MERCURY IN HOUSE PAINT AS A CAUSE OF ACRODYNIA*
Effect of Therapy with N-Acetyl-D,L-Penicillamine
SHALOM ZARACH HIRSCHMAN, M.D.,† MURRAY FEINGOLD, M.D.,‡ AND GEORGE BOYLEN, B.S.§
BOSTON
IN 1948 Warkany and Hubbard1 indicted mercury ingestion as an etiologic factor in acrodynia. Other reports establishing mercury as the most important cause of acrodynia soon followed.2–8
Dimercaprol (BAL), which chelates mercury, was quickly introduced as a therapeutic agent in 1948 but has given variable results.6,9–15 Edathamil calcium disodium (EDTA) when given for therapy of acrodynia did not significantly increase mercury excretion.16 Increased urinary elimination of mercury during penicillin therapy for infection has been observed,17 but the results of penicillin therapy in acrodynia have been equivocal.17,18
Aposhian19,20 has shown that N-acetyl-D,L-penicillamine is more effective than other penicillamine derivatives in protecting laboratory animals from induced inorganic mercury poisoning and that its toxicity is considerably less.19,20 Smith and Miller21 reported the successful treatment of mercury poisoning in a gilder with N-acetyl-D,L-penicillamine.
The patient described below was discovered to be excreting mercury in the urine. In this patient the urinary elimination of mercury was greatly enhanced by treatment with N-acetyl-D,L-penicillamine. The mercury was found in a water-base house paint, and we believe this to be the first report of acrodynia from this source of mercury. An organic compound, phenyl mercuric propionate, had been incorporated into the house paint to prevent growth of molds. Both ingestion of the paint and inhalation of its vapor could have resulted in mercury toxicity.
CASE REPORT
E.L. (M.G.H. 1182958), a 5-year-old white boy, was in good health until 3 months before admission, when generalized abdominal pain, which became more intense during or soon after meals, developed. Two months later pruritus of the hands, followed by complaints of pain in his shoulders, arms, legs and knee joints, developed. He had muscular weakness of the lower extremities and occasionally fell to the ground. Two weeks before admission here he entered another hospital with a tentative diagnosis of rheumatic fever. Two determinations of the erythrocyte sedimentation rate were 4 mm. and 5 mm. per hour. The antistreptolysin-O titer and an electrocardiogram were normal. He became irritable and continued to complain of pain in the extremities. He was transferred to another hospital, where the diagnosis of acrodynia was made by Dr. Douglas W.Walker, of Laconia,
Reprinted with permission from Firschman, Feingold, and Boylen, The New England Journal of Medicine 269(17):889–93, Copyright 1963, Massachusetts Medical Society.
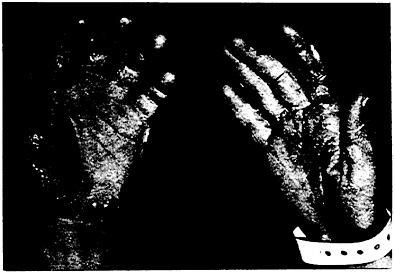
FIGURE 1. Typical Changes in the Skin of the Hands. The skin is scaly and has a pink color.
New Hampshire. A urinary level of 0.09 mg. of mercury per liter, with a urinary specific gravity of 1.004, confirmed the clinical diagnosis. (Normally, no mercury is found in the urine; the hazard level for industrial workers is 0.20 mg. of mercury per liter, with a specific gravity of 1.024.) The patient was referred to the Massachusetts General Hospital for further evaluation and treatment.
Upon admission he had the typical symptoms and signs of acrodynia. These included complaints of pain in the abdomen, extremities and joints, irritability, swinging changes of mood, a marked degree of photophobia, increased perspiration, desquamation and pink color of the hands (Fig. 1), hypertension, hypotonia, salaam positioning (Fig. 2), anorexia and insomnia. His weight was 17 kg., and the body-surface area 0.7 square meter.
Laboratory studies included a normal hemogram and normal electrolytes, blood urea nitrogen, albumin, globulin, serum glutamic oxalacetic transaminase and alkaline phosphatase. An L.E.-cell preparation was negative.
Lumbar puncture revealed a normal spinal-fluid pressure, protein, sugar and colloidal-gold curve. An electroencephalogram was interpreted as being a moderately abnormal waking record because of asymmetry of the 2 sides. There was poor driving and response to strobe on the left. A repeat electroencephalogram 3 days later revealed no marked change.
X-ray films of the skull, knees, shoulders and an intravenous urogram* were normal. X-ray study of the teeth revealed extensive caries involving the deciduous teeth, and several permanent teeth were loose.
Urinalysis was within normal limits. The urine contained trace amounts of lead, but no protein or arsenic. The creatinine clearances were 53 and 54 liters per day. The 24-hour urinary coproporphyrin excretion was normal. Catechol amine studies, done because of clinical signs of increased sympathetic activity, showed a urinary excretion of 3 microgm. of epinephrine and 79 microgm. of norepinephrine per 24 hours. The vanilmandelic acid excretion was 3.5 mg. per 24 hours.

FIGURE 2. Typical Posture Assumed by the Patient. He is burrowing his head into the pillow to blot out the light.
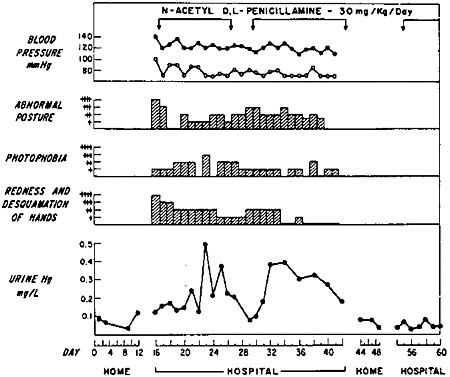
FIGURE 3. Response to N-acetyl-D,L-penicillamine (0= Normal, +=Slightly Abnormal, ++=Mildly Abnormal, +++=Moderately Abnormal, and ++++=Severely Abnormal, as Seen in Acrodynia).
Aliquots of twenty-four-hour urine collections were used for the mercury determinations. The average twenty-four-hour volume range was 500 to 800 ml.
Urine specimens were quantitatively analyzed for mercury throughout the course of the patient’s illness with the use of a modification of the Monkmon method.22 Samples of urine were cold digested with potassium permanganate and sulfuric acid to destroy the organic material. The excess potassium permanganate was bleached with hydroxylamine hydrochloride, and after adjustment to a pH of 6, the solution of the soluble divalent mercury was passed through a glass filter impregnated with cadmium sulfide. The mercury in solution was retained on the pad as a sulfide. The sulfide was then placed in a flask and heated. Evolved mercury was drawn through a General Electric Mercury Vapor Detector, and the readings plotted at 10-second intervals. Standard urines containing known amounts of mercury were treated in a similar manner, and the readings compared with that of the unknown solutions. (The method is very sensitive and is reproducible to less than 0.1 microgm. of mercury per aliquot.)
The patient was treated with N-acetyl-D,L-penicillamine,* 0.125 gm. given 4 times a day (30 mg. per kilogram of body weight per day). The urinary excretion of mercury is shown in Figure 3. The mercury levels of the urine samples rose with treatment, diminished upon discontinuation and were again elevated with the reinstitution of treatment. The daily clinical course, emphasizing change in blood pressure, frequency of abnormal posturing, photophobia and redness and desquamation of the hands, is charted in Figure 3. There was some increase of pain, a slight increase of erythema of the palms, more frequent salaam posturing and greater fluctuation of mood when therapy was discontinued.
With N-acetyl-D,L-penicillamine therapy the patient showed general improvement except for his behavior. This became progressively worse as evidenced by refusal to eat, lying on the floor, throwing away urine specimens and great fluctuation in mood. However, when he was informed of his impending discharge, his behavior became much improved. A follow-up electroencephalogram had reverted to normal.
At home his behavior again became a problem, necessitating readmission 11 days after discharge. He was given a 6-day course of N-acetyl-D,L-penicillamine. His behavior markedly improved although there was no significant increase in the urinary mercury excretion. After 8 days in the hospital he was discharged, and since this last discharge he has maintained his clinical improvement. Ten months later a urine sample contained 0.016 mg. of mercury per liter.
In an attempt to discover how this child was exposed to mercury, the patient’s home was examined by the New Hampshire Department of Public Health, but no source was found. It was then learned that the patient had helped his mother paint part of the kitchen and bedroom 4 months before the onset of symptoms. There was no definite history of ingestion of paint although this remains a possibility. The paint used was analyzed and found to contain mercury by the method already described for the urine samples. The sleeping quarters were very small. The parents, a 3-year-old brother and the patient all slept in the same room, whose dimensions were 10 by 10 by 8 cubic feet. Other members of the family whose urine was sampled for mercury had none in a single sample. They had no signs of mercury intoxication.
The concentration of metallic mercury in the paint was found to be 0.02 per cent on a weight basis, or 0.036 per cent phenyl mercuric propionate. To determine the rate of evaporation of mercury from the paint and whether the mercury concentration of the surrounding air could reach appreciable levels, a panel 8 by 2 3/8 inches was painted with an average coat of paint on a painted surface of 37 square inches. The panel was suspended in a 1.9-liter enclosed jar. Air was passed through the jar at a rate of 1 liter per minute, and periodic measurements of the mercury concentration in the jar were made with the General Electric Mercury Vapor Detector. The amount of vapor from the freshly painted panel in equilibrium with air at a flow rate of 1 liter per minute was 0.17 mg. of mercury per cubic meter of air at the end of the 1st 30 minutes, for a calculated average volatilization rate of 0.50 microgm. of mercury per minute per square foot. The test panel continued to emit mercury vapor in diminishing amounts for 6 weeks despite continuous air exchanges. On the basis of an average volatilization rate of 0.50 microgm. of mercury per minute per square foot, it was calculated that a room 10 by 10 by 8 cubic feet in which the 4 walls had been painted with an average coat of this mercury-containing paint and ventilated at the rate of 2 air exchanges per hour would have an average concentration of 0.21 mg. of mercury per cubic meter of enclosed air. The concentration in the surrounding air considered acceptable for continuous adult exposure without toxic effect is 0.10 mg. of mercury per cubic meter.*
DISCUSSION
The amount of mercury considered of etiologic importance in acrodynia may be small, and the interval between the exposure to mercury and the onset of the disease in the reported cases varies from one week to several months. That the patient was the only member of his family clinically affected by the mercury may be explained by his greater exposure during the painting of the rooms, by the possibility of ingestion of the paint or by an idiosyncrasy to mercury. It was not possible to quantitate the amount of mercury absorbed by the patient.
The improvement after the initiation of N-acetyl-D,L-penicillamine therapy may have been fortuitous. Normally, the course of untreated cases lasts from months to a year. Since mercury seems to be the offender in acrodynia its more prompt elimination from the body should be beneficial. The marked spontaneous variation in the daily elimination of mercury23 makes it difficult to evaluate precisely the effects of drugs on its excretion. Further
more, the marked individual susceptibility to mercury may lead to considerable variation in clinical course quite apart from the use of chelating compounds. Perhaps some people require a much greater reduction of the body pool of mercury before cessation of symptoms. Whether acrodynia represents an allergic reaction to mercury, as originally suggested by Helmick,24 or is merely an expression of individual idiosyncrasy to the toxic effects of the metal has been amply discussed by Warkany and Hubbard,25 who favor the latter hypothesis.
N-acetyl-D,L-penicillamine is the acetylated congener of D,L-penicillamine. Unlike D,L-penicillamine, it will not increase urinary excretion of copper.20 It appears that N-acetyl-D,L-penicillamine is a more effective sulfhydryl donor.
The course with N-acetyl-D,L-penicillamine in the case reported above compares favorably with that in cases treated with BAL.6,9–15 Although N-acetyl-D,L-penicillamine has not had as extensive a clinical trial as BAL, there is no evidence that it shares the known toxicity of BAL and, unlike that compound, it is administered orally. It has been shown to be less toxic than D,L-penicillamine in experiments in rats.19,20 The patient described above gave no sign of sensitivity to the drug such as rash, fever, leukopenia or thrombocytopenia. The six-day course of therapy during the last admission was marked by a vast clinical improvement although the urinary excretion of mercury did not increase. Presumably, the labile body stores of mercury had been depleted by the previous course of therapy. In the treated case of mercury poisoning reported by Smith and Miller21 clinical improvement with N-acetyl-D,L-penicillamine therapy could not be correlated with mercury excretion, and they suggested that the amount of mercury excreted may be much less important than the amount complexed in an inactive form in blood and tissues.
It is interesting that the twenty-four-hour urinary catechol amine excretion in the present case was elevated. Feer,26 in 1925, attributed acrodynia to a disorder of the vegetative nervous system and used atropine to treat his cases. Stolz27 reported hyperplasia of the chromaffin system in acrodynia. Blackfan and McKhann,28 after studying 40 cases, observed that sympathetic overactivity accounted for most of the symptoms; they found that the pulse rate of patients with acrodynia did not vary during sleep as in normal subjects. Day et al.29 concluded that emotional stresses failed to elicit normal vegetative responses from patients with acrodynia. They thought that this might be explained by pre-existing maximum stimulation of the sympathetic nervous system and compared acrodynia to pheochromocytoma. Hubble30 stressed the similarity between acrodynia and pheochromocytoma. Excessive vasoconstriction was found by Vulliamy31 in 10 of 11 cases of acrodynia. Reflex vaso -
dilatation of the hands, which normally follows heating of the trunk and legs, was absent. This capacity was regained with the use of tolazoline hydrochloride (Priscoline) and tetraethylammonium bromide. Farquhar et al.32 described increased urinary sympathin in 3 of 4 cases of acrodynia as compared with normal children. Cheek and his associates33,34 demonstrated that calomel potentiates the effect of epinephrine in the rat, and suggested that mercury potentiates sympathetic activity in acrodynia. Peterson and Laughmiller35 reported the relief of symptoms in 6 of 7 cases of acrodynia treated with tolazoline. Bower36 noted relief of all symptoms except for photophobia with sympatholytic drugs such as hexamethonium tartrate and pentolinium bromide; he confirmed the relief of arteriolar spasm in patients with acrodynia by these drugs. Ritzel, Berger and Roulet37 recently observed increased catechol amine excretion in a case of acrodynia. Now that better methods for the determinaton of urinary catechol amines are available, sympathetic activity in acrodynia should offer a field for fruitful investigation.
Another interesting and unique finding in this case is the apparent source of mercury in the house paint. The demonstration that potentially harmful levels of mercury could result from vaporization of these paints supports this conclusion. The patient’s home, household contents and surrounding areas were examined by both the New Hampshire Department of Health and ourselves. The only source of mercury that could be detected was found in the paint. The amount of mercury in the urine and the length of time during which it was excreted implies that the inhalation of mercury vapor by the patient occurred over a long period. The discovery of mercury in the paint and our studies of the continuing emission of mercury into the air surrounding the painted surfaces present a new and potentially common cause for mercury poisoning. One wonders if there may be patients with some of the more subtle signs and symptoms of acrodynia in whom this diagnosis is not being considered. The paint manufacturer’s responsibility is a matter of public-health interest. Mercury-containing paint should be labeled properly and should indicate the possible danger to children upon ingestion or exposure to the toxic vapors. These mercury-containing paints should be limited to outdoor use.
SUMMARY AND CONCLUSIONS
A case of acrodynia in a patient who had increased urinary excretion of mercury is presented. New methods for mercury analysis are described. The source of mercury was found in house paint, and the epidemiologic implications of this finding are discussed.
The patient was treated with N-acetyl-D,L-penicillamine, which markedly increased the urinary output of mercury.
The rationale for this form of therapy in acrodynia is presented and compared with previously reported therapeutic methods.
Increased excretion of catechol amines was found in the urine. The relation of this finding to theories of the pathogenesis of acrodynia is considered.
We are indebted to Dr. Douglas W.Walker of Laconia, New Hampshire, for referring this patient to our service and for assistance in the collection of essential data, to Drs. Harriet L.Hardy and John D.Crawford, of the Massachusetts General Hospital, for inspiration and guidance, to the New Hampshire State Department of Health for help and interest, to Mr. Frederick Viles, Jr., and Mr. Richard Chamberlin, of Massachusetts Institute of Technology, for aid in the mercury determinations and to Dr. Nathan B.Talbot, chief of the Children’s Service, Massachusetts General Hospital, for guidance and helpful suggestions in the preparation of the manuscript.
REFERENCES
1. Warkany, J., and Hubbard, D.M. Mercury in urine of children with acrodynia. Lancet 1:829, 1948.
2. Fanconi, G., and Botsztein, A. Die Feersche Krankheit (Akrodynie) und Quecksilbermedikation. Helvet. paediat. acta 3:264–271, 1948.
3. Andersen, D. Acrodynia caused by exposure to mercury. Acta paediat. 40(Supp. 83):123, 1951.
4. James, G.A. Mercury as cause of pink disease. Great Ormond St. J. 1:48–51, 1951.
5. Laplane, R., Fabiani, P., and Desarmenien, H. Acrodynie et mercure: à propos de neuf observations. Nourrison 39:235–247, 1951.
6. Warkany, J., and Hubbard, D.M. Adverse mercurial reactions in form of acrodynia and related conditions. Am. J. Dis. Child. 81: 335–373, 1951.
7. Holzel, A., and James, T. Mercury and pink disease. Lancet 1: 441–443, 1952.
8. Speirs, A.L. Further evidence of association between mercury and pink disease. Brit. M. J. 2:142, 1959.
9. Bivings, L., and Lewis, G. Acrodynia, new treatment with BAL. J. Pediat. 32:63–65, 1948.
10. Elmore, S.E. Ingestion of mercury as probable cause of acrodynia and its treatment with dimercaprol (BAL): report of 2 cases. Pediatrics 1:643–647, 1948.
11. Bivings, L. Acrodynia: summary of BAL therapy reports and case report of calomel disease. J. Pediat. 34:322–324, 1949.
12. Carithers. H.A. Mercury poisoning from calomel producing subacute acrodynia and its treatment with dimercaprol: report of case. Pediatrics 4:820–824, 1949.
13. Denys, P. Acrodynie, mercure et B.A.L. Acta paediat. belg. 4: 16–25, 1950.
14. Fischer, A.E., and Hodes, H.L. Subacute mercury poisoning (acrodynia) caused by protiodide of mercury: successful treatment with BAL . J. Pediat. 40:143–151, 1952.
15. Debre, R., Schapira, G., and Royer, S. Acrodynie et hydrargyrurie. Arch, franç. pédiat. 9:443–446, 1952.
16. McCoy, J.E., Carre, I.J., and Freeman, M. Controlled trial of edathamil calcium disodium in acrodynia. Pediatrics 25:304–308, 1960.
17. Launay, C., Fabiani, P., Grenet, P., Hadengue, A., and Radzievsky. Absorption massive et prolongée de calomel chez un enfant: etude de l’élimination urinaire du mercure. Arch, franç. pédiat. 7:75–79, 1950.
18. Bouineau, M. Quatre cas d’acrodynie traités par la pénicilline. Arch, franç. pédiat. 8:785, 1951.
19. Aposhian, H.V., and Aposhian, M.M. N-acetyl-DL-penicillamine, new oral protective agent against lethal effects of mercuric chloride. J. Pharmacol. & Exper. Therap. 126:131–135, 1959.
20. Aposhian, H.V. Penicillamine and its analogues: metabolic properties and oral activities against lethal effects of mercuric chloride. In Metal-Binding in Medicine. Edited by M.J.Seven. 400 pp. New York: Lippincott, 1960. Pp. 290–295.
21. Smith, A.D.M., and Miller, J.W. Treatment of inorganic mercury poisoning with N-acetyl-D,L-penicillamine. Lancet 1:640–642, 1961.
22. Monkmon, J.L., Maffett, P.A., and Doherty, T.F. Determination of mercury in air samples and biological materials. Am. Indust. Hyg. A. Quart. 17:418–420, 1956.
23. Zellweiger, H., and Wehrli, S. Der Quecksilbernachweis im Urin und seine Bedeutung für die Diagnose der Akrodynie. Helvet. paediat. acta 6:397–405, 1951.
24. Helmick, A.G. Symptomatology of acrodynia as basis for new line of investigation as to its etiology. Arch. Pediat. 44:405–410, 1927.
25. Warkany, J., and Hubbard, D.M. Acrodynia and mercury. J. Pediat. 42:365–386, 1953.
26. Feer, E. Eine eigenartige Neurose des vegetativen Systems beim Kleinkinde (Acrodynie, Erythrödem, Pink disease). Jahrb. f. Kinderh. 108:267–281, 1925.
27. Stolz, S. Cited in Woringer, P. L’acrodynie infantile. Rev. franç. de pédiat. 2:440–462, 1926.
28. Blackfan, K.D., and McKhann, C.F. Acrodynia, note on pathologic physiology. J. Pediat. 3:45–54, 1933.
29. Day, R., Smith, J.R., and Klingman, W.O. Tests of function of vegetative nervous system in acrodynia. Am. J. Dis. Child. 57: 269–277. 1939.
30. Hubble, D. Phaeochromocytoma in children. Arch. Dis. Childhood 26:340–350, 1951.
31. Vulliamy, G.D. Vasomotor disturbance in pink disease. Lancet 2:1248–1251, 1952.
32. Farquhar, J.W., Crawford, T.B.B., and Law, W. Urinary sympathin excretion of normal infants and of infants with pink disease. Brit. M. J. 2:276–281, 1956.
33. Cheek, D.B., and Wu, F. Effect of calomel on plasma epinephrine in rat and relationship to mechanisms in pink disease. Arch. Dis. Childhood 34:502–504, 1959.
34. Cheek, D.B., Bondy, R.K., and Johnson, L.R. Effect of mercurous chloride (calomel) and epinephrine (sympathetic stimulation) on rats: importance of findings to mechanisms in infantile acrodynia (pink disease). Pediatrics 23:302–313, 1959.
35. Peterson, J.C., and Laughmiller, R. Acrodynia, treatment with adrenolytic drugs. Acta paediat. 43(Supp. 100):517–525, 1954.
36. Bower, B.D. Pink disease: autonomic disorder and its treatment with ganglion-blocking agents. Quart. J. Med. 23:215–230, 1954.
37. Ritzel, G., Berger, H., and Roulet, D.L.A. Increased catecholamine excretion in case of acrodynia: (pink disease). Ann. Paediat. 198:81–88, 1962.





