Proceedings of a Workshop
| IN BRIEF | |
|
SEPTEMBER 2021 |
Pivotal Interfaces of Environmental Health and Infectious Disease Research to Inform Responses to Outbreaks, Epidemics, and Pandemics
Proceedings of a Workshop—in Brief
INTRODUCTION
Pathogens are the cause of infectious diseases, but the environment can play an important role in influencing the conditions under which pathogens spread and cause harm. For example, factors such as temperature, precipitation, land use, and social dynamics can affect the likelihood that people will be exposed to infectious agents, while exposure to pollutants may affect the severity of the disease in those who become infected. Understanding the complex interplay among people, pathogens, and the environment—broadly encompassing the chemical, biological, physical, and social surroundings—can lead to a more complete picture of where and how infectious diseases emerge, how they spread, and how to respond to outbreaks. As understanding of the environment’s role in infectious disease increases, this knowledge can help to inform and improve tools for monitoring, containing, and preventing outbreaks, epidemics, and pandemics.
The virtual workshop Pivotal Interfaces of Environmental Health and Infectious Disease Research to Inform Responses to Outbreaks, Epidemics, and Pandemics was held on June 8–9, 2021. This workshop provided a venue for experts in infectious diseases, environmental health, and data science from government, academia, and the private sector to examine current knowledge about the environment–infectious disease interface and to explore how this knowledge can be used to inform public health decisions. Key workshop topics included how advances in environmental exposure assessments can be applied to identify, predict, and monitor critical infectious disease exposure pathways, and how climate and environmental modeling techniques can be applied to better understand the biology and transmission dynamics of pathogens and provide early warning of emerging threats. In addition, workshop sessions explored critical data gaps at the environment–infectious disease interface and provided insight on how new and emerging techniques can be applied to address those data gaps, especially through the integration of tools used in environmental health and infectious disease research.
This Proceedings of a Workshop—in Brief provides the rapporteurs’ high-level summary of the topics addressed in the workshop, including participants’ suggestions for advancing research, improving models, and applying tools to enhance infectious disease preparedness and response. Additional details and ideas can be found in materials available online, including videos, slides, and breakout group reports.1 Readers are encouraged to use this proceedings to gain insight into potential opportunities for action but should not view these ideas as consensus conclusions or National Academies recommendations.
________________
1 See https://www.nationalacademies.org/our-work/pivotal-interfaces-of-environmental-health-and-infectious-disease-researchto-inform-responses-to-outbreaks-epidemics-and-pandemics-a-workshop.
![]()
Workshop Impetus and Organization
The workshop was organized by a planning committee of the Standing Committee on the Use of Emerging Science for Environmental Health Decisions, a program of the National Academies of Sciences, Engineering, and Medicine focused on the use of new science, tools, and methodologies for environmental health research and decisions. The event built on the 2019 workshop Toward Understanding the Interplay of Environmental Stressors, Infectious Diseases, and Human Health.2 In an introductory video, Melissa Perry (The George Washington University), chair of the 2021 workshop, and Robert Newman (The Aspen Institute), chair of the 2019 workshop, described how the two events together draw attention to the critical need to foster community, facilitate communication, and enhance collaboration to investigate the environment–infectious disease interface and integrate the knowledge gained into public health strategies. Emerging between the two workshops, the COVID-19 pandemic has only increased the sense of urgency for closing knowledge gaps and improving public health interventions. Newman and Perry noted that while pandemics are inevitable, the ability to respond effectively depends on society’s capacity to leverage scientific knowledge and tools, translate insights into interventions, and communicate and collaborate across communities.
While the 2019 workshop focused on the interplay among environmental stressors, infectious disease, and human health at the individual level, the 2021 workshop focused on the environment’s role in infectious disease across populations. In a series of presentations and panel discussions, participants examined the application of environmental science perspectives to pathogen transmission, the translation of technical tools from environmental surveillance to monitor and predict the spread of infectious disease, and the integration of complex data sets to enable the transition from data collection to data utilization. Participants also explored new, emerging, and potential future uses of big data and artificial intelligence (AI) at the interface of infectious disease and environmental health. In breakout sessions, attendees built on the strategies discussed during workshop plenary sessions to reflect on research needs and policy interventions relevant to four hypothetical real-world scenarios at the intersection of environmental health and infectious disease (summarized in Boxes 1–4). These scenarios included airborne exposure and detection (see Box 1 on p. 5); wastewater surveillance and waterborne exposure (see Box 2 on p. 7); antimicrobial resistance emergence (see Box 3 on p. 8); and environmental change (see Box 4 on p. 11).
Throughout all of this workshop’s activities, many attendees emphasized the importance of cross-disciplinary collaboration among environmental health and infectious disease experts to improve infectious disease research and response, discussed the range of stakeholders and types of expertise from which these collaborations could benefit, identified barriers to establishing effective partnerships, and explored opportunities to enhance collaborative efforts to combat existing and future health threats.
Agency Perspectives
Cristina Cassetti (National Institute of Allergy and Infectious Diseases [NIAID]) and Gwen Collman (National Institute of Environmental Health Sciences [NIEHS]) offered perspectives from two U.S. government agencies that play a lead role in advancing research at the intersection of environmental health and infectious disease.
NIAID has a dual mandate to advance scientific knowledge and respond to infectious disease threats, said Cassetti. Drawing examples from NIAID’s decades of experience in these areas, Cassetti described how environmental factors influence where and how diseases emerge, points of interaction between pathogens and humans, and the spread of disease. She noted how the environment can play a role in enabling (or blocking) infectious disease at each of four main stages: exposure, infection, transmission, and epidemic spread. For example, changes in land use such as deforestation and habitat fragmentation can increase exposure by bringing humans into closer contact with animals such as bats that transmit zoonotic diseases, a dynamic that led to outbreaks of Nipah virus in Southeast Asia. Cassetti explained how changes in the movement of people, such as through increased urbanization and international travel, can facilitate the spread of pathogens to new areas, exemplified in the movement of West Nile virus to North America from Europe. Changes in weather and climate can also cause ecological cascades that set the stage for diseases to emerge, as happened in the Southwestern United States when a confluence of weather conditions led to a spike in deer mouse populations that fueled
________________
2 National Academies of Sciences, Engineering, and Medicine. 2019. Toward Understanding the Interplay of Environmental Stressors, Infectious Diseases, and Human Health: Proceedings of a Workshop—in Brief. Washington, DC: The National Academies Press. https://doi.org/10.17226/25493.
an outbreak of hantavirus. Given the influence of the environment in past outbreaks, Cassetti stressed the importance of integrating environmental data into efforts to predict and prevent future outbreaks, including the work of the Centers for Research in Emerging Infectious Diseases,3 a global research network NIAID established in 2020 to facilitate infectious disease research, surveillance, and data sharing.
NIEHS advances understanding of how the environment affects human health. Collman described four main ways environmental exposures and infectious agents cause or exacerbate disease: (1) pathogens and toxicants can cause disease alone or in combination; (2) the association between a pathogen and a disease can be altered by the presence of a chemical toxicant; (3) the association between a chemical toxicant and a disease can be altered by the presence of a pathogen; and (4) environmental exposures can cause co-morbidities that influence a person’s susceptibility to infectious diseases. While scientists have learned a great deal about these relationships, Collman noted that much remains that is unknown. For example, it is unclear if exposure to toxicants such as dioxin, polychlorinated biphenyls, heavy metals, or endocrine-disrupting chemicals may modify a person’s response to vaccines, potentially affecting the containment of diseases such as COVID-19 at the population level. To enhance understanding of the complex environmental influences on infectious disease dynamics and translate this understanding into better public health responses, Collman suggested taking a broader view of which populations face increased risks from infectious diseases, measuring environmental exposures across populations, exploring the relationship between environmental exposures and disease susceptibility and response, and translating this work into public policy and clinical practice.
To better bridge between environmental health and infectious disease research, Cassetti and Collman pointed to a need for cross-disciplinary collaboration and team science approaches, which could lead to more creative and innovative research to ask and answer new types of questions. In particular, Cassetti suggested that collaboration between public health researchers and ecologists could improve understanding and the prediction of vector-borne diseases, while Collman said that integrating data on infectious diseases into long-term cohort studies on environmental exposures could further elucidate how the environment and pathogens interact to cause or exacerbate disease.
KNOWLEDGE AND TOOLS AT THE ENVIRONMENT–INFECTIOUS DISEASE INTERFACE
Understanding Exposure and Transmission
Basic science and modeling studies have helped elucidate some of the myriad ways environmental factors might affect exposure to pathogens and the pathways through which diseases spread. Speakers and panelists highlighted research insights in this area and underscored the importance of accounting for environmental factors in models to understand and predict outbreaks, particularly as changes in climate and land use may alter many of these factors.
Donald Milton (University of Maryland, College Park) noted that studies at the environment–infectious disease interface have a long history, going back, for example, to studies of aerosols and the transmission of tuberculosis in the 1950s. While this work provided important foundational knowledge and highlighted the value of collaboration between medical and environmental experts, Milton noted that the dissemination of knowledge, particularly on aerosols, has been limited by classified work and biodefense concerns. More recently, as scientists have learned more about pathogen transmission, such as through the Evaluating Modes of Influenza Transmission study,4 researchers have worked to adapt epidemiological models, such as the susceptible-exposed-infectious-removed model, to include environmental conditions. To further improve understanding of pathogen transfer processes and inform control and prevention efforts, Milton suggested it will be important to delineate the differences between touch, spray, and inhalation routes of transmission; to further investigate how the environment influences host susceptibility; and to integrate this knowledge into models of disease spread.
Similarly, Joseph Eisenberg (University of Michigan) described how he and collaborators have extended the traditional susceptible-infectious-removed (SIR) model to include a variety of environmental parameters in an effort to capture a more comprehensive picture of infectious disease dynamics. While scientists and public health practitioners frequently divide diseases by taxonomic grouping, Eisenberg said that when focusing on environmental determinants of how infectious diseases spread, it is useful to group them by the process through
________________
which they are transmitted. Eisenberg described four general categories of transmission systems for pathogens: (1) direct transmission, in which a pathogen is transmitted person to person via intimate proximity with no environmental reservoir of the pathogen; (2) vector-borne transmission, in which a pathogen is transmitted via a vector (biting arthropods such as mosquitoes and ticks) from an infected human host to a susceptible human host, a process that could also involve nonhuman intermediate or alternative hosts; (3) environmentally mediated transmission, in which a pathogen is transmitted to a susceptible human host via the environment with or without the presence of a nonhuman host (examples include respiratory, waterborne, and foodborne pathogens); and (4) zoonotic transmission, in which animals serve as the natural host and reservoir for a pathogen but susceptible human hosts can become infected through various means of transmission (see Figure 1).
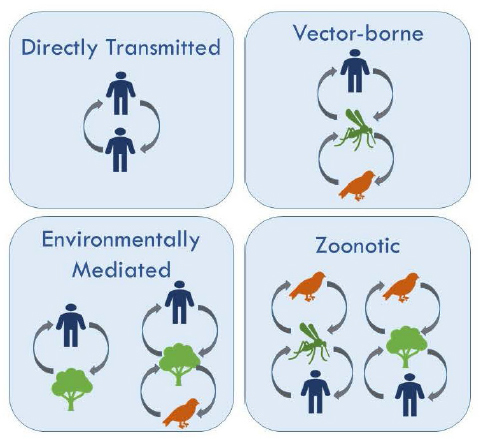
Although the environment’s role is explicit in only one of these categories, Eisenberg noted that environmental factors are present in all of them. He discussed that even transfer routes considered “direct,” such as those for respiratory, foodborne, or waterborne pathogens, can be heavily influenced by environmental factors such as the concentration, persistence, and movement of pathogens in the environment and factors that affect where and how people come into contact with infectious agents. For example, Eisenberg said, temperature often affects the persistence of a pathogen in the environment, while precipitation often affects a waterborne pathogen’s transport through the environment. Studies of diarrheal disease in Ecuador, for example, show that a lack of rain causes waterborne pathogens to accumulate and then, during a precipitation event, the pathogens are released. In contrast, Eisenberg said, persistent rain dilutes pathogens and flushes them away. This dynamic is known as the concentration dilution hypothesis. Given the power of environmental measurements to elucidate such mechanisms in disease emergence and spread, Eisenberg urged a systems approach to epidemiology that incorporates the role of the environment in mediating interactions between hosts and infectious agents.
For vector-borne diseases transmitted by vectors, including mosquitoes, the environment can influence both the vectors themselves and the process through which humans are exposed to pathogens. Erin Mordecai (Stanford University) described how environmental changes in climate and land use, for example, can affect vector-borne disease dynamics. While the impacts are nonlinear, they can be predicted if models appropriately account for key environmental variables and relationships. For example, Mordecai explained how
temperature is a key factor in mosquito-borne diseases because it affects mosquitoes’ survival, fecundity, and rate of development. The optimal temperature for the transmission of mosquito-borne diseases, Mordecai said, is different for each pathogen and mosquito species;5 as a result, the same climate shift could have different implications for different diseases. In central Africa, for example, Mordecai’s work suggests that climate change is predicted to lead to an increase in dengue in areas where malaria is currently the primary threat,6 which would have important public health implications as the method of disease control differs between the two. Changes in land use can also alter the relationships between human populations and vectors, Mordecai explained, as exemplified in a bidirectional relationship between malaria transmission and forest clearing in the Brazilian Amazon.7 Mordecai urged attention to these important environmental dynamics in models and tools for informing public health decisions.
Some participants discussed how a greater understanding of the environment’s role in exposure and transmission could translate to more informed public health policy in a panel discussion that included presenters as well as M. Christian Bautista (U.S. Department of Defense), Wayne Cascio (U.S. Environmental Protection Agency), and Bill Lindsley (Centers for Disease Control and Prevention [CDC]). The discussion began with a focus on key gaps. Noting that only a tiny fraction of pathogens are responsible for fueling pandemics, Eisenberg stressed the need for basic biology to elucidate the components that cause transmission and allow pathogens to move efficiently through a population. He added that there is a need to better understand how environmental toxicants influence the susceptibility aspect of the SIR model. Milton and Lindsley pointed to a need for infrastructure to understand the source and transmission routes for pathogens, including enhanced disease surveillance, sequencing, and animal models to study disease, even (and perhaps especially) during “peacetime” between outbreaks.
Milton and Cascio noted the persistent challenge that lies in differentiating among transmission via touch, spray, and inhalation. These routes of transmission have drastically different implications for public health interventions, with disinfectants and surface cleaning playing a larger role when touch is a primary route of transmission and ventilation and air flow playing a key role for reducing inhalation-based transmission. Milton said ongoing studies are likely to advance understanding of the relative importance of these transmission routes for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, and other viruses in the coming years, but Milton and Cascio emphasized that it is important for public health decisions to remain responsive to the science as it evolves. For example, Milton cautioned that many school systems invested in plexiglass partitions for classrooms when this was thought to help block the spread of SARS-CoV-2 via spray droplets, but more recent evidence suggests that these partitions increase, rather than decrease, transmission via
BOX 1 Breakout Scenario on Airborne Exposure and Detection
Participants in this breakout session considered research and policy interventions relevant to the emergence of an unknown pathogen that is suspected to be airborne. Assuming uncertainties regarding the pathogen, its movement, and its impacts, participants discussed examples of research needs to inform outbreak response and interventions, including
- developing diagnostic tools and containment measures;
- validating novel technologies; and
- bridging research pillars between public health, laboratory science, epidemiology, and big data modeling.
Several participants suggested that research and policy interventions in an outbreak would be driven by the pathogen’s impacts and activities could focus on identifying data needs early on to inform decisions and clear communication, with robust recommendations informed by real-time, high-volume monitoring, analysis of transmission risk, and data integration across scales.
________________
5 Mordecai, E.A., J.M. Caldwell, M.K. Grossman, C.A. Lippi, L.R. Johnson, M. Neira, J.R. Rohr, S.J. Ryan, V. Savage, M.S. Shocket, R. Sippy, A.M. Stewart Ibarra, M.B. Thomas, and O. Villena. 2019. Thermal biology of mosquito-borne disease. Ecology Letters 22(10):1690–1708.
6 Mordecai, E.A., S.J. Ryan, J.M. Caldwell, M.M. Shah, and A.D. LaBeaud. 2020. Climate change could shift disease burden from malaria to arboviruses in Africa. The Lancet 4(9):E416–E423.
7 MacDonald, A.J., and E.A. Mordecai. 2019. Amazon deforestation drives malaria transmission, and malaria burden reduces forest clearing. Proceedings of the National Academy of Sciences 116(44):22212–22218.
smaller airborne particles by counteracting ventilation. Eisenberg added that the relative importance of various routes of transmission can depend not only on the virus but also on the venue and how people behave there. Strategies for reducing transmission may need to be different in a daycare versus a stadium, for example. Lindsley added that more work is needed to improve the ability to detect airborne viruses in air.
Milton noted that collaboration will be essential to further knowledge of disease transmission and translate knowledge into public health policy: “I think it is important to bring together the infectious disease community and the aerosols, industrial hygiene, and exposure science communities to be really talking to each other.... That’s the bridge we need to build.” There is precedent for such cross-disciplinary collaboration in the context of studying airborne pollutants and allergens, he noted, but less collaboration in the context of infectious disease. Eisenberg and Bautista added that social scientists are also crucial to this research, given the importance of individual behavior and the social determinants of health in transmission dynamics.
Disease Surveillance
David Larsen (Syracuse University) discussed the role of infectious disease surveillance as a means of supporting health security8 by confirming the absence of risk from a pathogen within a community or alerting communities to an increased risk from a pathogen. Many disease surveillance systems were overwhelmed during the first wave of the COVID-19 pandemic, which Larsen attributed to a heavy reliance on event-based diagnostic testing of individuals. He posited that wastewater surveillance, testing for a known pathogen’s genetic material in community wastewater, offers a complementary way to monitor infectious disease at the population level with several advantages over the testing of individuals. While wastewater surveillance cannot reveal which individuals are infected, this approach offers rapid insight into the presence (or absence) of a pathogen within a community. Importantly, it can provide early warning when transmission is increasing in an area—potentially weeks sooner than diagnostic testing—in time to implement measures to curb the spread. Larsen suggested the trajectory of the COVID-19 pandemic may have been quite different if wastewater surveillance systems had been in place at the start.
Participants explored the strengths and weaknesses of wastewater surveillance and other environmental monitoring approaches in a panel discussion. Bautista underscored the need for concrete, reliable surveillance information, noting that hints from social media or other sources can come too late or be too unreliable to inform accurate predictions. Cascio said it would be helpful to have a standardized methodology for detecting viral RNA and ways to associate detected RNA level in wastewater with infectivity, though Larsen noted that wastewater surveillance can be useful for informing public health decisions even before these details are fully understood. Eisenberg said that molecular techniques such as wastewater surveillance are particularly powerful for outbreaks that are more difficult to predict with traditional methods, such as the emergence of a novel virus. Mordecai added that it may be possible to use similar approaches to detect pathogens circulating in populations of wild animals for an early warning of vector-borne disease outbreaks.
Participants also raised several ethical considerations. Larsen noted that, because wastewater treatment plants typically cover fairly large populations, wastewater surveillance should not pose a privacy risk to individuals in the community. However, he said it is important to consider ethical and privacy implications for environmental monitoring approaches at smaller scales, such as the neighborhood level. Cascio emphasized the importance for policies and data collection to benefit marginalized communities.
Larsen, Lindsley, Milton, and Mordecai stressed the need to invest in public health capacity and communication to translate science to policy for better disease surveillance. Panelists mentioned that maintaining robust surveillance systems relies on adequate funding and attention to not only symptomatic cases of known diseases but also the capacity to detect novel diseases, asymptomatic cases, and the environmental conditions that make outbreaks more likely. “I think we’ve got to change the mindset of how we think about early warning systems being environmental instead of clinical,” Eisenberg said. In addition, Bautista, Eisenberg, and Larsen emphasized the need for surveillance systems to not only monitor infectious diseases but also report the findings in ways that are actionable for health officials. Larsen suggested training local public health departments on the appropriate use of environmental monitoring data, adding that it is important to continue monitoring even in the absence of disease outbreaks and to appropriately value negative results confirming that a pathogen is not present.
________________
8 See https://www.who.int/health-topics/health-security/#tab=tab_1.
BOX 2 Breakout Scenario on Wastewater Surveillance and Waterborne Exposure
Participants in this breakout session considered a scenario in which routine wastewater surveillance systems detect an unknown pathogen, while at the same time sick animals are found around wastewater sources. In this scenario, participants discussed possible components of a research agenda:
- determining if and how the animal cases are linked to the detected pathogen by examining geographic patterns;
- establishing clinical monitoring of human and animal populations;
- identifying the infectivity of the pathogen to determine if wastewater exposure is a primary exposure route to animals and humans; and
- sampling of wastewater inputs including those upstream and downstream of wastewater treatment plants.
To coordinate, facilitate, and potentially support these efforts, some participants suggested that wildlife and agricultural agencies could play a key role, and suggested that a One Health model could help to coordinate disease surveillance in veterinary and human clinics. Some participants noted a desire to invest in capacity for sampling and modeling wastewater inputs and outputs, including through investments in building remote, real-time wastewater sampling technologies in sewer infrastructure. They also discussed the importance of a dynamic conceptual site model to organize thoughts and policy interventions available related to the pathogen’s source, transport pathways, and exposure routes.
IMPROVING MODELS TO INFORM PUBLIC HEALTH DECISIONS
Opportunities in Combining Data and Expertise Across Disciplines
Collaboration to advance knowledge and inform decisions at the environment–infectious disease interface could benefit from combining data and expertise across disciplines. Amelia Bertozzi-Villa (Bill & Melinda Gates Foundation and Institute for Disease Modeling) and William Pan (Duke University) presented examples demonstrating how combining data sets can improve infectious disease prediction, early warning, and response strategies.
Bertozzi-Villa described a project that modeled malaria dynamics in sub-Saharan Africa in an effort to determine if eradication is feasible. To answer this complex question, she said it was necessary to bring together multiple areas of expertise and share data across fields in unprecedented ways. For example, the model needed to incorporate the dynamics of the disease itself, the mosquitoes that carry it, the impacts of climate change, and the anticipated effects of various policy interventions. Different stakeholders interpreted the resulting analysis in different ways and Bertozzi-Villa pointed out how this underscores the importance of intersectional collaboration at the early stages of public health planning, noting that the model helped establish a shared understanding of the factors that can inform future investments and actions.
Pan described his team’s efforts to combine landscape and meteorological data and models with malaria surveillance data and models of human movement to predict malaria outbreaks in the Amazon. In validation studies in Peru, he said, the approach was demonstrated to detect malaria outbreaks 12 weeks in advance. For any use of models, Pan said, it is critical to be able to quantify assumptions, strengths, weaknesses, and uncertainties. In the context of environmental science and infectious disease modeling specifically, it is also important to bridge across disciplines and consider nonlinear dynamics, multiple scales of analysis, and feedbacks. “Environmental change doesn’t occur in a vacuum, and you have these three interacting dimensions of climate, land, and human behavior ... to think about,” Pan said. One important challenge in bridging data across disciplines is that epidemiological data and models tend to focus on discrete outcomes in discrete scales of space and time, while land and climate models are usually continuous in space and time, Pan noted. In addition, he said, while infectious diseases are generally tracked in terms of one-time measurements, for environmental exposures it is important to understand the timing and duration of the exposure. To inform optimal study designs, Pan emphasized the importance of identifying the characteristic scales at which an environmental driver is most likely to influence a human health outcome.
The speakers were joined by Abdisalan Noor (World Health Organization), Charles Ben Beard (CDC), and Juli Trtanj (National Oceanic and Atmospheric Administration) for a panel discussion examining the barriers and opportunities for sharing data across disciplines and the roles of government, academia, and the public in
advancing collaboration. To drive effective collaboration and enhance the meaningful exchange of data, Trtanj said it is important to start with defining the nature of the problem, then identify the key decision points and what types of data will be useful to inform those decisions, and finally identify the appropriate funding strategy for supporting the work. Noor added that focusing on the policy implications early in the process is crucial to ensuring the results are relevant to policy decisions.
Bertozzi-Villa and Beard urged researchers to engage early and work collaboratively with data collectors, rather than simply using their data products. Toward this end, Noor stressed the importance of trust, which requires a common dialogue around a shared problem or goal, followed by sustained relationship building throughout the life of the project. While it takes time to build such relationships, Beard said data collectors will be more willing to share data if they trust that researchers will be cognizant of the limitations of the data and not misuse it. Noor noted that this is especially true in countries with weaker surveillance systems and bigger problems with data quality; to overcome this barrier, he said, it is vital to show how sharing data will benefit data collectors and decision makers in that country.
Listening to partners and communities is crucial to maintaining trust, Pan and Trtanj said. As part of this, they said it is important to be willing to pivot to address evolving needs, as Pan’s team did when they shifted focus from malaria to mercury contamination in their research in the Amazon. Trtanj noted, however, that shifting focus can be challenging depending on the funding model. Another barrier is that science is sometimes perceived as threatening to people’s livelihoods or political structures, as seen in the backlash Pan’s team experienced when its research suggested the local mining industry was posing health problems. In such cases, regaining a community’s trust can take a tremendous amount of work. Trtanj noted that, based on many decades of experience, the public today has a high degree of trust in weather forecasts even though they are wrong sometimes; with more time and experience, she suggested that the public may build a similar degree of trust in public health and climate predictions. Bertozzi-Villa added that it is key to be transparent about data reliability, noting that uncertainty is inevitable and the strength of a model is reliant on that of the underlying data. Beard, Pan, and Trtanj added that efforts to bring the public into the scientific process, such as through citizen science or other forms of community engagement, can also help to establish trust as long as there is a meaningful feedback loop whereby the involved communities benefit from the outcomes.
To improve the quality of data available for intersectional research, Pan said academia has a key role to play in facilitating interdisciplinary connections, but that funding mechanisms could further encourage this type of work. Trtanj urged the public health community to better articulate its data needs in order to inform investments in observation infrastructure and the overall vision for environmental observation systems. “Those decisions are made every year, and a lot of money is going to be spent, and there’s an opportunity to make it more relevant for what we’re trying to do to serve the health community,” she said. In addition to enhancing and combining the many sources of quantitative data, Bertozzi-Villa, Noor, and Pan emphasized the importance of qualitative data, which informs the interpretation of quantitative data and helps fill the knowledge gaps. “It is absolutely critical that we contextualize the quantitative data with some understanding of what’s happening in the place where you’ve made that measurement qualitatively,” Noor said.
BOX 3 Breakout Scenario on Antimicrobial Resistance Emergence
Participants in this session discussed a scenario in which resistance to a newly introduced antibiotic is detected in E. coli strains in some hospitals around the United States. The emergence of resistance may or may not be linked to cases of heavy metal exposure in nearby farming regions. They suggested examples of critical research needs:
- elucidate the mechanisms of resistance including through whole genome sequencing;
- understand transmission and exposure trends;
- determine if there are specific interactions among existing host factors, exposure to environmental contaminants, and bacterial infections; and
- conduct basic science research to understand the clinical effects of the environmental contaminant.
To answer cross-disciplinary, cross-sector questions related to the drivers of antimicrobial resistance, they suggested bringing stakeholders together in a multi-step effort involving federal, state, local, and Tribal agencies. Participants also underscored the importance of evidence-based risk communication for informing health care providers and the public.
Opportunities in Big Data and AI
Emerging data sources and techniques offer new opportunities for insight at the intersection of environmental science and infectious disease. Ayesha Mahmud (University of California, Berkeley) and Pascale Fung (The Hong Kong University of Science and Technology) presented examples of how big data and AI can be leveraged to gain knowledge and inform decisions across a wide range of areas, from identifying disease hot spots and predicting spread to addressing misinformation and mental health problems surrounding outbreaks and epidemics.
Mahmud highlighted how nontraditional sources of data can illuminate how seasonal patterns, population mobility, and climate change influence the spread of infectious diseases. It is critical to understand human population dynamics to prepare for outbreaks, identify at-risk populations, efficiently allocate resources, and target interventions, she said, and novel data streams—including data from social media platforms and telecommunications data—can fill gaps where traditional epidemiological data sources fall short. Demonstrating the usefulness of some of these nontraditional data streams, in Bangladesh, Mahmud and colleagues combined epidemiological surveys with telecommunications data to model the spread of chikungunya during a travel-intensive holiday period.9 When a cyclone sparked a cholera outbreak in Mozambique, the researchers combined information on previous cholera dynamics with flooding data and models of human mobility to identify populations at high risk and inform vaccine allocation.10 To ensure forecasts are actionable and useful, Mahmud said, requires basic health surveillance infrastructure along with partnerships among government, academia, and private industry that are centered in community needs. While academic research is useful for building capacity and developing tools and methods, she argued that “the bulk of this work really needs to happen within local public health agencies,” which she suggested should establish direct links with novel data streams such as telecommunications providers and social media platforms and use the data to inform outbreak response and control efforts. Such data sources can provide valuable insights, particularly in situations where traditional laboratory-based testing and monitoring lags in comparison to disease spread. But Mahmud cautioned that it is vital to address privacy concerns and remain cognizant of the limitations and biases within each data stream.
AI has emerged as a powerful tool for insight at the intersection of the environment and infectious disease, Fung said. She described how she and colleagues built on AI work that was ongoing before the pandemic to help inform various aspects of the response to COVID-19. Before the pandemic, Fung’s team was asked to develop tools for detecting early warning signs of epidemics on news sites. During the COVID-19 “infodemic,” they used AI to help identify and debunk misinformation about the virus based on the content and writing style of various information sources. To help facilitate COVID-19 research, they also developed an AI-based tool to help scientists find the most relevant papers within a deluge of research on COVID-19 and a tool to help speed vaccine development by analyzing coronavirus sequences. They also developed an interactive simulation that shows users how mask wearing can reduce disease transmission and a virtual mental health coach tool to help address mental health challenges fueled by isolation and disruptions to daily life.
In a discussion that included Steven Foley (U.S. Food and Drug Administration) and Charles Schmitt (NIEHS), panelists examined the strategies for and barriers to the use of big data and AI in the context of this workshop and considered the implications for privacy, security, and communication. They began with a discussion of current and future opportunities in leveraging big data. Foley pointed to efforts to combine genomics data and drug research databases to identify promising drug targets for COVID-19. To speed such efforts, he said it would be helpful to address intellectual property issues and incentivize companies to share information, potentially looking to Operation Warp Speed as a model. In addition, he said recent sequencing-based advances in the detection of foodborne pathogens could represent a new model for integrating genomics, geography, and human activity to look for early warning signs and contain outbreaks sooner. Mahmud stressed that there remains a strong need to invest in traditional sources of epidemiological data, including sequencing and disease surveillance, but said novel data streams related to the environment such as satellite data, hydrology data, and information on city infrastructure can help to inform public health responses in contexts where
________________
9 Mahmud, A.S., I. Kabir, K. Engø-Monsen, S. Tahmina, B. Khoorshid Riaz, A. Hossain, F. Khanom, M. Rahman, K. Rahman, M. Sharmin, D. Mashrur Hossain, S. Yasmin, M. Ahmed, M.A.F. Lusha, and C.O. Buckee. 2021. Megacities as drivers of national outbreaks: The 2017 chikungunya outbreak in Dhaka, Bangladesh. PLOS Neglected Tropical Diseases 15(2):e0009106.
10 Khan, R., A. Mahmud, A. Schroeder, L. Aguilar Ramirez, J. Crowley, J. Chan, and C. Buckee. 2019. Rapid forecasting of cholera risk in Mozambique: Translational challenges and opportunities. Prehospital and Disaster Medicine 34(5):557–562.
traditional data sources are lacking. Furthermore, she added that interdisciplinary collaborations can help integrate these types of spatial and geographic data sets with public health data to make those data useful and actionable.
Fung and Schmitt posited that AI holds great potential for mining research literature and data sets to generate new hypotheses, but said that bringing heterogeneous data sets together for this purpose comes with a host of potential pitfalls. Foley and Schmitt described how fusing data from different domains such as genomics, infectious disease, environmental health, and geography has challenges related to not only the data itself, but also the ability to extract meaningful insight from it and the ability for experts in multiple domains to work together effectively. Schmitt suggested that approaches such as natural language processing could potentially help fuse data sets across domains. Foley noted that visualizations can help researchers identify the most important pieces on which to focus, and Fung added that many barriers to the use of big data and AI relate to interfaces and design issues, rather than algorithms themselves.
Panelists then turned to the privacy implications of big data and AI. Patient data can provide powerful insights on infectious disease and environmental health, but the use of health data raises a variety of issues surrounding ethics, privacy, and security. Noting that access to data is critical for training AI systems, Schmitt said the demand for patient data is often filled by private companies outside the reach of the ethics rules that guide the use of data in academia and government, raising questions about ethical oversight. Fung suggested that federated learning—a process through which AI systems are trained on decentralized, locally stored, institution-specific data sets without moving or exchanging data—approaches can potentially help mitigate privacy concerns. Schmitt said public–private partnerships (PPPs) to make private-sector data more accessible for research within appropriate ethical frameworks could help, though Mahmud noted that brokering PPPs can be challenging depending on the level of government involvement.
Data outside of the traditional health sphere also raise concerns about privacy, as well as data reliability. Mahmud noted that digital data such as social media streams were not designed to collect health information in ways that protect privacy, and the onus has been on researchers to employ protective measures, such as aggregating data to reduce the risk of identifying individuals. “With the pandemic there’s been this sort of avalanche of data being provided by all kinds of companies, and I think that there needs to be more thought about the ethics and the privacy, rather than these ad hoc efforts,” she said. On the topic of data reliability, Mahmud also urged researchers to be cognizant of the biases of each data set and consider how combining those biased data sets affects the ability to generate useful results. When it comes to human behavior, Mahmud mentioned that no single data stream offers the full picture of how people are moving, aggregating, and interacting. She cautioned that researchers should be careful not to over-interpret the information gained from a given data source. Other panelists agreed, noting the importance of detecting and mitigating bias and in ensuring that the data used to build and train AI tools are of high quality.
Panelists noted that AI, like other areas of science and technology, has received both a welcome and a wariness on the part of the public. Panelists discussed the need for clear communication to help the public understand research findings, but noted that significant challenges remain with regard to building trust and communicating about uncertainty. Foley suggested including social scientists and communication experts in efforts to communicate about uncertainty in science, which he noted can be easily misunderstood. Other panelists agreed, noting the critical role that social and behavioral scientists can play in public health messaging and building trust in useful tools, even when uncertainty is present. Fung added that natural language processing could potentially also be leveraged at the end of the research cycle to help translate scientific findings into lay terms to aid in the dissemination of new knowledge, though she stressed the need for careful and responsible messaging when communicating with the public. For addressing issues of trust, Fung said it may help to create a system for certifying the reliability and ethical practices of AI technology, but speculated that explaining or certifying technology will not necessarily be sufficient to engender trust. “We’re in a bind here, regarding not just AI, but also scientific knowledge in general,” she said, noting that many people still distrust COVID-19 vaccines despite extensive efforts to explain the science of how they work. In addition, establishing an AI certification would require ethicists, policy makers, and AI engineers to agree on what that certification would entail, Fung said, which is not necessarily an easy task. Even in the context of individual AI research projects, Schmitt noted that there has not been full consensus on what mix of expertise teams should include, though he argued that expertise in ethics, communications, and quality assessment is important.
BOX 4 Breakout Scenario on Environmental Change
Participants in this session considered a scenario in which predicted heavy rainfall across the U.S. east coast threatens to compromise private well water supplies and flood basements, potentially exposing people to pathogens and contaminants. They noted critical uncertainties in baseline data and the limitations of AI-based forecasting, particularly regarding the timing of weather events and local-scale impacts. The scenario revealed numerous areas for potential future research, including
- flood prediction,
- health infrastructure,
- cost-benefit analyses,
- social behavior, and
- risk communication.
To inform policy, infrastructure, and environmental interventions, many participants suggested a stepwise approach as forecasts evolve, the flexibility to allocate funds when and where they are needed, and coordination across public, private, and nonprofit sectors.
A VISION FOR PREVENTING THE NEXT PANDEMIC
In the closing remarks, Perry urged participants to consider how the workshop’s themes of tools, collaboration, and translation can help guide future progress toward a vision for preventing the next pandemic. She underscored the need for many types of tools, including those for detecting and monitoring infectious diseases, such as genomic surveillance and crowdsourcing approaches, and tools for monitoring and modeling the environment. She pointed to the role of AI and data science in advancing the capacity to integrate complex data streams and tools, while recognizing the need to address biases, standards, privacy concerns, and regulatory issues in the collection, integration, and use of data. Perry listed numerous areas of expertise that she said should be involved in this work, including contributions from infectious disease physicians; social scientists; virologists and microbiologists; epidemiologists; exposure scientists and airway biologists; climate and atmospheric scientists; veterinarians and agricultural scientists; and engineers, modelers, and data scientists, along with other fields. Collaborations will be essential to advancing methods, closing knowledge gaps, and delivering meaningful, actionable information to decision makers and the public, she said. To enable rapid detection of emerging pathogens and effective responses to complex, evolving health threats, she urged researchers to stay focused on questions and data that can inform decisions. “It will be upon us to continue to push forward to make those decisions about how our science can best translate into protective and robust policies,” Perry concluded.
DISCLAIMER: This Proceedings of a Workshop—in Brief was prepared by Anne F. Johnson, Andrew Bremer, Julie Liao, and Audrey Thévenon as a factual summary of what occurred at the workshop. The statements recorded here are those of the individual workshop participants and do not necessarily represent the views of all participants, the workshop planning committee, the Standing Committee on the Use of Emerging Science for Environmental Health Decisions, or the National Academies of Sciences, Engineering, and Medicine.
REVIEWERS: To ensure that this Proceedings of a Workshop—in Brief meets institutional standards for quality and objectivity, it was reviewed by Christine Johnson (University of California, Davis), David Larsen (Syracuse University), and Amy Pruden (Virginia Tech University). The review comments and draft manuscript remain confidential to protect the integrity of the process.
Workshop planning committee members: Melissa Perry (Chair), The George Washington University; David Blazes, Bill & Melinda Gates Foundation; Gary L. Ginsberg, New York State Department of Health; Christine K. Johnson, University of California, Davis; Kristen Malecki, University of Wisconsin–Madison; Jade Mitchell, Michigan State University; Vincent J. Munster, National Institute of Allergy and Infectious Diseases; and Svitlana Volkova, Pacific Northwest National Laboratory.
The Standing Committee on the Use of Emerging Science for Environmental Health Decisions, under which this workshop was organized, is supported by the National Institute of Environmental Health Sciences.
Suggested citation: National Academies of Sciences, Engineering, and Medicine. 2021. Pivotal Interfaces of Environmental Health and Infectious Disease Research to Inform Responses to Outbreaks, Epidemics, and Pandemics: Proceedings of a Workshop—in Brief. Washington, DC: The National Academies Press. https://doi.org/10.17226/26270.
Division on Earth and Life Studies
Copyright 2021 by the National Academy of Sciences. All rights reserved.












