdisciplinary, multidimensional research strategy be deployed to improve RPD use and safety. Such a research strategy might include various forms of interdisciplinary scientific research. An evaluation of the different needs of different users could be conducted through ethnographic studies on work-as-imagined versus work-as-done. Safety risks and other problems, Gurses said, can be identified through failure mode and effects analyses and what-if analyses, while new human-centered RPD designs can prioritize resilience whenever possible. Test solutions developed using human-centered design could be iteratively developed and piloted. Implementation science can be harnessed to tailor, implement, and disseminate those solutions, coupled with effective feedback mechanisms to inform public health systems about the real-world use and effectiveness of RPDs, Gurses said. Gurses also commented on the need for communication in addition to mere education. The existing focus on improving communication about RPDs—both to users and from users—should be maintained. The public’s perceptions, problems, and needs must be heard and acknowledged so that they can be addressed, she added, noting that a top-down approach is not suitable for addressing the communication needs related to RPDs. Gurses said that there are feedback mechanisms in place to engage users of RPDs and assess the effectiveness of RPDs. To ensure the success of new national strategies to support the use of RPDs among the public, these mechanisms must be maintained as new systems and devices are developed, she added.
USE OF RESPIRATORS BY THE GENERAL PUBLIC
Barbara Materna, the chief of the Occupational Health Branch of the California Department of Public Health, explained that in her work as a certified industrial hygienist she has been involved with the use of respirators in health care under the California Occupational Safety and Health Administration (Cal/OSHA). She helped to develop Cal/OSHA’s aerosol transmissible diseases standard and has collaborated with the National Institute for Occupational Safety and Health (NIOSH) and the federal OSHA to develop a respiratory protection program toolkit for hospitals. She explained that during various emergency responses, when workers or members of the general public have been at risk for health effects from inhaled hazards, public health officials have recommended respirators as a necessary control measure outside of a formal respiratory protection program. When this has occurred, the events give rise to recurring questions, including (1) how much protection is provided by respirators that
have not been fit tested, (2) how should those with pre-existing heart or lung disease be advised, and (3) how to address individuals’ improper use of respirators and consequent lack of protection. Materna explained that she has encountered such issues primarily in the context of responding to California wildfire emergencies where the respiratory hazards in question are particulates in smoke or ash. She has also worked on developing guidance for the Environmental Protection Agency’s updated wildfire smoke guide regarding the use of respirators by the public or outdoor workers who have not been fit tested. Other emergencies where particulate hazards become an issue include volcanic ash from eruptions, mold exposure after floods, and infectious disease pandemics, such as the COVID-19 pandemic. She suggested that the public would benefit from better use of respirators in certain non-emergency situations if they had access to clear and accurate information about the technical details as well as access to equipment designed with their ease of use in mind.
Regarding the use of respirators among nontraditional workers, Materna suggested focusing on providing the same level of protection to these workers as is provided to all workers who rely on respirators. She said she would concentrate her remarks on the use of respirators by the public. In consideration of this aim, she raised three questions: (1) What is needed to provide the best protection for the public who use respirators without the benefit of fit testing? (2) Can N95s or other filtering facepiece respirators (FFRs) be used by those with heart or lung conditions? and (3) What is needed to better communicate to the public about proper respirator use?
Providing the Best Respiratory Protection Without Fit Testing
Materna said that communication to the public often conveys the importance of achieving a seal close to the face in order to provide adequate protection. However, one drawback of the N95 and other FFRs is that, unlike other elastomeric half-mask respirators, it is difficult, or impossible, to conduct an effective user seal check to assess their fit, Materna said. If filtering facepiece models were put on the market in multiple sizes that had been proven to fit a variety of facial shapes and sizes well, then the public would be better served in situations where fit testing is not feasible, she added. She suggested that RPD manufacturers ought to be required to meet a minimum fit criteria before being allowed to market their products. In some cases, stockpiles of RPDs have contained poorly fitting devices that, upon being deployed during an emergency, failed fit testing among a high proportion of users. NIOSH has recognized the need to add a fit standard to the NIOSH certification process, Materna said. The issue of fit is urgent and must be addressed as soon as possible, she added. There may be a role for innovation and development of new products in addressing these
concerns. The flexibility and stickiness of facepiece materials in elastomeric half-mask respirators make them easier for most people to achieve a good seal and conduct user seal checks with these devices, she added. However, Materna said, existing reusable elastomeric respirators are often perceived as too industrial in appearance or too expensive to be acceptable. Newer, more lightweight devices that afford a good seal and easy user seal checking for a wide range of users would be beneficial, she added. As has been discussed, user acceptance testing would be critical to assess how useful such new devices would be for addressing the needs of various groups.
Use of Respirators by Those with Heart or Lung Conditions
Materna next considered the question of whether N95s or other FFRs can be safely worn by people with heart or lung conditions, including during physical exertion. She explained that during wildfire emergencies some jurisdictions broadcast messages warning against the use of respirators by those with pre-existing heart or lung conditions. However, during wildfire emergencies, those with heart or lung conditions may be the most in need of respiratory protection should they be outdoors in the presence of smoke or ash. This has also been a concern for outdoor workers in the vicinity of smoke and ash from wildland fires, who frequently have been advised to wear a respirator despite never having been medically cleared to use a respirator. A similar situation emerged during the COVID-19 pandemic, which raised questions about whether older people with heart or lung conditions—who are at higher risk—should wear N95s when in public. Materna said the most common guidance on these questions has been that individuals should speak with their physicians before using a respirator, but the majority of physicians know little about respirators and the risk they may pose to users with various kinds of pre-existing conditions. Thus, evidence-based guidance on the potential risks of respirator use would be helpful, she added. This may require that additional research be conducted, or it may require better translation of existing research on respirator use and potential risk. Additionally, she said, physician education about respiratory protection would make physicians better prepared to provide accurate information to patients about these questions.
Improving Public Communication About the Proper Use of Respirators
Materna emphasized the need for better communication to educate the public on how to use respirators properly, pointing out that depictions in the media often show respirators being used incorrectly. Proper respirator use needs to be better conveyed, she said, using clear visuals and messaging developed by experts in advertising and media campaigns. These messages
could be piloted and evaluated for effectiveness, then distributed via channels such as social media and short YouTube videos, Materna added. The persistent use of the term “mask” is another challenge that can be addressed through improved communication, she said. This term means different things to different people, and the use of the term causes confusion among both members of the public and public officials. This confusion has become widespread in the response to the COVID-19 pandemic, she added. Individuals frequently confuse devices worn as source control with respirators that are designed to protect the wearer from inhaling hazardous particles, Materna said. As a result, she added, it has been necessary to develop guidance to differentiate respirators, surgical masks, and cloth face coverings. The technical details related to respirator use have complicated this guidance, as these details are not widely understood. She emphasized that the general public must be made more comfortable using the term “respirator” when the device being discussed is, in fact, a respirator. The public understanding of respirators needs to be improved so that individuals understand what respirators are, how they work, their limitations, and where to obtain accurate information about respirators from experts. Research evaluating the knowledge and perceptions about respiratory protection among the public may help to create effective messaging on this subject. Materna said that because NIOSH is the most respected source of information about respirators, it has an important role to play in addressing the need for messaging even though its typical audience is groups of workers rather than the public.
DISCUSSION
Veenema listed several reoccurring needs discussed during the session’s presentations, including public awareness, user acceptance, and human factors that affect decision making. She reviewed the comments made by Jim Johnson, a consultant for JSJ & Associates, in an earlier session about the need to (1) understand the hazard, (2) identify options for protection from that hazard and educate people about their options, (3) explore how people internalize the perception of risk, and (4) examine how that may affect people’s willingness to use RPDs and to learn how to use these devices properly and consistently.
User-Centered Compliance Programs
Veenema highlighted Jones’s comments regarding the need for social and behavioral research to better understand the context in which people will wear devices, noting an intersection between Jones’s comment about making programs more acceptable and easier to implement in smaller
businesses and Gurses’s comment about organizational ergonomics. Jones commented that user needs must be understood in order to create a user-centered design and that this pertains not only to the design of the technology, but also to the design of communications. Jones explained that communications may take the form of labeling, public-facing advertising, or communicating through the workplace as a way to reach more people. Additionally, Jones said, workplace education can influence how people engage with these devices in their personal lives. This underscores the need to understand why people behave as they do, whether approaching this via occupational health, a human factors approach, or an advertising/marketing perspective. Questions to explore include why some people are successful in using devices and some are not, as well as why some people are engaging in actions that are not easy to understand. She asked how all of those perspectives can be brought together to tailor messaging, technologies, and programs.
Gurses said she agreed with Jones’s point about exploring the needs of small organizations. In her research, both in this context and in patient safety, she has found that one organization will have various differences from another. Community health centers differ from academic centers, and the workflow and available resources vary from one organization to the next. Therefore, Gurses said, it is important to tailor implementation approaches to the organization. Gurses emphasized the role that an organization’s culture plays in implementation, and she mentioned research that she conducted with workers providing environmental care services at Johns Hopkins via room cleaning. While these environmental service associates are not nontraditional workers, they are also not nurses or physicians, and Gurses said she found that they did not think of themselves as part of the team. The rooms were not being cleaned as well as the organization wanted, which Gurses attributed to the safety climate and to relations between environmental service associates and nurses. The feeling of being part of the team can affect workers’ behavior, which in turn affects safety climate and follow-through on guidelines provided by the respiratory protection program, she said.
Respirator Public Awareness
Veenema referred to the comments made by Materna regarding challenges with educating the public on the selection and use of RPDs. Public education topics include knowing what a respirator is, understanding the use of the device known by the blanket-term “mask,” and identifying the type of respirator or covering one should use in the workplace or for the COVID-19 response. Veenema said that misinformation and myths related to respiratory devices have been at play in 2020 and asked whether any
progress has been made with respect to bolstering the public understanding of what a respirator is. She also asked how key stakeholders can be educated to enable them to advise the public.
Materna said that progress has been made, citing the example of the response to wildfire smoke. Wildfire smoke is a hazard affecting many different parts of the country, and because people can see and smell smoke, it is a hazard that is perhaps easier for people to understand than COVID-19, she suggested. Through media coverage of wildfire events, people have become familiar with the use of the Air Quality Index to assess the degree of hazard they are facing. People can smell the smoke, and they understand it is not healthy to have the smoke in their lungs; therefore, Materna said, at least a certain proportion of the public is motivated to protect themselves. Another sign of progress is that more people have respirators on hand as part of emergency preparedness. Materna said that where she lives, many people had FFRs in their emergency kits, and they began using them on visits to the grocery store before face coverings were rolled out as part of the COVID-19 response. She said that older people who understood they were at higher risk for COVID-19 seemed especially aware of the need to protect themselves. Materna concluded that there is slow and steady progress and that much more remains to be done.
Physician Respirator Knowledge and Medical Clearance
Veenema relayed a question from a participant regarding the standards that physicians are using to clear workers in respiratory protection programs if those physicians know little about respirators. Furthermore, she asked whether these physicians are instructed on follow-up testing that would ensure the safe use of a respirator. Materna, emphasizing that she is not a medical doctor and is not speaking for all doctors, said she had noted a difference between primary care providers and the occupational medicine physicians and nurse practitioners who typically perform respirator medical clearances. The latter group, Materna said, seems to be better informed on what to look for, as they typically know what to do when a person indicates on an initial screening questionnaire having asthma or other indicators of breathing issues, she noted. For instance, those practitioners may perform pulmonary function testing to assess the true degree of impairment. Materna said that primary care providers are typically less informed and this can lead to problems when members of the public are told not to use a respirator until cleared by one’s doctor and then the doctors are unsure of how to proceed. Materna said that this lack of knowledge regarding medical clearance leads some public officials who are physicians to recommend that people use FFRs that have low breathing resistance and advise users
that, if they experience problems, they should immediately take the respirator off, leave the area, and pursue other options. She added that some people have expressed concerns that they will be held liable in the event of respirator-related issues.
Human Factors Engineering
Veenema repeated the suggestion made by Gurses that the concepts of work imagined versus work done could be considered in addition to robust interdisciplinary science on RPDs. Using the example of workers in agriculture and landscaping who are exposed to hazards such as air pollution and wildfire smoke, Veenema asked how HFE can enhance successful respiratory protective device performance and programs for nontraditional workers. Gurses replied that there are multiple ways to improve work-as-done versus work-as-imagined. Some of the protocols being communicated via guidelines, protocols, or training materials may be perceived in the actual work setting as being impossible—or at least very difficult—to implement. There is a gap, Gurses said, between the protocol and the implementation and understanding these gaps requires not only perfecting the tool or technology, but also understanding its use in actual settings, whether it is a wildfire, agricultural, or meatpacking setting. The challenges to that particular environment and the strategies that people have developed can be identified and learned from, she added.
Human factors engineers have expertise in using in-depth ethnography and qualitative and quantitative studies to identify these gaps, Gurses said. Once gaps are identified, all stakeholders are brought together using a participatory ergonomics approach to develop solutions. Gurses added that a systemic engineering approach could benefit the development of training and education protocols. She noted that if a technology is easy to use, it will not require instructions or training. Labeling, instructions, and training are developed to supplement device design limitations, and that training should be developed based on risk points and evaluated via systemic analysis of why people are perceiving communications differently than intended, Gurses said. At that point, she added, training can be altered to address sources of misunderstanding.
Oxygen Deficiency Myths
Veenema asked a participant’s question about how to effectively address people’s unfounded fear about oxygen deficiencies being caused by masks and barrier facial coverings. Materna said that a trusted spokesperson is needed to address this issue by way of mass media. Misconceptions and rumors are used as excuses not to pursue these control measures, and mis-
information needs to be addressed head on through the clear communication of the facts, she said.
Workshop planning committee member John Balmes of the University of California, San Francisco, said that a national strategy for respiratory protection is necessary, especially in the context of the COVID-19 pandemic. Recounting information presented by Stephanie Holm of the Western States Pediatric Environmental Health Specialty Unit, he said that the physiologic impacts of wearing almost any type of respiratory protection are not severe. Balmes added that improperly designed cloth masks may have higher air flow resistance and might not perform as well as N95s or surgical masks, but there is very little evidence to indicate that wearing these masks results in negative physiological consequences. Balmes emphasized the need to develop clear and simple messaging to counter misinformation and added that some county public health officers also have knowledge gaps. He offered the example of public health officers in California who have emphasized the harm that wearing N95s might cause people with pre-existing asthma, but Balmes said these are the very people who should be wearing N95s when going out during a wildfire air quality episode. Jones also noted that misperceptions extend beyond the general public. She has worked with manufacturers in Utah who have questions or concerns about the use of respirators in the context of COVID-19, despite being people who wear respirators with some regularity. She said that this represents an underlying gap in knowledge about how these devices work. COVID-19 has made this gap more prominent, but Jones contended that it was already there before the pandemic.
NIOSH Research and Funding
Jones said that NIOSH is a trusted source that could potentially expand its role in public communication and research. Balmes added that to do so, NIOSH would need more funding. Gurses pointed out that more funding also needs to be allocated to improve the collective understanding of the science of implementing the use of RPDs efficiently, consistently, and safely because this is an ongoing research gap. Gurses suggested NIOSH could collaborate on this research with the Agency for Healthcare Research and Quality because health care worker safety and patient safety are interrelated.
Final Reflections on the Session
Veenema offered her reflections on the presentations and discussions of Session 5: Research and Communication Gaps and Opportunities, noting that the research questions at hand are numerous and diverse, ranging from issues about the performance of particular RPDs to the exploration
of human factors on individual adoption and proper use of RPDs. Overall, the session speakers recognize that a systems perspective will be key for investigating why certain RPDs are used or not used and what can be done to increase their proper use and understanding. Additionally, Veenema recognized the time constraints at play, such as the urgent need to address the concerns related to the use of cloth face coverings by the public as soon as possible. Given the need to answer many of the questions raised by the workshop’s speakers within the context of these time constraints, strategic prioritization and advocacy for targeted research will be the best path forward for optimizing public health impact, she added.
FINAL REFLECTIONS AND DISCUSSION
Training
Reflecting on comments made by Gurses, Johnson suggested that if an RPD requires extensive training (e.g., multiple workdays) it is a sign of a defective approach to respiratory protection. One design aim in respiratory safety could be to make equipment for which the proper use is self-evident. Gurses replied that this would be more aptly considered a design limitation than a defect; it is impossible to design a perfect tool or technology, and there will be some limitation to every type of product. Training needs to be developed systematically to address those limitations so that training, instructions, programs, and design make up an overall system with the best possible outcome, Gurses said. Shipp remarked that respiratory protection is so complex in occupational and industrial settings that training on RPDs will always be required because products will have to be designed specifically to protect workers against inhalation hazards that cannot be engineered out. Workers in particularly hazardous settings, Shipp added, will need more extensive training to ensure they are afforded enough protection. Gurses clarified that training should not be used as a means to overcome bad design. Training itself should be developed in accordance with the principles of good training, such as commander’s intent (e.g., telling people why they are doing the training). Melissa McDiarmid of the University of Maryland School of Medicine commented that the shortcomings of RPDs are often linked to the shortcomings—or even total lack—of respiratory protection programs in which these RPDs are being used. For instance, she suggested that the defects in the use of RPDs and face coverings in response to the COVID-19 pandemic are linked to the historical failure of governments to invest in public health infrastructure and the inadequacy of national stockpiles of needed equipment for a pandemic response. Balmes said that there is clearly a role for well-designed training in occupational settings. For public use, this role must be fulfilled through
different types of messaging, as respiratory protection training for the general public is unlikely to be practical, Balmes said.
COVID-19 Pandemic and Future Opportunities
Balmes said that NIOSH’s increasing visibility due to the COVID-19 pandemic could be used to promote a heightened awareness of occupational and respiratory health and safety in the public health discourse. In particular, NIOSH’s special competence and expertise for occupational safety and health issues can be brought to bear in this discourse, Balmes said. Under normal (non-pandemic) circumstances, only a limited population needs or has any interest in RPDs. However, the COVID-19 pandemic has provided an opportunity to take advantage of public interest to increase investment in RPDs, Balmes said. The role of the National Personal Protective Technology Laboratory (NPPTL) could be expanded to act as the single source of messaging and training about RPDs, both for occupational settings and the public, Balmes added. Nicas commented that creating a new approval process for RPDs intended only for public use would not be feasible. He proposed using the Defense Production Act to force companies in the United States to make N95 FFRs, rather than creating a new structure for approving public use respirators.
Messaging and Awareness
Holm said that educating both the public and medical professionals about respiratory health is a key concern. While the amount of training on RPDs may vary among medical professionals, most general providers know little more about respiratory protection than any member of the general public. The COVID-19 pandemic has presented an opportunity to raise awareness about respiratory protection. Veenema suggested finding ways to clarify and harmonize risk messaging about RPDs, which would require additional funding for agencies involved in this area, such as NIOSH. Cohen said that there has been a lack of clarity in messaging to the public about the intended function and appropriate use of respirators versus face masks in the context of the COVID-19 pandemic. McDiarmid also highlighted the need for careful messaging and clear communication to different populations about the use of true respirators versus masks.
Developing Unifying Standards, Messaging, and Strategies
Emiel DenHartog, an associate professor and an associate director of the Textile Protection and Comfort Center at North Carolina State University, highlighted the importance of supporting individuals and small
companies who are designing and producing masks during the COVID-19 pandemic (e.g., by providing them with guidelines or creating an ASTM standard for general-purpose face masks). He suggested drawing a distinction between PPE for occupational safety and general-purpose masks for the public, with the latter having looser requirements but accurate labeling to clearly indicate its intended usage (e.g., wildfire, pesticide exposure). Jeff Stull, the president of International Personnel Protection, Inc., added that standards can apply not only to products but also to use, care, and creating awareness. Making standards and documentation more accessible to end users and leveraging more nimble organizations in concert with direction from NIOSH and NPPTL would help to make these standards more effective, Stull added.
Maryann D’Alessandro, the director of NPPTL, explained that NIOSH has been working to develop a comprehensive national strategy for respiratory protection that includes CA and research. While NIOSH has expertise in CA and certain areas of research, the people there are aware of their need for assistance. Thus, D’Alessandro said, the path forward likely includes the development of centers of excellence for personal protection technologies and equipment across the United States. She added that the expertise of these centers can be leveraged in areas such as human factors, behavioral issues, and other areas discussed in this workshop. Partnerships across federal agencies, universities, and manufacturers will also be invaluable, D’Alessandro said, for identifying and executing strategies to enhance domestic production of RPDs, despite a lack of funding for such production. D’Alessandro closed the meeting on a note of optimism, remarking that NIOSH and the occupational health community more broadly seem committed to expanding their mission to protect respiratory health in the workplace and beyond.
This page intentionally left blank.


















