3
Building Pathways and Broadening Recruitment (Steps 1 and 2)
HIGHLIGHTS
- Building diverse faculty members begins long before health professions school. (Sánchez)
- Formal pre-faculty development can help recruit, retain, and support diverse practitioners and faculty. (Sánchez)
- There are multiple factors that facilitate or inhibit a person’s decision to pursue a faculty career, including visibility and representation of diverse faculty. (Sánchez)
- It is a professional obligation for faculty to pull others “up the ladder.” (Chappell)
Kathy Chappell introduced the moderator and speaker of the next session, Norma Poll-Hunter, senior director at the Association of American Medical Colleges, and John Paul Sánchez, director of the learning environment fellowship from the University of New Mexico, whose personal and professional experiences guided the participants through steps 1 and 2 of the framework. To begin, said Chappell, the title selected for these steps looks to build an early “pipeline” into health professions education, but it was brought to the attention of the planning committee while preparing for the workshop that a pipeline can be seen as a straight line into the health professions. This may not be indicative of how many from underserved communities find their way into the health professions, which may more resemble a series of “on” and “off-ramps” in career development. This speaks to the fluidity of the framework where building pathways (versus a
pipeline) into education and broadening recruitment—particularly with a lens of diversity, equity, and inclusion—will be incorporated.
PRE-FACULTY DEVELOPMENT: A CRITICAL FACTOR IN DIVERSIFYING HEALTH PROFESSIONS FACULTY
John Paul Sánchez, Health Sciences Center, University of New Mexico
Pre-faculty development is a critical factor in diversifying health professions faculty, said Sánchez, who is also president and founder of Building the Next Generation of Academic Physicians (BNGAP). Building a diverse and inclusive next generation of faculty requires starting early by broadening recruitment and building a pathway to health professions education. There are a number of significant challenges in diversifying health professions faculty, said Sánchez; however, there are also numerous opportunities to engage with students and prepare them to become the faculty of the future.
Sánchez began by reflecting on his own journey to becoming a faculty member. Sánchez is of Puerto Rican ancestry and grew up in the Bronx, New York. During college, Sánchez participated in formal programs that strengthened his academic skills and awareness of professional opportunities, gave him reassurance that he would be valued in becoming a practitioner, and helped him develop a professional portfolio. As a person of color, said Sánchez, these formal programs helped him in attaining his master in public health and his medical degree. Sánchez asked the other workshop participants to reflect on their own journeys and to share in the chat box responses to “When did you first gain formal guidance on becoming an educator or faculty member?” A selection of responses is shown in Box 3-1. Sánchez noted that many of his colleagues and mentors had little formal guidance on the way to becoming faculty members, and that they tend to report the rise to faculty as “serendipitous,” “happenstance,” or “incidental.”
When considering why health professional education has not achieved greater diversity within the faculty workforce, said Sánchez, it is important to reflect on the lack of diversity even within the practitioner workforce. A significant factor in building a diverse faculty is for diverse individuals to first be practitioners, he said. As seen in Tables 3-1 and 3-2, African Americans, Hispanics, and American Indians together make up about 30 percent of the U.S. population; however, the proportion of graduate students, practitioners, and faculty from these groups is significantly lower than 30 percent. Within specific health professions, the disparity is even greater; for example, Hispanics make up around 16 percent of the U.S. workforce, but only 3.7 percent of pharmacists and chiropractors are Hispanic (HRSA, 2017).
Sánchez said there are two significant disparities that need attention: one, representation within practitioner ranks, and two, representation within faculty ranks. Faculty are critical in many ways, said Sánchez, because they serve as role models and mentors to students and new professionals, they are champions for programs and policies, and they sit on admissions and other important committees. Sánchez asked “What factors influence an individual’s trajectory to a faculty career, particularly diverse individuals?” Poll-Hunter, who works within AAMC’s Diversity Policy and Programs unit, quickly scanned the responses for the most common
TABLE 3-1 U.S. Health Occupations by Race/Ethnicity, 2011–2015
| Hispanic | ||
|---|---|---|
| White | ||
| U.S. Workforcea (#) | 25,776,728 | 102,850,895 |
| U.S. Workforcea (%) | 16.1 | 64.4 |
| Health Occupationsb (%) | ||
| Community and Social Services Occupations | ||
| Counselors | 10.7 | 64.6 |
| Social Workers | 12.0 | 60.6 |
| Life, Physical, and Social Sciences Occupations | ||
| Psychologists | 6.3 | 83.5 |
| Health Diagnosing and Treating Practitioners Occupations | ||
| Advanced Practice Registered Nursesc | 4.5 | 84.0 |
| Chiropractors | 3.7 | 86.7 |
| Dentists | 6.1 | 74.8 |
| Dietitians and Nutritionists | 8.5 | 68.7 |
| Optometrists | 3.9 | 78.4 |
| Pharmacists | 3.7 | 70.4 |
| Physicians | 6.3 | 67.0 |
| Physician Assistants | 10.0 | 72.7 |
| Occupational Therapists | 4.0 | 83.8 |
| Physical Therapists | 4.8 | 77.8 |
a Population 16 years and older who are employed or seeking employment.
b Self-reported occupations.
c Includes nurse anesthetists, midwives, and nurse practitioners.
NOTES: Occupations are titled and grouped as in the U.S. government’s Standard Occupation Classification system. NR = data not reported because relative standard errors (RSE) > 30; estimate does not meet standards of reliability or data not present. Numbers in parenthesis represent estimates with relative standard errors (RSE) > 20 percent and should be interpreted with caution. Not all totals equal to 100 percent due to rounding.
SOURCES: Presented by Sánchez, August 11, 2020; HRSA Sex, Race, and Ethnic Diversity of U.S. Health Occupations (2011–2015) 2017 Report.
| Non-Hispanic | ||||
|---|---|---|---|---|
| Black | Asian | American Indian/Alaska Native | Native Hawaiian and Other Pacific Islander | Multiple/Other Race |
| 18,597,223 | 8,534,837 | 902,977 | 251,578 | 2,910,645 |
| 11.6 | 5.3 | 0.6 | 0.2 | 1.8 |
| 18.8 | 2.8 | 0.8 | 0.1 | 2.2 |
| 21.5 | 3.0 | 0.8 | 0.1 | 2.0 |
| 4.9 | 3.4 | 0.2 | (0.0) | 1.6 |
| 5.7 | 4.1 | 0.2 | NR | 1.3 |
| 1.9 | 5.4 | 0.5 | NR | 1.8 |
| 3.0 | 14.3 | (0.1) | NR | 1.7 |
| 15.0 | 6.0 | 0.3 | (0.1) | 1.4 |
| 1.8 | 13.7 | NR | NR | 1.8 |
| 5.9 | 17.9 | 0.2 | 0.1 | 1.8 |
| 4.8 | 19.6 | 0.1 | 0.0 | 2.1 |
| 7.1 | 7.3 | 0.6 | NR | 2.2 |
| 4.4 | 6.6 | 0.2 | NR | 1.1 |
| 4.4 | 11.1 | 0.2 | (0.1) | 1.6 |
TABLE 3-2 Approximate Hispanic, African American/Black, and American Indian/Alaska Native Population and U.S. Workforce Demographics by Discipline, 2015
| Population % | Graduate Students % | Clinicians % | Faculty % | |
|---|---|---|---|---|
| Physician Assistant | 30 | 10 | 11 | 10 |
| Medicine | 30 | 15 | 10 | 7 |
| Dentist | 30 | 12 | 7 | 15 |
NOTE: American Indian or Alaska Native plus Native Hawaiian and Other Pacific Islanders for data of census, graduates, and faculty.
SOURCES: Presented by Sánchez, August 11, 2020; AAMC, 2020; NCCPA, 2020; U.S. Census Bureau, 2020.
themes, which included mentorship, sponsors, seeing diverse faculty as role models, academic advisors, and leadership (see Box 3-2). These responses highlighted the importance of the role of others in either identifying or inspiring individuals to pursue faculty careers.
Given the responses of the workshop participants, Sánchez noted that “the problem is definitely multifactorial.” He shared two frameworks to help elucidate the various factors that contribute to recruitment, retention, and success of faculty. The first was an adaptation of a framework on social determinants of health (see Figures 3-1a and 3-1b), which Sánchez called “determinants of health in academia.” The second framework was a modified model of social cognitive career theory, and it includes factors that influence a person’s career decision making (see Figure 3-2). Sánchez shared anonymous quotes from three potential faculty members that illuminate some of the factors that may prevent diverse students from considering faculty careers:
- Self-doubt about being good enough: “I don’t know that my grades are as stellar as they should be because I picture an academic teacher
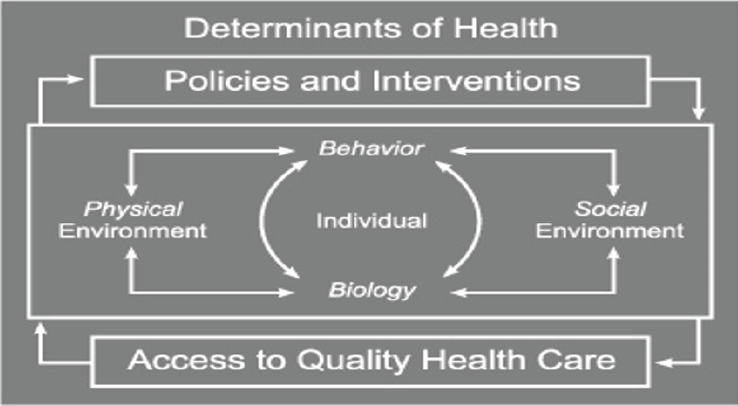
SOURCES: Presented by Sánchez, August 11, 2020; adapted from Satcher and Higginbotham, 2008.
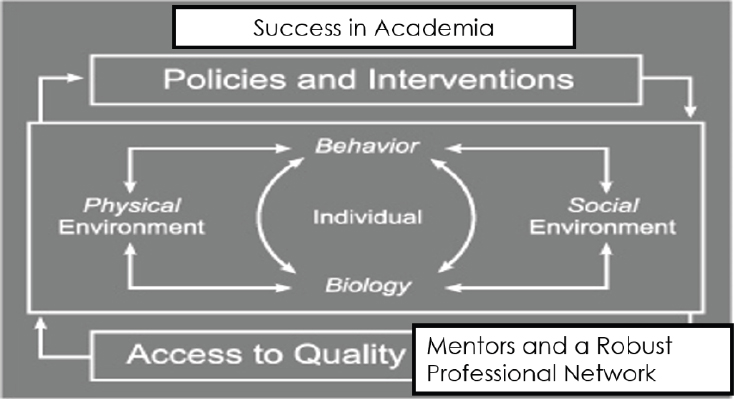
SOURCES: Presented by Sánchez, August 11, 2020; adapted from Satcher and Higginbotham, 2008.
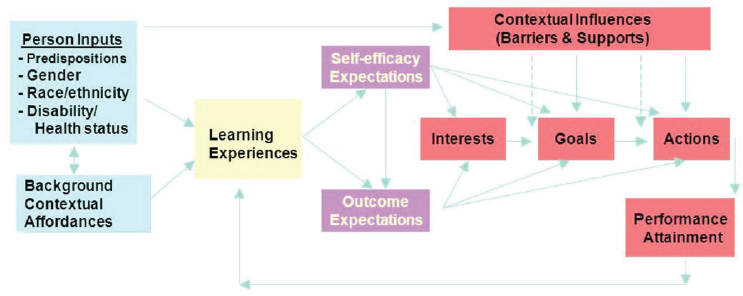
SOURCES: Presented by Sánchez, August 11, 2020; adapted from Lent et al., 1994.
- as somebody with excellent grades and I’m just kind of a floater. I’m not really someone who stands out academically. I mean, obviously we all stand out as medical students, but among those I’m pretty average. I would love to do it, but I don’t think I have the research or the academic excellence” (Sanchez et al., 2013).
- Parents’ view of clinical versus faculty careers: “I think a lot of people in our parents’ generation, especially among Asian immigrants, see clinical practice as the ‘iron rice bowl.’ Basically, once you get the training, you can keep on eating out of it with a steady income and steady job” (Zhang et al., 2017).
- Difficulty finding LGBT mentors: “I haven’t had any mentors, and I feel like because I lack that, I kind of want to provide support later on. There are no mentors who do research or teaching in LGBT health or who are out or who are supporting or very supportive of people who might be out in academic medicine” (Sanchez et al., 2015).
Sánchez then stated:
If we’re serious about diversifying our faculty workforce, if we’re serious about creating equitable processes in the recruitment, retention, and promotion of our faculty, and if we’re serious about creating a sense of belonging, attention must be paid to pre-faculty development.
Sánchez defined pre-faculty development as providing potential faculty with “foundational self-efficacy, knowledge, skills, and experiences to be successfully appointed, and eventually promoted and tenured, within an academic institution” (Sánchez and Williams, 2020). Sánchez asked
workshop participants to reflect on what types of formal pre-faculty development programs were a part of their journey. Poll-Hunter scanned the responses in the chat box and noted that the common theme among them was there are “not a lot of resources for pre-faculty development.” Sánchez agreed with this assessment, and said that he never had formal pre-faculty development, despite having served in various faculty positions and as a dean. As a consequence, it is extremely gratifying for Sánchez to help his trainees and to give them a better experience than he had.
Sánchez told participants about his organization—Building the Next Generation of Academic Physicians (BNGAP, 2020)—that is aimed at supporting pre-faculty development. The mission of BNGAP is to “help diverse trainees become aware of, interested in, and prepared to explore academic careers.” The group started by engaging with diverse trainees to understand the perceived challenges and facilitators to becoming future faculty, said Sánchez. The information that was gathered served to develop educational interventions to support a diverse pre-faculty workforce and to help build a pre-faculty identity for trainees. At each step of the way, the organization assesses outcomes and effects. BNGAP originally focused on medicine, but it has been adapted for dentistry, nursing, pharmacy, and public health.
Three concepts have emerged through the work of BNGAP, Sánchez said. First, it is critical to build community through conferences, chapters, newsletters, and by identifying role models and mentors who can connect with pre-faculty to keep them on track. One community-building entity, said Sánchez, is the BNGAP National Center for Pre-Faculty Development, which is a resource for networking and sharing best practices. Second, BNGAP seeks to address and dispel misconceptions about being a diverse faculty member. One example is the “minority tax” (extra responsibilities placed on minority faculty in the name of diversity);1 BNGAP encourages trainees to transform this “tax” into “capital” by seeking writing fellowships or publishing opportunities. Finally, BNGAP helps trainees build career knowledge and skills through curricula that have been developed. There are curricula aimed at a variety of audiences ranging from college students to graduate students to those finding their first faculty position. Sánchez added that it is not only critical to encourage trainees to become faculty, but also to become deans and chairs of departments.
In closing, Sánchez encouraged workshop participants to take three steps after the workshop. First, keep talking about pre-faculty development, with colleagues, leaders, and trainees. Second, he encouraged collaboration to build formal, interprofessional pathway programs for a diverse pre-faculty. Third, he asked participants to “turn to a diverse trainee” and tell
___________________
1 See https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-015-0290-9 (accessed December 9, 2020).
them, “I want you to be a future faculty member. I am here to answer any questions that you may have, and I’m going to tell you how great it is to be a faculty member.” Sánchez encouraged participants to reach out to trainees to make them aware of potential faculty careers, to cultivate their interest in education, and to recognize the work they already do as educators. This type of conversation, said Sánchez, was fundamental for his journey, and it “does not require funding or protected time, and it is something really easy that we can all do.” Chappell agreed with Sánchez, and added that at a certain point in a professional’s career, it is a “professional obligation to reach back and pull somebody up the ladder.”
REFERENCES
AAMC (Association of American Medical Colleges). 2020. Medical education facts: Applicants, matriculants, enrollment, graduates, MD-PhD, and residency applicants data. https://www.aamc.org/data-reports/students-residents/report/facts (accessed December 15, 2020).
BNGAP (Building the Next Generation of Academic Physicians). 2020. About BNGAP. http://bngap.org/about-us (accessed December 15, 2020).
HRSA (Health Resources and Services Administration). 2017. HRSA Sex, Race, and Ethnic Diversity of U.S. Health Occupations (2011–2015) 2017 Report. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/diversity-us-health-occupations.pdf (accessed December 15, 2020).
Lent, R. W., S. D. Brown, and G. Hackett. 1994. Toward a unifying social cognitive theory of career and academic interest, choice, and performance. Journal of Vocational Behavior 45(1):79–122.
NCCPA (National Commission on Certification of Physician Assistants). 2020. Reports. https://www.nccpa.net/news-press.aspx?id=63&page=1&category=2&newsPressYear=2020 (accessed December 15, 2020).
Sánchez, J. P., and V. N. Williams. 2020. Introduction. In Succeeding in academic medicine: A roadmap for diverse medical students and residents, edited by J. P. Sánchez. Cham, Switzerland: Springer Nature. P. viii. https://doi.org/10.1007/978-3-030-33267-9.
Sánchez, J. P., L. Peters, E. Lee-Rey, H. Strelnick, G. Garrison, K. Zhang, D. Spencer, G. Ortega, B. Yehia, A. Berlin, and L. Castillo-Page. 2013. Racial and ethnic minority medical students’ perceptions of academic medicine careers. Academic Medicine 88(9):1299–1307.
Sánchez, N., S. Rankin, E. Callahan, H. Ng, L. Holaday, K. McIntosh, N. Poll-Hunter, and J. P. Sánchez. 2015. LGBT health professionals perspectives on academic careers—Facilitators and challenges. LGBT Health 2(4):346–357. https://pdfs.semanticscholar.org/5aa5/b29ff7a4c387ffd782147f302c55bc8d373a.pdf (accessed December 15, 2020).
Satcher, D., and E. J. Higginbotham. 2008. The public health approach to eliminating disparities in health. American Journal of Public Health 98(9 Suppl):S8–S11.
U.S. Census Bureau. 2020. Explore data. https://www.census.gov/data.html (accessed December 15, 2020).
Zhang, L., Lee, E. S., Kenworthy, C. A., Chiang, S., Holaday, L., Spencer, D. J., Poll-Hunter, N. I., & Sánchez, J. P. 2017. Asian medical students’ perceptions of careers in medicine. Journal of Career Development 46(3):235–250. https://doi.org/10.1177/0894845317740225 (accessed December 27, 2020).










