7
Educating Nurses for the Future
You cannot transmit wisdom and insight to another person. The seed is already there. A good teacher touches the seed, allowing it to wake up, to sprout, and to grow.
—Thich Nhat Hanh, global spiritual leader and peace activist
Throughout the coming decade, it will be essential for nursing education to evolve rapidly in order to prepare nurses who can meet the challenges articulated in this report with respect to addressing social determinants of health (SDOH), improving population health, and promoting health equity. Nurses will need to be educated to care for a population that is both aging, with declining mental and physical health, and becoming increasingly diverse; to engage in new professional roles; to adapt to new technologies; to function in a changing policy environment;
and to lead and collaborate with professionals from other sectors and professions. As part of their education, aspiring nurses will need new competencies and different types of learning experiences to be prepared for these new and expanded roles. Also essential will be recruiting and supporting diverse students and faculty to create a workforce that more closely resembles the population it serves. Given the growing focus on SDOH, population health, and health equity within the public health and health care systems, the need to make these changes to nursing education is clear. Nurses’ close connection with patients and communities, their role as advocates for well-being, and their placement across multiple types of settings make them well positioned to address SDOH and health equity. For future nurses to capitalize on this potential, however, SDOH and equity must be integrated throughout their educational experience to build the competencies and skills they will need.
The committee’s charge included examining whether nursing education provides the competencies and skills nurses will need—the capacity to acquire new competencies, to work outside of acute care settings, and to lead efforts to build a culture of health and health equity—as they enter the workforce and throughout their careers. A thorough review of the current status and future needs of nursing education in the United States was beyond the scope of this study, but in this chapter, the committee identifies priorities for the content and nature of the education nurses will need to meet the challenge of addressing SDOH, advancing health equity, and improving population health. Nursing education is a lifelong pursuit; nurses gain knowledge and skills in the classroom, at work, through continuing professional development, and through other formal and informal mechanisms (IOM, 2016b). While the scope of this study precluded a thorough discussion of learning outside of nursing education programs, readers can find further discussion of lifelong learning in A Framework for Educating Health Professionals to Address the Social Determinants of Health (IOM, 2016b), Redesigning Continuing Education in the Health Professions (IOM, 2010), and Exploring a Business Case for High-Value Continuing Professional Development: Proceedings of a Workshop (NASEM, 2018a).
To change nursing education meaningfully so as to produce nurses who are prepared to meet the above challenges in the decade ahead will require changes in four areas: what is taught, how it is taught, who the students are, and who teaches them. This chapter opens with a description of the nursing education system and the need for integrating equity into education, and then examines each of these four areas in turn:
- domains and competencies for equity,
- expanded learning opportunities,
- recruitment of and support for diverse prospective nurses, and
- strengthening and diversification of the nursing faculty.
In addition to changes in these specific areas, there is a need for a fundamental shift in the idea of what constitutes a “quality” nursing education. Currently, National Council Licensure Examination (NCLEX) pass rates are used as the primary indicator of quality, along with graduation and employment rates (NCSBN, 2020a; O’Lynn, 2017). This narrow focus on pass rates has been criticized for diverting time and attention away from other goals, such as developing student competencies, investing in faculty, and implementing innovative curricula (Giddens, 2009; O’Lynn, 2017; Taylor et al., 2014). In addition, the NCLEX is heavily focused on acute care rather than on such areas of nursing as primary care, disease prevention, SDOH, and health equity (NCSBN, 2019). In response to such concerns about the NCLEX, the National Council of State Boards of Nursing (NCSBN) conducted a study to identify additional quality indicators for nursing education programs; indicators were identified in the areas of administration, program director, faculty, students, curriculum and clinical experiences, and teaching and learning resources (Spector et al., 2020). To realize the committee’s vision for nursing education, it will be necessary for nursing schools, accreditors, employers, and students to look beyond NCLEX pass rates and include these types of indicators in the assessment of a quality nursing education.
OVERVIEW OF NURSING EDUCATION
Nurses are educated at universities, colleges, hospitals, and community colleges and can follow a number of educational pathways. Table 7-1 identifies the various degrees that nurses can hold, and describes the programs that lead to each degree and the usual amount of time required to complete them. In 2019, there were more than 200,000 graduates from baccalaureate, master’s, and doctoral nursing programs in the United States and its territories, including 144,659 who received a baccalaureate degree (AACN, 2020a) (see Table 7-2).
Nursing programs are nationally accredited by the Accreditation Commission for Education in Nursing (ACEN); the Commission on Collegiate Nursing Education (CCNE); the Commission for Nursing Education and Accreditation (CNEA); and other bodies focused on specialty areas of nursing, such as midwifery. Graduating registered nurses (RNs) seek licensure as nurses through state boards, and take examinations administered by the NCSBN as graduates with their first professional degree and then as specialists with certification exams offered through specialty organizations. These bodies set minimum standards for nursing programs and establish criteria for certification and licensing, faculty qualifications, course offerings, and other features of nursing programs (Gaines, n.d.).
TABLE 7-1 Pathways in Nursing Education
| Type of Degree | Description of Program |
|---|---|
| Doctor of Philosophy in Nursing (PhD) and Doctor of Nursing Practice (DNP) | PhD programs are research focused, and graduates typically teach and conduct research, although these roles are expanding. DNP programs are practice focused, and graduates typically serve in advanced practice registered nurse (APRN) roles and other advanced clinical positions, including faculty positions. Time to completion: 3−5 years. Bachelor of science in nursing (BSN)- or master of science in nursing (MSN)-to-nursing doctorate options available. |
| Master’s Degree in Nursing (MSN/MS) | Prepares APRNs: nurse practitioners, clinical nurse specialists, nurse midwives, and nurse anesthetists, as well as clinical nurse leaders, educators, administrators, and other areas or roles. Time to completion: 18−24 months. Three years for associate’s degree in nursing (ADN)-to-MSN option. |
| Accelerated BSN or Master’s Degree in Nursing | Designed for students with a baccalaureate degree in another field. Time to completion: 12−18 months for BSN and 3 years for MSN, depending on prerequisite requirements. |
| Bachelor of Science in Nursing (BSN) Registered Nurse (RN) | Educates nurses to practice the full scope of nursing responsibilities across all health care settings. Curriculum provides additional content in physical and social sciences, leadership, research, and public health. Time to completion: 4 years or up to 2 years for ADN/diploma RNs and 3 years for licensed practical nurses (LPNs), depending on prerequisite requirements. |
| Associate’s Degree in Nursing (ADN) (RN) and Diploma in Nursing (RN) | Prepares nurses to provide direct patient care and practice within the legal scope of nursing responsibilities in a variety of health care settings. Offered through community colleges and hospitals. Time to completion: 2 to 3 years for ADN (less in the case of LPN entry) and 3 years for diploma (all hospital-based training programs), depending on prerequisite requirements. |
| Licensed Practical Nurse (LPN)/Licensed Vocational Nurse (LVN) | Trains nurses to provide basic care (e.g., take vital signs, administer medications, monitor catheters, and apply dressings). LPN/LVNs work under the supervision of physicians and RNs. Offered by technical/vocational schools and community colleges. Time to completion: 12−18 months. |
SOURCES: Adapted from IOM, 2011 (AARP, 2010. Courtesy of AARP. All rights reserved).
The Need for Nursing Education on Social Determinants of Health and Health Equity
A report of the Institute of Medicine (IOM) from nearly two decades ago asserts that all health professionals, including nurses, need to “understand determinants of health, the link between medical care and healthy populations, and professional responsibilities” (IOM, 2003, p. 209). The literature is replete with calls for all nurses to understand concepts associated with health equity, such as disparities, culturally competent care, equity, and social justice. For example, Morton and colleagues (2019) identify essential content to prepare nurses for
TABLE 7-2 Number of Graduates from Nursing Programs in the United States and Territories, 2019
| Type of Degree or Certificate | Number of Graduates |
|---|---|
| Licensed practical nurse (LPN)/licensed vocational nurse (LVN)a | 48,234 |
| Associate’s degree in nursing (ADN)a | 84,794 |
| Generic entry-level baccalaureate (includes accelerated BSN and LPN-to-BSN) | 78,394 |
| RN-to-baccalaureate programs | 66,265 |
| Master’s | 49,895 |
| Doctor of nursing practice (DNP) | 7,944 |
| PhD | 804 |
| Postdoctoral | 57 |
a Number of first-time NCLEX test takers, which is proxy for new graduates (NCSBN, 2020a).
SOURCE: AACN, 2020a.
community-based practice, including SDOH, health disparities/health equity, cultural competency, epidemiology, community leadership, and the development of enhanced skills in community-based settings. O’Connor and colleagues (2019) call for an inclusive educational environment that prepares nurses to care for diverse patient populations, including the study of racism’s impacts on health from the genetic to the societal level, systems of marginalization and oppression, critical self-reflection, and preparation for lifelong learning in these areas. And Thornton and Persaud (2018) state that the content of nursing education should include instruction in cultural sensitivity and culturally competent care, trauma-informed care and motivational interviewing, screening for social needs, and referring for services. These calls align with the Health Resources and Services Administration’s (HRSA’s) most recent strategic plan, which prioritizes the development of a health care workforce that is able to address current and emerging needs for improving equity and access (HRSA, 2019). Additionally, recommendations of the National Advisory Council on Nurse Education and Practice (NACNEP) (2016) include that population health concepts be incorporated into nursing curriculum and that undergraduate programs create partnerships with HRSA, the U.S. Department of Veterans Affairs (VA), and the Indian Health Service (IHS), agencies that serve rural and frontier areas, to increase students’ exposure to different competencies, experiences, and environments.
In concert with these perspectives and recommendations, nursing organizations have developed guidelines for how nursing education should prepare nurses to work on health equity issues and address SDOH. In 2019, the National League for Nursing (NLN) issued a Vision for Integration of the Social Determinants of Health into Nursing Education Curricula, which describes the importance of SDOH to the mission of nursing and makes recommendations for how SDOH should be integrated into nursing education (see Box 7-1).
As described in Chapter 9, the American Association of Colleges of Nursing’s (AACN’s) Essentials1 provides an outline for the necessary curriculum content and expected competencies for graduates of baccalaureate, master’s, and doctor of nursing practice (DNP) programs. Essentials identifies “Clinical Prevention and Population Health” as one of the nine essential areas of baccalaureate nursing education. Among other areas of focus, Essentials calls for baccalaureate programs to prepare nurses to
- collaborate with other health care professionals and patients to provide spiritually and culturally appropriate health promotion and disease and injury prevention interventions;
- assess the health, health care, and emergency preparedness needs of a defined population;
- collaborate with others to develop an intervention plan that takes into account determinants of health, available resources, and the range of activities that contribute to health and the prevention of illness, injury, disability, and premature death;
- participate in clinical prevention and population-focused interventions with attention to effectiveness, efficiency, cost-effectiveness, and equity; and
- advocate for social justice, including a commitment to the health of vulnerable populations and the elimination of health disparities.
Curriculum content and expected competencies laid out in Essentials for master’s- and DNP-level nursing education also address SDOH, disparities, equity, and social justice (AACN, 2006, 2011). While Essentials only guides baccalaureate, master’s, and DNP programs, the document’s emphasis on health equity and SDOH demonstrates the importance of these topics to the nursing profession as a whole.
As of 2020, AACN has been shifting toward a competency-based curriculum. As part of this effort, AACN published a draft update to Essentials that identifies 10 domains for nursing education: knowledge for nursing practice; person-centered care; population health; scholarship for nursing discipline; quality and safety; interprofessional partnerships; systems-based practice; informatics and health care technologies; professionalism; and personal, professional, and leadership development. Within these 10 domains are specific competencies that AACN believes are essential for nursing practice (AACN, 2020b), including
- engage in effective partnerships,
- advance equitable population health policy,
- demonstrate advocacy strategies,
___________________
1 See https://www.aacnnursing.org/Education-Resources/AACN-Essentials (accessed April 13, 2021).
- use information and communication technologies and informatics processes to deliver safe nursing care to diverse populations in a variety of settings, and
- use knowledge of nursing and other professions to address the health care needs of patients and populations.
Nurses themselves have also indicated the need for more education and training on these topics. The 2018 National Sample Survey of Registered Nurses (NSSRN) asked the question, “As of December 31, 2017, what training topics would have helped you do your job better?” Figure 7-1 shows the percentage of six different training topics that RNs said would help them do their job better. Overall, RNs working in schools, public health, community health, and emergency and urgent care were more likely than RNs working in all other employment settings listed in Figure 7-1 to indicate that they could have done their job better if they had received training in SDOH, population health, working in underserved communities, caring for individuals with complex health and social needs, and especially mental health. These results could reflect RNs encountering increasingly complex individuals and populations, rising numbers of visits and caseloads, the fact that the RNs working in these settings frequently provide
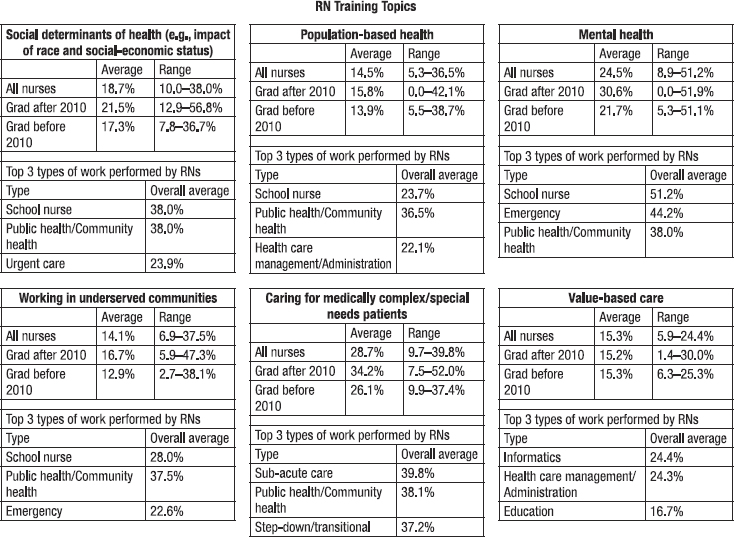
SOURCE: Calculations based on the 2018 National Sample Survey of Registered Nurses (HRSA, 2020).
care for people facing multiple social risk factors that harm their health and well-being, or inadequacy of the training in these areas that RNs had received. RNs—particularly those working in informatics, health care management and administration, and education—also indicated that training in value-based care would have been helpful. Additionally, RNs who had graduated after 2010 were more likely than those who had graduated before then to indicate that they could have done their job better with training across all of these topics.
Nurse practitioners (NPs) have also indicated the need for more training in SDOH. In response to the 2018 NSSRN question described above, NPs working in public health and community health, emergency and urgent care, education, and long-term care reported that they could have done their job better if they had received training in SDOH, mental health, working in underserved communities, and providing care for medically complex/special needs. Across all types of practice settings, one-third felt that training in mental health issues would have helped them do their job better, while very few NPs indicated that training in value-based care would have been helpful. Additionally, NPs who had graduated since 2010 were more likely than those who had graduated before then to indicate that they would have benefited from training in these topics. Figure 7-2 shows the percentage of six different training topics that NPs mentioned would have helped them do their job better.
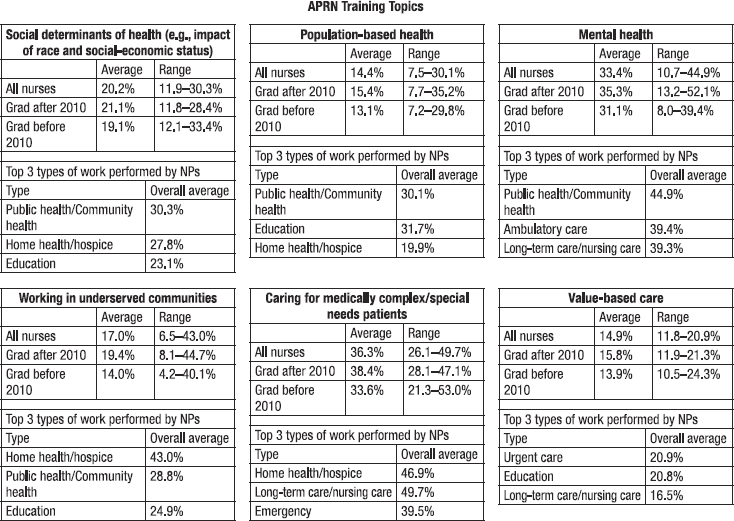
SOURCE: Calculations based on the 2018 National Sample Survey of Registered Nurses (HRSA, 2020).
The Need for Integration of Social Determinants of Health and Health Equity into Nursing Education
Despite guidelines from both the American Association of Colleges of Nursing (AACN) and the National League for Nursing (NLN) and numerous calls for including equity, population health, and SDOH in nursing education, SDOH and related concepts are not currently well integrated into undergraduate and graduate nursing education. Nor has the degree to which nurses are prepared and educated in these areas been studied systematically (NACNEP, 2019; Tilden et al., 2018). The committee was unable to locate a central repository of information about the coursework and other educational experiences available to nursing students across types of programs and institutions, or any other source of systematic analysis of nursing curricula. This lack of information about nursing preparation programs limits the conclusions that can be drawn about them. Thus, the discussion in this chapter is based on the assumption that some nursing programs are likely already pursuing many of the goals identified herein, but that this critically important content is not yet standard practice throughout nursing education.
One way to explore whether and how health equity and related concepts are currently integrated into nursing education is to look at accreditation standards. While the standards do not detail every specific topic to be covered in nursing curricula, they do set expectations, convey priorities, and identify important areas of study. For example, the accreditation standards of the CCNE state that advanced practice registered nurse (APRN) programs must include study of advanced physiology, advanced health assessment, and advanced pharmacology (CCNE, 2018). Accreditation standards could be used to prioritize the inclusion of health equity and SDOH in nursing curriculum; however, this is not currently the case. The CCNE standards state that accredited programs must incorporate the AACN Essentials into their curricula, and while these standards do not specifically mention equity, SDOH, or other relevant concepts (CCNE, 2018), that is expected to change to correspond with the updates to the Essentials described previously (see Box 7-1). CNEA’s accreditation standards likewise include no mention of population health, SDOH, or health equity (NLN, 2016), although a more recent document from NLN makes a strong case for the integration of SDOH into nursing education curricula (NLN, 2019). ACEN’s associate’s and baccalaureate standards call for inclusion of “cultural, ethnic, and socially diverse concepts” in the curriculum; the master’s and doctoral standards require that curriculum be “designed so that graduates of the program are able to practice in a culturally and ethnically diverse global society,” but do not address health equity, population health, or SDOH.
Another approach for examining the inclusion of these concepts in nursing education is to look at exemplar programs. As part of the Future of Nursing: Campaign for Action, the Robert Wood Johnson Foundation commissioned a study of best practices in nursing education to support population health (Campaign for
Action, 2019b). That report notes that although many nursing programs reported including population health content in their curriculum, few incorporated the topic substantially. However, the report also identifies exemplars of programs with promising population health models. These exemplars include Oregon Health & Science University, which incorporates population health throughout the curriculum as a key competency; Rush University, which incorporates cultural competence throughout the curriculum; and Thomas Jefferson University, which offers courses in health promotion, population health, health disparities, and SDOH. NACNEP has also examined exemplars of nursing programs that incorporate health equity and SDOH into their curricula (NACNEP, 2019). The programs highlighted include the University of Pennsylvania School of Nursing, which has a course called Case Study—Addressing the Social Determinants of Health: Community Engagement Immersion (Schroeder et al., 2019). This course offers experiential learning opportunities that focus on SDOH in vulnerable and underserved populations and helps students design health promotion programs for these communities. The school also offers faculty education in SDOH.
As far as the committee was able to determine, most programs include content on SDOH in community or public health nursing courses. However, this material does not appear to be integrated thoroughly into the curriculum in the majority of programs, nor could the committee identify well-established designs for curricula that address this content outside of community health rotations (Campaign for Action, 2019b; Storfjell et al., 2017; Thornton and Persaud, 2018). In the committee’s view, a single course in community and/or public health nursing is insufficient preparation for creating a foundational understanding of health equity and for preparing nurses to work in the wide variety of settings and roles envisioned in this report. Ideally, education in these concepts would be integrated throughout the curriculum to give nurses a comprehensive understanding of the social determinants that contribute to health inequities (NACNEP, 2019; NLN, 2019; Siegel et al., 2018). Moreover, academic content alone is insufficient to provide students with the knowledge, skills, and abilities they need to advance health equity; rather, expanded opportunities for experiential and community learning are critical for building the necessary competencies (Buhler-Wilkerson, 1993; Fee and Bu, 2010; NACNEP, 2016; Sharma et al., 2018). All those involved in nursing education—administrators, faculty, accreditors, and students—need to understand that health equity is a core component of nursing, no less important than alleviating pain or caring for individuals with acute illness. Graduating students need to understand and apply knowledge of the impact of such issues as classism, racism, sexism, ageism, and discrimination and to be empowered to advocate on these issues for people who they care for and communities.
As currently constituted, then, nursing education programs fall short of conveying this information sufficiently in the curriculum or through experiential learning opportunities. Yet, the existing evidence on what nursing education programs offer is scant. Research is therefore needed to assess whether and how
many nursing programs are offering sufficient coursework and learning opportunities related to SDOH and health equity and to examine the extent to which graduating nurses have the competencies necessary to address these issues in practice.
The Need for BSN-Prepared Nurses
The 2011 The Future of Nursing report includes the recommendation that the percentage of nurses who hold a baccalaureate degree or higher be increased to 80 percent by 2020. The report gives several reasons for this goal, including that baccalaureate-prepared nurses are exposed to competencies including health policy, leadership, and systems thinking; they have skills in research, teamwork, and collaboration; and they are better equipped to meet the increasingly complex demands of care both inside and outside the hospital (IOM, 2011, p. 170). In 2011, 50 percent of employed nurses held a baccalaureate degree or higher; as of 2019, that proportion had increased to 59 percent (Campaign for Action, 2020). Both the number of baccalaureate programs and program enrollment have increased substantially since 20112 (AACN, 2019a), and the number of RNs who went on to receive BSNs in RN-to-BSN programs increased 236 percent between 2009 and 2019 (Campaign for Action, n.d.). However, the goal of 80 percent of nurses holding a BSN was still not achieved by 2020, for a number of reasons. Although the proportion of new graduates with a BSN is higher than the proportion of existing nurses with a BSN, the percentage of new graduates joining the nursing workforce each year is small. Given this ratio, it would have been “extraordinarily difficult” to achieve the goal of 80 percent by 2020 (IOM, 2016a; McMenamin, 2015). Nurses already in the workforce face barriers to pursuing a BSN, including time, money, work–life balance, and a perception that additional postlicense education is not worth the effort (Duffy et al., 2014; Spetz, 2018). Moreover, schools and programs have limited capacity for first-time nursing students and ADN, LPN nurses, or RNs without BSN degrees (Spetz, 2018).
Nonetheless, the goal of achieving a nursing workforce in which 80 percent of nurses hold a baccalaureate degree or higher remains relevant, and continuing efforts to increase the number of nurses with a BSN are needed. Across the globe, the proportion of BSN-educated nurses is correlated with better health outcomes (Aiken et al., 2017; Baker et al., 2020), and there are clear differences as well as similarities between associate’s degree in nursing (ADN) programs and BSN programs. In particular, BSN programs are more likely to cover topics relevant to liberal education, organizational and systems leadership, evidence-based practice, health care policy, finance and regulatory environments, interprofessional collaboration, and population health (Kumm et al., 2014). Accelerated, nontraditional, and other pathways to the BSN degree are discussed later in this chapter.
___________________
2 See Chapter 3 for demographic information on employed nurses in the United States.
The Need for PhD-Prepared Nurses
There are two types of doctoral degrees in nursing: the PhD and the DNP. The former is designed to prepare nurse scientists to conduct research, whereas the latter is a clinically focused doctoral degree designed to prepare graduates with advanced competencies in leadership and management, quality improvement, evidence-based practice, and a variety of specialties. PhD-prepared nurses are essential to the development of the research base required to support evidence-based practice and add to the body of nursing knowledge, and DNP-educated nurses play a key role in translating evidence into practice and in educating nursing students in practice fundamentals (Tyczkowski and Reilly, 2017) (see Chapter 3 for further discussion of the role of DNPs).
The number of nurses with doctoral degrees has grown rapidly since the 2011 The Future of Nursing report was published (IOM, 2011). As a proportion of doctorally educated nurses, however, the number of PhD graduates has remained nearly flat. In 2010, there were 1,282 graduates from DNP programs and 532 graduates receiving a PhD in nursing. By 2019, the number of DNP graduates had grown more than 500 percent to 7,944, while the number of PhD graduates had grown about 50 percent to 804 (AACN, 2011, 2020a).
The slow growth in PhD-prepared nurses is a major concern for the profession and for the nation, because it is these nurses who serve as faculty at many universities and who systematically study issues related to health and health care, including the impact of SDOH on health outcomes, health disparities, and health equity. PhD-prepared nurses conduct research on a wide variety of issues relating to SDOH, including the effect of class on children’s health; linguistic, cultural, and educational barriers to care; models of care for older adults aging in place; and gun violence (Richmond and Foman, 2018; RWJF, 2020; Szanton et al., 2014). Nurse-led research provided evidence-based solutions in the early days of the COVID-19 pandemic for such challenges as the shift to telehealth care, expanding demand for health care workers, and increased moral distress (Lake, 2020). However, Castro-Sánchez and colleagues (2021) note a dearth of nurse-led research specifically related to COVID-19; they posit that this gap can be attributed to workforce shortages, a lack of investment in clinical academic leadership, and the redeployment of nurses into clinical roles. More PhD-prepared nurses are needed to conduct research aimed at improving clinical and community health, as well as to serve as faculty to educate the next generation of nurses (Broome and Fairman, 2018; Fairman et al., 2020; Greene et al., 2017).
Nursing practice is dependent on a robust pipeline of research to advance evidence-based care, inform policy, and address the health needs of people and communities (Bednash et al., 2014). The creation of the BSN-to-PhD direct entry option has helped produce more research-oriented nurse faculty (Greene et al., 2017), but time, adequate faculty mentorship, mental health issues, and financial hardships, including the cost of tuition, are barriers for nurses pursuing these
advanced degrees (Broome and Fairman, 2018; Fairman et al., 2020; Squires et al., 2013). One approach for increasing the number of PhD-prepared nurses is the Future of Nursing Scholars program, which successfully graduated approximately 200 PhD students through an innovative accelerated 3-year program (RWJF, 2021). Similar programs have been funded by such foundations as the Hillman Foundation and Jonas Philanthropies to help stimulate the pipeline, build capacity (especially in health policy) among graduates, and model innovative curricular approaches (Broome and Fairman, 2018; Fairman et al., 2020).
DOMAINS AND COMPETENCIES FOR EQUITY
As noted earlier, a number of existing recommendations specify what nurses need to know to address SDOH and health inequity in a meaningful way. In addition, the Future of Nursing: Campaign for Action surveyed and interviewed faculty and leaders in nursing and public health, asking about core content and competencies for all nurses (Campaign for Action, 2019b). Respondents specifically recommended that nursing education cover seven areas:
- policy and its impact on health outcomes;
- epidemiology and biostatistics;
- a basic understanding of SDOH and illness across populations and how to assess and intervene to improve health and well-being;
- health equity as an overall goal of health care;
- interprofessional team building as a key mechanism for improving population health;
- the economics of health care, including an understanding of basic payment models and their impact on services delivered and outcomes achieved; and
- systems thinking, including the ability to understand complex demands, develop solutions, and manage change at the micro and macro system levels.
Drawing on all of these recommendations, guidelines, and perspectives, as well as looking at the anticipated roles and responsibilities outlined in other chapters of this report, the committee identified the core concepts pertaining to SDOH, health equity, and population health that need to be covered in nursing school and the core knowledge and skills that nurses need to have upon graduation. For consistency with the language used by the AACN, these are referred to, respectively, as “domains” (see Box 7-2) and “competencies” (see Box 7-3). The domains in Box 7-2 are fundamental content that the committee believes can no longer be covered in public health courses alone, but need to be incorporated and applied by nursing students throughout nursing curricula. All nurses, regardless of setting or type of nursing, need to understand and be prepared to address the underlying barriers to better health in their practice.
The committee believes that incorporation of these domains and competencies can guide expeditious and meaningful changes in nursing education. The committee acknowledges that making room for these concepts will inevitably require eliminating some existing material in nursing education. The committee does not believe that it is the appropriate entity to identify what specific curriculum changes should be made; a nationwide evaluation will be needed to ensure that nursing curricula are preparing the future workforce with the skills and competencies they will need. The committee also acknowledges that nursing programs differ in length, and that an ADN program cannot cover SDOH equity to the same extent as a BSN program. The specific knowledge and skills a nurse will need will vary depending on her or his level of nursing education. For example, a nurse with a BSN may need to understand and be able to use the technologies that are relevant to his or her area of work (e.g., telehealth applications, electronic health records [EHRs], home monitors), while an APRN may need a deeper understanding of how to analyze health records in order to provide care and monitor health status for populations outside clinical settings.
Nonetheless, nursing education at all levels—from licensed practical nurse (LPN) to ADN to BSN and beyond—needs to incorporate and integrate the domains and competencies in Boxes 7-2 and 7-3 to the extent possible so as to develop knowledge and skills that will be relevant and useful to nurses and essential to achieving equity in health and health care. Given the relationship among SDOH, social needs, and health outcomes and the increasing focus of health care systems on addressing these community and individual needs, the domains and competencies identified here are essential to ensure that all nurses understand and can apply concepts related to these issues; work effectively with people, families, and communities across the spectrum of SDOH; promote physical, mental, and social health; and assume leadership and entrepreneurial roles to create solutions, such as by fostering partnerships in the health and social sectors, scaling successful interventions, and engaging in policy development. While none of the domains listed in Box 7-2 are new to nursing, the health inequities that have become increasingly visible—especially as a result of the COVID-19 pandemic—demand that these domains now be substantively integrated into the fabric of nursing education and practice.
Many sources highlight both the challenges faced by front-line graduates when confronted with these issues, and the reality that many nursing schools lack faculty members with the knowledge and competencies to educate nurses effectively on these issues (Befus et al., 2019; Effland et al., 2020; Hermer et al., 2020; Levine et al., 2020; Porter et al., 2020; Rosa et al., 2019; Valderama-Wallace and Apesoa-Varano, 2019). To remedy the latter gap, educators need to have a clear understanding of these issues and their links to both educational and patient outcomes (see the section below on strengthening and diversifying the nursing faculty). It is important to note as well that some of these topics, including the connections among implicit biases, structural racism, and health equity, may be difficult for educators and students to discuss (see Box 7-4).
Given the limited scope of this report, the committee has chosen to highlight three of the competencies from Box 7-3 in this section.3 The first is delivering person-centered care to diverse populations. As the United States becomes increasingly diverse, nurses will need to be aware of their own implicit biases and be able to interact with diverse patients, families, and communities with empathy and humility. The second is learning to collaborate across professions, disciplines, and sectors. As discussed previously in this report, addressing SDOH is necessarily a multisectoral endeavor given that these determinants go beyond health to include such issues as housing, education, justice, and the environment. The third is continually adapting to new technologies. Advances in technology are reshaping both health care and education, and making it possible for both to
___________________
3 For further discussion of domains and competencies, see AACN, 2020b; Campaign for Action, 2019b; IOM, 2016b; NACNEP, 2019; NLN, 2019; Thornton and Persaud, 2018.
be delivered in nontraditional settings and nontraditional ways. In the present context, technology can expand access to underserved populations of patients and students—for example, telehealth and online platforms can be used to connect with those living in rural areas—but it can also exacerbate existing disparities and inequities. Nurses need to understand both the promises and perils of technology, and be able to adapt their practice and learning accordingly.
Delivering Person-Centered Care and Education to Diverse Populations
As discussed in Chapter 2, people’s family and cultural background, community, and other experiences may have profound impacts on their health. Given the increasing diversity of the U.S. population, it is critical that nurses understand the impact of these factors on health, can communicate and connect with people of different backgrounds, and can be self-reflective about how their own beliefs and biases may affect the care they provide. To this end, the committee believes it is essential that nursing education include the concepts of cultural humility and implicit bias as a thread throughout the curriculum.
An integral part of learning about these concepts is an opportunity to reflect on what one is learning and to draw connections with past learning and experiences. Researchers have established that instruction that guides students in reflection helps reinforce skills and competencies (see, e.g., NASEM, 2018c). This idea has been explored in the context of education in health professions and has been identified as a valuable way to foster understanding of health equity and SDOH (IOM, 2016b; Mann et al., 2007). While the strategies, goals, and structure of such reflection may vary, the process in general helps learners in health care settings examine their own values, assumptions, and beliefs (El-Sayed and El-Sayed, 2014; Scheel et al., 2017). In the course of structured reflection, for example, students might consider how such issues as racism, implicit bias, trauma, and policy affect the care people receive and create conditions for poor health, or how their own experiences and identities influence the care they provide.
Cultural Humility
In recent years, the focus in discussions of patient care has shifted from cultural competency to cultural humility (Barton et al., 2020; Brennan et al., 2012; Kamau-Small et al., 2015; Periyakoil, 2019; Purnell et al., 2018; Walker et al., 2016). The concept of cultural competency has been interpreted by some as limited for a number of reasons. First, it implies that “culture” is a technical skill in which clinicians can develop expertise, and it can become a series of static dos and don’ts (Kleinman and Benson, 2006). Second, the concept of cultural competency tends to promote a colorblind mentality that ignores the role of power, privilege, and racism in health care (Waite and Nardi, 2017). Third,
cultural competency is not actively antiracist but instead leaves institutionalized structures of White privilege and racism intact (Schroeder and DiAngelo, 2010).
In contrast, cultural humility is defined by flexibility, a lifelong approach to learning about diversity, and a recognition of the role of individual bias and systemic power in health care interactions (Agner, 2020). Cultural humility is considered a self-evaluating process that recognizes the self within the context of culture (Campinha-Bacote, 2018). The concept of cultural humility can be woven into most aspects of nursing and interprofessional education. For example, case studies in which students learn about the experience of a particular disease or strategies for disease prevention can be designed to model culturally humble approaches in the provision of nursing care and the avoidance of stereotypical thinking (Foronda et al., 2016; Mosher et al., 2017). One effective approach to cultivating cultural humility is to accompany experiential learning opportunities or case studies with reflection that expands learning beyond skills and knowledge. This includes questioning current practices and proposing changes to improve the efficiency and quality of care, equality, and social justice (Barton et al., 2020; Foronda et al., 2013). Programs designed to develop nurses’ cultural sensitivity and humility, as well as cultural immersion programs, have been developed, and research suggests that such programs can effectively develop skills that strengthen nurses’ confidence in treating diverse populations, improve patient and provider relationships, and increase nurses’ compassion (Allen, 2010; Gallagher and Polanin, 2015; Sanner et al., 2010).
Implicit Bias
Implicit bias is an unconscious or automatic mental association made between members of a group and an attribute or evaluation (FitzGerald and Hurst, 2017). For example, a clinician may unconsciously view White patients as more medically compliant than Black patients (Sabin et al., 2008). These types of biases not only can have consequences for individual health outcomes (Aaberg, 2012; Linden and Redpath, 2011) but also may play a role in maintaining or exacerbating health disparities (Blair et al., 2011). There are many resources available for implicit bias awareness and training; for example, Harvard University offers a number of Implicit Association Tests (IATs), the Institute for Healthcare Improvement offers free online resources to address implicit bias, and the AACN offers implicit bias workshops for nurses (AACN, n.d.; Foronda et al., 2018).
Evidence on the use of implicit bias training is limited. One review of the use of an IAT in health professions education found that the test had contrasting uses, with some curricula using it as a measure of implicit bias and others using it to initiate discussions and reflection. The review found a dearth of research on the use of IATs; the authors note that the nature of implicit bias is highly complex and cannot necessarily be reduced to the “time-limited” use of an IAT (Sukhera et al., 2019). A systematic review of interventions designed to reduce implicit bias
found that many such interventions are ineffective, and some may even increase implicit biases. The authors note that while there is no clear path for reducing biases, the lack of evidence does not weaken the case for “implementing widespread structural and institutional changes that are likely to reduce implicit biases” (FitzGerald et al., 2019). One promising model is an intervention that helps participants break the “prejudice habit” (Devine et al., 2012). This multifaceted intervention, which includes situational awareness of bias, education about the consequences of bias, strategies for reducing bias, and self-reflection, has been shown to reduce implicit racial bias for at least 2 months (Devine et al., 2012). Clearly, more research is needed in this area.
Learning to Collaborate Across Professions, Disciplines, and Sectors
As discussed in Chapter 9, eliminating health disparities will require the active engagement and advocacy of a broad range of stakeholders working in partnership to address the drivers of structural inequities in health and health care (NASEM, 2017). In these efforts, nurses may lead or work with people from a variety of professions, disciplines, and sectors, including, for example, physicians, social workers, educators, policy makers, lawyers, faith leaders, government employees, community advocates, and community members. Working across sectors, especially as they relate to SDOH (food insecurity, transportation barriers, housing, etc.), is a critical competence. Collaboration among these types of stakeholders has multiple benefits, including broader expertise and perspective, the capacity to address wide-ranging social needs, the ability to reach underserved populations, and sustainability and alignment of efforts (see Chapter 9 for further discussion). A traditional nursing education, which focuses on what is taught rather than on building competencies, is unlikely to give students the understanding of broader social, political, and environmental contexts that is necessary for working in these types of strategic partnerships (IOM, 2016b). If nursing students are to be prepared to practice interprofessionally after graduation, they must be given opportunities to collaborate with others before graduation (IOM, 2013) and to build the competencies they will need for collaborative practice. The Interprofessional Education Collaborative (IPEC) identified four core competencies for interprofessional collaborative practice (IPEC, 2016). While these competencies were developed specifically to prepare students for interprofessional practice within health care, they are also applicable to broader collaborations among other professions, disciplines, and sectors both within and outside of health care:
- Work with individuals of other professions to maintain a climate of mutual respect and shared values.
- Use the knowledge of one’s own role and those of other professionals to appropriately assess and address the health care needs of patients and to promote and advance the health of populations.
- Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease.
- Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles in planning, delivering, and evaluating patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable.
There are opportunities for nursing students to gain interprofessional and multisector collaborative competencies through both experiential learning in the community (discussed in detail below) and classroom work. Increasingly, nursing schools are working with other institutions to offer students classes in which they learn with or from students and professionals in other disciplines. For example, the University of Michigan Center for Interprofessional Education offers courses in such topics as health care delivery in low- and middle-income countries, social justice, trauma-informed practice, interprofessional communication, and teamwork. Courses are open to students from the schools of social work, pharmacy, medicine, nursing, dentistry, physical therapy, public health, and business.4
Despite the benefits of interprofessional education, however, there are barriers that affect the implementation of such programs in health professions education, including different schedules, lack of meeting space, incongruent curricula plans, faculty not trained to teach interprofessionally, faculty overload, and the challenge of providing adequate opportunities for all levels of students (NLN, 2015a). The use of simulation has been proposed as a vehicle for overcoming such barriers to impart interprofessional collaborative competencies (NLN, 2013); a systematic review of the evidence found that this approach can be effective (Marion-Martins and Pinho, 2020). Nurses can also gain interprofessional experience by pursuing dual degrees. For example, the University of Pennsylvania offers dual degrees that combine nursing with health care management, bioethics, public health, law, or business administration.
Continually Adapting to New Technologies
Nurses can use a wide variety of existing and emerging technologies and tools to address SDOH and provide high-quality care to all patients (see Box 7-5). Broadly speaking, these technologies and tools fall into three categories: patient-facing, clinician-facing, and data analytics. Patient- and clinician-facing tools collect data and help providers and patients connect and make decisions
___________________
4 Not all courses are open to students from all schools.
about care. Data analytics uses data, collected from patients or other sources, to analyze trends, identify disparities, and guide policy decisions. Beginning as students, all nurses need to be familiar with these technologies, be able to engage with patients or other professionals around their appropriate use, and understand how their use has the potential to exacerbate inequalities.
Patient-facing technologies include apps and software, such as mobile and wearable health devices, as well as telehealth and virtual visit technologies (FDA, 2020). These tools allow nurses and other health care providers to expand their reach to those who might otherwise not have access because of geography, transportation, social support, or other challenges. For example, telehealth and mobile apps allow providers to see people in their homes, mitigating such barriers to care as transportation while also helping providers understand people in the context of their everyday lives. Essential skills for nurses using these new tools will include
the ability to project a caring relationship through technology (Massachusetts Department of Higher Nursing Education Initiative, 2016) and to use technology to personalize care based on patient preferences, technology access, and individual needs (NLN, 2015b). The role of telehealth and the importance of training nurses in this technology have been recognized for several years (NONPF, 2018; Rutledge et al., 2017), but the urgent need for telehealth services during the COVID-19 pandemic has made it “imperative” to include telehealth training in nursing curricula (Love and Carrington, 2020). Moreover, it is anticipated that the shift to telehealth for some types of care will become a permanent feature of the health care system in the future (Bestsennyy et al., 2020).
Clinician-facing technologies include EHRs, clinical decision support tools, mobile apps, and screening and referral tools (Bresnick, 2017; CDC, 2018; Heath, 2019). A number of available digital technologies can facilitate the collection and integration of data on social needs and SDOH and help clinicians hold compassionate and empathetic conversations about those needs (AHA, 2019; Giovenco and Spillane, 2019). In 2019, for example, Kaiser Permanente launched its Thrive Local network (Kaiser Permanente, 2019), which can be used to screen for social needs and connect people with community resources that can meet these needs. The system is integrated with the EHR, and it is capable of tracking referrals and outcomes to measure whether needs are being met; these data can then be used to continuously improve the network.
Nurses will need to understand how and when to use these types of tools, and can leverage their unique understanding of patient and community needs to improve and expand them. As described in Chapter 10, such technologies as EHRs and clinical alarms can burden nurses and contribute to workplace stress. However, nurses have largely been left out of conversations about how to design and use these systems. For example, although nurses are one of the primary users of EHR systems, little research has been conducted to understand their experiences with and perceptions of these systems, which may be different from those of other health care professionals (Cho et al., 2016; Higgins et al., 2017). Out of 346 usability studies on health care technologies conducted between 2003 and 2009, only 2 examined use by nurses (Yen and Bakken, 2012). Educating nurses to understand and assess the benefits and drawbacks of health care technologies and have the capacity to help shape and revamp them can ultimately improve patient care and the well-being of health professionals.
Tools for data analytics are increasingly important for improving patient care and the health of populations (Ibrahim et al., 2020; NEJM Catalyst, 2018). Analysis of large amounts of data from such sources as EHRs, wearable monitors, and surveys can help in detecting and tracking disease trends, identifying disparities, and finding patterns of correlation (Breen et al., 2019; NASEM, 2016a; Shiffrin, 2016). The North Carolina Institute for Public Health, for example, collaborated with a local health system in analyzing data to inform a community health improvement plan (Wallace et al., 2019). Data on 12 SDOH indicators were sourced
from the American Community Survey and mapped by census tract. The mapping provided a visualization of the disparities in the community and allowed the health system to focus its efforts strategically to improve community health. The North Carolina Department of Health and Human Services later replicated this strategy across the entire state (NCDHHS, 2020).
There are opportunities for nurses to specialize in this type of work. For example, nursing informatics is a specialized area of practice in which nurses with expertise in such disciplines as information science, management, and analytical sciences use their skills to assess patient care and organizational procedures and identify ways to improve the quality and efficiency of care. In the context of SDOH, nursing informaticists will be needed to leverage artificial intelligence and advanced visualization methods to summarize and contextualize SDOH data in a way that provides actionable insights while also eliminating bias and not overwhelming nurses with extraneous information. Big data are increasingly prevalent in health care, and nurses need the skills and competencies to capitalize on its potential (Topaz and Pruinelli, 2017). Even nurses who do not specialize in informatics will need to understand how the analysis of massive datasets can impact health (Forman et al., 2020; NLN, 2015b). Investments in expanding program offerings, certifications, and student enrollment will be needed to meet the demand for nurses with such skills.
As noted, however, despite its promise for improving patient care and community health, technology can also exacerbate existing disparities (Ibrahim et al., 2020). For example, people who lack access to broadband Internet and/or devices are unable to take advantage of such technologies as remote monitoring and telehealth appointments (Wise, 2012). Older adults, people with limited formal education, those living in rural and remote areas, and the poor are less likely to have access to the Internet. As health care becomes more reliant on technology, these groups are likely to fall behind (Arcaya and Figueroa, 2017). In addition, such technologies as artificial intelligence and algorithmic decision-making tools may exacerbate inequities by reflecting existing biases (Ibrahim et al., 2020). Nursing education needs to prepare nurses to understand these potential downsides of technology in order to prevent and mitigate them. This has become a particularly critical issue during the COVID-19 pandemic, with the rapid shift to telehealth potentially having consequences for those with low digital literacy, limited English proficiency, and a lack of access to the Internet (Velasquez and Mehrotra, 2020).
Not all nurses will need to acquire all of the key technological competencies; curricula can be developed according to the likely needs of nurses working at different levels. For example, most nurses will need the knowledge and skills to use telehealth, digital health tools, and data-driven clinical decision-making skills in practice, whereas nurse informaticians and some doctoral-level nurses will need to be versed in device design, bias assessment in algorithms, and big data analysis.
EXPANDING LEARNING OPPORTUNITIES
As stated previously, the domains and competencies enumerated above cannot be conveyed to nursing students through traditional lectures alone. Building the competencies to address population health, SDOH, and health inequities will require substantive experiential learning, collaborative learning, an integrated curriculum, and continuing professional development throughout nurses’ careers (IOM, 2016b). The 2019 Campaign for Action survey of nursing educators and leaders found that a majority of respondents identified “innovative community clinical experiences” and “interprofessional education experiences” as the top methods for teaching population health (Campaign for Action, 2019b). A recurrent theme in interviews with respondents was the importance of active and experiential learning, with opportunities for partnering with nontraditional agencies (Campaign for Action, 2019b). These types of community-based educational opportunities, particularly when they involve partnerships with others, are critical for nursing education for multiple reasons.
First, experience in the community is essential to understanding SDOH and gaining the competencies necessary to advance health equity (IOM, 2016b). In fact, restricting education in SDOH to the classroom may even be harmful, given the finding of a 2016 study that medical students who learned about SDOH in the classroom rather than through experiential learning demonstrated an increase in negative attitudes toward medically underserved populations (Schmidt et al., 2016).
Second, community-based education offers opportunities for students to engage with community partners from other sectors, such as government offices of housing and transportation or community organizations, preparing them for the essential work of participating in and leading partnerships to address SDOH. An example is a pilot interdisciplinary partnership between a school of nursing and a city fire department in the Pacific Northwest that allows students to practice such skills as motivational interviewing to identify the range of problems (e.g., transportation issues, difficulty accessing insurance or providers, lack of caregiving support) faced by people calling emergency services (Yoder and Pesch, 2020).
Third, nursing is increasingly practiced in community settings, such as schools and workplaces, as well as through home health care (WHO, 2015). Nursing students are prepared to practice in hospitals, but do not necessarily receive the same training and preparation for these other environments (Bjørk et al., 2014). Education in the community allows nursing students to learn about the broad range of care environments and to work collaboratively with other professionals who work in these environments. For example, students may work in a team with community health workers, social workers, and those from other sectors (e.g., housing and transportation), work that both enriches the experience of student nurses and creates bridges between nursing and other fields (Zandee et
al., 2010). Nurses who have these experiences during school may then be more prepared to lead and participate in multisector efforts to address SDOH—the importance of which is emphasized throughout this report—once they enter practice. Evidence suggests that graduating students are more likely to seek work in areas that are familiar to them from their education, clinical experience, and theoretical training (Jamshidi et al., 2016); thus, these nontraditional educational experiences may increase the number of nurses interested in working in the community. Moreover, while training in acute care settings has often been regarded as more valuable than that provided in community settings, evidence indicates that the two offer comparable opportunities for learning clinical skills (Morton et al., 2019). In fact, clinical care in community-based settings can present greater complexity relative to that in the hospital, and some technical skills (e.g., epidemiologic disease tracking, tuberculosis assessment and management, immunizations) are more available in community than in acute care settings (Morton et al., 2019).
Some nursing programs have incorporated community-based experiential learning into their programs. At community colleges and universities, schools have implemented nurse-managed clinics that serve the local population and their own students while also giving students technical skills and experience in interacting with the community. Lewis and Clark Community College, for example, operates a mobile health unit that brings health and dental care to six counties in southern Illinois (Lewis and Clark, n.d.), while nursing students at Alleghany College of Maryland can gain experience in the Nurse Managed Wellness Clinic, which offers such services as immunizations, screenings, and physicals (Alleghany College, 2020). At the baccalaureate and master’s level, a number of schools offer longitudinal, integrated experiences in settings as varied as federally qualified health centers (FQHCs), public health departments, homeless shelters, public housing sites, public libraries, and residential addiction programs (AACN, 2020c). Students and faculty at the University of Washington School of Nursing, for example, support community-oriented projects in partnership with three underserved communities in the Seattle area. Graduate students work for 1 year on grassroots projects (e.g., food banks, school health) and then reinforce this experience with 1 year of work at the policy level (AACN, 2020c). At the doctoral level, Washburn University transformed its DNP curriculum to incorporate SDOH and reinforce that instruction through experiential learning in the community (see Box 7-6). In addition to clinical education, nursing students can participate in nontraditional clinical community engagement and service learning opportunities, such as volunteering at a homeless shelter or working in a service internship for a community organization. These opportunities get students into the community, help them build relationships with people from health care and other sectors, and promote understanding of and engagement with SDOH (Bandy, 2011).
Simulation-Based Education
Simulation-based education is another useful tool for teaching nursing concepts and developing competencies and skills (Kononowicz et al., 2019; Poore et al., 2014; Shin et al., 2015). It can range from very low-tech (e.g., using oranges to practice injections) to very high-tech (e.g., a virtual reality emergency room “game”), but all simulations share the ability to bridge the gap between education and practice by imparting skills in a low-risk environment (SSIH, n.d.).
Simulations give students an opportunity to make real-time decisions and interact with virtual patients without having to face many of the challenges of traditional clinical education (Hayden et al., 2014). They can be used to enhance many types of skills, including communication (NASEM, 2018b), cultural sensi-
tivity (Lau et al., 2016), and screening for SDOH (Thornton and Persaud, 2018). Several simulation-based tools are available for learning about the realities of poverty, such as the Community Action Poverty Simulation (see Box 7-7) and the Cost of Poverty Experience (ThinkTank, n.d.). Such tools can help nurses identify ways in which their practice could directly mitigate the effects of poverty on individuals, families, and communities. Evaluations of poverty simulations have found that they can positively impact attitudes toward poverty and empathy among nurses and nursing students (Phillips et al., 2020; Turk and Colbert, 2018), although one study noted that the simulations should be accompanied by the inclusion of social justice concepts throughout the curriculum to achieve lasting change (Menzel et al., 2014).
Individual schools may or may not have the resources or faculty to support some types of simulation activities. For those that do not, simulation centers shared by schools of multiple professions and hospitals can provide access (Marken et al., 2010). For example, the New York Simulation (NYSIM) Center was created through a public–private partnership to manage interprofessional, simulation-based education for students and hospital employees across multiple sites (NYSIM, 2017). The opportunity to take part in simulation experiences with students from other health professions can also improve collaboration and teamwork and prepare nurses for practicing interprofessionally in the workplace (von Wendt and Niemi-Murola, 2018).
Limitations on in-person clinical training during the COVID-19 pandemic conditions have demonstrated the promise of simulation-based education as
a way to supplement traditional nursing education, allowing students to complete their education and sustaining the nursing workforce pipeline (Horn, 2020; Jiménez-Rodríguez et al., 2020; Yale, 2020). Before the pandemic, the NCSBN conducted a longitudinal, randomized controlled trial of the use of simulation and concluded that substituting simulation-based education for up to half of a nursing student’s clinical hours produces comparable educational outcomes and students who are ready to practice (Hayden et al., 2014). The COVID-19 pandemic has necessitated and accelerated the use of simulation to replace direct care experience in nursing schools, and state boards of nursing have loosened previous restrictions on its use (NCSBN, 2020b). Evaluation of this expanded use of simulation and other virtual experiences during the pandemic is needed, both in preparation for future emergencies and for use in nursing education generally.
RECRUITING AND SUPPORTING DIVERSE PROSPECTIVE NURSES
The composition of the population of prospective nurses and the ways they are supported throughout their education are important factors in how prepared the future nursing workforce will be to address SDOH and health equity. As discussed in prior chapters, developing a more diverse nursing workforce will be key to achieving the goals of reducing health disparities, providing culturally relevant care for all populations, and fostering health equity (Center for Health Affairs, 2018; IOM, 2011, 2016; Williams et al., 2014). A diverse workforce is one that reflects the variations in the nation’s population in such characteristics as socioeconomic status, religion, sexual orientation, gender, race, ethnicity, and geographic origin.
The nursing workforce has historically been overwhelmingly White and female, although it is steadily becoming more diverse (see Chapter 3). The 2016 IOM report assessing progress on the 2011 The Future of Nursing report notes that shifting the demographics of the overall workforce is inevitably a slow process since only a small percentage of the workforce leaves and enters each year (IOM, 2016a). The pipeline of students entering the field, on the other hand, can respond much more rapidly to efforts to increase diversity (IOM, 2016a). Since the 2011 report was published, significant gains have been realized in the diversity of nursing students. The number of graduates from historically underrepresented ethnic and racial groups more than doubled for BSN programs, more than tripled for entry-level master’s programs, and more than doubled for PhD programs (AACN, 2020a). The number of underrepresented students graduating from DNP programs grew by more than 1,000 percent, although this gain was due in large part to rapid growth in these programs generally. Yet, despite these gains, nursing students remain largely female and White: in 2019, 85–90 percent of students were female, and around 60 percent were White. The percentages of ADN, BSN, entry-level master’s, PhD, and DNP graduates in 2019 by race/ethnicity and gender are shown in Tables 7-3 and 7-4, respectively. For example, the
proportion of Hispanic or Latino nurses is highest among ADN graduates (12.8 percent) and lowest among PhD (5.5 percent) and DNP (6 percent) graduates, while the proportion of Asian nurses is highest among MSN graduates (11.2 percent) and lower among graduates with all other degrees. The proportion of PhD graduates who are male (9.9 percent) is significantly lower than the proportion of graduates with other degrees who are male.
Diversifying and strengthening the nursing student body—and eventually, the nursing workforce—requires cultivating an inclusive environment, recruiting and admitting a diverse group of students, and providing students with support and addressing barriers to their success throughout their academic career and into practice. In addition, it is essential to make available information that will enable prospective students to make informed decisions about their education and give them multiple pathways for completing their education (e.g., distance learning, accelerated programs). Accrediting bodies can play a role in advancing diversity and inclusion in nursing schools by requiring certain policies, practices, or systems. For example, the accreditation standards for medical schools of the Liaison Committee on Medical Education (LCME) include the following expectation (LCME, 2018):
TABLE 7-3 Nursing Program Graduates by Degree Typea and by Race/Ethnicity, 2019
| Race/Ethnicity | ADNb | BSN | MSNc | PhD | DNP |
|---|---|---|---|---|---|
| Total number of degrees | 75,470 | 77,363 | 3,254 | 801 | 7,944 |
| Native Hawaiian or other Pacific Islander | 0.3% | 0.5% | 0.4% | 1.2% | 0.3% |
| American Indian or Alaska Native | 0.7% | 0.4% | 0.6% | 0.6% | 0.5% |
| Asian | 4.6% | 7.9% | 11.2% | 6.6% | 6.9% |
| Hispanic or Latino | 12.8% | 10.2% | 11.3% | 5.5% | 6.0% |
| Black or African American | 12.1% | 8.7% | 8.7% | 12.1% | 15.0% |
| White | 63.2% | 63.6% | 59.4% | 59.2% | 63.7% |
| Two or more races | 2.5% | 2.8% | 2.5% | 1.4% | 2.4% |
| Non-U.S. residents (International) | 0.6% | 1.0% | 0.5% | 9.1% | 0.6% |
| Unknown | n/a | 5.0% | 5.5% | 4.2% | 4.6% |
NOTE: ADN = associate degree in nursing; BSN = bachelor of science in nursing; DNP = doctor of nursing practice; LPN/LVN = licensed practical/vocational nurse; MSN = master of science in nursing.
a Data not available for LPN/LVN.
b ADN data are from 2018.
c Entry-level master’s degree.
SOURCE: American Association of Colleges of Nursing, Enrollment & Graduations in Baccalaureate and Graduate Programs in Nursing (series); Integrated Postsecondary Education Data System (IPEDS), Completions Survey (series) for ADN data.
TABLE 7-4 Nursing Program Graduates by Degree Typea and Gender, 2019
| Gender | ADNb | BSN | MSNc | PhD | DNP |
|---|---|---|---|---|---|
| Total number of degrees | 77,993 | 77,363 | 3,254 | 801 | 7,944 |
| Male | 14.4% | 13.6% | 15.2% | 9.9% | 13.1% |
| Female | 85.6% | 85.1% | 84.7% | 89.9% | 86.6% |
| Unknown | n/a | 1.4% | 0.1% | 0.2% | 0.3% |
NOTE: ADN = associate degree in nursing; BSN = bachelor of science in nursing; DNP = doctor of nursing practice; LPN/LVN = licensed practical/vocational nurse; MSN = master of science in nursing.
a Data not available for LPN/LVN.
b ADN data are from 2018.
c Entry-level master’s degree.
SOURCE: American Association of Colleges of Nursing, Enrollment & Graduations in Baccalaureate and Graduate Programs in Nursing (series); Integrated Postsecondary Education Data System (IPEDS), Completions Survey (series) for ADN data.
A medical school has effective policies and practices in place, and engages in ongoing, systematic, and focused recruitment and retention activities, to achieve mission appropriate diversity outcomes among its students, faculty, senior administrative staff, and other relevant members of its academic community. These activities include the use of programs and/or partnerships aimed at achieving diversity among qualified applicants for medical school admission and the evaluation of program and partnership outcomes.
Currently, none of the major nursing accreditors (ACEN, CCNE, CNEA) includes similar language in its accreditation standards. As shown in Table 7-5, of six possible areas for standards on diversity and inclusion, ACEN and CCEN have standards only for student training, while CNEA has standards for student training and faculty diversity. No nursing accreditors have standards for student diversity; in comparison, accrediting bodies for pharmacy, physician assistant, medical, and dental schools all have such standards.
Cultivating an Inclusive Environment
Efforts to recruit and educate prospective nurses to serve a diverse population and advance health equity will be fruitless unless accompanied by efforts to acknowledge and dismantle racism within nursing education and nursing practice (Burnett et al., 2020; Schroeder and DiAngelo, 2010; Villaruel and Broome, 2020; Waite and Nardi, 2019). The structural, individual, and ideological racism that exists in nursing is rarely called out, and this silence further entrenches the idea of Whiteness as the norm within nursing while marginalizing and silencing other groups and their perspectives (Burnett et al., 2020; Iheduru-Anderson, 2020; Schroeder and DiAngelo, 2010). Non-White students report a wide variety of negative experiences in nursing school, including unsupportive faculty, discrim-
TABLE 7-5 Diversity and Inclusion in Accreditation Standards
| Accrediting Body | Student Diversity | Faculty Diversity | Academic Leadership Diversity | Pipeline Programs | Student Training | Faculty Training |
|---|---|---|---|---|---|---|
| Accreditation Commission for Education in Nursing (ACEN) | — | — | — | — | Yes | — |
| Accreditation Council for Pharmacy Education (ACPE) | Yes | — | — | — | Yes | — |
| Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) | Yes | Yes | — | — | Yes | — |
| Commission for Nursing Education Accreditation (CNEA) | — | Yes | — | — | Yes | — |
| Commission on Collegiate Nursing Education (CCNE) | — | — | — | — | Yes | — |
| Commission on Dental Accreditation (CODA) | Yes | Yes | — | — | Yes | — |
| Commission on Osteopathic College Accreditation (COCA) | Yes | Yes | Yes | — | Yes | Yes |
| Committee on Accreditation of Canadian Medical Schools (CACMS) | Yes | Yes | Yes | — | Yes | — |
| Liaison Committee on Medical Education (LCME) | Yes | Yes | Yes | Yes | Yes | — |
SOURCE: Batra and Orban, 2020.
ination and microaggressions5 on the part of faculty and peers, bias in grading, loneliness and social isolation, feeling unwelcome and excluded, being viewed as a homogeneous population despite being from varying racial/ethnic groups, lack of support for career choices, and a lack of mentors (Ackerman-Barger et al., 2020; Graham et al., 2016; Johansson et al., 2011; Loftin et al., 2012; Metzger et al., 2020). These experiences are associated with adverse outcomes that include disengagement from education, loss of “self,” negative perceptions of inclusivity and diversity at the institution, and institutions’ inability to recruit and retain a diversity of students (Metzger et al., 2020). By contrast, when students characterize the learning environment as inclusive, they are more satisfied and confident in their learning and rate themselves higher on clinical self-efficacy and clinical belongingness (Metzger and Taggart, 2020).
Notably, however, underrepresented and majority students describe inclusive environments differently. In a study of fourth-year baccalaureate nursing students, both groups described an inclusive classroom as one where they felt comfortable and respected and had a sense of belonging, but underrepresented minority students also noted the importance of feeling safe, feeling free from hostility, and being seen as themselves and not a representative of their group (Metzger and Taggart, 2020). Both groups agreed that inclusivity requires a top-down approach, and that faculty are particularly influential in creating an inclusive environment, yet underrepresented students shared many experiences in which faculty either disrupted the sense of belonging or did not intervene when someone else did (Metzger and Taggart, 2020).
While increased attention has recently been focused on increasing diversity in nursing education, the pervasiveness of racism requires more open acknowledgment and discussion and a systematic and intentional approach that may, as discussed earlier, be uncomfortable for some (Ackerman-Barger et al., 2020; Villaruel and Broome, 2020). Cultivating an inclusive environment requires acknowledging and challenging racism in all aspects of the educational experience, including curricula, institutional policies and structures, pedagogical strategies, and the formal and informal distribution of resources and power (Iheduru-Anderson, 2020; Koschmann et al., 2020; Metzger and Taggart, 2020; Schroeder and DiAngelo, 2010; Villaruel and Broome, 2020; Waite and Nardi, 2019). Nursing school curricula have historically focused on the contributions of White and female nurses (Waite and Nardi, 2019). The weight given to this curricular content sends a message to students—both White students and students of color—about what faculty consider important (Villaruel and Broome, 2020). Moving forward, curricula need to include a critical examination of the history of racism within nursing and an acknowledgment and celebration of the contribution of nurses of color (Waite and Nardi, 2019). Such efforts need to be led by a broad group of individuals from all levels within an institution; racism in institutional practices
___________________
5 Brief and commonplace daily indignities (see Chapter 10).
can be so ingrained that it is difficult for those with power to recognize (Villaruel and Broome, 2020). Faculty often understand the importance of an inclusive learning environment, but struggle with moving from intention to action (Beard, 2013, 2014; Metzger et al., 2020).
While institutional efforts to change organizational culture are thoroughly described in the literature, they remain too rare to address the problems described above effectively (Breslin et al., 2018). In the early 2000s, the University of Washington School of Nursing implemented a project designed to change the “climate of whiteness” at the school (Schroeder and DiAngelo, 2010). The project involved many facets, including year-long antiracist workshops; a comprehensive and institutionalized diversity statement; and action plans for addressing admission barriers, encouraging ongoing education for faculty, and disseminating antiracist information to the entire campus. The authors of an evaluation of the project note that while initial feedback was positive, changing the sociopolitical climate of a school is a long-term process that requires institutional commitment, innovative leadership, long- and short-term strategies, and patience (Schroeder and DiAngelo, 2010). Unfortunately, many administrators and leaders may hesitate to initiate dialogues about these issues or may lack knowledge of how to address the challenges, and in many institutions, faculty and administrators from underserved groups have been expected to carry this burden, which can allow their colleagues to remain passive (Lim et al., 2015). The committee stresses that addressing racism and discrimination within the nursing profession requires more than mere programs or statements; it requires developing action-oriented strategies, holding difficult conversations about privilege, dismantling long-standing structures and traditions, conducting curricular reviews to detect biases and correct as necessary, and exploring how interpersonal and structural racism shapes the student experience both consciously and unconsciously (Burnett et al., 2020; Iheduru-Anderson, 2020; Waite and Nardi, 2019).
Recruitment and Admissions
Many social and structural barriers impede the entry of underrepresented students into the nursing profession (NACNEP, 2019). Several approaches can be taken to improve access for prospective underrepresented students and, by extension, increase the diversity of the nursing workforce. Recruitment of underrepresented students can start years before nursing school through such approaches as improved K–12 science education (AAPCHO, 2009) and outreach to junior high and high school students, such as through summer pipeline programs (Katz et al., 2016) or health career clubs (Murray et al., 2016). K–12 education is particularly important for sparking students’ interest in the health professions, as well as for giving them the foundational knowledge necessary for success (NASEM, 2016b). One innovative approach to preparing young people for a career in nursing is the Rhode Island Nurses Institute Middle College Charter High School (RINIMC).
RINIMC offers a free, 4-year, nursing-focused, high school education open to any student in Rhode Island; students graduate with experience in health care as well as up to 20 college credits. Nearly half of the program’s students are Latinx, and more than one-third are Black (RINIMC, n.d.). Establishing a pathway to nursing education for diverse students well before undergraduate school is important, particularly for first-generation students (Katz et al., 2016; McCue, 2017). Some states offer dual enrollment programs. An example is Ohio’s College Credit Plus program, in which students in grades 7 to 12 have the opportunity to earn college and high school credits simultaneously, thus preparing them for postsecondary success.6
Once students have applied to nursing school, a system of holistic admissions can improve the diversity of the incoming class (Glazer et al., 2016, 2020). A holistic admissions system involves evaluating an applicant based not only on academic achievement but also on experiences, attributes, potential contributions, and the fit between the applicant and the institutional mission (DeWitty, 2018; NACNEP, 2019). Schools that have implemented such a system have seen an increase in the diversity of their student body (Glazer et al., 2016, 2018). Academic measures (e.g., graduation and exam pass rates) have remained unchanged or improved, and schools have reported increases in such measures as student engagement, cooperation and teamwork, and openness to different perspectives (Artinian et al., 2017; Glazer et al., 2016, 2020). In a recent paper published by AACN (2020d), the following promising practices in holistic admissions were identified: (1) review institutional mission, vision, and values statements to ensure that they value diversity and inclusion; (2) create an “experience, attributes, and metrics (E-A-M) model” (p. 16) that connects back to the institution’s mission statement; (3) identify recruitment practices that align with the E-A-M model; (4) design rubrics to be used by admissions committees that are reflective of the E-A-M model; (5) engage faculty and staff in the holistic admissions review process; (6) use technology resources such as a centralized application system to maintain efficiencies; (7) develop tailored support services for underrepresented students; and (8) engage in a review and assessment of the entire process.
Addressing Barriers to Success
Part of cultivating an inclusive educational environment is acknowledging and addressing barriers that may prevent students from achieving their potential. As noted previously, some students—particularly those from underrepresented groups—may need support in a number of areas, including economic, social and emotional, and academic and career progression. Attention to the barriers faced by students is essential at each step along the pathway from high school preparation; to recruitment, admission, retention, and academic success in nurs-
___________________
6 See https://www.ohiohighered.org/collegecreditplus (accessed April 13, 2021).
ing school; to graduation and placement in a job; to retention and advancement within a nursing career (IOM, 2016b).
Providing Economic Supports
Cost is a key factor in decisions about nursing education for most students, and is particularly salient for those from underrepresented groups, who come disproportionately from families with comparatively low incomes and levels of wealth (Diefenbeck et al., 2016; Graham et al., 2016; Sullivan, 2004). Sabio and Petges (2020) interviewed associate’s degree nursing students in a Midwestern state and found that the total cost of a baccalaureate degree and student debt was the greatest barrier to pursuing a degree, followed by family and personal, such as head-of-household, responsibilities. This challenge is pervasive in higher education, and there are indications that the problem is growing (Advisory Committee on Student Financial Assistance, 2013). Students need to have the financial resources not only for tuition but also for an array of education-related expenses, including housing, food, work attire, books, and supplies.
Providing clear information about the costs of nursing education and available financial supports early in the recruitment and admission process is key to identifying those who need help and encouraging them to enroll (Pritchard et al., 2016). Recruitment and admission practices need to take into account student finances and how future salaries affect choices, particularly for certain groups of students. Most health care systems provide some level of tuition reimbursement for baccalaureate and higher education, and this support may lead students toward certain settings (e.g., acute care) and away from others (e.g., public health, primary care) (Larsen, 2012). Other financial support options are available, including the Public Service Loan Forgiveness program, which offers full forgiveness after 10 years for employees of nonprofit or government organizations (U.S. Department of Education, n.d.b), and programs through HRSA that award loan repayment to RNs and advanced practice nurses who work in health professions shortage areas for at least 2 years (HRSA, 2021).
State policy reform can help remove some of the structural barriers to education. For example, New York State has implemented a program that allows New York households earning less than $125,000 annually to qualify for free instate tuition at state public universities (New York State, n.d.). New nurses who complete an associate’s degree in New York are required to complete a bachelor’s degree within 10 years of graduation; free in-state tuition could make a considerable difference for these nurses in pursuing their next degree. While it is too early to assess the effects on the composition of the nursing workforce, this approach bears further evaluation. Certainly it is critical for state policies to facilitate the financing of nursing education using models other than additional student loans. There are demonstrated disparities in the burden of student debt between Black and White students (Brookings Institution, 2016), and the risk of assuming large
amounts of debt for students from disadvantaged backgrounds may be one they cannot afford to take. Therefore, innovative financing models are necessary to ensure that all nurses can pursue educational opportunities.
It is also important to note that as they progress in their education, students of many backgrounds may experience food insecurity, struggles with housing, or issues with transportation that affect their ability to perform (AAC&U, 2019; Laterman, 2019; Strauss, 2020). Institutions need to ensure that students’ basic needs are met during their studies through sustained, multiyear funding and resources to support students facing financial emergencies.
Social and Academic Supports
Once students have been admitted, some nursing schools offer programs, such as summer programs that bridge high school and college, designed to prepare them academically and socially for the rigors of nursing education. Some of these programs are designed specifically for underrepresented and/or first-generation college students (Pritchard et al., 2016), who may lack adequate family, emotional, and moral support; mentorship opportunities; professional socialization; and academic support (Banister et al., 2014; Loftin et al., 2012). A study at the University of Cincinnati College of Nursing found that the impact of its summer bridge program lasted throughout the first year of school, and that grade point averages and retention were similar between underrepresented and majority students (Pritchard et al., 2016). The Recruitment & Retention of American Indians into Nursing (RAIN) program at the University of North Dakota conducts a “No Excuses Orientation” workshop to give incoming American Indian students an opportunity to create connections and become acquainted with people and resources at the university (UND, 2020). Tribal leaders are included in the orientation, along with discussions of cultural and family values and issues.
Another approach for supporting students is through mentoring programs. As discussed in Chapter 9, these programs create supportive environments by providing peer and faculty role modeling, academic guidance, and support (Wilson et al., 2010). Evidence indicates that mentoring programs for students from underrepresented groups are more effective when they include nurses and faculty from those groups, who have firsthand understanding of the unique challenges these students and nurses regularly confront (Banister et al., 2014). This observation underscores the need for diverse faculty, mentors, and preceptors with the availability and willingness to guide these students and teach them leadership. For example, the RAIN program provides mentoring to American Indian students; staff and leaders are heavily involved in the local American Indian communities, and many are tribal members themselves (Minority Nurse, 2013).
Students who represent the first generation in their families to enter a postsecondary institution may face challenges other students do not, and are more
likely to graduate if they receive support (Costello et al., 2018). Parents and significant others can be a crucial source of support (Pritchard et al., 2020); socializing and educating family members about the rigors of nursing programs may facilitate their support for students. A variety of programs around the country have succeeded in increasing graduation rates among first-generation students, including pipeline programs that have successfully increased the diversity of candidates entering nursing. These programs include HRSA pipeline programs; HOSA-Future Health Professionals; and university-based programs such as the Niganawenimaanaanig program at Bemidji State University in Minnesota, created to support American Indian nursing students (HOSA, 2012; HRSA, 2017; Wilkie, 2020). Federal funding is available for these types of programs from sources that include HRSA’s Health Careers Opportunity Program and Nursing Workforce Diversity Grant program. However, the need for such programs exceeds the available funding. Box 7-8 lists some of the ways in which nursing programs can support their students’ success.
Data on Quality
One important tool for recruiting a more diverse student population is providing relevant data to prospective students so they can make informed decisions about where to study. These data could include NCLEX pass rates; however, these rates alone are insufficient to determine whether a school is likely to have the resources to support a student through to graduation. Data on student reten-
tion, graduation by demographic, full cost to attend, tuition, and other quality indicators can signal to both consumers and funders whether a nursing education program has the necessary infrastructure and support to retain students from diverse backgrounds. Pass rates can be reported by race, ethnicity, socioeconomic status, first-time college/university attendees, adult learners with children living at home, and status as an English as a second language (ESL) learner to help students choose a program that best suits their needs. It is also important for schools to provide on their websites demographic information about their current enrollees. As discussed above, NCSBN identified additional quality indicators for nursing education; as these indicators begin to be measured and reported, the data can help prospective students make more informed choices.
Educational Pathways and Options
As nursing education programs adapt their curricula and other learning experiences to better address SDOH and health equity, it will be important to consider the educational pathways students may follow, both in their initial preparation and as they progress in their careers. A key way of strengthening the nursing workforce will be to encourage nurses to pursue the next level of education and certification available to them and to improve access to these educational opportunities, especially for those from underrepresented communities (Jones et al., 2018; Phillips and Malone, 2014).
One way to improve access and encourage nurses to take the next step in their education is by offering expedited programs that allow them to complete their degree in less time. For example, there are articulation agreements, either among educational institutions or at the state or regional level, that align the content and requirements of programs. These types of agreements accelerate the RN-to-BSN and RN-to-MSN pathways and allow students to easily transfer credits between community colleges and universities (AACN, 2019b). There are also bridge programs available for LPNs who wish to pursue the ADN or BSN degree. Investments in articulation programs have been responsible in part for an increase in the number of employed nurses with a baccalaureate degree, from 49 percent in 2010 to 59 percent in 2019 (Campaign for Action, n.d.). Further progress in this area is needed, however, particularly for partnerships between baccalaureate nursing programs and academic institutions that serve underrepresented populations (e.g., tribal colleges, historically Black colleges and universities). A model of this type of partnership can be found in the New Mexico Nursing Education Consortium,7 which coordinates prelicensure nursing curricula in 16 locations at state, tribal, and community colleges.
Nursing education can also be expedited through the use of a competency-based curriculum that allows students to progress by demonstrating the required
___________________
7 See https://www.nmnec.org (accessed April 13, 2021).
competencies rather than meeting specific hour requirements (U.S. Department of Education, n.d.a). With this approach, which is currently used, for example, by Western Governors University, students can self-pace their education and potentially save time and money by learning the material quickly or tapping previous knowledge (WGU, 2020). This type of educational approach may be particularly useful for nontraditional students who are entering nursing with other experiences and education. For example, a person with a background as a nursing or medical assistant may find that he or she can quickly master some of the required material for a nursing degree, particularly at the beginning. Workers from other sectors may also be able to pivot to nursing. During the COVID-19 pandemic, a study identified health care jobs, such as nursing assistant, that out-of-work hospitality workers could quickly transition to pursue (Miller and Haley, 2020). While the study did not include jobs that required further education or certification, the shared skill sets that the authors identified include many skills that are central to nursing.
Another approach for increasing access to nursing education is to expand the use of distance learning opportunities. Distance learning gives students flexibility, and may be particularly beneficial for those from rural areas or other areas without a nursing school in the vicinity (NCSBN, 2020b). Rural areas face multiple challenges: rural populations have high rates of chronic disease and have difficulty accessing care because of provider shortages in these areas (see Chapter 2). Relative to their urban counterparts, rural nurses are less likely to hold a BSN (Merrell et al., 2020). Distance learning has been used for many years to reach rural populations, but there are challenges with respect to regulation and ensuring the quality of education (NCSBN, 2020a). Efforts have been made to assess and improve the quality of distance learning; Quality Matters, for example, is an organization that provides peer-reviewed evaluation of distance or hybrid programs using a set of quality standards.8 While many nursing programs are adhering to these standards (Quality Matters, 2020), many are not, and the quality of distance learning remains uneven. The rapid rollout of distance learning during the COVID-19 pandemic has provided a unique opportunity to evaluate the effectiveness of different strategies for distance learning and to leverage this experience to expand and improve distance learning opportunities in the future.
STRENGTHENING AND DIVERSIFYING THE NURSING FACULTY
A system of nursing education that can prepare students from diverse backgrounds to address SDOH and health equity requires a diverse faculty (NACNEP, 2019; Thornton and Persaud, 2018). Unfortunately, the faculty currently teaching in nursing programs is overwhelmingly White and female: as of 2018, full-time faculty in nursing schools were about 93 percent female, and only 17.3 percent were from underrepresented groups, up from 11.5 percent in 2009 (AACN, 2020c).
___________________
8 See https://www.qualitymatters.org (accessed April 13, 2021).
In addition to this lack of diversity, the number of faculty may be inadequate to prepare the next generation of nurses: not only were there 1,637 faculty vacancies in 2019 across 892 nursing schools, but the schools surveyed hoped to create 134 new faculty positions in that year (AACN, 2020c). These shortages contributed to decisions to turn away more than 80,000 qualified applicants, although other insufficiencies also played a part. The AACN report cites several key reasons for faculty shortages: increasing average age of faculty members and associated increasing retirement rates, high compensation in other settings that attracts current and potential nurse educators, and an insufficient pool of graduates from master’s and doctoral programs (AACN, 2020c; Fang and Bednash, 2017). A 2020 NACNEP report calls the faculty shortage a “long-standing crisis threatening the supply, education, and training of registered nurses” and recommends federal efforts as well as a coordinated private–public response to address the shortage (NACNEP, 2020).
Finally, faculty must have the knowledge, skills, and competencies to prepare their students for the challenges of advancing health equity and fully understanding the implications of SDOH for their daily practice (NACNEP, 2019). If health equity and SDOH are to be integrated throughout the curriculum (as discussed earlier in this chapter), all faculty, including tenure-track faculty, clinical instructors, mentors, and preceptors, must have these competencies (Thornton and Persaud, 2018). To develop these competencies, nursing schools must commit resources and support to faculty development (Thornton and Persaud, 2018).
Diversifying the Faculty
As noted, diverse faculty are needed to broaden the perspectives and experiences to which nursing students are exposed and to serve as mentors and role models for diverse students (Phillips and Malone, 2014). Unfortunately, minority faculty members often face barriers similar to those faced by students, including an unwelcoming environment; feeling marginalized, underappreciated, and invisible; a lack of support; feelings of tokenism; and the inability to integrate into existing faculty structures (Beard and Julion, 2016; Hamilton and Haozous, 2017; Iheduru-Anderson, 2020; Kolade, 2016; Salvucci and Lawless, 2016; Whitfield-Harris and Lockhart, 2016). Faculty from underrepresented groups report feeling isolated, lacking in mentorship and collegial support, and burdened by having to represent the entire underrepresented community (Kolade, 2016; Whitfield-Harris et al., 2017). In addition, as discussed in Chapter 9, faculty from underrepresented racial and ethnic groups face a “diversity tax,” in which they are asked to be part of efforts to improve diversity and inclusion to serve on committees; mentor underrepresented students; and participate in other activities that are uncompensated, unacknowledged, and unrewarded (Gewin, 2020). These demands on underrepresented faculty can lead to frustration, burnout, and a feeling that they have been given responsibility for institutional diversity (Gewin, 2020).
These experiences of minority faculty can result in high attrition and low satisfaction (Whitfield-Harris et al., 2017), and further research is needed on specific ways in which institutions can recruit and support a diverse faculty (Whitfield-Harris et al., 2017). Proposed approaches include cultivating an inclusive educational environment (Hamilton and Haozous, 2017), taking intentional action and holding open discourse to strengthen the institutional commitment to diversity (Beard and Julion, 2016), improving financial assistance and mentorship opportunities for faculty (Salvucci and Lawless, 2016), and conducting climate surveys to better understand the feelings and experiences of underrepresented faculty and using these data to improve the institutional culture (DeWitty and Murray, 2020). The challenges these faculty face and the opportunities to address these challenges highlight the importance of efforts by schools of nursing to recruit, support, and retain diverse faculty.
Faculty Development
Collectively, nursing school faculty need to be prepared to teach their students about the complex linkages among population health, SDOH, and health outcomes (NLN, 2019; Thornton and Persaud, 2018). To do so, as discussed above, nurse educators need to move beyond teaching abstract principles to integrating the core concepts and competencies related to these linkages into the entire learning experience across nursing education programs. They also need to create a truly inclusive and safe educational environment and prepare nurses to care for a diverse population, which, as discussed above, requires that they understand issues of racism and systems of marginalization and engage in critical self-reflection (O’Connor et al., 2019, Peek et al., 2020). Yet, many faculty in nursing schools lack the knowledge and experience needed to develop curricula and strategies for incorporating SDOH into all areas of nursing education (NACNEP, 2019; Valderama-Wallace and Apesoa-Varano, 2019).
Several approaches are available for preparing nursing school faculty to teach content related to SDOH and health equity. One approach, discussed above, is to actively recruit more diverse faculty who reflect the nation’s population and provide different perspectives and role models for students (The Macy Foundation, 2020). Another approach is to encourage the development and dissemination of evidence-based methods for teaching nursing students how they can incorporate these core concepts into nursing practice. For example, educators involved in developing innovative models of classroom and experiential learning could focus on disseminating these models with the assistance of nursing associations and organizations, including through publication, continuing education programs, or faculty-to-faculty education and mentoring. Finally, institutions can provide in-depth and sustained learning opportunities for faculty, staff, and preceptors focused on how they can support their students in learning about SDOH and health equity both within and outside of the classroom (IOM, 2016b). While some fund-
ing sources are available for these types of efforts, including support from private foundations and HRSA grants for faculty development, the critical importance of this content to health outcomes argues for providing more such resources.
IMPLICATIONS OF COVID-19 FOR NURSING EDUCATION
It has been 100 years since a global event has had an impact on nursing education in the United States and around the world equal to that of the COVID-19 pandemic. Both World War I and the influenza pandemic of 1918 to 1920 led to transformations in nursing education, including standardization of training and professionalization of the field. The COVID-19 pandemic has already led to innovations that are likely to shape the future of nursing education. Faculty have adopted new teaching strategies, demonstrating creativity and adaptability, within a span of days or weeks, while such technologies as simulation-based education have quickly been adapted to replace in-person clinical hours (Jiménez-Rodríguez et al., 2020). In one example of a rapid pivot, educators at the University of Pennsylvania School of Nursing transitioned a community immersion course from in-person to virtual form when all in-person classes were canceled. While they faced challenges, the educators found that students were able to remain dedicated to their community partnerships and to think creatively about how to meet their learning objectives (Flores et al., 2020). These and similar innovations may ultimately guide the way to expanding and improving nursing education.
At the same time, however, the pandemic has highlighted challenges and inequities in nursing education. Simulated clinical experiences are practical only if a school and its students have access to computers with enough power to run the software, for example. While online learning has been in use for more than a decade, not all schools or faculty are prepared to deliver content in this way, nor are all students capable of accessing the necessary technology. Moreover, as practice settings have been emptied of non-COVID patients, programs have been facing multiple challenges in providing students with sufficient hours of instruction, training, and clinical practice. These challenges have underscored the limitations of traditional ways of educating nurses even as they have presented unique opportunities for innovation. To translate these short-term challenges into long-term improvements in nursing education will require
- evaluation of such practices as distance learning and virtual experiential learning to identify and disseminate best practices;
- a sense of urgency in the development of substantial changes, such as modifications of curriculum and the adoption of new technologies; and
- partnership with public- and private-sector organizations, associations, and researchers that can bring both resources and expertise to the tasks of strengthening nursing education.
CONCLUSIONS
Currently, most nursing schools tend to cover the topics of SDOH, health equity, and population health in isolated, stand-alone courses. This approach is insufficient for creating a foundational understanding of these critical issues and for preparing nurses to work in a wide variety of settings. This content needs to be integrated and sustained throughout nursing school curricula and paired with community-based experiential opportunities whereby students can apply their knowledge, build their skills, and reflect on their experiences.
Conclusion 7-1: A curriculum embedded in coursework and experiential learning that effectively prepares students to promote health equity, reduce health disparities, and improve the health and well-being of the population will build the capacity of the nursing workforce.
Preparing nursing students to address SDOH and improve health equity will require more than didactic learning and traditional clinical experiences. It will require that students engage actively in experiences that will expand and diversify their understanding of nursing practice, prepare them to care for diverse populations with empathy, and allow them to build the necessary skills and competencies for the nursing practice of tomorrow.
Conclusion 7-2: Increasing the number of nurses with PhD degrees who focus on the connections among social determinants of health, health disparities, health equity, and overall health and well-being will build the evidence base in this area. Building capacity in schools of nursing will require financial resources, including scholarship/loan repayment opportunities; adequate numbers of expert faculty available to mentor; and curriculum revisions to focus more attention on social determinants of health and health equity.
Having more nurses prepared at the PhD level will help build the knowledge base in the nursing profession for other nurses to translate (DNPs) and use in practice settings (LPNs, RNs, APRNs).
- develop such technical competencies as use of telehealth, digital health tools, and data analytics; and
- gain substantive experience with delivering care in diverse community settings, such as public health departments, schools, libraries, workplaces, and neighborhood clinics.
Building a diverse nursing workforce is a critical component of the effort to prepare nurses to address SDOH and health equity. While the nursing workforce has steadily grown more diverse, nursing schools need to continue and expand their efforts to recruit, support, and mentor diverse students.
Conclusion 7-4: Successfully diversifying the nursing workforce will depend on holistic efforts to support and mentor/sponsor students and faculty from a wide range of backgrounds, including cultivating an inclusive environment; providing economic, social, professional, and academic supports; ensuring access to information on school quality; and minimizing inequities.
REFERENCES
Aaberg, V. A. 2012. A path to greater inclusivity through understanding implicit attitudes toward disability. Journal of Nursing Education 51(9):505–510.
AAC&U (Association of American Colleges & Universities). 2019. Majority of college students experience food insecurity, housing insecurity, or homelessness. https://www.aacu.org/aacu-news/newsletter/majority-college-students-experience-food-insecurity-housing-insecurity-or (accessed March 29, 2021).
AACN (American Association of Colleges of Nursing). 2006. The essentials of doctoral education for advanced nursing practice. Washington, DC: American Association of Colleges of Nursing.
AACN. 2011. The essentials of master’s education in nursing. https://www.aacnnursing.org/portals/42/publications/mastersessentials11.pdf (accessed July 6, 2021).
AACN. 2019a. 2018–2019 enrollment and graduations in baccalaureate and graduate programs in nursing. Washington, DC: American Association of Colleges of Nursing.
AACN. 2019b. Articulation agreements among nursing education programs. https://www.aacnnursing.org/News-Information/Fact-Sheets/Articulation-Agreements (accessed January 25, 2021).
AACN. 2020a. 2019–2020 enrollment and graduations in baccalaureate and graduate programs in nursing. https://www.aacnnursing.org/Store/product-info/productcd/IDSR_20ENROLLBACC (accessed January 8, 2021).
AACN. 2020b. Essentials task force. https://www.aacnnursing.org/About-AACN/AACN-Governance/Committees-and-Task-Forces/Essentials (accessed May 18, 2020).
AACN. 2020c. Nursing faculty. https://www.aacnnursing.org/news-information/fact-sheets/nursing-faculty-shortage (accessed March 9, 2021).
AACN. 2020c. Curriculum improvement. https://www.aacnnursing.org/Population-Health-Nursing/Curriculum-Improvement (accessed January 25, 2021).
AACN. 2020d. Promising practices in holistic admissions review: Implementation in academic nursing. https://www.aacnnursing.org/Portals/42/News/White-Papers/AACN-White-Paper-Promising-Practices-in-Holistic-Admissions-Review-December-2020.pdf (accessed January 25, 2021).
AACN. n.d. Diversity & inclusion offerings. https://www.aacnnursing.org/Diversity-Inclusion/Holistic-Admissions/Diversity-and-Inclusion-Offerings (accessed April 23, 2020).
AAPCHO (Association of Asian Pacific Community Health Organizations). 2009. Pipeline programs to improve racial and ethnic diversity in the health professions. https://www.aapcho.org/wp/wp-content/uploads/2012/11/PipelineToImproveDiversityInHealthProfessions.pdf (accessed June 2, 2021).
AARP. 2010. Preparation and roles of nursing care providers in America. http://championnursing.org/resources/preparation-and-roles-nursing-care-providers-america (accessed October 28, 2020).
Ackerman-Barger, K., D. Boatright, R. Gonzalez-Colaso, R. Orozco, and D. Latimore. 2020. Seeking inclusion excellence: Understanding racial microaggressions as experienced by underrepresented medical and nursing students. Academic Medicine 95(5):758–763.
Advisory Committee on Student Financial Assistance. 2013. Federal Register 78(152). https://fsapartners.ed.gov/sites/default/files/attachments/fregisters/FR080713AdvisoryCommitteeonStudentFinancialAssistance.pdf (accessed June 2, 2021).
Agner, J. 2020. Moving from cultural competence to cultural humility in occupational therapy: A paradigm shift. American Journal of Occupational Therapy 74(4):7404347010.
AHA (American Hospital Association). 2019. Screening for social needs: Guiding care teams to engage patients. https://www.aha.org/system/files/media/file/2019/09/screening-for-social-needs-tool-value-initiative-rev-9-26-2019.pdf (accessed November 11, 2020).
Aiken, L. H., D. Sloane, P. Griffiths, A. M. Rafferty, L. Bruyneel, M. McHugh, C. B. Maier, T. Moreno-Casbas, J. E. Ball, D. Ausserhofer, and W. Sermeus. 2017. Nursing skill mix in European hospitals: Cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Quality & Safety 26(7):559–568.
Alleghany College of Maryland. 2020. Nurse managed wellness clinic. https://www.allegany.edu/health-clinics/nurse-managed-wellness-clinic (accessed June 2, 2021).
Allen, J. 2010. Improving cross-cultural care and antiracism in nursing education: A literature review. Nurse Education Today 30(4):314–320.
Arcaya, M. C., and J. F. Figueroa 2017. Emerging trends could exacerbate health inequities in the United States. Health Affairs (Millwood) 36(6):992–998.
Artinian, N. T., B. M. Drees, G. Glazer, K. Harris, L. S. Kaufman, N. Lopez, J. C. Danek, and J. Michaels. 2017. Holistic admissions in the health professions: Strategies for leaders. College & University 92(2):65–68.
Baker, C., A. H. Cary, and M. da Conceicao Bento. 2020. Global standards for professional nursing education: The time is now. Journal of Professional Nursing 37(1):86–92. doi: 10.1016/j. profnurs.2020.10.001.
Bandy, J. 2011. What is service learning or community engagement? Vanderbilt University Center for Teaching. https://cft.vanderbilt.edu/guides-sub-pages/teaching-through-community-engagement (accessed March 29, 2021).
Banister, G., H. M. Bowen-Brady, and M. E. Winfrey. 2014. Using career nurse mentors to support minority nursing students and facilitate their transition to practice. Journal of Professional Nursing 30(4):317–325.
Barton, A. J., T. A. Murray, and D. R. Spurlock, Jr. 2020. An open letter to members of the nursing education community. Journal of Nursing Education 59(4):183.
Batra, S., and J. Orban. 2020. Social mission and accreditation standards. Oral presentation at the National Center for Interprofessional Education and Practice NEXUS Summit 2020, October 15, 2020, Virtual.
Beard, K. V. 2014. How much diversity in nursing is enough? American Journal of Nursing 114(9):11.
Beard, K. V., and W. A. Julion. 2016. Does race still matter in nursing? The narratives of African-American nursing faculty members. Nursing Outlook 64:583–596. https://doi.org/10.1016/j.outlook.2016.06.005PMID:27432213.
Bednash, G., E. T. Breslin, J. M. Kirschling, and R. J. Rosseter. 2014. PhD or DNP: Planning for doctoral nursing education. Nursing Science Quarterly 27(4):296–301.
Befus, D. R., T. Kumodzi, D. Schminkey, and A. S. Ivany. 2019. Advancing health equity and social justice in forensic nursing research, education, practice, and policy: Introducing structural violence and trauma-and violence-informed care. Journal of Forensic Nursing 15(4):199–205.
Bestsennyy, O., G. Gilbert, A. Harris, and J. Rost. 2020. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality (accessed February 24, 2021).
Bjørk, I. T., K. Berntsen, G. Brynildsen, and M. Hestetun. 2014. Nursing students’ perceptions of their clinical learning environment in placements outside traditional hospital settings. Journal of Clinical Nursing 23(19–20):2958–2967.
Blair, I. V., J. F. Steiner, and E. P. Havranek. 2011. Unconscious (implicit) bias and health disparities: Where do we go from here? The Permanente Journal 15(2):71–78. PMID: 21841929.
Breen, N., J. S. Jackson, F. Wood, D. Wong, and X. Zhang. 2019. Translational health disparities research in a data-rich world. American Journal of Public Health 109(S1):S41–S42.
Brennan, A. M. W., J. Barnsteiner, M. L. Siantz, V. T. Cotter, and J. Everett. 2012. Lesbian, gay, bisexual, transgendered, or intersexed content for nursing curricula. Journal of Professional Nursing 28(2):96–104.
Breslin, E. T., K. Nuri-Robins, J. Ash, and J. M. Kirschling. 2018. The changing face of academic nursing: Nurturing diversity, inclusivity, and equity. Journal of Professional Nursing 34(2):103–109.
Bresnick, J. 2017. Understanding the basics of clinical decision support systems. Health IT Analytics. https://healthitanalytics.com/features/understanding-the-basics-of-clinical-decision-support-systems (accessed November 11, 2020).
Brookings Institution. 2016. Black-White disparity in student loan debt more than triples after graduation. https://www.brookings.edu/research/black-white-disparity-in-student-loan-debt-more-than-triples-after-graduation (accessed November 11, 2020).
Broome, M. E., and J. Fairman. 2018. Changing the conversation about doctoral education in nursing. Nursing Outlook 66(2018):217–218.
Buhler-Wilkerson, K. 1993. Bringing care to the people: Lillian Wald’s legacy to public health nursing. American Journal of Public Health 83(12):1778–1786.
Burnett, A., C. Moorley, J. Grant, M. Kahin, R. Sagoo, E. Rivers, L. Deravin, and P. Darbyshire. 2020. Dismantling racism in education: In 2020, the year of the nurse & midwife, “it’s time.” Nurse Education Today 93:104532. https://doi.org/10.1016/j.nedt.2020.104532.
Campaign for Action. 2019a. New RN graduates by degree type, by gender. https://campaignforaction.org/resource/new-rn-graduates-degree-type-gender (accessed May 13, 2020).
Campaign for Action. 2019b. Nursing education and the path to population health improvement. https://campaignforaction.org/wp-content/uploads/2019/03/NursingEducationPathtoHealthImprovement.pdf (accessed March 13, 2020).
Campaign for Action. 2020. Campaign for Action dashboard. https://campaignforaction.org/wpcontent/uploads/2019/07/r2_CCNA-0029_2019-Dashboard-Indicator-Updates_1-29-20.pdf (accessed May 14, 2020).
Campaign for Action. n.d. Transforming nursing education. https://campaignforaction.org/issue/transforming-nursing-education (accessed May 14, 2020).
Campinha-Bacote, J. 2018. Cultural competemility: A paradigm shift in the cultural competence versus cultural humility debate—part I. The Online Journal of Issues in Nursing 24(1).
Castro-Sánchez, E., A. M. Russell, L. Dolman, and M. Wells. 2021. What place does nurse-led research have in the COVID-19 pandemic? International Nursing Review 1–5.
CCNE (Commission on Collegiate Nursing Education). 2018. Standards for accreditation of baccalaureate and graduate nursing programs. https://www.aacnnursing.org/Portals/42/CCNE/PDF/Standards-Final-2018.pdf (accessed September 29, 2020).
CDC (Centers for Disease Control and Prevention). 2018. Health care provider/clinician apps. https://www.cdc.gov/mobile/healthcareproviderapps.html (accessed November 11, 2020).
Center for Health Affairs. 2018. LPNs crucial to nursing workforce diversity. https://neohospitals.org/TheCenterForHealthAffairs/MediaCenter/NewsReleases/2018/August/Nursing-Workforce-Diversity (accessed May 14, 2020).
Cho, I., E. Kim, W. H. Choi, and N. Staggers. 2016. Comparing usability testing outcomes and functions of six electronic nursing record systems. International Journal of Medical Informatics 88:78–85.
Costello, M., A. Ballin, R. Diamond, and M. L. Gao. 2018. First generation college students and non-first generation college students: Perceptions of belonging. Journal of Nursing Education and Practice 8(12):59–65.
Devine, P. G., P. S. Forscher, A. J. Austin, and W. T. Cox. 2012. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology 48(6):1267–1278. https://doi.org/10.1016/j.jesp.2012.06.003.
DeWitty, V. P. 2018. What is holistic admissions review, and why does it matter? Journal of Nursing Education 57(4):195–196.
DeWitty, V. P., and T. A. Murray. 2020. Influence of climate and culture on minority faculty retention. Journal of Nursing Education 59(9):483–484.
DiAngelo, R. 2011. White fragility. International Journal of Critical Pedagogy 3(3):54–71.
DiAngelo, R. J. 2018. White fragility: Why it’s so hard for White people to talk about racism. Boston, MA: Beacon Press.
Diefenbeck, C., B. Michalec, and R. Alexander. 2016. Lived experiences of racially and ethnically underrepresented minority BSN students: A case study specifically exploring issues related to recruitment and retention. Nursing Education Perspectives 37(1):41–44.
Duffy, M. T., M. A. Friesen, K. G. Speroni, D. Swengros, L. A. Shanks, P. A. Waiter, and M. J. Sheridan. 2014. BSN completion barriers, challenges, incentives, and strategies. The Journal of Nursing Administration 44(4):232–236.
Effland, K. J., K. Hays, F. M. Ortiz, and B. A. Blanco. 2020. Incorporating an equity agenda into health professions education and training to build a more representative workforce. Journal of Midwifery & Women’s Health 65(1):149–159.
El-Sayed, M., and J. El-Sayed. 2014. Achieving lifelong learning outcomes in professional degree programs. International Journal of Process Education 6(1):37–42.
Fairman, J. A., N. A. Giordano, K. McCauley, and A. Villaruel. 2020. Invitational summit: Re-envisioning research focused PHD programs of the future. Journal of Professional Nursing 37. doi: 10.1016/j. profnurs.2020.09.004.
Fang, D., and G. D. Bednash. 2017. Identifying barriers and facilitators to future nurse faculty careers for DNP students. Journal of Professional Nursing 33(1):56–67. doi: 10.1016/j. profnurs.2016.05.008.
FDA (U.S. Food and Drug Administration). 2020. Digital health. https://www.fda.gov/medicaldevices/digital-health (accessed May 14, 2020).
Fee, E., and L. Bu. 2010. The origins of public health nursing: The Henry Street Visiting Nurse Service. American Journal of Public Health 100(7):1206–1207.
FitzGerald, C., and S. Hurst. 2017. Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics 18(1):19.
Flores, D. D., C. Bocage, S. Devlin, M. Miller, A. Savarino, and T. H. Lipman. 2020. When community immersion becomes distance learning: Lessons learned from a disrupted semester. Pedagogy in Health Promotion. Epub October 16, 2020. https://journals.sagepub.com/doi/pdf/10.1177/2373379920963596 (accessed November 11, 2020).
Forman, T. M., D. A. Armor, and A. S. Miller. 2020. A review of clinical informatics competencies in nursing to inform best practices in education and nurse faculty development. Nursing Education Perspectives 41(1):E3–E7.
Foronda, C., S. Liu, and E. B. Bauman. 2013. Evaluation of simulation in undergraduate nurse education: An integrative review. Clinical Simulation in Nursing 9(10):E409–E416.
Foronda, C., D. L. Baptiste, M. M. Reinholdt, and K. Ousman. 2016. Cultural humility: A concept analysis. Journal of Transcultural Nursing 27(3):210–217.
Foronda, C. L., D. L. Baptiste, T. Pfaff, R. Velez, M. Reinholdt, M. Sanchez, and K. W. Hudson. 2018. Cultural competency and cultural humility in simulation-based education: An integrative review. Clinical Simulation in Nursing 15:42–60.
Gaines, K. n.d. Why nursing school accreditation matters. https://nurse.org/education/nursing-school-accreditation (accessed April 30, 2020).
Gallagher, R. W., and J. R. Polanin. 2015. A meta-analysis of educational interventions designed to enhance cultural competence in professional nurses and nursing students. Nurse Education Today 35(2):333–340.
Gewin, V. 2020. The time tax put on scientists of colour. Nature 583:479–481.
Giddens, J. F. 2009. Changing paradigms and challenging assumptions: Redefining quality and NCLEX-RN pass rates. Journal of Nursing Education 48(3):123–124.
Giovenco, D. P., and T. E. Spillane. 2019. Improving efficiency in mobile data collection for place-based public health research. American Journal of Public Health 109(S2):S123–S125.
Glazer, G., A. Clark, and K. Bankston. 2016. Holistic admissions in nursing: We can do this. Journal of Professional Nursing 32(4).
Glazer, G., B. Tobias, and T. Mentzel. 2018. Increasing healthcare workforce diversity: Urban universities as catalysts for change. Journal of Professional Nursing 34(4):306–313.
Graham, C. L., S. M. Phillips, S. D. Newman, and T. W. Atz. 2016. Baccalaureate minority nursing students perceived barriers and facilitators to clinical education practices: An integrative review. Nursing Education Perspectives 37(3):130–137.
Greene, M. Z., M. K. FitzPatrick, J. Romano, L. H. Aiken, and T. S. Richmond. 2017. Clinical fellowship for an innovative, integrated BSN-PhD program: An academic and practice partnership. Journal of Professional Nursing 33(4):282–286.
Hamilton, N., and E. A. Haozous. 2017. Retention of faculty of color in academic nursing. Nursing Outlook 65(2):212–221. https://doi.org/10.1016/j.outlook.2016.11.003. PMID: 28087139.
Hayden, J., R. Smiley, M. Alexander, S. Kardong-Edgren, and P. Jeffries. 2014. The NCSBN national simulation study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation 5(2S):S1–S64.
Heath, S. 2019. Top considerations for SDOH screening, referral technologies. Health IT Analytics. https://patientengagementhit.com/news/top-considerations-for-sdoh-screening-referral-technologies (accessed April 21, 2021).
Hermer, J., A. Hirsch, B. Bekemeier, C. Nyirati, D. Wojnar, L. Wild, and G. Oneal. 2020. Integrating population health into nursing education: The process of gaining commitment from Washington’s nursing deans and directors. Journal of Professional Nursing 36(2):6–12.
Higgins, L. W., J. A. Shovel, A. L. Bilderback, H. L. Lorenz, S. C. Martin, D. J. Rogers, and T. E. Minnier. 2017. Hospital nurses’ work activity in a technology-rich environment: A triangulated quality improvement assessment. Journal of Nursing Care Quality 32(3):208–217.
Horn, C. 2020. COVID-19 response: Virtual simulation keeps nursing students on track for graduation. University of South Carolina. https://www.sc.edu/uofsc/posts/2020/04/covid_resilience_virtual_simulation_nursing.php#.X5S1e0JKjfY (accessed April 28, 2021).
HOSA (Future Health Professionals/Health Occupations Students of America). 2012. About HOSA. http://www.hosa.org/about (accessed March 30, 2020).
HRSA (Health Resources and Services Administration). 2017. Health careers pipeline and diversity programs. https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/program-highlights/diversity-and-pipeline-training-programs-2017.pdf (accessed April 30, 2020).
HRSA. 2019. Strategic plan FY 2019–2022. https://www.hrsa.gov/about/strategic-plan/index.html (accessed April 30, 2020).
HRSA. 2020. 2018 national sample survey of registered nurses. https://data.hrsa.gov/DataDownload/NSSRN/GeneralPUF18/2018_NSSRN_Summary_Report-508.pdf (accessed April 30, 2020).
HRSA. 2021. NHSC loan repayment program. HRSA National Health Service Corps. https://nhsc.hrsa.gov/loan-repayment/nhsc-loan-repayment-program.html (accessed March 29, 2021).
Ibrahim, S. A., M. E. Charlson, and D. B. Neill. 2020. Big data analytics and the struggle for equity in health care: The promise and perils. Health Equity I(1):99–101.
Iheduru-Anderson, K. C. 2020. The White/Black hierarchy institutionalizes White supremacy in nursing and nursing leadership in the United States. Journal of Professional Nursing. Advance online publication. https://doi.org/10.1016/j.profnurs.2020.05.005.
Iheduru-Anderson, K. C., and M. M. Wahi. 2017. Prevention of lateral violence in nursing through education: The bullying awareness seminar. The Journal of Nursing Education 56(12):762–763.
IOM (Institute of Medicine). 2003. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
IOM. 2010. Redesigning continuing education in the health professions. Washington, DC: The National Academies Press.
IOM. 2011. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
IOM. 2013. Interprofessional education for collaboration: Learning how to improve health from interprofessional models across the continuum of education to practice: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2016a. Assessing progress on the Institute of Medicine report The Future of Nursing. Washington, DC: The National Academies Press.
IOM. 2016b. A framework for educating health professionals to address the social determinants of health. Washington, DC: The National Academies Press.
IPEC (Interprofessional Education Collaborative). 2016. Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: Interprofessional Education Collaborative. https://ipec.memberclicks.net/assets/2016-Update.pdf (accessed June 2, 2021).
Jamshidi, N., Z. Molazem, F. Sharif, C. Torabizadeh, and M. Najafi Kalyani. 2016. The challenges of nursing students in the clinical learning environment: A qualitative study. Scientific World Journal 2016:1846178.
Jiménez-Rodríguez, D., M. D. M. Torres Navarro, F. J. Plaza Del Pino, and O. Arrogante. 2020. Simulated nursing video consultations: An innovative proposal during COVID-19 confinement. Clinical Simulation of Nursing 48:29–37. doi: 10.1016/j.ecns.2020.08.004.
Johansson, P., D. E. Jones, C. C. Watkins, M. E. Haisfield-Wolfe, and F. Gaston-Johansson. 2011. Physicians’ and nurses’ experiences of the influence of race and ethnicity on the quality of healthcare provided to minority patients, and on their own professional careers. Journal of National Black Nurses Association 22(1):43–56.
Jones, C. B., M. Toles, G. J. Knafl, and A. S. Beeber. 2018. An untapped resource in the nursing workforce: Licensed practical nurses who transition to become registered nurses. Nursing Outlook 66(1):46–55.
Kaiser Permanente. 2019. Kaiser Permanente launches social health network to address needs on a broad scale. https://permanente.org/kaiser-permanente-launches-social-health-network-to-address-needs-on-a-broad-scale (accessed November 11, 2020).
Kamau-Small, S., B. Joyce, N. Bermingham, J. Roberts, and C. Robbins. 2015. The impact of the care equity project with community/public health nursing students. Public Health Nursing 32(2):169–176.
Katz, J. R., C. Barbosa-Leiker, and S. Benavides-Vaello. 2016. Measuring the success of a pipeline program to increase nursing workforce diversity. Journal of Professional Nursing 32(1):6–14.
Kleinman, A., and P. Benson. 2006. Anthropology in the clinic: The problem of cultural competency and how to fix it. PLoS Medicine 3(10).
Kolade, F. M. 2016. The lived experience of minority nursing faculty: A phenomenological study. Journal of Professional Nursing 32(2):107–114. https://doi.org/10.1016/j.profnurs.2015.09.002.
Kononowicz, A. A., L. A. Woodham, S. Edelbring, N. Stathakarou, D. Davies, N. Saxena, L. Tudor Car, J. Carlstedt-Duke, J. Car, and N. Zary. 2019. Virtual patient simulations in health professions education: Systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research 21(7):e14676. https://doi.org/10.2196/14676.
Koschmann, K. S., N. K. Jeffers, and O. Heidari. 2020. “I can’t breathe”: A call for antiracist nursing practice. Nursing Outlook 68(5):539–541. doi: 10.1016/j.outlook.2020.07.004.
Kumm, S., N. Godfrey, D. Martin, M. Tucci, M. Muenks, and T. Spaeth. 2014. Baccalaureate outcomes met by associate degree nursing programs. 2014. Nurse Education 39(5):216–220. doi: 10.1097/NNE.0000000000000060. PMID: 24978014.
Lake, E. T. 2020. How effective response to COVID-19 relies on nursing research. Research in Nursing and Health 43(3):213–214.
Larsen, R., L. Reif, and R. Frauendienst. 2012. Baccalaureate nursing students’ intention to choose a public health career. Public Health Nursing 29:424–432. https://doi.org/10.1111/j.1525-1446.2012.01031.x.
Laternman, 2019 (May 2). Tuition or dinner? Nearly half of college students surveyed in a new report are going hungry. The New York Times. https://www.nytimes.com/2019/05/02/nyregion/hunger-college-food-insecurity.html (accessed March 29, 2021).
LCME (Liaison Committee on Medical Education). 2018. Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the MD degree. http://lcme.org/wp-content/uploads/filebase/standards/2019-20_Functions-and-Structure_2018-09-26.docx (accessed November 16, 2020).
Levine, S., C. Varcoe, and A. J. Browne. 2020. “We went as a team closer to the truth”: Impacts of interprofessional education on trauma-and violence-informed care for staff in primary care settings. Journal of Interprofessional Care 35(1):46–54.
Lewis and Clark Community College. n.d. Lewis and Clark mobile health unit. https://www.lc.edu/Mobile_Clinics (accessed February 21, 2021).
Lim, F., M. Johnson, and M. Eliason. 2015. A national survey of faculty knowledge, experience, and readiness for teaching lesbian, gay, bisexual, and transgender health in baccalaureate nursing programs. Nursing Education Perspectives 36:144–152.
Linden, M. A., and S. J. Redpath. 2011. A comparative study of nursing attitudes towards young male survivors of brain injury: A questionnaire survey. International Journal of Nursing Studies 48(1):62–69.
Loftin, C., S. D. Newman, B. P. Dumas, G. Gilden, and M. L. Bond. 2012. Perceived barriers to success for minority nursing students: An integrative review. International Scholarly Research Network Nursing 2012:806543.
Love, R., and J. M. Carrington. 2020. Introducing telehealth skills into the doctor of nursing practice curriculum. Journal of the American Association of Nurse Practitioners. Epub ahead of print. doi: 10.1097/JXX.0000000000000505.
Mann, K., J. Gordon, and A. MacLeod. 2009. Reflection and reflective practice in health professions education: A systematic review. Advances in Health Sciences Education Theory and Practice 14(4):595–621.
Marion-Martins, A. D., and D. L. M. Pinho. 2020. Interprofessional simulation effects for healthcare students: A systematic review and meta-analysis. Nurse Education Today 94:104568.
Marken, P. A., C. Zimmerman, C. Kennedy, R. Schremmer, and K. Smith. 2010. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. American Journal of Pharmaceutical Education 74(7):120.
Massachusetts Department of Higher Education Nursing Initiative. 2016. Massachusetts nursing of the future nursing core competencies. https://www.mass.edu/nahi/documents/NOFRNCompetencies_updated_March2016.pdf (accessed January 12, 2021).
McCue, P. L. 2017. The pre-collegiate pipeline to diversify the nursing workforce. Open Access Dissertations. Paper 575.
McMenamin, P. 2015. Diversity among registered nurses: Slow but steady progress. ANA Community blog. https://community.ana.org/blogs/peter-mcmenamin/2015/08/21/rn-diversity-note?ssopc=1 (accessed June 2, 2021).
Menzel, N., L. H. Willson, and J. Doolen. 2014. Effectiveness of a poverty simulation in Second Life®: Changing nursing student attitudes toward poor people. International Journal of Nursing Education Scholarship (11)11. doi: 10.1515/ijnes-2013-0076.
Merrell, M., J. Probst, E. Crouch, D. Abshire, S. McKinney, and E. Haynes. 2020. A national survey of RN-to-BSN programs: Are they reaching rural students? Journal of Nursing Education 59(10):557–565.
Metzger, M., and J. Taggart. 2020. A longitudinal mixed methods study describing 4th year baccalaureate nursing students’ perceptions of inclusive pedagogical strategies. Journal of Professional Nursing 36(4):229–235.
Metzger, M., T. Dowling, J. Guinn, and D. T. Wilson. 2020. Inclusivity in baccalaureate nursing education: A scoping study. Journal of Professional Nursing 36(1):5–14.
Miller, S., and P. Haley. 2020. Transitioning from hospitality to health care occupations. Federal Reserve Bank of Atlanta. https://www.frbatlanta.org/cweo/workforce-currents/2020/08/28/transitioning-from-hospitality-to-health-care-occupations (accessed February 24, 2021).
Minority Nurse. 2013. Mentors to the max. https://minoritynurse.com/mentors-to-the-max (accessed November 11, 2020).
Morton, J. L., F. M. Weierbach, R. Sutter, K. Livsey, E. Goehner, J. Liesveld, and M. K. Goldschmidt. 2019. New education models for preparing pre-licensure students for community-based practice. Journal of Professional Nursing 35(6):491–498.
Mosher, D. K., J. N. Hook, L. E. Captari, D. E. Davis, C. DeBlaere, and J. Owen. 2017. Cultural humility: A therapeutic framework for engaging diverse clients. Practice Innovations 2(4):221.
Murray, T. A., D. C. Pole, E. M. Ciarlo, and S. Holmes. 2016. A nursing workforce diversity project: Strategies for recruitment, retention, graduation, and NCLEX-RN success. Nursing Education Perspectives 37(3):138–143. PMID: 27405194.
NACNEP (National Advisory Council on Nurse Education and Practice). 2016. Preparing nurses for new roles in population health management. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/2016-fourteenthreport.pdf (accessed May 15, 2020).
NACNEP. 2019. Integration of social determinants of health in nursing education, practice, and research. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/nacnep-2019-sixteenthreport.pdf (accessed March 29, 2021).
NACNEP. 2020. Preparing nurse faculty, and addressing the shortage of nurse faculty and clinical preceptors. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/nacnep-17report-2021.pdf (accessed March 29, 2021).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016a. Big data and analytics for infectious disease research, operations, and policy: Proceedings of a workshop. Washington, DC: The National Academies Press
NASEM. 2016b. Developing a national STEM workforce strategy: A workshop summary. Washington, DC: The National Academies Press.
NASEM. 2017. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press.
NASEM. 2018a. Exploring a business case for high-value continuing professional development: Proceedings of a workshop. Washington, DC: The National Academies Press.
NASEM. 2018b. How people learn II: Learners, contexts, and cultures. Washington, DC: The National Academies Press.
NASEM. 2018c. Improving health professional education and practice through technology: Proceedings of a workshop. Washington, DC: The National Academies Press.
NASEM. 2019. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press.
NCDHHS (North Carolina Department of Health and Human Services). 2020. North Carolina health atlas. https://schs.dph.ncdhhs.gov/data/hsa (accessed November 11, 2020).
NCSBN (National Council of State Boards of Nursing). 2019. NCLEX-RN examination. https://www.ncsbn.org/2019_RN_TestPlan-English.pdf (accessed May 1, 2020).
NCSBN. 2020a. Number of candidates taking NCLEX examination and percent passing, by type of candidate. https://www.ncsbn.org/Table_of_Pass_Rates_2019_Q4.pdf (accessed May 1, 2020).
NCSBN. 2020b. Distance education. https://www.ncsbn.org/6662.htm (accessed November 11, 2020).
NEJM (New England Journal of Medicine) Catalyst. 2018. Healthcare big data and the promise of value-based care. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0290 (accessed November 11, 2020).
New York State. n.d. Leading the way to college affordability. https://www.ny.gov/programs/tuition-free-degree-program-excelsior-scholarship (accessed May 15, 2020).
NLN (National League for Nursing). 2013. Interprofessional education and healthcare simulation symposium. http://www.nln.org/docs/default-source/professional-development-programs/white-papersymposium-ipe-in-healthcare-simulation-2013-(pdf).pdf?sfvrsn=0 (accessed February 24, 2021).
NLN. 2015a. A vision for the changing faculty role: Preparing students for the technological world of health care. A diving Document from the National League for Nursing NLN Board of Governors. http://www.nln.org/docs/default-source/about/nln-vision-series-%28position-statements%29/nlnvision_8.pdf?sfvrsn=4 (accessed January 25, 2021).
NLN. 2015b. Interprofessional collaboration in education and practice. http://www.nln.org/docs/default-source/default-document-library/ipe-ipp-vision.pdf?sfvrsn=14 (accessed January 25, 2021).
NLN. 2016. Accreditation standards for nursing education programs. http://www.nln.org/docs/default-source/accreditation-services/cnea-standards-final-february-201613f2bf5c78366c709642ff00005f0421.pdf?sfvrsn=12 (accessed January 10, 2020).
NLN. 2019. A vision for integration of the social determinants of health into nursing education curricula. http://www.nln.org/docs/default-source/default-document-library/social-determinants-of-health.pdf?sfvrsn=2 (accessed January 10, 2020).
NONPF (National Organization of Nurse Practitioner Faculties). 2018. NONPF supports telehealth in nurse practitioner education 2018. https://cdn.ymaws.com/www.nonpf.org/resource/resmgr/2018_Slate/Telehealth_Paper_2018.pdf (accessed January 18, 2020).
NYSIM (City University of New York Grossman School of Medicine). 2017. NYSIM Center. http://nysimcenter.org (accessed May 18, 2020).
O’Connor, M. R., W. E. Barrington, D. T. Buchanan, D. Bustillos, M. Eagen-Torkko, A. Kalkbrenner, and A. B. de Castro. 2019. Short-term outcomes of a diversity, equity, and inclusion institute for nursing faculty. Journal of Nursing Education 58(11):633–640.
O’Lynn, C. 2017. Rethinking indicators of academic quality in nursing programs. Journal of Nursing Education 56(4):195–196.
Peek, M. E., M. B. Vela, and M. H. Chin. 2020. Practical lessons for teaching about race and racism: Successfully leading free, frank, and fearless discussions. Academic Medicine 95(12S):S139–S144.
Periyakoil, V. S. 2019. Building a culturally competent workforce to care for diverse older adults: Scope of the problem and potential solutions. Journal of the American Geriatrics Society 67(2):S423–S432.
Phillips, J. M., and B. Malone 2014. Increasing racial/ethnic diversity in nursing to reduce health disparities and achieve Health Equity. Public Health Reports 129(Suppl 2):45–50.
Phillips, K. E., A. Roberto, S. Salmon, and V. Smalley. 2020. Nursing student interprofessional simulation increases empathy and improves attitudes on poverty. Journal of Community Health Nursing 37(1):19–25.
Poore, J. A., D. L. Cullen, and G. L. Schaar. 2014. Simulation-based interprofessional education guided by Kolb’s experiential learning theory. Clinical Simulation in Nursing 10(5):e241–e247.
Porter, K., G. Jackson, R. Clark, M. Waller, and A. G. Stanfill. 2020. Applying social determinants of health to nursing education using a concept-based approach. Journal of Nursing Education 59(5):293–296.
Pritchard, T. J., J. D. Perazzo, J. A. Holt, B. P. Fishback, M. McLaughlin, K. D. Bankston, and G. Glazer. 2016. Evaluation of a summer bridge: Critical component of the Leadership 2.0 Program. Journal of Nursing Education 55(4):196–202.
Pritchard, T. J., G. Glazer, K. D. Bankston, and K. McGinnis. 2020. Leadership 2.0: Nursing’s next generation: Lessons learned on increasing nursing student diversity. The Online Journal of Issues in Nursing 25(2).
Purnell, T. S., J. K. Marshall, I. Olorundare, R. W. Stewart, S. Sisson, B. Gibbs, and L. A. Cooper. 2018. Provider perceptions of the organization’s cultural competence climate and their skills and behaviors targeting patient-centered care for socially at-risk populations. Journal of Health Care for the Poor and Underserved 29(1):481–496.
Quality Matters. 2020. QM-Certified Programs. https://www.qualitymatters.org/qm-membership/faqs/qm-certified-programs (accessed November 11, 2020).
Richmond, T. S., and M. Foman. 2019. Firearm violence: A global priority for nursing science. Journal of Nursing Scholarship 51:229–240. https://doi.org/10.1111/jnu.12421.
RINIMC (Rhode Island Nurses Institute Middle College Charter High School). n.d. RINIMC Charter High School. https://rinimc.org/rinimc-charter-high-school (accessed March 29, 2021).
Rosa, W. E., M. T. Ojemeni, V. Karanja, G. Cadet, A. Charles, C. McMahon, and S. Davis. 2019. Education equity in nursing: A cornerstone of sustainable development goal attainment. Public Health Nursing 36(4):447–448.
Rutledge, C. M., K. Kott, P. A. Schweickert, R. Poston, C. Fowler, and T. S. Haney. 2017. Telehealth and eHealth in nurse practitioner training: Current perspectives. Advances in Medical Education and Practice 8:399–409. https://doi.org/10.2147/AMEP.S116071.
RWJF (Robert Wood Johnson Foundation). 2020. Future of nursing scholars: PhD nurse profiles. http://futureofnursingscholars.org/phd-nurse-profiles (accessed November 11, 2020).
RWJF. 2021. Future of nursing scholars. http://futureofnursingscholars.org (accessed June 2, 2021).
Sabin, J. A., F. P. Rivara, and A. G. Greenwald. 2008. Physician implicit attitudes and stereotypes about race and quality of medical care. Medical Care 46(7):678–685.
Sabio, C., and N. Petges. 2020. Understanding the barriers to BSN education among ADN students: A qualitative study. Teaching and Learning in Nursing 15(1):45–52.
Salvucci, C., and C. A. Lawless. 2016. Nursing faculty diversity: Barriers and perceptions on recruitment, hiring, and retention. Journal of Cultural Diversity 23(2):65–75. PMID: 27439233.
Sanner, S., D. E. E. Baldwin, K. A. Cannella, and J. Charles. 2010. The impact of cultural diversity forum on students’ openness to diversity. Journal of Cultural Diversity 17(2).
Scheel, L. S., M. D. Peters, and A. C. M. Møbjerg. 2017. Reflection in the training of nurses in clinical practice settings: A scoping review protocol. JBI Database of Systematic Reviews and Implementation Reports 15(12):2871–2880.
Schmidt, S., M. George, and J. Bussey-Jones. 2016. Welcome to the neighborhood: Service-learning to understand social determinants of health and promote local advocacy. Diversity Equality Health Care 13(6):389–390.
Schroeder, C., and R. DiAngelo. 2010. Addressing whiteness in nursing education: The sociopolitical climate project at the University of Washington School of Nursing. Advances in Nursing Science 33(3):244–255. doi: 10.1097/ANS.0b013e3181eb41cf. PMID: 20693833.
Schroeder, K., B. Garcia, R. S. Phillips, and T. H. Lipman. 2019. Addressing social determinants of health through community engagement: An undergraduate nursing course. Journal of Nursing Education 58(7):423–426.
Sharma, M., A. D. Pinto, and A. K. Kumagai. 2018. Teaching the social determinants of health: A path to equity or a road to nowhere? Academic Medicine 93(1):25–30.
Shiffrin, R. M. 2016. Drawing causal inference from big data. Proceedings of the National Academy of Sciences 113(27):7308–7309.
Shin, S., J. H. Park, and J. H. Kim. 2015. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Education Today 35(1):176–182. doi: 10.1016/j.nedt.2014.09.009.
Siegel, J., D. L. Coleman, and T. James. 2018. Integrating social determinants of health into graduate medical education: A call for action. Academic Medicine 93(2):159–162.
Spector, N., J. Silvestre, M. Alexander, B. Martin, J. Hooper, A. Squires, and M. Ojemeni. 2020. NCSBN regulatory guidelines and evidence-based quality indicators for nursing education programs. Journal of Nursing Regulation 11(2S):S1–S64.
Spetz, J. 2018. Projections of progress toward the 80% bachelor of science in nursing recommendation and strategies to accelerate change. Nursing Outlook 66(4):394–400.
Squires, A., C. Kovner, F. Faridaben, and D. Chyun. 2013. Assessing nursing student intent for PhD study. Nurse Education Today 34(11):1405–1410.
SSIH (Society for Simulation in Healthcare). n.d. About simulation. https://www.ssih.org/About-SSH/About-Simulation (accessed January 12, 2021).
Storfjell, J., B. Winslow, and J. Saunders. 2017. Catalysts for change: Harnessing the power of nurses to build population health in the 21st century. Princeton, NJ: Robert Wood Johnson Foundation.
Strauss, V. 2020. Housing and food insecurity affecting many college students, new data says. https://www.washingtonpost.com/education/2020/02/20/housing-food-insecurity-affecting-many-college-students-new-data-says (accessed January 12, 2021).
Sukhera, J., M. Wodzinski, M. Rehman, and C. M. Gonzalez. 2019. The implicit association test in health professions education: A meta-narrative review. Perspectives in Medical Education 8(5):267–275.
Sullivan, L. W. 2004. Missing persons: Minorities in the health professions. A report of the Sullivan Commission on Diversity in the Healthcare Workforce. The Sullivan Commission. https://campaignforaction.org/wp-content/uploads/2016/04/SullivanReport-Diversity-in-Healthcare-Workforce1.pdf (accessed March 29, 2021).
Szanton, S. L., J. W. Wolff, B. Leff, R. J. Thorpe, E. K. Tanner, C. Boyd, Q. Xue, J. Guralnik, D. Bishai, and L. N. Gitlin.2014. CAPABLE trial: A randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: Rationale and design. Contemporary Clinical Trials 38(1):102–112. https://doi.org/10.1016/j.cct.2014.03.005.
Taylor, H., C. Loftin, and H. Reyes. 2014. First-time NCLEX-RN pass rate: Measure of program quality or something else? Journal of Nursing Education 53(6):336–341.
The Macy Foundation. 2020. Addressing harmful bias and eliminating discrimination in health professions learning environments. Conference recommendations February 24–27, 2020. Atlanta, GA: Josiah Macy Jr. Foundation.
The Poverty Simulation. n.d. The Poverty Simulation. http://www.povertysimulation.net/about (accessed May 14, 2020).
ThinkTank, n.d. The cost of poverty experience. https://thinktank-inc.org/cope (accessed November 11, 2020).
Thornton, M., and S. Persaud. 2018. Preparing today’s nurses: Social determinants of health and nursing education. The Online Journal of Issues in Nursing 23(3).
Tilden, V. P., K. S. Cox, J. E. Moore, and M. D. Naylor. 2018. Strategic partnerships to address adverse social determinants of health: Redefining health care. Nursing Outlook 66(3):233–236.
Topaz, M., and L. Pruinelli. 2017. Big data and nursing: Implications for the future. Studies in Health Technology and Informatics 232:165–171.
Turk, M. T., and A. M. Colbert. 2018. Using simulation to help beginning nursing students learn about the experience of poverty: A descriptive study. Nurse Education Today 71:174–179. Epub September 29, 2018. doi: 10.1016/j.nedt.2018.09.035. PMID: 30292059.
Tyczkowski, B. L., and J. Reilly. 2017. DNP-prepared nurse leaders: Part of the solution to the growing faculty shortage. The Journal of Nursing Administration 47(7–8):359–360.
UND (University of North Dakota). 2020. RAIN: No excuses orientation. https://cnpd.und.edu/rain/no-excuses.html (accessed November 11, 2020).
U.S. Department of Education. n.d.a. Competency-based learning or personalized learning. https://www.ed.gov/oii-news/competency-based-learning-or-personalized-learning (accessed November 11, 2020).
U.S. Department of Education. n.d.b. Public service loan forgiveness. https://studentaid.gov/manage-loans/forgiveness-cancellation/public-service (accessed September 2, 2020).
Valderama-Wallace, C. P., and E. C. Apesoa-Varano. 2019. “Social justice is a dream”: Tensions and contradictions in nursing education. Public Health Nursing 36(5):735–743.
Velasquez, D., and A. Mehrotra. 2020. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. Health Affairs Blog. doi: 10.1377/hblog20200505.591306.
Villarruel, A. M., and M. E. Broome. 2020. Beyond the naming: Institutional racism in nursing. Nursing Outlook 68(4):375–376.
von Wendt, C. E. A., and L. Niemi-Murola. 2018. Simulation in interprofessional clinical education. Simulation in Healthcare 13(2):131–138.
Waite, R., and D. Nardi. 2019. Nursing colonialism in America: Implications for nursing leadership. Journal of Professional Nursing 35(1):18–25. doi: 10.1016/j.profnurs.2017.12.
Walker, K., M. Arbour, and J. Waryold. 2016. Educational strategies to help students provide respectful sexual and reproductive health care for lesbian, gay, bisexual, and transgender persons. Journal of Midwifery and Women’s Health 61(6):737–743.
Wallace, J., K. Decosimo, and M. Simon. 2019. Applying data analytics to address social determinants of health in practice. North Carolina Medical Journal 80:244–248.
WGU (Western Governors University). 2020. Competency-based education. https://www.wgu.edu/about/competency-based-education.html (accessed November 11, 2020).
Whitfield-Harris, L., and J. S. Lockhart. 2016. The workplace environment for African American faculty employed in predominantly White institutions. The Association of Black Nursing Faculty Journal 27(2):28–38. PMID: 27263232.
Whitfield-Harris, L., J. S. Lockhart, R. Zoucha, and R. Alexander. 2017. The lived experience of Black nurse faculty in predominantly White schools of nursing. Journal of Transcultural Nursing 28(6):608–615.
WHO (World Health Organization). Regional Office for the Eastern Mediterranean. 2015. The growing need for home health care for the elderly: Home health care for the elderly as an integral part of primary health care services. https://apps.who.int/iris/handle/10665/326801 (accessed March 29, 2021).
Wilkie, M. L. 2020. Empowered by cultural identity and catalyzed by resilience: A path to support American Indian nursing student success. Creative Nursing 26(1):43–47.
Williams, S. D., K. Hansen, M. Smithey, J. Burnley, M. Koplitz, K. Koyama, and A. Bakos. 2014. Using social determinants of health to link health workforce diversity, care quality and access, and health disparities to achieve health equity in nursing. Public Health Reports 129(1):32–36.
Wilson, A. H., S. Sanner, and L. E. McAllister. 2010. An evaluation study of a mentoring program to increase the diversity of the nursing workforce. Journal of Cultural Diversity 17(4).
Wise, P. H. 2012. Emerging technologies and their impact on disability. The Future of Children 169–191.
Yale School of Nursing. 2020. Simulation technology redirects nursing curriculum during COVID-19. https://nursing.yale.edu/news/simulation-technology-redirects-nursing-curriculum-during-covid-19 (accessed January 12, 2021).
Yen, P. Y., and S. Bakken. 2012. Review of health information technology usability study methodologies. Journal of the American Medical Informatics Association 19(3):413–422.
Yoder, C. M., and M. S. Pesch. 2020. An academic–fire department partnership to address social determinants of health. Journal of Nursing Education 59(1):34–37.
Zandee, G., D. Bossenbroek, M. Friesen, K. Blech, and R. Engbers. 2010. Effectiveness of community health worker/nursing student teams as a strategy for public health nursing education. Public Health Nursing 27(3):277–284.
This page intentionally left blank.


























































