Summary
INTRODUCTION
Of the top ten most frequently reported diseases in 1995 in the United States, five are sexually transmitted diseases (STDs) (CDC, 1996c). With approximately 12 million new cases of STDs occurring annually (CDC, DSTD/HIVP, 1993), rates of curable STDs in the United States are the highest in the developed world.1 In 1995, STDs accounted for 87 percent of all cases reported among the top ten most frequently reported diseases in the United States (CDC, 1996c). Despite the tremendous health and economic burden of STDs, the scope and impact of the STD epidemic are underappreciated and the STD epidemic is largely hidden from public discourse. Public awareness and knowledge regarding STDs are dangerously low, but there has not been a comprehensive national public education campaign to address this deficiency. The disproportionate impact of STDs on women has not been widely recognized. Adolescents and young adults are at greatest risk of acquiring an STD, but STD prevention efforts for adolescents remain unfocused and controversial in the United States. There are many biological and social factors that hinder effective prevention efforts, but few have been elucidated and addressed on a national basis. In addition, the roles
|
1 |
For the purposes of this report, developed countries are western and northern European countries, Canada, Japan, and Australia. For example, th reported incidence of gonorrhea in 1995 was 150 cases per 1000,000 persons in theUnited States versus 3 cases per 100,000 in Sweden (CDC, DSTDP, 1996; Swedish Institute for Infectious Disease Control, unpublished data, 1996). |
and responsibilities of public versus private health care professionals in STD prevention have not been clarified in light of recent changes in health care delivery and financing.
Given the above observations regarding STDs in the United States, the Institute of Medicine (IOM) convened the 15-member Committee on Prevention and Control of Sexually Transmitted Diseases in 1994 to “(a) examine the epidemiological dimensions of STDs in the United States and factors that contribute to the epidemic; (b) assess the effectiveness of current public health strategies and programs to prevent and control STDs;2 and (c) provide direction for future public health programs, policy, and research in STD prevention and control.3” The committee was charged to focus its study on STDs other than HIV infection.
BROAD SCOPE AND IMPACT OF STDS
The term “STD” is not specific for any one disease but denotes the more than 25 infectious organisms that are transmitted through sexual activity and the dozens of clinical syndromes that they cause.4 STDs are almost always transmitted from person to person by sexual intercourse.5 These infections are most efficiently transmitted by anal or vaginal intercourse, and generally less efficiently by oral intercourse. Some STDs, such as hepatitis B virus infection and HIV infection, are also transmitted by parenteral routes—particularly among intravenous drug users through contaminated injecting drug equipment. In addition, pregnant women with sexually transmitted infections may pass their infection to infants in the uterus, during birth, or through breast-feeding.
STDs are transmitted among all sexually active people, including heterosexual persons, men who have sex with men, and women who have sex with women (AMA, Council on Scientific Affairs, 1996). Men who have sex with men
|
2 |
Although the committee examined the effectiveness of major strategies and programs in STD prevention, it did not conduct a systematic, in-depth evaluation of every STD-related program in the public and private sector. In this report, the committee focuses its discussions on effective strategies and highlights major effective programs. |
|
3 |
The terms “STD prevention” and “STD control” traditionally have been used by public health workers without clear distinction. These terms have been commonly used to refer to behavioral interventions (e.g., counseling for behavior change), treatment of symptomatic disease, and other interventions that prevent the spread of infection (e.g., partner notification). The committee believes that most interventions for STDs both “prevent” and “control” STDs and all prevent acquisition or transmission of STDs in a population. Essentially, effective prevention of STDs brings STDs under control. Therefore, in this Summary and the full report, the committee uses the term “STD prevention” rather than “STD prevention and control” to encompass all interventions, whether behavioral, curative, environmental, or otherwise, that are needed to reduce the spread of infection in a population. |
|
4 |
See Appendix A of the full report. |
|
5 |
The term “sexual intercourse” is used throughout this summary and the full report to refer to all forms of intercourse, including vaginal, anal, and oral intercourse. |
are at greater risk for many life-threatening STDs, including HIV infection, hepatitis B virus infection, and anal cancer compared to heterosexual men (AMA, Council on Scientific Affairs, 1996). Less is known about the risk of STD transmission among women who have sex with women (Kennedy et al., 1995; AMA, Council on Scientific Affairs, 1996), but women who have sex only with women (and whose partners do likewise) are generally at substantially lower risk for acquisition of STDs compared with men who have sex with men and heterosexual persons.
Impact of STDs on Women's and Adolescents' Health
Complications of STDs are more severe and occur more frequently among women than men for a number of reasons (Wasserheit and Holmes, 1992). Many STDs are transmitted more easily from a man to a woman than from a woman to a man (Harlap et al., 1991). Sexually transmitted infections also are more likely to remain undetected in women, resulting in delayed diagnosis and treatment.
Every year, approximately 3 million American teenagers acquire an STD (CDC, DSTD/HIVP, 1993). Adolescents and young adults are the age groups at greatest risk of acquiring an STD for a number of reasons: they are more likely to have multiple sex partners; they may be more likely to engage in unprotected intercourse; and their partners may be at higher risk of being infected (CDC, DSTDP, 1995; AGI, 1994; Quinn and Cates, 1992; Cates, 1990). Compared with older adult women, female adolescents and young women are more susceptible to cervical infections, such as gonorrhea and chlamydial infection, because the cervix of female adolescents and young women is especially sensitive to infection by certain sexually transmitted organisms (Cates, 1990). In addition, adolescents and young people are at greater risk than older persons for substance use and other behaviors that may increase risk for STDs.
STDs as Emerging Infections
STDs are not a stationary group of infections and syndromes; eight new sexually transmitted pathogens have been identified since 1980, including HIV. In contrast to newly recognized viral STDs, some bacterial STDs, such as syphilis and gonorrhea, have been documented for centuries and have recently reemerged in the United States along with a spectrum of barriers to prevention (Wasserheit, 1994). As demonstrated by the recent finding that bacterial vaginosis in pregnant women increases the risk for premature delivery of a low-birthweight infant (Hillier et al., 1995; Hauth et al., 1995), the full clinical spectrum of many STDs is still being described.
STDs are severe social, health, and economic burdens worldwide. The World Bank estimates that STDs, excluding AIDS, are the second leading cause of healthy life lost among women between the ages of 15 and 44 in the developing
world (World Bank, 1993; Over and Piot, 1993). The World Health Organization (WHO) recently estimated that there were 333 million new cases of the four curable STDs (gonorrhea, chlamydial infection, syphilis, and trichomoniasis) worldwide in 1995 among adults 15– 49 years of age (WHO, Global Programme on AIDS, 1996). New sexually transmitted infections appear on a regular basis in the United States and are likely to continue to do so as long as the rates of risky sexual behaviors remain high and global economic and demographic factors continue to promote the emergence of STDs.
HEALTH CONSEQUENCES OF STDS
The general population is largely unaware of the health consequences of STDs, and STDs are “hidden” from public attention for three reasons. First, many STDs are often asymptomatic and thus go undetected (Judson, 1990; Fish et al., 1989; Stamm and Holmes, 1990). Second, major health consequences, such as infertility, certain cancers, and other chronic diseases, occur years after the initial infection, so that there is a lack of awareness of any link to the original STD. Third, the stigma associated with having an STD has inhibited public discussion and education concerning the consequences of STDs and frequently prevents clinicians from educating their patients regarding STDs. These factors are discussed later in this summary.
Cancers Caused by STDs
Several sexually transmitted pathogens cause cancer. Certain types of sexually acquired human papillomavirus are now considered to cause nearly all cancers of the cervix, vagina, vulva, anus, and penis. Cervical infections with oncogenic types of human papillomavirus are associated with at least 80 percent of invasive cervical cancer cases (NIH, 1996a); and women with human papillomavirus infection of the cervix are 10 times more likely to develop invasive cervical cancer than are women without such infection (Schiffman, 1992). Approximately 4,900 American women will die from cervical cancer in 1996, and approximately 16,000 new cases of cervical cancer are diagnosed each year, making cervical cancer the third most common reproductive tract cancer in women and the seventh most common type of cancer overall in women (ACS, 1996). Much of the cervical cancer burden related to human papillomavirus infection may be averted by preventing high-risk sexual behaviors (Brinton, 1992). Screening with the Pap smear is currently the best available method for reducing both incidence of and mortality associated with invasive cervical cancer, but this technique is not widely utilized among certain population groups (NIH, 1996a). Hepatitis B virus is a sexually transmitted virus that causes hepatocellular carcinoma (liver cancer), one of the most common forms of cancer. Other sexually transmitted pathogens that are associated with cancers include
human T-cell lymphotrophic virus type I (HTLV-I), linked to adult T-cell leukemia and lymphoma; human herpes virus type 8 (HHV8), linked to Kaposi's sarcoma; and Epstein-Barr virus (EBV), linked to lymphoma and nasopharyngeal (nasal cavity and pharynx) carcinoma.
Reproductive Health Problems
One of the most serious threats to the reproductive capability of women is pelvic inflammatory disease, a preventable complication of certain STDs, most commonly chlamydial infection and gonorrhea (Washington et al., 1991; Jossens et al., 1994). Each year more than one million U.S. women experience an episode of pelvic inflammatory disease (Rolfs et al., 1992; Washington and Katz, 1991). At least one-quarter of women with acute pelvic inflammatory disease experience serious long-term sequelae, the most common and important of which are ectopic pregnancy (the development of a fetus outside the uterus) and tubal-factor infertility (infertility resulting from blockage or damage to the fallopian tubes).
Ectopic pregnancy usually results from partial tubal blockage associated with pelvic inflammatory disease. In 1992, the estimated number of ectopic pregnancies was 108,800, or one in 50 pregnancies (CDC, 1995a). In the same year, approximately 9 percent of all pregnancy-related deaths were a result of ectopic pregnancy (NCHS, 1994), making ectopic pregnancy one of the leading and most preventable causes of maternal death during pregnancy (Marchbanks et al., 1988). At least 15 percent of all infertile American women are infertile because of tubal damage caused by pelvic inflammatory disease. Of all women infertile because of tubal damage, no more than one-half have previously been diagnosed and treated for acute pelvic inflammatory disease.
Health Consequences for Pregnant Women and Infants
STDs are associated with multiple acute complications for pregnant women and their infants (Brunham et al., 1990). Various sexually transmitted pathogens may be transmitted to the fetus, newborn, or infant through the placenta (congenital infection), during passage through the birth canal (perinatal infection), or after birth through breast-feeding or close direct contact. Active sexually transmitted infection during pregnancy may result in spontaneous abortion, stillbirth, premature rupture of membranes, and preterm delivery. Preterm delivery accounts for approximately 75 percent of neonatal deaths not caused by congenital malformations (Main and Main, 1991). Women with bacterial vaginosis are 40 percent more likely to deliver a premature infant compared with women without this condition (Hillier et al., 1995). In addition, up to 80 percent of pregnancies associated with untreated early syphilis result in stillbirth or clinical evidence of congenital syphilis in the newborn (Schulz et al., 1990). Sexually transmitted pathogens that have serious consequences among adults tend to cause even more
severe, potentially life-threatening health conditions in the fetus or newborn, whose immune system is immature. Damage to the central nervous system, eyes, and auditory system is of particular concern.
Deaths Associated with STDs
Of 513,486 persons with AIDS reported in the United States through December 1995, more than 62 percent (319,849) have died (CDC, 1995b). The largest number of deaths related to STDs other than AIDS is caused by cervical and other human papillomavirus-related cancers; liver disease (e.g., chronic liver disease and liver cancer) caused by hepatitis B virus; pelvic inflammatory disease; ectopic pregnancy; and various pregnancy, fetal, and neonatal complications. A recent study found that more than 150,000 deaths were directly attributed to STDs, including AIDS, from 1973 through 1992 among American women 15 years of age and older (Ebrahim et al., 1995). The three leading causes of STD-related deaths in 1992 among these women were all related to viral STDs: cervical cancer, AIDS, and hepatitis B virus infection. The high rate of viral STD-related deaths and morbidity and the high costs of managing viral STDs and their complications in the United States underscore the importance of effective prevention programs for viral STDs.
IMPACT OF STDS ON HIV TRANSMISSION
Both “ulcerative” STDs, such as chancroid, syphilis, and genital herpes, and “inflammatory” STDs, such as gonorrhea, chlamydial infection, and trichomoniasis, increase the risk of HIV infection. Prospective cohort studies in Africa have demonstrated increased risk of HIV infection following genital ulcer disease as well as with inflammatory STDs (Cameron et al., 1989; Plummer et al., 1991; Laga et al., 1993; Nyange et al., 1994). Genital ulcer disease may increase the risk of transmission per exposure by a factor of 10 to 50 for male-to-female transmission and by a factor of 50 to 300 for female-to-male transmission (Hayes et al., 1995). Numerous studies support the concept that STDs increase both infectivity of and susceptibility to HIV (Kreiss et al., 1994; Plummer et al., 1991; Clemetson et al., 1993; Mostad et al., 1996; John et al., 1996; Gys et al., 1996; Moss et al., 1995; Hoffman et al., 1996; de Vincenzi, 1994; Deschamps et al., 1996).
Early detection and treatment of STDs can have a major impact on sexual transmission of HIV (Moss et al., 1995; Hoffman et al., 1996; Laga et al., 1994). For example, a large, prospective, randomized controlled trial in Tanzania found that the incidence of HIV infection was 42 percent lower in communities with improved management of STDs after two years compared with control communities (Grosskurth et al., 1995a, b).
In the absence of prospective studies or formal trials of strengthened STD
interventions to reduce sexual transmission of HIV in the United States (which may not be feasible), mathematical modeling may be essential to assess the potential impact of reducing STDs on HIV transmission. Robinson and colleagues (1995) predicted that a 50 percent reduction in the duration of STDs in Uganda could decrease HIV transmission by 43 percent—a prediction remarkably close to that observed in the intervention trial in nearby Tanzania. Boily has developed a model that shows that HIV infection could not be established in the general U.S. heterosexual population in the absence of chlamydial infection (or other STDs with comparable effects on HIV transmission). 6 In addition, it is estimated that successfully treating or preventing 100 cases of syphilis among high-risk groups for STDs would prevent 1,200 HIV infections that are ordinarily linked to those 100 syphilis infections during a 10-year period (Over and Piot, 1993).
ECONOMIC CONSEQUENCES OF STDS
The costs of a few STDs have been estimated (IOM, 1985; Washington et al., 1987; Washington and Katz, 1991), but no comprehensive, current analysis of the direct and indirect costs of STDs is available. Partly based on updated estimates of the economic burden of STDs by Siegel, 7 the committee estimates that the total costs for a selected group of major STDs and related syndromes, excluding HIV infection, were approximately $10 billion in 1994. This rough, conservative estimate does not capture the economic consequences of several other common and costly STDs and associated syndromes such as vaginal bacteriosis and trichomoniasis. The estimated annual cost of sexually transmitted HIV infection in 1994 was approximately $6.7 billion.8 Including these costs raises the overall cost of STDs in the United States to nearly $17 billion in 1994. These cost estimates underscore the enormous burden of STDs on the U.S. economy. Much of the direct costs of STDs result from failure to detect and effectively manage STDs in their initial, acute stages. For example, nearly three-fourths of the $1.5 billion cost of chlamydial infections is due to preventable complications resulting from untreated, initially uncomplicated infections (Washington et al., 1987).
FACTORS THAT CONTRIBUTE TO THE HIDDEN EPIDEMIC
Biological Factors
Behavioral, biological, and social factors contribute to the transmission of STDs (Wasserheit, 1994). In addition to preexisting or concurrent STDs, biologi-
|
6 |
See Appendix C of the full report. |
|
7 |
See Appendix D of the full report. |
|
8 |
See Chapter 2 of the full report. |
cal factors that contribute to the hidden nature and spread of STDs include the lack of conspicuous signs and symptoms in infected persons (asymptomatic infections), the long lag time from initial infection to signs of severe complications, and the propensity for STDs to more easily infect young women and female adolescents than men. Many STDs, such as chlamydial infection, do not produce acute symptoms or clinical signs of disease, or they do not produce symptoms sufficiently severe for an infected individual to seek medical attention (Stamm et al., 1982; Keim et al., 1992). The long period of time (sometimes years or decades) from initial infection until the appearance of clinical problems, such as in the cases of human papillomavirus infection and genital cancer, and hepatitis B virus infection and liver cancer, often results in failure to attribute cases of STD-related cancers and other long-term complications to sexually transmitted infections. This failure, in turn, reduces the perceived seriousness of STDs and the motivation to undertake preventive action. Other biological factors that may increase risk for acquiring, transmitting, or developing complications of certain STDs include presence of male penile foreskin, vaginal douching, risky sexual practices, use of hormonal contraceptives or intrauterine contraceptive devices, cervical ectopy, immunity resulting from prior sexually transmitted or related infections, and nonspecific immunity conferred by normal vaginal flora.
Social Factors
Some fundamental societal problems such as poverty, inadequate access to health care, inadequate education, and social inequity indirectly increase the prevalence of STDs in certain populations. In addition, lack of openness and mixed messages regarding sexuality create obstacles to STD prevention for the entire population and contribute to the hidden nature of STDs.
Poverty and Inadequate Access to Health Care
Health insurance coverage enables individuals to obtain professional assistance in order to prevent potential STD exposures and to seek care for suspected STDs. Persons who are uninsured delay seeking care for health problems longer than those who have private insurance or Medicaid coverage (Donelan et al., 1996; Freeman et al., 1987). The age and ethnic groups with the highest rates of STDs are also the groups with the poorest access to health services. One-third of persons in age groups at high risk for STDs are uninsured or covered by Medicaid (UCLA Center for Health Policy Research, unpublished data, 1996).
Inadequate access to STD-related services may also be a problem for those with private health insurance. For example, those with private health insurance who are living at or near the poverty level have limited access to health care because of copayments and deductibles that are typically part of private insurance coverage (Freeman and Corey, 1993). In addition, many health plans either do
not cover certain important preventive reproductive health services related to STDs or they require copayments and deductibles for these services (WREI, 1994). Poverty and other socioeconomic factors also contribute to STD risk in other ways. Even if a person in poverty perceives himself or herself to be at risk for an STD, he or she may not practice preventive behaviors if there are other risks that appear more imminent or more threatening or both (Ramos et al., 1995; Mays and Cochran, 1988).
Substance Use
Substance use, especially drug and alcohol use, is associated with STDs. At the population level, rates of STDs are high in geographic areas where rates of substance use are also high, and the rates of substance use and STDs have also been shown to co-vary temporally (Greenberg et al., 1991). At the individual level, persons who use substances are more likely to acquire STDs than those who do not (Marx et al., 1991; Anderson and Dahlberg, 1992; Shafer et al., 1993). Use of drugs and other substances may undermine an individual's cognitive and social skills, making it more difficult to take protective actions against STDs (Marx et al., 1991).
Numerous studies show that drug use is associated with increased risk of STDs, including HIV infection (Marx et al., 1991; Edlin et al., 1994). Crack use, in particular, strongly contributes to STD transmission by discouraging health-care-seeking behavior (Webber et al., 1993) and modifying social norms with respect to behavior such as engaging in unprotected sex (Finelli et al., 1993) or having multiple sex partners (Greenberg et al., 1991); these factors may lengthen the duration of infectiousness. A number of studies have reported strong associations between alcohol use and high-risk sexual behaviors among the general population (Anderson and Dahlberg, 1992; Caetano and Hines, 1995), adolescents (Shafer et al., 1993; Hingson et al., 1990; Lowry et al., 1994), men who have sex with men (Siegel et al., 1989; Stall et al., 1986), runaway youth (Koopman et al., 1994), and mentally ill adults (Kalichman et al., 1994).
Sexual Abuse and Violence
Sexual violence against women and sexual abuse of children contribute to the transmission of STDs. Women who have been sexually abused during childhood are twice as likely to have gynecological problems, including STDs, than women who do not have such a history (Plichta and Abraham, 1996). In addition, women with a history of involuntary sexual intercourse are more likely to have voluntary intercourse at an earlier age (a risk factor for STDs) and to have subsequent psychological problems (Miller et al., 1995). Many women who experience sexual violence may not be able to implement practices to protect against STDs or pregnancy (Plichta and Abraham, 1996; O'Leary and Jemmott, 1995).
STDs among children presenting for care after the neonatal period almost always indicate sexual abuse (CDC, 1993a; Gutman et al., 1991; AAP, Committee on Child Abuse and Neglect, 1991). Sexually abused children may have severe and long-lasting psychological consequences, may become sexual abusers themselves, and may abuse other children (Guidry, 1995). In addition, they may participate in a pattern of high-risk behavior that often puts them at risk for further abuse and subsequent STDs.
STDs Among Disenfranchised Populations
STDs disproportionately affect disenfranchised groups, including sex workers9 (Plummer and Ngugi, 1990; Rosenblum et al., 1992), runaways (Sherman, 1992), homeless persons (Johnstone et al., 1993; Breakey et al., 1989), adolescents in detention (AMA, Council on Scientific Affairs, 1989; Shafer et al., 1993; Shafer, 1994), adults in detention (CDC, 1996a; Hammett et al., 1995), and migrant workers (CDC, 1992a; Jones et al., 1991). These groups are important from an STD prevention perspective because they represent “core” transmitters of STDs and are potential reservoirs of infection for the general population (Thomas and Tucker, 1996).
Rates of STDs, including HIV infection, are many times higher among incarcerated adolescents and adults than among the general population (CDC, 1996a; CDC, 1992b). Within prisons, unprotected sex, intravenous drug use, and tattooing are potential modes of transmission of STDs, including HIV infection (Dolan et al., 1995; Hammett et al., 1995; Doll, 1988). A wide range of unprotected consensual and nonconsensual sexual activity occurs among prisoners and between prisoners and staff (Mahon, 1996). In detention facilities, more emphasis is placed on HIV education than on education about other STDs, and very few correctional facilities provide access to condoms because of security concerns (Hammett et al., 1995; CDC, 1996a). The high annual rate of turnover among prisoners, 800 and 50 percent in jails and prisons, respectively, is a major barrier to screening programs and follow-up treatment for STDs (Glaser and Greifinger, 1993).
SECRECY AS A CONTRIBUTING FACTOR
Although sex and sexuality pervade many aspects of American culture and sexuality is a normal aspect of human functioning, sexual behavior is a private—and secret—matter in the United States. The committee uses the term “secrecy” in this report to describe certain aspects of sexuality in the United States. By the
|
9 |
The term “sex worker” is commonly used by public health workers to refer to persons who exchange sex for drugs, money, or other goods. This term is preferable to the term “prostitute.” |
term “secrecy,” the committee includes both the passive by-product of the inherent difficulties of discussing intimate aspects of life, and the ongoing efforts by some groups to prevent open dissemination of information regarding sexuality and its health consequences. The secrecy surrounding sexuality in the United States may have origins in the late Victorian social system (Brandt, 1988, 1985; Sokolow, 1983).
The depiction of sexuality has been paradoxical within modern American culture. On the one hand, there is a saturation and sensationalism of sexual images and messages in the mass media, and the public is fascinated with sexual subjects. On the other hand, sexuality remains an extremely private and uniquely complex sphere of human behavior with sociocultural taboos and rules of behavior that make talking openly and comfortably about sexuality difficult. The secrecy surrounding sexuality and STDs adversely impacts on STD prevention in the United States by impeding sexuality and STD education programs for adolescents, hindering communication between parents and their children and between sex partners, promoting unbalanced sexual messages in mass media, compromising education and counseling activities of health care professionals, hindering community activism regarding STDs, and impeding research on sexual behaviors.
Barriers to open discussion regarding sexuality include gender roles; modesty; and cultural, family, or religious taboos against discussions of sex. Ironically, it may require greater intimacy to discuss sex than to engage in it. The kind of communication that is necessary to explore a partner's sexual history, establish STD risk status, and plan for protection against STDs is made difficult by the taboos surrounding sex and sexuality (Lear, 1995). The discomfort that many Americans feel discussing sexual behavior is reflected in a recent nationwide survey showing that, including married couples, approximately one of four women and one of five men surveyed had no knowledge of their partner's sexual history (EDK Associates, 1995).
Only 11 percent of teenagers get most of their information regarding STDs from parents and other family members (ASHA, 1996). Because many parents do not talk to their children about sex, children are more likely to learn about sex through clandestine and secretive exchanges with peers that result in a massive amount of misinformation (Smith and Lanthrop, 1993). Americans, especially adolescents, receive unbalanced mass media messages about sexuality, sexual behavior, and sexual responsibility. Premarital sex, cohabitation, and nonmarital relationships are depicted as the norm for adults (Lichter et al., 1994), but the mass media provide little frank and informed advice about STDs, sexuality, contraception, or the harsh realities of early pregnancy and parenting. Television is currently the most significant mass media influence for adolescents (Strasburger, 1990), and children spend more time watching television than they do in school (Dietz and Strasburger, 1991). A recent study found an average of 10 incidents of sexual behavior per hour on network television during prime time
(Lowry and Shidler, 1993). Although sex is frequently portrayed on television, protective behavior is rarely shown and references to adverse consequences are rare; there are approximately 25 instances of sexual behavior portrayed on prime-time television for every instance of protective behavior shown or comment regarding STDs or unintended pregnancy (Lowry and Shidler, 1993). Advertisers and program sponsors have implicitly supported sexual content in programming and commonly use sexual appeals to sell products, but they generally have refused to support the incorporation of explicit information regarding protective behaviors for STDs for fear of offending viewers (Brown and Steele, 1995; Lebow, 1994; Strasburger, 1989). Opinion polls, however, show that most Americans support incorporating information regarding STDs and contraceptives, including condom advertisements, into mass media (Harris and Associates, 1987; EDK Associates, 1994).
The secrecy surrounding sexuality compromises effective clinical preventive services. STD-related risk assessment and counseling are not routinely performed by most primary care clinicians (ARHP and ANPRH, 1995). Embarrassment and discomfort discussing sexual health issues (Risen, 1995; Merrill et al., 1990) and inadequate time and training (Poorman and Albrecht, 1987; Lewis and Freeman, 1987) are major hurdles for clinicians to overcome in order to effectively communicate with their patients regarding sexuality and STDs. The stigma associated with STDs hinders public discourse and, as a result, community activism for STDs. Because having an STD is still socially unacceptable, there are few if any patient-based constituent groups that advocate publicly or lobby for STD-related programs. In contrast, persons with cancer and other common diseases have successfully advocated for additional funding for their causes.
An examination of the social policies and experiences of other developed countries regarding sexuality underscores the adverse impact of the secrecy surrounding sexuality on STD prevention in the United States. For example, the Scandinavian countries have comparable levels of sexual activity, but their rates of curable STDs and unintended pregnancy are much lower than in the United States (Piot and Islam, 1994; IOM, 1995). These differences may be attributable to the pragmatic, rather than moralistic, approach to sexuality issues and universal access to health services in these European countries (David et al., 1990).
Research and Training Issues in Sexuality
Despite the recent surge of research activity regarding sexual behaviors in response to the HIV epidemic, comprehensive data on contemporary sexual behaviors, attitudes, and practices are limited, and it is not understood how these factors are shaped by different societal, cultural, and familial contexts. Many epidemiological studies of human sexuality are outdated (di Mauro, 1995; Laumann, Gagnon, et al., 1994). While some government funding has been provided, there has been little major or consistent support from either the govern-
ment or the private sector for behavioral and social science research on human sexuality since the work of Kinsey and his colleagues (di Mauro, 1995). Furthermore, societal ambivalence regarding sexuality poses substantial obstacles to sexual behavior research. For example, in 1991, there was unprecedented political interference with scientific research when federal administration officials, under pressure by congressional critics, blocked funding for studies of adolescent and adult sexual behavior after these studies had been approved for funding by a scientific peer review process at the National Institutes of Health (Suplee, 1991; Laumann, Michael, et al., 1994).
Trends in Sexual Activity
Rates of sexual intercourse among American adolescents have increased dramatically in the last few decades (CDC, 1992d; Kost and Forrest, 1992; Hofferth et al., 1987). From 1971 to 1988, the proportion of sexually active adolescents and young women aged 15 to 19 years with more than one lifetime sex partner increased nearly 60 percent (Kost and Forrest, 1992). In the United States, nearly 70 percent of students in the twelfth grade have had sexual intercourse (Figure S-1), and 27 percent of twelfth grade students have had four or more sex partners (CDC, 1995d). Sexual intercourse among adolescents is sometimes initiated before the teenage years. A 1992 survey of 2,248 students in grades 6, 8, and 10 from an urban public school district found that 28 percent of sixth-graders and one-half of eighth-graders reported ever having had sexual intercourse (Barone et al., 1996).
Knowledge and awareness of STDs among Americans is poor (ASHA, 1995). In a 1993 national survey of 1,000 women from 18 through 60 years of age, almost two-thirds knew nothing or very little about STDs other than HIV/AIDS, and only 11 percent were aware that STDs can be more harmful to women than to men (EDK Associates, 1994). The lack of knowledge among women in high-risk groups was dramatic: 65 percent of young women reported “almost none” or “very little” knowledge regarding STDs.
REDUCING EXPOSURE AND TRANSMISSION
The rate of spread of STDs in a population is determined by three factors: (1) the rate of exposure of susceptible persons to infected individuals; (2) the probability that an exposed, susceptible person will acquire the infection; and (3) the length of time that newly infected persons remain infectious and are able to spread the infection to others.
Individual factors that influence exposure to and transmission of STDs include sexual behavior, perception of risk, and personal skills. Sexual and other behaviors that place individuals at greater risk of STDs include early onset of intercourse, greater number of partners, intercourse with high-risk partners, more
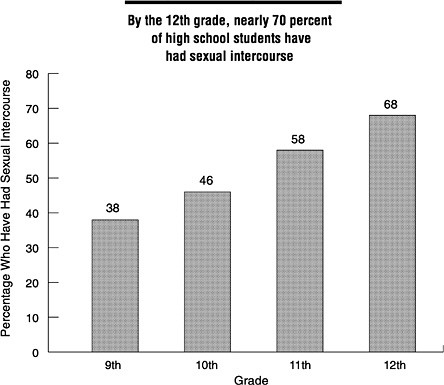
FIGURE S-1 Percentage of U.S. high school students who reported ever having sexual intercourse by grade level, 1993. SOURCE: CDC (Centers for Disease Control and Prevention). Youth risk behavior surveillance —United States, 1993. CDC Surveillance Summaries, MMWR 1995;44(No. SS-1).
frequent intercourse and certain sexual practices, lack of male circumcision, vaginal douching, and lack of barrier contraceptive use (Aral, 1994). As a result of poor knowledge and awareness of STDs, Americans commonly underestimate their risk of infection. For example, in the 1993 national survey mentioned previously, 84 percent of women surveyed were not concerned about acquiring an STD, including 72 percent of young women (age 18 to 24) and 78 percent of women who reported having had “many” sex partners (EDK Associates, 1994). Knowledge, however, is necessary but not sufficient to motivate action. Individuals also need motivation, personal skills, and interpersonal resources to implement complicated behavior changes, including interpersonal communication and negotiation skills and a sense of self-efficacy regarding accomplishment of the relevant behaviors (Bandura, 1990; Wulfert and Wan, 1993).
Behavioral Methods
Behavioral interventions represent promising approaches to preventing STDs. While there are many reports of behavioral interventions to prevent STDs including HIV infection, most studies have not been conducted in a methodologically sound manner to determine their effectiveness in improving health outcomes (Oakley, Fullerton, Holland, 1995; Oakley, et al., 1995). Many studies, however, show that behavioral interventions can have a positive effect on self-reported sexual health behaviors (Kalichman et al., 1996). In addition, two recent studies have demonstrated that certain feasible behavioral interventions are effective in reducing the risk of STDs (Kamb et al., 1996; Shain et al., 1996) and support a strong role for such interventions as part of a comprehensive approach to STD prevention.
A variety of strategies can lead to sustained behavior change to reduce risk of STDs. These intervention strategies include individually focused strategies; group- or community-based interventions (Kelly, 1994); and structural or “macro” level legislative solutions. The intent of behavioral interventions is to reduce the incidence of new STDs by assisting individuals in changing behaviors in ways that decrease risk of contracting STDs, such as increasing condom use, delaying initiation of sexual intercourse, or reducing number of partners. A review of federally funded HIV prevention studies that evaluated the impact of individual-and community-based behavioral interventions found that most interventions had positive effects on knowledge of AIDS and sexual behavior (IOM, 1994). An evaluation of the effectiveness of HIV prevention programs revealed that some behaviorally based prevention programs are actually cost-saving, and others are likely to be cost-effective relative to other health programs (Holtgrave et al., 1995).
Individual-Focused, Community-Based, and Mass Media Interventions
Intensive small-group risk reduction interventions, largely guided by cognitive-behavioral theory, have been shown to be very effective in promoting self-protective behavior change (Kelly, 1994; Cleary et al., 1995). Preliminary results of a major randomized, controlled trial evaluating the impact of enhanced prevention counseling for HIV and STD risk reduction strongly support individual-focused counseling (Kamb et al., 1996). In its latest report, the U.S. Preventive Services Task Force recommended that primary care clinicians counsel their adolescent and adult patients regarding measures to prevent STDs and that such counseling be tailored to the risk factors, needs, and abilities of each patient (U.S. Preventive Services Task Force, 1996). It is important to note that clinician counseling does not work in isolation, but it is a necessary component of appropriate clinical management of STDs. Couple-based interventions to prevent high-risk behaviors are also promising approaches (Allen et al., 1992).
Community-based interventions to promote behavior change include both interventions that target specific high-risk groups and interventions that attempt to change community norms, most commonly through mass media messages. A number of intervention trials involving high-risk groups have been successful in improving knowledge and promoting behavior change (Kelly et al., 1991, 1992; IOM, 1994; O'Reilly and Higgins, 1991). Some interventions have successfully changed norms in a community by utilizing peer opinion leaders and educators to endorse condoms and educate regarding their use (Kelly et al., 1991, 1992). Such interventions have resulted in a dramatic decline in the frequency of unprotected intercourse within several months (Kelly et al., 1992).
Public health workers recognize that, in order for behavior change to occur, the community environment should not be a barrier but be supportive of such changes. In response to this issue, “enabling approaches” to prevention have recently gained attention (Tawil et al., 1995; O'Reilly and Piot, 1996). These interventions are intended to either remove barriers to adoption of protective behaviors or to erect barriers to risky behaviors. Recent data indicate that environmental interventions that adequately address structural or other barriers to behavior change are necessary for the adoption of healthy sexual behaviors (Nelson et al., 1996).
There is compelling evidence that properly designed mass media campaigns can have beneficial effects on health behaviors (Flay, 1987). A recent review of HIV prevention mass media campaigns concluded that, with the exception of campaigns in Australia and Britain, most of the campaigns that were intended to increase knowledge were successful (Flora et al., 1995).10 One prominent example is a Swiss multimedia campaign to promote condom use among adolescents and young adults that has significantly increased condom use among these groups (Wasserfallen et al., 1993).
School-Based Interventions
School is the primary source of STD information for most teenagers (ASHA, 1996). Although many states require schools to provide instruction in HIV or STD prevention (CDC, 1996b; Collins et al., 1995), these legal mandates are often underfunded and restrictive in the content of the instruction (NARAL Foundation, 1995). For example, 19 states prohibit or restrict availability of, or in some cases information regarding, contraceptives to students through school health and education programs. Other limitations of current school-based education are the lack of consistent STD-related education at lower grade levels and inconsistent preparation of teachers who provide instruction on these topics (Collins et al., 1995; CDC, 1996b). The quality of studies that have evaluated the
|
10 |
See Appendix E of the full report. |
effectiveness of school-based programs to reduce risky sexual behaviors varies greatly. A comprehensive review of 23 studies of school-based sex and AIDS and STD education programs found that programs that included instruction on contraception either delayed the onset of sexual intercourse or had no effect on onset (Kirby et al., 1994). An evaluation of 23 local programs, including school-based programs, related to unintended pregnancy came to a similar conclusion (IOM, 1995).
Only 2.2 percent of all public high schools and 0.3 percent of all high school districts in the United States make condoms available to their students (Kirby and Brown, 1996). There are only limited data on the effectiveness of school-based condom availability programs in increasing health-protective sexual behaviors and decreasing STD rates, since these programs are relatively few and newly established (Kirby, 1993; Stryker et al., 1994). Studies, however, show that the benefits of such programs clearly outweigh the risks (Kirby et al., 1991; Wolk and Rosenbaum, 1995). There seems to be wide support for school condom availability programs among the public (The Roper Organization, 1991), students (Fanburg et al., 1995), parents (Guttmacher et al., 1995), and health care professionals (AAP, Committee on Adolescence, 1995). There is no evidence that students in schools with condom availability programs initiate sexual intercourse earlier or have intercourse more frequently compared with students in schools without such programs (Kirby et al., 1991; Kirby, 1994).
Other Methods
Prophylaxis
Currently, the only effective vaccine available for prevention of an STD is hepatitis B vaccine, but vaccines for other STDs are in various stages of development (NIH, 1996b). The Advisory Committee on Immunization Practice (ACIP) has recommended that hepatitis B vaccine be given to all infants (CDC, 1991b), all 11–12-year-old children who have not been previously vaccinated as part of a routine adolescent immunization visit (CDC, 1995e), and certain adults at high risk. Current data on hepatitis B vaccination coverage of persons in high-risk groups, including sexually active adolescents and men who have sex with men, are limited, but vaccination coverage is considered to be low (CDC, 1996d). Reasons for inadequate vaccination of these groups include lack of awareness among clinicians of groups at high risk for hepatitis B virus infection and lack of clinical opportunities to provide immunization, especially for adolescents (CDC, 1991b). Hepatitis B vaccination of adolescents has been successfully implemented in school-based clinics, primary care clinics, and other clinical settings (CDC, 1994; Kollar et al., 1994). Outside of limited federal demonstration projects, there are no major programs or public funds to increase vaccination of adults at high risk for sexually transmitted hepatitis B virus infection.
Condoms and Other Contraceptives
When used correctly and consistently (during every act of intercourse), condoms are highly effective against bacterial and viral STDs including HIV infection (Roper et al., 1993; Weller, 1993; Cates and Stone, 1992). Data show that condom use has increased in the United States in the last few decades, especially among younger persons (Peterson, 1995; Pleck et al., 1993; DeBuono et al., 1990). Factors that influence condom use include demographic factors, such as age, education level, race, and gender (Pleck et al., 1993; Tanfer et al., 1993); ability to negotiate condom use (Catania et al., 1992); individual perceptions of condoms (Anderson et al., 1996; Norris and Ford, 1994); and concerns that compete with protective behaviors among disenfranchised persons (Mays and Cochran, 1988; Donovan, 1996). Factors that are particularly important determinants of condom use among adolescents include access, availability, confidentiality, and cost of condoms (AAP, Committee on Adolescence, 1995; Kirby, 1994).
Women who rely on sterilization, oral contraceptives, or another method for protecting against pregnancy are less likely to use condoms for disease prevention compared with other women (CDC, 1992c, 1992e; Anderson et al., 1996; Santelli et al., 1996). Sterilization and oral contraceptives are highly effective against pregnancy, but not effective against HIV infection or other STDs. Because no single method of preventing STDs or pregnancy confers the maximum level of protection against both conditions (Cates and Stone, 1992), use of dual protection—that is, a condom and another effective contraceptive for pregnancy—is especially important. It is not clear, however, how well the public understands the need for dual protection against STDs and pregnancy. Although the female condom has recently been approved for use in the United States (CDC, 1993b; IOM, 1996a), additional female-controlled contraceptive methods that are effective against all STDs are needed (Stein, 1992; Cates et al., 1992; Rosenberg and Gollub, 1992), including chemical or physical barriers to conception and to transmission of STDs (IOM, 1996a).
Partner Notification and Treatment
Partner notification has been a component of STD programs in the United States for many years (Rothenberg and Potterat, 1990). Recent studies, however, show that current methods for partner notification are not highly effective (Gunn et al., 1995) for a number of reasons. These include concerns about the safety of the interviewers working in high-crime communities; the cultural sensitivity of the STD interviewers; and the large number of anonymous partners involved in sex-for-drug activities (Andrus et al., 1990; Oxman and Doyle, 1996). Implementing alternative case finding methods (CDC, 1991a; Engelgau et al., 1995) and refocusing partner outreach toward communities and social networks (Gunn
et al., 1995; Rothenburg and Narramore, 1996; Klovdahl et al., 1994; Trotter et al., 1995), rather than utilizing traditional methods of partner identification, have been suggested as more effective strategies for reaching high-risk individuals (Rothenberg and Potterat, in press).
Screening
Screening programs for many STDs are cost-effective, and sometimes cost-saving (Trachtenberg et al., 1988; Handsfield et al., 1986; Hillis et al., 1995; Britton et al., 1992; Randolph and Washington, 1990; Arevalo and Washington, 1988; Scholes et al., 1996). For example, using a decision model, Trachtenberg and colleagues (1988) estimated a net savings of more than $60 million (1986 dollars) over the first five years of a California statewide chlamydia screening program for asymptomatic women in family planning clinics. The Centers for Disease Control and Prevention (CDC) estimates that approximately $12 in costs associated with the complications of chlamydia and gonococcal infection could be saved for every $1 spent on early detection and treatment (CDC, DSTD/HIVP, 1995a). The U.S. Preventive Services Task Force (1996) recently recommended a group of screening activities for primary care clinicians based on the age and STD risk categories of patients.11
Not all screening programs are effective prevention measures. For example, as of 1996, 15 states still require premarital syphilis testing as a requirement for marriage licenses (CDC, Division of STD Prevention, unpublished data, 1996). The number of previously undetected cases of syphilis identified through premarital testing is extremely low (Haskell, 1984; Felman 1981). In addition, studies show that premarital tests for syphilis or HIV are not cost-effective and have little public health impact (Haskell, 1984; Cleary et al., 1987; Peterson and White, 1990).
REDUCING DURATION OF INFECTION
Reducing the duration of STDs can be accomplished primarily by ensuring early diagnosis and treatment of infected persons and by reducing barriers to diagnostic and treatment services. Reducing the duration of STDs among infected individuals will reduce the period of time that an individual is infectious, and consequently reduce the numbers of partners exposed to infection. Early, specific diagnosis and treatment of symptomatic and asymptomatic individuals will prevent further transmission of STDs to their partners.
Appropriate diagnosis of an STD often requires multiple specific diagnostic tests because of the variety of STDs. Further complicating the diagnosis of STDs is the availability of several different diagnostic tests for each STD. Unfortu-
|
11 |
See Appendix F of the full report. |
nately, many clinicians fail to appreciate that no single laboratory test is optimal for use in all settings. In addition, some laboratory tests are unavailable at certain clinical sites, test results are often unavailable during the initial patient visit, and the expense of these tests may limit their availability and utility.
The diagnosis of an STD should lead to either curative or preventive therapy for the infected individual. While ideal therapy does not exist for many infections, highly effective antimicrobial therapy is available for all bacterial STDs as well as those caused by protozoa and ectoparasites (CDC, 1993a). In contrast, drugs for viral STDs have largely been limited to alleviating symptoms because they cannot eradicate the organism. A significant barrier to appropriate treatment is failure to comply with a full course of medication. To address this problem, effective single-dose therapy for several STDs (e.g., chancroid, gonorrhea, syphilis, trichomoniasis) has been available for some time and single-dose therapy for chlamydial infection has recently become available. These single-dose regimens, while more expensive, have been shown to be as effective as multiple-dose regimens (CDC, 1993a; Thorpe et al., 1996; Zenilman, 1996). Other major barriers to early diagnosis and treatment of infected persons include inadequate access to health care, lack of health-seeking behavior, inadequate training of health care professionals,, inadequate financial and physical access to laboratory tests, and geographic factors.
CURRENT STD-RELATED SERVICES
Clinical services for STDs are provided in dedicated public STD clinics 12operated by local health departments, community-based health clinics operated by community-based health professionals or public agencies, and private health care settings. Most clinicians providing STD-related care in public or private settings emphasize diagnosis and treatment and, to a lesser extent, management of sex partners, rather than other approaches to STD prevention (Bowman et al., 1992). Most do not provide adequate STD risk assessment, prevention counseling, or other STD-related education (Bowman et al., 1992; ARHP and ANPRH, 1995; Boekeloo et al., 1991).
Services in Dedicated Public STD Clinics
The concept of a dedicated public STD clinic is based on evidence that many
|
12 |
The committee uses the term “dedicated public STD clinics” to refer to publicly funded clinics whose main purpose is to provide STD-related services. Other clinics that provide STD-related services in the context of other services, such as community health centers, family planning clinics, migrant health centers, and school-based clinics, are not considered to be dedicated public STD clinics. The term “categorical STD clinic” is not used because it invites confusion with “categorical funding.” |
persons with STDs prefer anonymous and confidential services, cannot afford to obtain care elsewhere, and are unable to obtain care from private sector health care professionals who are unable or unwilling to provide STD-related care. The CDC is the only federal agency that supports dedicated public STD clinics. State and local health departments also provide financial support for these clinics and programs and are often given responsibility for operating the clinics under federal policies and guidelines.
Persons attending dedicated public STD clinics are generally young, disproportionately of certain racial or ethnic groups, and at high risk for multiple STDs (Celum et al., 1995). A substantial number of patients in dedicated public STD clinics have private health insurance coverage, and many privately insured patients use public STD clinics without acknowledging their health insurance status.
Based on published data, the committee's interactions with other health professionals, site visits, results of site assessments conducted by the CDC, and personal experience working with dedicated public STD clinics, it was concluded that the quality of care, scope of services provided, and other characteristics of these clinics are quite variable. In addition, the scope and level of services provided by many such clinics are limited by available resources, and these clinics often emphasize diagnosis and treatment and partner notification activities for a limited number of STDs. Further, counseling and health education activities often are not emphasized, and providers receive little training in techniques and skills for conducting education or counseling (Lewis et al., 1987; Roter et al., 1990; Stein, 1996). The performance of these clinics is usually evaluated on the basis of quantitative measures, such as numbers of patients seen and number of cases of specific diseases diagnosed, rather than on quality of care or other performance measures. Access to services after hours and on weekends is uncommon. For example, a large survey of local health agencies showed that only 23 percent of agencies offered services after 6 p.m. and only 5 percent had weekend hours (Landry and Forrest, in press).
Services in Community-Based and School-Based Clinics
Many types of community-based clinics, such as family planning clinics, prenatal clinics, youth and teen clinics, homeless programs, community-based health centers, and school-based clinics, provide STD-related services. STDs are not the primary focus for these clinics, but rather are dealt with in a context of providing general or specific (e.g., family planning) health care services. Although the populations served by community-based clinics overlap substantially with STD clinic patients, there is surprisingly little communication between these facilities. School-based health clinics in elementary and high schools and student health services on university and college campuses often provide STD-related services for their students. In 1994, diagnostic and treatment services for STDs
were available in 16 percent of all middle and junior high schools and in 20 percent of all senior high schools in the United States (Leavy Small et al., 1995).
Services in Private Sector Settings
Most cases of STDs are diagnosed by private sector health care professionals (Berg, 1990), but very little is known about the volume, extent, disease prevalence, or spectrum of STDs encountered in private sector settings compared with either dedicated public STD clinics or community-based clinics. Available data suggest that the patterns of diseases seen in these settings may be quite different from those seen in public clinics (CDC, DSTDP, 1995). Studies of the scope and appropriateness of STD-related services in private sector settings indicate that such services need to be improved. For example, in a recent survey, 55 percent of California primary care physicians reported treating at least one case of pelvic inflammatory disease during the previous 12-month period and, of these physicians, 52 percent were either unsure of or did not follow the CDC's treatment guidelines for this STD (Hessol et al., 1996). Partner notification is not well supported in private sector settings probably because most private sector clinicians do not accept responsibility for partner notification, there is no reimbursement for care of sex partners, and providers may be either reluctant or not trained to interview patients regarding sexual practices.
Services in Managed Care Organizations and Other Health Plans
The rapid growth of managed care organizations13 in the United States (GHAA, 1995) and the rapid pace of conversion of state Medicaid programs to prepaid managed care plans (The Kaiser Commission on the Future of Medicaid, 1995) have generated concerns regarding the design and implementation of these new programs and the accountability of the new managed care plans for quality (Fisher, 1994).
There are both opportunities and concerns associated with the increased involvement of managed care organizations in the delivery of preventive and public health services (CDC, 1995c). Compared with traditional indemnity health insurance plans and private practice providers, managed care organizations may
|
13 |
The committee uses the term “managed care organization” to refer to health plans that are prepaid for health care services and that are covered by the defined benefits of the plan—that is, health plans that provide, or arrange and pay for, all covered health services needed by the enrollee, in return for a specified premium plus any allowed copayments. This definition best describes health maintenance organizations (HMOs). The committee applies the term “managed care organization” only to health plans that use methods similar to those of health maintenance organizations. The committee uses the general term “ health plan” to refer to all types of health insurance plans, including managed care organizations and fee-for-service indemnity plans. |
be better able to improve STD-related services because they have an incentive to provide preventive services; can more readily implement planwide programs; are more likely to have a population-based perspective; can support the services of highly trained health professionals; usually have highly developed information systems to monitor STD-related trends; and can be held accountable to purchasers for specific performance standards. A recent study showed that identifying, testing, and treating women at increased risk for asymptomatic chlamydial infection in a managed care organization reduced the rate of pelvic inflammatory disease by more than 50 percent compared with women who received routine care (Scholes et al., 1996).
The potential concerns regarding the increased role of managed care organizations in STD prevention include the following: STDs are not a high priority for most managed care organizations; there is a wide range of technical ability among such organizations in delivering services; managed care organizations may be reluctant to provide STD-related services that have not been shown to be cost-saving; persons with STDs may prefer to receive care outside of the plan for confidentiality or other reasons; and managed care organizations may not provide services to sex partners of plan members if the partner is not a plan member.
A committee survey14 of managed care organizations selected primarily on the basis of their likelihood of serving high-risk populations (i.e., Medicaid, inner city), and therefore their increased likelihood of providing STD-related services, found that more than half (57 percent) of these organizations attempted to define high-risk groups for STDs and approximately half reported providing STD-related services that specifically targeted adolescents. Only 26 percent of managed care organizations reported that they provided STD-related services to persons outside their plan.
NATIONAL SURVEILLANCE AND INFORMATION SYSTEMS
National surveillance for STDs is part of the national public health notifiable disease reporting system coordinated by the CDC. This system is fundamentally a “passive” system, and active case finding for STDs is not routinely conducted. The passive reporting system for STDs has several major limitations, including underestimation of true STD incidence and reporting bias toward public sector providers (Anderson et al., 1994). Surveillance data are especially difficult to interpret when new diseases are added to the list of notifiable diseases or when new diagnostic technologies become available and are increasingly utilized.
A crucial but underdeveloped tool for directing and targeting STD prevention programs is the behavioral health survey. Examples of periodic surveys that are important in monitoring national trends in STD-related health behaviors in-
|
14 |
See Appendix H of the full report. |
clude the Behavioral Risk Factors Surveillance Survey, the Youth Risk Behavior Surveillance System, the National Survey of Family Growth, the National Health and Nutrition Examination Survey (NHANES), and the National Survey of Adolescent Males. Other health behavior surveys and studies that are not periodically administered, such as the National Health and Social Life Survey (Laumann, Gagnon, et al., 1994), have also produced important data regarding sexual behavior. Serologic testing of sera collected as part of nationally representative data sets, such as the National Health and Nutrition Examination Survey, are potentially valuable adjuncts to routine disease or behavioral surveillance data, but such linked testing has been very limited.
The committee is not aware of nongovernmental organizations or associations that routinely collect data regarding STDs. However, the National Committee for Quality Assurance, through its Committee on Performance Measurement, is currently evaluating an STD-related performance measure (i.e., the percentage of women between the ages of 15 and 25 who were screened for chlamydial infection in the past year) for inclusion in subsequent versions of the Health Plan Employer Data Information System (HEDIS)15 (NCQA, Committee on Performance Measurement, 1996).
TRAINING AND EDUCATION OF HEALTH PROFESSIONALS
Training and education of clinicians is important because inadequate STD training and education results in inappropriate or inadequate clinical care for STDs (Hessol et al., 1996). Studies show that training in STD-related clinical skills in U.S. medical schools is generally inadequate (MacKay et al., 1995; Stamm et al., 1982). Another IOM committee that examined the future of primary care concluded that the current system of clinical training for health care professionals is inadequate in preparing effective primary care professionals (IOM, 1996b). That committee recommended that clinical training be based on a common core set of clinical competencies, regardless of their disciplinary background, to be defined by a coalition of educational and professional organizations and accrediting bodies. New advances in information technology, such as the Internet and telemedicine, may prove to be important facilitators of training and education. Information technology, for example, has enabled many primary care clinicians to learn new skills or improve current practice through distance learning activities such as televised courses.
|
15 |
This performance measurement tool is utilized primarily by employers and other purchasers of health care to compare and evaluate large managed care organizations and has great potential for monitoring STD-related services among such health plans. |
FUNDING OF SERVICES
Funding for state and local health department activities in STD prevention comes from the CDC through cooperative agreements, and from state and local governments. Reimbursement for STD-related services in the private sector comes from third-party reimbursement, such as private health insurance and Medicaid. Community-based health facilities such as family planning clinics and community health centers receive federal and other support to provide STD-related care. Local health departments only receive reimbursement for services provided by public STD clinics to persons with private insurance to the extent allowed by law or under written contract.
Using some broad assumptions regarding public funding for prevention and research activities and state and local contributions to STD-related services, the committee estimates that the total national public investment in STD prevention in federal fiscal year 1995 was approximately $230.8 million and that an additional $105.4 million was invested in biomedical and clinical STD research.16 Comparing these estimates to the estimated total costs of selected STDs (approximately $10 billion), the total costs associated with STDs in the United States in 1994 were approximately 43 times the total national public investment in STD prevention and 94 times the total national investment in STD-related research (Figure S-2). State and local governments vary widely in their financial support for STD-related programs.
Current legislative proposals seek to consolidate some federal categorical programs, including STD programs, into block grants to the states. Proponents of block grants argue that categorical funding has forced programmatic rigidity and excess administrative costs upon local programs, thereby restraining innovation and local flexibility. Opponents of consolidating STD funding into a block grant along with other public health programs believe that STDs will suffer in competition with less controversial public health problems or other state priorities, because STD programs have traditionally weak political constituencies and cannot compete with programs that have powerful constituencies. In addition, allowing states to set funding allocations would increase the already wide variability in STD programs among the states because some states may seriously neglect STD programs.
CONCLUSIONS AND RECOMMENDATIONS
The committee concludes that an effective national system for STD prevention currently does not exist and, as a result, STDs are a severe health burden in
|
16 |
Further details regarding the methods for estimating the costs of STDs and national investments in STD prevention are presented in Chapters 2 and 5 of the full report. |
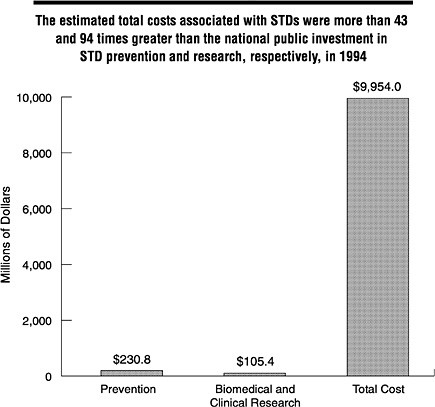
FIGURE S-2 Comparison of estimated annual total costs for selected STDs and their complications in 1994 versus national investment in STD prevention and research in federal fiscal year 1995. NOTE: The estimate for investment in STD prevention provided here represents public funding for all interventions, behavioral, curative, or otherwise, that are needed to reduce the spread of infection in a population. SOURCES: Total cost of illness estimates calculated by the IOM Committee on Prevention and Control of STDs; estimate of federal, state, and local investment in STD prevention based on unpublished data from the CDC, Division of STD Prevention, 1996; and estimate of national investment in research based on unpublished data from the National Institutes of Health, 1996.
the United States. Many components of an effective system need to be redesigned and improved through innovative approaches and closer collaborations. In addition, programs that address important gaps in the current fragmented system of services have not yet been designed and implemented. The committee's recommendations are outlined below and presented in complete detail in Chapter 6 of the full report.
In formulating a strategy to prevent STDs, the committee developed the following vision statement to guide its deliberations.
Vision
An effective system of services and information that supports individuals, families, and communities in preventing STDs, including HIV infection, and ensures comprehensive, high-quality STD-related health services for all persons
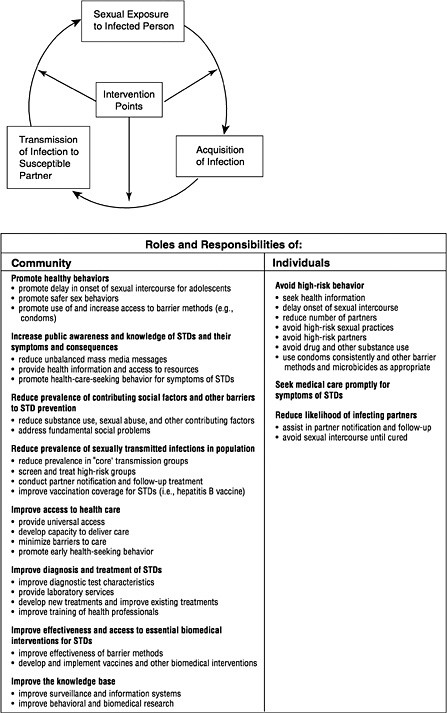
This vision and the committee's proposed model for improving STD prevention are founded on a multifaceted approach to STD prevention, shared responsibility and active participation by individuals and the community, coordination of related programs, and adequate resources and support for implementation (Figure S-3).
To realize this vision, the committee recommends that:
-
An effective national system for STD prevention be established in the United States.
The committee envisions a system based on national policy, coordinated at all levels, and composed of local, state, and national prevention programs. A national system is essential because STDs are a threat to the nation's health, because many interventions are most effectively or efficiently developed and implemented at the national level, and because STDs do not recognize geographic borders.
To establish a national system for STD prevention, the committee recommends four major strategies for public and private sector policymakers at the local, state, and national levels:
-
Overcome barriers to adoption of healthy sexual behaviors.
-
Develop strong leadership, strengthen investment, and improve information systems for STD prevention.
-
Design and implement essential STD-related services in innovative ways for adolescents and underserved populations.
-
Ensure access to and quality of essential clinical services for STDs.
Before describing the recommended tactics for these four strategies, the committee makes the following recommendations regarding two important concepts that need to be incorporated into a national strategy to prevent STDs: the impact of STDs on HIV transmission and the impact of STDs on cancer.
-
Improved prevention of STDs should be an essential component of a national strategy for preventing sexually transmitted HIV infection.
-
Government agencies and private organizations concerned with cancer prevention should support STD prevention activities as an important strategy for prevention of STD-related cancers.
Strategy 1: Overcome barriers to adoption of healthy sexual behaviors.
Barriers to effective STD prevention efforts include biological, social, and structural factors. One of the primary obstacles is this country's reluctance to openly confront issues regarding sexuality and STDs. Failure to acknowledge and discuss sexuality impedes STD education programs, open communication between parents and their children and between sex partners, balanced messages from mass media, education and counseling activities of clinicians, community activism for STDs, and behavioral research.
Catalyzing Change Through Open Discussion and Promoting Awareness and Balanced Mass Media Messages
A new social norm of healthy sexual behavior should be the basis for long-term prevention of STDs. This is because in one way or another all interventions to prevent STDs are partly dependent on, and must be integrated with, healthy behaviors. In order for societal norms regarding sexual behavior to change, open discussion of and access to information regarding sexual behaviors, their health consequences, and methods for protecting against STDs must occur. Therefore, the committee believes that a significant national campaign to foster social change toward a new norm of healthy sexual behavior in the United States is necessary. An independent entity is needed to promote a social norm of healthy sexual behavior because, based on experience with past initiatives, limitations on government agencies regarding public education programs related to sexuality are particularly problematic.
Lack of awareness regarding STDs and misperception of individual risk and consequences are major barriers to healthy sexual behavior, especially among adolescents and young adults. Lack of open communication and information regarding sexuality and STDs fosters misperceptions and may actually encourage high-risk sexual behaviors. Increased awareness regarding STDs should result in increased individual motivation to prevent STDs and should improve the detection and management of STDs by clinicians. A national campaign to increase public and health care provider awareness of STDs requires active participation of both private and public agencies and organizations to succeed.
Despite their current lack of involvement in promoting healthy sexual behav-
iors, the mass media can be extremely powerful allies in efforts to prevent STDs by increasing knowledge and changing behavior. Mass media messages that promote healthy sexual behaviors will facilitate needed changes in social norms regarding sexual behaviors because mass media help define these norms. Children and adolescents are particularly exposed and susceptible to explicit and implicit messages in such media. Many adolescents are not receiving appropriate information regarding STDs and sexual behavior from their parents or other sources. Therefore, mass media companies should disseminate information regarding STDs and healthy sexual behaviors, including delaying sexual intercourse and using condoms, with a special focus on reaching adolescents and young adults. Comprehensive public health messages regarding STDs, including HIV infection; sexual abuse; and unintended pregnancy are essential.
With respect to the above issues, the committee makes the following recommendations:
-
An independent, long-term, national campaign should be established to (a) serve as a catalyst for social change toward a new norm of healthy sexual behavior in the United States; (b) support and implement a long-term national initiative to increase knowledge and awareness of STDs and promote ways to prevent them; and (c) develop a standing committee to function as an expert resource and to develop guidelines and resources for incorporating messages regarding STDs and healthy sexual behaviors into all forms of mass media.17
-
Television, radio, print, music, and other mass media companies should accept advertisements and sponsor public service messages that promote condom use and other means of protecting against STDs and unintended pregnancy, including delaying sexual intercourse.
Improving Professional Skills in Sexual Health Issues
It is important that clinicians, educators, and other professionals develop knowledge and awareness of sexual health issues and become comfortable discussing them. This will enable clinicians to utilize clinical opportunities to effectively counsel patients regarding healthy sexual behaviors, and therefore improve clinical care for STDs. Communicating effectively with patients regarding sexual health is a particularly critical skill for clinicians and other professionals, but most are not adequately trained in communication and counseling skills.
With respect to the above issues, the committee makes the following recommendation:
|
17 |
This recommendation condenses three recommendations presented in Chapter 6 of the full report. |
-
The Health Resources and Services Administration, health professional schools and associations, and schools and associations for training educators should support comprehensive sexuality training for health care professionals, educators, and researchers in order to increase their comfort working with sexual health issues and to increase their effectiveness in sexual behavior counseling.
Supporting Sexual Health Behavior Research
Population-based surveys and studies of STD-related health behaviors are critical for monitoring population trends in health behaviors, developing effective interventions, and evaluating program effectiveness. Such research, however, have been severely criticized by some policymakers and interest groups. This committee, while recognizing the sincere concerns expressed, strongly believes that research regarding STD-related health behaviors, especially among adolescents, is critical to STD prevention. Federal funding and support for sexual health behavior research is essential. The committee found no evidence that asking questions regarding sexual activity increases sexual activity among survey respondents. Restrictions on collecting behavioral information from adolescents would seriously jeopardize behavioral research and the ability to prevent high-risk behaviors among adolescents. The committee also believes that the objectivity and integrity of the peer-review process for scientific research should be protected.
With respect to the above issues, the committee makes the following recommendation:
-
The National Institutes of Health and other federal agencies should continue to support research on health behaviors, including sexual behaviors, and their relationship to STDs.
Strategy 2. Develop strong leadership, strengthen investment, and improve information systems for STD prevention.
Developing Leadership and Catalyzing Partnerships
To build an effective national system, highly visible and strong leadership and support are needed from both the public and private sectors, and especially from elected officials. Among public agencies, the Department of Health and Human Services, especially the CDC, and state and local health departments have critical leadership roles. The public sector must continue to play a major role in preventing STDs, but does not have the resources or the organizational reach to
fully implement a national system of STD-related services. The private sector must therefore take more responsibility.
The barriers to an effective national system for STD prevention are found in government, private sector organizations, and political factors and social norms. Overcoming these barriers is a challenge that requires the active participation of all levels of government, the private health care sector, businesses, labor leaders, the mass media, schools, and many community-based organizations. In developing and implementing a national system for STD prevention, it is important that stakeholders be involved in all steps of the process; however, a formal mechanism for collaboration among agencies and organizations does not exist. Therefore, a neutral forum is needed to maximize the range of participants and to catalyze the collaborative process.
With respect to the above issues, the committee makes the following recommendations:
-
Private sector organizations and clinicians should assume more leadership and responsibility for STD prevention.
-
Federal, state, and local governments, through the leadership of their respective health agencies, should ensure that all persons have access to comprehensive, high-quality STD-related services. 18
-
An independent, long-term national roundtable should be established as a neutral forum for public and private sector agencies and organizations to collaboratively develop and implement a comprehensive system of STD-related services in the United States.
Strengthening Investment
To establish an effective system of STD prevention, a substantially greater investment from both the public and private sectors is needed. The current national public investment in STD prevention is not commensurate with the health and economic costs of STDs. As mentioned previously, the committee estimates that only $1 is invested in STD prevention for every $43 spent on the STD-associated costs every year. Similarly, only $1 is invested in biomedical and clinical research for every $94 in STD-related costs. Investing in preventive services and research will avert substantial human suffering and save billions of dollars in treatment costs and lost productivity. Additional funding for STD prevention should come from local, state, and federal governments and from the private sector. Private health plans, in particular, need to increase support for
|
18 |
This recommendation condenses three recommendations presented in Chapter 6 of the full report. |
STD-related services that benefit their enrolled population and ultimately benefit the health plan's financial status. In addition, because STDs are emerging infections and a global public health problem, the United States has a national interest in preventing STDs worldwide. Despite the problems in the current system of categorical funding for STDs, moving to a system of block grants would have a devastating impact on STD prevention because STDs will fare poorly in competing with other more visible and “acceptable” health conditions for funding.
With respect to the above issues, the committee makes the following recommendations:
-
Federal, state, and local elected officials should provide additional funding for STD prevention.
-
The CDC should retain and immediately redesign categorical funding for STD programs.
-
The federal government, through the Department of Health and Human Services and the U.S. Agency for International Development, and international organizations, such as the World Health Organization and the World Bank, should provide resources and technical assistance to global efforts to prevent STDs.
Improving Surveillance and Other Information Systems
National surveillance and other information systems for STDs are important in monitoring and evaluating a national system for prevention. Data from these information systems are critical to long-term program planning as well as to day-to-day management of programs. The current surveillance system needs enhancement because it does not give accurate estimates of disease incidence. This is because not all persons with STDs seek medical care and because many clinical encounters with health care professionals, especially in private sector settings, are not reported. It is critical that a systematic, comprehensive evaluation of the national surveillance system be conducted to describe the attributes of the system and to provide guidance for future improvements. STD surveillance systems should include and link information from public sector, community-based, and private health care professionals. Special emphasis should be placed on educating clinicians about reporting and on collaborating with and collecting data from private sector providers, including health plans.
With respect to the above issues, the committee makes the following recommendations:
-
The CDC should lead a coordinated national effort to improve the surveillance of STDs and their associated complications and improve the monitoring of STD prevention program effectiveness.
-
Federal, state, and local STD programs should encourage and provide technical assistance to employers and other purchasers of health care (including Medicaid programs), managed care organizations and other health plans, and other health care professionals to develop and utilize information systems that effectively integrate preventive services performance data with community health status indicators and STD program data.
-
STD-related performance measures should be included in the Health Plan Employer Data Information System (HEDIS) and other health services performance measures to improve quality-assurance monitoring of STDs.
Strategy 3: Design and implement essential STD-related services in innovative ways for adolescents and underserved populations.
Adolescents and underserved populations require special emphasis in an effective national system for STD prevention because they are at high risk for STDs and they do not have adequate access to STD-related services. Innovative methods for delivering STD-related services to such populations should immediately be designed and implemented because these groups are difficult to reach through traditional clinical settings and approaches.
Focusing on Prevention
A national strategy for STDs should emphasize prevention because averting illness is desirable, many STDs are incurable, and STD-related complications may be irreversible. Effective prevention programs are usually the result of extensive research and evaluation and continuous quality improvement. They should be regularly modified based on the epidemiology of STDs and continuous evaluation of programs. Prevention-related research allows program managers and policymakers to maximize the effectiveness of interventions and available resources. Areas of prevention-related research that should be emphasized include determinants of sexual behavior and sustained behavior change; determinants of initiation of sexual intercourse among adolescents; influence of social and other community-related factors on risk of STDs; interventions to improve condom use and reduce high-risk behaviors; effectiveness of sexual risk behavior assessment and counseling; biomedical interventions such as vaccines that do not rely primarily on individual behavior; female-controlled prevention methods; cost effectiveness of interventions; methods for preventing STDs among disenfranchised populations; interventions for preventing STDs among persons of all sexual orientations; and methods to assess prevention program effectiveness.
With respect to the above issues, the committee makes the following recommendations:
-
The National Institutes of Health and the CDC should continue to support and expand both basic and applied research in STD prevention.
-
The National Institutes of Health, the Food and Drug Administration, and pharmaceutical, biotechnology, and medical device companies should collaboratively develop effective female-controlled methods for preventing STDs.
Focusing on Adolescents
Although many of the severe health consequences of STDs manifest themselves among adults, these complications usually result from infections acquired or health behaviors initiated during adolescence. By the twelfth grade, nearly 70 percent of adolescents have had sexual intercourse, and approximately one-quarter of all students have had sex with four or more partners. Therefore, a national strategy to prevent STDs needs to focus on adolescents. The committee believes that adolescents should be strongly encouraged to delay sexual intercourse until they are emotionally mature enough to take responsibility for this activity. However, most individuals will initiate sexual intercourse during adolescence, and they should have access to information and instruction regarding STDs (including HIV infection) and unintended pregnancy and methods for preventing them.
Many school-based programs and mass media campaigns are effective in improving knowledge regarding STDs and in promoting healthy sexual behaviors, and these two interventions should be major components of an STD prevention strategy. The committee believes that there is strong scientific evidence in support of school-based programs for STD prevention, that adolescence is the critical period for adopting healthy behaviors, and that schools are one of the few venues available to reach adolescents. Given the high rates of sexual intercourse among adolescents and the significant barriers that hinder the ability of adolescents to purchase and use condoms, condoms should be available in schools as part of a comprehensive STD prevention program. There is no evidence that condom availability or school-based programs for sexuality or STD education promote sexual activity.
STD-related clinical services for adolescents, including hepatitis B immunization, should be expanded through school and student health clinics, because adolescents are less likely than adults to have health insurance and they infrequently use regular health care facilities. Adolescents who are not enrolled in school also need access to clinical services. Because confidentiality is a major concern for adolescents, they should be able to consent to STD-related services without parental knowledge.
With respect to the above issues, the committee makes the following recommendations:
-
A major part of a national strategy to prevent STDs should focus on
-
adolescents and interventions should begin before sexual activity is initiated, which may be before adolescence is reached. Interventions should focus on preventing the establishment of high-risk sexual behaviors.
-
All health plans and health care providers should implement policies in compliance with state laws to ensure confidentiality of STD- and family planning-related services provided to adolescents and other individuals.
-
All school districts in the United States should ensure that schools provide essential, age-appropriate STD-related services, including health education, access to condoms, and readily accessible and available clinical services, such as school-based clinical services, to prevent STDs.
-
All health plans, clinicians, and publicly sponsored health clinics should provide or arrange for hepatitis B immunizations for their adolescent and adult patients according to the Advisory Committee on Immunization Practices (ACIP) guidelines. Given the difficulty in reaching adolescents in health care settings, public health officials should ensure that adolescents who are not immunized in health care settings are immunized through school-based or other community programs.
Establishing New Venues for Interventions
Although services for disenfranchised groups, including substance users, sex workers, the homeless, prisoners, and migrant workers, do not have popular support, these populations represent reservoirs of infection for the entire community. Innovative methods and alternate venues for intervention are needed because these groups are difficult to reach through traditional health care settings. Nontraditional venues for delivering STD-related services, such as prisons, drug treatment clinics, the streets, and other sites where high-risk persons gather, are appropriate sites for preventive services. Health departments should establish linkages with programs that serve populations at high risk for STDs, and government agencies should coordinate their various STD-related programs because the lack of coordination and unevenness of services have resulted in critical gaps in service coverage. To contain persisting epidemics of STDs among disenfranchised persons, new biomedical, epidemiological, and behavioral tools should be developed collaboratively by the public and private sector.
With respect to the above issues, the committee makes the following recommendations:
-
Federal, state, and local agencies should focus on reducing STDs among disenfranchised populations (e.g., substance users, persons in detention facilities, sex workers, the homeless, migrant workers).
-
Prisons and other detention facilities should provide comprehensive STD-related services including STD prevention counseling and education, screening, diagnosis and treatment, partner notification and treatment, and
-
methods for reducing unprotected sexual intercourse and drug use among prisoners.
-
The National Institutes of Health, the Food and Drug Administration, and the CDC should work with pharmaceutical and biotechnology companies to develop improved STD diagnostic tools (e.g., rapid saliva and urine tests) that are suitable for use in nontraditional health care settings (e.g., prisons, mobile clinics, the streets).
Strategy 4: Ensure access to and quality of essential clinical services for STDs.
Both public and private sector clinical services for STDs are currently fragmented, inadequate, and sometimes of poor quality. This situation leads to coverage gaps, inadequate access to services, and ineffective clinical care.
Ensuring Access to Services in the Community
Access to services is facilitated by expanding the availability of STD-related services through primary care and by coordinating services at the local level. Universal and timely access to curative and preventive services are supported by eliminating financial barriers to obtaining health services, minimizing other barriers, ensuring that patients are not stigmatized, and ensuring that services are culturally appropriate. Given the broad spectrum of risk groups, access to STD-related services in multiple settings—including private sector clinics, family planning clinics, prenatal clinics, adolescent and school-based clinics, HIV clinics, community health centers, and other settings not traditionally targeted by STD programs—is important. STD-related services need to be incorporated into primary care because primary care fosters ongoing relationships between the clinician and the individual, increasing the likelihood of effective preventive interventions and early detection of STDs. In addition, incorporating STD-related services into primary care may increase access to and improve quality of STD-related care.
Each community has responsibility for ensuring universal access to comprehensive STD-related services. However, because communities differ widely in their health needs and capacity to support a system of STD-related services, the organization of community STD-related services should be tailored to local needs and conditions. Depending on local situations, health departments should incorporate STD-related services into public and private primary health care services. Depending on epidemiologic patterns, health insurance coverage, population density, and other community characteristics, they may continue to support dedicated public STD clinics, or may shift such services to community-based clinics or the private sector.
With respect to the above issues, the committee makes the following recommendations:
-
Comprehensive STD-related services should be incorporated into primary care, including reproductive health services.
-
Local health departments, with the assistance of the state health department, and in consultation with the community, should determine how to provide high-quality, comprehensive STD-related clinical services that meet federal and state quality standards most effectively in their communities.
Improving Dedicated Public STD Clinics
There is wide variation in the quality, scope, accessibility, and availability of services provided by dedicated public STD clinics, and these clinics need significant improvement. Many local health departments operate dedicated public STD clinics that are isolated from other public health and clinical services and for which quality monitoring and assessment have not been priorities. The committee supports incorporating STD-related services in primary care settings, but it also believes that dedicated public STD clinics should continue to be an important component of STD prevention. In some situations these clinics are the primary providers of STD-related services for the uninsured and provide an important focus for STD prevention in the community. In all cases, health departments operating dedicated public STD clinics should ensure that these clinics collaborate with community-based health clinics (including family planning clinics and school-based programs), university and hospital medical centers, and private sector health care professionals to improve access and quality of care. Standards to maintain access to confidential services and to monitor quality should be developed for STD-related services provided by public STD clinics, health plans, and by public-private sector arrangements.
With respect to the above issues, the committee makes the following recommendations:
-
Based upon local conditions and health department determination, dedicated public STD clinics should continue to function as a “safety net” provider of STD-related services for uninsured and disenfranchised persons and for those who prefer to obtain care from such clinics.
-
The CDC, in collaboration with state and local health departments, should ensure that services provided by dedicated public STD clinics are of high quality.
-
Health professional schools, including schools of medicine, nursing, and physician assistants, should partner with a local health department for purposes of STD clinic staffing, management, and professional training.
Involving Health Plans and Purchasers of Health Care
The committee believes that if certain concerns are adequately addressed, there is substantial potential for managed care to improve the quality of and access to STD-related services. Compared with other health plans, the structure and resources of most managed care organizations allow for improved coordination and integration of care, accountability of services, incentives to provide preventive services, and monitoring of service quality. However, the current performance of managed care in STD prevention has not yet lived up to its potential. With very few exceptions, STDs are not high priorities among health plans, and few are involved in activities to prevent STDs in the larger community beyond plan members. Managed care organizations and other health plans should take on more responsibility for providing STD prevention services, both among plan members and in the community in which they operate. By supporting such activities among plan members and the community, significant health care costs associated with serious complications of STDs will be averted; health plan members will be less likely to be exposed to infected partners or to acquire reinfections; and long-term complications of STDs will be prevented among current and future plan members in the community. Employers, government agencies, and other purchasers of health care services are vital to ensuring that health plans provide comprehensive, high-quality STD-related services. Health plans should develop collaborative agreements with local public health agencies that include payment for public sector STD-related services utilized by their enrollees. Most local health departments have not developed billing arrangements with health plans; since most public sector providers are not in managed care networks, their services are considered to be “out of plan” and not reimbursable.
With respect to the above issues, the committee makes the following recommendations:
-
Health plans should provide for or cover comprehensive STD-related services, including screening, diagnosis and treatment, and counseling regarding high-risk behavior for plan members and their sex partners, regardless of the partners' insurance status.
-
Federal, state, and local health agencies should educate employers, Medicaid programs, and other purchasers of health care regarding the broad scope and impact of STDs and the effectiveness of preventive services for STDs.
-
Health plans, including managed care organizations, should develop collaborative agreements with local public health agencies to coordinate STD-related services, including payment for STD-related services provided to plan enrollees by public sector providers, including public STD clinics.
Improving Training and Education of Health Care Professionals
Well-trained primary care clinicians are essential for effective STD diagnosis and treatment. The current system of clinical training for health care professionals, however, is inadequate in preparing clinicians to effectively manage patients with STDs. Inadequate professional training contributes to the widespread tendency of clinicians to oversimplify and underestimate the importance of STDs. Familiarity with population-based health promotion and disease prevention techniques, skills in evidence-based clinical decision making, and patient communication skills are all essential for every clinician. STD training programs should be expanded at the primary care level to improve clinician skills in both public and private settings to effectively prevent, diagnose, and treat patients with STDs. Other factors that influence a clinician's ability to provide comprehensive services, including practice format constraints, also need to be addressed.
With respect to the above issues, the committee makes the following recommendation:
-
The training of primary care providers should be improved by focusing on core clinical competencies, expanding training opportunities, gaining additional federal support, and monitoring and improving STD-related education.19
Improving Clinical Management of STDs
Major components of effective clinical management of STDs include screening, diagnosis and treatment, risk reduction counseling and education, identification and treatment of partners, and access to quality laboratory services for STDs. Screening allows for the detection of infected persons who would otherwise remain undetected, develop complications of STDs, and transmit the infection to their sex partners. Screening for STDs is cost-effective and sometimes cost-saving. Some screening programs, however, such as mandatory premarital testing for syphilis, are not cost-effective and contribute little to STD prevention. Therefore, screening should be appropriately focused and should be based on surveillance data and knowledge of the populations or prevalence of STDs. Screening programs for STDs such as chlamydial infection need to be expanded, because such programs can dramatically reduce rates of STD-related complications. Family planning clinics, prenatal clinics, and other settings where obstetric or gynecological care is available should screen and treat women and their partners for STDs.
|
19 |
This recommendation condenses a detailed recommendation presented in Chapter 6 of the full report. |
With respect to the above issues, the committee makes the following recommendations:
-
All primary care providers, including managed care organizations and other health plans, should implement the recommendations of the U.S. Preventive Services Task Force and the CDC regarding clinical screening and management of STDs.
-
States that still have laws requiring premarital syphilis testing as a condition for marriage licenses should repeal these laws.
National treatment guidelines for STDs help promote appropriate therapy for STDs. However, because there is limited awareness of and compliance with these guidelines, especially among private sector health care professionals, such guidelines should be more widely disseminated. Single-dose therapy for bacterial STDs is important in preventing STDs because it averts the problems of ineffective treatment associated with the failure of infected individuals to return for subsequent treatment or to take multiple doses of drugs.
With respect to the above issues, the committee makes the following recommendations:
-
All clinicians should follow STD treatment guidelines recommended by the CDC and national medical professional organizations.
-
Single-dose therapy for bacterial and other curable STDs should be available and reimbursable in all clinical settings where STD-related clinical care is routinely provided to populations in which treatment compliance or follow-up are problems.
Risk reduction counseling and education of patients during routine clinical encounters and during evaluations for potential STDs is an important component of clinical management. Focused counseling in both specialized and general clinical settings has substantial potential for changing STD-related behaviors, particularly for adolescents and other high-risk groups. Major barriers that hinder clinicians from providing counseling that need to be addressed include inadequate training in counseling, lack of time allocated for counseling, and lack of reimbursement for such services.
With respect to the above issues, the committee makes the following recommendation:
-
All health care professionals should counsel their patients during routine and other appropriate clinical encounters regarding the risk of STDs and methods for preventing high-risk behaviors. Counseling for STDs, including HIV infection, should be reimbursed without copayments or other
-
financial disincentives by Medicaid programs, managed care organizations, and other health plans.
Current methods of partner notification are inefficient and extremely resource-intensive and should be redesigned. The optimal combination of activities that are most effective in reaching partners at risk for STDs will vary depending on the local epidemiology of STDs, available staff and other resources, and the spectrum of local health care professionals providing STD-related care. STD programs need to develop new strategies and techniques for community outreach in partnership with other professionals rather than relying solely on public sector staff.
With respect to the above issues, the committee makes the following recommendation:
-
State and local health departments, with the assistance of the CDC, should redesign current partner notification activities for curable STDs in public health clinics to improve outreach, mobilize public health staff in new ways, and enlist support from community groups or other programs that provide services to high-risk populations.
Partner diagnosis and treatment should be provided as part of standard STD-related care, regardless of the clinical setting. The committee believes that health plans and clinicians have an ethical and public health obligation to ensure that sex partners of infected patients are appropriately identified, screened, and treated, regardless of health insurance status. This belief is based on the concept that health plans have a responsibility to improve the health of the communities from which they draw their revenue and that treating partners is in both the short- and long-term interest of the health plan. By treating partners, health plan members will not return with reinfections and the reservoir of infection in the community will be reduced.
With respect to the above issues, the committee makes the following recommendations:
-
All health plans and clinicians should take responsibility for partner treatment and provide STD diagnosis and treatment to sex partners of plan members or others under their care as part of standard clinical practice. Diagnosis and treatment of partners should be reimbursable by third-party payers, including Medicaid, or by the partner's health plan if he or she is insured.
-
Public sector laboratories should be reimbursed for STD-related laboratory tests performed on persons who have private health insurance coverage.
CONCLUDING STATEMENT
STDs are hidden epidemics of enormous health and economic consequence in the United States. They are hidden because many Americans are reluctant to address sexual health issues in an open way and because of the biologic and social characteristics of these diseases. All Americans have an interest in STD prevention because all communities are impacted by STDs and all individuals directly or indirectly pay for the costs of these diseases. STDs are public health problems that lack easy solutions because they are rooted in human behavior and fundamental societal problems. Indeed, there are many obstacles to effective prevention efforts. The first hurdle will be to confront the reluctance of American society to openly confront issues surrounding sexuality and STDs. Despite the barriers, there are existing individual-and community-based interventions that are effective and can be implemented immediately. That is why a multifaceted approach is necessary at both the individual and community levels.
To successfully prevent STDs, many stakeholders need to redefine their mission, refocus their efforts, modify how they deliver services, and accept new responsibilities. In this process, strong leadership, innovative thinking, partnerships, and adequate resources will be required. The additional investment required to effectively prevent STDs may be considerable, but it is negligible when compared with the likely return on the investment. The process of preventing STDs must be a collaborative one. No one agency, organization, or sector can effectively do it alone; all members of the community must do their part. A successful national initiative to confront and prevent STDs requires widespread public awareness and participation and bold national leadership from the highest levels.
REFERENCES
AAP (American Academy of Pediatrics), Committee on Adolescence. Condom availability for youth. Pediatrics 1995;95:281-5.
AAP, Committee on Child Abuse and Neglect. Guidelines for the evaluation of sexual abuse of children. Pediatrics 1991;87:254-60.
ACS (American Cancer Society). Cancer facts &figures—1996. Atlanta: American Cancer Society, 1996.
AGI (Alan Guttmacher Institute). Sex and America's teenagers. New York: AGI, 1994.
Allen S, Tice J, Van de Perre P, Serufilira A, Hudes E, Nsengumuremyi F, et al. Effect of serotesting with counselling on condom use and seroconversion among HIV discordant couples in Africa. British Med J 1992;304:1605-9.
AMA (American Medical Association), Council on Scientific Affairs . Health care needs of gay men and lesbians in the United States. JAMA 1996;275:1354-9.
AMA, Council on Scientific Affairs. Health care needs of homeless and runaway youths. JAMA 1989;262:1358-61.
Anderson JE, Brackhill R, Mosher WD. Condom use for disease prevention among unmarried U.S. women. Fam Plann Perspect 1996;28:25-8, 39.
Anderson JE, Dahlberg LL. High-risk sexual behavior in the general population. Results from a national survey, 1988-1990. Sex Transm Dis 1992;17:320-5.
Anderson JE, McCormick L, Fichtner R. Factors associated with self-reported STDs: data from a national survey. Sex Transm Dis 1994;21:303-8.
Andrus JK, Fleming DW, Harger DR, Chin MY, Bennet DV, Horan JM, et al. Partner notification: can it control epidemic syphilis [see comments]? Ann Intern Med 1990;112:539-43.
Aral SO. Sexual behavior in sexually transmitted disease research. An overview. Sex Transm Dis 1994;21(March-April Suppl):S59-S64.
Arevalo JA, Washington AE. Cost-effectiveness of prenatal screening and immunization for hepatitis B virus. JAMA 1988;259:365-9.
ARHP, ANPRH (Association of Reproductive Health Professionals and Association of Nurse Practitioners in Reproductive Health). STD counseling practices and needs survey. Silver Spring, MD: Schulman, Ronca, and Bucuvalas, Inc., January 1995.
ASHA (American Social Health Association). International survey reveals lack of knowledge about STDs. STD News 1995;3(Fall):1, 10.
ASHA. Teenagers know more than adults about STDs, but knowledge among both groups is low. STD News 1996;3(Winter):1, 5.
Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection Eval Program Plann 1990;13:9-17.
Barone C, Ickovics JR, Ayers TS, Katz SM, Voyce CK, Weissberg RP. High-risk sexual behavior among young urban students. Fam Plann Perspect 1996:28;69-74.
Berg AO. The primary care physician and sexually transmitted diseases control In: Holmes KK, Mårdh PA, Sparling PF, Wiesner PJ, Cates W Jr, Lemon SM, et al., eds. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:1095-8.
Boekeloo BO, Marx ES, Kral AH, Coughlin SC, Bowman M, Rabin DL. Frequency and thoroughness of STD/HIV risk assessment by physicians in a high-risk metropolitan area. Am J Public Health 1991;81:1645-8.
Bowman MA, Russell NK, Boekeloo BO, Rafi IZ, Rabin DL. The effect of educational preparation on physician performance with a sexually transmitted disease-simulated patient. Arch Intern Med 1992;152:1823-8.
Brandt AM. AIDS in historical perspective: four lessons from the history of sexually transmitted diseases. Am J Public Health 1988;78:367-71.
Brandt AM. No Magic Bullet: A Social History of Venereal Disease in the United States Since 1980. New York: Oxford University Press, Inc., 1985.
Breakey WR, Fischer PJ, Kramer M, Nestadt G, Romanovski AJ, Ross A, et al. Health problems of homeless men and women in Baltimore. JAMA 1989;262:1352-7.
Brinton LA. Epidemiology of cervical cancer—overview. In: Munoz N, Bosch FX, Shah KV, Meheus A, eds. The Epidemiology of Cervical Cancer and Human Papillomavirus. Lyon, France: IARC, 1992:3-23.
Britton TF, DeLisle S, Fine K. STDs and family planning clinics: a regional program for chlamydia control that works. Am J Gynecol Health 1992;6:80-7.
Brown JD, Steele JR. Sex and the mass media. Report prepared for the Henry J. Kaiser Family Foundation and presented at the meeting “Sex and Hollywood: should there be a government role? ” American Enterprise Institute, June 21, 1995, Washington, D.C.
Brunham RC, Holmes KK, Embree JE. Sexually transmitted diseases in pregnancy. In: Holmes KK, Mårdh P-A, Sparling PF, Weisner PJ, Cates W Jr, Lemon SM, et al., eds. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:771-801.
Caetano R, Hines AM. Alcohol, sexual practices, and risk of AIDS among blacks, Hispanics, and whites. J Acquir Immune Defic Syndr 1995;10:554-61.
Cameron DW, Simonsen JN, D'Costa LJ, Ronald AR, Maitha GM, Gakinya MN, et al. Female to male transmission of human immunodeficiency virus type 1: risk factors for seroconversion in men. Lancet 1989; 2:403-7.
Catania JA, Coates TH, Kegeles S, Fullilove MT, Peterson J, Marin B, et al. Condom use in multi-ethnic neighborhoods of San Francisco: the population-based AMEN (AIDS in Multi-Ethnic Neighborhoods) Study. Am J Public Health 1992;82:284-7.
Cates W Jr. Epidemiology and control of sexually transmitted diseases in adolescents In: Schydlower M, Shafer MA, eds. AIDS and Other Sexually Transmitted Diseases. Philadelphia: Hanly & Belfus, Inc., 1990:409-27.
Cates W Jr, Stone KM. Family planning, sexually transmitted diseases, and contraceptive choice: a literature update. Fam Plann Perspect 1992;24:75-84.
Cates W Jr, Stewart FH, Trussell J. Commentary: the quest for women's prophylactic methods—hopes vs science. Am J Public Health 1992;82:1479-82.
CDC (Centers for Disease Control and Prevention). Alternate case-finding methods in a crack-related syphilis epidemic —Philadelphia. MMWR 1991a;40:77-80.
CDC. Hepatitis B virus: a comprehensive strategy for eliminating transmission in the United States through universal childhood vaccination: recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1991b;40(RR-13):1-20.
CDC. HIV infection, syphilis, and tuberculosis screening among migrant farm workers—Florida, 1992. MMWR 1992a;41:723-5.
CDC. HIV prevention in the U.S. correctional system, 1991. MMWR 1992b;41:389-91, 397.
CDC. HIV-risk behaviors of sterilized and nonsterilized women in drug-treatment programs—Philadelphia, 1989–1991. MMWR 1992c;41;149-52.
CDC. Premarital sexual experience among adolescent women—United States, 1970–1988. MMWR 1992d;39;929-32.
CDC. Surgical sterilization among women and use of condoms—Baltimore, 1989–1990. MMWR 1992e;41;568-75.
CDC. 1993 Sexually transmitted diseases treatment guidelines. MMWR 1993a;42(No. RR-14);56-66.
CDC. Update: barrier protection against HIV infection and other sexually transmitted diseases. MMWR 1993b ;42;589-91, 597.
CDC. Hepatitis B vaccination of adolescents—California, Louisiana, and Oregon, 1992–1994. MMWR 1994;43;605-9.
CDC. Ectopic pregnancy—United States, 1990–1992. MMWR 1995a ;44;46-8.
CDC. HIV/AIDS Surveillance Report. Atlanta: Centers for Disease Control and Prevention, 1995b; 7(2).
CDC. Prevention and managed care: opportunities for managed care organizations, purchasers of health care, and public health agencies. MMWR 1995c ;44(No. RR-14);1-12.
CDC. Trends in sexual risk behavior among high school students—United States, 1990, 1991, and 1993. MMWR 1995d;44;124-5, 131-2.
CDC. Update: recommendations to prevent hepatitis B virus transmission —United States. MMWR 1995e ;44;574-5.
CDC. HIV/AIDS education and prevention programs for adults in prisons and jails and juveniles in confinement facilities—United States, 1994. MMWR 1996a ;45;268-71.
CDC. School-based HIV-prevention education—United States, 1994. MMWR 1996b ;45;760-5.
CDC. Ten leading nationally notifiable infectious diseases—United Sates, 1995. MMWR 1996c ;45;883-4.
CDC. Undervaccination for hepatitis B among young men who have sex with men—San Francisco and Berkeley, California, 1992-1993. MMWR 1996d;45;215-7.
CDC, DSTDP (Division of STD Prevention). Sexually transmitted disease surveillance 1994. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1995.
CDC, DSTDP. Sexually transmitted disease surveillance 1995. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, September 1996.
CDC, DSTD/HIVP (Division of STD/HIV Prevention). Annual report 1992. U.S. Department of Health and Human Services, Public Health Service. Atlanta: Centers for Disease Control and Prevention, 1993.
CDC, DSTDP/HIVP. Plan for a national partnership to prevent STD-related infertility Draft internal document, January 10, 1995a.
Celum CL, Hook EW, Bolan GA, Spauding CD, Leone P, Henry KW, et al. Where would clients seek care for STD services under health care reform? Results of a STD client survey from five clinics. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans [abstract no. 101].
Cleary PD, Barry MJ, Mayer KH, Brandt AM, Gostin L, Fineberg HV. Compulsory premarital screening for the human immunodeficiency virus: technical and public health considerations. JAMA 1987;258:1757-62.
Cleary PD, Van Devanter N, Steilen M, Stuart A, Shipton-Levy R, McMullen W, et al. A randomized trial of an education and support program for HIV-infected individuals. AIDS 1995;9:1271-8.
Clemetson DB, Moss GB, Willerford DM, Hensel M, Emonyi W, Holmes KK, et al. Detection of HIV DNA in cervical and vaginal secretions. Prevalence and correlates among women in Nairobi, Kenya. JAMA 1993;269:2860-4.
Collins JL, Small ML, Kann L, Collins Pateman B, Gold RS, Kolbe LJ. School health education. J School Health 1995;65:302-11.
David HP, Morgall JM, Osier M, Rasmussen NK, Jensen B. United States and Denmark: different approaches to health care and family planning. Stud Fam Plann 1990;21:1-19.
DeBuono BA, Zinner SH, Daamen M, McCormack WM. Sexual behavior of college women in 1975, 1986, and 1989. N Engl J Med 1990;322:821-5.
Deschamps MM, Pape JW, Hafner A, Johnson WD. Heterosexual transmission of HIV in Haiti. Ann Intern Med 1996;125:324-30.
de Vincenzi I. A longitudinal study of human immunodeficiency virus transmission by heterosexual partners. European Study Group on Heterosexual Transmission of HIV [see comments]. N Engl J Med 1994;331:341-6.
Dietz WH, Strasburger VC. Children, adolescents and television. Curr Probl Pediatr 1991;21:8-32.
di Mauro D. Executive summary of sexuality research in the United States: an assessment of the social and behavioral sciences. New York: Social Science Research Council, 1995.
Dolan K, Wodak A, Penny R. AIDS behind bars: preventing HIV spread among incarcerated drug injectors AIDS 1995;9:825-32.
Doll DC. Tatooing in prison and HIV infection [letter]. Lancet 1988;331:66-7.
Donelan K, Blendon RJ, Hill CA, Hoffman C, Rowland D, Frankel M, et al. Whatever happened to the health insurance crisis in the United States? Voices from a national survey. JAMA 1996;276:1346-50.
Donovan P. Taking family planning services to hard-to-reach populations. Fam Plann Perspect 1996;28:120-6.
Ebrahim SH, Peterman TA, Zaidi AA, Kamb ML. Mortality related to sexually transmitted diseases in women, U.S., 1973–1992. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995, New Orleans [abstract no. 343].
EDK Associates. Women & sexually transmitted diseases: The dangers of denial. New York: EDK Associates, 1994.
EDK Associates. The ABCs of STDs. New York: EDK Associates, 1995.
Edlin BR, Irwin KL, Faruque S, McCoy CB, Word C, Serrano Y, et al. Intersecting epidemics—crack cocaine use and HIV infection among inner-city young adults The Multicenter Crack Cocaine and HIV Infection Study Team. N Engl J Med 1994;31:1422-7.
Engelgau MM, Woernle CH, Rolfs RT, Greenspan JR, O'Cain M, Gorsky, RD. Control of epidemic early syphilis: the results of an intervention campaign using social networks. Sex Transm Dis 1995;22:203-9.
Fanburg JT, Kaplan DW, Naylor KE. Student opinions of condom distribution at a Denver, Colorado, high school. J Sch Health 1995;65:181-5.
Felman Y. Repeal of mandated premarital tests for syphilis: a survey of state health officers. Am J Public Health 1981;71:155-9.
Finelli L, Budd J, Spitalny KC. Early syphilis. Relationship to sex, drugs, and changes in high-risk behavior from 1987-1990. Sex Transm Dis 1993;20:89-95.
Fish AN, Fairweather DV, Oriel JD, Ridgeway GL. Chlamydia trachomatis infection in a gynecology clinic population: identification of high-risk groups and the value of contact tracing Eur J Obstet Gynecol Reprod Biol 1989;31:67-74.
Fisher RS. Medicaid managed care: the next generation? Acad Med 1994;69:317-22.
Flay BR. Mass media and smoking cessation: a critical review. Am J Public Health 1987;77:153-60.
Flora JAM, Miabach EW, Holtgrave D. Communication campaigns for HIV prevention: using mass media in the next decade. In: Institute of Medicine. Assessing the Social and Behavioral Science Base for HIV/AIDS Prevention and Intervention. Background Papers. Washington, D.C.: National Academy Press, 1995:129-54.
Freeman HE, Corey CR. Insurance status and access to health services among poor persons Health Serv Res 1993;28:531-41.
Freeman HE, Blendon RJ, Aiken LH, Sudman S, Mullix CF, Covey CR. Americans report on their access to health care. Health Aff Millwood 1987;6:6-18.
GHAA (Group Health Association of America, currently American Association of Health Plans). 1995 National Directory of HMOs. Washington, D.C.: Group Health Association of America, 1995.
Glaser JB, Greifinger RB. Correctional health care: a public health opportunity. Ann Intern Med 1993;118:139-45.
Greenberg MSZ, Singh T, Htoo M, Schultz S. The association between congenital syphilis and cocaine/crack use in New York City: a case-control study. Am J Public Health 1991;81:1316-8.
Grosskurth H, Mosha F, Todd J, Mwijarubi E, Klokke A, Senkoro K, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomized controlled trial [see comments]. Lancet 1995a ;346:530-6.
Grosskurth H, Mosha F, Todd J, Senkoro K, Newell J, Klokke A, et al. A community trial of the impact of improved STD treatment on the HIV epidemic in rural Tanzania: 2 baseline survey results. AIDS 1995b;9:927-34.
Guidry HM. Childhood sexual abuse: role of the family physician. Am Fam Physician 1995;51:407-14.
Gunn RA, Montes JM, Toomey KE, Rolfs RT, Greenspan JK, Spitters CE, et al. Syphilis in San Diego County 1983–1992: crack cocaine, prostitution, and the limitations of partner notification. Sex Transm Dis 1995;22:60-6.
Gutman LT, St. Claire K, Herman Giddens ME. Prevalence of sexual abuse in children with genital warts [letter; comment]. Pediatr Infect Dis J 1991;10:342-3.
Guttmacher S, Lieberman L, Ward D, Radosh A, Rafferty Y, Freudenberg N. Parents' attitudes and beliefs about HIV/AIDS prevention with condom availability in New York City public high schools. J Sch Health 1995;65:101-6.
Gys PD, Fransen K, Diallo MO, Ettiegne-Traore V, Maurice C, Hoyi-Adansou YM, et al. The association between cervico-vaginal HIV-1 shedding and STD, immunosuppression, and serum
HIV-1 load in female sex workers in Abidjan, Cote D'Ivoire. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC 332].
Hammett TM, Widom R, Epstein J, Gross M, Sifre S, Enos T. 1994 Update: HIV/AIDS and STDs in correctional facilities. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, National Institute of Justice/U.S. Department of Health and Human Services, Public Health Service, CDC, December 1995.
Handsfield HH, Jasman LL, Roberts PL, Hanson VW, Kothenbeutel RL, Stamm WE. Criteria for selective screening for Chlamydia trachomatis infection in women attending family planning clinics. JAMA 1986;255:1730-4.
Harlap S, Kost K, Forrest JD. Preventing Pregnancy, Protecting Health: A New Look at Birth Control Choices in the United States. New York: Alan Guttmacher Institute, 1991.
Harris L and Associates. Attitudes about television, sex and contraception. A survey of a cross-section of adult Americans. Conducted for Planned Parenthood Federation of America. February 1987.
Haskell RJ. A cost-benefit analysis of California's mandatory premarital screening program for syphilis. West J Med 1984;141:538-41.
Hauth JC, Goldenberg RL, Andrews WW, Dubard MD, Copper RL. Reduced incidence of preterm delivery with metronidazole and erythromycin in women with bacterial vaginosis. N Engl J Med 1995;333:1732-6.
Hayes RJ, Schulz KF, Plummer FA. The cofactor effect of genital ulcers on the per-exposure risk of HIV transmission in sub-Saharan Africa. J Trop Med Hyg 1995;98:1-8.
Hessol NA, Priddy FH, Bolan G, Baumrind N, Vittinghoff E, Reingold AL, et al. Management of pelvic inflammatory disease by primary care physicians: a comparison with Centers for Disease Control and Prevention Guidelines Sex Transm Dis 1996;23:157-63.
Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, et al. Association between bacterial vaginosis and preterm delivery of a low birth-weight infant. N Engl J Med 1995;333:1737-42.
Hillis SD, Nakashima A, Amsterdam L, Pfister J, Vaughn M, Addiss D, et al. The impact of a comprehensive chlamydia prevention program in Wisconsin Fam Plann Perspect 1995;27:108-11.
Hingson RW, Strunin L, Berlin BM, Hereen T. Beliefs about AIDS, use of alcohol and drugs, and unprotected sex among Massachusetts adolescents. Am J of Public Health 1990;80:295-9.
Hofferth SL, Kahn JR, Baldwin W. Premarital sexual activity among U.S. teenage women over the past three decades. Fam Plann Perspect 1987;19:46-53.
Hoffman I, Maida M, Royce R, Costello-Daly C, Kazembe P, Vernazza P, et al. Effects of urethritis therapy on the concentration of HIV-1 in seminal plasma. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. mo.C.903].
Holtgrave DR, Qualls NL, Curran JW, Valdiserri RO, Guinan ME, Parra WC. An overview of the effectiveness and efficiency of HIV prevention programs. Public Health Rep 1995;110:134-46.
IOM (Institute of Medicine). New Vaccine Development: Establishing Priorities; Vol. I, Diseases of importance in the United States. Washington, D.C.: National Academy Press, 1985.
IOM. Understanding the Determinants of HIV Risk Behavior. In: Auerbach JD, Wypijewska C, Brodie HKH, eds. AIDS and Behavior. Washington, D.C.: National Academy Press, 1994:78-123.
IOM. Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. Brown SS, Eisenberg L, eds. Washington, D.C.: National Academy Press, 1995.
IOM. Contraceptive Research and Development: Looking to the Future. Harrison PF, Rosenfield A, eds. Washington, D.C.: National Academy Press, 1996a.
IOM. Primary Care: America's Health in a New Era. Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Washington, D.C.: National Academy Press, 1996b.
John G, Nduati R, Mbori-Ngacha D, Overbaugh J, Welch M, Richardson B et al. Cervico-vaginal HIV-1 DNA in pregnancy. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC 331].
Johnstone H, Tornabene M, Marcinak J. Incidence of sexually transmitted diseases and Pap smear results in female homeless clients from the Chicago Health Outreach Project Health Care Women Int 1993;14:293-9.
Jones JL, Rion P, Hollis S, Longshore S, Leverette WB, Ziff L. HIV-related characteristics of migrant workers in rural South Carolina South Med J 1991;84:1088-90.
Jossens MO, Schachter J, Sweet RL. Risk factors associated with pelvic inflammatory disease of differing microbial etiologies. Obstet Gynecol 1994;83:989-97.
Judson FN. Gonorrhea. Med Clin North Am 1990;74:1353-67.
The Kaiser Commission on the Future of Medicaid. Medicaid and managed care: lessons from the literature. Menlo Park, CA: The Henry J. Kaiser Family Foundation, 1995.
Kalichman SC, Carey MP, Johnson BT. Prevention of sexually transmitted HIV infection: a metaanalytic review of the behavioral outcome literature. Ann Behav Change 1996;18:6-15.
Kalichman SC, Kelly JA, Johnson JR, Bulto M. Factors associated with risk for HIV infection among chronic mentally ill adults. Am J Psychiatry 1994;151:221-7.
Kamb ML, Douglas JM, Rhodes F, Bolan G, Zenilman J, Iatesta M, et al. A multi-center, randomized controlled trial evaluating HIV prevention counseling (Project RESPECT): preliminary results. Eleventh International Conference on AIDS, July 7-12, 1996 Vancouver [abstract no. Th.C.4380].
Keim J, Woodard MP, Anderson MK. Screening for Chlamydia trachomatis in college women on routine gynecological exams. J Am Coll Health 1992;41:17-9, 22-3.
Kelly JA. Sexually transmitted disease prevention approaches that work. Interventions to reduce risk behavior among individuals, groups, and communities Sex Transm Dis 1994;21[No.2 supplement]: S73-S75.
Kelly JA, St. Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Grasfield TL, et al. HIV risk behaviors reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health 1991;81:168-71.
Kelly JA, St. Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. Am J Public Health 1992; 82:1483-9.
Kennedy MB, Scarlett MI, Duerr AC, Chu SY. Assessing HIV risk among women who have sex with women: scientific and communication issues. J Am Med Wom Assoc 1995;50:103-7.
Kirby D. Research and evaluation. In: Samuels SE, Smith MD, eds. Condoms in the Schools. Menlo Park, CA: Henry J. Kaiser Family Foundation, 1993:89-109.
Kirby D. Sexuality and HIV education programs in schools. In: Garrison J, Smith MD, Besharov DJ, eds. Sexuality and American Social Policy: A Seminar Series. Sex Education in the Schools. Menlo Park, CA: Henry J. Kaiser Family Foundation, 1994;1-41.
Kirby DM, Brown NL. Condom availability programs in U.S. schools. Fam Plann Perspect 1996;28:196-202.
Kirby D, Short L, Collins J, Rugg D, Kolbe L, Howard M, et al. School-based programs to reduce sexual risk behaviors: a review of effectiveness. Public Health Rep 1994;109:339-60.
Kirby D, Waszak C, Ziegler J. Six school-based clinics: their reproductive health services and impact on sexual behavior. Fam Plann Perspect 1991;23:6-16.
Klovdahl AS, Potterat JJ, Woodhouse DE, Muth JB, Muth SQ, Darrow WW. Social networks and infectious disease: the Colorado Springs study Soc Sci Med 1994;38:79-88.
Kollar LM, Rosenthal SL, Biro FM. Hepatitis B vaccine series compliance in adolescents. Pediatr Infect Dis J 1994;13:1006-8.
Koopman C, Rosario M, Rotheram-Borus MJ. Alcohol and drug use and sexual behaviors placing runaways at risk for HIV infection. Addict Behav 1994;19:95-103.
Kost K, Forrest JD. American women's sexual behavior and exposure to risk of sexually transmitted diseases Fam Plann Perspect 1992;24:244-54.
Kreiss JK, Willerford DM, Hensel M, Emonyi W, Plummer F, Nkinya-Achola J, et al. Association between cervical inflammation and cervical shedding of human immunodeficiency virus DNA. J Infect Dis 1994;170:1597-601.
Laga M, Alary M, Nzila N, Manoka AT, Tuliza M, Behets F, et al. Condom promotion, sexually transmitted diseases treatment, and declining incidence of HIV-1 infection in female Zairian sex workers. Lancet 1994;344:246-8.
Laga M, Manoka A, Kivuvu M, Malele B, Tuliza M, Nzila N, et al. Nonulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS 1993;7:95-102.
Landry DJ, Forrest JD. Public health departments providing STD services. Fam Plann Perspect 1996;28, in press.
Laumann EO, Gagnon JH, Michael RT, Michaels S. The Social Organization of Sexuality: Sexual Practices in the United States. Chicago: University of Chicago Press, 1994.
Laumann EO, Michael RT, Gagnon JH. A political history of the National Sex Survey of Adults. Fam Plann Perspect 1994;26:34-8.
Lear D. Sexual communication in the age of AIDS; the construction of risk and trust among young adults. Soc Sci Med 1995; 41:1311-23.
Leavy Small M, Smith Majer L, Allensworth DD, Farquhar BD, Kann L, Pateman BC. School health services. J Sch Health 1995;65:319-26.
Lebow MA. Contraceptive advertising in the United States. Women's Health Issues 1994;4:196-208.
Lewis CE, Freeman HE. The sexual history-taking and counseling practices of primary care physicians. West J Med 1987;147:165-7.
Lewis CE, Freeman HE, Corey CR. AIDS-related competence of California's primary care physicians. Am J Public Health 1987;77:795-9.
Lichter SR, Lichter LS, Rothman S. Prime time. How TV Portrays American Culture. Washington, D.C.: Regnery Publishing, Inc., 1994.
Lowry DT, Schidler JA. Prime time TV portrayals of sex, “safe sex” and AIDS: a longitudinal analysis. Journalism Q 1993;70:628-37.
Lowry R, Holtzman D, Truman BI, Kann L, Collins JL, Kolbe LJ. Substance use and HIV-related sexual behaviors among US high school students: are they related? Am J Public Health 1994;84:1116-20.
MacKay HT, Toomey KE, Schmid GP. Survey of clinical training in STD and HIV/AIDS in the United States Proceedings of the IDSA Annual Meeting, September 16-18, 1995, San Francisco [abstract no. 281].
Mahon N. New York inmates' HIV risk behaviors: the implications for prevention policy and programs Am J Public Health 1996;86:1211-5.
Main DM, Main EK. Preterm birth. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 2nd ed. New York: Churchill Livingstone, Inc., 1991:829-80.
Marchbanks PA, Annegers, JF, Coulam CB, Strathy JH, Kurland LT. Risk factors for ectopic pregnancy. A population-based study. JAMA 1988;259:1823-7.
Marx R, Aral SO, Rolfs RT, Sterk CE, Kahn JG. Crack, sex, and STD. Sex Transm Dis 1991;18:92-101.
Mays VM, Cochran SD. Issues in the perception of AIDS risk and risk reduction activities by black and Hispanic/Latina women. Am Psychol 1988;43:949-57.
Merrill JM, Laux LF, Thornby JI. Why doctors have difficulty with sex histories. Southern Med J 1990;83:613-17.
Miller BC, Monson BH, Norton MC. The effects of forced sexual intercourse on white female adolescents Child Abuse Negl 1995;19:1289-301.
Moss GB, Overbaugh J, Welch M, Reilly M, Bwayo J, Plummer FA, et al. Human immunodeficiency virus DNA in urethral secretions in men: association with gonococcal urethritis and CD4 depletion. J Infect Dis 1995;172:1469-74.
Mostad S, Welch M, Chohan B, Reilly M, Overbaugh J, Mandaliya K, et al. Cervical and vaginal HIV-1 DNA shedding in female STD clinic attenders Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC 333].
NARAL (National Abortion Rights Action League) Foundation. Sexuality education in America: a state-by-state review, 1995. [Rev. ed.] Washington, D.C., September 1995.
NCHS (National Center for Health Statistics). Advanced report of final mortality statistics, 1992. Hyattsville, MD: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, 1994. Monthly vital statistics report 43;(6 Suppl).
NCQA (National Committee for Quality Assurance), Committee on Performance Measurement. HEDIS 3.0 Draft for public comment. Washington, D.C.: National Committee for Quality Assurance, July 1996.
Nelson KE, Celentano DD, Eiumtrakol S, Hoover DR, Beyrer C, Suprasert S, et al. Changes in sexual behavior and a decline in HIV infection among young men in Thailand. New Engl J Med 1996;335:297-303.
NIH (National Institutes of Health). Consensus Development Conference statement on cervical cancer. Bethesda, MD: National Institutes of Health, April 1-3, 1996a.
NIH. The Jordan report: accelerated development of vaccines 1996. Bethesda, MD: National Institutes of Health, National Institute of Allergy and Infectious Diseases, Division of Microbiology and Infectious Diseases 1996b.
Norris AE, Ford K. Associations between condom experiences and beliefs, intentions, and use in a sample of urban, low-income, African-American and Hispanic youth. AIDS Educ Prev 1994;6:27-39.
Nyange P, Martin H, Mandaliya K, Jackson D, Ndinya-Achola JO, Ngugi E, et al. Cofactors for heterosexual transmission of HIV to prostitutes in Mombasa Kenya. Ninth International Conference on AIDS and STD in Africa, December 10-14, 1994; Kampala, Uganda.
Oakley A, Fullerton D, Holland J. Behavioural interventions for HIV/AID prevention. AIDS 1995;9:479-86.
Oakley A, Fullerton D, Holland J, Arnold S, France-Dawson M, Kelley P, et al. Sexual health education interventions for young people: a methodological review. Br Med J 1995;310:158-62.
O'Leary A, Jemmott LS. Future directions. In: O'Leary A, Jemmott, LS, eds. Women at Risk: Issues in the Primary Prevention of AIDS. New York: Plenum Press, 1995:257-9.
O'Reilly KR, Higgins DL. AIDS Community Demonstration Projects for HIV prevention among hard-to-reach groups. Public Health Rep 1991; 106:714-20.
O'Reilly KR, Piot P. International perspectives on individual and community approaches to the prevention of sexually transmitted disease and human immunodeficiency virus infection. J Infect Dis 1996;174(Suppl 2):S214-S222.
Over M, Piot P. HIV infection and sexually transmitted disease. In: Jamison DT, Mosley WH, Measham AR, Bobadilla JL, eds. Disease Control Priorities in Developing Countries. New York: Oxford University Press, 1993:455-527.
Oxman GL, Doyle L. A comparison of the case-finding effectiveness and average costs of screening and partner notification. Sex Transm Dis 1996;23:51-7.
Petersen LR, White CR. Premarital screening for antibodies to human immunodeficiency virus type 1 in the United States. The Premarital Screening Study Group Am J Public Health 1990;80:1087-90.
Peterson LS. Contraceptive use in the United States: 1982–90. Advance Data, No. 260. Hyattsville, MD: National Center for Health Statistics, February 14, 1995.
Piot P, Islam MQ. Sexually transmitted diseases in the 1990s. Global epidemiology and challenges for control. Sex Transm Dis 1994;21(2 Suppl):S7-S13.
Pleck JH, Sonenstein FL, Ku L. Changes in adolescent males' use of and attitudes toward condoms, 1988–1991. Fam Plann Perspect 1993;25:106-10, 17.
Plichta SB, Abraham C. Violence and gynecological health in women < 50 years old. Am J Obstet Gynecol 1996;174:903-7.
Plummer FA, Ngugi EN. Prostitutes and their clients in the epidemiology and control of sexually transmitted diseases. In: Holmes KK, March P-A, Sparling, PF, Wiesner PJ, Cates W Jr, Lemon SM, et al., eds. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:71-6.
Plummer FA, Simonsen JN, Cameron DW, Ndinya-Achola JO, Kreiss JK, Gakinya MN, et al. Co-factors in male-female transmission of human immunodeficiency virus type 1. J Infect Dis 1991;163:233-9.
Poorman S, Albrecht L. Human sexuality and the nursing process. Norwalk, CT: Appleton & Lange Publishing Co., 1987.
Quinn TC, Cates W Jr. Epidemiology of sexually transmitted diseases in the 1990s. Adv Host Defen Mech 1992; 8:1-37.
Ramos R, Shain, RN, Johnson L. “Men I mess with don't have anything to do with AIDS”: Using ethno-theory to understand sexual risk perception. Sociol Q 1995;36:483-504.
Randolph AG, Washington AE. Screening for Chlamydia trachomatis in adolescent males: A cost-based decision analysis. Am J Public Health 1990;80:545-50.
Risen CB. A guide to taking a sexual history. Clinical Sexuality 1995;18:39-53.
Robinson NJ, Mulder DW, Auvert B, Hayes RJ. Modeling the impact of alternative HIV intervention strategies in rural Uganda. AIDS 1995; 9:1263-70.
Rolfs RT, Galaid EI, Zaidi AA. Pelvic inflammatory disease: trends in hospitalizations and office visits, 1979 through 1988. Am J Obstet Gynecol 1992;166:983-90.
The Roper Organization. AIDS: public attitudes and education needs. 1991. New York.
Roper WL, Peterson HB, Curran JW. Commentary: condoms and HIV/STD prevention—clarifying the message. Am J Public Health 1993;83:501-3.
Rosenberg MJ, Gollub EL. Commentary: methods women can use that may prevent sexually transmitted diseases, including HIV. Am J Public Health 1992;82:1473-8.
Rosenblum L, Darrow W, Witte J, Cohen J, French J, Gill PS, et al. Sexual practices in the transmission of hepatitis B virus and prevalence of hepatitis delta virus infection in female prostitutes in the United States. JAMA 1992;267:2477-81.
Roter DL, Knowles N, Somerfield M, Baldwin J. Routine communication in sexually transmitted disease clinics: an observational study. Am J Public Health 1990;80:605-6.
Rothenberg R, Narramore J. The relevance of social network concepts to sexually-transmitted disease-control. Sex Transm Dis 1996;23:24-9.
Rothenberg RB, Potterat JJ. Strategies for management of sex partners. In: Holmes KK, Mårdh P-A, Sparling PF, Wiesner PJ, Cates W Jr, Lemon SM, et al., eds. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:1081-6.
Rothenberg RB, Potterat JJ. Partner notification for STD/HIV. In: Holmes KK, Sparling PF, Mårdh P-A, Lemon SM, Stamm WE, Piot P, et al., eds. Sexually Transmitted Diseases. 3rd ed. 1997. New York: McGraw-Hill, Inc., in press.
Santelli JS, Kouzis AC, Hoover DR, Polacsek M, Burwell LG, Celentano DD. Stage of behavior change for condom use: the influence of partner type, relationship and pregnancy factors. Fam Plann Perspect 1996;28:101-7.
Schiffman MH. Recent progress in defining the epidemiology of human papillomavirus infection and cervical neoplasia. J Natl Cancer Inst 1992;84:394-8.
Scholes D, Stergachis A, Heidrich FE, Andrilla H, Holmes KK, Stamm WE. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. New Engl J Med 1996; 334:1362-6.
Schulz KF, Murphy FK, Patamasucon P, Meheus AZ. Congenital syphilis. In: Holmes KK, Mårdh PA, Sparling PF, Weisner PJ, Cates W Jr, Lemon SM, et al., eds. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:821-42.
Shafer MA. Sexual behavior and sexually transmitted diseases among male adolescents in detention. Sex Transm Dis 1994;21:181-2.
Shafer MA, Hilton JF, Ekstrand M, Keogh J, Gee L, DiGiorgio-Haag L, et al. Relationship between drug use and sexual behaviors and the occurrence of sexually transmitted diseases among high-risk male youth. Sex Transm Dis 1993;20:307-13.
Shain R, Piper J, Newton E, Perdue S, Ramos R, Dimmitt J, et al. Preventing sexually transmitted disease among minority women: results of a controlled randomized trial at 12 months' followup. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no.Mo.D.1773-Mo.D.1779].
Sherman DJ. The neglected health care needs of street youth. Public Health Rep 1992;107:433-40.
Siegel K, Mesango FP, Chen J, Christ G. Factors distinguishing homosexual males practicing risky and safer sex. Soc Sci Med 1989;28:561-9.
Smith L, Lanthrop L. AIDS and human sexuality. Can J Public Health 1993;84(1 Suppl):S14-S18.
Sokolow JA. Eros and modernization: Sylvester Graham, health reform, and the origins of Victorian sexuality in America. Cranbury, NJ: Associated University Presses, Inc., 1983.
Stall R, McKusick L, Wiley J, Coates TJ, Ostro DG. Alcohol and drug use during sexual activities and compliance with safe sex guidelines for AIDS. Health Educ Q 1986;13:359-71.
Stamm WE, Holmes KK. Chlamydia trachomatis infections in the adult. In: Holmes KK, Mårdh PA, Sparling PF, Weisner PJ, Cates W Jr, Lemon SM, et al., eds. Sexually Transmitted Diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:181-93.
Stamm WE, Kaetz SK, Holmes KK. Clinical training in venereology in the United States and Canada. JAMA 1982;248:2020-4.
Stein ZA. Editorial: the double bind in science policy and the protection of women from HIV infection. Am J Public Health 1992;82:1471-2.
Stein ZA. Editorial: family planning, sexually transmitted diseases, and prevention of AIDS—divided we fail? Am J Public Health 1996;86:783-4.
Strasburger VC. Adolescent sexuality and the media. Pediatr Clin North Am 1989;36:747-73.
Strasburger VC. Television and adolescents: Sex, drugs, and rock 'n' roll. Adoles Med: State of the Art Rev 1990;1:161-94.
Stryker J, Samuels SE, Smith M. Condom availability in schools: the need for improved program evaluations Am J Public Health 1994;84:1901-6.
Suplee C. Apprehensive NIH defers sex survey; political concerns cited for decision. Washington Post, September 25, 1991, A1.
Tanfer K, Grady WR, Klepinger DH, Billy JOG. Condom use among US men, 1991. Fam Plann Perspect 1993;25:61-6.
Tawil O, Verster A, O'Reilly KR. Enabling approaches for HIV/AIDS prevention: can we modify the environment and minimize the risk? AIDS 1995;9:1299-1306.
Thomas JC, Tucker MJ. The development and use of the concept of a sexually transmitted disease core. J Infect Dis 1996;174(Suppl 2):S134-43.
Thorpe EM, Stamm WE, Hook EW III, Gall SA, Jones RB, Henry K, et al. Chlamydial cervicitis and urethritis: single-dose treatment compared with doxycycline for seven days in community-based practises. Genitourin Med 1996;72:93-7.
Trachtenberg AI, Washington AE, Halldorson A. A cost-based decision analysis for chlamydia screening in California family planning clinics. Obstet Gynecol 1988;71:101-8.
Trotter RT 2d, Rothenberg RB, Coyle S. Drug abuse and HIV prevention research: expanding paradigms and network contributions to risk reduction. Connections 1995;18:29-45.
U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2nd ed. Washington, D.C.: U.S. Department of Health and Human Services, 1996.
Washington AE, Katz P. Cost of and payment source for pelvic inflammatory disease. Trends and projections, 1983 through 2000 [see comments]. JAMA 1991;266:2565-9.
Washington AE, Cates W Jr, Wasserheit JN. Preventing pelvic inflammatory disease [see comments]. JAMA 1991;266:2574-80.
Washington AE, Johnson RE, Sanders LL. Chlamydia trachomatis infections in the United States: what are they costing us? JAMA 1987;257:2070-2.
Wasserfallen F, Stutz ST, Summermater D, Hausermann M, Duboi-Arber F. Six years of promotion of condom use in the framework of the National Stop AIDS Campaign: experiences and results in Switzerland. Ninth International Conference on AIDS, June 6-11, 1993, Berlin [abstract no. WS-D27-3].
Wasserheit JN. Effect of changes in human ecology and behavior on patterns of sexually transmitted diseases, including human immunodeficiency virus infection Proc Natl Acad Sci 1994;91:2430-5.
Wasserheit JN, Holmes KK. Reproductive tract infections: challenges for international health policy, programs, and research. In: Germain A, Holmes KK, Piot P, Wasserheit JN, eds. Reproductive Tract Infections: Global Impact and Priorities for Women 's Health. New York: Plenum Press, 1992.
Webber MP, Lambert G, Bateman DA, Hauser WA. Maternal risk factors for congenital syphilis: a case-control study Am J Epidemiol 1993;137:415-22.
Weller SC. A meta-analysis of condom effectiveness in reducing sexually transmitted HIV. Soc Sci Med 1993;36:1635-44.
WHO (World Health Organization, Global Programme on AIDS). Global prevalence and incidence of selected curable sexually transmitted diseases: overview and estimates. Geneva: WHO, 1996.
Wolk LI, Rosenbaum R. The benefits of school-based condom availability—cross-sectional analysis of a comprehensive high school-based program J Adolesc Health 1995;17:184-8.
World Bank. World development report, 1993: investing in health. New York: Oxford University Press, 1993.
WREI (Women's Research and Education Institute). Women's health care costs and experiences. Washington, D.C.: Women's Research and Education Institute, 1994.
Wulfert E, Wan CK. Condom use: a self-efficacy model. Health Psychol 1993;12:346-53.
Zenilman JM. Gonococcal susceptibility to antimicrobials in Baltimore, 1988–1994. What was the impact of ciprofloxcin as first-line therapy for gonorrhea? Sex Transm Dis 1996;23:213-8.