9
Payment to Support High-Quality Primary Care
The committee supports a low-burden payment model that enables sustainable, team- and relationship-based, high-quality, integrated primary care; allows all people to have ready access to primary care teams across modalities; and assists people in addressing social determinants of health (SDOH). Payment should be adequate to support high-quality, independent primary care practices and flexible enough to support an emerging array of new delivery models. Payment reform should not, however, be a mechanism for reducing U.S. health care costs significantly in the short term but rather represent an investment for improving the health of the population.
WHY MONEY MATTERS
A fundamental assumption in the vision above is that money matters for achieving policy priorities. Payment models create the fiscal space in which care delivery can either flourish or be constrained. Vision statements, research evidence, leadership, and well-intentioned policy will not change the structure and performance of a system if they are not supported by adequate, goal-aligned resources. While a broad range of personal and social values motivate maintaining health and providing health care, an element of health care is transactional, with payment rendered for services provided. During the committee’s information-gathering activities, patients underscored the difficulty and burdensome nature of navigating the health system and payment for services, highlighting that the fragmented and fee-for-service (FFS) U.S. payment system has observable effects on patient care and outcomes. How much payment is rendered and how significantly affect
the volume and nature of primary care services available to a population (Quinn, 2015).
Primary care clinicians work in many organizational contexts, as discussed throughout this report. This chapter briefly touches upon income but does not focus on how clinicians are compensated within their organization or how funds flow from payers through organizations to clinicians; rather, it addresses how their organizations are paid by governments, insurers, and people seeking care. Although compensation plays an important role in individual behavior, the extent and methods of payment from third parties to the organization have more fundamental effects on the extent and nature of primary care in the United States, the focus of the committee’s work. However, how primary care payments flow through organizations to reach and influence primary care delivery, and whether they are aligned with overall intent, remains a critical issue.
For the purposes of this chapter and the committee’s report, the committee assumes that the current multi-payer, largely employment-based system will implement its recommendations. Changes to this assumption would affect the committee’s recommendations significantly but are outside of its scope of work. Please see other work from the Institute of Medicine and the National Academies of Sciences, Engineering, and Medicine for discussions on financing insurance in the United States (IOM, 2004, 2009; NASEM, 2019b).
How Much Payment Is Rendered
How much payment is rendered for a service confers social value. In the United States, primary care physicians (PCPs), while well compensated relative to average overall wages, are poorly compensated relative to their peers in specialty services. The ratio of average annual income for a specialty physician compared to a PCP in the United States was 1.6 in 2003–2004 (Fujisawa and Lafortune, 2008). By 2017, the median compensation in radiology, procedural, and surgical specialties had an almost twofold difference compared with primary care (Doximity, 2019; MedPAC, 2019). While the difference is less, primary care nurses and physician assistants also make less than those in other specialties (AAPA, 2020; Nurse.org, 2020).
As this chapter will describe, this valuation is not derived from market-based negotiations governed by the laws of supply and demand. Rather, it starts with the idiosyncratic process by which Medicare values services, which attempts to account for training, operational costs, and professional risks. This approach, however, places little intrinsic value on promoting health or keeping people healthy. Rather, it is skewed toward procedures, tests, and specialists over relationships, holistic consideration of the individual and their diagnoses, and population health. Usually, the sicker the
patient and the more technical care they receive, the more clinicians are paid. In addition, the U.S. health care system is focused, and paid, on the notion of treating illness rather than on maintaining health. Technology-enabled services oriented primarily to diagnosing and treating advanced disease draw higher prices than reimbursement for clinician time spent with patients and their families.
Money is but one factor affecting clinicians’ decisions, yet payment methods clearly affect whether, how, and how much care they provide (Quinn, 2015). Because they are more likely to provide services with greater returns, relative prices affect use and the mix of services provided. Indeed, when prices change, this has measurable effects on the number and mix of services provided to patients (Clemens and Gottlieb, 2014; Cromwell and Mitchell, 1986; Gruber et al., 1998; Hadley, 2003; Rice, 1983). Examples include hospital length of stay, diagnostic imaging in physician offices, home health care visits, coordination between physicians and hospitals, the volume and mix of services delivered, and which drugs are used for treatment (Bodenheimer, 2008; Coulam and Gaumer, 1991; GAO, 2012; Jacobson et al., 2010; Schlenker et al., 2005; Schroeder and Frist, 2013).
The results of primary care’s devaluation are not surprising. The portion of total health care expenses devoted to primary care in the United States is at or lower than most other countries (Koller and Khullar, 2017; Phillips and Bazemore, 2010), and evidence suggests that it is declining (The Larry A. Green Center and PCC, 2020). One result is that retaining seasoned primary care clinicians has become challenging. Moreover, when faced with the prospect of medical education debt, more limited future financial remuneration, and lower perceived social and professional status, many medical students opt for specialty professions over primary care. The COVID-19 pandemic has further distressed the primary care profession by limiting in-person visits, driving a significant number of practices to close (Basu et al., 2020; Phillips et al., 2020).
A health care system oriented more to primary care would result in a healthier population (Basu et al., 2019) with more consistent access to primary care and potentially a more equitable distribution of health care (Dwyer-Lindgren et al., 2017; Friedberg et al., 2010; Macinko et al., 2007). As recently reiterated by The Commonwealth Fund’s 2020 Task Force on Payment and Delivery System Reform (2020), the nation will only achieve these goals with changes in how and how much primary care is paid (Zabar et al., 2019).
How Payment Is Rendered
How payment is rendered influences the behavior of both clinicians and care-seekers in primary care. Payment methods matter because of the
incentives they create and the actions they reward. The historically dominant method of FFS payment encourages a focus on providing and receiving individual, billable services. Generally, the unit of service and analysis is the short office visit. While FFS is considered to promote access and accountability (Dowd and Laugesen, 2020; Kern et al., 2020), it discourages other team members who may not be able to bill for their services from providing care. It also disincentivizes the primary care team from focusing on non-billable services, outside of a brief office visit, that may have beneficial effects on the health of individuals or a population, such as identifying and educating people with chronic disease (Berenson and Goodson, 2016).
The Spectrum of Physician Payment Models
Theory and evidence show that payment methods have distinctive effects on clinician behavior. Generally, the models fall along a spectrum according to the unit of payment, such as FFS (which pays for each individual service provided) or a bundled payment (which pays for a group of services or a specific period) (see Figure 9-1). On the one hand, concerns about stinting in providing care dominate when clinicians bear financial risk in a bundled payment model, because health care use can be unpredictable. On the other hand, concerns about overtreatment dominate when the financial risk is on payers, such as in FFS, where the insurer pays a given fee for each service. Most research shows empirical results in parallel with theory: FFS encourages use, and capitation—a payment model that provides a fixed amount of money per patient per unit of time paid in advance to the physician for the delivery of health care services, whether or not that patient seeks care and how much it costs—discourages resource consumption; productivity-based pay encourages and capitated payments undermine productivity (Berenson et al., 2020; Hellinger, 1996; Kralewski et al., 2000).
All payment methods have inherent incentives, both good and bad, that cannot be eliminated even with optimal design (Robinson, 2001). Their perverse effects can be attenuated to some extent through design, but even the most sophisticated mechanisms merely diminish the incentives for overtreatment, undertreatment, and other undesirable behaviors. Blended methods, using the best attributes of each, outperform pure FFS and pure capitation in supporting primary care (Berenson et al., 2020; Ellis and McGuire, 1990; Robinson, 2001).
Simplicity is a virtue for several reasons when it comes to designing and implementing payment models. The administrative costs of designing, negotiating, implementing, disbursing, disputing, and adjudicating complex payment methods are high. Simplicity is especially important in the multi-payer U.S. context because adoption of payment models is undermined when physicians face different policies and incentives from multiple
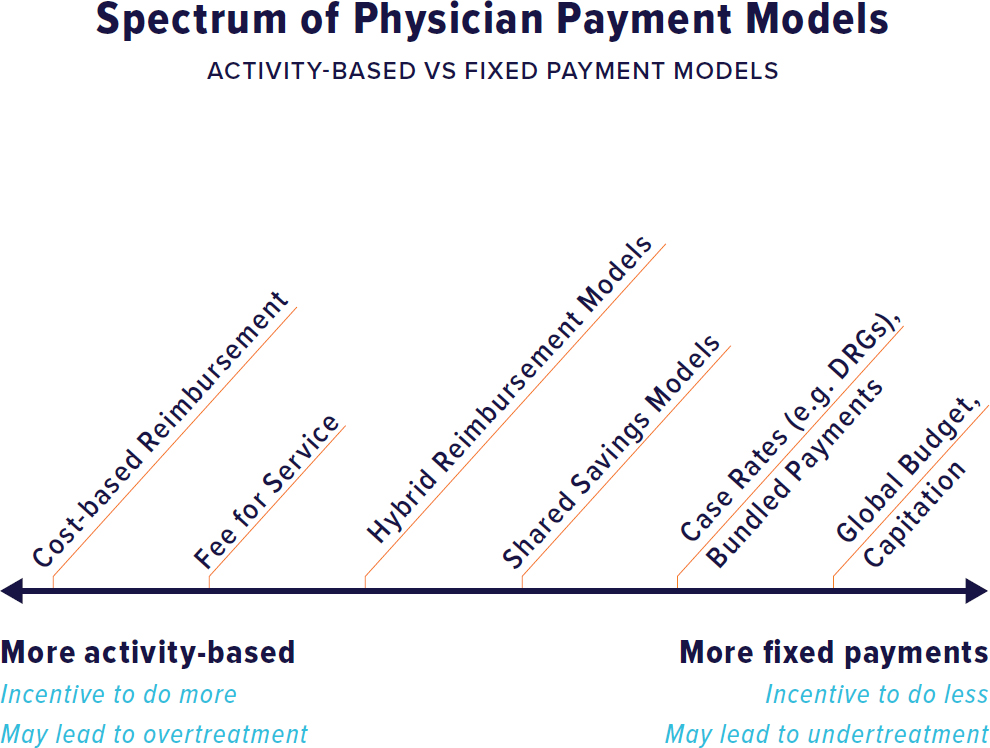
NOTE: DRG = diagnosis-related group.
insurers. Simplicity also supports transparency for all stakeholders, including clinicians, patients, and policy makers.
HISTORY OF PRIMARY CARE PAYMENT
As part of an effort to manage the rising costs of health care and ensure the solvency of Medicare, Congress enacted the Medicare prospective payment system for hospitals in 1983 (Altman, 2012). Instead of paying hospitals for each service delivered, Medicare pays a set fee per stay based on the diagnosis and treatment path. This change incentivized hospitals to reduce length of stay and shift more care to outpatient settings. Although it was not intended to impact primary care, it had many downstream consequences.
In the late 1980s, rising and varied physician-set prices and the widening gap between generalist and specialist incomes led Congress to establish the resource-based relative value scale to set prices for physician services, which account for about 20 percent of Medicare spending (CMS, 2019b). The Physician Fee Schedule (PFS), implemented in 1992, was designed to
be built around a scientific measurement of work and practice expenses (Hsiao et al., 1993), with physician work accounting for around 50 percent of the total relative value unit. Changes to the original measures during the implementation process resulted in a fee redistribution to PCPs about half as large as that projected by the original estimates (Berenson, 1989).
The Patient Protection and Affordable Care Act (ACA),1 passed in 2010, included two provisions to adjust payments to PCPs upward: (a) a 10 percent incentive payment under the Medicare primary care incentive payment (PCIP) for 5 years and (b) raising the Medicaid primary care payment rates up to at least 100 percent of the Medicare rate for 2 years (Davis et al., 2011; Mulcahy et al., 2018). Federal funding for this Medicaid increase expired in 2014, but as of 2016, 19 states had continued this “fee bump” in whole or in part (Zuckerman et al., 2017) and some have called for payment equity between Medicaid and Medicare to be a permanent strategy to improve access and equity for children (Perrin et al., 2020). Not all PCPs were eligible for the PCIP because the criteria were based on meeting a 60 percent threshold of allowed charges for specific ambulatory evaluation and management codes. Some family physicians, particularly in rural areas, perform procedures and provide care in hospitals such that they did not meet the threshold (The Lewin Group, 2015).
The PCIP program had a modestly positive impact on the availability and use of primary care services in Medicare. An early analysis found the almost 75 percent Medicaid rate increase improved primary care appointment availability for enrollees with participating clinicians without generating longer wait times (Polsky et al., 2015; Zuckerman and Goin, 2012). However, a recent analysis concluded the payment increase had no association with PCP participation in Medicaid or on Medicaid service volume (Mulcahy et al., 2020).
Medicare has also added supplemental primary care services to the PFS to improve quality (Berenson et al., 2020).2 An additional focus in the 2019 and 2020 PFS updates was liberalizing payment for a variety of relatively new telehealth codes. Given these codes’ complexity and stringent requirements, uptake has been inconsistent, particularly by small practices (Carlo et al., 2020; Dewar et al., 2020; Reddy et al., 2020). Despite barriers to adoption, including billing and workflow adjustments, uptake is increasing,
___________________
1 Patient Protection and Affordable Care Act, Public Law 111-148 (March 23, 2010).
2 These include covering certification of home health and hospice services, managing care transitions from hospital to the community, managing care for patients with chronic conditions, advance care planning, managing care for patients with cognitive impairment and behavioral health conditions in collaborative arrangements with behavioral health professionals, and providing add-on payments for visits that last at least 31 minutes or prolonged management services conducted before and/or after direct care.
improving value to beneficiaries and the program while increasing revenue to practices (Berenson et al., 2020).
In 2019, the Centers for Medicare & Medicaid Services (CMS) implemented the Merit-Based Incentive Payment System, providing additional payments to organizations participating in alternative payment models and financially rewarding or penalizing clinicians based on quality measures, promoting interoperability, and improvement activities (PAI, 2020). In this zero-sum game, where bonuses for the highest performers come from penalties of lower-performing practices, research has shown that independent practices—those that are not part of a larger system—and safety net practices are more likely to have lower performance and suffer financially (Colla et al., 2020).
PRIMARY CARE PAYMENT TODAY
Financing health care in the United States is complex, with health care organizations receiving revenue from multiple sources: public payers (directly and also indirectly through contracted insurers), commercial insurers, self-insured employers (directly and also through their administrators), and directly from patients. In addition, separate systems exist for veterans and active-duty military families. Oversight authority is divided between private and public payers and between state and federal regulators. This complexity is a contributing factor to the fragmentation of care and why implementing changes to payment models is difficult. In 2017, family physicians reported that their patient panel was 41 percent private insurance, 28 percent Medicare, 18 percent Medicaid, and 7 percent uninsured. Since 2012, notable shifts have taken place in the payer mix for family physicians, with Medicare and Medicaid comprising a greater percentage (AAFP, 2017a). Among pediatricians, that payer mix looks different, at 49 percent Medicaid, 46 percent private insurance, and about 4 percent uninsured (AAP, 2019).
Primary care spending accounted for 6.5 percent of total U.S. health care expenditures in 2002 and 5.4 percent in 2016 (Martin et al., 2020). The proportion was even lower among Medicare FFS beneficiaries, with primary care representing 2.12–4.88 percent of total medical and prescription spending in 2015 (Reid et al., 2019). Medicare Advantage beneficiaries had higher rates of primary care visits and lower costs for these services, but the differences were not substantial (Park et al., 2020). Among commercially insured groups, children had the highest primary care spending as a share of their total health care spending, with 20.33 percent in 2013 and 19.54 percent in 2017, and individuals aged 55–64 years had the lowest, with 7.25 percent in 2013 and 6.33 percent in 2017 (Reiff et al., 2019).
Across payers in 2013, FFS was the dominant method: nearly 95 percent of all physician office visits, with the remaining 5 percent via
capitation. The exact numbers varied by geography and payer (Zuvekas and Cohen, 2016). In 2016, 83.6 percent of practice revenue was FFS, while bundled payments accounted for almost 9 percent, pay-for-performance and capitation made up close to 7 percent, and shared shavings made up only 2 percent (Rama, 2017).
The traditional Medicare program still mainly pays primary care through FFS, with modest adjustments for quality and efficiency (MedPAC, 2020a). A quarter of beneficiaries fall under an alternative payment model (such as an accountable care organization [ACO], described below). In 2019, 34 percent of beneficiaries were enrolled in a Medicare Advantage plan (MedPAC, 2020b), where payment for primary care services varies by plan but is generally FFS and anchored to the Medicare fee schedule (Trish et al., 2017). About 10 percent of beneficiaries in Medicare Advantage are in a plan that passes on global financial risk to clinician teams (Galewitz, 2018).
In Medicaid, states have broad flexibility to determine payments for physician services. While 81 percent of enrollees are in managed care plans, the majority of Medicaid spending occurs under direct state FFS arrangements (MACPAC, 2020). Medicaid physician fees are well below that of fees for Medicare and private payers: only roughly 54 percent of Medicare rates for primary care services (MACPAC, 2013). These lower rates are thought to negatively impact physician participation in Medicaid (Cunningham and May, 2006; Decker, 2012; Holgash and Heberlein, 2019).
State Medicaid programs use different types of managed care arrangements: comprehensive risk-based managed care (35 states), primary care case management (7 states), or a combination of the two (5 states). Some states carve out specific services from their managed care arrangements such as oral health, institutional care, or transportation (Hinton et al., 2019; MACPAC, 2011). Sixty-nine percent of Medicaid enrollees in 2018 received their benefits though a comprehensive risk-based arrangement (KFF, 2020). In primary care case management, enrollees have a designated primary care team paid a monthly case management fee to assume responsibility for care management and coordination. Individual clinicians are not at financial risk; they continue to be paid on an FFS basis for providing covered services. In some cases, financial incentives for both primary care teams and the care management entity are added.
In risk-based arrangements, Medicaid managed care organizations (MCOs) are paid a capitation rate that is calculated based on the state’s FFS rates. The MCO, in turn, contracts with health care organizations through a series of privately negotiated, proprietary arrangements. The MCO is responsible for assembling a network of clinicians that meets state access requirements based on minimum standards set by CMS, which also maintains separate network access standards for Medicaid FFS programs.
The access standards for Medicaid MCOs were promulgated by CMS under its Medicaid Managed Care Rule in 2016, but none are specific to primary care. Prior to the 2016 rule, inadequate enforcement of Medicaid access policies was the source of dozens of suits against states (Rosenbaum, 2009, 2020). In 2020, CMS eliminated an access standard for the time and distance traveled to access a clinician, only requiring states to set a quantitative minimum access standard, such as minimum clinician-to-enrollee ratios; a minimum percentage of contracted clinicians that are accepting new patients; maximum wait times for an appointment; or hours of operation requirements (BPC, 2020; CMS, 2020e).
More than half of managed care states (21 of 40) set a target percentage in their contracts for the percentage of payments, network clinicians, or plan members that must be paid via alternative payment models in fiscal year 2019 (Hinton et al., 2019). Most plans use FFS with incentives or bonus payments tied to performance measures. Fewer plans reported using bundled or episode-based payments or shared savings and risk arrangements.
Commercial health insurance consists of employer-sponsored coverage and individual insurance. Insurers and administrators assemble provider networks through proprietary confidential contracts. Analysis of multiple sources indicates that commercial insurers pay on average 143 percent of Medicare rates for physician services, with considerable variation by specialty type (Lopez et al., 2020). Codes most frequently billed by PCPs were paid at 107 percent of Medicare (Trish et al., 2017). This disparity in payments relative to Medicare likely reflects greater negotiating leverage for specialty physicians. More than half of commercial contract payments use FFS without any quality or performance bonuses (HCPLAN, 2019).
Findings for Primary Care Today
- Primary care makes up a small and declining proportion of medical spending.
- FFS is the dominant payment mechanism for primary care clinicians.
- Compared to Medicare, Medicaid pays substantially less for primary care services and commercial insurers slightly more.
- Medicaid determines payment sufficiency through the ability of states and managed care contractors to maintain adequate networks of clinicians. Federal oversight of these standards is not specific to primary care, and, while they were already inadequate, they have recently been further relaxed.
- Commercial insurers pay specialty physicians more relative to Medicare than they pay PCPs.
REFORMING PAYMENT TO PRIMARY CARE
In this section, the committee presents a spectrum of options for improving payment for primary care to better meet people’s needs. These options are not mutually exclusive, and it will likely be necessary to employ multiple levers to produce the changes necessary to support primary care.
- Option 1 builds incrementally on the existing PFS to value primary care services more accurately.
- Option 2 discusses overarching models to blend FFS and fixed payments.
- Option 3 discusses global payment models for practices prepared to take on further financial risk.
- Option 4 discusses creating a societal goal for the proportion of health care spending that goes to primary care.
Option 1: The Medicare Physician Fee Schedule and the Relative Value Scale Update Committee
While Medicare accounts for 20 percent of national health spending (KFF, 2019), the relative prices set by the PFS have a profound effect on professional prices beyond Medicare beneficiaries. Three-quarters of the services physicians billed to commercial insurers are pegged to Medicare’s relative prices (Clemens et al., 2015), and TRICARE, the health care program for uniformed service members, also uses the Medicare PFS. Many state Medicaid and state workers compensation programs use the Medicare rates as a benchmark. In addition, many alternative payment models are based on spending projections that use the PFS, and payers use shadow prices from the PFS to calculate capitation rates.
The Role of the Relative Value Scale Update Committee (RUC)
Shortly after CMS implemented the Medicare PFS, the American Medical Association created the RUC and offered the committee’s expertise to the Health Care Financing Administration, CMS’s predecessor. The RUC selects physician procedures for review and determines the value of services relative to other physician services for three categories of activity: physician work, practice expense, and malpractice risk. The RUC passes the resulting numerical assessments on to CMS, which can accept or modify recommendations and then convert them into an entry on the PFS using a geographic adjustment and inflation multiplier. Historically, CMS has deferred to nearly all the RUC’s recommendations, accepting them unaltered 87.4 percent of
the time between 1994 and 2010. On average, RUC-recommended work values were higher than final CMS values (Laugesen et al., 2012).
Today, the RUC comprises 31 physicians and 300 advisors representing medical specialties. Primary care has one rotating seat and three seats appointed by the American Academy of Family Physicians (AAFP), the American College of Physicians (representing internal medicine), and the American Academy of Pediatrics. Two seats also rotate between internal medicine subspecialties. Of the 31 physician seats, only one each is dedicated to child health and geriatrics (AMA, 2016).
There are reasons to question the accuracy and independence of the RUC process, including documented voting alliances in the RUC among proceduralists that often distort the equitable allocation of valuing work (Laugesen, 2016). Researchers working with CMS and the Assistant Secretary for Planning and Evaluation have gathered evidence that the PFS’s time estimates for clinician work are inflated (MedPAC, 2018b; Merrell et al., 2014; Zuckerman et al., 2016), suggesting a bigger gap between estimated and actual times for surgical and procedural services than office visits, especially those occurring in primary care (McCall et al., 2006; MedPAC, 2018b). The available evidence suggests that surgical services are overvalued, while primary care visits and services are largely undervalued (CMS, 2019a; Reid et al., 2019).
Inaccuracies in relative pricing along with CMS acceptance of most RUC recommendations have contributed to the differences in compensation across specialties, the distribution of physicians across specialties, inefficient distortions in use, and inadequate beneficiary access to undervalued services, as described above (MedPAC, 2018b; Nicholson and Souleles, 2001). These deficiencies in the RUC process compound over time because changes to Medicare’s fee schedule must be budget neutral. As a result, primary care services generally, and evaluation and management codes specifically, have become passively devalued in the PFS as their relative prices fall as a result of other service prices (including new technologies) increasing. A variety of factors interplay to cause this devaluation:
- For procedure-based services, work time often falls as physicians become familiar with the service and technology improves. However, work relative value units (RVUs) for these services often are not re-evaluated (MedPAC, 2006). Evaluation and management services consist largely of activities that require specified clinician time.
- Requests for new codes or refinement are initiated by specialty societies, and refinement generally results in increases (Laugesen, 2016). New technologies and methods of diagnosis and treatment
- can create pathways to higher relative values, compared to visits, which have few new technologies (Zuckerman et al., 2015).
- Procedural, task-driven work may lend itself more easily to judgments of physician work units, which are composites of time, mental effort, judgment, technical skill, physical effort, and psychological stress. Measurement may be harder in evaluation and management services with a broad range of clinical issues, less defined temporal sequences, and a more nonlinear workflow, as found in the management of chronic conditions in primary care (Katz and Melmed, 2016; Laugesen, 2016). Furthermore, primary care has involved increasing complexity over time, at the level of different organ systems, individual factors, societal variables, and population dynamics. It is difficult to measure the continuity, comprehensiveness, coordination, trust, personal connection, and personal accessibility necessary to provide high-quality primary care (Shi, 2012).
- Under budget neutrality, an increase in units for the large number of evaluation and management visits would mean relative prices fall for everything else, making the RUC less likely to recommend these changes. Most evaluation and management codes are passed in the RUC below the 25th percentile of the range of clinician responses regarding work time, whereas procedures typically end up between the 25th and 50th percentile of survey responses (Laugesen, 2016).
- Documented voting alliances in the RUC among proceduralists often distort the equitable allocation of valuing work (Laugesen, 2016).
Thus, because the fee schedule is budget neutral and the phenomena described above are routine, primary care services have become passively devalued. For example, the total RVUs for a Level III office or outpatient visit for an established patient (HCPCS 99213), the most frequently billed office or outpatient visit, declined slightly from 2.14 in 2013 to 2.06 in 2018 (MedPAC, 2018b). This devaluation is reflected in a widening gap in pay between primary care and specialists. Data from the Medical Group Management Association indicate that from 1995 to 2004, the median income for PCPs increased by 21.4 percent, while that for specialists increased by 37.5 percent (Bodenheimer, 2006). In 2017, median compensation for nonsurgical, procedural specialists, surgical specialties, and primary care was $426,000, $420,000, and $242,000 (MedPAC, 2019), respectively. This compensation gap is associated with reduction in medical student choice of primary care careers and with shifting hospital graduate medical
education priorities away from primary care (COGME, 2010; Phillips et al., 2009; Weida et al., 2010).
Recent Reforms
Several effective steps have been taken in the last decade, including revising misvalued codes, temporarily increasing the primary care fee, and adding new primary care codes. Nonetheless, the definition and conceptualization of physician work inherent in the PFS do not support the committee’s conceptualization of high-quality primary care.
For the last decade, CMS and the RUC have identified and reviewed “potentially misvalued services,” including codes associated with fast use growth or services that have not been reviewed since the PFS was implemented. The Protecting Access to Medicare Act of 20143 and Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 20154 provided CMS with new powers to change misvalued codes and collect data to evaluate the PFS. The law expanded the number of codes that would potentially be evaluated, creating a new target for relative value adjustments, with a savings target of 0.5 percent of expenditure every year between 2017 and 2020 (Laugesen, 2016). A recent survey of the RUC process resulted in a major upward revision in the 2021 Medicare PFS for fees for office visits (CMS, 2020d). CMS endorsed the RUC recommendation for the two most commonly billed office visit codes: a 34 percent increase for code 99213 and a 28 percent increase for 99214.
CMS remains limited, however, by the lack of current, accurate, and objective data on clinician work time and practice expenses (GAO, 2015; Mulcahy et al., 2020; Wynn et al., 2015; Zuckerman et al., 2016). As a result, CMS continues to depend on a RUC process that has drifted away from science-based estimates toward interest group input. This drift is facilitated because complexity and lack of transparency effectively mask payment policy. The complexity of the PFS and its determinants, paired with the lack of resources at CMS, has led to a situation where physician societies have informational advantages and leverage them to achieve higher valuations (Laugesen, 2016; McCarty, 2013; Shapiro, 2008).
CMS and other policy makers have little recourse to change the RUC structure or processes. As a private organization, the RUC has an important voice in the policy process and substantial autonomy to determine how it chooses its valuation practices. Many have noted that without more oversight or coordination of a fair arbitration process, the relative value scale
___________________
3 Protecting Access to Medicare Act of 2014, Public Law 113-93 (April 1, 2014).
4 Medicare Access and CHIP Reauthorization Act of 2015, Public Law 114-10 (April 16, 2015).
was bound to be biased toward specialty care (Berenson and Goodson, 2016; Laugesen et al., 2012).
However, the committee sees no regulatory or institutional barrier to CMS establishing its own parallel capacity to independently value physician services that aligns better with its stated organizational goals to move toward value-based, accountable payment and away from the misvalued PFS. In fact, it is hard to imagine that it could do so in the absence of an independent valuing mechanism within or external to the agency, such as the Medicare Payment Advisory Commission (MedPAC).5 Establishing such a capacity will require allocating a relatively modest level of resources and staff and would not prevent the RUC from continuing to make its recommendations to CMS and other entities. However, by having an additional resource to evaluate and compare its own estimates with that of the RUC and others, CMS would be able to more adequately and fairly price primary care services in a way that accounts for their complexity and value to patients and society.
Altering the Fee Schedule to Accomplish Policy Objectives
Direct changes to relative prices could include a payment increase for ambulatory evaluation and management services, such as the change implemented in January 2021, or freezing rates for these services while reducing others. In 2015, MedPAC recommended establishing per-beneficiary payments for primary care clinicians to encourage care coordination, including the non-face-to-face activities that are a critical component of care coordination. MedPAC recommended setting the per-beneficiary payment at 10 percent of primary care spending, which at that time would have meant an annual payment of $28 per patient with no beneficiary cost sharing. To be budget neutral, this funding level would have required reducing fees for non–primary care services in the PFS by 1.4 percent (MedPAC, 2015). A hybrid reimbursement approach such as this is discussed more below.
In its June 2018 report, MedPAC modeled a 10 percent payment rate increase for evaluation and management services. In 2019, a 10 percent increase would have raised annual spending for ambulatory evaluation and management services by $2.4 billion. To maintain budget neutrality, payment rates for all other PFS services would be reduced by 3.8 percent (MedPAC, 2018b). Other options to offset a payment increase for ambulatory evaluation and management codes include automatic reductions to
___________________
5 MedPAC is a non-partisan legislative branch agency that provides the U.S. Congress with analysis and policy advice on the Medicare program. Additional information is available at www.medpac.gov (accessed February 27, 2021).
prices of new services after their introduction or automatic reductions in services with high growth rates (MedPAC, 2018b).
In summary, the Medicare PFS is not well designed to support primary care. It is oriented toward discrete, often procedural, technical services with defined beginnings and ends, the antithesis of high-quality continuous primary care. Some have gone so far as to say that the RUC and the PFS have led to more procedures, the recruitment of more physicians into the procedure-oriented specialties, the underrepresentation of primary care in the workforce, the under-provision of primary care, and the consolidation of primary care practices into larger delivery systems (Berenson and Goodson, 2016; Calsyn and Twomey, 2018; Laugesen, 2016).
Findings for Option 1
- The relative prices set by the Medicare PFS have profound effects on prices paid by Medicaid, commercial payers, and others. The RUC exerts significant influence on the relative prices assigned by CMS.
- The RUC, together with the structure of the PFS, have resulted in systematically devaluing primary care services relative to other services and its population health benefit, reflected in large and widening gaps between primary care and specialty compensation.
- The widening compensation gap between primary care and other physician specialties is associated with reductions in medical trainees’ likelihood of choosing primary care careers and with hospitals’ graduate medical education training priorities.
- With adequate resources and leadership, CMS has the authority to address these weaknesses and internalize the functions of the RUC (data collection and valuation tools) to generate payment levels aligned with high-quality primary care.
Option 2: Hybrid Reimbursement Models
A second option for increasing and reforming payment to primary care is to mix FFS payment mechanisms with lump-sum or per-person payments to encourage team-based, technology-enabled advanced primary care.
Patient-Centered Medical Home Model
Over the past 15 years, implementation of advanced primary care in the United States has focused largely on the hybrid patient-centered medical home (PCMH) model. Early PCMH models showed promising results in
terms of reducing spending and avoidable use, especially among the chronically ill (Maeng et al., 2016).
Commercial payers began to sponsor limited tests of these models within their care networks, usually with small care management fees on top of FFS. By 2010, these tests encompassed more than 14,000 physicians in 18 states caring for almost 5 million patients (Bitton et al., 2010), but they were hampered by the low levels of care management fees, often under $5 per patient per month, and a lack of multi-payer participation. The early results of studies on PCMH effects on total spending were mixed (Jackson et al., 2013; Sinaiko et al., 2017). These evaluations rarely factored the cost of practice transformation or the provision of care management fees into the analysis.
As the PCMH model spread, payers provided more substantial care management fees, multi-payer participation increased somewhat, and payer-initiated PCMH models began to include shared savings incentives (Edwards et al., 2014). The total amount of money, and transformation resources in the form of facilitation, generally increased. Nonetheless, FFS continued to be the mainstay of payment, and robust multi-payer involvement was the exception, not the norm. The cost effects of these PCMH initiatives continued to be mixed, though quality and patient experience were more often improved (Jackson et al., 2013; Kern et al., 2016; Lebrun-Harris et al., 2013; Sinaiko et al., 2017).
However, more recent research on PCMH outcomes from nearly 6,000 practices in 14 states found reductions in total expenditures of more than 8 percent after up to 9 years of implementation, as well as significant decreases in emergency department utilization and outpatient care (Saynisch et al., 2021). Emergency department reductions were highest among practices that offered electronic access, suggesting that the choice of adopted capabilities is important.
The PCMH model has also been implemented for pediatric populations. Integrated Care for Kids, a child- and family-centered integrated delivery care model, is one example with a matched state payment model for children insured by Medicaid or CHIP (see Chapter 5 for more detail).
Comprehensive Primary Care Model
To test a multi-payer approach to primary care transformation at scale, the Center for Medicare & Medicaid Innovation (CMMI) launched the Comprehensive Primary Care (CPC) model as a 4-year, multi-payer demonstration in 2012. CPC provided population-based care management fees and shared savings opportunities, on top of standard FFS, to nearly 500 participating primary care practices in seven regions as a means of supporting the provision of a core set of five “comprehensive” primary
care functions (CMS, 2020a). Regions were selected based on the ability of their payer partners to provide participating practices with at least 60 percent of combined revenue. CPC showed mixed results on the cost and quality outcomes assessed in its evaluation. The growth rate in overall FFS expenditures was reduced for attributed beneficiaries, though the decrease was not enough to offset the care management fees (Peikes et al., 2018). In addition, those fees were not sufficient to enable upfront and long-term investments in staff. Though practice quality improvements as measured through claims were modest, an analysis of electronic clinical quality measures (used by practices themselves to measure improvement) showed significant gains compared to benchmarks established during the initiative (LaBonte et al., 2019).
Comprehensive Primary Care Plus Program
CPC was a precursor to the CPC+ program launched in 2017. CPC+ is a national multi-payer advanced primary care model that aims to strengthen primary care through regionally based, multi-payer payment reform and care delivery transformation (Burton et al., 2017). It is active in 18 regions, with more than 50 payers and more than 3,000 participating practices serving more than 3 million Medicare beneficiaries and an estimated 15 million people overall (CMS, 2020b). CPC+ includes two practice tracks with incrementally advanced care delivery requirements and payment options and has three major payment elements: (1) a risk-adjusted care management fee per beneficiary that is paid quarterly and not visit based; (2) performance-based incentives paid prospectively with retrospective reconciliation, with performance measures that include patient experience, clinical quality, and use; and (3) payment under the PFS. In Track 1, PFS payment continues as usual along with the care management fees and performance-based payments, but in Track 2, PFS payments are reduced and shifted into a CPC payment.
CPC+’s first evaluation6 focused on Medicare FFS enrollees in 2,905 practices that started CPC+ in 2017. The median care management fees per practitioner in the first year equaled $32,000 in Track 1 and $53,000 in Track 2, with CMS providing the most fees relative to other participating payers. Other payers were slower to adopt the reduced PFS payments and partially capitated payments in Track 2. In the first year, 71 percent of Track 2 practices opted for the lowest FFS reduction of 10 percent in exchange for capitated payments; only 16 percent of CPC+ Track 2 practices,
___________________
6 This reflects available evaluations at the time of writing. The reader should refer to https://innovation.cms.gov/innovation-models/comprehensive-primary-care-plus (accessed February 27, 2021) for updated evaluations.
or roughly 8 percent of all participants, opted for a 40 or 65 percent reduction in FFS in exchange for larger capitated payments. As expected, CPC+ in its first year had small effects on quality of care and health care spending, and the care management investments were larger than any cost savings.
Despite the investments in care management, data feedback, and learning support, participating practices also expressed challenges implementing care delivery requirements, though system-owned practices and those with a robust health information technology infrastructure found it easier to identify the resources for practice transformation and manage reporting requirements. Commercial insurer participation in the CPC+ model has persisted, indicating they perceive value in the model. There are also non-peer-reviewed analyses of multi-payer projects in Arkansas, Ohio, and Oregon that show more promising performance for commercially insured people and improvements over time (Bianco et al., 2020; Brown and Tilford, 2020; Dulsky Watkins, 2019).
Challenges to Implementing Hybrid Reimbursement Models
Most PCMH-like primary care transformation efforts implemented by individual payers have used hybrid payment methods largely based on FFS and struggled to provide the financial resources to cover transformation costs or the ongoing cost of maintaining integrated team-based care. Some commercial payers, such as the Capital District Physicians’ Health Plan (CDPHP) in New York and the Hawaii Medical Service Association, have moved further to structure payments for primary care practices around a risk-adjusted primary care capitation model. An evaluation of the CDPHP model showed some pharmacy cost savings and use declines in people with chronic conditions but no overall cost savings (Salzberg et al., 2017). An initial assessment of the Hawaii program found improvements in quality but did not assess cost or use changes (Navathe et al., 2019).
As with payer-specific hybrid payment models, it was likely difficult for practices to change their overall structure when one payer offered risk-adjusted capitation for 10 to 20 percent of patients but FFS contracts constituted the rest. With the advent of large multi-payer initiatives, such as CPC+, this dynamic is changing, as payers in some regions are starting to increase available capital to practices and change payment for a plurality, if not majority, of patients in a practice. Nonetheless, most U.S. primary care practices, even those involved in PCMH efforts, are not paid substantially extra for these efforts.
Poorly funded incremental PCMH efforts across practices have diluted the effects of the limited capital invested in them, and until recently, this capital has not been explicitly tied to reductions in total cost of care. The majority of payer-initiated PCMH and advanced primary
care demonstrations have shown mixed or no effects on total cost. The lack of spending reductions has limited further investment in augmented PCMH or advanced primary care models, whose high ongoing staff and transformation costs are well documented. Without a substantial source of new, predictable, and sustainable revenue from multiple payers to maintain and expand new services, practices find it difficult to maintain focus on overlapping practice transformation aims, including quality improvement, team formation, chronic care coordination, and patient engagement. Thus, minimal investments, initiative overlap, and an underlying focus on visit volume impede the ability to focus on reducing total spending, which is difficult when primary care practices drive small fractions of spending themselves and have incomplete control over where and when their patients utilize care.
Nonetheless, the literature on impact of payment reform on total spending remains mixed and may depend on organizational and patient characteristics (Veet et al., 2020). For example, some integrated delivery systems have improved outcomes, and low-income patients have improved clinical outcomes (van den Berk-Clark et al., 2018). Many payer-reported efforts have suggested savings (Jabbarpour et al., 2017), but most peer-reviewed published analyses have been more widely divergent or null in their findings (Jackson et al., 2013; Sinaiko et al., 2017). One study with a 6-year observation period and another that took place after up to 9 years of implementation both found significant savings (Maeng et al., 2016; Saynisch et al., 2021). A key area of overlapping conclusion is that potential savings are concentrated in patients with multiple comorbidities and chronic conditions, where regression to the mean is possible.
This imperative to demonstrate short-term health care cost savings serves as a key challenge to child health–focused primary care models, as high-cost pediatric patients make up a much smaller proportion of the population. For example, just 5 percent of children account for about 50 percent of Medicaid spending for children (Berry et al., 2014). Most often, health care savings realized by primary care transformation may result as children and adolescents age into healthier young adults, with healthier behaviors (e.g., lower smoking rates, higher immunization rates) and fewer chronic illnesses (less obesity, lower rates of depression). Savings may also be realized outside of health care, in education (greater graduation rates, less need for special education services) (Zimmerman and Woolf, 2014), the workforce, and the criminal justice system (Wen et al., 2014). These, of course, are not costs that are considered in time-limited evaluations of primary care transformation. Thus, a recent review of child-focused ACOs concluded that the area of child health requires specific payment models to account for these issues (Perrin et al., 2017).
Ten years of experience with CMMI hybrid reimbursement models has generated some key lessons for future primary care model development (Peikes et al., 2020):
- Though participating practices valued the care delivery innovations, they often struggled to find the time or resources necessary to fully implement desired changes, even with multi-payer models.
- Busy primary care clinicians need education about what they are required to implement and why. They also require simplified and harmonized reporting requirements across payers to reduce administrative burden on practices.
- Practices need some flexibility from payers to adapt payment models to their circumstances.
- Involving an extended care team other than those in primary care can enhance model impact.
- The redesign of care can take time to yield impact.
Layering care management fees and shared savings on a largely unchanged chassis of FFS does not drive robust and focused practice change to reduce expensive specialty and hospital-based use; practices largely continue to operate within the confines of FFS, visit-based mentality (Bitton et al., 2012). Alternative payment models need to have stronger incentives to counter FFS, and multi-payer participation with more substantial shifts away from FFS toward risk-based contracting can help achieve this (Burton et al., 2018; Martin et al., 2020). However, many practices may not be immediately able to take on complex risk. Payments need to be clearly defined, relatively simple, and transparent. Data and feedback on performance are necessary, but they must be salient and actionable, and training on using data effectively may be necessary for model participants.
Particularly in the wake of the COVID-19 pandemic, attention has focused on another advantage to partially capitated models: they ensure a steady and predictable cash flow in times of severe service disruption (Phillips et al., 2020). To the extent that the declines of pandemic-induced visit volumes remain, greater implementation of hybrid payment arrangements would forestall the closure of primary care practices or their absorption into larger, more expensive health systems with no corresponding improvement in service value.
Findings for Option 2
- FFS models discourage successful engagement of primary care practices in structure and process improvements.
- Hybrid payment models in support of advanced primary care mitigate FFS incentives for increased use and provide resources for team-based care and non-PFS services, though this produces modest to no reductions in spending and use in the short term.
- With adequate time, hybrid reimbursement models show improvements in care and reductions in use, particularly for people with multiple complex chronic conditions.
- The likelihood of practice improvement increases in markets where one payer has a large market share or when multiple payers align.
Option 3: Broad Risk-Sharing Models
The types of organizations delivering primary care vary greatly, as discussed throughout this report. In 2018, health systems employed nearly half of primary care clinicians, and this number continues to grow (Abelson, 2019), with potential acceleration from the COVID-19 pandemic. In health care systems, primary care clinicians are often employees and operate under contracts established by the system at large. In those instances, where health care organizations have greater capability and often experience with financial risk, they can assume accountability for overall use and spending. Referred to collectively as “risk sharing”—where risk is the probability of the assigned population using medical services—practices can assume risk accountability in their own contracts, form new entities to participate in risk-sharing models, or participate as part of a larger medical group or integrated delivery system.
Accountable Care Organizations
ACOs are groups of clinicians participating in capitated or shared-risk contracts paired with incentives for quality performance. CMS manages several ACO programs7 that have implications for primary care payment, and many commercial payers have ACO programs as well (Peiris et al., 2016). In 2019, there were 1,588 existing public and private ACO contracts covering almost 44 million lives (Muhlestein et al., 2019). When an ACO succeeds in both delivering high-quality care and spending health care dollars more wisely, it will share the savings. Some ACO contracts also include shared risk if spending exceeds targets (Peck et al., 2019). Under an ACO
___________________
7 CMS and CMMI manage multiple types of ACOs, including the Medicare Shared Savings Program, the ACO Investment Model, and the Advance Payment Model for qualifying Medicare Shared Savings Program ACOs; the Comprehensive ESRD Care Initiative for beneficiaries receiving dialysis services; the Next Generation ACO Model for ACOs experienced in managing care for populations of patients; the Pioneer ACO Model (no longer active); and the Vermont All-Payer ACO Model.
contract, payments to clinicians typically continue on an FFS basis, and the ACO assumes the performance risk and associated incentives. Primary care is a central component of ACOs, and organizations differ in the extent to which they emphasize, incorporate, pay for, and support it.
In general, research on the impact of ACOs shows modest savings in total spending alongside quality and patient satisfaction improvements. Research has demonstrated that ACOs with a higher share of PCMH practices (Jabbarpour et al., 2018) and a greater proportion of PCPs perform better on cost and quality outcomes (Albright et al., 2016; Ouayogodé et al., 2017). Similarly, physician-led ACOs, compared to hospital-integrated ACOs, produce greater savings (Bleser et al., 2018; McWilliams et al., 2018). Medicaid ACO arrangements now exist in 14 states, showing mixed results (CHCS, 2017; McConnell et al., 2017; NAACOS, 2020). The Alternative Quality Contract, BlueCross BlueShield’s Medicaid ACO program in Massachusetts, has shown consistent improvement in quality and savings (Song et al., 2019), while the same commercial ACO program showed little effect in care quality or spending in children (Chien et al., 2014). However, Partners for Kids, a pediatric ACO in Ohio taking full risk for Medicaid enrollees, demonstrated a lower rate of cost growth without reduced quality measures or outcomes (Kelleher et al., 2015). Minnesota’s Medicaid ACO also showed promising results in the pediatric population (Christensen and Payne, 2016). ACO programs also show some evidence of reducing disparities (McConnell et al., 2018; Song et al., 2017).
ACOs have different structures for distributing performance-based payments across participants that can affect compensation of PCPs (Siddiqui and Berkowitz, 2014). ACO-affiliated practices are more likely than unaffiliated practices to use performance improvement strategies, such as feedback of quality data to clinicians, yet performance measures contribute little to physician compensation (Peiris et al., 2016; Rosenthal et al., 2019).
Primary Care Contracting
In response to the piecemeal efforts and heterogeneous results of hybrid payment models, recent Medicare payment reform efforts focus less on streamlining primary care transformation and more on total cost-of-care reductions. In 2019, CMMI announced several new risk-sharing models that will begin in 2021. Primary Care First combines capitated and reduced FFS payments, with greater potential for shared savings and expansion to a larger number of geographic regions (CMS, 2020f). The payments include performance-based incentives that use regional and historical benchmarks for spending, quality, and hospital use (CMS, 2020g). The capitated payment was calibrated to constitute about 60 percent of primary care payments.
CMMI also announced it would enable direct contracting models, which are capitated or partially capitated models that are broad in scope and touch on primary care in several ways (CMS, 2020c). The program has two voluntary risk-based payment arrangements. The professional option offers organizations capitated, risk-adjusted monthly payment for a defined set of enhanced primary care services. The global option provides the highest risk-sharing arrangements in exchange for capitated, risk-adjusted monthly payments for all services provided by a direct contracting entity and its preferred providers.
Direct primary care models typically work by charging patients a monthly, quarterly, or annual fee to cover all or most services, including preventive care, basic illness treatment for acute and chronic conditions, clinical and laboratory services, consultative services, care coordination, and comprehensive care management (AAFP, 2020; Doherty et al., 2015). Many direct primary care practices also arrange access to other discounted services, such as prescription drugs, laboratory tests, and imaging (Busch et al., 2020).
Patients from all segments of the health insurance market—commercially insured, uninsured, and beneficiaries of Medicare, Medicare Advantage, and Medicaid—can be direct primary care members. Additionally, employers can offer a direct primary care option through their self-insured group health benefit plans, where they cover the fees. As a result of the relative newness of direct primary care, the literature assessing outcomes is small. In addition, studies are plagued by the difficulty of adjusting for the selection of healthy patients into these practices. One recent study found that after adjusting for differences in health status, a matched employer-based direct primary care cohort experienced a statistically significant reduction in total claim costs relative to the traditional cohort during the same period, meaning that enrollment in direct primary care was associated with reduced overall demand for health services. Direct primary care has similarities to concierge care, but key differentiators are direct primary care practices have lower membership fees and do not bill third parties on an FFS basis (Busch et al., 2020).
Finally, other primary care payment models have been proposed but not broadly tested, such as the Comprehensive Primary Care Payment Calculator (George et al., 2019), AAFP’s Advanced Primary Care Model (AAFP, 2017b), an Innovative Model for Primary Care Office Payment (Antonucci, 2018), and the Comprehensive Care Physician Payment Model (Meltzer, 2018; Tingley, 2018).
Findings for Option 3
- With almost half of primary care clinicians employed in health systems, attention should be paid to primary care payment methods in those settings. Many ACOs continue to pay primary care internally based on FFS, even though the larger organization may participate in risk-sharing models.
- ACOs have demonstrated modest savings in total spending alongside quality and patient satisfaction improvements. ACOs that are predominately primary care, PCMH based, or physician led achieve better performance than other ACOs. Some evidence indicates that pediatric-focused ACO models are effective for pediatric populations.
- Medicare is developing models to engage primary care practices more directly in managing the cost and quality of their care. These broad risk-sharing models have yet to be implemented.
Option 4: Increase the Allocation of Spending to Primary Care
The poor performance of the United States in many areas of population health has in part been attributed to a lack of “primary care orientation” of the country’s health system (Friedberg et al., 2010). Clear evidence suggests that systems oriented toward primary care in both policy and relative resource allocation show improved population outcomes and better efficiency over time (Bitton et al., 2017; Shi, 2012). One way to measure primary care orientation is simple: the portion of total health care expenses spent on primary care services. Although comparisons are difficult, it appears the United States spends a smaller (Koller and Khullar, 2017; PCC, 2018) to similar proportion (Berenson et al., 2020) of total expenses compared to other Organisation for Economic Co-operation and Development (OECD) countries, depending on the definition (OECD, 2018). In 2016, the year for which the most recent comparable data are available, the United States spent approximately 5.4 percent of total health expenditure on primary care, compared with an average among 22 OECD countries of 7.8 percent (OECD, 2019). Within the United States, higher state-level proportions of health care spending devoted to primary care are associated with fewer emergency department visits, total hospitalizations, and hospitalizations for ambulatory care–sensitive conditions (Jabbarpour et al., 2019). Given this, a fourth option for influencing the flow of funds to primary care teams focuses on a desired policy priority of increasing the share of health care spending devoted to primary care. To achieve this priority, policy makers would direct third-party payers to increase the proportion devoted to primary care and hold them accountable to achieving it.
This strategy was first developed in Rhode Island for commercial insurers as part of a set of Affordability Standards promulgated by the Office of the Health Insurance Commissioner (Koller et al., 2010). The original iteration of the Affordability Standards called on commercial insurers to raise their “primary care spend figure” by 1 percentage point per year for 5 consecutive years without adding to overall premiums. It also required the increased spending not be accomplished through FFS increases and authorized specific uses as qualifying, notably a statewide health information exchange. Oregon has now followed Rhode Island’s lead, and at least six other states have passed laws for public measurement and sometimes set targets for insurers (Jabbarpour et al., 2019). For example, Delaware, at the end of 2020, released a report through its Department of Insurance developing affordability standards for health insurance premiums and setting targets for insurance carrier investment (Delaware DOI, 2020).
Achieving the goal of implementing high-quality primary care through a strategy of regulating the proportion of spend devoted to primary care offers several advantages. It increases available funds, a key constraint to implementing high-quality primary care, and though the portion to be reallocated is a relatively small amount of total health care expenses, it would have large marginal effects in the primary care sector. It also addresses the failure of private health plan negotiations or Medicare to recognize the collective social value of primary care. In addition, this approach is relatively simple to understand and focuses public prioritization of primary care and the social benefits it delivers (Bolnick et al., 2020).
However, operational and policy challenges to such a strategy remain:
- Defining the policy goal: Target additional resources toward all primary care or specifically the desired elements of it? Are all means of distribution of equal merit? For example, Rhode Island specifically directed that the increase not be in FFS rates.
- What constitutes an acceptable rate of spend? Current spend differs by payer type because of population characteristics—an older and sicker population, such as with Medicare, consumes a greater share of health care resources on acute care, while a younger, healthier child population consumes considerably smaller levels of resources, with a resulting much greater share to primary care (AHRQ, 2020; Rui and Okeyode, 2016).
- Administering the measure requires a standard, administrable definition of primary care, and oversight and enforcement mechanisms.
- Is the state willing and able to coordinate its policy levers? Rhode Island’s work was for commercially insured populations only and did not extend to Medicaid or its public employees.
- The strategy is inherently redistributive, and while the amounts may be small, this strategy will generate public discussion and conflict over the relative value of different health care services.
- The multi-payer nature of U.S. health care financing dictates that any spending increase by one payer type will have only an incremental effect on overall spending on primary care services.
Since Rhode Island enacted its spending mandate, the share of commercial insurance spending going to primary care has risen from 5.7 percent in 2008 to 12.3 percent in 2018, with more than 55 percent of these payments now in non-FFS methods (OHIC, 2020). Unlike Rhode Island, Oregon’s statute extends to health insurers in Medicare and Medicaid and requires health insurance carriers and the risk-bearing provider organizations in Medicaid to allocate at least 12 percent of their health care expenditures to primary care by 2023. As of 2018, insurers had met these requirements (OHA, 2019).
Researchers investigating the effects of Rhode Island’s Affordability Standards have also found that since their implementation, commercial health insurance costs rose at a slower rate than in a matched comparison group (Baum et al., 2019). They attributed most of this effect to hospital price inflation caps rather than the primary care spend requirement but noted declines in outpatient use that are not statistically significant and could have resulted from more comprehensive primary care services. Oregon’s primary care spend requirement has been coupled with the creation of a primary care transformation office in state government that establishes and implements statewide standards for patient-centered primary care homes (PCPCHs) and a statutorily established oversight commission. Evaluations of the PCPCH program have shown positive results on cost and quality (OHA, 2015).
Rhode Island’s and Oregon’s efforts show that it is possible to use government action to increase the portion of health care expenses going to primary care. Both initiatives have attempted to influence how this additional money is spent, without being overly prescriptive, and both have been underpinned by state law or regulation and public support, oversight, and accountability. Public oversight has enabled both states to build political support to continue with these policies despite the lack of objective evidence conclusively identifying their positive effects on spending and quality. This support is based on public recognition of the value of primary care, a compelling argument that an insufficient share of resources is dedicated to it, an acceptance that this imbalance will not be corrected without public action, and directionally favorable evidence (Koller and Khullar, 2017).
Implementing a primary care spend requirement remains vexing, however, primarily because the local leadership required to build political
support and the overlapping state and federal authorities attenuate a requirement’s effects. While oversight of commercial health insurance and Medicaid are the province of state officials, Medicare, Medicare Advantage, and self-insured arrangements remain the responsibility of federal authorities. Because health plans often administer self-insured arrangements and tend to operate with a common provider contract for both commercial and self-insured populations, there may be spillover effects to self-insured populations. Furthermore, with the notable exception of Rhode Island, commercial statutory standards for health insurers do not include system-wide affordability efforts, circumscribing regulators’ authority to impose spending requirements without additional statute.
Although these remain fundamental barriers to any systemic approach to health care delivery system reform in the United States, existing state reforms have generated significant additional dollars flowing into primary care. To the extent that these are coordinated across multiple payment types, as is the case in Oregon, any resulting benefits in improved primary care capacity and performance are shared across all populations.
Findings for Option 4
- At a national level, primary care–oriented health care systems are associated with better population health and lower spending.
- The portion of total health care expenses going to primary care is a way to measure primary care orientation. By this measure, the United States is at or below the proportion in other developed countries.
- State-level policies to increase primary care spending rates have been politically sustainable, resulted in significant additional resources for primary care through non-FFS mechanisms, and supported statewide efforts to build primary care capacity. When coupled in Rhode Island with hospital price inflation caps to pay for increasing funds to primary care, there were attributable spending reductions.
PAYMENT AS A FACILITATOR OF HIGH-QUALITY PRIMARY CARE
In developing recommendations for payment policies to implement high-quality primary care—in addition to the evidence and experience on the effects of payment on cost, population health, and consumer experience—design considerations must be assessed, including the models’ effect on the development and deployment of interprofessional teams, the delivery of integrated care across settings, the patient’s relationship with the primary care team, and equity.
Primary Care Team–Patient Relationships
Throughout this report (most notably in Chapter 4), the committee has underscored the importance of the relationship between the primary care team and the patient. Ideally, this relationship is built on a foundation of trust and, relevant to payment specifically, a lack of conflict of interest (Emanuel and Dubler, 1995). The managed care era featured a concern over the erosion of clinician–patient relationships and patient trust (Gray, 1997; Mechanic, 1996; Mechanic and Schlesinger, 1996; Sulmasy, 1992), though few studies have measured the effect of payment models on clinician–patient relationships. One found that FFS patients had slightly higher levels of trust than those in salary, capitated, or managed care plans (Kao et al., 1998b). Most patients, however, did not know how their physician was paid, potentially indicating that payment model is not a salient issue for patients (Kao et al., 1998a). Patient trust and good interpersonal relationships with clinicians are major predictors of patient satisfaction and loyalty in primary care (Platonova et al., 2008), and many pay-for-performance programs include patient satisfaction measures. ACO and PCMH models have shown mixed effects on patient satisfaction, with some studies showing improvements (McWilliams et al., 2014b; Sarinopoulos et al., 2017) and others no association (Hong et al., 2018; Martsolf et al., 2012). Considering patient trust and satisfaction in any payment model design is of paramount importance, yet we have little evidence to guide payment based on research to date.
Finding
- Little consistent evidence suggests that payment models affect patient experience or clinician trust, but these considerations should be central to payment design.
Interprofessional Teams and Integrated Delivery of Care
Considerable evidence shows that high-quality primary care is best delivered by interprofessional teams in multiple settings (see Chapter 6). Chronic care, for example, requires routine telephonic or video access to nurse care managers, and the acutely ill need access to sophisticated diagnostic skills. Pregnant women often benefit from in-home education by community health workers, and children and families benefit from care within a medical home with team members focused on preventive care services and care coordination for children with medical and social complexity. FFS payment is not compatible with the committee’s definition of high-quality primary care, in that it discourages person-centered,
team-based care by requiring the identification of specific services delivered by contracted clinicians in permitted settings. Part of the appeal of capitated or bundled payment is the flexibility they offer for care in multiple settings from an integrated, interprofessional care team. This notion echoes that of the “New Primary Care Paradigm” (AAFP et al., 2020), a joint statement from seven PCP societies and boards that called for a shift from FFS payment to models that are compatible with care that is more person centered, team based, and integrated.
A specific example of this flexibility is the ability to integrate behavioral health care into primary care. Behavioral health care, when fully integrated, is effective in improving population health by addressing the underlying behavioral conditions that often manifest as somatic complaints (Basu et al., 2017; Reiss-Brennan et al., 2010, 2016). A meta-analysis of randomized controlled trials of integrated primary care–behavioral health models for children and adolescents demonstrated better outcomes for the integrated care model compared with usual care, with the strongest effects for collaborative care models in which PCPs, care managers, and mental health specialists took a team-based approach (Asarnow et al., 2015). FFS payment models, particularly when paired with subcontracts by insurers for the management of behavioral health benefits, can discourage this integration by imposing licensing and billing restrictions. In addition, research has shown that current payment models cannot sustain integrated behavioral health care (Reiss-Brennan et al., 2016).
Primary care practices organized in response to FFS payment maximize revenue-producing in-person visits but are not configured to provide the integrated team-based care necessary to address the comprehensive preventive and chronic care needs of people and families, which must include behavioral, social, and oral health. Most attempts to develop these capacities in practices have recognized that it is insufficient to merely begin to pay practices differently; it is also necessary to invest in sustainable transformation resources, such as technical assistance and reimbursing practices for revenues forfeited as a result of staff development time. Medicare’s CPC+ payment model provides these additional resources through a combination of consultant payments and care management fees. Oregon has an office of primary care transformation funded through its Medicaid waiver. Some commercial insurance PCMH programs have provided similar transformation resources that are financed individually or jointly. Evidence has emerged that facilitating practice transformation improves and sustains the change process (Baskerville et al., 2012; Bitton, 2018; Harder et al., 2016). The ACA authorized a Primary Care Extension Program designed to support practice transformation facilitation. Though it was not funded, it became the basis for EvidenceNOW, a multi-state practice transformation trial funded by the Agency for Healthcare Research and Quality.
Findings
- FFS payment methods can discourage the integration of services in primary care.
- Payment support for external, supporting services, such as practice facilitation, is important for helping practices evolve but difficult to support with traditional FFS payments.
Equity
Equity is a critical element of high-quality primary care and financial barriers, along with structural and procedural characteristics, can enhance or limit equitable access to health care. However, the precise effects of payment models on access to care are elusive. Each payment method presents risks to equitable access that must be managed by the payer, often through contract terms and oversight.
Addressing SDOH, including housing, nutrition, and education, has been an important piece of improving equity in recent years. A recent National Academies report set forth specific recommendations for how health care organizations can integrate care that addresses SDOH (NASEM, 2019a). These activities, such as assisting in referrals to social services and aligning services with them, do have a cost, and practices must fund them through their revenues. Primary care–based models that have undertaken these activities, such as Vermont’s Blueprint for Health, Rhode Island’s Community Health Teams, and various Oregon coordinated care organizations, have relied on flexible payment arrangements, including capitation, that encourage team-based care.
A systematic review found reimbursement models have limited effects on socioeconomic and racial inequity in access, use, and quality of primary care. The review found capitation has a small beneficial impact on inequity in access to primary care and number of ambulatory care–sensitive admissions compared to FFS but performed worse on patient satisfaction (Tao et al., 2016). Another survey found only 16 percent of physician practices (including primary care practices) screened for SDOH. Among practices, federally qualified health centers, bundled payment participants, participants in primary care improvement models, and Medicaid ACOs had higher rates of screening for all needs (Fraze et al., 2019). By targeting health disparities as measures of performance, enabling fair comparisons among interprofessional teams based on their patient populations, and incorporating community input in payment design, payment models can promote equity (Crumley and McGinnis, 2019). See Chapter 5 for more on integrating social needs into primary care delivery.
Finding
- Enhanced primary care payments delivered through non-FFS mechanisms can improve the ability of primary care teams to coordinate social services and address inequitable access to services.
TECHNICAL CONSIDERATIONS
When thinking about options for payment reform, several technical aspects must be considered, including alignment of multiple payers, attribution of patients to health care organizations, and risk adjustment.
Multi-Payer Alignment
As noted earlier in this chapter, the committee is making recommendations based on the current reality in the United States of a fragmented hybrid public–private financing system. Two large public payers—Medicaid and Medicare—constitute close to 50 percent of health care payments and are often represented by many contracted MCOs (CMS, 2019c). The rest comes from the hundreds of insurers and third-party administrators who act as intermediaries for employers and other purchasers.
To accommodate this mix, a primary care office may have scores of insurance contracts, each potentially with different administrative rules, payment standards, and quality or cost measures. Setting aside the administrative expenses incurred by this system, the office operates in a sea of confusing financial incentives from insurers that not only have no incentive to coordinate payment terms but often see their payment methodologies as a source of competitive differentiation.
To influence a practice, any payment methodology that facilitates the implementation of high-quality primary care must be implemented consistently and at sufficiently broad scale. Some authors estimate the required penetration to be 60 percent of the practice’s patients (CMS, 2011; Friedberg et al., 2015, 2018) to change its economic incentives (Anglin et al., 2017). This dictates that payers align payment practices, because apart from closed models, such as the Veterans Health Administration, no one payer, not even Medicare, reaches this figure.
Even if insurers in each geographic market accept the desirability of multi-payer alignment, they are forbidden from explicitly coordinating under federal antitrust laws (Takach et al., 2015). Several attempts to address this barrier have been undertaken. State officials may invoke a state action exemption, permissible under federal laws, and declare it in the state’s interests for competing insurers to share certain information in a process actively overseen by state government, with a goal of aligning payment
methodologies to primary care. Many states used this authority to secure multi-payer participation in PCMH models (AcademyHealth, 2010; Takach et al., 2015).
Under its CPC and CPC+ payment initiatives, CMMI has required multi-payer participation and alignment, rather than payment coordination. Payers make a commitment to payment models similar to CMMI’s as a precondition to participation, with similarity adjudicated by CMMI based on a confidential review of the proposed model. The effects of the models’ multi-payer design have not been assessed independent of the rest of the components, such as payment amounts and methodology, practice transformation resources, and practice feedback tools. Anecdotally, a multi-payer forum often facilitated by the CPC payment models to address areas of common concern and improvement, such as quality measurement alignment, practice transformation and feedback, and health information exchange, has been beneficial in markets for promoting both better payer/ clinician relations and high-quality primary care.
Finally, the CMMI-funded Healthcare Payment Learning and Action Network has been an attempt to facilitate national multi-payer discussions focused on speeding the adoption of alternative payment models by public and private payers. Lacking authority, however, and subject to varying levels of interest and support in the succeeding administration, it remains a relatively weak lever for aligning payer activities.
In terms of fostering multi-payer alignment, the broad historical influence of Medicare’s payment policies for physicians, hospitals, and ancillary providers on commercial and Medicaid payers is instructive. FFS physician payments predominate in the United States because of Medicare’s policies and size—where it goes, other payers inevitably follow. CMMI’s primary care payment models have defined the field of experimentation and yielded instructive experience. Other payers have also tested payment and delivery models and provided important technical support to practices, yet information about these models is less available in the public domain. The sooner Medicare can move from voluntary models to mandatory ones—agreeing on how to pay all primary care teams for Medicare beneficiaries—the more likely other payers are to fall in line. This alignment can then be facilitated by market-based efforts focused on other elements of primary care transformation, including measurement and feedback alignment.
Attribution
As discussed in Chapter 6, empanelment is an important component to high-quality primary care. It can be defined as a continuous, iterative set of processes that identify and assign populations to practices, care teams, or clinicians that have a responsibility to know their assigned population and
proactively deliver coordinated primary care (Bearden et al., 2019). Under hybrid reimbursement or risk-sharing models, payers and clinicians need a clear definition of the people the risk-sharing entity is responsible for in order to measure cost and quality. Making sure any capitated payment goes to the correct practice when a patient retains full freedom of choice of clinician, as in traditional Medicare, Medicare Advantage, and commercial preferred provider organizations, and in many Medicaid programs, is necessary and challenging.
Payers use two processes to assign patients to clinicians: voluntary alignment and attribution. In voluntary alignment, patients document whom they consider to be their primary care clinician. Alternatively, they can be attributed to clinician organizations using care patterns in insurance claims data. Where possible, voluntary alignment is likely to be more compatible with the goals of high-quality primary care, by virtue of engaging people and their preferences, yet the process is administratively complex and rarely used (MedPAC, 2018a).
Claims-based attribution based on care patterns can be prospective, meaning that clinicians are given a list of whom they are responsible for in the beginning of the year, or retrospective, when they are notified at the end of the year. Most attribution rules assign patients based on the plurality of their outpatient visits, while some focus specifically on primary care services. The details are important; the specific services that qualify for attribution (only outpatient evaluation and management codes or a larger set of services), how the quantity of services is measured (e.g., number of visits or allowed charges), how clinicians are grouped into teams to determine plurality (by the system, practice, or individually), whether specialists or associates count toward attribution, and whether any preference is given to primary care clinicians each impact who is attributed and resulting outcomes.
Research has found substantial turnover in attribution year over year, yet most patients are attributable using retrospective methodology (e.g., 88 percent of Medicare beneficiaries are attributable based on evaluation and management visits) (Hsu et al., 2016; McWilliams et al., 2014a; Ouayogodé et al., 2018). One study found that although both prospective and retrospective attribution have benefits and drawbacks, retrospective attribution yielded greater overlap of attributed patients and those treated during the year and resulted in a higher proportion of care concentrated within an ACO (Lewis et al., 2013). Furthermore, certain patient populations are difficult to capture via attribution, including the healthy, who use few qualifying health care services, and those at the end of life (Ouayogodé et al., 2018).
Most of these research studies had no “gold standard” attribution to compare the alignment of various methodologies. An exception is a study
of empaneled patients at The Mayo Clinic, where researchers compared five methods and found the proportion of patients correctly attributed to their paneled clinician was 22–45 percent, with ACO attribution capturing the most empaneled patients and marked variation in use and spending by method (McCoy et al., 2018). All stakeholders need to understand how differences in attribution method affect the way that health care is measured, evaluated, and reported (Higuera and Carlin, 2017; McCoy et al., 2016; Mehrotra et al., 2010; NQF, 2019).
Risk Adjustment
In any model where a portion of the payment is not FFS, or those services vary in intensity based on the illness and case complexity, risk adjustment is of paramount importance. Risk adjustment involves quantifying the patient’s complexity based on observable data in order to adjust the payment. In the absence of strong risk adjustment for health status, clinicians might “cream-skim,” or shun sicker, costlier patients who would take up more time and resources in favor of healthier ones for whom payment would be the same (Berenson et al., 2016).
Risk adjustment must address the time and effort clinicians provide for patients of different complexity. Risk adjustment for primary care capitation as a full replacement for PFS payment needs to be a much more accurate predictor of performance risk than in hybrid payment models that continue to include a substantial percentage of PFS payments; PFSs serve as a reasonably effective form of risk adjustment for most patients (because more complex patients typically generate more visits).
Some payment models adopt the standard hierarchical condition category (HCC) model of risk adjustment that was initially used for full risk Medicare Advantage plans (Pope et al., 2004). HCCs were designed to adjust payment via a dominant factor of predicting hospitalization spending. This tool makes sense if the primary care practice were held accountable for the total cost of care but may not be the best measure of the relative effort and practice-based resource expenditures for primary care teams managing patients with different complexities.
An alternative view is that primary care capitation should seek to adjust for “activity level,” the care that primary care clinicians should provide, accounting for the variation between healthy and complex patients (Goroll et al., 2007). An assessment of one risk adjustment approach to support this payment model found that the predicted and apparent costs of providing comprehensive primary care vary more than 100-fold across patients. It also showed that sophisticated risk adjustment is required to adequately distinguish across such differences (Ash and Ellis, 2012).
Current methods of risk adjustment relying on diagnosis- and use-based algorithms to predict future use may not capture nonclinical contributors to patient complexity (Berry et al., 2015; Fuentes and Coker, 2018; Hong et al., 2015), which should include SDOH. Patients identified as complex by physicians had only modest overlap with those identified using claims data, because clinicians consider medical, behavioral, and socioeconomic complexity domains. Primary care clinicians’ qualitative assessment of future hospitalization risk among patients in their panels was an important independent predictor of subsequent hospitalization (Hwang et al., 2017). A study of primary care practices participating in CPC found that adding clinical intuition to clinical algorithms was associated with higher enrollment in care management within primary care practices (Reddy et al., 2017). Other models have proposed simple risk assessment methods, such as relying on “How’s Your Health” self-assessments of pain, emotional issues, medical complexity (polypharmacy), medication side effects, and health care confidence (Antonucci, 2018). Self-reported health measures may also provide a promising way to prospectively profile likely health care needs (Wherry et al., 2014). In the future, more electronic health record or self-reported measures could be added to risk adjustment, but the technology does not exist yet to do this comprehensively.
A payment formula that accounts for medical problems but ignores social risk can underpay for vulnerable populations, potentially exacerbating inequality (Ash et al., 2017; Schrager et al., 2016). Building on studies that found neighborhood deprivation was associated with worse health status, recent work has progressed in risk adjustment for social factors (Nobel et al., 2017). In 2016, Massachusetts began adjusting payments based on SDOH, adding predictors describing housing instability, behavioral health issues, disability, and neighborhood-level stressors (Ash, 2016; Ash and Mick, 2016). Medical spending in residents of the most stressed neighborhoods was more than 23 percent higher than that in the least stressed neighborhoods. Overall, the model including these social factors performed slightly better than the diagnosis-based model, explaining most spending variation and reducing underpayments for vulnerable populations (Ash et al., 2017). In addition to adjusting for the proportion of a practices’ patients covered by Medicaid, Vermont uses an indicator variable for members with more than $500 in annual payments for “special Medicaid services” (day treatment, residential treatment, case management services, and special school services covered by the U.S. Department of Education) to adjust payments for social needs. This is in addition to adjustment for the proportion of a practice’s patients covered by Medicaid insurance and an interaction term for Medicaid coverage and use of maternity services, given the high risk for poor outcomes (Finison et al., 2017).
Findings for Technical Considerations
- Multi-payer alignment across financial incentives, quality measurement, and data feedback is critical but challenging.
- The federal government plays an important role in convening and guiding multi-payer alignment.
- Antitrust law can be a barrier to multi-payer alignment, yet states can act to facilitate it.
- Reliable patient attribution at the practice level is fundamental to any non-FFS primary care payment methodology.
- Risk adjustment of any capitation payment is important for fair payment; the greater the share of payment made by capitation, the more important risk adjustment precision is. Diagnosis use-based algorithms are the most common. Mechanisms using social risk adjustment factors are being tested and have shown promise.
GOALS AND MEASURES OF SUCCESS FOR PRIMARY CARE PAYMENT
The measure of whether a payment system for primary care is effective requires an understanding of the goals of payment design. The delivery of high-quality primary care as defined by the committee should drive the design of a payment system to support it adequately and effectively. In the United States, unfortunately, the converse has been true for the last four decades: an idiosyncratic, not-fit-for-purpose payment system has driven the design of a volume- and visit-based delivery system unable to support the provision of continuous long-term relationships or a strong connection between primary care, the rest of the health care system, and relevant parts of public health. If adequately supported, primary care will offer societal benefits as well as individual ones. For this reason, the committee believes primary care should be a common good and that payment models should reflect this. Furthermore, as the COVID-19 pandemic has demonstrated, the current, piecemeal system built on a chassis of FFS is unable to withstand health or volume shocks, making primary care particularly vulnerable at moments when it is most needed to be consistently effective. The underlying FFS basis, with layers of value-based payment reform and complex and sometimes competing incentives to an already stretched workforce, often yields mixed results or unsustainable improvements.
Effective primary care will require higher levels of predictable payment that allow patients to build, maintain, and access long-term relationships with integrated care teams. As has been discussed in previous chapters, such relationships are formed in different clinician settings based on patient circumstances, and payment should be flexible to support all of them.
Getting to a level of adequate spending to support relationship-based care will take time and experimentation with a variety of hybrid models. As this chapter has shown, all payment designs have pros and cons. Multi-payer collaboration to create a mix of approaches that minimizes the drawbacks and effectively blends incentives matched to a particular community of patients and clinicians will likely work best, though this will need further empirical testing and validation. Furthermore, careful attribution and risk adjustment, including for social factors, will be key to ensure that primary care practices are paid sufficiently and equitably to take care of a clearly defined population for which they will be appropriately and fairly held accountable and to precipitate unintended consequences that could result in expanding, not diminishing, disparities in care.
The organization of primary care in the United States is quite diverse, and primary care payment models must match the capacity and capabilities of different organizations. Payers should continue to maintain a portfolio of primary care payment methods to accommodate different organizational structures, geographic cultural variations, and community realities, yet the hybrid reimbursement models reviewed here should constitute alternative base payment models, with an option remaining for the assumption of more financial risk. Primary care models oriented to comprehensive care for a broad population have different financial needs and risk tolerance than those focused on narrow segmentation for high-cost, high-need patients or a pediatric population, in which costs savings are a more long-term horizon and often attributed to sectors outside of health care. The committee believes it is important to maintain the diversity of primary care practice settings that currently exist but that a base-level, multi-payer hybrid reimbursement model, with reimbursement levels adequate to support an integrated, team-based care, should be the default rather than FFS.
Measuring the ultimate success of increasing both the levels and trends in primary care spending, while changing the type, is necessarily multimodal. At the practice level, it should encourage accountability and high performance for standards set forth in Chapter 8. Workforce measures, such as attrition, burnout, practice closure, and recruitment into the field, tell a deeply discouraging story (Steinwald et al., 2018), especially in underserved or historically marginalized communities. The ability and interest of primary care practices, especially independent ones, to continue to serve their communities despite often overwhelming pandemic and financial shocks is another measure of the success, or failure, of near-term payment reform.
Primary care alone should not be saddled with the burden of reducing the excessive costs of health care in the United States. Clear evidence (Song and Gondi, 2019) is emerging that primary care transformation and payment reform does not reduce total costs of care in the short or medium
term, despite many stakeholders’ best wishes. Over the long term, clear national and global evidence suggests that primary care–oriented systems with more robust primary care payment are more efficient than specialty-oriented and FFS payment models, but it can take decades to achieve these results (WHO, 2018). While in the medium term, strengthening primary care can achieve cost savings by reducing ambulatory care–sensitive emergency room visits and hospitalizations (Maeng et al., 2016; OECD, 2020; Saynisch et al., 2021), system-wide changes that reorient the health care workforce and practice patterns to primary care can take much longer (Friedberg et al., 2010). Thus, primary care payment reform should serve to start to rebalance the specialist–generalist ratios and spending in the United States but not have to assume that it can “pay for itself” in the short term.
Fundamentally, primary care payment reform should be thought of as an investment in future health asset capacity and equity production, instead of a simplistic return on investment for near-term savings. If cost savings are paramount, other means are more effective at reducing costs. What should motivate interested stakeholders more are the measures of population health, equitable outcomes, changing mortality and chronic disease prevalence trends, and overall increased health and well-being for individuals and families (OECD, 2020; WHO, 2018) that primary care can produce with larger, more predictable, payment (Basu et al., 2018).
Findings for Goals and Measures of Success
- Long-term payment reform plus redistribution toward primary care can deliver a reorientation of the entire health system toward more equitable and efficient goals.
- Primary care payment reform can be seen as an investment in future health system capacities and orientation, as opposed to a short-term driver of cost savings.
- Prospective, population-based payment can serve as a source of predictable revenue during times of crisis and service disruption.
FINDINGS AND CONCLUSIONS
Evidence shows that the dominant FFS payment mechanism, in combination with the process CMS uses to set relative prices for primary care and other services in the PFS, continues to devalue and shortchange primary care relative to its population health benefit, resulting in the large and widening gaps between primary care and specialty care compensation. In fact, using the portion of total health care expenses going to primary care as a measure of primary care orientation, the United States is at or below the proportion in other developed countries. This widening compensation gap
is associated with reductions in medical trainees’ likelihood of choosing primary care careers and with hospitals’ graduate medical education training priorities. However, if CMS is provided with adequate leadership and resources to establish its own data collection and valuation tools, rather than relying on the RUC recommendations that reflect the dominance of specialty care in RUC membership, it has the authority to address the weaknesses of the current system and generate payment levels aligned with high-quality primary care.
Such action, however, would not negate the inherent shortcomings of FFS payment models. Evidence supports the finding that FFS models discourage successful engagement of primary care practices in structure and process improvements and the integration of other services into primary care, while hybrid payment models can mitigate FFS incentives for increased use and provide resources for integrated, team-based care and non-FFS services consistent with the committee’s definition of high-quality primary care. In that respect, hybrid payment models should be seen as a mechanism to support high-quality care rather than a means of reducing spending and use in the short term. That said, in the long run, hybrid reimbursement models have potential to improve care and reduce use, particularly when they are aligned across payers and for people with multiple complex chronic conditions.
With almost half of primary care clinicians employed in health systems, attention should be paid to primary care payment methods in those settings. Many ACOs, which have demonstrated modest savings in total spending alongside quality and patient satisfaction improvements, continue to pay primary care internally based on FFS, even though the larger organization itself may participate in risk-sharing models. ACOs that are predominately primary care, PCMH based, or physician led achieve better performance (better population health and lower spending) than other ACOs. Some evidence indicates that pediatric-focused ACO models are effective.
State-level policies to increase primary care spending rates, which have been politically sustainable, resulted in significant additional resources for primary care through non-FFS mechanisms and supported statewide efforts to build primary care capacity. When coupled in Rhode Island with hospital price inflation caps to pay for increasing funds to primary care, there were attributable spending reductions. In addition, state-level action can address antitrust-associated barriers that can encourage multi-payer alignment across financial incentives, quality measurement, and data feedback, which can increase the likelihood of practice improvement in markets that lack one dominant payer. The federal government can also play an important role in convening and guiding multi-payer alignment.
In summary, primary care payment reform is an investment in future health system capacities and orientation. Long-term payment reforms plus
redistribution toward primary care can reorient the entire health system, resulting in improved population health and greater health equity. While such reform may reduce health care expenditures in the long run, short-term cost savings should not be the priority policy outcome.
REFERENCES
AAFP (American Academy of Family Physicians). 2017a. AAFP member survey provides valuable perspective. https://www.aafp.org/news/blogs/inthetrenches/entry/20170801ITT_Survey.html (accessed September 4, 2020).
AAFP. 2017b. Advanced primary care: A foundational alternative payment model (APC-APM) for delivering patient-centered, longitudinal, and coordinated care; a proposal to the Physician-Focused Payment Model Technical Advisory Committee. Leawood, KS: American Academy of Family Physicians.
AAFP. 2020. Direct primary care. https://www.aafp.org/family-physician/practice-and-career/delivery-payment-models/direct-primary-care.html (accessed November 23, 2020).
AAFP, AAP (American Academy of Pediatrics), ABFM (American Board of Family Medicine), ABIM (American Board of Internal Medicine), ABP (American Board of Pediatrics), ACP (American College of Physicians), and SGIM (Society of General Internal Medicine). 2020. A new primary care paradigm. https://www.newprimarycareparadigm.org (accessed December 23, 2020).
AAP (American Academy of Pediatrics). 2019. Pediatricians’ practice and personal characteristics: U.S. only, 2018–2019. https://www.aap.org/en-us/professional-resources/Research/pediatrician-surveys/Pages/Personal-and-Practice-Characteristics-of-Pediatricians-USonly.aspx (accessed December 18, 2020).
AAPA (American Academy of Physician Assistants). 2020. Top 10 paying specialties in the PA profession. https://www.aapa.org/news-central/2020/12/top-10-paying-specialties-in-the-pa-profession (accessed December 17, 2020).
Abelson, R. 2019. High medical bills are at center of hospital group’s trial. The New York Times, October 3. https://www.nytimes.com/2019/10/03/health/sutter-hospitals-medicalbills.html (accessed December 18, 2020).
AcademyHealth. 2010. Navigating antitrust concerns in multi-payer initiatives. Washington, DC: AcademyHealth.
AHRQ (Agency for Healthcare Research and Quality). 2020. Mean events per person by age groups, United States, 1996–2018. https://www.meps.ahrq.gov/mepstrends/hc_use (accessed October 19, 2020).
Albright, B. B., V. A. Lewis, J. S. Ross, and C. H. Colla. 2016. Preventive care quality of Medicare accountable care organizations: Associations of organizational characteristics with performance. Medical Care 54(3):326–335.
Altman, S. H. 2012. The lessons of Medicare’s prospective payment system show that the bundled payment program faces challenges. Health Affairs 31(9):1923–1930.
AMA (American Medical Association). 2016. Composition of the RVS update committee (RUC). https://www.ama-assn.org/about/rvs-update-committee-ruc/composition-rvs-update-committee-ruc (accessed September 8, 2020).
Anglin, G., H. A. Tu, K. Liao, L. Sessums, and E. F. Taylor. 2017. Strengthening multipayer collaboration: Lessons from the Comprehensive Primary Care Initiative. Milbank Quarterly 95(3):602–633.
Antonucci, J. 2018. An innovative model for primary care office payment. https://aspe.hhs.gov/system/files/pdf/255906/ProposalAntonucci.pdf (accessed February 1, 2021).
Asarnow, J. R., M. Rozenman, J. Wiblin, and L. Zeltzer. 2015. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta-analysis. JAMA Pediatrics 169(10):929–937.
Ash, A. 2016. Masshealth risk adjustment model social determinants of health. Boston, MA: Executive Office of Health & Human Services.
Ash, A. S., and R. P. Ellis. 2012. Risk-adjusted payment and performance assessment for primary care. Medical Care 50(8):643–653.
Ash, A., and E. Mick. 2016. UMass risk adjustment project for Masshealth payment and care delivery reform: Describing the 2017 payment mode. Worcester, MA: UMass Medical School Center for Health Policy and Research.
Ash, A. S., E. O. Mick, R. P. Ellis, C. I. Kiefe, J. J. Allison, and M. A. Clark. 2017. Social determinants of health in managed care payment formulas. JAMA Internal Medicine 177(10):1424–1430.
Baskerville, N. B., C. Liddy, and W. Hogg. 2012. Systematic review and meta-analysis of practice facilitation within primary care settings. Annals of Family Medicine 10(1):63–74.
Basu, S., B. E. Landon, J. W. Williams, Jr., A. Bitton, Z. Song, and R. S. Phillips. 2017. Behavioral health integration into primary care: A microsimulation of financial implications for practices. Journal of General Internal Medicine 32(12):1330–1341.
Basu, S., R. S. Phillips, A. Bitton, Z. Song, and B. E. Landon. 2018. Finance and time use implications of team documentation for primary care: A microsimulation. Annals of Family Medicine 16(4):308–313.
Basu, S., S. A. Berkowitz, R. L. Phillips, A. Bitton, B. E. Landon, and R. S. Phillips. 2019. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Internal Medicine 179(4):506–514.
Basu, S., R. S. Phillips, R. Phillips, L. E. Peterson, and B. E. Landon. 2020. Primary care practice finances in the United States amid the COVID-19 pandemic. Health Affairs 10.1377/hlthaff.2020.00794.
Baum, A., Z. Song, B. E. Landon, R. S. Phillips, A. Bitton, and S. Basu. 2019. Health care spending slowed after Rhode Island applied affordability standards to commercial insurers. Health Affairs 38(2):237–245.
Bearden, T., H. Ratcliffe, J. Sugarman, A. Bitton, L. Anaman, G. Buckle, M. Cham, D. Chong Woei Quan, F. Ismail, B. Jargalsaikhan, W. Lim, N. Mohammad, I. Morrison, B. Norov, J. Oh, G. Riimaadai, S. Sararaks, and L. Hirschhorn. 2019. Empanelment: A foundational component of primary health care. Gates Open Research 3(1654).
Berenson, R. A. 1989. Physician payment reform: Congress’s turn. Annals of Internal Medicine 111(5):351–353.
Berenson, R. A., and J. D. Goodson. 2016. Finding value in unexpected places—fixing the Medicare physician fee schedule. New England Journal of Medicine 374(14):1306–1309.
Berenson, R. A., D. K. Upadhyay, S. F. Delbanco, and R. Murray. 2016. Payment methods: How they work. Washington, DC: Urban Institute.
Berenson, R. A., A. Shartzer, and R. C. Murray. 2020. Strengthening primary care delivery through payment reform. Paper commissioned by the Committee on Implementing High-Quality Primary Care. https://www.nap.edu/catalog/25983 (accessed May 4, 2021).
Berry, J. G., M. Hall, J. Neff, D. Goodman, E. Cohen, R. Agrawal, D. Kuo, and C. Feudtner. 2014. Children with medical complexity and Medicaid: Spending and cost savings. Health Affairs 33(12):2199–2206.
Berry, J. G., M. Hall, E. Cohen, M. O’Neill, and C. Feudtner. 2015. Ways to identify children with medical complexity and the importance of why. Journal of Pediatrics 167(2):229–237.
Bianco, D., C. Demars, L. Miller, and E. Sites. 2020. The impact of federal value-based primary care programs on participating Oregon practices: A snapshot. New York: Milbank Memorial Fund.
Bitton, A. 2018. Finding a parsimonious path for primary care practice transformation. Annals of Family Medicine 16(Suppl 1):S16–S19.
Bitton, A., C. Martin, and B. E. Landon. 2010. A nationwide survey of patient centered medical home demonstration projects. Journal of General Internal Medicine 25(6):584–592.
Bitton, A., G. R. Schwartz, E. E. Stewart, D. E. Henderson, C. A. Keohane, D. W. Bates, and G. D. Schiff. 2012. Off the hamster wheel? Qualitative evaluation of a payment-linked patient-centered medical home (PCMH) pilot. Milbank Quarterly 90(3):484–515.
Bitton, A., H. L. Ratcliffe, J. H. Veillard, D. H. Kress, S. Barkley, M. Kimball, F. Secci, E. Wong, L. Basu, C. Taylor, J. Bayona, H. Wang, G. Lagomarsino, and L. R. Hirschhorn. 2017. Primary health care as a foundation for strengthening health systems in low- and middle-income countries. Journal of General Internal Medicine 32(5):566–571.
Bleser, W. K., R. S. Saunders, D. Muhlestein, S. Q. Morrison, H. H. Pham, and M. McClellan. 2018. ACO quality over time: The MSSP experience and opportunities for system-wide improvement. American Journal of Accountable Care 6(1):e1–e15.
Bodenheimer, T. 2006. Primary care—will it survive? New England Journal of Medicine 355(9):861–864.
Bodenheimer, T. 2008. Coordinating care—a perilous journey through the health care system. New England Journal of Medicine 358(10):1064–1071.
Bolnick, H. J., A. L. Bui, A. Bulchis, C. Chen, A. Chapin, L. Lomsadze, A. H. Mokdad, F. Millard, and J. L. Dieleman. 2020. Health-care spending attributable to modifiable risk factors in the USA: An economic attribution analysis. The Lancet Public Health 5(10):e525–e535.
BPC (Bipartisan Policy Center). 2020. Advancing comprehensive primary care in Medicaid. Washington, DC: Bipartisan Policy Center.
Brown, C. C., and J. M. Tilford. 2020. Value-based primary care: Insights from a commercial insurer in Arkansas. New York: Milbank Memorial Fund.
Burton, R., R. Berenson, and S. Zuckerman. 2017. Medicare’s evolving approach to paying for primary care. Washington, DC: Urban Institute.
Burton, R. A., N. M. Lallemand, R. A. Peters, and S. Zuckerman. 2018. Characteristics of patient-centered medical home initiatives that generated savings for Medicare: A qualitative multi-case analysis. Journal of General Internal Medicine 33(7):1028–1034.
Busch, F., D. Grzeskowiak, and E. Huth. 2020. Direct primary care: Evaluating a new model of delivery and financing. Schaumburg, IL: Society of Actuaries.
Calsyn, M., and M. Twomey. 2018. Rethinking the RUC: Reforming how Medicare pays for doctors’ services. https://www.americanprogress.org/issues/healthcare/reports/2018/07/13/453159/rethinking-the-ruc (accessed December 7, 2020).
Carlo, A. D., L. Drake, A. D. H. Ratzliff, D. Chang, and J. Unützer. 2020. Sustaining the collaborative care model (COCM): Billing newly available COCM CPT codes in an academic primary care system. Psychiatric Services 71(9):972–974.
CHCS (Center for Health Care Strategies). 2017. Medicaid ACO programs: Promising results from leading-edge states. Trenton, NJ: Center for Health Care Strategies.
Chien, A. T., Z. Song, M. E. Chernew, B. E. Landon, B. J. McNeil, D. G. Safran, and M. A. Schuster. 2014. Two-year impact of the alternative quality contract on pediatric health care quality and spending. Pediatrics 133(1):96–104.
Christensen, E. W., and N. R. Payne. 2016. Effect of attribution length on the use and cost of health care for a pediatric Medicaid accountable care organization. JAMA Pediatrics 170(2):148–154.
Clemens, J., and J. D. Gottlieb. 2014. Do physicians’ financial incentives affect medical treatment and patient health? American Economic Review 104(4):1320–1349.
Clemens, J., J. D. Gottlieb, and T. L. Molnár. 2015. The anatomy of physician payment: Contracting subject to complexity. Cambridge, MA: National Bureau of Economic Research.
CMS (Centers for Medicare & Medicaid Services). 2011. Solicitation for the comprehensive primary care initiative. Baltimore, MD: Centers for Medicare & Medicaid Services.
CMS. 2019a. HHS news: HHS to delivery value-based transformation in primary care. https://www.cms.gov/newsroom/press-releases/hhs-news-hhs-deliver-value-based-transformation-primary-care (accessed November 30, 2020).
CMS. 2019b. National health expenditures 2019 highlights. Baltimore, MD: Centers for Medicare & Medicaid Services.
CMS. 2019c. National health expenditure data (by source of funds). https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical (accessed July 22, 2020).
CMS. 2020a. Comprehensive primary care initiative. https://innovation.cms.gov/innovationmodels/comprehensive-primary-care-initiative (accessed July 20, 2020).
CMS. 2020b. Comprehensive primary care plus. https://innovation.cms.gov/innovationmodels/comprehensive-primary-care-plus (accessed September 3, 2020).
CMS. 2020c. Direct contracting model options. https://innovation.cms.gov/innovation-models/direct-contracting-model-options (accessed September 3, 2020).
CMS. 2020d. Final rule and interim final rule: Medicare program; CY 2021 payment policies under the physician fee schedule and other changes to Part B payment policies; etc. As published on December 28, 2020. Federal Register 85(248). https://www.govinfo.gov/content/pkg/FR-2020-12-28/pdf/2020-26815.pdf (accessed March 11, 2021).
CMS. 2020e. Final rule: Medicaid program; Medicaid and Children’s Health Insurance Program (CHIP) managed care. As published on November 13, 2020. Federal Register 85(220):72802–72807. https://www.govinfo.gov/content/pkg/FR-2020-11-13/pdf/202024758.pdf (accessed February 26, 2021).
CMS. 2020f. Primary Care First model options. https://innovation.cms.gov/innovation-models/primary-care-first-model-options (accessed September 3, 2020).
CMS. 2020g. Primary Care First: Payment webinar. Baltimore, MD: Centers for Medicare & Medicaid Services.
COGME (Council on Graduate Medical Education). 2010. Advancing primary care. Rockville, MD: Council on Graduate Medical Education.
Colla, C. H., T. Ajayi, and A. Bitton. 2020. Potential adverse financial implications of the merit-based incentive payment system for independent and safety net practices. JAMA 324(10):948–950.
Commonwealth Fund Task Force on Payment and Delivery System Reform. 2020. Health care delivery system reform: Six policy imperatives. Washington, DC: The Commonwealth Fund.
Coulam, R. F., and G. L. Gaumer. 1991. Medicare’s prospective payment system: A critical appraisal. Health Care Financing Review (Annual Supplement):45–77.
Cromwell, J., and J. B. Mitchell. 1986. Physician-induced demand for surgery. Journal of Health Economics 5(4):293–313.
Crumley, D., and T. McGinnis. 2019. Advancing health equity in Medicaid: Emerging value-based payment innovations. https://www.chcs.org/advancing-health-equity-in-medicaid-emerging-value-based-payment-innovations (accessed July 20, 2020).
Cunningham, P., and J. May. 2006. Medicaid patients increasingly concentrated among physicians. Tracking Report (16):1–5.
Davis, K., M. Abrams, and K. Stremikis. 2011. How the Affordable Care Act will strengthen the nation’s primary care foundation. Journal of General Internal Medicine 26(10):1201–1203.
Decker, S. L. 2012. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Affairs 31(8):1673–1679.
Delaware DOI (Department of Insurance). 2020. Delaware health care affordability standards: An integrated approach to improve access, quality and value. Dover, DE: Delaware Department of Insurance.
Dewar, S., J. Bynum, and J. A. Batsis. 2020. Uptake of obesity intensive behavioral treatment codes in Medicare beneficiaries, 2012–2015. Journal of General Internal Medicine 35(1):368–370.
Doherty, R., N. S. Damle, J. A. Blehm, C. M. Reimer, M. Auron, E. Barrett, J. W. Fincher, A. L. Fuisz, C. S. Hunter, M. D. Leahy, M. D. Mignoli, R. McLean, A. L. Clark, M. Newman, J. O’Neill, Jr., C. M. Soppet, F. Syed, and M. P. Tschanz. 2015. Assessing the patient care implications of “concierge” and other direct patient contracting practices: A policy position paper from the American College of Physicians. Annals of Internal Medicine 163(12):949–952.
Dowd, B. E., and M. J. Laugesen. 2020. Fee-for-service payment is not the (main) problem. Health Services Research 55(4):491–495.
Doximity. 2019. 2019 physician compensation report: Third annual study. San Francisco, CA: Doximity.
Dulsky Watkins, L. 2019. Comprehensive primary care in Ohio and Kentucky—positive findings. https://www.milbank.org/2019/01/comprehensive-primary-care-in-ohio-and-kentucky-positive-findings (accessed July 20, 2020).
Dwyer-Lindgren, L., A. Bertozzi-Villa, R. W. Stubbs, C. Morozoff, J. P. Mackenbach, F. J. van Lenthe, A. H. Mokdad, and C. J. L. Murray. 2017. Inequalities in life expectancy among U.S. counties, 1980 to 2014: Temporal trends and key drivers. JAMA Internal Medicine 177(7):1003–1011.
Edwards, S. T., A. Bitton, J. Hong, and B. E. Landon. 2014. Patient-centered medical home initiatives expanded in 2009–13: Providers, patients, and payment incentives increased. Health Affairs 33(10):1823–1831.
Ellis, R. P., and T. G. McGuire. 1990. Optimal payment systems for health services. Journal of Health Economics 9(4):375–396.
Emanuel, E. J., and N. N. Dubler. 1995. Preserving the physician–patient relationship in the era of managed care. JAMA 273(4):323–329.
Finison, K., M. Mohlman, C. Jones, M. Pinette, D. Jorgenson, A. Kinner, T. Tremblay, and D. Gottlieb. 2017. Risk-adjustment methods for all-payer comparative performance reporting in Vermont. BMC Health Services Research 17(1):58.
Fraze, T. K., A. L. Brewster, V. A. Lewis, L. B. Beidler, G. F. Murray, and C. H. Colla. 2019. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by us physician practices and hospitals. JAMA Network Open 2(9):e1911514.
Friedberg, M. W., P. S. Hussey, and E. C. Schneider. 2010. Primary care: A critical review of the evidence on quality and costs of health care. Health Affairs 29(5):766–772.
Friedberg, M. W., P. G. Chen, C. White, O. Jung, L. Raaen, S. Hirshman, E. Hoch, C. Stevens, P. B. Ginsburg, L. P. Casalino, M. Tutty, C. Vargo, and L. Lipinski. 2015. Effects of health care payment models on physician practice in the United States. Santa Monica, CA: RAND Corporation.
Friedberg, M. W., P. G. Chen, M. M. Simmons, T. Sherry, P. Mendel, L. Raaen, J. Ryan, P. Orr, C. Vargo, L. Carlasare, C. Botts, and K. Blake. 2018. Effects of health care payment models on physician practice in the United States: Follow-up study. Santa Monica, CA: RAND Corporation.
Fuentes, M., and T. R. Coker. 2018. Social complexity as a special health care need in the medical home model. Pediatrics 142(6).
Fujisawa, R., and G. Lafortune. 2008. The remuneration of general practitioners and specialists in 14 OECD countries. OECD Health Working Papers No. 14.
Galewitz, P. 2018. Medicare advantage plans shift their financial risk to doctors. https://www.modernhealthcare.com/article/20181008/NEWS/181009920/medicare-advantage-plans-shift-their-financial-risk-to-doctors (accessed October 17, 2020).
GAO (U.S. Government Accountability Office). 2012. Higher use of advanced imaging services by providers who self-refer costing Medicare millions. Washington, DC: U.S. Government Accountability Office.
GAO. 2015. Medicare physician payment rates: Better data and greater transparency could improve accuracy. Washington, DC: U.S. Government Accountability Office.
George, A., N. Sachdev, J. Hoff, S. Borg, T. Weida, M. O’Connor, and K. N. Davis. 2019. Development, value, and implications of a comprehensive primary care payment calculator for family medicine report from Family Medicine for America’s Health Payment Tactic Team. Family Medicine 51(2):185–192.
Goroll, A. H., R. A. Berenson, S. C. Schoenbaum, and L. B. Gardner. 2007. Fundamental reform of payment for adult primary care: Comprehensive payment for comprehensive care. Journal of General Internal Medicine 22(3):410–415.
Gray, B. H. 1997. Trust and trustworthy care in the managed care era. Health Affairs 16(1):34–49.
Gruber, J., J. Kim, and D. Mayzlin. 1998. Physician fees and procedure intensity: The case of cesarean delivery. NBER Working Paper Series (Working Paper 6744).
Hadley, J. 2003. Sicker and poorer—the consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Medical Care Research and Review 60(Supplement to June 2003):3S–75S; discussion 76S–112S.
Harder, V. S., W. E. Long, S. E. Varni, J. Samuelson, and J. S. Shaw. 2016. Pediatric-informed facilitation of patient-centered medical home transformation. Clinical Pediatrics 56(6):564–570.
HCPLAN (Health Care Payment Learning & Action Network). 2019. Measuring progress: Adoption of alternative payment models in commercial, Medicaid, Medicare Advantage, and traditional Medicare programs. McLean, VA: The MITRE Corporation.
Hellinger, F. J. 1996. The impact of financial incentives on physician behavior in managed care plans: A review of the evidence. Medical Care Research and Review 53(3):294–314.
Higuera, L., and C. Carlin. 2017. A comparison of retrospective attribution rules. American Journal of Managed Care 23(6):e180–e185.
Hinton, E., R. Rudowitz, M. Diaz, and N. Singer. 2019. 10 things to know about Medicaid managed care. San Francisco, CA: Kaiser Family Foundation.
Holgash, K., and M. Heberlein. 2019. Physician acceptance of new Medicaid patients: What matters and what doesn’t. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20190401.678690/full (accessed December 18, 2020).
Hong, C. S., S. J. Atlas, J. M. Ashburner, Y. Chang, W. He, T. G. Ferris, and R. W. Grant. 2015. Evaluating a model to predict primary care physician-defined complexity in a large academic primary care practice-based research network. Journal of General Internal Medicine 30(12):1741–1747.
Hong, Y. R., K. Sonawane, S. Larson, A. G. Mainous, and N. M. Marlow. 2018. Impact of provider participation in ACO programs on preventive care services, patient experiences, and health care expenditures in U.S. adults aged 18–64. Medical Care 56(8):711–718.
Hsiao, W. C., D. L. Dunn, and D. K. Verrilli. 1993. Assessing the implementation of physician-payment reform. New England Journal of Medicine 328(13):928–933.
Hsu, J., M. Price, J. Spirt, C. Vogeli, R. Brand, M. E. Chernew, S. K. Chaguturu, N. Mohta, E. Weil, and T. Ferris. 2016. Patient population loss at a large Pioneer accountable care organization and implications for refining the program. Health Affairs 35(3):422–430.
Hwang, A., J. Ashburner, C. Hong, W. He, and S. Atlas. 2017. Can primary care physicians accurately predict the likelihood of hospitalization in their patients? American Journal of Managed Care 23:e127–e128.
IOM (Institute of Medicine). 2004. Insuring America’s health: Principles and recommendations. Washington, DC: The National Academies Press.
IOM. 2009. America’s uninsured crisis: Consequences for health and health care. Washington, DC: The National Academies Press.
Jabbarpour, Y., E. DeMarchis, A. Bazemore, and P. Grundy. 2017. The impact of primary care practice transformation on cost, quality, and utilization. Washington, DC: Patient-Centered Primary Care Collaborative, Robert Graham Center.
Jabbarpour, Y., M. Coffman, A. Habib, Y. Chung, W. Liaw, S. B. Gold, H. Jackson, A. Bazemore, and W. D. Marder. 2018. Advanced primary care: A key contributor to successful ACOs. Washington, DC: Patient-Centered Primary Care Collaborative.
Jabbarpour, Y., A. Greiner, A. Jetty, M. Coffman, C. Jose, S. Petterson, K. Pivaral, R. Phillips, A. Bazemore, and A. Neumann Kane. 2019. Investing in primary care: A state-level analysis. Washington, DC: Patient-Centered Primary Care Collaborative.
Jackson, G. L., B. J. Powers, R. Chatterjee, J. P. Bettger, A. R. Kemper, V. Hasselblad, R. J. Dolor, R. J. Irvine, B. L. Heidenfelder, A. S. Kendrick, R. Gray, and J. W. Williams. 2013. The patient centered medical home. A systematic review. Annals of Internal Medicine 158(3):169–178.
Jacobson, M., C. C. Earle, M. Price, and J. P. Newhouse. 2010. How Medicare’s payment cuts for cancer chemotherapy drugs changed patterns of treatment. Health Affairs 29(7):1391–1399.
Kao, A. C., D. C. Green, N. A. Davis, J. P. Koplan, and P. D. Cleary. 1998a. Patients’ trust in their physicians: Effects of choice, continuity, and payment method. Journal of General Internal Medicine 13(10):681–686.
Kao, A. C., D. C. Green, A. M. Zaslavsky, J. P. Koplan, and P. D. Cleary. 1998b. The relationship between method of physician payment and patient trust. JAMA 280(19):1708–1714.
Katz, S., and G. Melmed. 2016. How relative value units undervalue the cognitive physician visit: A focus on inflammatory bowel disease. Gastroenterology & Hepatology 12(4):240–244.
Kelleher, K. J., J. Cooper, K. Deans, P. Carr, R. J. Brilli, S. Allen, and W. Gardner. 2015. Cost saving and quality of care in a pediatric accountable care organization. Pediatrics 135(3):e582–e589.
Kern, L. M., A. Edwards, and R. Kaushal. 2016. The patient-centered medical home and associations with health care quality and utilization: A 5-year cohort study. Annals of Internal Medicine 164(6):395–405.
Kern, L. M., M. Rajan, H. A. Pincus, L. P. Cassalino, and S. S. Stuard. 2020. Health care fragmentation in Medicaid managed care vs. fee for service. Population Health Management 23(1):53–58.
KFF (Kaiser Family Foundation). 2019. An overview of Medicare. San Francisco, CA: Kaiser Family Foundation.
KFF. 2020. Total Medicaid MCO enrollment: 2018. https://www.kff.org/other/state-indicator/total-medicaid-mco-enrollment (accessed November 5, 2020).
Koller, C. F., and D. Khullar. 2017. Primary care spending rate—a lever for encouraging investment in primary care. New England Journal of Medicine 377(18):1709–1711.
Koller, C. F., T. A. Brennan, and M. H. Bailit. 2010. Rhode Island’s novel experiment to rebuild primary care from the insurance side. Health Affairs 29(5):941–947.
Kralewski, J., E. Rich, R. Feldman, B. Dowd, T. Bernhardt, C. Johnson, and W. Gold. 2000. The effects of medical group practice and physician payment methods on costs of care. Health Services Research 35:591–613.
LaBonte, C. T., P. Payne, W. Rollow, M. W. Smith, A. Nissar, P. Holtz, and L. L. Sessums. 2019. Performance on electronic clinical quality measures in the Comprehensive Primary Care Initiative. American Journal of Medical Quality 34(2):119–126.
Laugesen, M. J. 2016. Fixing medical prices: How physicians are paid. Cambridge, MA: Harvard University Press.
Laugesen, M. J., R. Wada, and E. M. Chen. 2012. In setting doctors’ medicare fees, CMS almost always accepts the relative value update panel’s advice on work values. Health Affairs 31(5):965–972.
Lebrun-Harris, L. A., L. Shi, J. Zhu, M. T. Burke, A. Sripipatana, and Q. Ngo-Metzger. 2013. Effects of patient-centered medical home attributes on patients’ perceptions of quality in federally supported health centers. Annals of Family Medicine 11(6):508–516.
Lewis, V. A., A. B. McClurg, J. Smith, E. S. Fisher, and J. P. Bynum. 2013. Attributing patients to accountable care organizations: Performance year approach aligns stakeholders’ interests. Health Affairs 32(3):587–595.
Lopez, E., T. Neuman, and L. Levitt. 2020. How much more than Medicare do private insurers pay? A review of the literature. https://www.kff.org/medicare/issue-brief/how-much-more-than-medicare-do-private-insurers-pay-a-review-of-the-literature (accessed November 5, 2020).
Macinko, J., B. Starfield, and L. Shi. 2007. Quantifying the health benefits of primary care physician supply in the United States. International Journal of Health Services 37(1):111–126.
MACPAC (Medicaid and CHIP Payment and Access Commission). 2011. Section C: Managed care plans. In Report to the Congress: The evolution of managed care in Medicaid. Washington, DC: Medicaid and CHIP Payment and Access Commission. Pp. 41–54.
MACPAC. 2013. Medicaid primary care physician payment increase. In Report to the Congress on Medicaid and CHIP. Washington, DC: Medicaid and CHIP Payment and Access Commission. Pp. 47–60.
MACPAC. 2020. Provider payment and delivery systems. https://www.macpac.gov/medicaid101/provider-payment-and-delivery-systems (accessed October 17, 2020).
Maeng, D. D., J. P. Sciandra, and J. F. Tomcavage. 2016. The impact of a regional patient-centered medical home initiative on cost of care among commercially insured population in the U.S. Risk Management and Healthcare Policy 9:67–74.
Martin, S., R. L. Phillips, Jr., S. Petterson, Z. Levin, and A. W. Bazemore. 2020. Primary care spending in the United States, 2002–2016. JAMA Internal Medicine 180(7):1019–1020.
Martsolf, G. R., J. A. Alexander, Y. Shi, L. P. Casalino, D. R. Rittenhouse, D. P. Scanlon, and S. M. Shortell. 2012. The patient-centered medical home and patient experience. Health Services Research 47(6):2273–2295.
McCall, N., J. Cromwell, and P. Braun. 2006. Validation of physician survey estimates of surgical time using operating room logs. Medical Care Research and Review 63(6):764–777.
McCarty, N. 2013. Complexity, capacity, and capture. In Preventing regulatory capture: Special interest influence and how to limit it, edited by D. Carpenter and D. A. Moss. Cambridge, UK: Cambridge University Press. Pp. 99–123.
McConnell, K. J., S. Renfro, B. K. S. Chan, T. H. A. Meath, A. Mendelson, D. Cohen, J. Waxmonsky, D. McCarty, N. Wallace, and R. C. Lindrooth. 2017. Early performance in Medicaid accountable care organizations: A comparison of Oregon and Colorado. JAMA Internal Medicine 177(4):538–545.
McConnell, K. J., C. J. Charlesworth, T. H. A. Meath, R. M. George, and H. Kim. 2018. Oregon’s emphasis on equity shows signs of early success for black and American Indian Medicaid enrollees. Health Affairs 37(3):386–393.
McCoy, R. G., S. M. Tulledge-Scheitel, J. M. Naessens, A. E. Glasgow, R. J. Stroebel, S. J. Crane, K. S. Bunkers, and N. D. Shah. 2016. The method for performance measurement matters: Diabetes care quality as measured by administrative claims and institutional registry. Health Services Research 51(6):2206–2220.
McCoy, R. G., K. S. Bunkers, P. Ramar, S. K. Meier, L. L. Benetti, R. E. Nesse, and J. M. Naessens. 2018. Patient attribution: Why the method matters. American Journal of Managed Care 24(12):596–603.
McWilliams, J. M., M. E. Chernew, J. B. Dalton, and B. E. Landon. 2014a. Outpatient care patterns and organizational accountability in Medicare. JAMA Internal Medicine 174(6):938–945.
McWilliams, J. M., B. E. Landon, M. E. Chernew, and A. M. Zaslavsky. 2014b. Changes in patients’ experiences in Medicare accountable care organizations. New England Journal of Medicine 371(18):1715–1724.
McWilliams, J. M., L. A. Hatfield, B. E. Landon, P. Hamed, and M. E. Chernew. 2018. Medicare spending after 3 years of the Medicare shared savings program. New England Journal of Medicine 379(12):1139–1149.
Mechanic, D. 1996. Changing medical organization and the erosion of trust. Milbank Quarterly 74(2):171–189.
Mechanic, D., and M. Schlesinger. 1996. The impact of managed care on patients’ trust in medical care and their physicians. JAMA 275(21):1693–1697.
MedPAC (Medicare Payment Advisory Commission). 2006. Report to the Congress: Medicare payment policy. Washington, DC: Medicare Payment Advisory Commission.
MedPAC. 2015. Report to the Congress: Medicare payment policy. Washington, DC: Medicare Payment Advisory Commission.
MedPAC. 2018a. Comment letter to CMS re: File code CMS-1701-P. http://www.medpac.gov/docs/default-source/comment-letters/10152018_aco_2018_medpac_comment_v2_sec283312adfa9c665e80adff00009edf9c.pdf (accessed February 1, 2021).
MedPAC. 2018b. Report to the Congress: Medicare and the health care delivery system. Washington, DC: Medicare Payment Advisory Commmission.
MedPAC. 2019. Report to the Congress: Medicare and the health care delivery system. Washington, DC: Medicare Payment Advisory Commission.
MedPAC. 2020a. A data book: Health care spending and the Medicare program. Washington, DC: Medicare Payment Advisory Commission.
MedPAC. 2020b. Report to the Congress: Fact sheet (updated). Washington, DC: Medicare Payment Advisory Commission.
Mehrotra, A., J. L. Adams, J. W. Thomas, and E. A. McGlynn. 2010. The effect of different attribution rules on individual physician cost profiles. Annals of Internal Medicine 152(10):649–654.
Meltzer, D. O. 2018. The Comprehensive Care Physician Payment Model (CCP-PM). Chicago, IL: The University of Chicago.
Merrell, K., C. Schur, and T. Oberlander. 2014. Analysis of physician time use patterns under the Medicare fee schedule. Washington, DC: Social & Scientific Systems, Urban Institute.
Muhlestein, D., W. K. Bleser, R. S. Saunders, R. Richards, E. Singletary, and M. B. Mcclellan. 2019. Spread of ACOs and value-based payment models in 2019: Gauging the impact of pathways to success. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20191020.962600/full (accessed December 18, 2020).
Mulcahy, A. W., T. Gracner, and K. Finegold. 2018. Associations between the Patient Protection and Affordable Care Act Medicaid primary care payment increase and physician participation in Medicaid. JAMA Internal Medicine 178(8):1042–1048.
Mulcahy, A. W., K. Merrell, and A. Mehrotra. 2020. Payment for services rendered—updating Medicare’s valuation of procedures. New England Journal of Medicine 382(4):303–306.
NAACOS (National Association of ACOs). 2020. State ACO activities. https://www.naacos.com/medicaid-acos (accessed October 17, 2020).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2019a. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press.
NASEM. 2019b. Vibrant and healthy kids: Aligning science, practice, and policy to advance health equity. Washington, DC: The National Academies Press.
Navathe, A. S., E. J. Emanuel, A. Bond, K. Linn, K. Caldarella, A. Troxel, J. Zhu, L. Yang, S. E. Matloubieh, E. Drye, S. Bernheim, E. O. Lee, M. Mugiishi, K. T. Endo, J. Yoshimoto, I. Yuen, S. Okamura, M. Stollar, J. Tom, M. Gold, and K. G. Volpp. 2019. Association between the implementation of a population-based primary care payment system and achievement on quality measures in Hawaii. JAMA 322(1):57–68.
Nicholson, S., and N. S. Souleles. 2001. Physician income expectations and specialty choice. Cambridge, MA: National Bureau of Economic Research.
Nobel, L., W. M. Jesdale, J. Tjia, M. E. Waring, D. C. Parish, A. S. Ash, C. I. Kiefe, and J. J. Allison. 2017. Neighborhood socioeconomic status predicts health after hospitalization for acute coronary syndromes: Findings from TRACE-CORE (transitions, risks, and actions in coronary events-center for outcomes research and education). Medical Care 55(12):1008–1016.
NQF (National Quality Forum). 2019. Attribution: Principles and approaches. Washington, DC: National Quality Forum.
Nurse.org. 2020. 15 highest paying nursing jobs in 2021. https://nurse.org/articles/15-highest-paying-nursing-careers (accessed December 17, 2020).
OECD (Organisation for Economic Co-operation and Development). 2018. Spending on primary care: First estimates. Paris, France: Organisation for Economic Co-operation and Development.
OECD. 2019. Deriving preliminary estimates of primary care spending under the SHA 2011 framework. Paris, France: Organisation for Economic Co-operation and Development.
OECD. 2020. Realising the potential of primary health care. Paris, France: Organisation for Economic Co-operation and Development.
OHA (Oregon Health Authority). 2015. The Oregon Health Authority patient-centered primary care home program: 2014–2015 annual report. Salem, OR: Oregon Health Authority.
OHA. 2019. Primary care spending in Oregon: A report to the Oregon legislature. Salem, OR: Oregon Health Authority.
OHIC (Office of the Health Insurance Commissioner). 2020. Primary care spending data update. Cranston, RI: Office of the Health Insurance Commissioner.
Ouayogodé, M. H., C. H. Colla, and V. A. Lewis. 2017. Determinants of success in shared savings programs: An analysis of ACO and market characteristics. Healthcare 5(1–2):53–61.
Ouayogodé, M. H., E. Meara, C. H. Chang, S. R. Raymond, J. P. W. Bynum, V. A. Lewis, and C. H. Colla. 2018. Forgotten patients: ACO attribution omits those with low service use and the dying. American Journal of Managed Care 24(7):e207–e215.
PAI (Physicians Advocacy Institute). 2020. 2020 Merit-Based Incentive Payment System (MIPS) overview. Raleigh, NC: Physicians Advocacy Institute.
Park, S., J. F. Figueroa, P. Fishman, and N. B. Coe. 2020. Primary care utilization and expenditures in traditional Medicare and Medicare Advantage, 2007–2016. Journal of General Internal Medicine 35(8):2480–2481.
PCC (Primary Care Collaborative). 2018. Fact sheet: Spending for primary care. Washington, DC: Primary Care Collaborative.
Peck, K. A., B. Usadi, A. J. Mainor, E. S. Fisher, and C. H. Colla. 2019. ACO contracts with downside financial risk growing, but still in the minority. Health Affairs 38(7):1201–1206.
Peikes, D., G. Anglin, S. Dale, E. F. Taylor, A. O’Malley, A. Ghosh, K. Swankoski, J. Crosson, R. Keith, A. Mutti, S. Hoag, P. Singh, H. Tu, T. Grannemann, M. Finucane, A. Zutshi, L. Vollmer, and R. Brown. 2018. Evaluation of the Comprehensive Primary Care Initiative: Fourth annual report. Princeton, NJ: Mathematica Policy Research.
Peikes, D., E. F. Taylor, A. S. O’Malley, and E. C. Rich. 2020. The changing landscape of primary care: Effects of the ACA and other efforts over the past decade. Health Affairs 39(3):421–428.
Peiris, D., M. C. Phipps-Taylor, C. A. Stachowski, L. S. Kao, S. M. Shortell, V. A. Lewis, M. B. Rosenthal, and C. H. Colla. 2016. ACOs holding commercial contracts are larger and more efficient than noncommercial ACOs. Health Affairs 35(10):1849–1856.
Perrin, J. M., E. Zimmerman, A. Hertz, T. Johnson, T. Merrill, and D. Smith. 2017. Pediatric accountable care organizations: Insight from early adopters. Pediatrics 139(2):e20161840.
Perrin, J. M., G. M. Kenney, and S. Rosenbaum. 2020. Medicaid and child health equity. New England Journal of Medicine 383(27):2595–2598.
Phillips, R. L., Jr., and A. W. Bazemore. 2010. Primary care and why it matters for U.S. health system reform. Health Affairs 29(5):806–810.
Phillips, R. L., Jr., M. Dodoo, S. Petterson, I. Xierali, A. Bazemore, B. Teevan, K. Bennett, C. Legagneur, J. Rudd, and J. Phillips. 2009. Specialty and geographic distribution of the physician workforce: What influences medical student and resident choices? Washington, DC: Robert Graham Center.
Phillips, R. L., Jr., A. Bazemore, and A. Baum. 2020. The COVID-19 tsunami: The tide goes out before it comes in. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20200415.293535/full (accessed December 18, 2020).
Platonova, E. A., K. N. Kennedy, and R. M. Shewchuk. 2008. Understanding patient satisfaction, trust, and loyalty to primary care physicians. Medical Care Research and Review 65(6):696–712.
Polsky, D., M. Richards, S. Basseyn, D. Wissoker, G. M. Kenney, S. Zuckerman, and K. V. Rhodes. 2015. Appointment availability after increases in Medicaid payments for primary care. New England Journal of Medicine 372(6):537–545.
Pope, G. C., J. Kautter, R. P. Ellis, A. S. Ash, J. Z. Ayanian, L. I. Lezzoni, M. J. Ingber, J. M. Levy, and J. Robst. 2004. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financing Review 25(4):119–141.
Quinn, K. 2015. The 8 basic payment methods in health care. Annals of Internal Medicine 163(4):300–306.
Rama, A. 2017. Payment and delivery in 2016: The prevalence of medical homes, accountable care organizations, and payment methods reported by physicians. Chicago, IL: American Medical Association.
Reddy, A., L. Sessums, R. Gupta, J. Jin, T. Day, B. Finke, and A. Bitton. 2017. Risk stratification methods and provision of care management services in Comprehensive Primary Care Initiative practices. Annals of Family Medicine 15(5):451–454.
Reddy, A., L. M. Marcotte, L. Zhou, S. D. Fihn, and J. M. Liao. 2020. Use of chronic care management among primary care clinicians. Annals of Family Medicine 18(5):455–457.
Reid, R., C. Damberg, and M. W. Friedberg. 2019. Primary care spending in the fee-for-service Medicare population. JAMA Internal Medicine 179(7):977–980.
Reiff, J., N. Brennan, and J. Fuglesten Biniek. 2019. Primary care spending in the commercially insured population. JAMA 322(22):2244–2245.
Reiss-Brennan, B., P. C. Briot, L. A. Savitz, W. Cannon, and R. Staheli. 2010. Cost and quality impact of Intermountain’s mental health integration program. Journal of Healthcare Management 55(2):97–113; discussion 113–114.
Reiss-Brennan, B., K. D. Brunisholz, C. Dredge, P. Briot, K. Grazier, A. Wilcox, L. Savitz, and B. James. 2016. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 316(8):826–834.
Rice, T. H. 1983. The impact of changing Medicare reimbursement rates on physician-induced demand. Medical Care 21(8):803–815.
Robinson, J. C. 2001. Theory and practice in the design of physician payment incentives. Milbank Quarterly 79(2):iii, 149–177.
Rosenbaum, S. 2009. Medicaid payment rate lawsuits: Evolving court views mean uncertain future for Medi-Cal. Sacramento, CA: California Health Care Foundation.
Rosenbaum, S. 2020. Children and Medicaid: Will the courts be there when they need them? Academic Pediatrics 20(2):157–159.
Rosenthal, M., S. Shortell, N. D. Shah, D. Peiris, V. A. Lewis, J. A. Barrera, B. Usadi, and C. H. Colla. 2019. Physician practices in accountable care organizations are more likely to collect and use physician performance information, yet base only a small proportion of compensation on performance data. Health Services Research 54(6):1214–1222.
Rui, P., and T. Okeyode. 2016. National Ambulatory Medical Care Survey: 2016 national summary tables. Atlanta, GA: Centers for Disease Control and Prevention.
Salzberg, C. A., A. Bitton, S. R. Lipsitz, C. Franz, S. Shaykevich, L. P. Newmark, J. Kwatra, and D. W. Bates. 2017. The impact of alternative payment in chronically ill and older patients in the patient-centered medical home. Medical Care 55(5):483–492.
Sarinopoulos, I., D. L. Bechel-Marriott, J. M. Malouin, S. Zhai, J. C. Forney, and C. L. Tanner. 2017. Patient experience with the patient-centered medical home in Michigan’s statewide multi-payer demonstration: A cross-sectional study. Journal of General Internal Medicine 32(11):1202–1209.
Saynisch, P. A., G. David, B. Ukert, A. Agiro, S. H. Scholle, and T. Oberlander. 2021. Model homes: Evaluating approaches to patient-centered medical home implementation. Medical Care 59(3):206–212.
Schlenker, R. E., M. C. Powell, and G. K. Goodrich. 2005. Initial home health outcomes under prospective payment. Health Services Research 40(1):177–193.
Schrager, S. M., K. C. Arthur, J. Nelson, A. R. Edwards, J. M. Murphy, R. Mangione-Smith, and A. Y. Chen. 2016. Development and validation of a method to identify children with social complexity risk factors. Pediatrics 138(3).
Schroeder, S. A., and W. Frist. 2013. Phasing out fee-for-service payment. New England Journal of Medicine 368(21):2029–2032.
Shapiro, S. 2008. Does the amount of participation matter? Public comments, agency responses and the time to finalize a regulation. Policy Sciences 41(1):33–49.
Shi, L. 2012. The impact of primary care: A focused review. Scientifica 2012:432892.
Siddiqui, M., and S. A. Berkowitz. 2014. Shared savings models for ACOs—incentivizing primary care physicians. Journal of General Internal Medicine 29(6):832–834.
Sinaiko, A. D., M. B. Landrum, D. J. Meyers, S. Alidina, D. D. Maeng, M. W. Friedberg, L. M. Kern, A. M. Edwards, S. P. Flieger, P. R. Houck, P. Peele, R. J. Reid, K. McGraves-Lloyd, K. Finison, and M. B. Rosenthal. 2017. Synthesis of research on patient-centered medical homes brings systematic differences into relief. Health Affairs 36(3):500–508.
Song, Z., and S. Gondi. 2019. Will increasing primary care spending alone save money? JAMA 322(14):1349–1350.
Song, Z., S. Rose, M. E. Chernew, and D. G. Safran. 2017. Lower- versus higher-income populations in the Alternative Quality Contract: Improved quality and similar spending. Health Affairs 36(1):74–82.
Song, Z., Y. Ji, D. G. Safran, and M. E. Chernew. 2019. Health care spending, utilization, and quality 8 years into global payment. New England Journal of Medicine 381(3):252–263.
Steinwald, B., P. Ginsburg, C. Brandt, S. Lee, and K. Patel. 2018. Medicare graduate medical education funding is not addressing the primary care shortage: We need a radically different approach. Washington, DC: The Brookings Institution.
Sulmasy, D. P. 1992. Physicians, cost control, and ethics. Annals of Internal Medicine 116(11):920–926.
Takach, M., C. Townley, R. Yalowich, and S. Kinsler. 2015. Making multipayer reform work: What can be learned from medical home initiatives. Health Affairs 34(4):662–672.
Tao, W., J. Agerholm, and B. Burstrom. 2016. The impact of reimbursement systems on equity in access and quality of primary care: A systematic literature review. BMC Health Services Research 16(1):542.
The Larry A. Green Center and PCC (Primary Care Collaborative). 2020. Quick COVID-19 primary care survey: Clinician series 9 fielded May 8–11, 2020. https://www.green-center.org/covid-survey (accessed September 15, 2020).
The Lewin Group. 2015. Health practitioner bonuses and their impact on the availability and utilization of primary care services. Falls Church, VA: The Lewin Group.
Tingley, K. 2018. Trying to put a value on the doctor-patient relationship. The New York Times Magazine. https://www.nytimes.com/interactive/2018/05/16/magazine/health-issue-reinvention-of-primary-care-delivery.html (accessed December 18, 2020).
Trish, E., P. Ginsburg, L. Gascue, and G. Joyce. 2017. Physician reimbursement in Medicare Advantage compared with traditional Medicare and commercial health insurance. JAMA Internal Medicine 177(9):1287–1295.
van den Berk-Clark, C., E. Doucette, F. Rottnek, W. Manard, M. A. Prada, R. Hughes, T. Lawrence, and F. D. Schneider. 2018. Do patient-centered medical homes improve health behaviors, outcomes, and experiences of low-income patients? A systematic review and meta-analysis. Health Services Research 53(3):1777–1798.
Veet, C. A., T. R. Radomski, C. D’Avella, I. Hernandez, C. Wessel, E. C. S. Swart, W. H. Shrank, and N. Parekh. 2020. Impact of healthcare delivery system type on clinical, utilization, and cost outcomes of patient-centered medical homes: A systematic review. Journal of General Internal Medicine 35(4):1276–1284.
Weida, N. A., R. L. Phillips, Jr., and A. W. Bazemore. 2010. Does graduate medical education also follow green? Archives of Internal Medicine 170(4):389–390.
Wen, H., J. M. Hockenberry, and J. R. Cummings. 2014. The effect of substance use disorder treatment use on crime: Evidence from public insurance expansions and health insurance parity mandates. NBER Working Paper Series (Working Paper No. 20537).
Wherry, L. R., M. E. Burns, and L. J. Leininger. 2014. Using self-reported health measures to predict high-need cases among Medicaid-eligible adults. Health Services Research 49(2):2147–2172.
WHO (World Health Organization). 2018. Building the economic case for primary health care: A scoping review. Geneva, Switzerland: World Health Organization.
Wynn, B. O., L. F. Burgette, A. W. Mulcahy, E. N. Okeke, I. Brantley, N. Iyer, T. Ruder, and A. Mehrotra. 2015. Development of a model for the validation of work relative value units for the Medicare physician fee schedule. Santa Monica, CA: RAND Corporation.
Zabar, S., A. Wallach, and A. Kalet. 2019. The future of primary care in the United States depends on payment reform. JAMA Internal Medicine 179(4):515–516.
Zimmerman, E., and S. H. Woolf. 2014. Understanding the relationship between education and health. Discussion Paper, Institute of Medicine, Washington, DC. https://nam.edu/perspectives-2014-understanding-the-relationship-between-education-and-health (accessed April 12, 2021).
Zuckerman, S., and D. Goin. 2012. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. Washington, DC: Kaiser Family Foundation.
Zuckerman, S., K. Merrell, R. A. Berenson, N. Cafarella Lallemand, and J. Sunshine. 2015. Realign physician payment incentives in Medicare to achieve payment equity among specialties, expand the supply of primary care physicians, and improve the value of care for beneficiaries. Washington, DC: Urban Institute, Social & Scientific Systems Inc.
Zuckerman, S., K. Merrell, R. Berenson, S. Mitchel, D. Upadhyay, and R. Lewis. 2016. Collecting empirical physician time data: Piloting an approach for validating work relative value units. Washington, DC: Urban Institute.
Zuckerman, S., L. Skopec, and M. Epstein. 2017. Medicaid physician fees after the ACA primary care fee bump: 19 states continue the Affordable Care Act’s temporary policy change. Washington, DC: Urban Institute.
Zuvekas, S. H., and J. W. Cohen. 2016. Fee-for-service, while much maligned, remains the dominant payment method for physician visits. Health Affairs 35(3):411–414.




















































