4
Communicating About Radiation-Induced Cancer Risks
As part of this study’s Statement of Task (see Box 1-2 in Chapter 1), the National Aeronautics and Space Administration (NASA) requested the committee to consider “how to express what is needed in the form of a radiation risk management process or approach NASA could apply to determine astronaut eligibility for crewed missions.” This chapter focuses on this aspect of the study task and specifically on communicating with astronauts about the risks associated with exposure to space radiation.
As NASA works to manage radiation-exposure health risks, it will be important for the agency to continue to adhere to the radiation safety principle of keeping radiation exposures as low as reasonably achievable (ALARA), employ the ethical principles of beneficence and non-maleficence in decision making, and communicate effectively about radiation risk to astronauts in a manner that respects the ethical principles of autonomy and justice (IOM, 2014; NCRP, 2014). A key component of risk management is evidence-based, thorough, and effective communication of the risks. NASA communications concerning radiation exposure are aimed at astronauts as well as NASA employees and contractors responsible for eliminating, minimizing, or mitigating these risks. Policy makers, other federal agencies, and commercial spaceflight companies are also audiences for NASA’s risk communication products.
This chapter provides a framework for how NASA can best communicate space radiation risks to astronauts. First, the chapter introduces the field of science communication (Fischhoff and Scheufele, 2013, 2014, 2019; NASEM, 2017), and then it identifies the risk communication needs of astronauts. When NASA presented to the committee its proposed revisions to the space radiation standard, it also presented a visual representation
of the radiation risk profile (“risk bands,” see Figure 4-1), which the agency is considering using as a system for communicating occupational radiation-induced health risk assessments to astronauts. The committee closely reviewed this visual aid and, in this chapter, presents its conclusions and recommendations on the benefits and deficiencies of this aid.
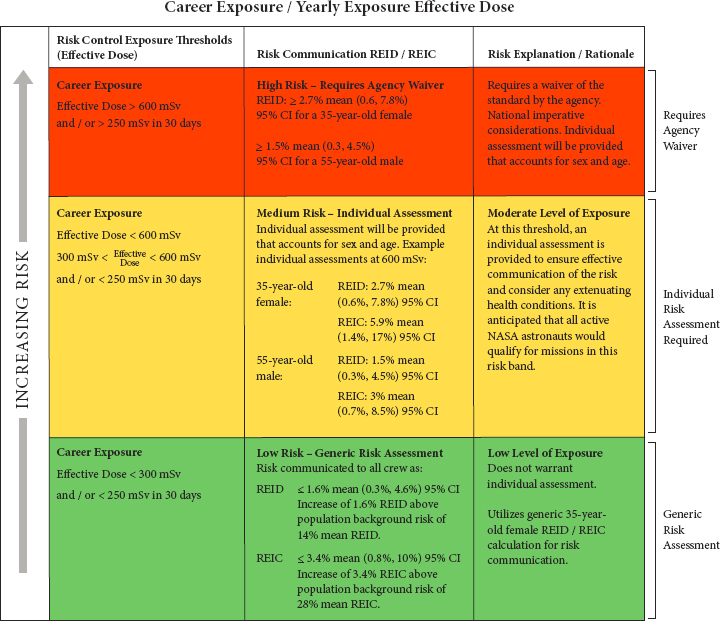
NOTES: If NASA chooses to use this system for communicating risk, the following text should be revised. In the green band “14% mean REID” should be revised to read “14% mean lifetime risk of death from cancer.” Similarly, “28% mean REIC” should be revised to “28% mean lifetime risk of being diagnosed with cancer.” These distinctions are important to communicating the meaning of REID and REIC. Confidence intervals are obtained by varying the input parameters of the NSCR NASA risk model according to “parameter uncertainty distributions” determined by NASA based on expert judgment. CI = confidence interval; mSv = millisievert; NASA = National Aeronautics and Space Administration; REIC = risk of exposure-induced cancer; REID = risk of exposure-induced death.
SOURCE: White paper provided by Dave Francisco, NASA, to the committee, February 12, 2021.
NASA’S AIMS WHEN COMMUNICATING CANCER RISK
The first step in communicating risk is to have a clear understanding of the goals of the communication. NASA communications about the cancer risk from radiation exposure during specific space missions and over the course of an astronaut’s career appear to have several aims:
- Enable astronauts to make their own health protective decisions;
- Provide the rationale for flight assignment determinations;
- Help astronauts plan their careers; and
- Protect astronaut health and space mission safety and viability.
Achieving these risk communication aims requires an understanding of the risks and the standard themselves, as well as comprehension of how astronauts understand and interpret the formal and informal communications about them. Achieving these aims is complicated by the dynamic nature of the risk communication situation, including but not limited to the evolution of radiation risk sciences, changes in the nature of space missions, diversification of the NASA Astronaut Corps, and the evolution of occupational exposure standards for terrestrial employees, which NASA may reference in developing risk management strategies.
RISK COMMUNICATION RECIPIENTS AND THEIR NEEDS
Health communication can be classified into three categories that differ in the degree of customization and audience segmentation (Hawkins et al., 2008): generic, targeted, and tailored. A generic health message, or a one-size-fits-all approach, provides information within a single communication without taking into account the characteristics of the audience. Targeted messages aim to reach a specific subgroup often based on sociodemographic characteristics such as gender and age. While targeted messages rely on such individual factors, targeting generally does not take into account aspects including cognitive and behavioral factors that can influence health decisions. Tailored messages “intend to reach a specific person based on characteristics that are unique to that person, related to the outcome of interest, and derived from an individual assessment” (Kreuter et al., 2013). Tailored messages are more likely to be read and remembered (Brug et al., 1998; Skinner et al., 1994), perceived to be personally relevant (Noar et al., 2009), and are more effective compared to non-tailored approaches (Noar et al., 2007; Richards et al., 2007; Rimer and Glassman, 1998; Sohl and Moyer, 2007). A systematic literature review of interventions designed to provide tailored information on cancer risk and screening methods showed that cancer information tailored
to individuals’ risk factors increased realistic risk perception compared to generic information (Albada et al., 2009).
Depending on its communication goals, NASA may wish to develop generic space radiation risk messages for public audiences, in addition to the targeted risk messages it uses to communicate the space radiation standard to NASA astronauts as a group and the tailored messages it uses for individual astronauts.
Risk Communication Needs for NASA Astronauts
In its discussion of why NASA is proposing to use a space permissible exposure limit standard based on an effective dose of 600 mSv as its new risk management standard, NASA noted that dose is more familiar to astronauts than risk (e.g., risk of exposure-induced death [REID]). Similarly, NASA suggested that the use of “traffic light” color bands to represent the three-stage risk profile would be familiar to astronauts, given the widespread use of color-coded risk matrices at NASA. Familiarity can be an important determinant of communication effectiveness, but it is not the only factor (Keller, 2011). Spaceflight radiation risk communication needs are best assessed relative to the decisions that will be made in response to the communication. To the best of the committee’s understanding, a systematic evaluation of astronauts’ risk communication needs has not yet been conducted.
The first step in risk communication design in this context is to determine what information astronauts need. Astronauts have prior training and significant expertise that is likely to influence their risk communication needs, which may include training in probability and statistics, as well as in radiation and its biological effects. It is also likely that there is variation among astronauts in expertise and interest regarding radiation-induced cancer risk. In addition, among astronauts, there are variations in decision contexts such as concerns about reproductive health that could influence individual astronauts’ decision risk communication needs.
Demographics and sociocultural differences may also influence perceptions of risk communications. While many studies have found that these types of variables (age, gender, race, political orientation) account for little variance, some studies do find effects. This might be because certain groups perceive they are at risk of higher rates of exposure or because some groups have lower institutional trust in a particular context (Griffin et al., 2004). Risk message recipients filter messages through their own values and beliefs (Balog-Way et al., 2020). For example, motivated reasoning, where individuals interpret information in a way that is consistent with their predetermined opinions, may explain challenges to designing effective communications, particularly in the context of uncertainty.
Risk Communication Needs for Other Audiences
While NASA astronauts are the primary audience for communication of radiation exposure risks, other communication recipients may include NASA program managers, engineers, and designers, as well as policy makers, other federal agencies, commercial spaceflight companies, and various interested publics. Each of these groups makes decisions that might be informed by the proposed new standard and associated risk communications.
Audiences outside of NASA may not have the same technical background or personal characteristics as NASA personnel, and thus they are likely to interpret and react differently to figures, data, and information about radiation-induced cancer risks. Numeracy and other individual characteristics affect the interpretation of graphical or visual information to communicate risk (Hess et al., 2011; Kreuzmair et al., 2016; Okan et al., 2016; Yang et al., 2021). Expertise also influences how information is processed and used in risk decision contexts; therefore, risk communication needs will vary depending on the specific expertise of the risk communication recipient (Cokely et al., 2018; Perko, 2014).
CONSIDERING NASA’S PROPOSED RISK COMMUNICATION TOOL FOR THE SPACE RADIATION STANDARD
In public meetings, NASA presented this committee with a figure that presents the proposed space permissible exposure limit, as seen in Figure 4-1.1 The committee understands that this visual aid is intended as NASA’s primary risk communication system for the updated space radiation standard. It is composed of three bands, colored in green, yellow, and red as a “traffic light” to represent increasing risk. Each band contains three cells, outlining the exposure thresholds, REID and the risk of exposure-induced cancer (REIC), and the explanation or rationale for each band. The matrix contains both numerical information (e.g., REID and REIC) and evaluative information (e.g., high, medium, low) to communicate the risk. It also includes risk management information, such as the corresponding mission determination for specific audiences (e.g., “all active NASA astronauts would qualify for missions in this band” or whether a waiver would be required for a given mission).
The effects of risk communications can be difficult to predict (Roth et al., 1990; van der Bles et al., 2019). Instead, risk communication methods
___________________
1 NASA presented two versions of this figure to the committee. The first version is available in NASA’s January white paper and the modified, second version, which will be referenced through the remainder of this report, is shown in Figure 4-1. NASA’s white papers may be requested by contacting the National Academies’ Public Access Records Office (PARO@nas.edu).
can be evaluated empirically (Fischhoff et al., 2011; NASEM, 2017; NRC, 1989; Spiegelhalter, 2017). Evaluating risk communications and risk messages first requires knowing or assuming the purposes of the communication (Fischhoff et al., 2011; NASEM, 2017; NRC, 1989). Once the goals are determined, attributes or characteristics of risk communications are evaluated based on empirical evidence gathered from the intended recipients or a representative sample thereof. Lacking such evidence, the committee comments on the elements and attributes of Figure 4-1 based on risk communication literature. The committee adapts the framework proposed by van der Bles et al. (2019) for communicating epistemic uncertainty. This framework assesses the source of the message, the content of the message, the format of the communication, and the anticipated effects of the communication on recipients.
Source of the Message
Presentations and materials provided to the committee by NASA show that both formal and informal communications with astronauts about radiation risks come from multiple sources including the Space Radiation Analysis Group at NASA, the Human System Risk Board, flight surgeons, and others. NASA shared several examples of risk communication materials with the committee, some of which have been used in briefings to the astronaut office or for individual astronauts (e.g., Astronaut Radiation Risk Reports; Semones, 2021). The typical process for astronauts to learn about radiation risk includes briefings by the NASA Radiation Health Officer, annual individual meetings with flight surgeons, as well as additional meetings with flight surgeons pre- and postflight.
While the committee understood from NASA’s public presentations that formal NASA communications are trusted by astronauts, no systematic evidence was presented on this point. Trust in the message source and messenger influences whether a risk message recipient interprets the message as expected, ignores the message, or responds in an opposite way, as in the case of risk communications that backfire (Cairns et al., 2013; McComas, 2006). NASA may consider developing templates to guide meetings between flight surgeons and astronauts, as this may have the benefit of standardizing what information is communicated to astronauts, regardless of the individual characteristics of the messenger. Astronauts may also see flight surgeons as gatekeepers, which could change how astronauts perceive the information they receive and, conversely, what information they share.
In addition to meetings where information on space radiation is presented by NASA’s Office of the Chief Health and Medical Officer or flight surgeons, it could be valuable to allow astronauts to access on their own
information on cancer risks associated with space radiation. Providing astronauts access to a searchable database or repository of scientific literature used by NASA in developing the space radiation standard and other resources from the radiation science literature could reduce any barriers—real or perceived—astronauts might face in developing their own understanding of space radiation risks. Some astronauts may prefer to explore the relevant research on their own, either instead of or in conjunction with briefings and one-on-one meetings with NASA flight surgeons.
Content of the Risk Communication Message
Individualized Risk Communication
For the purpose of this report, the committee defines individualized risk communication as the process of tailoring information based on an individual’s specific risk factors for a health condition (e.g., age, sex, family history, prior exposures) (Edwards et al., 2013). As discussed earlier in this chapter, tailored communications are generally found to be more effective than general communications (Albada et al., 2009), and this would seem to be particularly the case in considering how best to communicate with individual astronauts.
NASA proposes a generic risk assessment in the green risk band (exposures below ~300 mSv) and communicating REID and REIC for a 35-year-old female to all astronauts. NASA proposes individual risk assessments using sex and age with consideration of extenuating health conditions for the yellow risk band (exposures between ~300 and ~600 mSv) and the red risk band (exposures exceeding the ~600 mSv limit in the standard) (see Figure 4-1). For astronauts with a career exposure above ~600 mSv, a waiver would be required to fly additional missions. NASA’s proposed individual risk assessment is differentiated from the general assessment only by taking into account sex and age. An individual astronaut who wishes to interpret his or her own spaceflight-attributable cancer radiation risks from a proposed mission might need not only specific information about dose and dose rate, but also information about the influence of non-modifiable individual factors such as genetics and modifiable factors such as lifestyle and environmental factors that interact with spaceflight radiation, all of which contribute to their baseline cancer risk. An individual assessment may also include information about screening and early detection of cancers. NASA may consider exploring future opportunities to enhance the individual risk assessment.
While the Genetic Information Nondiscrimination Act (GINA) precludes the use of personal genetic information in NASA risk management (see Locke and Weil, 2016, for further discussion on this topic), NASA
could consider providing easy access to summary information regarding what is known about the genetic factors that might interact with spaceflight radiation exposures to influence long-term health outcomes for astronauts, as well as the influence of other lifestyle and environmental factors. Best practices indicate the importance of addressing relevant prior beliefs (Morgan et al., 2002; NASEM, 2017), and explicitly discussing uncertainties (Fischhoff, 2012; Fischhoff and Davis, 2014; Manski, 2019; van der Bles et al., 2020), although this poses challenges (NASEM, 2017; Politi et al., 2007; van der Bles et al., 2019).
Putting Risk in Context
Best practices in risk communication suggest communicating both absolute and relative risk to inform risk management decisions (Spiegelhalter, 2017). It is key, however, to also communicate a baseline for relative risks. Figure 4-1 includes REIC, REID, 30-day dose rate, and career effective dose limit. Furthermore, REIC and REID are also communicated as increases above population background cancer risk, for which absolute risk (point) estimates are provided, although it is unclear from Figure 4-1 what the reference population is. Evidence-based communication practices highlight the importance of representing risks in multiple ways (Fischhoff, 2012). For instance, complementing REID with estimates of years of life-loss for deaths that occur may help astronauts contextualize REID in relation to other mortality risks (Cucinotta, 2010). There is evidence that health consequences are easier to imagine and remember when they are presented as years of life loss or gained versus increase or decrease in disease risk (Galesic et al., 2011).
Figure 4-1 also uses evaluative language by characterizing the risk bands as “low,” “medium,” or “high.” Interpretations and evaluations of technical risk quantities such as REIC, REID, and effective dose can be strongly influenced by this sort of evaluative information (Budescu et al., 2014). It is unclear if the evaluative judgments in Figure 4-1 are intended to correspond to the absolute or relative risks in each band. For example, if a terrestrial worker was exposed to a hazard with a 2.7 percent REID, that would be more than an order of magnitude greater than the level determined by the U.S. Supreme Court to be acceptable for industrial workers.2
To help empower astronauts to understand the full picture of their cancer radiation risks, the background cancer risks in the population and risks from occupational radiation exposures can also be communicated in the context of factors that might influence the astronaut’s cancer risk (e.g., family history, lifestyle factors) and in the context of other sources of
___________________
2 29 U.S.C. 655(6)(b)(5).
mortality risk on space missions. Additionally, as the absolute and relative risks can change over time (e.g., chronic versus acute risks), it is helpful if the time interval is explicitly communicated.
NASA also needs to be prepared to answer questions from astronauts on their radiation risk profile, which includes current and past occupational exposures as well as other radiation doses received from medical diagnostic and therapeutic procedures, naturally occurring radioactivity in the environment, and other sources. While these discussions are important to allow astronauts to make informed decisions about missions and understand radiation risks, the committee cautions that communication about non-occupational exposures—in particular, medical exposures—needs to be done with great care. Specifically, NASA needs to communicate to astronauts how exposures other than those received as part of the astronaut’s career and space missions are recorded and managed by the agency although they do not contribute toward the astronauts’ permissible career dose (NCRP, 2014). Furthermore, NASA needs to make clear that decisions regarding medical diagnostic and therapeutic procedures that involve ionizing radiation are made by qualified medical professionals based on the principles of justification and optimization (ICRP, 2007a).
Format of the Communication
Appropriately designed visual aids can improve both risk understanding and health-relevant decision making (Garcia-Retamero and Cokely, 2017), but they do not always do so (Ancker et al., 2006).
Communicating Uncertainty
The sources of uncertainty in NASA’s cancer risk model are discussed at length in Chapter 2. This section will focus on strategies to communicate uncertainties and adequately incorporate uncertainties into NASA’s risk communication strategies. In many cases, it is valuable to represent uncertainty in multiple ways to support the understanding of a diverse audience.
Figure 4-1 presents 95 percent confidence intervals for REIC and REID. Even if astronauts have a clear understanding of the relationships between dose and REIC and REID, the presentation format may influence risk perceptions in unintended ways. Confidence intervals can be misinterpreted due to misunderstanding of what they mean, because of motivated reasoning (Dieckman et al., 2015; Viscusi et al., 1991), or because of the misinterpretation of a visual representation of the interval (Savelli and Joslyn, 2013). These misinterpretations can lead to unanticipated effects of the communication (Johnson and Slovic, 1998). Risk communication research suggests that decision makers are sensitive to the ambiguity (or range of
uncertainty) associated with a numerical forecast, although specific effects have proven difficult to predict (van der Bles et al., 2019). In some cases, decision makers may discount information with high ambiguity information to focus on more precise, although potentially less relevant, information (Hsee, 1995). In other contexts, it is valuable to use numerical, rather than only verbal, descriptions of uncertainty to improve understanding (Budescu et al., 2009; Dieckmann et al., 2010).
Effects of communicating the uncertainty around risks (also called ambiguity) are thus a function of the recipient’s risk attitudes, numeracy, and the format of the uncertainty communication (Han et al., 2011). Graphical presentations such as gradient bands, probability density functions, or cumulative distribution functions to represent the central tendency and associated uncertainty in estimated risk appear to help convey the actual estimated distribution of probability for the risk estimates (Ibrekk and Morgan, 1987; van der Bles et al., 2019).
Figure 4-1 currently does not distinguish sources of uncertainty, nor does it directly acknowledge risk assessment model limitations. The extent to which this does or should influence interpretations of Figure 4-1 is not clear, as risk communication research is inconclusive on this topic (Budescu and Wallsten, 1995; Budescu et al., 2009; Padilla et al., 2020; Teigen and Løhre, 2017; van der Bles et al., 2019). However, directly acknowledging measurement and model limitations may facilitate conversations with members of the NASA Astronaut Corps that acknowledge that the quality of evidence could be improved, which could in turn support shared decision making and increase trust and transparency.
While evidence suggests that multiple forms of communicating uncertainty may be beneficial, caution is warranted. Evidence-based practice also recommends simplifying and highlighting the essential information (Zikmund-Fisher et al., 2010). In the absence of evidence-based evaluations of NASA’s specific communications practices and materials, it is unclear how to best strike the balance between enough information and too much information, especially with regard to the communication of uncertainty.
Risk Matrices and Traffic Light Color Coding
As described previously, Figure 4-1 is a matrix containing three bands colored in green, yellow, and red as a “traffic light” to represent increasing risk. Each band contains numerical and evaluative information on the risk, as well as risk management information relevant to mission assignments. Although matrices can be helpful in tracking and prioritizing risks, they pose several communication challenges. The categorization of risk consequences is subjective, as it reflects a specific risk attitude, and therefore it
is best practice to be transparent about how risk categorization decisions are made (Cox, 2008).
Colors can be helpful in risk communication (Hill et al., 2010; Severtson and Henriques, 2009; Sutton and Fischer, 2021). Traffic light color-coded communications are used in numerous contexts to communicate risks, including health risks (Neuner-Jehle et al., 2011). For example, when used in nutrition labeling (Emrich et al., 2017), the traffic light has the advantage of being familiar to lay audiences and consequently can be more effective than numeric labels at influencing food purchases (Trudel et al., 2015; Zhang et al., 2020). The use of traffic light color coding may be particularly familiar to astronauts, because NASA uses this system to visualize other risks (Dillon et al., 2018, 2019).
In the context of radiation, colors represent approximate relative magnitude of risk; that is, they inherently provide evaluative descriptions of each band as “low,” “medium,” or “high.” In the case of radiation, stochastic health risks from radiation exposure increase continually with increased exposure, rather than in a stepwise fashion with distinct cutoffs or endpoints for risk levels. Therefore, categorizing radiation risks into traffic light color-coded bands may not accurately represent the risk. Additionally, the traffic light color-coded system could be intended to convey information on decision making: green means go, yellow slow, and red stop. In the case of Figure 4-1, it is not clear that distinct risk management decisions correspond to each band. It is particularly unclear if the red band means stop, because the waiver process is mentioned within the red band (see further discussion on the waiver below).
Shortcomings in the use of color-coded risk matrices at NASA have previously been identified. A study that assessed risks reported for NASA 21 Goddard Space Flight Center from the Cross Cutting Risk framework database from July 2015 to 2017 found that among 666 unique reported technical and programmatic risks, only 5 percent were categorized as red, 51 percent were yellow, and 44 percent were green (Dillon et al., 2018), consistent with extensive research showing tendencies for subjectively judged frequencies of risks to be compressed (overestimated for low probability risks, underestimated for high probability risks) (Fischhoff, 2015).
The committee reached the following conclusion:
Conclusion II: NASA has proposed to use a traffic light color-coded system to categorize and communicate space radiation risks. Without empirically testing the traffic light color-coded system, there is insufficient information to determine whether it is an effective way for NASA to communicate the space radiation risks to astronauts.
Anticipated Effects of the Communication
Ideally, any proposed communication tool or message should be designed based on stated communication goals, the evidence from prior research regarding how best to achieve those goals with the targeted audience, and at least exploratory (i.e., formative) empirical evaluations of the message or tool with representatives from the targeted audience. Anecdotal evidence was provided to the committee regarding astronaut radiation risk communications needs and experiences, but the committee was not given any systematic empirical evidence of risk communication effectiveness to review. NASA astronauts are heterogeneous and singularly dissimilar to general audiences (e.g., with regard to expertise and decision contexts), which further increases the difficulty of predicting the likely effects of specific risk communication tools, such as Figure 4-1, on NASA astronauts with regard to specific communication aims. While recognizing these challenges, the committee recommends modifying Figure 4-1 in light of current understanding of anticipated risk communication effects and ethical considerations (e.g., autonomy) as shown in Figure 4-2.
The committee reached the following conclusion:
Conclusion III: The committee reaches the conclusion that there are two concerns with the proposed traffic light system for communicating the space radiation health standard dose-based thresholds:
- At doses below the standard (i.e., in the green and yellow bands), there is insufficient clarity and detail about associated cancer risks.
- At doses above the standard (i.e., in the red band), inclusion of the waiver process suggests that an exception to the standard is built into the standard and its application.
The committee makes the following recommendation:
Recommendation 3: To inform astronauts about their radiation risk, NASA should provide all astronauts with an individual radiation risk assessment and revise the risk communication system (i.e., the traffic light) for the updated space radiation standard to do the following:
- Assess and communicate the radiation risk at an individual level (as opposed to generic risk assessments) for all astronauts independent of the actual or projected radiation exposure and risk.
- Communicate the mean value of the risk estimate associated with an astronaut’s radiation exposure.
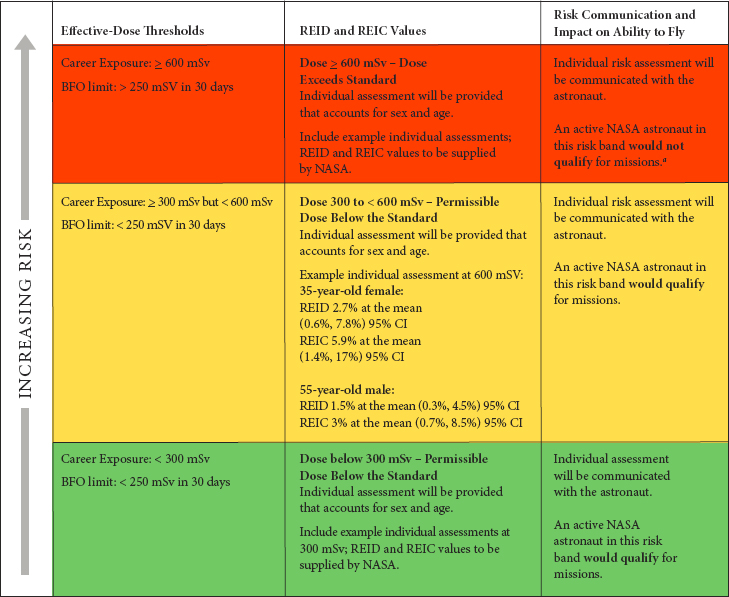
NOTES: Limits encompass cancer, cardiovascular, and central nervous system. Cancer is the constraining factor. BFO = blood forming organs; CI = confidence interval; mSv = millisievert; NASA = National Aeronautics and Space Administration; REIC = risk of exposure-induced cancer; REID = risk of exposure-induced death.
a Exposures ≥ 600 mSv would require a waiver of the standard by the agency based on considerations of national imperative, how essential the mission is, and individual risk considerations.
SOURCE: Created by the committee based on NASA’s proposed visual aid.
- Communicate the uncertainties for the risk distribution using both uncertainty intervals and limits, and visual representations of the risk distribution such as probability density curves, histograms, or heat maps.
- Address specific questions and concerns that individual astronauts may have regarding their overall health risks following communication of their actual or projected radiation dose, and help them place radiation risks into perspective compared to other mission risks.
The committee understands NASA may want to continue to use the traffic light color-coded method of communication because it is familiar to astronauts and is similar to risk matrices used to communicate other human health risks. If the traffic light communication system is used to convey radiation cancer risk, then the committee proposes modifications to Figure 4-1 (NASA’s diagram), which are shown in Figure 4-2. Specific updates include
- Remove the mention of the waiver from the red band.
- Explicitly label the red band as exceeding the standard.
- Replace evaluative descriptions of each band (low, medium, and high) with more appropriate risk management terms describing each band in the context of the standard, such as acceptable dose and dose exceeds standard.
- Include information on whether or not an astronaut qualifies for missions in each band.
The committee would like to note that the effectiveness of the modified matrix also needs to be tested.
The committee makes the following recommendation:
Recommendation 4: NASA should communicate a comprehensive picture of an individual astronaut’s cancer risks due to radiation exposure, beyond the information contained in the traffic light system. To do so, NASA should do the following:
- Respond to questions from astronauts regarding their total radiation exposure, and help astronauts put their radiation-induced cancer risk in context.
- Continue to discuss any changes in radiation risks as part of routine health briefings for the astronaut office, crews, and individual astronauts.
- Provide astronauts with an up-to-date resource on their radiation risks that they can access outside of formal meetings with NASA’s Office of the Chief Health and Medical Officer.
- Provide astronauts with easy access to summary information regarding what is known about the cancer risk factors that might interact with radiation exposures to influence long-term health outcomes for astronauts.
RISK COMMUNICATION AND NASA’S WAIVER PROCESS
Protection of the health and safety of astronauts is handled differently than for any other profession. Workers in terrestrial professions are primarily protected by health and safety standards and regulations established by the Occupational Safety and Health Administration (OSHA). However, the OSHA ground-based radiation standards do not apply to astronauts engaged in spaceflight. Instead, NASA is required to “establish supplemental standards appropriate for space missions” (Locke and Weil, 2016). For astronauts, NASA’s Health and Medical Technical Authority (HMTA) establishes and implements the agency’s own occupational exposure limits and other health standards, often relying on external scientific advice and expertise.
The mission of HMTA focuses on both the health and safety of astronauts and the viability of agency missions. To do this, HMTA standards, such as fitness for duty standards, are applied to individual astronauts to both protect the astronauts and also to assure they can perform at a level needed for any specific mission. NASA also establishes space permissible exposure limits (SPELs), which are quantifiable limits of exposure to a component of the environment during spaceflight over a given length of time, such as limits on lifetime radiation exposure (NASA, 2014). NASA’s exposure limits, like those of other agencies and organizations, consider the possibility or probability of adverse outcomes from hazards.
Exposure-related risk deemed acceptable by NASA is not specifically stated but it is implied by NASA SPELs and permissible outcome limits. NASA permissible outcome limits are described as the “acceptable maximum decrement or change in a physiological or behavioral parameter, during or after a spaceflight mission, as the result of exposure to the space environment” (NASA, 2014, p. 19).
Occupational exposure limits by OSHA and NASA, as well as those recommended by other agencies and nongovernmental organizations, are generally based on the best available scientific information when they are established. As a rule, there is a process for adjusting standards based on new or improved scientific information.
NASA generally addresses the need to meet a specific standard by implementing what is known as a hierarchy of controls, a well-established set of practices. For example, if the risk results from the use of a particular substance such as benzene or asbestos, NASA may choose to protect all employees by eliminating the use of the hazardous material and substituting a less hazardous alternative. When a chronic disease may result from cumulative exposure to a hazardous substance over time, NASA may choose to reduce the level of exposure to all employees through improved engineering and design, when and where it is feasible to do so. Exposure for any individual can also be reduced through “administrative controls,” such as
job assignments that take into consideration past accumulation of exposure and thus risk. An individual may be required to wear protective equipment designed to reduce risk associated with specific job duties.
If hazards associated with a particular potential work activity cannot be controlled or mitigated adequately using available technology, the employer may decide to postpone or abandon the potential work activity until they or others develop the technology needed to control the risk to the desired level.
However, space exploration missions may face challenges to risk mitigation that are not typically found in terrestrial high-hazard work. Terrestrial workers in high-risk jobs may choose to end their exposures by leaving their job. This is likely not the case for astronauts, particularly those on long-duration missions beyond low Earth orbit. An astronaut’s commitment to any particular mission is generally irrevocable once in space. There may be missions that the agency believes are so time sensitive and have sufficient urgency that there is justification for exceeding the established standard for all astronauts. In this instance, unlike employers subject to OSHA standards, NASA may seek to obtain permission for a mission waiver that would permit the agency to subject all volunteers for that mission to an unusual level of risk that would be unacceptable in less time-sensitive and critical missions.
Waivers for specific missions and potentially for individual participation in any given mission were considered in depth by the Institute of Medicine’s Committee on Ethics Principles and Guidelines for Health Standards for Long Duration and Exploration Spaceflights (IOM, 2014). That committee recommended that NASA follow a three-level, ethics-based decision framework when considering a waiver to an existing standard or standards. The threshold consideration would be to consider and explicitly make a determination as to whether “any missions that are unlikely to meet current health standards are ethically acceptable” and if so, what “specific conditions must be fulfilled” to approve the waiver (IOM, 2014, p. 144). The 2014 committee expected NASA would make this general determination to establish and articulate criteria independent of any specific mission and that these criteria would be known both to the NASA Astronaut Corps and the general public. Once the criteria were established, the 2014 committee recommended that NASA consider “whether a specific mission is ethically acceptable” by determining whether the particular mission meets the mission-independent criteria established and communicated by NASA (IOM, 2014, p. 144). If NASA decides the specific contemplated mission meets these criteria, the agency would then be in a position to consider individual astronaut participation and crew composition. This consideration would include the skills and expertise needed for the mission, as well as astronauts’ individual health and risk considerations. Astronauts would be making these decisions alongside NASA at this stage (IOM, 2014).
The waiver process recommended previously is consistent with the process of “justification” described by the International Commission on Radiological Protection (ICRP, 2007a). It notes that certain necessary occupational activities may result in uncontrolled exposures that exceed established limits. The ICRP says that these exposures need to be “justified” by a process that often includes public consultation:
The responsibility for judging the justification usually falls on governments or national authorities to ensure an overall benefit in the broadest sense to society and thus not necessarily to each individual. However, input to the justification decision may include many aspects that could be informed by users or other organizations or persons outside of government. As such, justification decisions will often be informed by a process of public consultation. (ICRP, 2007a)
NASA has not established an upper limit for its proposed waiver process. The main purpose for an upper dose limit to the waiver is to provide additional protection to astronauts from the expected adverse health effects of high radiation doses. High radiation doses carry high risks for cancer induction in the future and could induce tissue reactions (deterministic effects) (ICRP, 2007b). For example, on board a spacecraft, shielding and operational dosimetry systems are used effectively to mitigate exposure to a solar particle event (SPE). However, it is difficult to predict when an SPE will occur and how intense the radiation will be. If astronauts are performing an extravehicular activity in space or on a planetary surface when an SPE occurs, they could be in serious jeopardy. While an upper limit for the waiver is appropriate, the committee does not see it as appropriate to recommend to NASA what an upper limit should be.
The committee’s view is that the process of issuing a waiver needs to be separate from the process of setting, adhering to, and communicating the radiation health standard. As such, providing a recommendation on the radiation dose limit for the waiver is outside this committee’s task, which focuses on the assessment of the proposed revised radiation standard and effective risk management and communication. Establishing a universal upper limit to the waiver independent of the mission could lessen the value of setting and adhering to the radiation health standard, which in turn creates communication challenges on what the actual occupational health limit is. The goals of the missions that would require a waiver to individual astronauts could include advancing science and technology, space exploration, or national imperative. Therefore, the specific need to carry out a mission could differ in significance and urgency. NASA needs to maintain authority over the decision to carry out a mission as well as over the decision to issue a waiver to its astronauts following an established process.
The fact that NASA serves as both the employer and the organization that establishes and assures compliance with its own health standards confers particular ethical responsibilities and opens the agency to a high level of public scrutiny. The previous committee report (IOM, 2014) described the ethical principles serving as the foundation for this recommended stepwise process.
The committee reached the following conclusion regarding NASA’s waiver process:
Conclusion IV: The committee recognizes that NASA’s inclusion of the waiver in its space radiation risk management process may be necessary to maintain the flexibility for the agency to pursue missions in which astronauts are exposed to radiation doses that exceed its standard. The committee concludes there is a need for an explicit and public framework for how NASA will consider both mission and individual waivers.
The committee makes the following recommendation:
Recommendation 5: NASA should develop a protocol for waiver of the proposed space radiation standard that is judicious, transparent, and informed by ethics. To avoid the perception that an exception to the standard is built into the space radiation standard itself, NASA should follow the ethics decision framework in developing a waiver protocol and it should provide supporting analysis and explanation justifying any waiver to the standard.
RISK COMMUNICATION RESEARCH OPPORTUNITIES FOR NASA
Given the unique needs and characteristics of spaceflight programs and astronaut populations, NASA would benefit from engaging in risk communication evaluation and research. This would support evidence-based decision making about the use of specific metrics and visualizations. There is also an opportunity for NASA to contribute to important but under-researched questions in risk communication that would benefit other NASA programs and the field more broadly, such as communicating deep uncertainty. It is difficult to predict the effect of risk communications and empirical evidence is needed to determine if a particular communication has the intended effect. There is little existing risk communication research focused on astronauts or on communicating space radiation risk.
The discussion in this chapter highlights numerous opportunities to conduct risk communication research on NASA’s communications strategies and materials. It would be valuable to study the “red/yellow/green” tool
reviewed by this committee, strategies or templates used by flight surgeons in pre- and post-mission consultations, other communications materials and strategies used by NASA, and any tools or materials NASA might develop for astronauts to use at their own discretion for individualized radiation risk modeling or assessment. The published literature cited in this chapter includes many examples of empirical studies that illustrate viable approaches for designing and evaluating risk communications and methodological advances in risk communication research. One challenge in this instance is that the active NASA Astronaut Corps is a small population that could easily be overtaxed by risk communication studies. It would be valuable to characterize other populations and determine the extent to which their risk perceptions can and cannot be generalized to astronauts. Retired astronauts or astronauts in training may be a suitable population, as well as radiation professionals who have similar levels of expertise and numeracy.
The committee makes the following recommendation:
Recommendation 6: NASA should conduct research to develop evidence-based risk communication and the agency should develop a radiation risk communication research agenda to fill knowledge gaps such as (1) what information astronauts want; (2) how astronauts process risk information; and (3) who/what are the most effective sources of information for astronauts. In addition, NASA should carry out research to examine and improve the effectiveness of its current and proposed risk communication strategies and materials.
REFERENCES
Albada, A., M. G. Ausems, J. M. Bensing, and S. van Dulmen. 2009. Tailored information about cancer risk and screening: A systematic review. Patient Education and Counseling 77(2):155–171.
Ancker, J. S., Y. Senathirajah, R. Kukafka, and J. B. Starren. 2006. Design features of graphs in health risk communication: A systematic review. Journal of the American Medical Informatics Association 13(6):608–618.
Balog-Way, D., K. McComas, and J. Besley. 2020. The evolving field of risk communication. Risk Analysis 40(S1):2240–2262.
Brug, J., K. Glanz, P. Van Assema, G. Kok, and G. J. Van Breukelen. 1998. The impact of computer-tailored feedback and iterative feedback on fat, fruit, and vegetable intake. Health Education & Behavior 25(4):517–531.
Budescu, D. V., and T. S. Wallsten. 1995. Processing linguistic probabilities: General principles and empirical evidence. Psychology of Learning and Motivation 32:275–318.
Budescu, D. V., S. Broomell, and H. H. Por. 2009. Improving communication of uncertainty in the reports of the Intergovernmental Panel on Climate Change. Psychological Science 20(3):299–308.
Budescu, D. V., H.-H. Por, S. B. Broomell, and M. Smithson. 2014. The interpretation of IPCC probabilistic statements around the world. Nature Climate Change 4(6):508–512.
Cairns, G., M. de Andrade, and L. MacDonald. 2013. Reputation, relationships, risk communication, and the role of trust in the prevention and control of communicable disease: A review. Journal of Health Communication 18(12):1550–1565.
Cokely, E. T., A. Feltz, S. Ghazal, J. N. Allan, D. Petrova, and R. Garcia-Retamero. 2018. Skilled decision theory: From intelligence to numeracy and expertise. In The Cambridge handbook of expertise and expert performance, edited by K. A. Ericsson, R. R. Hoffman, A. Kozbelt, and A. M. Williams. Cambridge, UK: Cambridge University Press. Pp. 476–505.
Cox, L. A., Jr. 2008. What’s wrong with risk matrices? Risk Analysis 28(2):497–512.
Cucinotta, F. A. 2010. Radiation risk acceptability and limitations. https://three.jsc.nasa.gov/articles/astronautradlimitsfc.pdf (accessed May 10, 2021).
Dieckmann, N. F., R. Mauro, and P. Slovic. 2010. The effects of presenting imprecise probabilities in intelligence forecasts. Risk Analysis 30(6):987–1001.
Dieckmann, N. F., E. Peters, and R. Gregory. 2015. At home on the range? Lay interpretations of numerical uncertainty ranges. Risk Analysis 35(7):1281–1295.
Dillon, R. L., G. A. Klein, E. W. Rogers, and C. J. Scolese. 2018. Improving the use of risk matrices at NASA. In 2018 IEEE Aerospace Conference. Big Sky, MT: IEEE. Pp. 1–11.
Dillon, R. L., G. A. Klein, E. W. Rogers, and C. J. Scolese. 2019. Valuing rigor in the risk management process. In 2019 IEEE Aerospace Conference. Big Sky, MT: IEEE. Pp. 1–13.
Edwards, A. G., G. Naik, H. Ahmed, G. J. Elwyn, T. Pickles, K. Hood, and R. Playle. 2013. Personalised risk communication for informed decision making about taking screening tests. Cochrane Database Systematic Review Feb 28(2):CD001865.
Emrich, T. E., Y. Qi, W. Y. Lou, and M. R. L’Abbe. 2017. Traffic-light labels could reduce population intakes of calories, total fat, saturated fat, and sodium. PloS One 12(2):e0171188.
Fischhoff, B. 2012. Communicating uncertainty fulfilling the duty to inform. Issues in Science and Technology 28(4):63–70.
Fischhoff, B. 2015. Risk perception and communication. In Oxford textbook of global public health, 6th ed., edited by R. Detels, M. Gulliford, Q. Abdool Karim, and C. Chuan Tan. Oxford, UK: Oxford University Press.
Fischhoff, B., and A. L. Davis. 2014. Communicating scientific uncertainty. Proceedings of the National Academy of Sciences 111(Suppl 4):13664–13671.
Fischhoff, B., and D. A. Scheufele. 2013. The science of science communication. Proceedings of the National Academy of Sciences 110(Suppl 3):14031–14032.
Fischhoff, B., and D. A. Scheufele. 2014. The science of science communication II. Proceedings of the National Academy of Sciences 111(Suppl 4):13583–13584.
Fischhoff, B., and D. A. Scheufele. 2019. The science of science communication III. Proceedings of the National Academy of Sciences 116(16):7632–7633.
Fischhoff, B., N. T. Brewer, and J. S. Downs. 2011. Communicating risks and benefits: An evidence-based user’s guide. https://www.fda.gov/media/81597/download (accessed April 27, 2021).
Galesic, M., and R. Garcia-Retamero. 2011. Communicating consequences of risky behaviors: Life expectancy versus risk of disease. Patient Education and Counseling 82(1):30–35.
Garcia-Retamero, R., and E. T. Cokely. 2017. Designing visual aids that promote risk literacy: A systematic review of health research and evidence-based design heuristics. Human Factors 59(4):582–627.
Griffin, R. J., K. Neuwirth, S. Dunwoody, and J. Giese. 2004. Information sufficiency and risk communication. Media Psychology 6(1):23–61.
Han, P. K., W. M. Klein, T. Lehman, B. Killam, H. Massett, and A. N. Freedman. 2011. Communication of uncertainty regarding individualized cancer risk estimates: Effects and influential factors. Medical Decision Making 31(2):354–366.
Hawkins, R. P., M. Kreuter, K. Resnicow, M. Fishbein, and A. Dijkstra. 2008. Understanding tailoring in communicating about health. Health Education Research 23(3):454–466.
Hess, R., V. H. Visschers, and M. Siegrist. 2011. Risk communication with pictographs: The role of numeracy and graph processing. Judgment and Decision Making 6(3):263–274.
Hill, S., J. Spink, D. Cadilhac, A. Edwards, C. Kaufman, S. Rogers, R. Ryan, and A. Tonkin. 2010. Absolute risk representation in cardiovascular disease prevention: Comprehension and preferences of health care consumers and general practitioners involved in a focus group study. BMC Public Health 10(1):1–13.
Hsee, C. K. 1995. Elastic justification: How tempting but task-irrelevant factors influence decisions. Organizational Behavior and Human Decision Processes 62(3):330–337.
Ibrekk, H., and M. G. Morgan. 1987. Graphical communication of uncertain quantities to nontechnical people. Risk Analysis 7(4):519–529.
ICRP (International Commission on Radiological Protection). 2007a. The 2007 recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of the ICRP 37(2–4):1–332.
ICRP. 2007b. Radiological protection in medicine: Publication 105. Annals of the ICRP 37(6).
IOM (Institute of Medicine). 2014. Health standards for long duration and exploration spaceflight: Ethics principles, responsibilities, and decision framework. Washington, DC: The National Academies Press.
Johnson, B. B., and P. Slovic. 1998. Lay views on uncertainty in environmental health risk assessment. Journal of Risk Research 1:261–279.
Keller, C. 2011. Using a familiar risk comparison within a risk ladder to improve risk understanding by low numerates: A study of visual attention. Risk Analysis 31(7):1043–1054.
Kreuter, M. W., D. W. Farrell, L. R. Olevitch, and L. K. Brennan. 2013. Tailoring health messages: Customizing communication with computer technology. Abingdon-on-Thames, UK: Routledge.
Kreuzmair, C., M. Siegrist, and C. Keller. 2016. High numerates count icons and low numerates process large areas in pictographs: Results of an eye tracking study. Risk Analysis 36(8):1599–1614.
Locke, P. A., and M. M. Weil. 2016. Personalized cancer risk assessments for space radiation exposures. Frontiers in Oncology 6:38.
Manski, C. F. 2019. Communicating uncertainty in policy analysis. Proceedings of the National Academy of Sciences 116(16):7634–7641.
McComas, K. A. 2006. Defining moments in risk communication research: 1996–2005. Journal of Health Communication 11(1):75–91.
Morgan, M. G., B. Fischoff, A. Bostrom, and C. Atman. 2002. Risk communication: A mental models approach. New York: Cambridge University Press.
NASA (National Aeronautics and Space Administration). 2014. NASA spaceflight human system standard. Vol. 1, revision A: Crew health. NASA-STD-3001. https://standards.nasa.gov/standard/nasa/nasa-std-3001-vol-1 (accessed April 16, 2021).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2017. Communicating science effectively: A research agenda. Washington, DC: The National Academies Press.
NCRP (National Council on Radiation Protection and Measurements). 2014. Commentary 23: Radiation protection for space activities: Supplement to previous recommendations. Bethesda, MD: National Council on Radiation Protection and Measurements.
Neuner-Jehle, S., O. Senn, O. Wegwarth, T. Rosemann, and J. Steurer. 2011. How do family physicians communicate about cardiovascular risk? Frequencies and determinants of different communication formats. BMC Family Practice 12(1):1–9.
Noar, S. M., C. N. Benac, and M. S. Harris. 2007. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin 133(4):673.
Noar, S. M., N. G. Harrington, and R. S. Aldrich. 2009. The role of message tailoring in the development of persuasive health communication messages. Annals of the International Communication Association 33(1):73–133.
NRC (National Research Council). 1989. Improving risk communication. Washington, DC: National Academy Press.
Okan, Y., M. Galesic, and R. Garcia-Retamero. 2016. How people with low and high graph literacy process health graphs: Evidence from eye-tracking. Journal of Behavioral Decision Making 29(2–3):271–294.
Padilla, L. M., M. Powell, M. Kay, and J. Hullman. 2020. Uncertain about uncertainty: How qualitative expressions of forecaster confidence impact decision-making with uncertainty visualizations. Frontiers in Psychology 11:3747.
Perko, T. 2014. Radiation risk perception: A discrepancy between the experts and the general population. Journal of Environmental Radioactivity 133:86–91.
Perneger, T.V., and Agoritsas, T. 2011. Doctors and patients’ susceptibility to framing bias: A randomized trial. Journal of General Internal Medicine 26:1411–1417.
Politi, M. C., P. K. Han, and N. F. Col. 2007. Communicating the uncertainty of harms and benefits of medical interventions. Medical Decision Making 27(5):681–695.
Richards, K. C., C. A. Enderlin, C. Beck, J. C. McSweeney, T. C. Jones, and P. K. Roberson. 2007. Tailored biobehavioral interventions: A literature review and synthesis. Research and Theory for Nursing Practice 21(4):271–285.
Rimer, B. K., and B. Glassman. 1998. Tailoring communications for primary care settings. Methods of Information in Medicine 37(2):171–178.
Roth, E., M. G. Morgan, B. Fischhoff, L. Lave, and A. Bostrom. 1990. What do we know about making risk comparisons? Risk Analysis 10:375–387.
Savelli, S., and S. Joslyn. 2013. The advantages of predictive interval forecasts for non-expert users and the impact of visualizations. Applied Cognitive Psychology 27:527–541.
Semones, E. 2021. Space radiation overview, history, NSCR model, implementation. Presentation to the Committee on Assessment of Strategies for Managing Cancer Risks Associated with Radiation Exposure During Crewed Space Missions, January 25.
Severtson, D. J., and J. B. Henriques. 2009. The effect of graphics on environmental health risk beliefs, emotions, behavioral intentions, and recall. Risk Analysis: An International Journal 29(11):1549–1565.
Skinner, C. S., V. J. Strecher, and H. Hospers. 1994. Physicians’ recommendations for mammography: Do tailored messages make a difference? American Journal of Public Health 84(1):43–49.
Sohl, S. J., and A. Moyer. 2007. Tailored interventions to promote mammography screening: A meta-analytic review. Preventive Medicine 45(4):252–261.
Spiegelhalter, D. 2017. Risk and uncertainty communication. Annual Review of Statistics and Its Application 4(1):31–60.
Sutton, J., and L. M. Fischer. 2021. Understanding visual risk communication messages: An analysis of visual attention allocation and think-aloud responses to tornado graphics. Weather, Climate, and Society 13(1):173–188.
Teigen, K. H., and E. Løhre. 2017. Expressing (un)certainty in no uncertain terms: Reply to Fox and Ülkümen. Thinking & Reasoning 23(4):492–496.
Trudel, R., K. B. Murray, S. Kim, and S. Chen. 2015. The impact of traffic light color-coding on food health perceptions and choice. Journal of Experimental Psychology: Applied 21(3):255.
van der Bles, A. M., S. van der Linden, A. L. J. Freeman, J. Mitchell, A. B. Galvao, L. Zaval, and D. J. Spiegelhalter. 2019. Communicating uncertainty about facts, numbers, and science. Royal Society Open Science 6(5):181870.
van der Bles, A. M., S. van der Linden, A. L. Freeman, and D. J. Spiegelhalter. 2020. The effects of communicating uncertainty on public trust in facts and numbers. Proceedings of the National Academy of Sciences 117(14):7672–7683.
Viscusi, W. K., W. A. Magat, and J. Huber. 1991. Communication of ambiguous risk information. Theory and Decision 31(2–3):159–173.
Yang, B. W., C. Vargas-Restrepo, M. L. Stanley, and E. J. Marsh. 2021. Truncating bar graphs persistently misleads viewers. Journal of Applied Research in Memory and Cognition. ePub date February 16.
Zhang, X., Y. Liu, Y. Gu, S. Wang, and H. Chen. 2020. Red for “stop”: “Traffic-light” nutrition labels decrease unhealthy food choices by increasing activity and connectivity in the frontal lobe. Nutrients 12(1):128.
Zikmund-Fisher, B. J., A. Fagerlin, and P. A. Ubel. 2010. A demonstration of “less can be more” in risk graphics. Medical Decision Making 30(6):661–671.
This page intentionally left blank.
























