Challenges Facing the Cancer Careforce
Speakers discussed the following challenges that the cancer careforce may face:
Growing Demand for Cancer Care
Due to population growth and the aging of the U.S. population, more people are being diagnosed with cancer, even as the age-adjusted mortality rate from cancer is declining.2 The number of patients diagnosed with cancer each year in the United States is predicted to rise from 1.8 million in 2019 to 2.3 million in 2035.3 The number of cancer survivors is also expected to rise, from 15.5 million in 2016 to 20.3 million in 2026.4
— Suanna Bruinooge, American Society of Clinical Oncology (ASCO)
Distribution of the Workforce
Several speakers highlighted the uneven nationwide distribution of oncology clinicians and cancer care facilities.
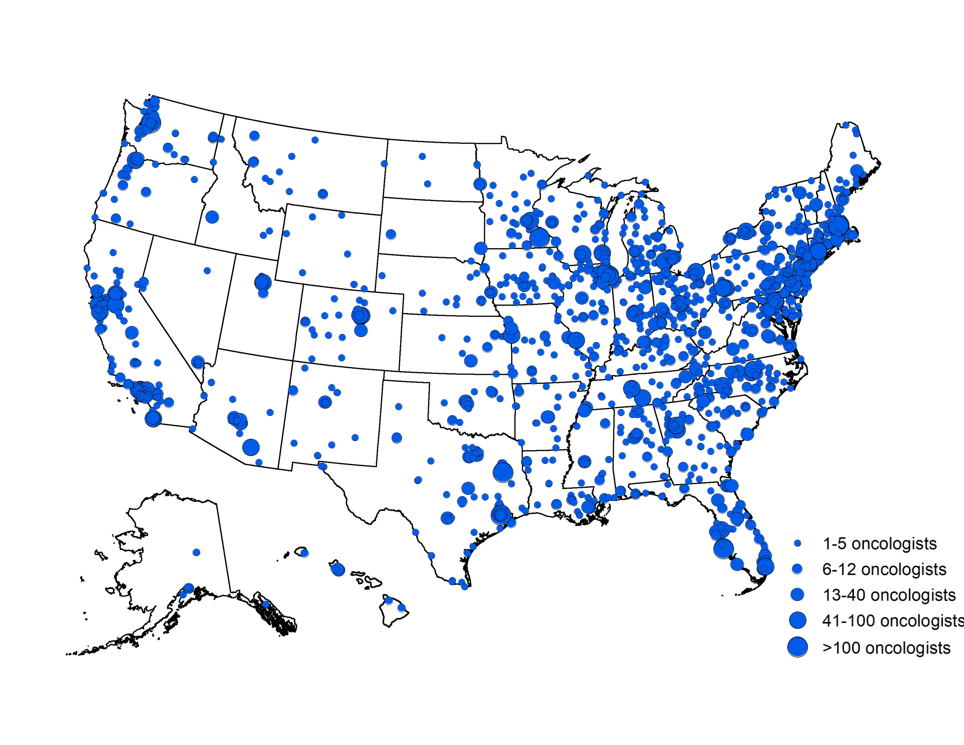
SOURCES: Bruinooge presentation, February 11, 2019; reprinted by permission from ASCO.
Complexity of Cancer Care
Speakers described a number of factors that contribute to increasing complexity in cancer care, such as:
- Advances in cancer research, screening and diagnostic practices, and cancer treatment
- New payment models with an emphasis on clinician accountability for the value of cancer care and interprofessional, collaborative practice
- Widespread adoption of technologies in clinical practice with variable levels of usability, efficiency, and clinician burden
- Responsibilities facing patients and family caregivers related to the outpatient nature of cancer care
Clinician Burnout
Several speakers discussed the relationship between clinician burnout and the use of electronic health records, particularly the time required for documentation and identifying the relevant information for patient care.
— Mia Levy, Rush University Cancer Center
Reliance on Family Caregiving
Speakers discussed the important role of family caregivers as members of the oncology careforce. Family caregivers often face a number of stressors and challenges, including a lack of training, fragmentation of care, not feeling valued and included in the care team, as well as economic and health burdens.
— Courtney Harold Van Houtven, Duke University
— Lawrence Shulman, Abramson Cancer Center of the University of Pennsylvania
Opportunities to Address Oncology Careforce Challenges
Workshop participants discussed potential strategies to improve cancer care delivery and better support the cancer careforce.
Organizational Opportunities
Speakers discussed the following approaches:
Promoting patient-centered care and including family caregivers on the oncology care team
- Integrate caregivers in the cancer care team (Suanna Bruinooge, Mary Jackson Scroggins, Courtney Van Houtven)
- Consider patient experiences in workplace design (Cynthia Cantril, Lawrence Shulman)
- Offer remote patient monitoring and clinical visits to relieve transportation and time burdens through emerging technologies (Susan Dentzer, Diane Portman, Mia Levy, Samuel Takvorian)
- Coordinate scheduling to enable all follow-up care in one visit (Linda Jacobs)
- Offer group visits with clinicians, particularly in survivorship care (Suanna Bruinooge)
- Offer navigation services throughout the continuum of cancer care (Howard Burris, Mary Jackson Scroggins, Cynthia Cantril, Eben Rosenthal)
- Screen patients regularly for their palliative care needs (Diane Portman, Mary Scroggins)
Improving partnerships among specialties and promoting multidisciplinary teams
- Facilitate partnerships between oncology clinicians and primary care clinicians (Linda Jacobs, Mary Jackson Scroggins, Lawrence Shulman)
- Extend the capacity of cancer care teams by increasing autonomy and roles of nurse practitioners, physician assistants, and pharmacists in patient navigation, treatment, follow-up care, and palliative care (Ruth Nemire, Lori Hoffman Högg, Diane Portman)
- Reduce practice inefficiencies through improved care delivery models that enhance coordination among team members (Courtney Van Houtven)
Leveraging organizational culture and leadership to promote clinician well-being
- Build teams on a foundation of dignity, respect, shared accountability, and core organizational values (Anthony Back, Robert Carlson, John Cox, Mia Levy)
- Institute policies to improve the clinical work environment, including measurement of clinician satisfaction, incentives for collaboration and teamwork (Anthony Back)
- Establish formal mentoring programs for clinicians (Robert Carlson, Brenda Nevidjon)
Technology Opportunities
Speakers discussed the following approaches:
Improving the design and usability of electronic health records (EHRs) to reduce administrative burdens
- Design EHRs so patient data are readily accessible (Lawrence Shulman)
- Incorporate improved clinical usability in EHR certification requirements (Anthony Back)
- Improve EHR design elements, such as text boxes that are too small to fully display text as well as requirements for redundant documentation (Mary Sesto)
- Standardize quality measures in EHRs and make them easier to report (Harold Paz, Mary Sesto)
Using innovative technologies, tools, and strategies to support the cancer careforce
- Develop and implement technologies for remote clinician visits (telemedicine) and remote patient monitoring to improve care efficiency and reduce burden for patients and caregivers (Susan Dentzer, Diane Portman, Mia Levy, Samuel Takvorian)
- Make health care technologies available on smartphones, the Internet, and other devices to improve uptake by clinicians and patients (Kathi Mooney, Lawrence Shulman)
- Predicate all technologies on interoperability, seamless data and information exchange, and data accessibility with appropriate privacy and security safeguards (Susan Dentzer)
- Create a public-private initiative to help health care systems acquire and implement the most clinically- and cost-effective technologies (Susan Dentzer)
Policy Opportunities
Speakers discussed the following approaches:
Implementing innovative payment models to improve care quality and reduce careforce burden
- Evaluate the effectiveness of innovative models of care delivery, including their impact on managing new treatments, technologies, and programs (Jon Cox, Suanna Bruinooge, Mia Levy, Lawrence Shulman)
- Move away from fee-for-service reimbursement and toward value-based reimbursement models (Leonard Lichtenfeld, Harold Paz, Kathi Mooney, Scott Shipman)
- Develop new payment models to support greater use of telemedicine (Susan Dentzer)
- Offer financial incentives for health care providers to implement effective innovations in care (Kathi Mooney)
Improving careforce education, training, accreditation, and licensure
- Provide earlier education opportunities in oncology and cancer prevention (Otis Brawley, Robert Winn, Brenda Nevidjon, Lawrence Shulman)
- Promote partnerships with health professional organizations to enhance teaching, educational programs, and demonstration projects (Courtney Van Houtven)
- Provide clinicians with training in effective communication and strategies for supporting health literacy (Courtney Van Houtven, Diane Portman, Anthony Back, Mary Jackson Scroggins)
- Provide undergraduate, graduate, and continuing education in palliative care for all cancer care professionals as well as patients (Mark Hyde, Mary Jackson Scroggins, Diane Portman)
- Create a national licensure system for clinicians that states could opt into to facilitate the practice of telemedicine across state lines (Susan Dentzer, Hildy Dillon, Mark Hyde, Ruth Nemire)
FOOTNOTES
[1] Institute of Medicine. 2013. Delivering high-quality cancer care: charting a new course for a system in crisis. Washington, DC: National Academies Press.
[2] Siegel, R. L., K. D. Miller, and A. Jemal. 2018. Cancer statistics, 2018. CA: A Cancer Journal for Clinicians 68(1):7-30.
[3] AACR (American Association for Cancer Research). 2018. AACR cancer progress report. https://www.cancerprogressreport.org/Pages/default.aspx (accessed May 16, 2019).
[4] ACS (American Cancer Society). 2016. Cancer treatment and survivorship facts and figures 2016-2017. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-treatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2016-2017.pdf
SOURCE: NASEM. 2019. Developing and Sustaining an Effective and Resilient Oncology Workforce: Proceedings of a Workshop
Statements, recommendations, and opinions expressed are those of the individual participants. They are not necessarily endorsed by the National Academies of Sciences, Engineering, and Medicine and should not be construed as reflecting any group consensus.
Workshop participant photos courtesy of Joao Salomao.