Summary1
The decade ahead will test the nation’s nearly 4 million nurses in new and complex ways. Nurses live and work at the intersection of health, education, and communities. In the decade since the prior The Future of Nursing report was issued by the Institute of Medicine, the world has come to understand the critical importance of health to all aspects of life, particularly the relationship among what are termed social determinants of health (SDOH), health equity, and health outcomes. In a year that was designated to honor and uplift nursing (the International Year of the Nurse and the Midwife 2020), nurses have been placed in unimaginable circumstances by the COVID-19 pandemic. The decade ahead will demand a stronger, more diversified nursing workforce that is prepared to provide care; promote health and well-being among nurses, individuals, and communities; and address the systemic inequities that have fueled wide and persistent health disparities.
The vision of the Committee on the Future of Nursing 2020–2030, which informs this report, is the achievement of health equity in the United States built on strengthened nursing capacity and expertise. By leveraging these attributes, nursing will help to create and contribute comprehensively to equitable public health and health care systems that are designed to work for everyone. To achieve health equity, the committee also envisions a major role for the nursing profession in engaging in the complex work of aligning public health, health care, social services, and public policies to eliminate health disparities and achieve health equity. Specifically, with implementation of this report’s recommendations, the committee envisions 10 outcomes that position the nursing profession to contribute meaningfully to achieving health equity (see Box S-1).
___________________
1 This Summary does not include references. Citations for the discussion presented in the Summary appear in the subsequent report chapters.
HEALTH AND HEALTH INEQUITIES
Health inequities, defined as “systematic differences in the opportunities that groups have to achieve optimal health, leading to unfair and avoidable differences in health outcomes,” disproportionately impact people of color; the lesbian, gay, bisexual, transgender, and queer (LGBTQ) community; people with disabilities; those with low income; and those living in rural areas. Indeed, growing evidence reveals a clear association between inequities in both health and access to health care and SDOH—the conditions in the environments in which people live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. SDOH include both the positive and negative aspects of these conditions. Examples of SDOH include education, employment, health systems and services, housing, income and wealth, the physical environment, public safety, the social environment (including structures, institutions, and policies), and transportation. Everyone is affected by SDOH. Some people who have more education or higher incomes will fare better healthwise as they may be able to make more informed choices, have better opportunities to access health care, and have the means to pay for health care. Others, without the benefit of these positive social determinants, are unlikely to fare as well.
A related concept is social needs—individual-level, nonmedical, acute resource needs for such things as housing, reliable transportation, and a strong support system at home that are necessary for good health outcomes and health equity. Health equity can be advanced at the individual level by addressing these needs and at the population level by addressing SDOH. Health equity benefits all individuals by promoting such macrostructural benefits as economic growth, a healthier environment, and national security.
For too long, the United States has overinvested in treating illness and underinvested in promoting health and preventing disease. The nation has spent more on medical care than any other high-income country, yet it has seen consistently worse health outcomes than those of its peer countries, including the lowest life expectancy, more chronic health conditions, and the highest rates of infant mortality. At the same time, the COVID-19 pandemic has starkly revealed Americans’ unequal access to opportunities to live a healthy life, often resulting from entrenched structural and systemic barriers that include poverty, racism, and discrimination. These two phenomena—suboptimal health outcomes and inequities in health and health care—are not unrelated. If the nation is to achieve better population health, it will have to meet the challenge of mitigating these inequities. Herein lies the greatest contribution of the nursing workforce in the decade ahead.
THE ROLE OF NURSES IN ADVANCING HEALTH EQUITY
A nation cannot fully thrive until everyone—no matter who they are, where they live, or how much money they make—can live the healthiest possible life, and help-
ing people live their healthiest life is and has always been the essential role of nurses. Whether in a school, a hospital, or a community health clinic, they have worked to address the root causes of poor health. The history of nursing is grounded in social justice and community health advocacy. The Code of Ethics for Nurses with Interpretive Statements from the American Nurses Association (ANA), for example, obligates nurses to “integrate principles of social justice into nursing and health policy.”2 Nurses work in a wide array of settings and practice at a range of professional levels. They often act as the first and most frequent line of contact with people of all backgrounds and experiences seeking care. The nursing workforce also represents the largest of the health care professions—nearly four times the size of the physician workforce. In their various capacities and given their numbers, nurses are uniquely positioned to manage teams and link clinical care, public health, and social services.
STUDY PURPOSE AND APPROACH
Nurses, then, have a critical role to play in achieving the goal of health equity. But to take on the pursuit of that goal, they need robust education, supportive work environments, and autonomy. Accordingly, the Robert Wood Johnson Foundation asked the National Academies of Sciences, Engineering, and Medicine to conduct a study aimed at charting a path forward for the nursing profession to help create a culture of health and reduce disparities in people’s ability to achieve their full health potential. To carry out this study, the National Academies convened an ad hoc committee of 15 experts in the fields of nursing leadership, education, practice, and workforce, as well as health policy, economics and health care finance, informatics, population health and health disparities, health care quality and delivery, and health care research and interventions.
To supplement the knowledge and expertise of its members, the committee solicited input from additional experts and interested members of the public at two public sessions held in conjunction with committee meetings. Further input came from several site visits that included town hall meetings. In addition, the committee reviewed the salient peer-reviewed and grey literature not associated with commercial publishers, carried out original data analyses, commissioned papers on topics of particular relevance, and considered public and organizational statements pertinent to this study.
To organize and consolidate this wealth of information, the committee developed the framework depicted in Figure S-1. This framework structures the report’s discussion of the key areas for strengthening the nursing profession to meet the challenges of the decade ahead. The heart of this framework is the key areas shown at the top of the figure: the nursing workforce, leadership, nursing
___________________
2 See https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-fornurses/coe-view-only (accessed April 13, 2021).
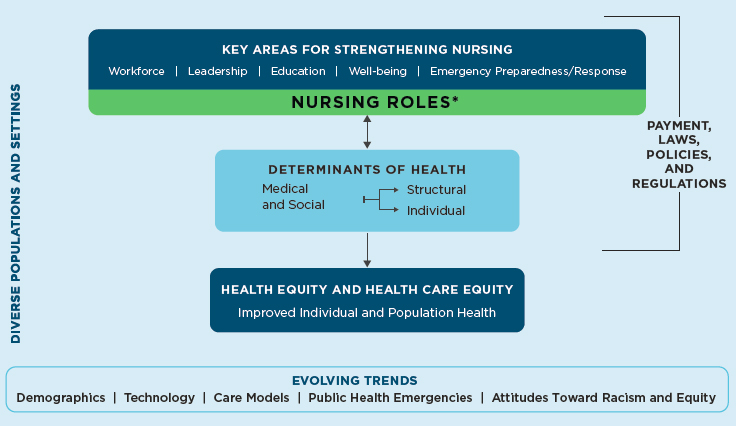
* Examples of nursing roles in acute, community, and public health settings include care coordinator, policy maker, clinician, educator, researcher/scientist, administrator, and informaticist.
education, nurse well-being, and emergency preparedness and response, and the responsibilities of nursing with respect to structural and individual determinants of health. Nurses play multiple roles in acute, community, and public health settings that include, but are not limited to, care team member and leader, primary care provider, patient and family advocate, population health coordinator, educator, public health professional, health systems leader, organizational and public policy maker, researcher and scientist, and informaticist. Through each of these roles, nurses impact the medical and social factors that drive health outcomes and health and health care equity. Nurses can address SDOH through interventions at both the individual level (e.g., referring an individual’s family to a food assistance program) and the structural level (e.g., alleviating the problem of food insecurity in the community). Similarly, nurses can address medical determinants of health at both the individual level (e.g., providing patient education and medication management) and the structural level (e.g., implementing a system of team-based multisector care that includes coordination of care across settings and sectors).
ACTING NOW TO IMPROVE THE HEALTH AND WELL-BEING OF THE NATION
The health and well-being of the nation are at an inflection point. In the decade ahead, in addition to growth in the overall size of the U.S. population,
other sociodemographic factors and health workforce imbalances will increase the demand for nurses, particularly in areas in which the current registered nurse (RN) and advanced practice registered nurse (APRN) workforce is inadequate to meet the nation’s health care needs. For instance, a 2020 report prepared for the American Association of Medical Colleges estimated that by 2033, current physician shortages, seen particularly in the areas of primary care, mental health, and gerontology and in rural areas, could increase—for primary care physicians, ranging between 21,400 and 55,200, and for non–primary care specialty physicians, between 33,700 and 86,700. Salient sociodemographic factors include the aging population, the increasing incidence of mental and behavioral health conditions, increases in lack of access to primary health care, persistently high maternal mortality rates, and worsening physician shortages. For example, the aging of the U.S. population means that over this decade, increasing numbers of people will age into their 70s, 80s, 90s, and beyond. In 2030, 73.1 million people, or 21 percent of the U.S. population, will be older than 65—a population that typically presents with morbidities at higher rates than are seen in younger people.
The strengths of the nursing workforce are many, yet they will be tested by formidable challenges that are already beginning to affect nurses and the health systems and organizations in which they work. These challenges will arise not only from the above changes occurring throughout the broader society but also from changes within the health care system itself and within the nursing and larger health care workforce. Further challenges for nursing will arise from health-related public policies and other factors that affect the scope of practice, size, distribution, diversity, and educational preparation of the nursing workforce. These many challenges include the need to
- increase the number of nurses available to meet the nation’s growing health care needs;
- rightsize the clinical specialty distribution of nurses;
- increase the distribution of nurses to where they are needed most;
- ensure a nursing workforce that is diverse and prepared with the knowledge and skills to address SDOH;
- overcome current and future barriers affecting workforce capacity; and
- anticipate long-term impacts of the COVID-19 pandemic on the nursing workforce.
Conclusion 3-1: A substantial increase in the numbers, types, and distribution of members of the nursing workforce and improvements in their knowledge and skills in addressing social determinants of health are essential to filling gaps in care related to sociodemographic and population factors. These factors include the aging population, the increasing incidence of mental and behavioral health conditions, and the increasing lack of access to primary and maternal health care.
Access to comprehensive health services is an essential precursor to equitable, high-quality health care. Nurses can help advance health care equity and improve health outcomes by assisting people in navigating the health care system, providing close monitoring and follow-up across the care continuum, focusing care on the whole person, and providing care that is appropriate and shows cultural humility.3 In the current system, care is often disjointed. Nurses can provide care management that helps ensure seamless care, serve as advocates for patients and communities, and assist in increasing individuals’ trust in and engagement with the health care system.
Lifting Barriers to Expand the Contributions of Nursing
Nurses can address SDOH and help improve health equity by providing care management and team-based care; expanding the capacity of primary care, including maternal and pediatric care, mental health care, and telehealth; and providing care in school, home, work, and public health settings. Yet, their ability to fulfill this potential is limited by state-level regulations restricting nurse practitioners’ (NPs’) scope of practice. While considerable progress has been made over the past two decades in lifting such regulations, 27 states still do not allow full practice authority for NPs. As of January 2021, 23 states and the District of Columbia allowed full practice authority for NPs, permitting them to prescribe medication, diagnose patients, and provide treatment without the presence of a physician. In 16 states, NPs need a physician’s authority to prescribe medication, and in 11 states, they require physician oversight for all practice.
Conclusion 3-2: Eliminating restrictions on the scope of practice of advanced practice registered nurses and registered nurses so they can practice to the full extent of their education and training will increase the types and amount of high-quality health care services that can be provided to those with complex health and social needs and improve both access to care and health equity.
Designing Better Payment Models
How care is paid for can directly influence access to care. The design of payment systems influences what health care is provided to individuals and communities, where care is provided, and by whom. Positioning health systems to work in partnership with other sectors to meet the complex health and social needs of individuals can help reduce health inequities. However, current payment systems are not designed to pay for services—including those provided by nurses, such as
___________________
3 Cultural humility is “defined by flexibility; awareness of bias; a lifelong, learning-oriented approach to working with diversity; and a recognition of the role of power in health care interactions.”
supporting team-based care and advancing proven interventions and strategies for reducing health disparities—that address social needs and SDOH. Going forward, payment systems need to be redesigned to recognize the value of those services.
Nurses are essential to whole-person care through their vital roles in coordinating and managing care, helping people navigate the health care system, and providing health education, as well as addressing SDOH and advancing health equity. By supporting team-based care, improved communication, and proven interventions and strategies that can reduce health disparities, payment systems can enable nurses to make these essential contributions to improving care and outcomes for all patients.
Conclusion 6-3: Payment mechanisms need to be designed to support the nursing workforce and nursing education in addressing social needs and social determinants of health in order to improve population health and advance health equity.
New payment models, such as accountable care organizations (ACOs), accountable health communities (AHCs), and value-based payment (VBP), can give health care organizations the flexibility to pursue these goals. Changing the ways in which the nation pays for health care will cause discomfort among some, but will also stimulate those seeking innovative ways of maximizing the population’s health. Payment reform represents an opportunity to consider who has access to health care and who does not, what types of services are needed to improve individual and population health, and how the nation’s resources can be used most wisely to these ends.
Strengthening Nursing Education
Nursing education needs to be markedly strengthened to prepare nurses to identify and act on the complex social, economic, and environmental factors that influence health and well-being. In particular, their education needs to provide nursing students with substantive, diverse, and sustained community-based experiences, as well as to substantially reorient curricula and reevaluate hiring and admission practices so as to achieve a diverse faculty and student population.
Nursing organizations have developed guidelines for how nursing education should prepare nurses to address health equity issues and SDOH in a meaningful way. The American Association of Colleges of Nursing’s (AACN’s) Essentials provides an outline for the necessary curriculum content and expected competencies for graduates of baccalaureate, master’s, and doctor of nursing practice (DNP) programs. Yet, despite this guidance and the numerous calls to incorporate equity, population health, and SDOH into undergraduate and graduate nursing education, these and related concepts are currently not well integrated into nursing curricula.
Conclusion 7-1: A curriculum embedded in coursework and experiential learning that effectively prepares students to promote health equity, reduce health disparities, and improve the health and well-being of the population will build the capacity of the nursing workforce.
Nursing is increasingly practiced in community settings, such as schools and workplaces, as well as through home health care and public health clinics. Other innovative care delivery models are situated in libraries and homeless shelters and implemented through telehealth visits. Nursing students are prepared to practice in hospitals, but do not necessarily receive the same level of training and preparation for community and telehealth settings. Education in the community allows nursing students to learn about the broad range of care environments and to work collaboratively with other professionals who work in these environments, including those from nonhealth sectors.
Building a diverse nursing workforce is a critical part of preparing nurses to address SDOH and health equity. While the nursing workforce has steadily grown more diverse, nursing schools need to continue and expand their efforts to recruit and support diverse students that reflect the populations they will serve.
Conclusion 7-4: Successfully diversifying the nursing workforce will depend on holistic efforts to support and mentor/sponsor students and faculty from a wide range of backgrounds, including cultivating an inclusive environment; providing economic, social, professional, and academic supports; ensuring access to information on school quality; and minimizing inequities.
Valuing Community Nursing
School and public health nurses play a vital role in advancing health equity. Adequate funding for these nurses is essential if they are to take on that role. School nurses are front-line health care providers, serving as a bridge between the health care and education systems and other sectors. Whether they are hired by school districts, health departments, or hospitals, school nurses focus on the physical and mental health of students in the context of educational environments. They serve as both essential care providers for individuals and links to broader community health issues through the student populations they serve.
School nurses are a particularly critical resource for students experiencing such challenges as food insecurity, homelessness, and living in impoverished circumstances, for whom the school nurse may be the only health care professional they see regularly. Accordingly, access to a school nurse is a health care equity issue for some students, especially in light of the increasing number of students who have complex health needs. School nurses also are well positioned to work with students and families in their neighborhoods and homes to address individual and family social needs, such as access to care, healthy food, and safe and healthy environments/neighborhoods. More school nurses need the practice authority to address in creative ways the complex health and social needs of the populations they serve.
Likewise, the COVID-19 pandemic has highlighted the pivotal role of nurses in improving health care equity. During the pandemic, public health and hospital nurses have had to work synergistically both to help flatten the infection curve and support mitigation strategies (public health nurses) and to care for the sick and critically ill (inpatient and intensive care unit [ICU] nurses). The pandemic also has heightened the need for team-based care, infection control, person-centered care, and other skills that reflect the strengths of community nurses.
Fostering Nurses’ Roles as Leaders and Advocates
Creating a future in which opportunities to optimize health are more equitable will require disrupting the deeply entrenched prevailing paradigms of health care, which in turn will require enlightened, diverse, courageous, and competent leadership. Nurses have always been key to the health and well-being of patients and communities, but a new generation of nurse leaders is now needed—one that recognizes the importance of diversity and is able to use and build on the increasing evidence base supporting the link between SDOH and health status. Today’s nurses are called on to lead in the development of effective strategies for improving the nation’s health with due attention to the needs of the most underserved individuals, neighborhoods, and communities and the crucial importance of advancing health equity. Implementing change to address SDOH and advance health equity will require the contributions of nurses in all roles and all settings; although no one nurse can successfully implement change without the collabo-
ration of others. In addition to collaboration among members of the nursing profession, the creation of enduring change will require the involvement of patients and community members. Rather than a more hierarchal system of leadership, moreover, collaborative leadership assumes that everyone involved has unique contributions to make and that constructive dialogue and joint resources are needed to achieve ongoing goals.
Conclusion 9-1: Nurse leaders at every level and across all settings can strengthen the profession’s long-standing focus on social determinants of health and health equity to meet the needs of underserved individuals, neighborhoods, and communities and to prioritize the elimination of health inequities.
Racism and discrimination are deeply entrenched in U.S. society and its institutions, and the nursing profession is no exception. Nurse leaders can play an important role in acknowledging the history of racism within the profession and in helping to dismantle structural racism and mitigate the effects of discrimination and implicit bias on health. If they are to take on this role, it will be essential to build a more diverse nursing workforce and support nurses of diverse backgrounds in pursuing leadership roles.
Conclusion 9-4: Nurse leaders have a responsibility to address structural racism, cultural racism, and discrimination based on identity (e.g., sexual orientation, gender), place (e.g., rural, urban), and circumstances (e.g., disability, mental health condition) within the nursing profession and to help build structures and systems at the societal level that address these issues to promote health equity.
Preparing Nurses to Respond to Disasters
The increasing frequency of natural and environmental disasters and public health emergencies, such as the COVID-19 pandemic, reveals in stark detail the critical importance of having a national nursing workforce prepared with the knowledge, skills, and abilities to respond to these events. COVID-19 has revealed deep chasms within an already fragmented U.S. health care system, resulting in significant excess mortality and morbidity, glaring health inequities, and the inability to contain a rapidly escalating pandemic. Most severely—and unfairly—affected are individuals and communities of color, who suffer from the compound disadvantages of racism, poverty, workplace hazards, limited health care access, and preexisting health conditions resulting from the foregoing factors. As other disasters and public health emergencies threaten population health in the decades ahead, articulation of the roles and responsibilities of nurses in disaster response and public health emergency management will be critical to the nation’s capacity to plan for and respond to these types of events.
Conclusion 8-2: A bold and expansive effort, executed across multiple platforms, will be needed to fully support nurses in becoming prepared for disaster and public health emergency response. It is essential to convene experts who can develop a national strategic plan articulating the existing deficiencies in this regard and action steps to address them, and, most important, establishing where responsibility will lie for ensuring that those action steps are taken.
Supporting the Health and Well-Being of Nurses
Nurses’ health and well-being are affected by the demands of their workplace, and in turn affect the quality and safety of the care they provide. Thus, it is essential to address the systems, structures, and policies that create workplace hazards and stresses that lead to burnout, fatigue, and poor physical and mental health among the nursing workforce. With the emergence of COVID-19, the day-to-day demands of nursing have been both illuminated and exacerbated. Nurses are coping with unrealistic workloads; insufficient resources and protective equipment; risk of infection; stigma directed at health care workers; and the mental, emotional, and moral burdens of caring for patients with a new and unpredictable disease and helping with contact tracing and testing. Moreover, if nurses are to contribute to addressing the many social determinants that influence health, they must first feel healthy, well, and supported themselves. Policy makers, employers of nurses, nursing schools, nurse leaders, and nursing associations all have a role to play to this end.
Conclusion 10-1: All environments in which nurses work affect the health and well-being of the nursing workforce. Ultimately, the health and well-being of nurses influence the quality, safety, and cost of the care they provide, as well as organizations and systems of care. The COVID-19 crisis has highlighted the shortcomings of historical efforts to address nurses’ health and well-being.
RECOMMENDATIONS
The committee’s recommendations (see Box S-2) call for change at both the individual and system levels, constituting a call for action to the nation’s largest health care workforce, including nurses in all settings and at all levels, to listen, engage, deeply examine practices, collect evidence, and act to move the country toward greater health equity for all. The committee’s recommendations also are targeted to the actions required of policy makers, educators, health care system leaders, and payers to enable these crucial changes.
FINAL THOUGHTS
In conclusion, the nation will never fully thrive until everyone can live the healthiest possible life. Promoting health and well-being has always been nurses’ business. Thus, it is essential to harness the vast expertise and untapped potential of nurses at every level and in every setting to build healthy communities for all. As evidenced in this report, nurses are bridge builders and collaborators who engage and connect with people, communities, and organizations to promote health and well-being. But they need ongoing support from the systems that educate, train, employ, and enable them to advance health equity. As of this writing, the COVID-19 pandemic has starkly revealed the challenges nurses face every day.
But this crisis has also given some nurses more autonomy, shifted payment models, and sparked overdue conversations about dismantling racism in health care. Policy makers and system leaders must seize this moment to support, strengthen, and transform the largest segment of the health care workforce so nurses can help chart the nation’s course to good health and well-being for all. Over the course of this decade, nurses will face a host of challenges—from addressing the lasting effects of COVID-19 on themselves and their communities to dismantling the racist systems that create and perpetuate inequities. No one is immune from hate and bigotry, but everyone has the capacity for empathy, understanding, and solidarity in a shared hope for a more just and equitable world. The nursing profession is resilient and well positioned to help usher in a new era in which everyone has a chance to live the healthiest possible life.
















