What Causes Legionnaires’ Disease?
Legionella bacteria reside in many natural environments including rivers, lakes, and soils. These bacteria are also found in a variety of engineered systems that support biofilm growth, including drinking water supplies,  cooling towers, hot tubs, fountains, and building plumbing systems and their outlets like faucets and showerheads. These water systems are often characterized by warm temperatures, stagnant water, and a lack of chemical disinfectants—conditions that promote the growth of biofilms and their associated protozoa, which are the hosts for Legionella bacteria. People are exposed to Legionella primarily through inhalation of contaminated aerosols into the respiratory system from these contaminated water systems. Those at higher risk for developing Legionnaires’ disease include the elderly, men, smokers, and the immunocomprised.
cooling towers, hot tubs, fountains, and building plumbing systems and their outlets like faucets and showerheads. These water systems are often characterized by warm temperatures, stagnant water, and a lack of chemical disinfectants—conditions that promote the growth of biofilms and their associated protozoa, which are the hosts for Legionella bacteria. People are exposed to Legionella primarily through inhalation of contaminated aerosols into the respiratory system from these contaminated water systems. Those at higher risk for developing Legionnaires’ disease include the elderly, men, smokers, and the immunocomprised.
Incidence of Legionnaires' Disease Has Increased
Although the Safe Drinking Water Act has been effective in reducing U.S. disease rates of enteric waterborne organisms, it has had little impact on managing Legionella in water systems and buildings. In fact, the incidence of Legionnaires’ disease has increased more than five-fold from 2000 to 2017 (see Figure 1). Facilities managers can play a major role in preventing the growth of Legionella in engineered environments like building water systems.
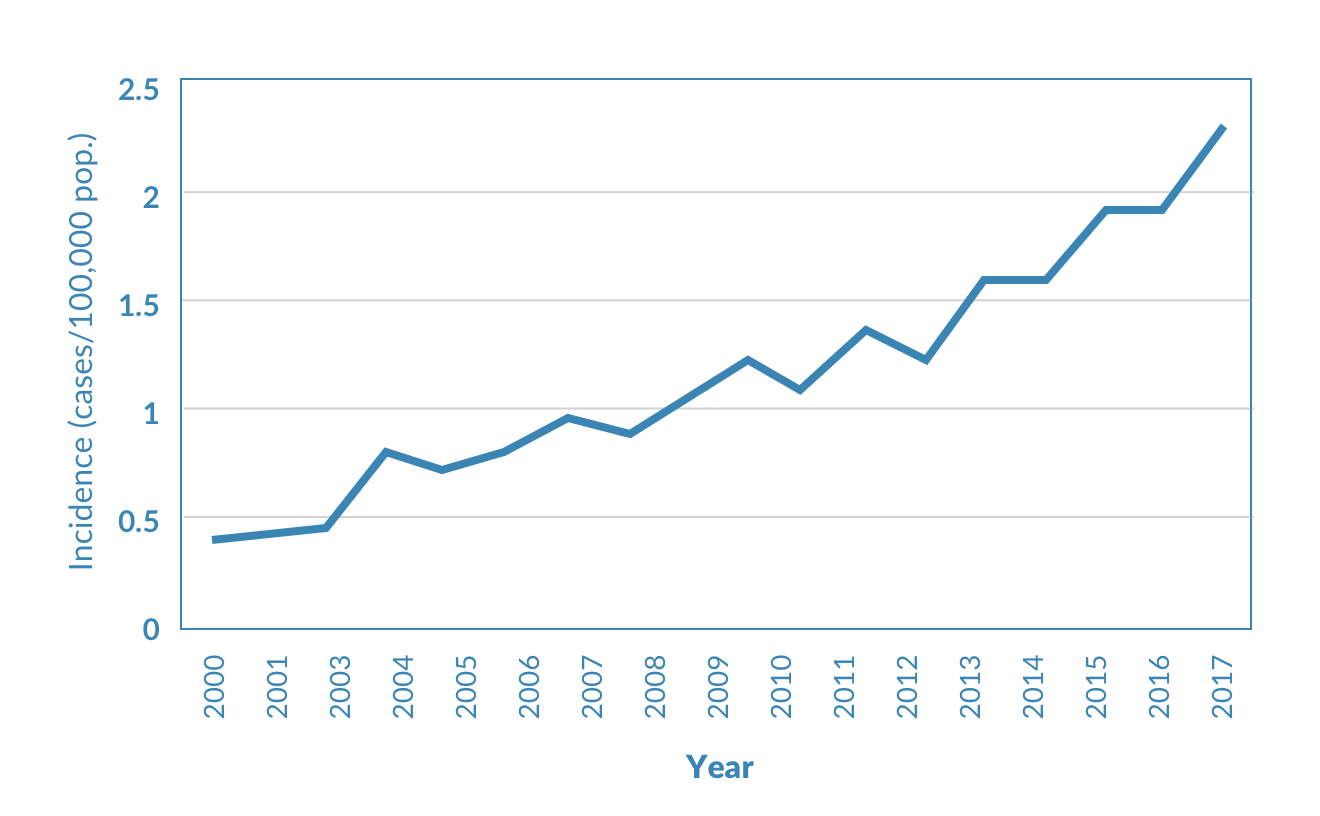
FIGURE 1
The reported incidence of Legionnaires’ disease in the United States has increased more than five-fold from 2000 to 2017. Many factors contribute to this increase: more people are at risk because of the aging population, increased use of immunosuppressant drugs, and higher prevalence of comorbid conditions such as diabetes and pulmonary disease. There is also a growing dependence on heating, ventilation, and cooling systems, as well as increasingly complex indoor plumbing systems in large buildings. In addition, efforts to conserve water within buildings are likely to result in an increased risk of Legionella growth due to water stagnation, temperature changes, and loss of disinfectant residual. Higher water temperatures as a result of climate change may also play a role.
Source: Adapted from Shaw et al. (2018) with 2016 and 2017 data from the National Notifiable Diseases Surveillance System.