![]()
Rapid Expert Consultation on Staffing Considerations for Crisis Standards of Care for the COVID-19 Pandemic (July 28, 2020)
July 28, 2020
Robert Kadlec, M.D.
Assistant Secretary for Preparedness and Response
200 Independence Avenue, SW
Washington, DC 20201
Dr. Kadlec:
Attached please find a rapid expert consultation that was prepared by the co-conveners of the Crisis Standards of Care (CSC) working group, Dan Hanfling and John Hick, and conducted under the auspices of the National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats.
Building on prior National Academies reports on CSC and the rapid expert consultation on March 28, 2020, the aim of this rapid expert consultation is to focus on staffing needs for the care of COVID patients, including the deployment and allocation of expert clinical staff during COVID-19. It does not attempt to dictate exactly what choices should be made under exactly what circumstances, as that should be left to the judgment of the professional, institutional, community, and civic leaders who are best situated to understand the local conditions.
We recognize that responsible officials seek a solution through obtaining a larger number of qualified, expert personnel to meet the clinical demand. We agree this is preferred. The purpose of this rapid expert consultation is to offer guidance when that solution cannot be implemented and available staffing is less than optimal.
CSC compel thinking in terms of what is best for an entire group of patients on the principle of saving the most lives (or achieving the best outcome for the group of patients) rather than focusing on only an individual patient under a clinician’s care. When equipment, staffing, and materials are sufficient, focusing on only what is best for each individual patient is tantamount to the best outcome for the collection of patients because the group outcome is simply the sum of the individual outcomes. Under conditions that drive CSC, this identity of outcomes for the individual and group breaks down, and the decision makers cannot avoid the hard choices before them. We hope the guidance in this rapid expert consultation can assist those charged with making these difficult decisions.
Respectfully,
Harvey V. Fineberg, M.D., Ph.D.
Chair
Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats
PROBLEM STATEMENT AND SCOPE
The availability of qualified staff, particularly for respiratory therapy and critical care nursing, is restricting many hospitals and states from meeting patient care needs as COVID-19 cases increase in their jurisdiction. Inconsistent staffing models across hospitals and jurisdictions highlight the importance of a fair and equitable process to meet staffing needs. Prioritization across multiple requests for staffing assistance from different health care coalitions and jurisdictions can be difficult as the effect of some variations in staffing patterns on patient outcomes is unclear.
An overview of the key considerations pertaining to the implementation of crisis standards of care (CSC) was delivered in the form of a Rapid Expert Consultation to Department of Health and Human Services (HHS) Assistant Secretaries Brett Giroir and Robert Kadlec on March 31, 2020, by the National Academies Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats. The standing committee was engaged on this topic again in mid-July 2020, specifically to consider staffing in the implementation of CSC. This document briefly defines aspects of the staffing problem, potential solutions, and considerations for deployment and allocation of staff during COVID-19.
BACKGROUND
Expansion of health care system capacity or “surge capacity” is predicated on the availability of:
- Systems that coordinate the response and both the appropriate and functioning structure in which to provide care;
- Space, including the use of non-traditional and non-patient care spaces when needed;
- Staff, including the use of non-traditional staff and non-traditional structure or roles; and
- Supplies, including the substitution or adaptation of available resources such as personal protective equipment (PPE), medications, or even critical care resources.1
According to the Institute of Medicine 2012 CSC guidance, along with related publications, disaster medical response is defined as occurring across a spectrum that spans from conventional care to crisis care:
- Conventional Capacity: The spaces, staff, and supplies used are consistent with daily practices within the institution. These spaces and practices are used during a major mass casualty incident that triggers activation of the facility emergency operations plan.
___________________
1 Hick et al. 2009. Refining surge capacity: Conventional, contingency, and crisis capacity. Disaster Medicine and Public Health Preparedness 3(S1):S59–S67.
- Contingency Capacity: The spaces, staff, and supplies used are not consistent with daily practices but provide care that is functionally equivalent to usual patient care. These spaces or practices may be used temporarily during a major mass casualty incident or on a more sustained basis during a disaster (when the demands of the incident exceed community resources).
- Crisis Capacity: Adaptive spaces, staff, and supplies are not consistent with usual standards of care, but provide sufficiency of care in the context of a catastrophic disaster (i.e., provide the best possible care to patients given the circumstances and resources available). Crisis capacity activation constitutes a significant adjustment to standards of care.2
Notably, these categories exist along a continuum, and there is no “bright line” between them. The goal is to maximize conventional and contingency capacity, avoiding crisis. When crisis conditions exist, the goal is to “gracefully degrade” services to the minimum degree needed to meet the demands, maintaining the maximum patient and provider safety. Of these surge elements, staff is the most elastic (i.e., staff can be “stretched” to provide coverage in a number of different ways). During COVID-19, space has not been a key limiting factor; however, the availability of qualified critical care and respiratory therapy staff has been a national problem. Thousands of federal and out-of-state providers have responded to the needs of states, such as New York, in an attempt to help meet a surge in need. However, as the crisis continues unabated, with nearly 40 of 50 states with “hotspots” (defined by rising case counts, rising hospitalizations, and decreasing bed availability in hospital intensive care units [ICUs]), adequate staffing may not be available to support all regions to the degree required to maintain a conventional level of care.
STRATEGY OVERVIEW
Two broad categories of response to an ongoing crisis are (1) community-wide strategies and (2) health care system–specific strategies. The first set of efforts may include:
- Reducing the burden of disease by implementation of non-pharmaceutical interventions whenever possible;
- Transferring patients at capacity-strained facilities to facilities with a lower census so as to “load balance” the delivery of services whenever possible;
- Curtailing the delivery of elective services, including the scheduling of routine care visits in the outpatient setting; and
- Ensuring support efforts are in place in order to meet the social and psychological needs of the existing health care workforce.
These strategies may help decompress a surge in demand for health care and expert providers of care. When these strategies are no longer sufficient to meet patient care needs, a set of health care system–specific strategies may be implemented. These may be in tandem with broader strategies above and include:
___________________
2 Institute of Medicine. 2012. Crisis standards of care: A systems framework for catastrophic disaster response. Washington, DC: The National Academies Press. https://doi.org/10.17226/13351.
- Mobilizing staff from out-of-hospital entities to assist in the delivery of hospital-based services;
- Recruiting non-practicing clinical providers who work in the hospital environment to work alongside and assist actively licensed practitioners and adjusting the scope of practice considerations;
- Adjusting the ratio of providers to patients in both the general medical/surgical units as well as in the critical care units;
- Changing the model of inpatient care delivery to a team-based rather than individual nursing approach; and
- Deploying telemedicine and other digital health solutions to provide critical care medical oversight and remote patient management capabilities.
COMMUNITY STRATEGIES
A variety of community-based strategies will need to be employed in order to meet COVID-19 surge demands.
Reduce the Burden of Disease
The number one way to address the need for health care surge is to ensure that community-based interventions are maximally applied. This needs to be more effectively messaged to the community at large. Given the impact of certain interventions on reducing the spread of disease and decreasing the stress to the health care system, the public needs to understand its role in keeping health care workers safe and available to work to care for those who become ill.. By the time that stress on the health care system is recognized, regardless of any mitigating actions taken, an increasing number of cases will continue for weeks. The mandatory use of masks in public areas, physical distancing, public messaging, and the imposition of limitations on public gatherings at certain locations (such as those that contact tracing and epidemiological studies identify as high risk for the spread of illness [e.g., bars, stadiums, religious gatherings]) are all techniques that should be maximally employed.
Transfer Patients to Diffuse Impact
The experience of several metropolitan areas has shown that the impact of COVID-19 is not consistent, even across a single city. Depending on the communities served, a disproportionate burden of cases may fall on a single or few facilities or a metropolitan area, while other hospitals continue to have capacity. The use of health care coalitions and Medical Operations Coordination Centers (MOCCs)3 as “level-loading” mechanisms should be in place to ensure that all available inpatient capacity is leveraged.4 This type of system facilitated approximately
___________________
3 Burkle et al. 2007. Definition and functions of health unified command and emergency operations centers for large-scale bioevent disasters within the existing ICS. https://pubmed.ncbi.nlm.nih.gov/18388641.
4 Federal Emergency Management Agency National Response Coordination Center Healthcare Resilience Task Force. 2020. Medical Operations Coordination Cells concept of operations toolkit, first edition. Washington, DC: Federal Emergency Management Agency. https://files.asprtracie.hhs.gov/documents/fema-mocc-toolkit.pdf.
1,000 transfers in the metro Detroit, Michigan, area during its spring surge. Some objections have been raised that patients with COVID-19 are “too sick to transfer.”5 It may not be appropriate to transfer patients who are in a dynamic state; however, because many facilities routinely transfer extremely ill persons on a routine basis (including on ECMO), determining who can safely be transferred, by what means, and to what destination may have tremendous benefit in equalizing loads. Some hospitals may be reluctant to participate in receiving patients. Future federal support programs, funding (e.g., the Coronavirus Aid, Relief, and Economic Security [CARES] Act), and mutual aid agreements should spell out reciprocal commitments to accept patients to achieve regional consistent levels of care, and should ensure all available measures are taken to increase focus on collaboration, rather than competition, among health care systems during this critical time. Jurisdictions have found that this mechanism can be helpful moving non-critical patients out to smaller community hospitals (Texas6) and that coordination of emergency medical services (EMS) rotor-wing or ground transport assets through the MOCC mechanism may contribute significantly to success during COVID-19 as it has during hurricane-related evacuations in the past (Texas SouthEast Texas Regional Advisory Council).
Curtail Elective Procedures and Appointments
Selective or complete cessation of elective procedures and appointments can rapidly increase the availability of staff. A ranking system for procedures may be helpful not only to determine prioritization (based on risk if the procedure is postponed) but also balanced against the need for the staff and the risk of transmission of COVID-19. As with patient transfers, some hospitals in an area may wish to continue elective procedures while others have to curtail them. The role of health care coalitions and jurisdictional public health, emergency management, and executive officers is important to maintain a coordinated approach so that the surge is able to be absorbed. These same stakeholders should also be consulted on the decision to recommend (mandating when necessary) when to curtail elective operations at a regional level (this may be across a metropolitan area, multi-county region, state, or even inter-state where the catchment area for health systems spans multiple states).
For the measures above to be maximally effective, it is critical that hospitals and health systems share comprehensive data through MOCCs and/or health care coalitions. While data may not only be valuable in understanding current capacity and in recognizing important trends, especially the often long lag time between initial infection and the onset of severe symptoms they are also essential to properly load balancing health care delivery across larger areas more comprehensively. In addition to the numbers (census, bed types, provider types, etc.) MOCCs have a role to play in ensuring that participating facilities are using common definitions to make direct comparisons and ensure the availability of a critical resources is not assumed to be more or less based on institution-specific terminology or usage. It is also important that facilities not rely
___________________
5 Department of Health and Human Services Assistant Secretary for Preparedness and Response. TRACIE—Establishing Medical Operations Coordination Cells (MOCCs) for COVID-19. Webinar recorded April 24, 2019. https://files.asprtracie.hhs.gov/documents/aspr-tracie-mocc-webinar--4-24-20-final-slides.pdf.
6 Mone, J. L., and N. Merchant. 2020. South Texas drenched by cyclone amid surge in virus cases. The Washington Post, July 25. https://www.washingtonpost.com/health/virus-weary-texas-hit-by-category-1-hurricanehanna/2020/07/25/9faec0e6-ced6-11ea-99b0-8426e26d203b_story.html.
on unstated assumptions about the meanings of various resource availabilities and constraints. Relying on commonly used assumptions about ICU beds being available for only cases of shock or ventilator-dependent patients in a mass casualty would result in a significant variance between assumed and actually available ICU beds.
In addition to hospital capacity and resource data, it is essential that MOCCs and healthcare coalitions, especially those that cross jurisdictional boundaries, share common definitions and reporting criteria for public health data. Community data such as testing capacity and results and infection incidence are needed in concert with hospital-collected data to best understand the impact of disease in the community and to assist in projecting resource requirements.
Ensure Support for Existing Staff
In some cases, existing staff may be capable of additional hours but are restricted due to family care issues or other home obligations. In some cases, they may have concerns about passing the disease to family members, being at higher risk for complications themselves, or may be uncomfortable about the availability of effective PPE.
Identifying inactive health care workers as a potential source of staffing (i.e., for deployment elsewhere to “hotspot” areas) should be made a high priority. Facility and state-based visibility of the availability of the health care workforce in the state based on the category of staffing (part time, as needed status; on leave; retired) should be implemented, in addition to making available all possible incentives and protections. It is possible that some staff may be furloughed due to financial challenges at a particular facility, these staff should quickly be identified as a potential source of surge staffing in the larger community. With regard to incentives, it may be possible to provide “hazard pay” benefits that serve as a motivation to continued work in a stressful and potentially hazardous environment. However, the sources of funds for this incentive need to be specifically identified in light of impacts from reductions of elective procedures and other financial stresses caused by COVID-19 responses. In some cases, additional pay has been needed to compete with unemployment benefits as well as increased compensation offered by staffing agencies.
Facilitating expanded availability of staff is not just a matter of identification and incentives. Current staff must also be supported psychologically, physically, and financially. A cycle of overwork from longer shifts and/or higher acuity patients can drive burnout and reduce commitment. Supporting current workers through recognition, peer and professional support for stress management and counseling, encouraging appropriate time off and use of time off, supporting healthy lifestyle choices (within reason given the constraints and requirements of the pandemic), and providing other support (transportation, child care, elder care, etc.) to ensure the health care worker is effective when at work may all be important contributors to staff maintenance. Additionally, it is important for employers to acknowledge the concerns of staff with regard to the risk of spreading workplace-acquired infections at home and, where possible, to develop resources to support self-isolation and other measures to protect family members, such as lodging, take home meals, and other resources.
The 2019 National Academies report on clinician burnout offers key points that are critically relevant and should be considered in developing policies and resources for staff support:
- A major driver of burnout is dysfunctional systems of care, so patient care processes should be examined with a human factors lens to improve quality and safety and reduce wasted effort and unnecessary workarounds.
- Adequate support must include confidence of PPE availability but also child care, especially when schools are closed or learning is home based.
- Moral distress is a contributor to burnout. Some of this distress comes from unavoidable situations of critical illness in the absence of family and friends, and some of it comes from having to make allocation decisions in the absence of clear guidelines. Crisis standards for resource allocation should be transparent and supported by leaders so frontline workers are not grappling with these issues alone. Ethicists can be essential to promoting optimal clinical dialogue, offering a way for frontline workers to ask tough questions and experience shared discourse about difficult decisions.
- Attention to racial equity as an important social force and a source of added tension and stress should be emphasized. People of color are both disproportionately represented in case numbers but also comprise the majority of the health care workforce in many areas. These issues need to be included in considerations about how to promote the well-being of staff as well as care of patients. Reinforcing staff to be mindful of implicit bias is relevant to sustaining a healthy, diverse workforce.7 Staff education, dialogue, and commitment to improve access to health care resources by communities of color should be a focus, particularly with a vaccine potentially available in the near future.
Finally, staff policies should also describe how potentially infected staff who might otherwise be off work could be engaged in caring for COVID-19-positive patients and support ongoing clinical work if they desire to continue working and are physically and psychologically able to do so. Potentially infected and quarantined staff could also contribute via telemedicine, remote work, or remote training support to allow them to continue to work without increasing the risk of exposure to themselves or others. Adequate time off for illness and recovery from COVID-19 is important and should be encouraged, as recovery is highly variable.
Implement Innovative Strategies to Increase Support to Patients in the Community and Reduce Emergency Department and Inpatient Loading
While much of the focus of CSC discussions is on critical inpatient populations, the support and management of less critical patients in the community can have a substantial impact on the resources available. The utilization of digital health technology and remote patient monitoring to create interactive systems that provide real-time “virtual care” and medical oversight should be considered for implementation. An example of this is the COVID Watch system created at the University of Pennsylvania, which allowed seven full-time nurses to manage 1,000 less acute
___________________
7 National Academies of Sciences, Engineering, and Medicine. 2019. Taking action against clinician burnout: A systems approach to professional well-being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25521.
patients ill at home on a 24/7 basis.8 Using digital health tools in order to reduce emergency department visits and increase patients’ ability to recover at home will be critically important in managing COVID-19 and future pandemics.9 In addition, the engagement of outpatient practices focused on at-risk special groups provides a trusted channel to reach some of the communities’ most medically fragile members. Alignment of public health messaging; interactive, virtual care tools; and the teams at outpatient specialty facilities could help protect vulnerable patients and potentially free up staff for other roles.
HEALTH CARE SYSTEM STRATEGIES
Obtain Additional Staffing
Health care coalitions can play an important role in obtaining additional staff from within the coalition or from neighboring coalitions. Existing staff-sharing agreements may be leveraged to move staff from one facility to another. In some cases, it may make sense to move staff from more rural hospitals into urban facilities (if more stable patients cannot be moved to those facilities). Long-term care facilities may also have some staffing resources available, although they are likely to be as burdened with staffing issues as hospitals.
Health care systems should also be moving staff among facilities in their networks when needed. This may also involve moving staff from outpatient to inpatient facilities (e.g., ambulatory surgical center Certified Registered Nurse Anesthetists [CRNA] and post-anesthesia nurses to hospitals) to maximally utilize provider skills. This includes national health care system movement of providers across state lines, which, in states that are not members of various interstate licensing compacts, or lack extensive reciprocity agreements may trigger inter-state licensure issues that must be addressed.
A significant number of outpatient staff (e.g., from orthopedics clinics and systems, specialty staff from ambulatory care centers) can be made available as elective appointments and procedures are curtailed, and these staff may be re-deployed to support inpatient response with appropriate on-boarding, assignment of appropriate duties, and supervision.
Many local and national contract agencies exist that can provide short-term support. These should be leveraged by both the public and private sectors to ensure that as many personnel are brought in as needed. In some cases, the exact skill set may not be available, but if licensed nursing personnel are available, appropriate duties can be found for them in most cases. Interstate licensure recognition should be available via executive orders if it does not currently exist within the state. In some cases in New York City, contract staff were not briefed on or prepared for the staffing situations they encountered and essentially walked off the job. Appropriate orientation and expectations are important. The number one barrier experienced was orientation
___________________
8 Morgan et al. 2020. Remote monitoring of patients with COVID-19: Design, implementation of the first 3,000 patients in COVID Watch. New England Journal of Medicine Catalyst. https://catalyst.nejm.org/doi/pdf/10.1056/CAT.20.0342.
9 In-Q-Tel. 2019. Roundtable report—leveraging digital health technologies during large-scale epidemics. https://www.bnext.org/wp-content/uploads/2019/12/Digital-Health-Roundtable-Report.pdf.
and facility with the electronic health record. Pairing contract staff with facility staff who can support and assist with documentation are important to using contract staff successfully.
State response teams, the Medical Reserve Corps, EMS, and the National Guard may also be sources of personnel. In many cases, deployment of licensed personnel on these teams does not make sense as they would be needed for their usual job duties. However, some personnel may be available, and in many cases the National Guard and other personnel have medical training but do not use it in their current employment. Medical Reserve Corps capabilities differ widely across jurisdictions, and unfortunately many of the registered providers either have commitment to their daily jobs or, if retired, may be uncomfortable returning to clinical care due to both competency issues as well as concerns about contracting COVID-19.
Federal medical teams such as HHS/Assistant Secretary for Preparedness and Response (ASPR) Disaster Medical Assistance Teams may also struggle to fill licensed staff rosters due to providers being needed in their daily roles. Department of Defense (DoD) and Department of Veterans Affairs (VA) medical staff may be deployed from lesser-affected regions to support civilian resp e, but the number of available providers may be substantially less than the demand.
Re-Deploy Staff and Adjust Job Responsibilities
Education and administration personnel with clinical backgrounds (nurse managers, supervisors, clinical educators) should be returned to practice and relieved of their other duties unless those duties involve direct COVID-19 or other critical operational roles. Limitations related to the “scope of practice” may be relaxed or revisited in order to allow for as many available personnel to play a role in health care service delivery as possible, while ensuring that patients receive appropriate clinical care.
Staff may be asked to “step up” the level of care they provide (i.e., provide care to patients with more acute or different conditions than they are used to). This should involve the least difference possible between daily and surge responsibilities. For example, an intermediate care nurse works in the ICU, a nurse from a cardiac rehabilitation unit staffs in intermediate care, a floor nurse staffs cardiac rehab, and a pre-induction surgical nurse with prior inpatient experience provides floor care. These “step ups” should be accompanied by appropriate training and orientation, ideally anticipated and provided before such a transition is needed both to improve acceptance and ensure appropriate job performance as well as work through any associated collective bargaining and administrative issues.
Staff may also be asked to “step over” by applying their knowledge to a different group of patients than they normally care for. This is particularly relevant for anesthesia and CRNA providers, post-anesthesia nursing, critical care surgical staff, and others who can apply their critical care knowledge to the medical intensive care environment.
Some staff may be asked to “step down” or generalize their practices. For example, specialty surgeons and physician assistants may be asked to take on general medicine rounding roles.
Finally, all job duties should be examined and responsibilities for documentation, education, departmental, and other tasks reduced to the minimum necessary (e.g., adopt “charting by exception” to document only relevant changes in condition particularly for daily notes). Several systems have reduced the nursing charting burden by dramatically simplifying intake assessments. Awareness of Centers for Medicare & Medicaid Services waivers is an important part of creating expectations that are still consistent with the conditions of participation.
Change Staffing Model
Most hospitals maintain a critical care staffing ratio of 1 nurse per 2 patients. This may vary depending on the case mix and responsibilities. Adjusting this ratio to 1:3 or even 1:4 may be possible with appropriate patient selection (e.g., one or two patients in early stages of illness and one or two who are more stable, but still require mechanical ventilation, for example).10 Alternatively, the hospital may maintain usual ratios in areas where the new admissions are boarded, as they tend to have more dynamic changes early in their hospitalization and require more frequent assessments and interventions, while adjusting the ratios for more stable patients.
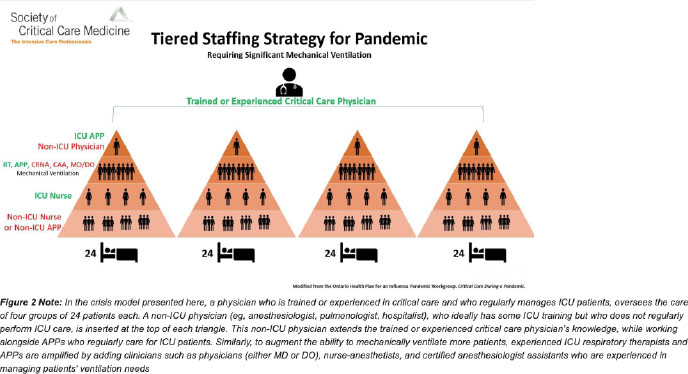
Despite available supplemental staff, in many cases the model of individual nursing cannot be sustained. In this case, the critical care nurses and physicians should move to a consulting role, supervising an increasing ratio of patients while other nursing providers and physicians (e.g., hospitalists) manage the bedside care, orders, and medications. This principle is illustrated below by a figure from the Society of Critical Care Medicine11 in which non-ICU nurses provide care at a 1:2 ratio with 1 critical care nurse supervising 6 patients, a hospitalist or other physician supervising 24 patients, and a critical care physician reviewing care and troubleshooting with the four “team” physicians to effectively supervise care for 96 patients. This is an extreme situation but illustrates a team-based model.
___________________
10 Abir et al. 2020. Critical care response strategies for the 2020 COVID-19 outbreak in the United States. Santa Monica, CA: RAND Corporation.
11 Halpern, N. A., and K. See Tan. 2020. U.S. ICU resource availability for COVID-19. Society of Critical Care Medicine. https://sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID19/United-States-Resource-Availability-for-COVID-19.pdf?lang=en-US.
Further assignment of responsibilities to teams may be needed and can include proning/rolling teams, airway teams and rapid intervention teams, vascular access teams, and others that the facility may not normally use. In particular, rapid intervention and airway teams have been in high demand in facilities experiencing surges, often responding to multiple calls each hour. CRNAs have been used successfully in several hospitals to provide staffing for these intervention teams along with other anesthesia and emergency medicine staff.
Respiratory therapists (RTs) are in significant demand and do not have correlate staff who can “step up” into their roles. Their hospital responsibilities should be closely examined and tailored to maximize their time spent performing ventilator set-up and addressing the needs of ventilated patients in areas where staff may not be comfortable with ventilator operations. Critical care and anesthesia staff, as well as CRNAs and other providers, will need to ensure that they know how to operate the ventilators in their area and be able to make necessary adjustments and respond to device alarms. Any responsibilities not related to ventilator management (e.g., giving nebulizer treatments, checking oxygen saturations, induced sputum collection) should be curtailed and/or assigned to other providers to allow them to focus on life-critical issues while presenting minimal risk for those other duties taken on by others.
In some cases, state laws and collective bargaining agreements have direct influence on staffing ratios and duties. These issues and the complex dynamics that underlie them should be anticipated and appropriate resolution sought in advance of the need to implement these changes.
Application of Telemedicine
Telehealth and telemedicine capabilities, which have become a mainstay of health care service delivery during the initial phases of the response to COVID-19, could have largely been employed in the out-of-hospital setting in order to maintain some degree of care delivery for
ambulatory-based practices. These same tools could be employed within the hospital for the direct medical oversight and management of selected patients, including critical care patients. A number of large medical systems have been deploying tele-critical care services that could be expanded and assist under circumstances where staffing shortages, especially physician shortages, might exist. While there is no substitution for bedside care delivered by nurses, technicians, and other health professionals, telemedicine could be used to manage some of the concerns related to real-time patient care physician oversight and allow community hospitals to broaden their scope of services and allow them to more effectively assist with “load balancing” ventilated patients who require continued respiratory support and weaning. Wearables and other digital health technologies could also be used to support the out-of-hospital management of infected patients who may not need hospitalization, but still require close medical monitoring.
ASSESSING IMPLEMENTATION OF STRATEGIES
Many facilities will make staffing requests based on conventional staffing ratios while some will make requests based on adjusted ratios or changed practices such as a tiered staffing model. Furthermore, some of these facilities may have elective cases that continue to occupy staffing resources and generate additional inpatient case volume. Some of the following questions may be helpful to assess staffing requests:
- Has the facility fully curtailed elective services?
- Have staff been re-deployed from procedural care to inpatient support?
- Have internal personnel been re-assigned from administrative to clinical duties as appropriate?
- Have health care coalition and health care system staff been requested and deployed?
- What contract agency staffing support has been obtained? If contract support is not available which agencies were contacted?
- What is the current ICU nurse to patient staffing ratio?
- Has a tiered supervision (team-based) strategy been implemented? What would be the threshold to do so?
- Have community and state resources been exhausted? (e.g., the Medical Reserve Corps, the National Guard, including 68W personnel, state-based teams)
- Have regional DoD and VA assets been engaged both to assist with level-loading but also with potential staffing support?
- Are federal assets available for deployment?
This information could be valuable at the health care coalition level to ensure that hospitals are providing a consistent approach and at a similar point on the crisis spectrum. If key staffing differences exist among hospitals, this may be as important a driver of load balancing of patients as the raw number of patients at a facility, but is likely to not show up in the usual elements of information. Often, “staffing” numbers collected have no comparator by which to judge how staff are being used. In order to most effectively utilize staff across facilities, staffing figures should be presented alongside ratios and other elements of information necessary for a common operating picture.
DETERMINING A NEED TO MAKE REQUESTS FOR STAFFING ASSISTANCE
Little guidance exists on when to request staffing assistance and how those requests should be prioritized. Based on the information above, the following could assist health care coalitions and other entities considering a large number of staffing needs versus a small number of deployable staff by helping to consider what has already been done and exploring any potential adjustments to be made locally that will inform the specific needs for staffing assistance.
- Has the community implemented maximal disease control measures to reduce future cases?
- What is the current request based on (assumptions of demand, ratios, etc.)?
- Is the current staffing considered contingency or crisis and why?
- Is any triage of critical care resources occurring due to shortages of staff (e.g., ECMO, ICU beds)?
- Is “level loading” implemented and if so, is there a potential to reach further geographically (e.g., would additional EMS resources enable further transfers)?
- Have elective procedures ceased not only for the facility but also across the coalition and area?
- Have the facility and system re-deployed their personnel maximally from elective and administrative?
- Have the facility and system implemented a tiered supervisory staffing model or significantly changed their staffing ratios?
- Is there other evidence (e.g., ventilators in use as a percent of inpatients, percentage of critical care patients of overall census) that a hospital or area is disproportionately impacted compared to another?
- Have the facilities exhausted contracting options? (This may involve checking with and comparing some agencies and regions.)
- Have other personnel (e.g., the National Guard) already been integrated to support hospital care?
CONCLUSION
The availability of trained staff, more than any other element, will likely continue to be the biggest challenge of COVID-19 hospital care. Training programs should be encouraged to include critical care elements for both medical and nursing students. Current providers should receive just-in-time education on the “step up” knowledge and roles that they will need.
Hospitals and health care coalitions should proactively manage inpatient volumes across their catchment area and also should share information to ensure that staffing strategies across their area are consistent. If not, this may help drive further load leveling or help guide the distribution of staffing resources. Many techniques may be implemented at the community and hospital level, but the most important is a shift to a team or “consultation”-based paradigm in which the critical care providers supervise, rather than provide, bedside care. Employing the use of telehealth and telemedicine services could be a key support for this transition in many hospitals.
Figuring out which providers to place in new roles and helping staff understand the triggers, which may be volume or staffing based, at the facility for implementing a team-based care model will be important to making this pivot most effective. Multiple staffing requests across a region or among states create challenges and necessitate gathering subjective information about how staff are being used in order to assess the state of current operations, adaptations, and judge the effectiveness of resource support.
OTHER RESOURCES
Department of Health and Human Services Assistant Secretary for Preparedness and Response. 2020. TRACIE Novel Coronavirus Resources. https://asprtracie.hhs.gov/COVID-19. Includes a variety of training, on-boarding, and other resources relevant to staffing, MOCCs, and other health care COVID-19 operations.
Department of Health and Human Services Assistant Secretary for Preparedness and Response. 2020. TRACIE Workforce Virtual Toolkit: Resources for Healthcare Decision-Makers Responding to COVID-19 Workforce Concerns. https://asprtracie.hhs.gov/WorkforceVirtual-Toolkit. Includes a variety of resources relevant to surge planning, regulatory and funding flexibilities, liability, licensure, and training.
Einav et al. 2014. Surge capacity logistics: Care of the critically ill and injured during pandemics and disasters: Chest consensus statement. Chest 146(4 Suppl):e17S–e43S. Provides additional information around staffing and other critical care strategies.
Hick et al. 2020. Duty to plan: Health care, crisis standards of care, and novel coronavirus SARS-CoV-2. Washington, DC: National Academy of Medicine. https://nam.edu/duty-toplan-health-care-crisis-standards-of-care-and-novel-coronavirus-sars-cov-2. Provides hospital planning information, including staffing relevant to CSC during COVID.
APPENDIX A
Triggers, Tactics, and Resources
In the 2013 Institute of Medicine report Crisis Standards of Care: A Toolkit for Indicators and Triggers, the committee identified several potential indicators related to staffing that have been seen in recent months in various areas of the United States. The table below (adapted from Tables 3-1, 7-1, 8-1, and 9-1 in that report) outlines the indicators and triggers, potential tactics to respond, and recent real-world examples from the COVID-19 response.
| Indicator or Trigger | Response Tactics | Practical Examples and Resources |
| Increasing staff requirements in the face of increasing demand Lack of qualified staff for specific cases | Tailor responsibilities to expertise, diverting nontechnical or nonessential care to others | ASPR TRACIE: COVID-19: Healthcare System Operations Strategies and Experiences Hospital Roles and Responsibilities in Healthcare Coalitions |
| Texas: Movement of NonCritical Patients in Face of Hurricane | ||
|
Activate plans for mutual aid or other means of supplementing human resources, including the use of support personnel for all noncritical tasks Obtain staff from coalition and system partners, contract entities, and other sources Recruit and credential staff from volunteer (Medical Reserve Corps [MRC], Emergency System for Advance Registration of Volunteer Health Professionals [ESAR-VHP]) or federal sources (Disaster Medical Assistance Team [DMAT], other National Disaster Medical System [NDMS] sources, etc.) |
ASPR TRACIE: Establishing Medical Operations Coordination Cells (MOCCs) for COVID-19 | |
| Establish remote consultation of specialized services such as telemedicine, phone triage, etc., if possible |
University of Pennsylvania COVID Watch Leveraging Digital Health Technologies During Large-Scale Epidemics |
|
| Out-of-hospital sector staff are being asked to volunteer (e.g., MRC) to provide care to higher acuity patients (e.g., alternate care sites and hospital surge) |
Adjust staffing hours and routines to accommodate more patients Implement “step-up” staffing model |
US ICU Resource Availability for COVID-19 |
| Decrease in worker functional capacity including, but not limited to: | Intensify stress management and resilience promotion training and activities (e.g., | NAM Action Collaborative on Clinician Well-Being |
|
psychological first aid) Continue regular and accurate surveillance of stress-related issues Explore specialized consultation from content experts in workplace stress in extreme situations Implement changes in personnel policies and practices |
APPENDIX B
Acknowledgment of Reviewers
The following individuals served as reviewers: Mahshid Abir, RAND Corporation; David Asch, University of Pennsylvania; Christine Cassel, University of California, San Francisco, Kaiser Permanente School of Medicine; Bernard Lo, University of California, San Francisco; and Nicole Lurie, CEPI. Bobbie A. Berkowitz, Columbia University School of Nursing; Ellen Wright Clayton, Vanderbilt University Medical Center; and Susan Curry, University of Iowa, served as arbiters of this review on behalf of the National Academies’ Report Review Committee and their Health and Medicine Division.
This activity was supported by a contract between the National Academy of Sciences and the U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response (75A50120C00093). Any opinions, findings, conclusions, or recommendations expressed in this publication do not necessarily reflect the views of any organization or agency that provided support for the project.
Copyright 2020 by the National Academy of Sciences. All rights reserved.
















