5
A Systems Approach to Increasing Vaccine Confidence and Uptake: Opportunities in Research, Communication, Legislation, and Technology
The third session of the workshop focused on how a systems approach can be employed to build vaccine confidence and increase uptake. The objective of the first half of the session was to explore opportunities in research, communication, legislation, and technology in influencing vaccine behavior, improving access, and building confidence in immunization practices. Dorit Reiss, professor of law at the University of California Hastings College of the Law, presented on legal approaches to promoting parental compliance with childhood vaccines. Michelle Mello, professor of law and medicine at Stanford University, explored lessons learned from California’s elimination of nonmedical vaccination exemptions. Dan Carucci, global medical director at McCann Health, presented on the Immunity Charm project, which harnessed cultural insights to promote vaccination. Todd Wolynn, chief executive officer at Kids Plus Pediatrics, presented on the role of physicians in building vaccine confidence and countering anti-vaccine attacks. Sean O’Leary, associate professor at the University of Colorado Denver, presented on strategies for health care providers to engage with vaccine-hesitant parents using face-to-face communication, participatory conversations, and motivational interviewing. The panel was moderated by Chandy C. John from the Indiana University School of Medicine.
LEGAL APPROACHES TO PROMOTE PARENTAL COMPLIANCE WITH CHILDHOOD VACCINES IN THE UNITED STATES
Presented by Dorit Reiss, University of California Hastings College of the Law
Reiss provided an overview of legal approaches to promote parental compliance and increase access to vaccines to help improve childhood vaccination rates in the United States. She discussed existing immunization laws, the state of children’s rights with regard to vaccines, legal tools for immunization coverage and school mandates, and the role of government in regulating against misinformation.
Existing Immunization Laws in the United States
Reiss described the interplay of existing federal- and state-level immunization laws in the United States. The U.S. federal government’s role in promoting vaccination rates is primarily a supportive and enabling role rather than coercive. The federal government does not—and likely could not—mandate vaccination, but it currently plays several roles in increasing vaccination rates. Although the Commerce Clause is one of the tools used by the federal government to regulate public health, it probably would not allow for a federal childhood vaccine mandate. The federal government can use spending power to encourage state-level vaccination mandates, but such incentives must not be coercive within established limits. Reiss described three roles that the federal government plays in promoting vaccination: (1) increasing access to vaccines for families through the Vaccines for Children Program;1 (2) setting vaccine schedules, recommendations, and messaging; and (3) ensuring informed consent through vaccine information statements, which are official documents that establish information about vaccines for use by other entities.
Reiss explained that the power to regulate vaccine compliance in the United States primarily lies with the states. States have broad leeway to use the law to increase vaccination in ways that are not being optimally leveraged, however. States have broad regulatory power in the area of childhood vaccines because vaccination lies at the intersection of two plenary powers of the state—police powers and the parens patriae doctrine. The police power of states to regulate public health has been acknowledged since before the 19th century. The power of states to regulate child vaccination is further affirmed by states’ parens patriae power, which gives states the power to pro-
___________________
1 More information about the Vaccine for Children Program is available at https://www.health.pa.gov/topics/programs/immunizations/Pages/VFC.aspx (accessed October 9, 2020).
tect the vulnerable. The combination of these powers creates a strong legal sphere, she noted. States have primarily regulated childhood vaccination through school immunization requirements and adult vaccination through workplace immunization requirements, but Reiss emphasized that states have many other tools available.
Children’s Rights and Childhood Vaccines
In more than 100 years of contentious jurisprudence on the issue, Reiss pointed out that no state or federal court has ever struck down an immunization mandate. When U.S. courts evaluate school immunization mandates and other vaccination laws, they use a framework to balance various rights and interests including parental autonomy, children’s rights, the individual rights of others, and overall community health. With respect to parental autonomy, courts recognize that parents have the right to make decisions in the interest of their child. Given the relatively favorable risk/benefit tradeoffs associated with vaccination, she noted a strong argument can be made in favor of children’s right to be vaccinated to the fullest extent medically possible. Additionally, the rights of individuals may be infringed upon if they are infected by an unvaccinated child who contracts a preventable disease. These considerations are bolstered by the states’ extensive power to take action to prevent the spread of disease. Together, these considerations are balanced against the consideration of parental autonomy alone. She said that in the eyes of the court, a parent’s resistance to vaccination puts not only their child but the community in general at risk, which is not a strong position. In this sense, the rights of other families’ interests, the child’s rights, and public health can outweigh parental autonomy.
Reiss considered whether the right to religious freedom tips the balance of these considerations. She described two reasons that rights of religious freedom are not barriers to childhood vaccination regulations. First, under Supreme Court jurisprudence, a mutually generally applicable law is not required to have a religious exemption. Because school immunization requirements are generally applicable (i.e., they do not target members of particular religions), they are not required to have religious exemptions. Second, the legal consideration of religious freedom rights is reduced in matters related to children because children do not make their own decisions. Parents cannot use their rights of religious freedom to put their children and others at risk.
School Immunization Mandates and Requirements in the United States
States have a broad set of actions at their disposal to help increase vaccination rates, but Reiss said school immunization mandates are the most
commonly used throughout the United States because they are legally sound and effective. School immunization mandates have been used in the United States since at least the 19th century, and every state currently has school immunization requirements. Reiss explained that some states offer medical exemptions only; some offer medical and religious exemptions only; and some offer medical, religious, and personal belief exemptions. As of August 2020, just five U.S. states offered only medical exemptions: California, Maine, Mississippi, New York, and West Virginia. Other states are considering such a policy but have not yet passed legislation. Every other state allows some degree of nonmedical exemptions on the basis of personal beliefs or religious beliefs, although the ease of obtaining such an exemption varies between states.
Reiss noted that many of the other tools available to states are less coercive than school immunization mandates, which limit access to schooling based on children’s immunization status. To explore options for broadening the scope of state-level activities in this domain, she presented the suite of legal tools for promoting vaccination on a continuum of coerciveness. Progressing from most coercive to least coercive, these tools include use of force, criminal law, conditioned access, cost internalization, mandated transparency, procedural tightening, positive incentives, and persuasion through education. Reiss said that many schools report data on immunization rates, but few states require schools to do so. Colorado has adopted a moderate vaccine policy that requires schools to send school immunization rates to parents. This policy is less coercive toward the individual parent, but it may help parents make informed choices. Laws that impose tort liability when non-vaccination causes harm are an example of a less directly coercive mandate available to states. Similarly, increasing access to immunizations through laws that allow minors to make their own vaccination choices is another non-coercive approach.
The Government’s Role in Regulating Against Misinformation
Reiss described opportunities for government action that could help curb disinformation around vaccines. The government has broad powers for messaging and making recommendations,2 but its power to regulate speech is limited by the right to freedom of speech granted by the First Amendment of the U.S. Constitution. However, this right is not absolute, and speech is in fact regulated constantly. For instance, commercial speech is widely regulated. Demonstrably false commercial speech can be and is prohibited
___________________
2 Reiss suggested that the government could better use these powers. For instance, government bodies could make statements about vaccine safety oversight during COVID-19 vaccine trials.
by the federal government. Furthermore, many states have consumer protection acts that regulate misinformation in both the commercial and nonprofit sectors. Thus, false information can, in theory, be regulated regardless of whether it comes from the commercial sector or not. Central Hudson Gas & Electric Corporation v. Public Service Commission of New York3 is the central leading case in public health about prohibiting speech, and it holds that false or misleading speech is not protected. However, Reiss pointed out this precedent is not as strong as it seems. First, there are risks involved in allowing government to directly arbitrate the truth of potentially misleading speech, because speech can be misleading in subtle ways. For instance, the National Vaccine Information Center, an anti-vaccine organization, posts the number of reports in the Vaccine Adverse Event Reporting System (VAERS) for every vaccine. These posts are truthful, but they can be misleading in that the VAERS reports are not sufficient to establish causation and do not necessarily reflect vaccine risk. Therefore, this type of speech is misleading, but it is not quite untruthful. Reiss described this example as highlighting the limits of the government’s power to regulate misinformation by acting only against false statements.
IMPACT OF ELIMINATING NONMEDICAL EXEMPTIONS IN CALIFORNIA
Presented by Michelle M. Mello, Stanford University Law School
Mello explored the effect of California’s elimination of nonmedical exemptions within its school immunization mandate. She discussed the nature of California’s legislation, the effects of California’s new exemption laws, and lessons learned from California’s experience that may inform other states pursuing such legislation.
Changes to California Immunization Exemption Laws (2014–2021)
Changes to California’s vaccination law have been unfolding gradually since 2014. Prior to then, Mello explained, California had a personal belief exemption that also incorporated religious belief exemptions. Assembly Bill (AB) 2109, which went into effect January 1, 2014, was aimed at reducing the use of these exemptions by imposing certain procedural requirements for obtaining them. The bill required that parents submit a health care provider’s testimony that the parent was counseled about the risks and benefits of the
___________________
3 More information about Central Hudson Gas & Electric Corporation v. Public Service Commission of New York is available at https://www.oyez.org/cases/1979/79-565 (accessed October 12, 2020).
relevant immunizations and communicable diseases when submitting their personal belief exemptions to the California Department of Public Health. This change did not successfully bring about a substantial decrease in exemptions, so the legislature subsequently adopted a stronger policy. Senate Bill (SB) 277, passed in 2015 and effective as of January 1, 2016, eliminated California’s personal belief exemption, making medical exemptions the only permissible basis for forgoing required vaccines. Mello said that SB277 allowed these exemptions to be written by any licensed physician for any medical reason, including simply “family medical history,” because the bill did not require that a specific medical reason be cited. SB277 applied to students in public and private elementary and secondary schools, day care centers, and youth development centers. However, it did not apply to students attending home-based private schools, students enrolled in independent study programs with no classroom instruction, or students with individualized education programs who would be barred from accessing related services. The bill also allowed children with personal belief exemptions filed within 6 months of the bill’s passage to continue in school until the next grade span began (e.g., kindergarteners could continue until seventh grade). These loopholes resulted in a substantial number of children obtaining exemptions. The legislature responded again, passing SB276 in 2020. Effective as of January 1, 2021, SB276 tightens the conditions under which medical exemptions can be written (see Box 5-1).
Effect of California’s Changes to Immunization Exemption Laws
The impacts of these bills have been well studied, said Mello (Delamater et al., 2019, 2020; Mohanty et al., 2018). These effects can be categorized into three groups: (1) effects on the any-exemption rate; (2) effects on the percentage of kindergarteners who are fully up to date on required vaccinations; and (3) effects on the rate of medical exemptions. Projections of the overall impact of SB277 and SB276 between 2015 and 2027 suggest that SB277 alone would decrease the number of children with any exemption from 2.59 percent to 1.87 percent during that period; the addition of SB276 is expected to further reduce the any-exemption rate to 1.41 percent by 2027 (Delamater et al., 2020). The authors of that analysis concluded that overall, SB277 had a modest effect on exemption rates. In the 2 years following the passage of SB277 in 2015, the percentage of up-to-date kindergarteners increased from 92.8 percent to 95.1 percent. Mello said that the increase in the percentage of up-to-date kindergarteners is a key effect of this legislation, because it has put the state over the threshold for herd immunity to measles, which has been a major issue in California since 2015. Still, the rates of medical exemptions had increased fourfold in the state in 2019, 4 years after SB277 was passed. Although the exemption rate among children in Califor-
nia was low (0.2 percent) in 2015, it represents a large relative increase if not a large absolute increase. This increase in exemptions was concentrated among a small number of physicians, which has raised concerns about the validity of medical exemptions. A small number of medical providers seem to be offering exemptions widely, and there is some concern that certain physicians (especially those not in relevant specialties) may be selling these certifications through Internet outreach. Mello noted these were among the concerns that motivated the passing of SB276.
Review of the Effect of State Vaccination Exemption Laws
Mello highlighted four conclusions from a systematic review of research on the effects of state vaccination exemption laws (Wang et al., 2014). First, states without nonmedical exemptions have lower rates of vaccination exemptions and vaccine-preventable diseases than states with such exemp-
tions. Second, the ease of obtaining exemptions is associated with higher exemption rates and disease outbreak risk. California’s experience with the physician counseling requirement notwithstanding, this suggests that the imposition of additional paperwork, for instance, should have an effect on risk of outbreak and exemption rates in a state. Third, even though the overall reductions in exemption rates may be modest in absolute terms, small reductions in exemption rates translate into large numbers of additional children vaccinated. For instance, if the projected reduction in exemptions in California are realized, reducing to 1.41 percent by 2027 (Delamater et al., 2020), that would result in an additional 84,000 children being up to date in their vaccinations. This would have a large effect, she said, especially considering that exempted children are not evenly distributed geographically across California. Rather, the areas with initially high localized exemption rates would see the most substantial improvement. Prior to the passage of SB277, approximately one-quarter of California’s kindergartens had immunization rates too low to achieve herd immunity for highly infectious diseases such as measles. This, she pointed out, demonstrates the critical importance of even small decreases in exemption rates. Fourth, if vaccination exemption laws leave open avenues for avoiding vaccination, parents opposed to vaccination will always find ways to do so.
Lessons Learned from California’s Experience
Mello described lessons learned from California’s experience in eliminating nonmedical exemptions. Chief among these is the importance of avoiding loopholes and large compromises in the scope of the law. For example, SB277 was passed with a grandfather clause that allowed parents to get exemptions for their children during a 6-month period after the passage of the law, which did not go into effect for nearly 1 year after its passage. This gave parents a substantial opportunity to avoid the law’s intended effect. Mello recommended that other states avoid such grandfather clauses. Additionally, SB277 allowed physicians to write medical exemptions for any reason, rather than exclusively requiring a valid and recognized contraindication to vaccination. Mello recommended that other states limit the basis for a medical exemption to only valid, medically recognized contraindications, rather than allowing for vaguely articulated reasons such as “family history.” California also initially allowed medical exemptions to be written by any health provider, regardless of their history with the child or their relevant expertise on vaccination. SB276 attempted to address some of these issues, but it was too late to address the challenges associated with the grandfather clause in SB277. Even now, California law does not require that the exemption be written by a child’s primary care physician; it merely imposes an additional explanation when the exemption is written by a physician
other than the child’s primary pediatrician. Instead, Mello explained, states should require that medical exemptions come from a pediatrician or family physician who the child sees for regular care. Mello added that it is not clear what the California Department of Public Health is going to do with information collected about why a physician other than a child’s pediatrician has submitted a child’s exemption.
Mello shared additional lessons that are relevant to other states pursuing this approach. Other states have chosen to adopt incremental legislation, despite the obvious flaws in this approach as exemplified by the shortcomings of SB277. She suggested that through these incremental bills, legislators may be hoping to first demonstrate that tightening exemption policies is effective for increasing vaccination before passing additional laws to address the flaws and loopholes in their initial policies. In Mello’s opinion, this approach is misguided because those who resist the initial laws are unlikely to be convinced or cease their efforts to resist vaccination upon seeing the effectiveness of the incremental policies. The opposition to tightening vaccination exemptions is likely to remain, so passing subsequent updates to exemption policies will likely be as difficult as passing initial incremental policies. She noted that there was great resistance to the passage of SB276, which culminated in an incident where anti-vaccination activists threw human blood onto the Senate gallery while the bill was being debated and physically assaulted one of the bill’s proponents. Mello said that this incident is an example of why exemption-tightening bills should be designed in a way that makes them more likely to be effective. She advised that states seeking to reduce vaccination exemptions should address the appropriate details from the outset to preclude the need for further legislation. States should also expect anti-vaccination groups to mobilize to help parents take advantage of loopholes in new requirements.
Mello also shared some aspects of California’s approach that serve as useful models for other states’ exemption-tightening policies (Mello, 2020). California’s legislation is broad in scope, eliminating all nonmedical exemptions and creating evenhanded rules that apply to private schools and day care centers, not just public schools. Additionally, California set forth a specific but comprehensive list of required immunizations.4 She suggested that states follow California’s lead in including provisions in their legislation that require annual data on school-level exemption rates to be made public. Such provisions empower parents to pressure schools and health departments to remain vigilant in enforcing exemption policies. Finally, Mello recommended
___________________
4 Mello contrasted this approach with that used by Washington State, where legislators focused on the measles, mumps, and rubella vaccine during a measles outbreak. She pointed out that because of the narrow scope of its law, Washington legislators will face the same issues and challenges again whenever an outbreak of another vaccine-preventable disease occurs.
that states’ exemption-tightening policies task departments of health (rather than schools) with reviewing medical exemptions, and that departments of health be empowered to take action against “frequent flyers” (i.e., physicians who write a large number of exemptions).
HARNESSING CULTURAL INSIGHTS TO INCREASE VACCINATION UPTAKE
Presented by Daniel Carucci, McCann Health
Carucci discussed the Immunity Charm project as an example of how cultural insights can be harnessed to increase vaccination uptake. The project was developed by McCann Health in its efforts to increase vaccine uptake as part of its commitment to apply its expertise in marketing and advertising to efforts to increase the impact of global health investments. He noted that McCann’s work on vaccination has focused on the demand side, developing creative ways to drive vaccine uptake in underserved and underdeveloped parts of the world. The development of the Immunity Charm project began when McCann Health was working with the Afghanistan Ministry of Public Health through a United Nations Children’s Fund (UNICEF) program to improve health communication strategies across the country through ministry programs.
Drivers of Underimmunization and the Need for Increased Vaccine Demand
Carucci spoke on the benefits of childhood immunizations and the potential for further improvements. Vaccines save the lives of an estimated 2–3 million children each year worldwide, but higher immunization rates could save the lives of an additional 1.5 million children if they received the vaccines they need and completed their full vaccine schedule.5 Although national statistics show improving vaccine coverage, there remain large regional coverage gaps. He remarked that “childhood immunizations … are arguably one of the most powerful and effective health interventions we have to reduce childhood mortality.”
Carucci presented an analysis of factors driving underimmunization, which he categorized as either access-related factors or demand-related factors. The five factors reducing access include lack of supply, poor distribution chain, conflict areas, inaccessibility, and poor logistics. He acknowledged
___________________
5 More information about how vaccinating the world’s children can save 1.5 million lives is available at https://www.unicefusa.org/stories/how-save-15-million-lives-year-vaccinateworlds-children/31793 (accessed October 13, 2020).
that international organizations such as UNICEF and Gavi, the Vaccine Alliance, have helped improve vaccine coverage with efforts that have increased access to vaccines. Despite these improvements, lack of access remains a factor in preventing children from receiving the vaccines they need, especially issues related to supply chains, distribution chains, logistics, and other technical problems. He noted that large regional gaps in immunization coverage remain even in settings where vaccines have become more accessible. These regional gaps may be attributable to lack of demand, because far too many parents fail to appropriately prioritize their children’s vaccinations. He listed five factors that suppress parental demand for childhood immunization: myths, misperceptions, indifference, ignorance, and illiteracy. He suggested that many parents do not bring their children to clinics for vaccination on the appropriate schedule largely because of these demand-related factors.
In areas where access is not a primary driver of underimmunization, increasing demand is critical for improving vaccination uptake and compliance. Carucci discussed underimmunization as a demand-driven problem that can be addressed by considering how young mothers perceive the value of childhood vaccinations. Young mothers often struggle with many life stresses, and their children’s vaccinations are often not prioritized. Mothers must choose to devote substantial time and resources to have their children vaccinated, but they will not make that choice unless they see immunization as a high priority. Carucci emphasized that a compelling and emotional message is needed to show mothers that vaccines are necessary to protect their children from serious illnesses so that they can grow up to be strong and healthy.
Increasing the Perceived Value of Childhood Vaccines with the Immunity Charm
Throughout South Asia, a simple bracelet is used as a symbol of protection against evil spirits, Carucci explained. Mothers and grandmothers often provide these bracelets to their children in early infancy, often adorned with a nazar (i.e., evil eye) charm as an additional form of protection. These bracelets can be found across socioeconomic classes and educational levels not only in South Asia, but in other communities as well, such as in Africa. Based on this cultural practice, McCann Health created the Immunity Charm, a bracelet that has the potential to increase vaccination uptake and compliance, potentially saving millions of children’s lives each year. In developing the project, they sought to associate existing cultural symbolism—bracelets as powerful symbols of protection against unknown forces—with the protection afforded by vaccines against serious disease. The Immunity Charm is a bracelet made of black thread with a screw closure; it comes preloaded with a nazar charm and a series of black beads (see Figure 5-1). Colored beads
representing each of the vaccines associated with the World Health Organization’s (WHO’s) Expanded Program on Immunization are added to the bracelet at the time of immunization.6 Thus, the Immunity Charm is also an immunization history that is worn by the child, and each new colored bead represents an additional level of protection against disease.
Response to the Immunity Charm Project
McCann conducted a small qualitative project in Kabul to assess the acceptability of the bracelet among health care staff and mothers attending a vaccine clinic, said Carucci. His team found that the bracelet was readily acceptable to mothers and health care workers at the immunization clinic. In fact, the bracelets were so popular that McCann encountered difficulties securing sufficient inventory. He reported that the overall response to the Immunity Charm was overwhelmingly positive from both health care providers and mothers; he also shared testimonials from some of the providers interviewed. Health care workers reported that the Immunity Charm fit into the existing traditional belief systems of their community and felt confident that the bracelet could be a driver of mothers’ appreciation for the role of vaccines in protecting their children. One health care worker remarked that he overheard mothers discussing which colored bead represented which vac-

SOURCE: Carucci presentation, August 19, 2020.
___________________
6 The Immunity Charm includes a colored bead for measles doses 1 and 2, oral polio vaccine doses 0 through 4, pneumococcal conjugate vaccines doses 1 through 3, pentavalent vaccine doses 1 through 3, and hepatitis B vaccine. More information is available at http://www.theimmunitycharm.org (accessed May 20, 2021).
cine. This health care worker said that they had never experienced mothers talking about vaccines in this way.
Potential Impact of the Immunity Charm Project
McCann Health sees the Immunity Charm as a potentially powerful driver for improving uptake in vaccine compliance in particular communities where this tradition in widespread, said Carucci. He suggested that the bracelet could drive vaccine compliance in three distinct ways. Mothers see the Immunity Charm as a symbol of protection against disease, in the same way that they see other bracelets as symbols of protection. Additionally, the bracelet serves as a symbol of a mother’s love for her child and of good mothering, thus increasing the perceived value of vaccines among mothers. For the community, the bracelet serves as a visible signal to other influential mothers and community members, thus encouraging other mothers who have not yet vaccinated their children to do so. For health care workers, the bracelet provides an additional and readily visible indication of a child’s immunization status, particularly if the official immunization record is not available. However, Carucci emphasized that the Immunity Charm is not intended to replace the standard immunization card. Carucci said that to build on this qualitative research, his team intends to launch a quantitative effectiveness study in India, although it has been delayed by the COVID-19 pandemic.
THE ROLE OF PHYSICIANS IN BUILDING VACCINE CONFIDENCE AND ACCEPTANCE
Presented by Todd Wolynn, Kids Plus Pediatrics
Wolynn discussed the role of physicians in building vaccine confidence and acceptance. He noted that perceptions of infectious diseases, physicians, and the field of medicine have all evolved over time. In the past, trust in physicians and the medical system was fairly high, but this began to decline by the beginning of the 21st century. He attributed this change, in part, to the increasing “businessification” of medicine, which has created a rift between physicians and their patients. Health care systems have become encumbered with administrative burdens, limitations on time spent with patients, increasing managerial meetings, and—at least in the United States—an increasing focus on profiting from health and illness, he said. Furthermore, health care providers have begun to lose their ability to communicate effectively with the families that they serve and are at risk of losing one of their most precious assets: a close and trusted longitudinal relationship with patients. He remarked that in addition to these changes in the health systems, providers
were also unaware of new and potentially devastating threats to public health that have emerged in the form of fake news, conspiracy theories, and pseudoscience. Vaccines have long been attacked by skeptics, but new digitally fueled disinformation and weaponized anti-vaccine attacks are rapidly eroding vaccine confidence, he cautioned. Because they are generally ill-equipped to address the challenges of these anti-vaccination forces, many health care providers have begun to lose confidence in their own ability to influence and help the populations they serve, he suggested.
Forces of Vaccine Hesitancy
Wolynn discussed the forces that act on vaccine hesitancy, explaining that approximately 75 percent of the U.S. population is vaccine accepting, 23 percent is vaccine hesitant, and 1–2 percent are anti-vaccine. Traditionally, discussion of vaccines usually took place only in health care settings. Today, however, millions of discussions about vaccines are taking place online each day on social media, including relentless aspersions against the safety, effectiveness, and necessity of vaccines. These messages can have great effect through the tendencies toward tribalism often observed on social media, he noted. For instance, a person may be more likely to believe content that has been posted by a fellow group member on a social media platform even if they have never met in person.
In a recent paper that evaluated the online competition between pro-vaccine and anti-vaccine views, the authors noted that anti-vaccine groups are growing quickly and are on pace to outgrow pro-vaccine groups (Johnson et al., 2020). Even seasoned physicians are often unprepared to address vaccine hesitancy in person, instead responding to vaccine hesitancy with fear tactics or data. Wolynn suggested that such responses from physicians can unwittingly push vaccine-hesitant families toward becoming further entrenched in their vaccine skepticism. Furthermore, many young physicians are entering the health care system with their own uncertainties about vaccines and may capitulate with families’ requests to delay or skip vaccinations. This kind of capitulation has a deleterious effect on the public perception of the importance of vaccines. Many physicians lack formal training in communication, active listening, and face-to-face engagement. Additionally, there is essentially no plan to develop training for physicians on how to communicate with patients when interacting virtually.
Unfortunately, the trust network that exists between millions of physicians, health care providers, and their patients is not being adequately used against vaccine hesitancy because of a lack of training and support from institutions, he said. These trusted relationships are at risk while the information vacuum is being filled by other actors who are more willing to listen and provide information, he warned. Fortunately, there are strategies that can be
implemented to address both the virtual and face-to-face forces contributing to vaccine hesitancy.
Communication Methodology for Building Vaccine Confidence
Wolynn presented a face-to-face communication methodology called AIMS (announce, inquire, mirror, and secure), developed by John ParrishSprowl and Angus Thomson,7 that can be used by health care providers who encounter vaccine hesitancy. This method, which focuses on using powerful active listening and communication skills to build a trusting relationship, involves four components: announce, inquire, mirror, and secure. The “announce” component of the approach capitalizes on the fact that approximately 75 percent of the U.S. population are already willing to accept vaccines, in that the provider makes a presumptive announcement to raise the topic of vaccines and with these patients they are not met with hesitancy. Inquiring and mirroring are features of active listening, a strategy that is particularly useful when engaging with parents who are vaccine hesitant. People need to feel that they are being heard and that the physician is on their side and understands their concerns. This process facilitates a meaningful conversation that can help encourage many people to choose to vaccinate, said Wolynn. The methodology also recognizes that some patients will choose not to vaccinate. In those situations, the provider focuses on the fourth component: securing the relationship between health care providers and their patients and establishing trust. Providers can secure this relationship with statements such as “Maybe we will not give all the vaccines I’ve recommended today, but we can discuss that next time.” The AIMS approach is not only effective for face-to-face interactions but also for busy health care settings that have relatively few vaccination-related interactions with patients.
Countering Anti-Vaccine Attacks
Wolynn noted that millions of conversations about vaccines occur online, with those who promote vaccines or call out disinformation at risk of being attacked. These attacks are designed to overwhelm, isolate, weaken, frighten, terrorize, cause damage, dissolve, and silence. They can be vicious and severe, leaving many victims feeling traumatized by the experience. While only 1–2 percent of the U.S. population is thought to be anti-vaccination, this group is disproportionately influential because there is a globally coordinated network that is working tirelessly, strategically, and effectively to promote anti-vacci-
___________________
7 More information on the AIMS approach applied to conversations on vaccination is available at https://www.fondation-merieux.org/wp-content/uploads/2017/01/vaccine-acceptance2017-john-parrish-sprowl.pdf (accessed May 20, 2021).
nation messages, he said. For instance, quaternary health systems have been shut down for fear of attack by anti-vaccination groups after posting about influenza vaccination as flu season approached. Providers and clinics have no instructions on how to deal with virtual attacks, no organized groups of allies to provide aid, and anti-vaccine attacks are extremely effective.
Wolynn shared the story of how an anti-vaccine attack on his practice led to his own research on effective counterattacks. In August 2017, his practice, Kids Plus Pediatrics, produced a 90-second public service announcement on the power of the human papillomavirus (HPV) vaccine in preventing cancer. One month later, his practice suffered a coordinated, week-long, global attack on its social media and online ratings pages. To combat these types of attacks, Wolynn and colleagues published an article on anti-vaccination campaigns and the 2017 attack on their practice (Hoffman et al., 2019). They created a toolkit and described how they organized a “digital cavalry” of nearly 900 people in 20 countries to launch an international awareness campaign. This campaign was aimed at teaching, uniting, strengthening, empowering, defending, recovering, emboldening, and galvanizing pro-vaccine health care providers on social media. These methods directly counter the attacks employed by anti-vaccine groups. Wolynn remarked that when confronted with science and data, anti-vaccination advocates and online bullies moved on to softer targets.
This experience led to the creation of Shots Heard Round the World, a rapid-response network dedicated to combating anti-vaccine attacks on the social media pages, web sites, and review sites of providers, practices, hospitals, and health systems.8 Wolynn said that for some people who have experienced these types of attacks, the Shots Heard network has helped to strengthen and empower them to become highly effective advocates. The original toolkit is being revamped and will be available in English, French, Portuguese, and Spanish. Shots Heard Round the World has partnered with Stronger, a national campaign aimed at stopping the spread of harmful misinformation about science, medicine, and vaccines by sharing correct information and arming people to fight back against misinformation.9
Strategies for Vaccine Advocacy
Wolynn emphasized that the battle between vaccine hesitancy and vaccine confidence spans both face-to-face and virtual communication, that there are ways to address both, and that effective communication can be
___________________
8 More information about Shots Heard Round the World is available at https://www.shotsheard.org (accessed October 13, 2020).
9 More information about Stronger is available at https://www.stronger.org (accessed October 13, 2020).
strengthened through appropriate training. He noted that it is exceedingly difficult to debunk misinformation once it has taken hold. To that end, the University of Cambridge has begun efforts to “prebunk” COVID-19 conspiracies by providing accurate information about vaccines before conspiracy theories begin to spread.10 This kind of activity has been shown to make individuals more resistant to being affected by disinformation. To promote vaccination and leverage their trusted relationships with patients, health care providers would benefit from improved communication training in medical school, residency, nursing school, public health education, and other educational settings, he added. Moreover, advocates of vaccination should work collectively to promote vaccines (e.g., through inoculation with facts), undermine disinformation campaigns, and defend against weaponized social media attacks.
COMMUNICATING WITH VACCINE-HESITANT PARENTS
Presented by Sean O’Leary, University of Colorado School of Medicine
O’Leary described various strategies that health care providers can use to communicate with vaccine-hesitant parents using face-to-face communication, presumptive conversations, and motivational interviewing. Although his presentation focused on effective communication in patient–provider encounters, he emphasized that patient–provider communication is only one strategy among many that need to be implemented simultaneously to achieve and maintain high vaccination coverage.
Impact of Provider Vaccine Recommendations
O’Leary emphasized the effect of recommendations from a health care provider in shaping parents’ attitudes toward vaccinating their children. Providers should recommend vaccines as part of their communication strategy with vaccine-hesitant parents because the quality and presence of a provider’s recommendation have consistently been associated with increased uptake of vaccines. This is consistent with polling data indicating that medical providers are among the most trusted individuals in society.11
___________________
10 More information about the University of Cambridge’s efforts to prebunk COVID-19 conspiracies is available at https://www.cam.ac.uk/stories/goviral (accessed October 13, 2020).
11 More information about Gallup’s ranking of honesty and ethics in professions is available at https://news.gallup.com/poll/274673/nurses-continue-rate-highest-honesty-ethics.aspx (accessed October 8, 2020).
Continuum of Vaccine Acceptance
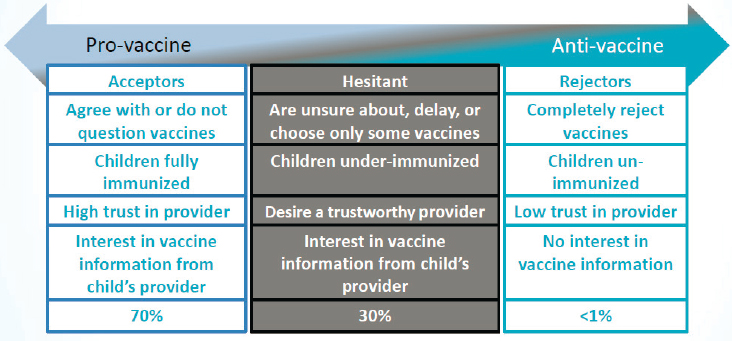
Providers should adapt their communication strategy based on where a parent is situated along the continuum of attitudes toward vaccines, said O’Leary. On the pro-vaccine end of the spectrum are vaccine acceptors (about 70 percent of the population), in the middle are those who are varying degrees of vaccine hesitant (around 30 percent of the population), and on the anti-vaccine end are vaccine rejectors (less than 1 percent of the population). Figure 5-2 provides more detail about common attitudes expressed by each of the three groups. Even though vaccine rejectors are often vocal, they make up an exceedingly small proportion of the population, he noted. O’Leary suggested using strategies for vaccine communication with parents who accept vaccines and those who are hesitant about vaccines but not with a parent who is determined to reject vaccines. Parents who would try to convince a provider that vaccines are bad will probably not be convinced to accept vaccines in a single patient encounter. He advised that when engaging with vaccine rejecters, providers should simply state their belief in the importance of vaccines and offer to keep the dialogue open. Otherwise, these types of encounters can escalate into arguments and leave little time to discuss other health and safety issues.
Evidence Regarding Face-to-Face Communication About Vaccines
O’Leary presented evidence regarding the effectiveness of face-to-face vaccine communication techniques. These have been investigated by two Cochrane reviews in the past decade, both of which determined that evidence for specific techniques is not conclusive. In 2013, a Cochrane review
SOURCE: O’Leary presentation, August 19, 2020.
concluded that the limited evidence available was of low quality and suggested that face-to-face interventions to inform or educate parents about childhood vaccination have little to no effect on immunization status, knowledge, or understanding of vaccination (Kaufman et al., 2013). In 2018, Cochrane published an updated version of the review which found low- to moderate-certainty evidence suggesting that face-to-face information or education may improve or slightly improve children’s vaccination status, parents’ knowledge, and parents’ intention to vaccinate (Kaufman et al., 2018).
O’Leary considered why better evidence about how to communicate about vaccines with parents and patients is not available. While much research has been conducted on parents’ and patient’s knowledge, attitudes, and beliefs, there has been relatively little research on which communication techniques change behavior. He characterized this research gap as a focus on the what rather than a focus on the how. He stated that it is still necessary to study the what questions: (1) what safety surveillance mechanisms work, (2) what ingredients are used to make vaccines, (3) what diseases are prevented by vaccines, (4) what is the immunology of vaccination, (5) what is recommended by the U.S. Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices, and (6) what facts address vaccine misconceptions. However, only studying the what is not sufficient to address vaccine hesitancy. The how questions must also be studied to find the most effective ways to convey information to parents or patients who are already resistant to vaccination so they might become more receptive to the information, he said.
Presumptive Versus Participatory Conversations About Vaccination
Conventional wisdom holds that if providers improve knowledge, patients and parents will make the right decisions, said O’Leary. However, this presumes that human decision making is rational, and that assumption is not always well founded. Thus, investigators have begun to focus on developing interventions to improve vaccination by studying how people actually think rather than how they ought to think.
An observational study performed by investigators in Seattle recorded parent–provider encounters during well-child visits to look for predictors of vaccine uptake (Opel et al., 2013). Parents were told that the investigators were examining communication techniques related to preventive care in children, rather than vaccine communication techniques, so as not to affect the vaccination discussion. Investigators administered a broad survey prior to the visit to identify vaccine-hesitant parents, which allowed the investigators to oversample this population. Of the 111 vaccine discussions recorded, half were with vaccine-hesitant parents.
The investigators found that the best predictor of vaccination uptake for both hesitant and non-hesitant parents was how the providers started the conversation (i.e., the first words uttered by the provider). The study used two conversation formats and found a striking difference in the outcomes associated with each approach. The first approach, the presumptive format, began with a declarative sentence that presupposes that the parents will have their children vaccinated (e.g., “Sara gets three shots today.”). The second approach, the participatory format, begins with an open-ended question that shifts decisional control to the parent (e.g., “How do you feel about shots today?”). When providers opened the conversation in a presumptive format, parents resisted the recommendation about 26 percent of the time. When providers opened the discussion in a participatory manner, parents resisted the provider’s recommendation about 83 percent of the time. This finding held true for both hesitant and non-hesitant parents.
O’Leary considered some of the possible reasons that presumptive conversations were associated with less parental resistance. He noted that when individuals perceive a decision to be complicated—such as when parents face the decision to have their children vaccinated—they tend to be affected by the status quo bias,12 which is the tendency to do what is expected or appears to be normal. By assuming a presumptive tone, providers convey that vaccination is the normal choice, making parents less likely to resist. In many cases, the presumptive format may make parents more comfortable with their decision to vaccinate, because the participatory format can leave parents questioning whether they have made the correct decision for their child. He added that a randomized controlled trial has confirmed the effectiveness of announcements versus conversations in improving uptake of human papillomavirus vaccination (Brewer et al., 2017b).
Motivational Interviewing
O’Leary explained that motivational interviewing is a technique that provides a framework for communication that reverses the traditional patriarchal approach of medicine—that is, the approach wherein patients are expected to change behavior because of a provider’s guidance. Instead, this framework uses guided conversation that is driven by the patient’s internal motivations. The provider guides the conversation so that the patient recognizes the importance of the behavior change to their own internal motivations. O’Leary endorsed the technique for its adaptability and because it can be used to improve conversations about most topics.
Evidence that this interview technique helps increase vaccine uptake comes from a study that tested the effect of motivational interviewing
___________________
12 The status quo bias is also called the default bias.
training on adolescent HPV vaccination (Dempsey et al., 2018). Clinics were randomly assigned to the control and intervention study arms. The intervention included several components with motivational interviewing training at the center of the intervention. The study found that the self-efficacy for changing parents’ minds about HPV vaccine improved among providers in the intervention arm, and time spent in HPV vaccine discussions remained the same or decreased from baseline at 4 months after the training in intervention clinics. Furthermore, there was a 9.5 percent increase in HPV vaccine initiation in the intervention arm versus the control arm.
Motivational Interviewing Skills for Use in Vaccine Conversations
O’Leary described five motivational interviewing skills that can be used for vaccine conversations, but noted that the broader practice of motivational interviewing can involve a longer process than the one used for vaccine conversations. The motivational interviewing process developed for vaccine conversations is intended to be effective but also efficient. Based on provider feedback, O’Leary’s team identified five skills that are most important when having discussions about vaccines: open-ended questions, affirmation, reflection, autonomy support, and asking permission to share. Open-ended questions help to explore and understand parents’ stance on vaccination. Affirmation improves parent engagement in an open discussion by helping them feel supported, appreciated, and understood. Reflection encourages partnerships, deepens rapport, and allows a parent to understand themselves and their motivations on a deeper level. Autonomy support enhances a parent’s sense of control and makes them feel more at ease with the conversation. Finally, asking permission to share puts parents in a less defensive posture and makes them more receptive to information that providers want to share.
O’Leary provided a brief demonstration of these skills through a hypothetical parent–provider encounter (see Box 5-2). The provider’s first response to the parent’s objection is an open-ended question. Upon hearing the parent’s concerns, the provider affirms the concerns and reflects them back to the parent. The provider takes care to ask for permission before offering their view of the HPV vaccine, and finally the provider exemplifies autonomy support by closing the exchange by putting the decisional power in the parent’s control.
O’Leary explained that teams in Colorado and Washington State are working to test this technique in a randomized trial in which providers are trained in motivational interviewing for addressing the infant series of vaccines. One experienced pediatrician involved in these trainings reported, “Asking permission to share has been a game changer.” She
said that this skill has changed her conversations and that she tries to implement this skill every time she uses the motivational interview technique. O’Leary acknowledged that numerous groups around the world are working with motivational interviewing techniques for vaccination conversations, specifically acknowledging promising results from a study conducted in Canada (Gagneur, 2020). He added that although other potentially effective communication frameworks are available, motivational interviewing is beneficial because it offers providers tools that they can adapt to address many health concerns in a mutually beneficial manner. The motivational interviewing technique lets providers and patients feel that their concerns have been heard, and it leaves providers feeling confident that they can communicate the facts without drawing patients into an argument.
DISCUSSION
Factors Affecting Herd Immunity
John asked whether herd immunity is helpful against outbreaks in settings where less than 10 percent of the population is unvaccinated. Mello explained that the prospects for achieving herd immunity vary across diseases as a function of two factors. First is the reproductive number of the disease (R0)—that is, how many new cases emerge for each existing case within the population. The more infectious a disease is, the greater the vaccination coverage must be in order to achieve herd immunity. The second factor is the effectiveness of the vaccine. Increased effectiveness of a vaccine will be associated with a lower vaccination coverage required to achieve herd immunity. These two factors vary widely across various diseases, she noted. For example, in the case of measles, the R0 is between 12 and 18, which is relatively high. Thus, a vaccination coverage rate of approximately 95 percent is required to achieve herd immunity against measles. Polio has an R0 of 5–7, so between 80 and 85 percent vaccination coverage is sufficient for achieving herd immunity against polio. The R0 of influenza is less than 2, so approximately 40 percent vaccination coverage against influenza is sufficient for herd immunity.13
Legal Options to Protect Children from Vaccine-Preventable Disease
John asked whether community members may seek a legal mandate to vaccinate a child with a vaccine exemption if that child is a known source of a vaccine-preventable disease. Reiss explained that it is not generally possible to take parents to court and ask for an order for that parent to have their child vaccinated. However, it may be possible in some cases—for example, when parents who share custody have a dispute about vaccinating their child—where the court may side with the parent who wants to vaccinate their child. Typically, only a guardian or the state can bring a case requesting for an order to vaccinate a child. She added that if a child is infected with a vaccine-preventable disease by another unvaccinated child, the parents may file a tort claim on the basis of parental negligence.
California Law and the Willingness of Physicians to Report Adverse Events
John expressed his concern that California vaccination policy may affect the willingness of physicians to accurately report adverse events encountered
___________________
13 For more information for the R0 of these pathogens, see Fine (1993).
after vaccination. He asked how physicians should proceed should they observe a serious adverse reaction that has not been enumerated by the CDC Advisory Committee on Immunization Practices. Mello commented that she saw no clear connection between California’s legislation and the willingness of physicians to report adverse effects after vaccination. She clarified that California legislation empowers the Department of Public Health to investigate physicians who write an exceedingly high number of vaccination exemptions, but it does not call for an investigation of physicians who report adverse effects after vaccination.
Shared Clinical Decision Making and Vaccination Discussions in Clinical Settings
John asked how physicians should approach shared clinical decision making in the context of vaccine discussions. O’Leary acknowledged that this issue has arisen in discussions around motivational interviewing techniques. Many health care providers are being trained using the shared clinical decision-making mode, which O’Leary applauded. However, this model is designed for preference-sensitive decisions, meaning that these decisions involve choosing between equally acceptable options. For instance, a patient may be eligible for either heart surgery or a stent to treat blocked arteries. There may be pros and cons to either option, so shared clinical decision making affords patients the opportunity to work through those options and their trade-offs. He noted that vaccination is a standard of care, so in that sense, vaccination discussions are not an appropriate context for using the shared clinical decision-making framework. Instead, techniques such as motivational interviewing are being implemented to help providers convey the facts related to vaccines and to help patients and parents understand those facts.
John asked whether physicians could engage in shared decision making with parents about the vaccination schedule if they are willing to vaccinate but express common concerns about the complexity and volume of childhood vaccinations. O’Leary remarked that this may be a question of semantics, because “shared decision making” refers to a specific set of practices. Providers working with families to vaccinate their children often use principles of shared decision making. However, the proper practices of shared decision making draw on a specific body of literature within the scientific and medical literature. He reiterated that these practices are intended to be used to make preference-sensitive decisions where there is no clear recommendation for physicians to make. In the case of vaccines, there are clear recommendations that are based on science. O’Leary remarked that when physicians and parents go outside of those recommendations, they are improvising and not properly engaging in a shared decision-making process. For instance, in shared decision making, elaborate decision aids may be used
by patients and providers to work through decisions based on the patient’s beliefs. There are no such processes for determining alternative vaccination schedules, because there is a clear and consistent recommended vaccination schedule that is based on a large body of scientific studies and a consensus of experts. Thus, any attempt to improvise or engage in shared decision making about vaccine schedules is, by definition, departing from the clear recommendations about vaccination schedules, said O’Leary.
Wolynn added that children whose parents delay vaccinations may be at an increased risk of not receiving all recommended vaccines (Smith et al., 2010). He said that in his practice, he stays within the confines of the periodicity of the well-child visits, which occur between the ages of 2–4 months, 4–6 months, and 6–9 months. If the vaccinations are to be spaced out, which he allows to accommodate breastfeeding mothers, he uses that periodicity along with a robust callback system within his practice’s electronic medical records system. O’Leary emphasized that there is no valid reason to depart from the recommended vaccination schedule to spread out a child’s vaccinations. While there are many reasons people wish to do so, spreading out vaccinations puts children at greater risk of having a vaccine-preventable illness and likely increases the total pain experienced by children.
The Immunity Charm Project
John raised a series of pragmatic questions about the Immunity Charm: (1) whether bracelets might be passed on to children other than the child who has actually been vaccinated; (2) whether the Immunity Charm might introduce stigma into communities impacting those children who have not received a bracelet, especially if the bracelet became a requirement for school enrollment; (3) whether increasing popularity of the bracelet within a community might create a black market for the bracelets; and (4) whether the bracelet might pose a choking hazard for the infants wearing them. Carucci explained that the design of the bracelet precludes the possibility of children opening their own bracelet, which reduces the potential choking hazard. Furthermore, beaded bracelets similar to the Immunity Charm are already widely used in the communities in question. Mothers are generally already familiar with how to open and close the bracelets, and they would be free to put the bracelet on their child’s ankle if they prefer. He reported that McCann’s qualitative study indicates a good level of overall acceptance of these bracelets in communities, and they are confident that the forthcoming larger-scale quantitative study will reveal a similar level of acceptance. Regarding the potential for a black market, Carucci explained that the Immunity Charm will be launched with a strong communications strategy that includes information about the quality of the charms, the origin of the beads, and how each bead is associated with specific vaccines. Furthermore,
the beads will be given at the time of immunization by health care workers who themselves will reinforce these messages. McCann has considered engaging with women’s groups in the communities where the Immunity Charm is used to have bracelets locally produced, thus adding a sense of community ownership to the intervention. Carucci added that many of the questions raised by John will be more fully addressed by the forthcoming quantitative study. In his opinion, the most critical question to be answered by that study is the percentage of parents who will choose to fully vaccinate their children as a result of the Immunity Charm intervention in their communities.
Designing Public Health Messages to Promote Vaccination
John asked about the approach of public service announcements that use shock value to promote public health awareness—such as advertisements about the risks of smoking and the importance of HPV vaccines—and whether this approach may be employed to promote forthcoming COVID-19 vaccines. Wolynn commented that these campaigns are designed to evoke an emotional response, which is known to be an effective approach. The designers of these campaigns try to avoid fearmongering, but they do intend to elicit an emotional response. Carucci added that the kinds of messages used in public service announcements should be, in part, determined by the context and health concern being addressed. For instance, polio vaccination rates are relatively low in Pakistan, but polio is rare in most Pakistani communities due to effective vaccination strategies in the past. Polio is primarily a concern in certain pockets of communities where the previous vaccination campaigns have not been effective. An advertising campaign aimed at increasing concern about polio would be unlikely to drive an increase in polio vaccinations in this setting, he added.
Advertising campaigns should account for the barriers to uptake, he suggested. In the case of vaccination against polio in Pakistan, the barriers had to do with mistrust of vaccinators rather than a lack of concern for the risk of polio. Communication strategies should be aligned with existing barriers, rather than developing strategies based on assumptions about the fear of a particular disease. For instance, he suggested that most cases of COVID-19 will result in a rather mild illness, so a campaign promoting COVID-19 vaccines on the basis of fear and the need for individuals to protect themselves from illness is unlikely to be effective. Reiss added that each public health campaign is narrowly targeted on the public health concern it addresses. For instance, HPV vaccination campaigns are aimed at increasing HPV vaccination to prevent cancer. While it is expected that new campaigns learn from the experience of existing and past campaigns, lessons learned may not be generally applicable across campaigns for all public health issues.
Carucci said that if a private-sector company were to launch a new vaccine product, it would create a market-shaping campaign in advance of the product’s release. Such a campaign would be global but tailored to be context-specific in each region, addressing local fears and concerns. He expressed his concern about releasing new vaccines first, then trying to address fears and concerns later, because it is critical for vaccine advocates to preemptively shape the market and public perceptions to ensure good vaccine uptake. Wolynn pointed out that anti-vaccine sentiments vary widely across cultures and may be driven by religious objections, political conspiracies, or other culturally specific issues in addition to health and safety concerns. Speaking from his own experience and his work with the International Pediatric Association, Wolynn said that he has encountered a wide range of diverse concerns about vaccination. For instance, members of the Somali American and Orthodox Jewish populations within the United States often have unique sets of concerns about vaccination.
Designing Campaigns for COVID-19 Vaccination
John asked whether any information was available about potential campaigns for forthcoming COVID-19 vaccinations. O’Leary said that CDC is considering these issues. However, until the safety profiles and other characteristics of forthcoming COVID-19 vaccines are known, the messaging to promote those vaccines cannot be fully developed. Regardless of the messaging around these vaccines, it will be crucial to engage with communities prior to the COVID-19 vaccine rollout in order to understand community concerns so that there is an open dialogue from the start of the COVID-19 immunization process. Wolynn added that because COVID-19 vaccines are being rapidly developed, there will be no information with which to preemptively inoculate the public against misinformation. Vaccination advocates will have to react quickly to address disinformation, which has already begun to be distributed in advance, once good information is available. Reiss said that long-standing vaccine advocates, such as Voices for Vaccines14 and Vaccinate Your Family,15 are preparing messaging to promote forthcoming COVID-19 vaccines. Wolynn said that leveraging trust and relationships is key to addressing vaccine hesitancy, and physicians and vaccine advocates must be armed with good information and use their trusting relationships appropriately. Carucci said that the sources of information should also be considered in designing campaigns, because there is a high degree of mistrust
___________________
14 More information about Voices for Vaccines is available at https://www.voicesforvaccines.org (accessed October 14, 2020).
15 More information about Vaccinate Your Family is available at https://www.vaccinateyourfamily.org (accessed October 14, 2020).
in government and science. Thus, it may be necessary to look beyond medical voices to provide information about vaccines.
Online Communication About Vaccination
John asked for specific advice about how vaccine advocates should communicate online about vaccines, noting that merely providing facts is not always effective. Wolynn said that Shots Heard Round the World has approximately 900 volunteer advocates. These volunteers need access to well-prepared and accurate information that is relevant to whatever vaccine-related issue that comes up, because they do not have the time to conduct their own research for each encounter. Furthermore, he added, health care providers are not necessarily required to spread beneficial information about vaccines. For instance, in the United States, community health workers and community health advocates are already embedded in communities and have trusting relationships with patients. Wolynn said that to get the right information to the right people, the information must be easily searchable and easy to cut and paste for use on social media platforms. He added that departments of health are generally more trusted at the community level, because the erosion in trust has most significantly affected larger health systems and government. He suggested finding ways to partner with departments of health and work to collaboratively share information both through social media and community-level campaigns; the latter may be especially valuable in areas and neighborhoods impacted by disparities in health resources.
Rationality of Decision Making
John pointed out the common sentiment in vaccination advocacy that human decision making is often irrational. However, this may be a misleading characterization, as decisions are often more rational when they are evaluated in the context of the various factors that influence individuals’ decisions (e.g., personal priorities and risk/benefit considerations). He voiced the concern that characterizing individuals’ decisions as “wrong,” “irrational,” or “misinformed” does not account for the numerous factors that influence decision making, and he asked how a more compassionate response to vaccine hesitancy might be encouraged. Wolynn commented that communication strategies, such as motivational interviewing and AIMS, teach practitioners to engage and communicate through active listening. O’Leary added that one purpose of conversational strategies, such as motivational interviewing, is to foster empathetic discourse so physicians can understand patients’ perspectives, meet them where they are, and convey information in a way that the patient may be receptive to—all while avoiding argument.
It is easy to fall into a back-and-forth conversation, which can then escalate into an argument, he said, and such conversations are not productive for either party. He clarified that the characterization of human decision making as “not always rational” is not intended as a sign of disrespect toward individuals’ beliefs or capacity for rationality. Rather, this characterization acknowledges the role of emotions, beliefs, and factors other than rationality or science in people’s decision making. Furthermore, individuals often need to “digest” these various factors throughout the decision-making process. In the case of child vaccination, parents face complex decisions that are influenced by numerous factors beyond the facts. It is because decision making is shaped by numerous factors that merely presenting individuals with facts may not be sufficient to give them confidence in the right decision.
Status of Immunization Exemption Policies Across the United States
John asked about the status of immunization exemption policies among states that are considering restricting their exemptions. Mello explained that the measles outbreaks in 2014, 2015, and 2018 have raised concerns about vaccination exemption policies among state legislators. Maine and New York have made changes similar to those made in California, and numerous states have attempted but failed to pass similar legislation. She added that along with efforts to restrict exemptions there are efforts under way to expand exemption policies in some states. The latter efforts are being driven by the anti-vaccination lobby in response to the growing concerns among lawmakers about outbreaks of vaccine-preventable diseases, she said. While there have been more bills introduced aimed at expanding exemptions than at restricting exemptions, bills introduced that are aimed at restricting exemptions have been more successful to date.
Promoting Seasonal Influenza Vaccination
John described a common scenario where parents have kept their children up to date on their childhood vaccinations but steadfastly refused the influenza vaccination. He asked whether physicians should press this issue and potentially risk upsetting the family’s adherence to the non-influenza vaccination schedule. Wolynn said that physicians can be well equipped to discuss flu vaccines, acknowledging the truthfulness of the common sentiment that the influenza vaccine is not always effective. While the influenza vaccine’s effectiveness varies, even a relatively low percentage of protection against disease is better than no protection. He explained that physicians can discuss the potential value of vaccination to reduce the severity of infection and mortality even if the patient becomes infected with influenza. Patients can also leverage the power of narrative, he added. For instance, he often
shares the story of a mother whose 17-year-old son told her he felt ill and then died within 24 hours. This mother now works with Families Fighting Flu to spread awareness about these issues.16 Narratives such as these can be powerfully leveraged to promote vaccination.
___________________
16 More information about Families Fighting Flu is available at https://www.familiesfightingflu.org (accessed October 15, 2020).






























