1
Introduction
It will never be comfortable or easy to advocate for change, but I am a nurse leader because I am comfortable with being uncomfortable…. I am unafraid to use my voice to influence positive change. In doing so, I have taught others how to advocate and inspired others to use their voices as well.
—Andrea Riley, RN, Nebraska 40 Under 40 Leader
Two decades ago, the Institute of Medicine (IOM) published Crossing the Quality Chasm: A New Health System for the 21st Century (IOM, 2001). That report delineates six aims for improving health care to reduce the burden of illness, injury, and disability and improve the functioning of the people of the United States. With the explicit purpose of securing these benefits for all people, equity was included as one of the six aims, incorporating a focus on both individuals and the population. In the intervening 20 years, among the six aims, equity in health and health care has been perhaps the least understood, considered, and addressed—until now.
Today, a rapidly growing body of evidence documenting the relationship among social determinants of health (SDOH), inequity in health and health care, and the health status of individuals and populations is generating a widespread call to action. Because of its impact on health status, achieving health equity is urgent. Achieving this goal will require stakeholders, including nurses and the nursing profession, to focus singular attention on closing the chasm between what is known about equity in health and health care and what can be done to achieve it. The 2011 IOM report The Future of Nursing: Leading Change, Advancing Health focuses on actions that can build critical capacity in nursing to meet increased demand for care and advance health system improvement. Significant progress has been made in building the capacity called for in that report; however, more remains to be done.
The vision of the Committee on the Future of Nursing 2020–2030, which informs this report, is the achievement of health equity in the United States built on strengthened nursing capacity and expertise. By leveraging these attributes, nursing will help to create and contribute comprehensively to equitable public
health and health care systems that are designed to work for everyone. To achieve health equity, the committee also envisions a major role for the nursing profession in engaging in the complex work of aligning public health, health care, social services, and public policies to eliminate health disparities and achieve health equity.
To provide a broad and deep foundation from which to achieve this vision, the committee formulated nine recommendations (see Chapter 11) that touch on virtually every component of the nursing profession. Implementing these recommendations to achieve the committee’s vision will require substantive and sustained action by the nursing profession. Nursing will need to consider and reset components of education, leadership, practice, and research, as well as the structures and priorities of vitally important nursing organizations. Nurses will need new knowledge on which to act, and the profession itself will need to reflect the diversity of the populations it serves. Nurses working in all settings will need to be prepared to participate on and lead multidisciplinary teams and multisector partnerships and, through data development, management, and use, identify and respond to challenges that disproportionately affect some segments of the U.S. population, ranging from public health emergencies to community characteristics.
The committee recognizes the significant scope and scale of its recommendations and the associated efforts required to implement them. Mobilizing to take the actions called for in this report will require change, commitment, and perseverance. Nurses will also need courage to engage in difficult conversations about racial inequities, address their own biases and those in the institutions where they work, and then participate actively in calling out and breaking down structural racism. Given the evidence delineating the adverse impacts of inequity on health, operationalizing the recommendations in this report will uphold nursing’s social responsibility to improve the health of all people.
The committee also notes, however, that for nursing to make the substantive contributions needed to advance health equity, the profession will require resources, autonomy, and positions of leadership as called for in this report. Across the coming decade, nurses will be key contributors to the substantial progress toward health and health care equity that is needed in the United States. They will do so by taking on expanded roles, working in new settings in innovative ways, and partnering with communities and other sectors. Achieving this vision will require much more rapid, substantive, and widespread efforts than those undertaken to date. If the path set forth in this report and its recommendations are followed, the committee envisions that this decade will usher in a new era of promoting health equity and well-being for all, and the nursing profession will have contributed substantially to making this so.
THE NURSING PROFESSION
Nursing is the nation’s largest health profession, numbering close to 4 million nurses in 2018 (HRSA, 2021). There are three categories of nurses, based on
education—licensed practical nurses (LPNs)/licensed vocational nurses (LVNs), registered nurses (RNs), and advanced practice registered nurses (APRNs)—practicing in many different specialties and settings (see Box 1-1). More information about the current and future nursing workforce can be found in Chapter 3.
STUDY CONTEXT
As of this writing, the world is confronting the pandemic caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Daily headlines report the growing numbers of sick and dying around the world. Many nurses are going to work every day, often for extended shifts, to care for patients despite the risk to themselves and their family members. Nurses are on the front lines of this crisis, in many cases without adequate personal protective equipment (PPE) or psychological PPE to promote their mental health and well-being. They are working in emergency rooms, hospitals, schools, and urgent care centers. They are in research labs and at policy-making tables. They are educating the public at the local, state, and national levels. And they are in their communities conducting testing and contact tracing and helping to dispense vaccines.
This crisis has occurred in the context of broader changes in health care in the United States that have important implications for the nursing profession. The nation is still adapting to the passage of the Patient Protection and Affordable Care Act of 2010, but additional policy changes will come in this decade with the recent passage of the American Rescue Plan Act of 2021.1 Significantly, low- and middle-income individuals and families will receive additional help with their insurance premiums and tax credits and mental health and substance abuse services.
Approaches to health care payment are evolving, with fee-for-service payment increasingly giving way to an emphasis on the use of payment to reward providers for achieving better health outcomes. Attention to the social determinants that influence health and well-being has also increased as researchers have demonstrated the direct effects of such environmental factors as inadequate housing, food insecurity, lack of transportation, lack of or underemployment, social isolation, and unhealthy environments on health, on demands on the health care system, and on health care costs (Adler et al., 2016). Policy makers focusing on these issues are seeking to address not only rising costs but also health inequities
___________________
1 American Rescue Plan Act of 2021, HR 1319, 117th Cong. See https://www.congress.gov/bill/117th-congress/house-bill/1319 (accessed April 10, 2021).
perpetuated by poverty, institutional and systemic racism, and discrimination, and it is important to recognize the key role of nurses in addressing these problems (Pittman, 2019).
A FOCUS ON SOCIAL DETERMINANTS OF HEALTH
The United States has devoted vast resources to medical care to improve the nation’s health. Medical care denotes services clinicians provide on a daily basis, such as performing surgeries, checking blood sugar, and titrating blood pressure medications, in settings that include hospitals, surgery centers, and clinics. However, medical care emphasizes disease treatment rather than prevention and rarely addresses SDOH, such as socioeconomic factors and physical environments, that are strong predictors of health outcomes (Hood et al., 2016; Nau et al., 2019). SDOH affect a wide range of outcomes in health, functioning, and quality of life; they affect individuals, communities, and the overall health of the national population; and they have consequences for the economy, national security, business, and future generations (NASEM, 2017). Chapter 2 provides a more detailed overview of SDOH and health equity.
Available evidence suggests that characteristics both of the health care system and of communities and society influence health outcomes and their equity in the United States (IOM, 2013). There are a number of ways to conceptualize the overlapping pursuit of goals for population health, health equity, and better health care. The Centers for Disease Control and Prevention (CDC), for example, describes population health interventions as the harnessing of multiple sectors (e.g., public health, industry, academia, health care, local government) to improve health outcomes (CDC, 2019). And the Institute for Healthcare Improvement has defined the primary objectives for health care improvement as simultaneously improving the patient experience of care, improving the health of populations, and reducing the per capita cost of health care (IHI, n.d.).
Nurses’ Accessibility
Nurses have long been advocates for health equity and worked to address the root causes of poor health (Pittman, 2019). Nurses at all levels are present in a wide range of settings outside of traditional health care facilities, working directly in communities to provide care in schools, workplaces, and prisons. They make home visits to families, provide primary care to school-age children, administer vaccines, provide health education, coordinate health care services within and across settings, and educate people on preventive measures for staying healthy (Bodenheimer and Mason, 2016). Nurses routinely work with people who have had adverse life experiences, including not only medical challenges but also social stressors such as trauma, lack of food, or homelessness. They are also key to the provision of long-term, hospice, and palliative care and support for care-
givers (Dahlin and Coyne, 2019; Pawlow et al., 2018). Nurse practitioners (NPs) working in primary care are often the only providers caring for low-income or uninsured people, Medicaid beneficiaries, and historically disadvantaged groups in both rural and urban populations (Auerbach et al., 2018; Barnes et al., 2018; Buerhaus, 2018), who cannot always easily access a physician. These interactions give nurses opportunities to get to know and engage meaningfully with people and families on matters related to health and well-being, health care, and the social factors that influence health.
Expansion of Nurses’ Responsibilities and Capabilities
Nurses are increasingly developing new kinds of expertise while transitioning to new roles and nurse-led alternative models of care (Pittman, 2019). They are helping to develop new ways of keeping individuals connected to health care services, such as telehealth and home care (Dillon et al., 2018; Glasgow et al., 2018; Machon et al., 2019). And they are increasingly moving into leadership positions in which they are serving as collaborative partners with other health care workers, as well as coordinating with others in non–health care settings and areas of focus (Dyess et al., 2016) to improve overall health.
Even as their capabilities and roles evolve, nurses will face new challenges over the coming decade. By 2030, the nursing profession will look very different than it does today and will need to provide care for a changing America. As the U.S. population changes in diversity, age, and health status, the distribution of people along those spectrums will change, and the roles of nurses will change accordingly. More than 1 million RNs in the baby boom generation, who have amassed a substantial body of knowledge and experience, will retire during this decade. Moreover, as the U.S. population ages, patients will include increasing percentages of older people, many of whom will have multiple comorbid conditions that will increase the complexity and intensity of the nursing care they require. As the population diversifies in race and ethnicity and other factors, nurses will need to be well-versed in providing care that is culturally respectful and appropriate. Nurses also will be called on to address the persistent and in most cases widening disparities in health tied to poverty, structural racism, and discrimination that have been magnified and exacerbated by the COVID-19 pandemic. There is an increasing need as well for mental health care among the general population, stemming from high rates of depression, suicide, anxiety, trauma, and stress due to such challenges as substance abuse, gun violence, and now the lingering effects of the pandemic (Baker et al., 2019). Shifts in care models, where care is delivered, and new technology applications will impact how nurses interface with individuals seeking health care. And nurses will have to expand their roles to supplement a shrinking primary care workforce, provide care to rural populations, help improve maternal health outcomes, and deliver more health and preventive care in community-based settings (Edmonson et al., 2017).
PREVIOUS WORK OF THE NATIONAL ACADEMIES ON THE FUTURE OF NURSING
Before embarking on this study, the National Academies produced two reports on the future of nursing. The first—The Future of Nursing: Leading Change, Advancing Health (IOM, 2011)—offered four key messages, embodied in that study committee’s recommendations:
- Nurses should practice to the full extent of their education and training.
- Nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression.
- Nurses should be full partners, with physicians and other health care professionals, in redesigning health care in the United States.
- Effective workforce planning and policy making require better data collection and information infrastructure.
In support of recommendations offered in The Future of Nursing, many organizations worldwide invested in bolstering the nursing workforce over the ensuing decade. The Center to Champion Nursing in America (CCNA) called for the Future of Nursing: Campaign for Action, which was organized to implement solutions to the challenges facing the nursing profession and to build on nurse-based approaches. CCNA, a joint effort of the Robert Wood Johnson Foundation (RWJF), AARP, and the AARP Foundation, is a leading national resource center created to ensure that the nation has the skilled nurses needed to provide care for all Americans, now and in the future. The Future of Nursing: Campaign for Action serves as a focal point for information, public policy research, and analysis at the state, federal, and international levels. The campaign has helped form state action coalitions—groups of nurses and other health care providers, employers, patients, students, and others—in every state to work with health, education, business, and other leaders in promoting better health through nursing to improve health equity and to create communities in which everyone has access to high-quality care. The campaign’s focus has been on implementing the recommendations of the 2011 The Future of Nursing report, as well as inspiring and specifying strategies for involving nurses in addressing SDOH and health equity.
The second prior National Academies study on the future of nursing is a 2016 assessment of the Campaign for Action’s effectiveness in achieving the goals set forth in the 2011 report. The committee that produced the report on that assessment—Assessing Progress on the Institute of Medicine Report The Future of Nursing (NASEM, 2016)—noted significant progress in galvanizing nurses at the national and state levels to implement the 2011 report’s recommendations. However, the committee strongly encouraged the Campaign for Action to
- engage a broader network of stakeholders to increase awareness of nurses’ ability to participate fully in practice, education, collaboration, and leadership among health professionals;
- promote diversity in the nursing workforce; and
- collect better data to assess and drive progress.
STATEMENT OF TASK
With the intent of building on the above two previous reports to engage nursing in efforts to achieve health equity, RWJF developed the Statement of Task for the present study, provided in Box 1-2.
STUDY APPROACH
To conduct this study, the National Academies assembled a committee of 15 experts in the fields of nursing leadership, education, practice, and workforce; some members have backgrounds in health policy, economics and health care finance, informatics,2 population health and health disparities, health care quality and delivery, and health care research and interventions. Biographical sketches of the committee members and study staff are provided in Appendix A.
The committee met eight times, including two meetings during which sessions open to the public were held. In addition, some committee members conducted site visits in Chicago, Philadelphia, and Seattle to better understand the context for the challenges and opportunities facing nurses working in different types of health care settings who are actively addressing social needs and SDOH in their work. The committee also conducted town hall meetings in those same cities to hear from other experts and gather input from interested members of the public.
Further information about the committee’s data and information gathering is available in Appendix B. Briefly, in addition to its members’ knowledge and expertise, its public sessions, and its town hall meetings, the committee relied on a variety of data and information sources to support its deliberations, including
___________________
2 Nursing informatics is “the specialty that integrates nursing science with multiple information and analytical sciences to identify, define, manage and communicate data, information, knowledge and wisdom in nursing practice” (ANA, 2016).
- staff searches of the published literature, such as a search for evidence-based examples of successful programs that improved health equity in which nurses played essential roles;
- grey3 literature searches focused on SDOH (including reports and articles from government agencies, universities, foundations, professional associations, and other organizations);
- data and analyses provided by AcademyHealth4 in response to the committee’s requests;
- papers commissioned for this study; and
- public and organizational statements pertaining to the committee’s task.
Committee’s Interpretation of Its Task
The committee interpreted its Statement of Task (see Box 1-2) as a challenge to map out a path for the nursing profession to help improve all aspects of the U.S. health care system and create a culture of health. As expressed by RWJF, the objective of a culture of health is “to help raise the health of everyone in the U.S.” (RWJF, n.d.). The committee interpreted the concept of a culture of health as essentially denoting health equity, and therefore considered health equity to be its primary focus as it considered the evolving roles of nurses and the nursing profession in helping to improve population health.
Challenges in Addressing the Task
In its information-gathering process, the committee was challenged by the lack of peer-reviewed, published literature regarding the involvement and/or impact of nurses in new and challenging roles. This paucity of published literature is not surprising, given that the sponsor’s charge to the committee was to look to the future. Although some published reports address innovative programs for which there is evidence and that feature nurses in key roles, many such programs are novel and have not yet reported outcomes. In other cases, reports on some programs assumed to rely heavily on nurses do not explicitly describe their roles or responsibilities. To address that challenge, the committee sought reports of potentially scalable, innovative models of care in which nurses have played key roles and for which evidence of improvement in health equity might be avail-
___________________
3 Grey literature is “literature that is produced by and on all levels of government, academia, private industry in both print and electronic formats, and is not associated with commercial publishers” (Farace and Frantzen, 2005).
4 AcademyHealth supports the production and use of evidence to inform policy and practice. The organization was formed in June 2000, following a merger between the Alpha Center and the Association for Health Services Research, to educate consumers and policy makers about the importance of health services research, secure funding for the field, and provide networking and professional development opportunities.
able. Similarly, new information regarding COVID-19 is continually emerging as knowledge of the novel SARS-CoV-2 is gained. Given all of these challenges, this report relies on the available knowledge base; however, the committee stresses that lessons will continue to be learned and that evidence will continue to build for years after this report has been released.
Study Framework
The committee developed a framework to guide its examination of how nursing can address medical and SDOH to improve the health of individuals and populations and increase equity in health and health care (see Figure 1-1). The framework structures this report’s discussion of the key areas for strengthening the nursing profession to meet the challenges of the decade ahead. The heart of this framework is the key areas, specifically the nursing workforce (see Chapter 3), leadership (see Chapter 9), nursing education (see Chapter 7), nurse well-being (see Chapter 10), and emergency preparedness and response (see Chapter 8) and the responsibilities of nursing with respect to structural and individual determinants of health. Nurses play multiple roles in acute, community, and public health settings that include, but are not limited to, care team member and leader, primary care provider, patient and family advocate, population health coordina-
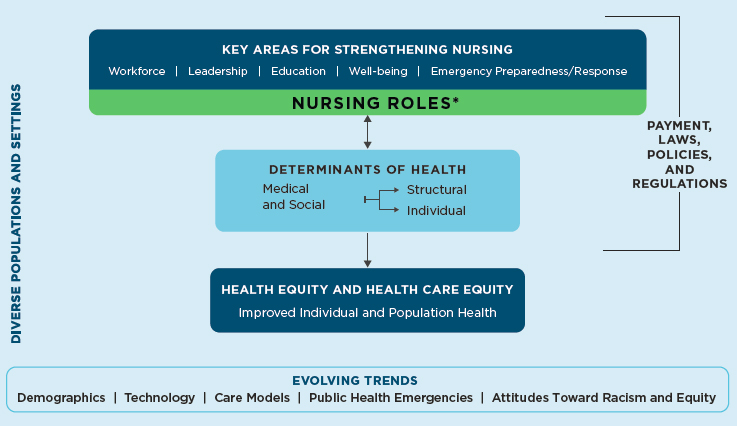
* Examples of nursing roles in acute, community, and public health settings include care coordinator, policy maker, clinician, advocate, educator, researcher/scientist, administrator, and informaticist.
tor, educator, public health professional, health systems leader, organizational and public policy maker, researcher and scientist, and informaticist. Through each of these roles, they impact the medical and social factors that drive health outcomes and the equity of health and health care. Nurses can address SDOH through interventions at both the individual level (e.g., referring an individual’s family to a food assistance program) and the structural level (e.g., alleviating the problem of food insecurity in the community). Similarly, nurses can address medical determinants at both the individual level (e.g., providing patient education and medication management) and the structural level (e.g., implementing a system of team-based multisector care that includes coordination of care across settings and sectors).
Nursing approaches need to be flexible given the complex, multiple, intersecting characteristics of individuals and families and the opportunities and demands of diverse populations and settings, as well as the many evolving trends that affect the nature of their work. Relevant trends include the aging and racial/ethnic diversification of the population, technology advances, evolving models of care, growing recognition of the importance of preparedness for and response to public health emergencies, and increasing awareness of racism and equity issues. Payment methods, laws, organizational policies, and regulations impact the ability of nurses to function successfully in addressing the determinants of health.
ORGANIZATION OF THIS REPORT
Following this introductory chapter, the report continues with Chapter 2, which provides an overview of SDOH and health equity to highlight the challenges nurses are being asked to address—themes that are repeated throughout the report. Chapter 3 explores the workforce needed to prepare the nursing profession of the future. In Chapters 4 and 5, respectively, the committee examines some of the current ways in which nurses are working to improve health care equity and health equity. Chapter 6 describes the financial infrastructure needed to support the nursing profession. Chapter 7 explores the changes in education needed to prepare and engage the nursing profession to address disparities and contribute to achieving equity in health and health care, and Chapter 8 describes the role of nurses in disaster preparedness and public health emergency response. Chapters 9 and 10, respectively, examine nursing leadership, with a focus on ensuring that nurses are leading and engaging across sectors and teams, and the importance of supporting nurses’ well-being as they take on new roles and challenges to meet evolving needs. The committee’s conclusions are presented in Chapters 2 through 10. Finally, Chapter 11 offers the committee’s key messages and perspectives for the future in the form of recommendations and research priorities.
The report’s appendixes provide additional information. The biosketches of the committee members and project staff are presented in Appendix A. Additional
detail on the committee’s information-gathering methods can be found in Appendix B. Appendix C presents a comprehensive overview of the methods used to gather information on the nursing workforce. Appendix D provides a glossary of the terms used throughout the report. Appendix E includes a supplemental statement on the report, followed by Appendix F, presenting the committee’s response to that supplemental statement. Appendix G includes illustrative profiles of nursing programs and organizations.
REFERENCES
Adler, N. E., M. M. Glymour, and J. Fielding. 2016. Addressing social determinants of health and health inequalities. Journal of the American Medical Association 316(16):1641–1642.
ANA (American Nurses Association). 2016. Nursing informatics: Scope and standards of practice. 2nd edition. Silver Spring, MD: American Nurses Association.
APRN (Advanced Practice Registered Nurse) Joint Dialogue Group. 2008. Consensus model for APRN regulation: Licensure, accreditation, certification & education. https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf (accessed March 23, 2021).
Auerbach, D. I., D. O. Staiger, and P. I. Buerhaus. 2018. Growing ranks of advanced practice clinicians—Implications for the physician workforce. New England Journal of Medicine 378(25):2358–2360.
Baker, M. W., C. Dower, P. B. Winter, M. M. Rutherford, and V. T. Betts. 2019. Improving nurses’ behavioral health knowledge and skills with mental health first aid. Journal for Nurses in Professional Development 35(4):210–214.
Barnes, H., M. R. Richards, M. D. McHugh, and G. Martsolf. 2018. Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Affairs 37(6):908–914.
Bodenheimer, T., and D. Mason. 2016. Registered nurses: Partners in transforming primary care. In Preparing Registered Nurses for Enhanced Roles in Primary Care. Conference conducted in Atlanta, GA, sponsored by the Josiah Macy Jr. Foundation. New York: Josiah Macy Jr. Foundation.
Buerhaus, P. 2018. Nurse practitioners: A solution to America’s primary care crisis. Washington, DC: American Enterprise Institute.
CDC (Centers for Disease Control and Prevention). 2019. What is population health? https://www.cdc.gov/pophealthtraining/whatis.html (accessed November 7, 2020).
Dahlin, C., and P. Coyne. 2019. The palliative APRN leader. Annals of Palliative Medicine 8(1):S30–S38.
Dillon, J., J. N. Himes, K. Reynolds, and V. Schirm. 2018. An innovative partnership to improve student health: Response to a community health needs assessment. Journal of Nursing Administration 48(3):149–153.
Dyess, S. M., B. A. Pratt, L. Chiang-Hanisko, and R. O. Sherman. 2016. Growing nurse leaders: Their perspectives on nursing leadership and today’s practice environment. Online Journal of Issues in Nursing 21(1).
Edmonson, C., C. McCarthy, S. Trent-Adams, C. McCain, and J. Marshall. 2017. Emerging global health issues: A nurse’s role. Online Journal of Issues in Nursing 22(1).
Farace, D. J., and J. Frantzen. 2005. A review of four information professionals—their work and impact on the field of grey literature. In GL5 Conference Proceedings. http://www.textrelease.com/images/TGJ_V1N3.pdf#page=34 (accessed July 23, 2021).
Glasgow, M. E. S., A. Colbert, J. Vator, and S. Cavanagh. 2018. The nurse–engineer: A new role to improve nurse technology interface and patient care device innovations. Journal of Nursing Scholarship 50(6):601–611.
Hood, C. M., K. P. Gennuso, G. R. Swain, and B. B. Catlin. 2016. County health rankings: Relationships between determinant factors and health outcomes. American Journal of Preventive Medicine 50(2):129–135.
HRSA (Health Resources and Services Administration). 2021. Technical report for the national sample survey of registered nurses. https://bhw.hrsa.gov/data-research/access-data-tools/national-sample-survey-registered-nurses (accessed March 23, 2021).
IHI (Institute for Healthcare Improvement). n.d. The IHI triple aim. http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx (accessed October 7, 2020).
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2011. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
IOM. 2013. U.S. health in international perspective: Shorter lives, poorer health. Washington, DC: The National Academies Press.
Machon, M., D. Cundy, and H. Case. 2019. Innovation in nursing leadership: A skill that can be learned. Nursing Administration Quarterly 43(3):267–273.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Assessing progress on the Institute of Medicine report The Future of Nursing. Washington, DC: The National Academies Press.
NASEM. 2017. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press.
Nau, C., J. L. Adams, D. Roblin, J. Schmittdiel, E. Schroeder, and J. F. Steiner. 2019. Considerations for identifying social needs in health care systems: A commentary on the role of predictive models in supporting a comprehensive social needs strategy. Medical Care 57(9):661–666.
Pawlow, P., C. Dahlin, C. L. Doherty, and M. Ersek. 2018. The hospice and palliative care advanced practice registered nurse workforce: Results of a national survey. Journal of Hospice & Palliative Nursing 20(4):349–357.
Pittman, P. 2019. Rising to the challenge: Re-embracing the Wald model of nursing. American Journal of Nursing 119(7):46–52.
RWJF (Robert Wood Johnson Foundation). n.d. About RWJF. https://www.rwjf.org/en/about-rwjf.html (accessed January 13, 2020).














