Costs, Values, and Reimbursement Issues Associated with Various Birth Settings
At several times during the course of the workshop discussion, participants commented on the need to consider the economic drivers of decision making around birth settings. While perceived health risks clearly impact both patient and provider decision making, so too do cost, value, and reimbursement issues. Moderated by Jeannette Rogowski, Ph.D., University of Medicine and Dentistry of New Jersey, Piscataway, New Jersey, Panel 6 participants considered some of these issues. This chapter summarizes the information that was presented and discussed in that panel. Box 7-1 summarizes key points made by individual speakers.
REIMBURSEMENT ISSUES AND PAYMENT INNOVATION1
The Center for Medicare and Medicaid Innovation (CMMI), also known as “the Innovation Center,” was mandated by the Affordable Care Act and appropriated $10 billion for testing new payment models. Its purpose is to find new ways to leverage different approaches to paying for care through providers, health systems, hospitals, and states, with the ultimate goal of improving quality, improving outcomes, and reducing total cost of care. While the Centers for Medicare & Medicaid Services (CMS) have long employed demonstration projects, CMMI provides a unique opportunity to “scale up” to the national-level models that demonstrate reductions in cost and no change in quality, or improvement in quality and no change
______________________________________
1This section summarizes information presented by William Shrank, M.D., M.S.H.S., Center for Medicare and Medicaid Innovation, Baltimore, Maryland.
BOX 7-1
Costs, Values, and Reimbursement Issues Associated with
Various Birth Settings
Key Points Made by Individual Speakers
- Medicaid is a major payer for births in the United States, paying for approximately 40 percent of all births nationwide. Medicaid also pays for many poor birth outcomes. To sustain itself, Medicaid is seeking ways to reduce costs. William Shrank discussed the wide range of new payment models being tested by the Center for Medicare and Medicaid Innovation (CMMI), also known as “the Innovation Center.” Many of these models impact perinatal care.
- After a decades-long history of state laws, regulations, and policies enacted or implemented to foster collaboration between midwives and physicians, Laurie Cawthon suggested that Washington State serves as a model for varied birth settings. She presented results from an unpublished study based on Medicaid claim and U.S. birth certificate data comparing expenditures between hospital, home, and birth center births. Expenditures for out-of-hospital births are consistently lower than for hospital births.
- While Medicaid interest in perinatal care is high, involving Medicaid in perinatal research is challenging. Kathleen Nolan identified several key challenges: data collection; state-level variation in Medicaid coverage; and the unknown impact of the shifting Medicaid landscape on pregnancy coverage.
in cost. The U.S. Department of Health and Human Services secretary has the authority to expand successful models through rule making, not legislation, leading to rapid implementation.
William Shrank described programs announced by CMMI to date (as of the time of the workshop). He stated that the Center was still in its infancy, having been established just 2 years ago, but that already it has announced a large agenda of new programs. He noted at the outset that he would describe each program’s relevancy to childbirth care but emphasized that the goal is to think more broadly about “the changing incentives, the changing environment, the changing platform and what that means for all of us as we strive to improve the quality and reduce the cost of care for the patients that we serve.”
The programs announced thus far by CMMI are grouped into several categories:
• Coordinated Care
![]() Coordinated care is a central theme of the Affordable Care Act and was written directly into the CMMI statute, that is, that CMMI should emphasize new programs that attempt to im-
Coordinated care is a central theme of the Affordable Care Act and was written directly into the CMMI statute, that is, that CMMI should emphasize new programs that attempt to im-
prove care coordination for the beneficiaries being served. There are two types of coordinated care programs: Accountable Care Organizations (ACOs), which include the Pioneer ACO Model and the Advance Payment ACO Model; and the Primary Care/Medical Home models, which are patient-centered models that emphasize and realign incentives for primary care physicians.
• Right Care
![]() Right care programs are focused on improving incentives to optimize outcomes and reduce costs for providers who are delivering acute care services. For example, the Bundled Payment for Care Improvement model is a bundling of hospital services to help realign incentives for hospitals to deliver higher-quality, lower-cost care.
Right care programs are focused on improving incentives to optimize outcomes and reduce costs for providers who are delivering acute care services. For example, the Bundled Payment for Care Improvement model is a bundling of hospital services to help realign incentives for hospitals to deliver higher-quality, lower-cost care.
• Innovation Infrastructure
![]() CMMI is investing in infrastructure to help train the next generation of leaders of health reform innovation. The programs include the Innovation Advisors Program and Healthcare Innovation Challenge.
CMMI is investing in infrastructure to help train the next generation of leaders of health reform innovation. The programs include the Innovation Advisors Program and Healthcare Innovation Challenge.
• State/Medicaid/Duals
![]() CMMI has announced several activities at the state level that focus on ways to better allocate funding and align incentives.
CMMI has announced several activities at the state level that focus on ways to better allocate funding and align incentives.
• Preventive Care
![]() Preventive care models include the Million Hearts Campaign and Strong Start.
Preventive care models include the Million Hearts Campaign and Strong Start.
Coordinated Care
Pioneer ACO Model
Shrank described several of the Coordinated Care models, beginning with the Pioneer ACO Model, which he observed has received significant media coverage. The goal of this initiative is to test the transition from a shared-savings payment model to a population-based payment model. In a broader sense, the goal is to transition to a health system that provides the full range of care for the beneficiaries it serves—a system that is responsible for all patient care and accountable for the total cost of care. Such a model requires that management of patient care be considered very broadly, by finding ways to reduce waste, improve coordination, improve health outcomes, and reduce downstream costs. Pioneer ACOs are reimbursed through rewards for delivering higher-quality, lower-cost care. A number of quality indicators serve as specific targets for higher remuneration. If the ACOs are able to provide higher-quality, lower-cost care to their beneficiaries and thereby reduce the total cost of care, CMS
will share the savings with them. The financial incentive is a strong incentive for perinatal care.
Shrank emphasized the importance of understanding what the evidence indicates is the best way to target, communicate, and work with patients and deliver them to the childbirth site that best meets their needs and preferences and delivers the best outcome at the lowest cost.
Advance Payment Model
According to Shrank, Pioneer ACOs are more advanced than other health systems with respect to already being well on their way to providing coordinating care. Advance payment programs, on the other hand, are generally rural ACOs that may not even have a main hospital or the other pieces required to deliver the full range of care. To help these models advance, CMS provides them with up-front capital to help recruit and otherwise invest in building the necessary infrastructure.
Comprehensive Primary Care Initiative (CPCi)
CPCi is committed to studying how to improve the role of the primary care doctor and delivery of care to patients by empowering doctors with opportunities to make more decisions and with resources for building the infrastructure needed to deliver comprehensive care. CPCi is a multipayer initiative, with all payers investing in comprehensive primary care and with Medicare paying approximately $20 per beneficiary per month to improve care coordination. On the front end, Shrank explained, the initiative helps physicians invest in delivering higher-quality and more efficient primary care, for example by hiring a nurse practitioner to help people with diabetes better manage their blood sugars or by hiring a pharmacist to help patients better adhere to their medications or understand drug side effects. On the back end, the initiative is a shared savings model.
In Shrank’s opinion, the CPCi model is an incentive for primary care physicians to think on a more “global” level about prevention and to deliver primary care in a holistic, coordinated way. The hope is that following patients more closely will reduce the total number of office visits (e.g., by handling issues via better management or over the phone or through e-mail), thereby reducing total cost of care. Medicare will pay a large portion of the difference.
With respect to relevancy to perinatal care, Shrank observed that such a model, whereby the primary care physician is accountable for care of the entire patient, would present opportunities for primary care physicians to play a role in facilitating early and appropriate obstetrician/gynecologist participation.
Right Care Initiatives
The Innovation Center is testing three right care initiatives: Partnership for Patients, Community-Based Care Transitions, and Bundled Payment for Care Improvement.
Partnership for Patients
The Partnership for Patients model is slightly different than the Innovation Center’s other models, which are generally focused on a specific new payment for doctors, health systems, or hospitals. It is a national campaign to promote healthier, safer care in hospitals, with very aggressive goals to reduce preventable hospital-acquired conditions and reduce readmissions. At the time of this workshop, nearly 4,000 hospitals, or about 75 to 80 percent of all U.S. hospitals, had signed the pledge to participate. The program’s main goal is to test and share approaches to improving the safety of care, which ultimately will lead to cost reduction. Shrank described the model as a “learning collaborative.” He observed that, with respect to perinatal care, there are a number of ways that the safety and cost of obstetric care could be improved, for example through the use of checklists.
Community-Based Care Transition Program (CCTP)
The Innovation Center has invested $500 million in CCTP to date (at the time of the workshop), through which community-based organizations play a unique role in helping transition patients from a hospital to a home or other outpatient setting. Shrank observed that there is likely a unique opportunity for CCTP to improve perinatal care, particularly during that time of transition when new parents take their baby home from the hospital for the first time. Shrank said, “Everyone says … ‘I didn’t get the handbook.’ … There’s unquestionably a unique opportunity here to help new parents at that time of transition to maintain the safety.”
Bundled Payments for Care Improvement
The Bundled Payments for Care Improvement model is one of the Innovation Center’s largest models. Historically, at least over the past 20 years, CMS has bundled the cost of a hospital stay, but with providers billing CMS as much as possible (i.e., for multiple referrals, etc.). The Bundled Payments for Care Improvement model is based on bundling for the entire care episode, so not just for the inpatient phase of care but also for the post-acute care period. The goal is to ensure that hospitals have incentive to bill CMS not as much as they can, but only for what is appropriate.
If, in so doing, a hospital is able to reduce the cost of care, it will receive a share of the savings. Hospitals are also rewarded for providing higher-quality care. That is, if patients are readmitted within 30, 60, or 90 days, the hospitals have to pay. Shrank explained, “There is a whole new level of accountability for [hospitals] to make sure that when those patients are sent home, they are sent home with a good plan.” Currently (i.e., at the time of the workshop), none of the program bundles are focused exclusively on childbirth. However, Shrank said that the program was announced only very recently and that it would likely evolve in the years to come.
State/Medicaid/Duals
The Innovation Center has announced many programs aimed at reducing spending on dually eligible patients (i.e., patients eligible for both Medicare and Medicaid) by coordinating payments. Shrank observed that, as states try to innovate and transform the models that they use to pay for care within their states, it would be short sighted not to include childbirth as an important target, given that such a large amount of Medicaid spending is focused on childbirth and perinatal care.
Conclusion
In conclusion, Shrank emphasized that efforts at the Innovation Center are aimed at the whole continuum of care. Whether the focus is on primary care physicians, hospitals, health systems, or the state, all of its efforts are aimed at realigning incentives to reward providers for delivering higher-quality and lower-cost care and improving health outcomes. Perinatal care is an important component of almost all of the delivery transformation models being tested by CMMI.
ASSESSING COSTS OF BIRTHS IN VARIED SETTINGS2
Before reporting on the costs of births in varied settings in Washington State, Laurie Cawthon provided some “quick facts” on the births themselves. In 2011, about 87,000 births were reported in the state of Washington, 3.1 percent of which occurred at homes or in birthing centers. Like the United States overall, out-of-hospital births have been increasing in Washington State. From 2004 to 2011, the number of home births nearly doubled, with the proportion of home births increasing from 1.1 to 1.9 percent of total births. From 2000 to 2011, the number of births in free-
______________________________________
2This section summarizes information presented by Laurie Cawthon, M.D., M.P.H., Washington State Department of Social and Health Services, Olympia, Washington.
standing birthing centers also nearly doubled, with the proportion of such births increasing from 0.7 to 1.2 percent of total births.
Cawthon said Medicaid covers 50 percent of total Washington births, with Washington being 1 of about 11 states with Medicaid reimbursement for direct entry midwives. In many ways, she suggested, Washington is a model for varied birth settings, with many state laws, regulations, and policies enacted or implemented over the past 30 years and with collaboration between midwives and physicians.
In 1989, the state faced a crisis in maternity care access. While midwives were welcomed to the ranks of prenatal care providers, at that time Medicaid did not reimburse for home births attended by any provider type. Out-of-hospital births remained a contentious issue throughout the 1990s. The Washington State Department of Social and Health Services Planned Home Births report, Planned Home Births: Outcomes Among Medicaid Women in Washington State (Cawthon, 1996), received sharp criticism. Not until 2001 did the state Medicaid agency begin reimbursing for planned home births. Vaginal births after Cesarean deliveries, multiple gestation, and breech births that occurred in home settings were excluded from Medicaid reimbursement.
Analysis of Medicaid Expenditures
Cawthon described results from an intent-to-treat analysis (unpublished data) based on the premise that pregnant women who sought prenatal care from licensed midwives were planning, or at least considering, out-of-hospital births. The cornerstone of the analytical methods used by Cawthon and colleagues at the Washington State Department of Social and Health Services was individual record linkage of Medicaid claims and vital records. They used attendant-at-birth and birth-place-type items from the birth certificate to identify birth attendant licensure or specialty (medical doctor/doctor of osteopathy, hospital administrator, certified nurse midwife [CNM]/certified midwife, other midwife, other) and place of birth (hospital, freestanding birth center, home birth, clinic or doctor’s office, other); they independently verified provider credentials using licensure data provided by the state.
They classified providers of out-of-hospital births into three mutually exclusively categories based on the typical location of where their deliveries occurred: home birth providers (providers who delivered at least 75 percent home births), birthing center providers (providers who delivered at least 75 percent birthing center births), and providers mixed (providers who delivered babies in both settings). Data collected from 2010 to 2012 showed home birth providers included 72 licensed midwives (LMs) and 8 CNMs; birthing center providers included 16 LMs and 1 CNM; providers mixed
included 33 LMs and 5 CNMs. For all out-of-hospital births, there were a total of 121 LMs and 14 CNMs. Cawthon noted that, in 2011, there were 1,674 home births and 1,006 birthing center births in Washington State.
The researchers identified prenatal care providers using Medicaid claim codes and assigned the women who they cared for into one of six categories: perinatologists (N = 3,544), all other Medicaid (N = 105,785), home birth providers (N = 598), birth center providers (N = 642), providers mixed (N = 911), and CNMs at hospitals (N = 16,653).
Cawthon presented data for both achieved birth and intended place of birth. The difference is illustrated by the fact that, for example, although 598 women received prenatal care from a provider identified as a home birth provider, only 410 (68 percent) actually achieved a home birth. Data for those who intended a home birth and those who achieved a home birth were analyzed separately.
Expenditure data based on Medicaid claim data were computed for both the achieved birth and the intended place of birth groups. The researchers collected Medicaid expenditure data from all Medicaid claims between 270 days prior to delivery and the second postpartum month.
Results of Achieved Birthplace Analysis
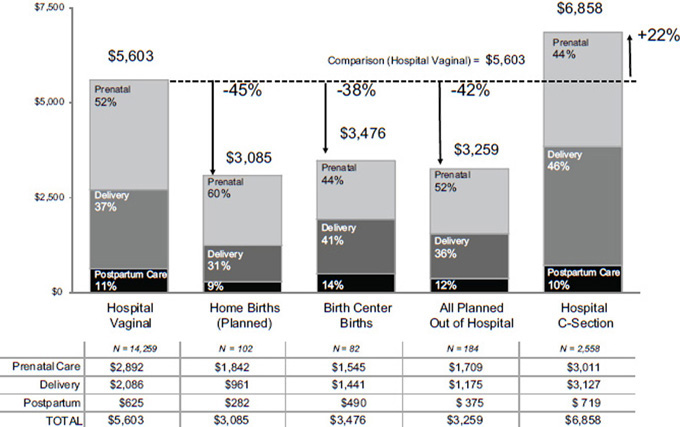
See Figure 7-1 for a breakdown of the expenditure results for low-risk women who gave birth in the various locations. The “all planned out of hospital” group is the sum of the home birth and birth center groups.
The researchers used birth certificate criteria to identify low-risk women. Specifically, they identified low-risk births as singletons that were delivered at term (37 to 41 weeks), and no indication of risk factors (based on check boxes on the birth certificate).
In Cawthon’s opinion, what is remarkable about the results depicted in Figure 7-1 is that, despite the very small denominators, expenditures for the various out-of-hospital birth groups are actually quite consistent and consistently lower ($3,085 for planned home births, $3,476 for birth center births, $3,259 for all planned out-of-hospital births) than those for the hospital birth groups ($5,603 for hospital vaginal births, $6,858 for hospital Cesarean deliveries). With respect to comparison groups, Cawthon said that they “struggled” to find appropriate comparison groups. Because no Cesarean deliveries occur at home, they decided the appropriate comparison group was vaginal births in the hospital. But they also examined hospital Cesarean deliveries. The data are fee-for-service data only. Washington has a large managed care component to their Medicaid program; this type of analysis does not work well for that type of managed care data due to the leveling of expenditures.
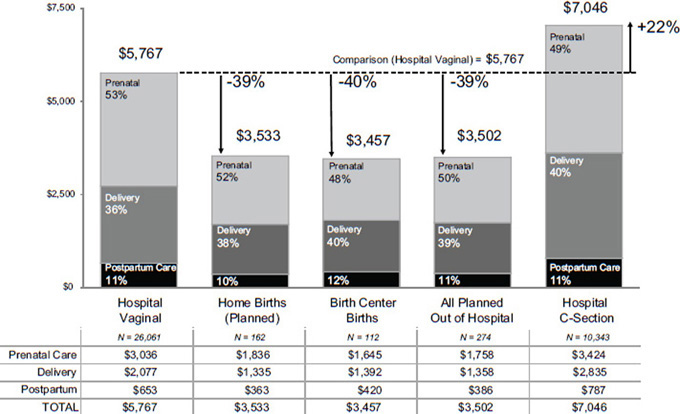
When all births, not just low-risk births, are included in the analysis,
the pattern is remarkably similar, Cawthon observed (see Figure 7-2). Also remarkable, in her opinion, is how small the added expenditure is when all births are included. The average expenditure for the hospital vaginal delivery group, the smallest group, was $5,767, representing only an incremental difference (compared to $5,603 for low-risk births); for the hospital Cesarean deliveries group, it was $7,046, again representing only an incremental difference (compared to $6,858 for low-risk births).
Results of Intent-to-Treat Analysis
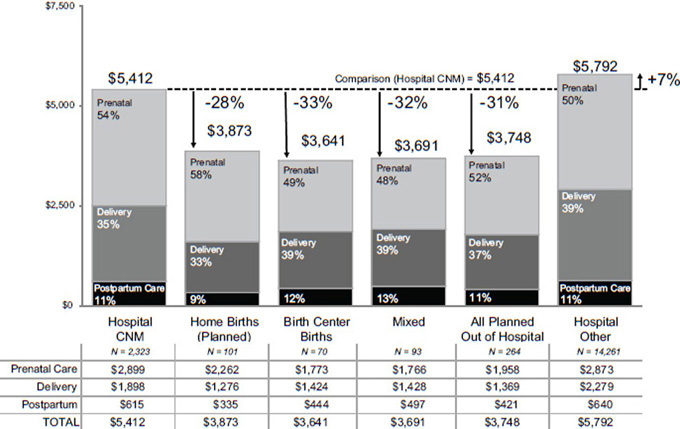
Cawthon and colleagues used different comparison groups for the intent-to-treat analysis (see Figure 7-3). Because they also tracked CNMs who delivered primarily in hospitals, they decided that a better comparison group than all hospital deliveries would be hospital deliveries for which women received prenatal care from a CNM (“hospital CNM”). Because this was an intent-to-treat analysis, Cesarean deliveries could have occurred in any group. The direct cost of Cesarean deliveries was included in overall expenditures. The researchers used the same definition of low risk that they used in the previous analysis. Cawthon observed that, remarkably, the costs were comparable to those computed in the first analysis: $5,412 for the hospital CNM group, $3,873 for the planned home birth group, $3,641 for birth center births, $3,691 for the mixed provider group, $3,748 for the all planned out-of-hospital group, and $5,792 for the “hospital other” group.
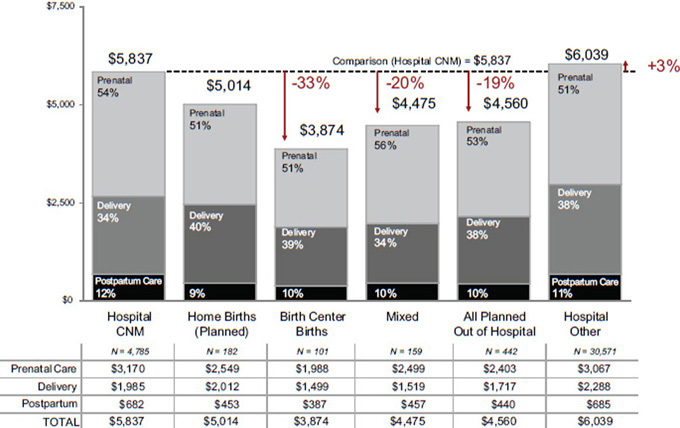
When they removed the low-risk constraint and examined all births, there was a slight shift in the pattern although, overall, not a great increase in Medicaid expenditures (see Figure 7-4). For the hospital CNM cases, average expenditure increased from $5,412 to $6,039. For the “hospital other” group, average expenditure increased from $5,792 to $6,309. For the birth center births group, savings (compared to the hospital CNM group) are exactly the same: a 33 percent in overall expenditures. For the planned home birth group, savings are not as great. Cawthon said that she was unsure as to why.
Cesarean delivery rates for the intent-to-treat groups show a dramatic reduction among the out-of-hospital groups compared to the “hospital all” group, for which the rate was 27.9 percent. The Cesarean delivery rate for home births was 9.4 percent; for birthing center births, 11.4 percent; for mixed providers, 12.2 percent; for all out-of-hospital births, 11.6 percent; for hospital CNM, 20.2 percent; and for hospital births with no CNM prenatal care, 29.4 percent. Cawthon remarked on the noteworthiness of the reduction in Cesarean delivery rates among hospital births to women who received prenatal care from a CNM compared to women who did not receive CNM prenatal care. In Cawthon’s opinion, the benefits of lower Cesarean delivery rates are not limited to reduced direct and immediate costs.
Limitations of Analyses
These analyses have several limitations. For example, the analysis did not reveal which aspects of delivery accounted for the lower Cesarean delivery rates or whether in some cases outcomes would have been better if Cesarean deliveries had been performed. There are several ways that the assessment of the costs of birth in varied settings can be improved. Cawthon encouraged other states with linked Medicaid claims and vital record data and with Medicaid reimbursement for out-of-hospital births to conduct similar analyses. By extending the analysis to other states, sample sizes and denominators would increase and some statistical power issues could be resolved. Also by extending the analysis to other states, it might be possible to study different models of care and reimbursement and describe other insurance issues.
Additionally, Cawthon encouraged more sophisticated types of analysis. For example, she and her colleagues did not adjust for risk factors other than by excluding high-risk women and by excluding a single outlier (based on infant medical care cost). The use of medical record review data or a detailed analysis of claims data could be used to identify the timing of the transfer of care and emergency transport expenses. Finally, to gain a broader perspective on cost of care, Cawthon suggested examining, in addition to expenditure data, costs of birth outcomes that are not recorded in immediate and direct Medicaid expenditures.
COST, VALUE, AND REIMBURSEMENT ISSUES: THE MEDICAID PERSPECTIVE3
Kathleen Nolan was invited to share her thoughts on issues raised by William Shrank and Laurie Cawthon. She emphasized that Medicaid is a major payer for births in the United States, paying for approximately 40 percent of all births nationwide. Medicaid also pays for many poor birth outcomes. Nolan observed that it has been generally accepted that Medicaid cannot be sustained in the future without efforts at cost containment and greater care coordination. Thus, as Shrank described previously, there is a great deal of work being done at the state level on delivery system and payment reform. Notably, a number of multipayer initiatives are under way. While long-term care is the most costly set of services in Medicaid, it does not have “a lot of resonance” with private payers, according to Nolan. Perinatal care, on the other hand, is an area where multipayer initiatives, with Medicaid involvement, might be especially applicable. Nolan
______________________________________
3This section summarizes information presented by Kathleen Nolan, M.P.H., National Association of Medicaid Directors, Washington, DC.
also noted the large number of mothers in managed care, which has some potential pluses with respect to the role that Medicaid can play. For all of these reasons, Nolan said, “Medicaid is a great opportunity to move this agenda forward.”
While Medicaid interest in perinatal care is “high,” involving Medicaid also represents a challenge. First are data collection issues, which Nolan observed that many other workshop speakers had already addressed. Compounding the data collection challenges are the many health and environmental challenges to leveraging the Medicaid population. Many women enrolled in Medicaid are in poor health. Also, they are more likely to be poor and have fewer resources in their lives, not just in health care, and to live in unsafe neighborhoods where midwives might not want to travel. Additionally, it is not uncommon for Medicaid women who are pregnant to not show up for perinatal care until late in their pregnancy.
Another challenge is that pregnancy coverage may be shifting in the future. Currently, Nolan reported, states must cover pregnant women with incomes up to 133 percent of poverty. About 20 states cover pregnant women with incomes at or above 185 percent of poverty. Although the Affordable Care Act froze these eligibility levels from 2009 to the present, in 2014 states can either raise or lower (not below 133 percent of poverty) their eligibility income criteria. The future consequences of this are unclear. It might mean that women will be circling in and out of Medicaid, with what Nolan described as a “lot of churn” among pregnant women. Not only will there be a lot of churn, but it will vary from state to state.
Nolan emphasized state variation in Medicaid coverage and in other important features of health care oversight. It is not just eligibility levels that vary, but all of the other components of Medicaid. In addition to Medicaid state-level variation, health facilities oversight and regulation vary as well, likewise with professional regulation and community norms. Such substantial state-level variation makes establishing a national agenda for a perinatal care delivery system and payment reform very difficult.
In summary, Nolan reiterated three key challenges: (1) data collection challenges, (2) state variability, and (3) the shifting Medicaid landscape. In her opinion, the temptation is to say that Medicaid should cover home birth. But Medicaid covering home birth does not mean that “all of the other pieces will be there in place for that to move forward.” Mandating coverage for home birth nationwide could be detrimental, as it could fail to recognize the different state environments and preparedness for this kind of shift. Nolan encouraged the sharing of best practices and moving forward collaboratively.
DISCUSSION WITH THE AUDIENCE4
At the end of Panel 6, members of the audience were invited to comment on issues raised or ask questions of the panelists. Topics covered included the need to improve outcomes in hospital settings, the dominant role of physicians in the U.S. health care system, the challenge of decreasing costs in a for-profit system, the challenge of measuring actual cost of care, payment reform and perinatal care, “supervision” language used by Medicaid, and Medicaid reimbursement for midwives.
Improving Outcomes in Hospital Settings
A member of the audience observed that the focus of the workshop discussion should be on improving the quality of all birth settings, not just home birth settings. Many steps could be taken now to improve outcomes in hospital settings, based on the evidence. Another audience member agreed and asked whether and how Medicaid payment incentives were being altered to encourage and maximize “normal physiologic birth” in hospitals. Kathleen Nolan replied that numerous initiatives are under way to accomplish that goal. She mentioned William Shrank’s descriptions of the many Innovation Center initiatives aimed at increasing accountability and value-based purchasing. She reiterated her opinion that, rather than simply saying, “there needs to be more home birth,” discussing ways to improve quality and improve value is the more salient conversation and would attract more interest from Medicaid. She cautioned, however, that Medicaid “can’t always be the only lever.” She suggested that multipayer initiatives present more opportunities for forward movement.
Dominant Role of Physicians in the U.S. Health Care System
An audience member expressed concern about the dominant role of physicians within the U.S. health care system, whether it be in hospitals, health insurance companies, malpractice insurance companies, or elsewhere, and the way that the American Medical Association has nurtured that role by discouraging support of nonphysician providers. She encouraged those who are thinking about ways to help the system function better to think beyond the realm of “just physicians.” Caitlin Cross-Barnet responded that the CMMI has been examining midlevel providers. For example, two of the Strong Start initiative models, the birth center model and the centering/group care model, focus on non-physician-based care. She cautioned, how-
______________________________________
4This section summarizes the discussion that took place at the conclusion of Panel 6, immediately following Nolan’s presentation.
ever, that midwifery does not always save the system money. In some states, midwives are reimbursed at the same level as physicians. But if midwives are reimbursed at a lower rate, then it does save money.
The Challenge of Decreasing Costs in a For-Profit System
A member of the audience asked how the “inherent conflict” of decreasing costs in a for-profit system can be resolved. Two panelists commented. Cross-Barnet commented on Medicare’s success in delivering more economically efficient health care and providing results compared to other health care delivery models. She wondered why there is not a broader public embrace of the program, given its success. Kathleen Nolan mentioned that there have been some conversations on this very issue, specifically the value purchasing conversation that CMMI and others are having. The value purchasing conversation in Medicaid is similar to the one in Medicare, and focused on payment alignment and incentives for quality, rather than whether it is a for-profit or nonprofit model.
The Challenge of Measuring Actual Cost of Care
A comment was made that measuring actual cost of care would yield a more accurate measure of care delivery than billable charges and Medicaid reimbursements. The commenter also challenged researchers to consider cost to the patient, not just cost to the government or to health care organizations. Nolan responded that measuring actual cost of care in hospitals is challenging but that growing interest in value purchasing has increased the desire to understand those costs. She noted that a couple of states have tried to take a closer look at actual cost of hospital care.
Payment Reform and Perinatal Care
An audience member commented on the growing number of organizations considering the use of bundled payments. She asked the panelists to comment on the use of bundled payments in perinatal care. Cross-Barnet replied that some prenatal care is already being bundled, with a set fee for prenatal care plus birth delivery; but that it is unclear how the bundling is impacting quality of care. Nolan added that there is plentiful opportunity in perinatal care to share best practices and find the best approach and then incorporate that approach into ongoing initiatives in payment reform.
“Supervision” Language Used by Medicaid
A member of the audience commented on the inability of a certain home birth services organization staffed by certified nurse-midwives to provide Medicaid care to their clients because of the “supervisory” language used in the Medicaid application. Specifically, the application required that a supervisory physician be present. She asked whether there is any federal-standard application that replaces “supervision” language with “collaboration” language. Nolan responded that there is no federal standard for use of “supervisory” language. Use of that language varies state by state, with respect to both practice laws and state Medicaid programs, and the two are not necessarily aligned (e.g., even though a state’s licensure laws might not require supervision, its Medicaid program might).
Medicaid Reimbursement for Midwives
A member of the audience clarified that there is a federal mandate that all state Medicaid programs reimburse nurse-midwives, regardless of where those births occur (at home, in a birth center, or in a hospital). Cross-Barnet added that Medicaid is mandated to pay for licensed midwifery care, that is, any midwife who is licensed in her or his state, but that other factors, like malpractice insurance, may restrict the care that licensed midwives are actually able to provide. To further clarify, Medicaid only reimburses midwives for care in certain settings, so while they do have to provide licensed midwives with reimbursement, they do not necessarily have to pay for home birth, though some states do.