Assessing the Science Behind Methodologies Being Used to Characterize Food as Addictive
Nutrition researchers are beginning to rely on data from neuroimaging studies and self-report questionnaires to answer questions about how food and food cues impact eating behavior. This chapter summarizes the workshop presentations and discussion that revolved around the use of neuroimaging and the Yale Food Addiction Scale (YFAS) (a self-report questionnaire for identifying “addictive eaters”) to characterize eating behavior (or food) as addictive and addictive-like. To start the session, moderator Richard Mattes of Purdue University provided a brief historical overview of energy intake research and the shift in focus toward eating behavior. Box 3-1 highlights key points made by speakers during this session.
A BRIEF HISTORY OF FOOD INTAKE RESEARCH1
Although scientists continue to debate whether the nation’s obesity problem is driven primarily by changes in energy expenditure versus energy intake, Mattes opined that enough evidence exists to support the hypothesis that energy intake is the primary driver. Based on their use of the doubly labeled water method to measure human energy expenditure, Dale Schoeller, John Speakman, and Klaas Westerterp unanimously and emphatically claim that there has been no change in energy expenditure over the past 15 to 20 years (e.g., Westerterp and Speakman, 2008).
______________
1 This section summarizes introductory remarks made by Richard D. Mattes, Ph.D., M.P.H., R.D., Purdue University, West Lafayette, Indiana.
BOX 3-1
Key Points Made by Individual Speakers
- Heightened food cue responses in the brain (e.g., responses to pictures or flavors of food), as measured by functional magnetic resonance imaging (fMRI), are associated with higher body mass index (BMI) and can predict feeding behavior and weight gain. According to Dana Small, the underlying mechanism driving brain cue responsivity, at least for carbohydrates, appears to be a postingestive metabolic effect. The greater the expected metabolic effect, the greater is the anticipatory response to food cues.
- Whether neuroimaging evidence reveals anything about eating behaviors, and “food addiction” in particular, is open to debate in Hisham Ziauddeen’s opinion. Ziauddeen called attention to key assumptions underlying neuroimaging studies of eating behavior and urged caution when interpreting the study results.
- The Yale Food Addiction Scale (YFAS) is a self-report questionnaire made available in 2009 as a tool for identifying individuals who may be experiencing addictive-like responses to food. The scale is based on criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), for diagnosing substance dependence. According to Ashley Gearhardt, addictive-like eating behavior as defined by the YFAS has since been associated in many studies with eating-related problems such as higher current and lifetime BMI and emotional eating. Additionally, Gearhardt outlined how the YFAS has been associated with risk factors and mechanisms implicated in other addictive disorders, such as hyperreactivity of reward-related neural regions to food cues, higher rates of impulsivity, and elevated craving. She noted the importance of replicating existing findings and conducting longitudinal studies. She also emphasized the need to identify which foods may be more likely to trigger an addictive process in humans and suggested that highly processed foods with added fats and refined carbohydrates may be more addictive than more naturally occurring foods.
- “Food addiction” was considered for inclusion in the DSM-5 category for substance use disorder but rejected because of a lack of data, according to Charles O’Brien. O’Brien emphasized that the criteria for substance use disorder were developed based on studies of drug addiction and questioned the appropriateness of “squeezing” what is a normal behavior—eating—into a set of criteria developed for drugs.
Mattes explained that while this claim may seem counterintuitive given how much time people spend watching television and sitting in front of computer screens, people have become heavier and therefore use more energy when they do move. Additionally, when energy expenditure for a large array of terrestrial mammals is plotted against body mass, human data align with what is expected. “What we’re doing is not aberrant,” Mattes said. Thus, in his opinion, the discussion should revolve around food intake, not energy expenditure.
While limiting the discussion to one side of the equation “should be comforting,” Mattes said, “it is not.” Measuring food intake is difficult. According to a recent analysis of various iterations of National Health and Nutrition Examination Survey (NHANES) data, not a single study over the past 39 years involved a majority of respondents reporting biologically plausible energy intakes (Archer et al., 2013). That lack of plausibility has led researchers to seek other predictors of intake for use in their studies.
According to Mattes, during the 1950s to 1970s, nutrition research as related to ingestion behavior focused primarily on macronutrients and other factors that tend to influence intermeal interval, not meal size. The focus during the past 15 to 20 years has shifted to gut peptides and their role in controlling meal size (Blundell, 2001; see Chapter 2). Mattes emphasized the need to integrate what has been learned about factors that control eating frequency with what researchers are learning about factors that control portion size. “There really hasn’t been much attempt to do that,” he said. Absent those data, he observed, researchers have begun to focus more on behavior and, with the advent of new imaging technologies, neurochemistry.
All of this new behavioral and neurochemistry research has raised important questions about characterizing food as addictive. Are there special properties of foods that drive intake to a point where it exceeds energy requirements? Or are there characteristics of consumers that make them especially responsive to whatever interceptive or external stimuli they encounter? “Most likely it’s the interaction between these two,” Mattes said.
WHAT IMAGING TECHNOLOGIES REVEAL ABOUT FOOD BEHAVIORS: PERSPECTIVE 12
“The obesity epidemic is a neurobehavioral problem that stems from a vulnerable brain in an unhealthy food environment.”
—Giles Yeo
Inasmuch as the brain is a key facet of Giles Yeo’s definition of the obesity epidemic, Dana Small began, neuroimaging will be critical to understanding how the modern food environment is engaging appetitive circuits, hedonic circuits, and their interaction. Small discussed how neuroimaging research is being used to understand food cue reactivity and its role in obesity.
______________
2 This section summarizes the presentation of Dana Small, Ph.D., Yale Medical School, New Haven, Connecticut.
Food Cue Reactivity
Many neuroimaging studies have demonstrated that when shown a palatable food or presented with the aroma or taste of a palatable food, individuals with a high body mass index (BMI) or a genetic predisposition show greater responses in many regions of the brain, particularly dopamine source and target areas. This type of heightened brain-food cue reactivity is important, Small opined, because it predicts eating behavior. In a neuroimaging study in subjects shown pictures of palatable foods, for example, Lawrence and colleagues (2012) demonstrated that response to food cues in the nucleus accumbens, a key reward region of the brain, correlates with subsequent snacking behavior. Notably, this same response was unrelated to self-reported hunger. The researchers also demonstrated that in contrast, a separate circuit involving the ventromedial prefrontal cortex showed no relationship with snacking behavior but a correlation with self-reported hunger. These results demonstrate that distinct responses are associated with hedonic versus homeostatic factors related to feeding. These hedonic responses in regions that may promote eating in the absence of hunger, such as the nucleus accumbens, make sense, Small said, because people can store excess energy as fat for times of famine.
If some circuits, such as the nucleus accumbens, promote eating or are associated with eating without hunger, one would expect the activity level of those circuits to be related to susceptibility to weight gain. Indeed, in a neuroimaging study of individuals taking small sips of chocolate and vanilla milkshake, Geha and colleagues (2013) observed a correlation between responses in the nucleus accumbens, ventral pallidum, and hypothalamus in individuals and change in BMI over the course of a year. In a study of individuals participating in a weight loss trial, Murdaugh and colleagues (2012) found greater activity in the nucleus accumbens among participants who were more likely to gain weight even as they were actively trying to lose weight. Together, these results suggest that food cue reactivity is a powerful predictor of eating behavior and can be used to predict weight gain.
Regulation of Food Cue Reactivity: Importance of Postingestive Signaling
In an effort to understand what regulates food cue reactivity, Small and her research team have been using a “flavor nutrient conditioning” paradigm. Flavor nutrient conditioning has been well studied in animals, largely by Tony Sclafani and his group (Sclafani et al., 1999).
Flavor nutrient conditioning studies typically involve hungry, thirsty rats that are presented on the first day with a sipper containing a particular flavor. When the rat licks the sipper, the lick is detected, a switch is flipped,
the pump turns on, and a nutrient such as glucose is infused directly into the gut. Thus, over the course of the day, the rat has an opportunity to learn to associate the flavor in the sipper with the postingestive effects of the nutrient in the gut. On the second day, the same rat, hungry and thirsty again, is presented with a sipper containing a different flavor. This time when the rat licks the sipper, the lick is detected, a switch is flipped, the pump turns on, and a saline placebo is infused directly into the gut. Over the course of the second day, the rat learns to associate the second flavor with the lack of any postingestive effect in the gut. Then on a subsequent day, the researchers can “ask” the rat which flavor it prefers by making both flavors available and measuring intake. Sclafani and colleagues (1999) showed that rats overwhelmingly preferred a flavor associated with a glucose infusion over a flavor associated with a saline placebo.
Of importance, Small noted, other studies have demonstrated that flavors associated with noncaloric exposures do not condition preference, suggesting that a postingestive effect is necessary to elicit a response (Ren et al., 2010; Yeomans et al., 2008). Other studies also have shown that the association learning that occurs over the course of exposure is highly dependent on dopamine and that blocking dopamine in multiple regions, including in the hypothalamus, the amygdala, and the nucleus accumbens, completely abolishes the learning (Sclafani et al., 2011; Touzani et al., 2010).
While most of the evidence for a postingestive effect comes from rats, Yeomans and colleagues (2008) demonstrated that postingestive effects, but not oral signals, are necessary and sufficient for the formation of flavor preference in humans as well. Because their subjects were human, these researchers did not use the intergastric infusion method. Rather, they administered a pretest during which subjects rated flavors on how pleasant they were, and intake was measured. Then they conducted a series of exposure sessions in which subjects were allowed to associate a novel flavor with a postingestive effect. After the exposure sessions, the researchers conducted a posttest during which, once again, flavors were ranked for pleasantness and intake was measured.
The exposure sessions involved exposing participants to one of three situations. One group received a flavor plus sucrose, a condition with both postoral effects (because sucrose is caloric) and oral effects (because sucrose is sweet). A second group received the same flavor plus maltodextrin, a condition with postoral effects but no oral effects (because maltodextrin is tasteless and odorless to humans). The third group received the same flavor with aspartame, a condition with oral effects but no postoral effects (because aspartame is sweet but has no calories).
The researchers found no change before and after exposure in the ranking of pleasantness or in intake among individuals in the third group—those
exposed to the flavor plus aspartame. However, they found a slight increase in the ranking of pleasantness and a significant increase in intake among those exposed to the flavor plus maltodextrin, and the greatest response in those exposed to the flavor plus sucrose. While the greatest changes were observed when both postoral and oral effects occurred, the lack of change seen in the flavor plus aspartame group and the changes seen in the flavor plus maltodextrin group together suggest that postoral effects by themselves are both necessary and sufficient for inducing flavor-nutrient association learning and for increasing the reward value of a flavor.
Postingestive Signaling: The Role of Glucose Metabolism
Given the evidence accumulated thus far, it appears clear that some postoral effect is a critical signal for flavor-nutrient association learning. What is less clear, Small said, is the nature of such postingestive signals. Ivan de Araujo and colleagues found that intake levels of sweet tastants are controlled by glucose oxidation and its modulatory effects on extracellular dopamine levels in the striatum (Tellez et al., 2013). When mice were allowed to lick and consume glucose, dopamine levels in the striatum increased. In contrast, when mice were allowed to lick and consume glucose while simultaneously being injected with intravenous 2-deoxy-D-glucose, which blocks glucose metabolism, dopamine levels in the striatum remained the same.
These results suggested to Small that glucose metabolism might be the critical signal behind flavor-nutrient conditioning—in other words—that the metabolic impact of glucose metabolism is what drives its reward value. To test whether this is in fact the case, Small and her research team conducted an experiment designed to determine whether responses to calorie-predictive flavors—that is, responses in dopamine source and target regions in the brain—are associated with changes in plasma glucose upon exposure to various flavor-sweetener combinations (de Araujo et al., 2013). Plasma glucose was used as a proxy for glucose oxidation (if glucose is to be used as a fuel, it needs to be present in the plasma). As in the Yeomans et al. (2008) study, there was a pretest in which subjects rated stimuli on pleasantness. In this case, the subjects were presented with 10 noncaloric flavored beverages, each distinctly flavored and distinctly colored. Only those individuals who identified at least three flavors as similarly pleasant continued in the study. Also, because the researchers wanted to use maltodextrin to identify postoral effects in the absence of oral effects (because maltodextrin is flavorless but caloric), subjects who were able to detect maltodextrin were excluded from the study.
Following the pretest, data were collected over the course of four exposure days. Individuals were exposed to two different conditions on alternate
days. On two days they were exposed to one of the noncaloric flavors from the pretest (one of the three flavors that was rated during the pretest as similarly pleasant to others). On the other two days they were exposed to a caloric version of a different flavor (one of the other flavors rated during the pretest as similarly pleasant to others, sweetened with 112.5 calories of maltodextrin).
A typical exposure day involved participants arriving at the laboratory at 11:30 AM. Upon their arrival, a saliva sample was collected, participants were asked to rate their hunger, and a catheter was inserted. Thirty minutes later, the first blood sample was collected and the participants were asked to rate their hunger again. Blood samples were used to measure six metabolic markers: glucose, ghrelin, insulin, trigylcerides, haematocrit, and haemoglobin. Then the participants drank one of the flavored beverages (one day caloric and another day noncaloric). A second blood sample was taken after another 30 minutes, and hunger was rated again. The 30-minute wait was used because 30 minutes postconsumption was about when plasma glucose levels were expected to be at their maximum. Participants would then eat lunch, go home, and return for a similar round of data collection and dinner. At the end of the day, they were sent home with a bottle of flavored beverage to drink at breakfast. Thus, a single exposure day involved three opportunities to learn the association between a flavor and its postingestive effect.
After exposure, the researchers conducted a posttest rating of the pleasantness of the flavors and measured brain responses using functional magnetic resonance imaging (fMRI). They found that after exposure, the flavor to which calories had been added became more pleasant, with participants changing their rating from “like slightly” to “like moderately.” In terms of metabolic changes, exposure to the caloric flavor led to greater changes in glucose, ghrelin, and insulin. When the difference in metabolic impact between the caloric and noncaloric beverages was regressed against brain response, the researchers detected only one significant relationship among the six metabolic markers measured, and that was with glucose. In other words, the magnitude of the brain response depended on how much the maltodextrin changed plasma glucose levels during the exposure sessions. Small concluded with an overview of additional studies her laboratory is undertaking to better understand what drives food cue reactivity.
Summary
In summary, Small emphasized that heightened food cue reactivity as assessed by fMRI is associated with BMI and eating in the absence of hunger and is a reliable biomarker of susceptibility to weight gain. Determining what drives food cue reactivity will be critical to understanding how the
modern food environment interacts with the brain to promote obesity. The results obtained by Small’s research team are consistent with the hypothesis that at least for carbohydrates, brain food cue reactivity is linked to their utilization as cellular food.
In Small’s opinion, better characterization of the metabolic impact of modern carbohydrate-containing foods and beverages will improve scientists’ understanding of how those foods and beverages interact with the brain to promote obesity. Small pointed to fat and sugar combinations that have never existed in human evolution until now and to liquid calories as two examples of modern carbohydrate-containing foods and beverages. But many unanswered questions remain.
More generally, Small called for a greater focus on the brain-gut axis, for which imaging will be critical. It is time, she said, to begin integrating the characteristics of foods with their physiological effects in the body and how those physiological effects, in turn, are regulating brain circuits.
WHAT IMAGING TECHNOLOGIES REVEAL ABOUT FOOD BEHAVIORS: PERSPECTIVE 23
Whether imaging data reveal anything about food behaviors, particularly “food addiction,” is open to debate in Hisham Ziauddeen’s opinion. The answer, he said, depends on what one asks and how one asks it. The question usually is asked in the context of obesity, without which, he suggested, it is doubtful that anyone would think about characterizing food as addictive. Before presenting some examples of how researchers are using neuroimaging to study the complexity of factors that drive energy balance, Ziauddeen provided a conceptual framework to help in understanding how imaging technology data are collected and analyzed.
Key Elements and Assumptions of Cognitive Neuroscience Experiments
Ziauddeen noted that several key assumptions underlie most cognitive neuroscience experiments: (1) there is a phenotype of interest (e.g., “food addiction”); (2) there is a process implemented in the brain that is reliably associated with that phenotype; (3) there is a task that can be used to examine the process; and (4) the method allows for a reasonable examination of the brain processes during the performance of the task.
Two levels of control are inherent in the design of neuroscience experiments. The first is the contrast between the phenotype of interest and a control phenotype. The second is that the task includes a test condition
______________
3 This section summarizes the presentation of Hisham Ziauddeen, M.R.C. Psych., Ph.D., University of Cambridge, Cambridge, United Kingdom.
and a control condition because most processes imaged are not single-level processes; most are integrated processes. The test condition usually involves manipulating the process of interest, while the control condition involves controlling for all the other processes engaged by doing that task.
The Importance of Task
Although Ziauddeen focused mainly on phenotype and process, he briefly highlighted the importance of task, which in his opinion is highly relevant when considering complex stimuli such as food. As an example, Ziauddeen described a motivational task that he and his research team developed for examining low- or high-fat food versus nonfood (Ziauddeen et al., 2014). The task involved having hungry people squeeze a rubber bulb while in the scanner. They were essentially “playing for lunch,” he said. The task produced some very robust neural activation, with the force of the squeeze for high-fat food being significantly greater than the force of the squeeze for nonfood, and the force of the squeeze for all food also being significantly greater than the force of the squeeze for nonfood.
However, a challenge with this task is that findings in the scanner may not be representative of what actually happens. It is unclear how people’s responses to images of food while they are in the scanner approximate what happens when they are outside the scanner.
With the aim of gaining better control over what is happening while subjects are in the scanner, Ziauddeen and his team developed another grip force–based task (in process, not published). Using an objective energy density criterion of 250 calories per 100 grams to define high fat or low fat, they had a pilot group of individuals rate pictures of food in terms of how much they liked the foods, how appetizing the foods were, and how healthy or unhealthy they thought the foods were. The researchers then had the participants perform the task that required squeezing a grip force bulb to indicate how much they wanted the item being displayed. After the task, the participants rated the pictures themselves, and these ratings matched well with those of the pilot groups. When the researchers examined the force responses for the food items, there were no differences between high-fat and low-fat effect foods. In other words, once the pictures were controlled such that all foods appeared equally appetizing and equally edible, there were no differences between high-fat and low-fat foods or indeed between healthy and unhealthy foods. This finding is important, as many studies have been conducted by comparing, for example, hamburgers with raw cabbage, Ziauddeen observed, and such high-fat versus low-fat comparisons are confounded by other dimensions such as appetizing versus bland and edible versus not (usually) edible.
Considering the Phenotype
Ziauddeen identified two questions worth keeping in mind when considering the phenotype being evaluated. First, is there a shared similarity between drug addiction and “food addiction”? Second, is there a shared similarity between drug addiction literature and food addiction literature?
Drug Addiction Versus “Food Addiction”
There are at least two views of “food addiction.” The first is that certain foods are addictive and activate brain-reward systems in the same way that drugs do. The second is that certain people show a pattern of overeating that resembles drug addiction or drug dependence, with binge eating disorder being the most commonly considered candidate. Similar views can be held on drug addiction: that certain substances are addictive and activate brain-reward systems and that certain people show an addictive or dependent pattern of overconsumption of drugs. However, Ziauddeen noted, the reality is that drug addiction is a combination of an addictive drug and a susceptible individual resulting over time in the development of drug addiction or dependence. Drug addiction develops in only about 15 percent of drug users (Anthony et al., 1994). Ziauddeen emphasized the importance of the element of time and the evolution of a syndrome when thinking about an addiction and observed that most people who are thinking about “food addiction” are not thinking about these components of addiction.
Drug Addiction Literature Versus Food Addiction Literature
In the food addiction literature, researchers have examined three “food addiction” phenotypes thus far: (1) obesity; (2) eating disorders, mainly binge eating disorder but also bulimia nervosa on occasion; and (3) food addiction itself, based on the YFAS, which itself is based on the criteria for substance dependence in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (APA, 2000). While obesity is an extremely heterogeneous phenotype, most researchers use BMI as a measure of obesity. With regard to the use of DSM-IV criteria for modeling food addiction, Ziauddeen expressed skepticism and suggested that the criteria be acknowledged for what they are: current best practice consensus guidelines. Also, the DSM-IV criteria are for a behavioral syndrome related to a substance of abuse; they were not designed for a substance such as food that people need to ingest.
That the DSM-IV criteria were not designed for substances that people need to ingest raises a question: For foods, what exactly is the potential substance of abuse? There are several candidates, including high fat, high
sugar, the combination of high fat and high sugar, and refined and processed foods. But all of these potential substances are “terribly imprecise,” Ziauddeen said. Without precision, it becomes very difficult to know just what is being studied.
When comparing the DSM-IV criteria for substance dependence (APA, 2000) and their proposed food addiction equivalents (Gearhardt et al., 2009; Volkow and O’Brien, 2007), there are a few things to note, said Ziauddeen. One is that the DSM-IV criteria for substance dependence tend to conflate what are thought of as hallmarks of the addiction syndrome—such as persistent use despite negative consequences, loss of control of consumption, and escalation of use (Deroche-Gamonet et al., 2004; Vanderschuren and Everitt, 2004)—with features that relate to chronicity and severity of use of certain drugs, such as tolerance and withdrawal. The DSM-IV tolerance criterion for substance dependence is “increasing amounts of drug are required to reach intoxication”; the withdrawal criterion is “withdrawal symptoms on drug discontinuation, including dysphoria and autonomic symptoms such as shakes and sweats.” The proposed food addiction equivalent for tolerance is “increasing amounts of food are required to reach satiety”; the proposed equivalent for withdrawal is “distress and dysphoria during dieting.” There are some problematic elements in the DSM-IV criteria that do not map well to food, in Ziauddeen’s opinion. He highlighted tolerance and withdrawal not because they are necessarily critical when defining addiction, as they are not associated with all drugs of abuse, but to emphasize the importance of knowing exactly what tolerance and withdrawal mean if they are to be included as proposed food addiction equivalents.
The YFAS, the current tool for defining the food addiction phenotype, is a straight translation of the DSM-IV criteria. However, it is based on adjustments that needed to be made given that food is something people need to ingest, and it uses severity criteria to demarcate what is normal from what extends into the realm of pathology (Gearhardt et al., 2009). While the severity criteria are necessary for this purpose, Ziauddeen’s reservations about the YFAS are related to the validity of directly translating the DSM-IV criteria to food and the fact that some of the criteria are not precisely defined (as described on previous page). He also expressed concern about the sample for which the YFAS was developed and validated (Gearhardt et al., 2009). He observed that it was a young and largely nonobese sample. Of even greater concern, the results correlated strongly with a standard measure of eating disorders, suggesting that the YFAS, particularly in this sample, was capturing elements of known eating disorder pathologies rather than any unique syndrome. The YFAS has since been validated in other samples (Davis et al., 2011; Eichen et al., 2013; Gearhardt et al., 2012, 2013b). In these samples, there is a strong concordance with diagnosed binge eating disorder, raising the possibility that the scale may be
measuring the same pathology in another way. Also of concern is that in these studies, significant percentages of the samples endorsed the tolerance and withdrawal criteria, and these are criteria for which the scale itself does not have a clear definition.
In summary, Ziauddeen urged greater consideration of the limitations of phenotypes being studied.
The Processes
Regarding processes at play, neuroimaging studies on food addiction are guided largely by what is known about drug addiction. Broadly and briefly, Ziauddeen described some key models in the drug addiction field. Drug taking starts as voluntary and goal directed but becomes habitual and compulsive over time. Over time, the drug taking sensitizes the dopaminergic systems and makes drug-related cues more salient and motivating. The cues tend to become more rewarding than actual receipt of the reward, which becomes less rewarding. This process has been conceptualized as an enhancement of the anticipation of the drug and a blunting of the consummation of the reward. These changes, which are accompanied by decreases in D2 dopamine receptor levels in the striatum, lead to impairments in the control systems that regulate behavior. Finally, drug taking eventually becomes driven more by the need to prevent the discomfort of withdrawal than by the thrill of taking the drug itself.
Considering the adaptation of this process of drug addiction to foods, Ziauddeen focused on three key questions: (1) Do food cues become more salient and motivating over time? (2) Is there an enhancement of anticipation triggered by the cue, compared with actual receipt of the food? (3) Is there a change in D2 dopamine receptor levels? More broadly, Ziauddeen identified three key contextual issues to consider: (1) the notion that foods and drugs act on the same reward systems; (2) the reality that much of scientists’ understanding of drug addiction processes comes from animal neuroscience studies, with many of the ideas not having been fully tested in humans; and (3) the risk of borrowed legitimacy, that is, whether a finding with food that resembles a finding with drugs necessarily means that the food is “addictive.” To highlight the latter issue, Ziauddeen referred workshop participants to data presented in Carelli et al. (2000, 2003). Based on recordings of single neurons in the nucleus accumbens, the researchers detected that a very distinct neuronal population responds to water compared with the populations that respond to cocaine. A human imaging study would not have the resolution to capture that difference. Instead, it would probably show similar responses in the same region of the brain. In other words, imaging data showing similar responses in the same region of the brain do not necessarily mean that the same circuits are being engaged.
More concerning for Ziauddeen than these contextual issues are two key conceptual questions: (1) Is there an addictive aspect to normal eating behavior? (2) Is there a fundamental addictive mechanism in the brain that controls normal eating? In Ziauddeen’s opinion, there is no neural signature of addiction in the brain. He cautioned against observing a neural finding that is different in two different populations—for example, lean versus obese individuals—and assuming that the signature reflects a fundamentally addictive process.
Brief Overview of Neuroimaging Data
Wang and colleagues (2001) were the first to observe reduced D2 dopamine receptors in the striata of obese individuals. They reported a powerful and compelling graphic, in Ziauddeen’s opinion, showing a clear difference in the relationship between D2 binding potential and BMI in morbidly obese (BMI > 40) versus lean (control) subjects (see Figure 3-1a). However, Ziauddeen noted a fair bit of overlap between the findings for the morbidly obese and lean individuals. If the same graphic is flipped on its side (see Figure 3-1b), it is easier to see that D2 receptor levels are fairly comparable for some BMI comparisons (e.g., there is one person with a BMI of about 50 who shows the same D2 receptor levels as a person with a BMI of about 27).
The Wang et al. (2001) finding has been replicated once with a slightly different but similar enough experimental design (de Weijer et al., 2011). However, several other studies have failed to replicate this finding (Dunn et al., 2012; Eisenstein et al., 2013; Haltia et al., 2007), the most striking of these, like Figure 3-1a also from Nora Volkow’s laboratory, showing an opposite effect (Dunn et al., 2012). In Ziauddeen’s opinion, findings collectively suggest that there is probably a D2 dopamine receptor abnormality in obesity, but thus far at least, only for morbid obesity. For more common levels of obesity, the evidence is unclear.
In a recent review of functional neuroimaging studies examining obesity, binge eating disorder, BMI (as a continuous variable), and food addiction, Ziauddeen and colleagues (2012) found a lack of consistent findings regardless of phenotype studied. The reviewed studies evaluated brain responses to presentation of food, anticipation of food, and consumption of food. Only one of the reviewed studies examined food addiction as a phenotype (Gearhardt et al., 2011c). Even then, Ziauddeen observed, only 2 of the 48 individuals sampled by Gearhardt and colleagues (2011c) actually had food addiction based on YFAS criteria; the others had food addiction symptoms, but not food addiction. Ziauddeen urged acknowledgment of the assumptions of that study—the first being that the YFAS is a valid measure of food addiction, and another being that the YFAS scores reflect
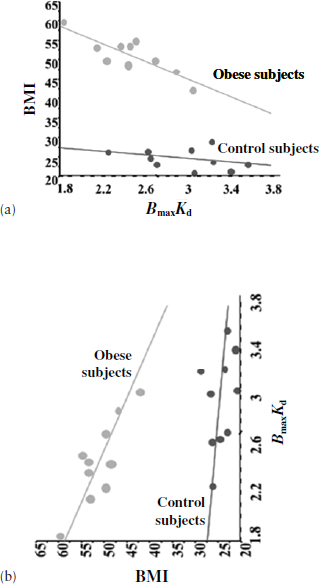
FIGURE 3-1 The relationship between D2 binding (BmaxKd) and BMI in morbidly obese and lean (control) individuals.
NOTE: Graph (b) depicts Graph (a) flipped on its side.
SOURCES: Volkow and Wise, 2005; Wang et al., 2001. Adapted by permission from MacMillan Publishers Ltd.: Nature Neuroscience (Volkow, N. D., and R. A. Wise. 2005. How can drug addiction help us understand obesity? Nature Neuroscience 8[5]:555-560), Copyright 2005. Reprinted from Lancet, Vol. number 357, Wang, G. J., N. D. Volkow, J. Logan, N. R. Pappas, C. T. Wong, W. Zhu, N. Netusil, and J. S. Fowler, Brain dopamine and obesity, Page No. 354-357, Copyright 2001, with permission from Elsevier.
a continuum of severity (i.e., having two symptoms is worse than having one, having three is worse than having two, and so on). Beyond the fact that only two individuals had a diagnosis of food addiction based on the YFAS, the results are unclear in Ziauddeen’s opinion. The individuals were provided with either a chocolate milkshake or a neutral tasteless solution while in the scanner. Based on the model described above from the drug addiction field, one would expect an enhanced anticipatory response to cues that predict the chocolate milkshake and a decreased consumption response to actual receipt of the milkshake in individuals identified as being addicted to food. However, there was no difference in the anticipatory response to the chocolate milkshake between those identified and not identified as having food addiction. Rather, the difference was in the anticipatory response to the neutral cue. Both groups (scoring low and high on food addiction) showed a decreased consumption response.
Future Research
There is little direct neuroimaging evidence to support the idea of food addiction, Ziauddeen concluded. And he suggested that what little direct evidence exists should be interpreted with caution. He called for what he described as a post hoc a priori approach to studying “food addiction”: first, define the addictive agent; next, define the behavioral syndrome that relates to that agent; then find a way to measure the syndrome; and finally, examine the syndrome’s neurobiology and natural history.
Ideally, the field should conduct long-term prospective studies, Ziauddeen suggested. Most studies conducted thus far have been cross-sectional, which he observed may merely reflect the infancy of the field.
In closing, Ziauddeen commented that the overriding question for him is the purpose of investigating “food addiction.” Is it for diagnosis and treatment, for policy change aimed at tackling the obesity crisis, or as a scientific construct for further research? Each of those purposes has not only a different standard of evidence, but also different implications. For example, if developing a clinical diagnosis for “food addiction” is the goal, who would be served as a result and how? Similarly with policy, if the field reaches a point where either an addictive food or a group of people who suffer from a food addiction can be clearly identified, what steps can be taken and what policies can be formulated?
ASSESSING THE VALIDITY OF QUESTIONNAIRES FOR FOOD BEHAVIORS AND ADDICTION4
A key goal for Ashley Gearhardt and her research team is to determine whether there is an addictive-like process that may contribute to certain types of problematic eating. The notion that addiction might be playing a role started to gain traction in the early 2000s, according to Gearhardt, for several reasons (Gold et al., 2003; Lilenfeld et al., 2008; Volkow et al., 2013). She explored those reasons and then described the development and validation of the YFAS.
The Notion of Food Addiction
Gearhardt identified several factors that have contributed to the greater scientific attention focused on the notion of “food addiction.” First, obesity rates have continued to skyrocket over the past few decades, despite widespread attempts to lose weight that often result in failure. Even the most successful dieters typically regain their lost weight within 2 years, according to Gearhardt. This phenomenon has raised the question of whether an addictive-like process may contribute to this chronic relapsing pattern.
Additionally, there has been greater clinical acknowledgment that binge eating disorder, which entails repeated periods during which people lose control of their food consumption despite a desire to maintain control, is a verifiable mental health issue. Gearhardt noted that many of the phenotypes that present clinically with binge eating disorder resemble what is seen when people present with an addiction: they typically have lost control of consumption, show elevated cravings, and have tried repeatedly to cut down but keep failing. Because many factors that contribute to binge eating disorder are similar to those that contribute to addiction-like disorders, some experts suspect the two disorders may share some common mechanisms, such as impulsivity, reward dysfunction, depression, and issues with emotional regulation. In addition to some potential mechanistic overlap, there are some genetic similarities between binge eating disorder and substance use disorders.
Additionally, there is evidence to suggest neuromechanistic overlap. Gearhardt explained that the reward system in the human brain evolved to ensure that individuals seek out what they need to survive. A common conception about drug addiction is that drugs of abuse are so potent that they are able to hijack the brain’s reward system and attribute reward to the addictive substance rather than to things needed for survival. Although
______________
4 This section summarizes the presentation of Ashley Gearhardt, Ph.D., University of Michigan, Ann Arbor.
humans need to eat, Gearhardt observed that with certain types of food, it appears as though people are eating not to survive but in a hedonically driven manner. She said, “They have lost control of their eating, and they are doing it in a compulsive way.”
All of these changes (e.g., rising rates of obesity, acknowledgment of binge eating disorder as a verifiable mental health issue, increases in hedonic eating) have occurred in a changing food environment, with greater availability of ultra-processed foods high in fat, refined carbohydrates (e.g., sugar), and salt (Gearhardt et al., 2012; Monteiro et al., 2010). Gearhardt observed that ultra-processed foods are very different from the foods humans evolved to eat, which included no foods naturally high in both fat and sugar (coconut milk comes the closest, she noted). Foods tend to be either high in sugar, like fruits, or high in fat, like nuts and meats, but not high in both.
The fact that foods have changed over the course of human history, with today’s ultra-processed foods being high in both fat and sugar, raises the question for Gearhardt of whether foods have changed over the course of human history in an addictive way, that is, in a way that may trigger an addictive or addictive-like response in certain individuals. She argued that humans have altered the food supply in many of the same ways in which they have made addictive substances in the past. Two of the major mechanisms for accomplishing the latter are (1) increasing the potency, that is, the dose of the rewarding substance, and (2) increasing the speed of absorption and creating a large spike in reward-related responses (Samaha and Robinson, 2005; Verebey and Gold, 1988). When chewed, for example, the coca leaf does not provide a very high dose, nor is it rapidly absorbed into the system. Levels of addiction resulting from chewing a coca leaf are quite small even in places where chewing coca leaves is a common cultural practice. In contrast, when processed and made into a more potent substance that is more rapidly absorbed—that is, when made into cocaine—coca leaf becomes much more addictive. When it is processed even further into crack cocaine, its addictive nature becomes even more intense. Gerhardt noted that the foods people most commonly struggle with and lose control over are ultra-processed foods with elevated potency and elevated speed of absorption into the system. Thus, as with drugs of abuse, these foods may be more likely to trigger an addictive process compared with more naturally occurring foods.
Identifying “Addictive Eaters”
To further investigate the hypothesis that an addictive process contributes to problematic eating, Gearhardt and her colleagues focused on methodologically sound ways of identifying “addictive eaters.” When she first started exploring this question, Gearhardt found that existing methods
for identifying addictive eaters were too limiting. One method was self-identification. For example, individuals would be asked if they were “carb cravers” or “chocoholics.” But it is not clear what a chocoholic is, given how common the addiction language is in the popular press. Gearhardt asked, rhetorically, whether researchers can consider a response such as “Yes, I am addicted to chocolate” to be evidence of an addiction.
In the past, the most common way of assessing addictive-like eating, according to Gearhardt, was weight status, with obesity being interpreted as evidence for an addiction to food and lean body weight being interpreted as evidence for lack of an addiction to food. But that method raises a number of concerns. First, obesity is a medical endpoint with many causal pathways, including medication side effects, genetics, physical inactivity, and the overconsumption of food. Equating such a highly heterogeneous condition with food addiction likely overidentifies many people. It is like equating cirrhosis of the liver with alcohol addiction, when in fact many people who are not addicted to alcohol have cirrhosis of the liver and many people who are addicted to alcohol never develop that condition. Additionally, the assumption that people with normal BMIs have healthy relationships with food is not necessarily valid. Making that assumption likely underidentifies people who have an unhealthy relationship with food but are not yet obese or who are using such means as purging or excessive exercise to mask their unhealthy relationship with food. In sum, said Gearhardt, using body weight as the only way to predict addictive-like eating behavior results in either over- or underidentification.
A third method used in the past involves defining binge eating disorder as addictive-like eating. Individuals with binge eating disorder show a pattern of consumption that entails losing control and being unable to stop despite wishing to do so. However, observed Gearhardt, there are many differences between binge eating disorder and addictive-like eating. Binge eating disorder involves a discrete period of time in which the individual loses control and is aware that he or she has done so. But with addiction—for example, with cigarette smoking—there are people who chronically and consistently use the addictive substance throughout the day without experiencing any discrete episodic binge. Also, people who are addicted to a substance are not necessarily aware that they have lost control. Most important, Gearhardt noted, binge eating disorder is commonly thought to be a consequence of dietary restraint. That is, people who go on extreme diets and are unable to maintain that level of dietary restraint end up binging. Treating people with binge eating disorder involves minimizing the restraint around eating behavior and teaching them that there is no “good” or “bad” food. From this perspective, it is only the way the person relates to food that is a problem; the attributes of the food (e.g., high sugar, high fat) do not contribute to the eating issues. In contrast, from an addiction perspec-
tive, the characteristics of certain foods may contribute to the problematic eating pattern. For example, highly processed foods with unnaturally high levels of sugar and fat may be more likely to trigger biological and psychological addictive-like responses relative to more naturally occurring foods such as fruits and vegetables. Thus, all foods are not considered equally likely to contribute to problematic eating patterns, and it may be more difficult for someone with addictive-like eating to consume these highly processed foods in moderation compared with other foods. As an example, Gearhardt asked the audience members to think about coming home after a hard day of work and whether they would be more likely to overeat a bowl of strawberries or a bowl of strawberry ice cream from Ben & Jerry’s. “There seems to be a difference between these items,” she said. Thus, both the mechanisms and treatments for binge eating disorder and addictive-like eating are notably different, which does not make binge eating an optimal proxy for food addiction.
The Yale Food Addiction Scale
Gearhardt and colleagues developed the YFAS to improve the level of specificity in the identification of addictive eaters. They began by considering the relevance of DSM-IV criteria used to diagnose other addictions (APA, 2000). Draft YFAS questions were reviewed by experts who work with addiction, obesity, eating pathology, and binge eating patients to ensure that the questions adequately captured the context and would be clear to test takers. The scale has since been validated in nonclinical, clinical, and epidemiological samples (Flint et al., 2014; Gearhardt et al., 2009, 2012, 2013b). It is currently available in five languages (Meule and Gearhardt, 2014).
Gearhardt acknowledged that DSM-IV is not a perfect document. That said, there are no other agreed-upon criteria for addiction. The DSM-IV criteria have been applied successfully to a wide range of disorders, behaviors, and substances. Even though a heroin addiction looks very different from a cigarette addiction, the same diagnostic criteria have been used to study both disorders. For many years, people argued that cigarettes were not addictive because they did not “look” like heroin—one can legally consume them, one does not get intoxicated when one smokes them, one can smoke them while watching one’s children, etc. But as the field moved forward, people began to realize that cigarettes are not just addictive but potentially more addictive than heroin.
Some researchers have suggested that neurobiological rather than behavioral indicators should be used to identify who may or may not be experiencing addictive-like processes in relation to food (Ziauddeen et al., 2012). But Gearhardt noted that it is not currently possible to diagnose known addictions (such as to alcohol) by imaging the brain. Thus, it is even
less plausible to use this means to identify a phenomenon like addictive eating that is still being evaluated. Presently, the field relies on behavioral indicators to diagnose the presence of an addiction, and the YFAS applies this same approach to the identification of addictive-like eating.
Gearhardt also acknowledged that no self-report questionnaire is sufficient to answer whether an addictive process is at play in problematic eating. Indeed, no self-report questionnaire is sufficient to determine whether any mental health disorder exists, especially one as controversial and complex as problematic eating behavior. However, the YFAS can be used, Gearhardt proposed, to identify individuals who may be the most likely to be experiencing an addictive-like response to food and then to evaluate whether mechanisms implicated in other addictions are also contributing to this pattern of problematic eating. Gearhardt stressed the importance of the fact that the YFAS goes beyond weight as a proxy. The focus of the scale is not on weight, but on people’s relationships with food. Also important, the word “addiction” is not mentioned on the scale, which should reduce biased answers based on self-identification as a food addict. Thus, while the development of the YFAS does not prove that food addiction is a valid concept, Gearhardt noted, it does provide a more methodologically sound tool than has previously been available for evaluating empirically whether an addictive process is contributing to compulsive eating behavior.
A Review of YFAS Literature
Gearhardt noted that since the YFAS was published in 2009, many studies have used it to examine addictive-like eating. Individuals with addictive-like eating as defined by the YFAS have been shown to have higher current and lifetime BMIs (Flint et al., 2014; Gearhardt et al., 2014a; Pedram et al., 2013); a greater risk for negative health outcomes, such as hypertension, high cholesterol, and diabetes (Flint et al., 2014); more severe binge eating, with a tendency to binge more frequently, and more severe eating disorder pathologies such as emotional overeating (Davis et al., 2011; Gearhardt et al., 2012); elevated craving for certain foods, particularly fatty foods (Gearhardt et al., 2014b); higher emotion dysregulation in general (Gearhardt et al., 2011c); and in children, higher BMI, less satiety responsiveness, and higher emotional eating (Gearhardt et al., 2013a).
Gearhardt proposed that the effects observed in children with addictive-like eating behaviors are among the most important potential outcomes of this work. If certain foods are capable of triggering an addictive response, it is likely that the response will be greater in children than in adults. Children’s brains are more plastic, children have not developed the same coping strategies that adults have, and their reward striatal system is more reactive than their executive control system. Children are frequently targeted
for the marketing of unhealthy foods, with children and adolescents seeing approximately 6,000 food commercials a year (Dembek et al., 2014). Gearhardt observed that almost all those commercials are for foods that she suspects lend themselves to an addictive process.
Addictive-like eating as measured by the YFAS also is associated with factors implicated in other addictions, including elevated impulsivity and delay discounting, whereby short-term reward takes priority over long-term consequences (Davis et al., 2011; Jasinska et al., 2012); increased attentional biases for food cues, whereby the food cues become more salient for individuals who report addictive-like eating than for those who do not (Meule et al., 2012); greater risk of developing a substance use disorder following bariatric surgery, which may be indicative of a cross-addiction transfer (Reslan et al., 2014); greater likelihood of having a higher dopamine multilocus genetic profile score, with differences in dopamine signaling being related to genotype (Davis et al., 2013); differential responses to dopamine agonist in the brain (Davis et al., 2013); and patterns of neural response associated with addiction (Gearhardt et al., 2011c).
Regarding this last association, Gearhardt and colleagues (2011c) found that women with higher scores on the YFAS exhibited elevated activation in the dorsolateral prefrontal cortex, medial orbitofrontal cortex, and amygdala during anticipatory cues for foods. When the women started to actually consume the food, the researchers observed less activation in the lateral orbital cortex, a brain region implicated in cognitive control. This same pattern of neural response has been identified in other types of addictions. Gearhardt explained that with addiction, the reward system often stops responding to nonaddiction cues; that is, it becomes hyposensitive, with the only cue activating it being the addictive cue. Gearhardt and colleagues (2011c) found that addictive-like eaters expressed that same hypo-active response to other stimuli, but when they were shown a milkshake cue, their neural response increased to a more normative level. That finding is consistent with what has been observed with other addictive disorders. Notably, Gearhardt said, she and her team controlled for BMI, so the effects “occurred above and beyond” BMI. In the future, Gearhardt would like to test these findings in a sample with more severe levels of food addiction, as few participants in this study met the clinical cut-off point for food addiction. Given the large effect sizes found in this study, it is likely that more severely addicted eaters may exhibit even more differences in neural function in response to food cues and consumption.
Next Steps
A first next step will be to examine DSM-5 and see whether the current thinking about addictive-like eating reflects scientists’ changing understand-
ing of addiction. Also, Gearhardt would like to know how people interpret the YFAS questions and whether a clinical interview would yield more clinical specificity. Most important, existing findings need to be replicated and longitudinal studies need to be conducted.
The field is in its infancy; the YFAS was developed only 5 years ago. So, suggested Gearhardt, it is no surprise that there are many gaps in the literature. But now that scientists have a better understanding of who additive-like eaters may be, they can begin to test more mechanisms, such as tolerance and withdrawal. Do additive-like eaters show signs of tolerance? Do they show signs of withdrawal?
Finally, which foods are at issue? Gearhardt opined that the term “food addiction” is a misnomer. There appears to be a certain subclass of food that people struggle with—foods that are processed and designed to be as hedonically rewarding as possible. But which foods in particular are capable of triggering an addictive-like response? Answering this question and determining the socioeconomic implications (e.g., living in a neighborhood of lower socioeconomic status and having access only to certain types of foods) will be “incredibly important” for treating and preventing obesity and eating disorders, Gearhardt said. Understanding how obesity is framed—for example, the difference between framing it as a problem related to personal responsibility as opposed to a problem potentially caused by an addictive-like response to food—will also have important implications for treatment and prevention.
In closing, Gearhardt made a call for continued research funding in this area. Conducting this type of research is challenging, she noted, not only because of the controversial nature of the topic, but also because the topic often cuts across multiple funding bodies.
DSM-5: SUBSTANCE-RELATED AND ADDICTIVE DISORDERS5
Charles O’Brien observed that his perspective on the workshop topic comes from having spent more than 40 years treating people with unquestioned addiction. He began working in the field of addiction during the Vietnam War, when few people knew anything about addiction, especially its clinical aspects, because there had been so little research in the area. O’Brien served as chair of the substance use disorders section of the most recent DSM update, DSM-5, published in 2013. He discussed differences between DSM-IV and DSM-5 criteria for a substance use disorder diagnosis and the relevance of the criteria to food.
______________
5 This section summarizes the presentation of Charles P. O’Brien, M.D., Ph.D., University of Pennsylvania, Philadelphia.
Changes in DSM-5
O’Brien explained that the committee responsible for updating the substance use disorders section of DSM-5 attempted to keep the changes to a minimum (APA, 2013). Several candidate “addictions” were proposed for addition to DSM-5, food addiction being among them. Eventually, the committee decided that food addiction should not be added, but that binge eating disorder should be retained. Sex addiction was also proposed but similarly rejected. The most likely new candidate for inclusion at some point is Internet gaming disorder, which is becoming an important clinical problem in many countries worldwide. It was included in Section III of DSM-5 (i.e., as a potential diagnostic category requiring further research). As more data accumulate, it may be added as an actual diagnosis. O’Brien suggested that Internet gaming disorder may be a useful model for food addiction.
The DSM-5 criteria for substance use disorder begin with tolerance and withdrawal. Both of these criteria used to be considered signs of opioid addiction (APA, 2013), but they can also occur when medications are used appropriately under a physician’s prescription. Thus, tolerance and withdrawal can be considered normal responses to drugs administered repeatedly that act on the nervous system (i.e., antidepressants, opioid analgesics, antianxiety drugs, and antihypertensive drugs). The DSM-5 substance use disorder committee decided that tolerance and withdrawal should not be used as criteria for addiction if the substance in question has been prescribed by a physician as a form of treatment. O’Brien noted that that exclusion is one of the changes from DSM-IV (APA, 2000).
All of the other DSM-5 criteria for substance use disorder besides tolerance and withdrawal deal with loss of control (APA, 2013). “Control is really a big thing,” O’Brien said. It is considered essential for drug addiction and is important for “food addiction” as well, which is why, in the view of the DSM-5 substance use disorder committee, binge eating disorder comes the closest among eating problems to “food addiction.” Another change in the DSM-5 criteria for substance use disorder is the addition of craving for the substance. Craving was added based on brain imaging data showing that people who are in treatment for any kind of addiction tend to have a craving for the substance that can last for years. The long-term “memory” of addiction has also been studied extensively in rats, according to O’Brien. The other criteria for substance use disorder are all classic signs of addiction: loss of ability to cut down, spending excessive time acquiring the substance, giving up other activities for the substance, using the substance despite its negative effects, failure to fulfill major role obligations, recurrent use in hazardous situations, and continued use despite consistent social or interpersonal problems.
An overall goal of DSM-5 was to make psychiatric diagnoses more neuroscience based (APA, 2013). Unfortunately, in O’Brien’s opinion, researchers have spent years searching for biomarkers for psychiatric disorders but have yet to identify any that serve the same clinical purpose as that served by metabolic disorder and cardiology biomarkers. In fact, according to O’Brien, the need for biomarkers is why the National Institute of Mental Health launched its Research Domain Criteria (RDoC) project.
While the field lacks sufficiently reliable biomarkers, it does have very good animal models. In terms of “food addiction,” animal models show both similarities and differences in central nervous system responses to drugs of abuse and sweet foods. In work from Friedbert Weiss’s laboratory, for example, rats were allowed to self-administer either sweetened condensed milk, which is an intensely sweet substance, or alcohol. With both substances, the rats demonstrated a high level of self-administration and self-administered until the substance was no longer available. However, the animals showed an important difference during the reinstatement period of the experiment, that is, when the rats were provided with the same self-administration tool but with no actual substance available. Rats previously exposed to alcohol continued to try to self-administer even though they were not actually getting any alcohol. The rats previously exposed to sweetened condensed milk, on the other hand, did not continue to try to self-administer. The same was true of cocaine: during the reinstatement period, the rats reinstated quickly to cocaine but not to sweetened condensed milk. Together, these results suggest that the self-administration value of sweetened condensed milk does not last as it does with alcohol or cocaine, even though all three substances are activating the same part of the brain—the nucleus accumbens and ventral striatum.
O’Brien emphasized that while human brain imaging is useful (in fact, gambling was added to the DSM-5 list of addictions based on human brain imaging data), correlation between a report of pleasure and activation of the brain reward structures is expected and is not evidence that the pleasure in question is an addiction.
Factors that need to be considered before adding a new disorder to DSM-5 include a clinical need that is common and severe enough to warrant a new diagnosis, the potential for harm, the potential for treatment, and whether the condition meets the criteria for a mental disorder. O’Brien noted that the substance use disorder committee spent a great deal of time debating the last of these factors. The field of psychiatry has been criticized for overmedicalizing behaviors. For example, some people think that social anxiety disorder could be characterized as shyness and that making shyness a diagnosis robs the world of diversity. Someone diagnosed with social anxiety disorder can be treated with medication and can become more relaxed and sociable. O’Brien asked, rhetorically, “Is that good or bad?”
DSM and the YFAS
The “big issue” with the YFAS, in O’Brien’s opinion, is taking a clinical problem from one field and trying to “squeeze” it into another. Changing the concepts and terminology used in one field so they can be used in another is particularly problematic with addiction because there has always been a certain amount of debate about the words used for the different concepts and various aspects of addiction. The addiction criteria in DSM-IV are based on classic opioid addiction and studies with opioids dating back to the 1930s and 1940s. Other forms of addiction are based on that addiction. O’Brien suspects that the developers of the YFAS will do a good job of adapting the scale to DSM-5. But is “squeezing” something meant for drugs into something that is normal behavior for people (i.e., eating) a good idea, he asked, especially since the goal for food obviously cannot be abstinence?
Compounding the challenge is the fact that the word “addiction” has been misused for many years now, and not just in the clinic. O’Brien cited articles about the president saying that the United States is “addicted” to oil and about women being “addicted” to pink. He said, “You could say I am addicted to skiing because I really get euphoric when I see a field of powdered snow. I am sure that if I were in a brain scanner, you would see activation of my ventral striatum and nucleus accumbens. But does that mean it is an addiction?”
In O’Brien’s opinion, for the addiction model to be useful with food, the issue of severity needs to be addressed. For example, O’Brien suggested that severity might be based on some degree of complication, such as diabetes or morbid obesity. When he entered the field of addiction research, the only way to measure severity was the number of bags of heroin someone used daily, and the goal was to try to get that person to go from a 10-bag-per-day habit to a 2-bag-per-day habit. That approach is not very useful, he said. Most people with a heroin habit typically have multiple other problems. So the Addiction Severity Index (ASI) was developed in the 1970s as a way to measure severity based on those other problems as well, not just drug use. Today, the ASI is used worldwide and is available in more than 20 languages. It covers seven categories of problems, or domains: drug use, alcohol use, medical problems, employment problems, legal problems, family problems, and psychiatric problems (see Figure 3-2). In DSM-5, severity for substance use disorders is based on the number of symptoms a person has, with a maximum of 11.
Conclusion
In conclusion, O’Brien observed that there is a group of well-intentioned people who already think that food addiction is a diagnosis and needs to be
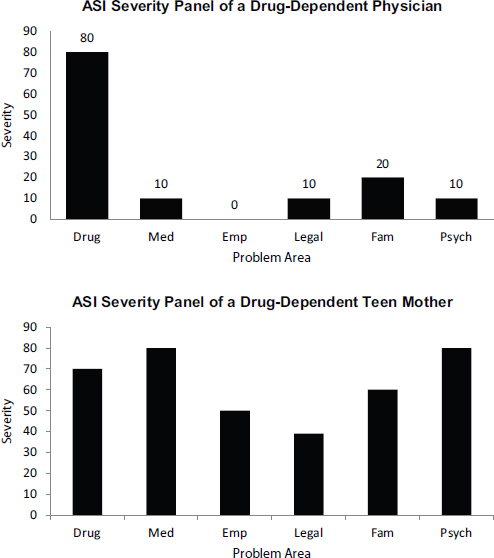
FIGURE 3-2 Severity of symptoms for six of the seven problem areas, or domains, associated with addiction, based on the Addiction Severity Index (ASI), for two individuals.
NOTE: Emp = employment/support; Fam = family/social; Med = medical; Psych = psychiatric.
SOURCE: O’Brien, 2014.
treated. “We have to be cautious,” he warned. “[A diagnosis of food addiction] has to be founded on science rather than on enthusiasm.”
Following O’Brien’s presentation, the speakers from the afternoon session participated in a panel discussion with the audience. Questions covered a wide range of topics.
Identifying the Potentially Addictive (or Addictive-Like) Substance in Food: A Key Research Challenge
An audience member observed that discussions of drug addiction generally do not revolve around drug addiction per se; rather, the focus usually is on addiction to specific drugs, such as cocaine, heroin, and so on. The audience member asked whether there is a specific food-related chemical reaction that is having an impact when the brain’s reward system overrides its satiety system.
Gearhardt replied that such knowledge does not yet exist for food. Evidence from animal models suggests that sugar may be a possibility. But studies in humans are “really just beginning,” Gearhardt observed. Food is complicated in so many ways. A Pop-Tart, for example, has some 60 ingredients, and it is difficult to tease them apart. Gearhardt suspects that the combination of extremely high levels of refined carbohydrates, fat, and salt is likely what is triggering the response observed in the brain, but much more data and science are needed to answer this question.
Ziauddeen agreed that having a clearly identifiable substance is “critical.” An assumption underlying the DSM-IV criteria is that an addictive substance exists and that the behavioral criteria apply within the context of using that substance. With food, it is not yet clear what is being consumed that is important. Presently, researchers are accumulating evidence on behavior based on a potential agent that has yet to be identified; all potential substances are being lumped together. With drugs, researchers are beginning to accumulate evidence for other elements besides the behavioral syndrome of addiction that characterize an addiction. However, they are able to do so only because they have a substance as a starting point. “I think it is important to actually clarify what the agent is to use any of this [food-related evidence] meaningfully,” Ziauddeen said. “I do not mean this as criticism, as in, we have no substance [and] therefore there is no addiction. But I think the fact that there is no substance is very much of a problem.”
The Modern Diet: High-Fat/High-Sugar Combinations
In her presentation, Gearhardt emphasized the high-fat/high-sugar content of modern foods not found in any naturally occurring foods. A member of the audience pointed out that human breast milk has the highest sweetness content of any mammalian milk and a fat content equivalent to cow’s milk, goat’s milk, and certain other milks. Small agreed that human milk is a high-fat/high-sugar substance, but observed that it is probably unique among naturally occurring foods in this regard.
The same audience member also commented on the historical use of fruit/nut combinations and observed that the combination of milk and honey, for example, goes back at least several thousand years. In response, Small said the relevant historical scale is hundreds of thousands of years, not thousands of years, and those kinds of mixtures do not extend far enough back in time to influence the evolution of the system. She repeated what she had emphasized during her presentation: modern foods challenge human physiology in a way that has not been seen over the course of time until now.
Later, another audience member observed that creative sugar/fat combinations have been in the human diet at least for decades or hundreds of years and asked why such an increase in obesity has been seen only recently. Small replied that she was unaware of any research on the origin of the current trend in increasing weight and its relationship to the introduction of high-fat/high-sugar combinations in the diet. She stressed the importance of looking at other components of the environment that may contribute to increasing weight. In addition to access to ultra-processed foods, examples of other factors that may contribute to increasing weight include stress, lack of sleep, and loss of insulin sensitivity because of reduced physical activity. “Perhaps we hit a critical mass of these things,” she said.
At another point in the discussion, an audience member asked the panelists to elaborate on the potential role of stress and whether the dramatic rise in obesity over the past several decades might be cortisol related. The audience member mentioned single mothers who work hard during the day and “eat hard” at night. Small pointed to work by Rajita Sinha showing that people with high cortisol levels in the morning, an indicator of chronic stress, exhibit higher cue reactivity. Small reiterated that addictive-like eating behavior is a confluence of multiple factors. “It is not just the nature of the food product,” she said.
In Ziauddeen’s opinion, there are clear differences between the foods available today and those available 50 or 100 years ago. He suspects that highly palatable high-fat/high-sugar foods are stressing human physiology in novel ways and are likely to be having public health consequences. However, none of that necessitates invoking an addictive mechanism, he said. “[Foods] can be ‘bad’ even if they are not addictive,” he noted.
Ultra-Processed Foods: What Makes Them “Addictive”?
In reference to Gearhardt’s statement during her presentation that substances that are absorbed more rapidly have a higher abuse potential, Timothy Moran expressed puzzlement at the relationship between that hypothesis and ultra-processed foods. In other words, what is it about ultra-processed foods that makes them potentially addictive? Is it a taste phenomenon, or is there a metabolic effect? Gearhardt replied that her research team is currently investigating that question. Based on the drug addiction literature and experiments conducted with sham feeding, she suspects that a metabolic effect is involved. But it is very challenging to disentangle responses to a sweet flavor from responses to absorption of a high glycemic load into the system.
Pressing for more clarity, Moran asked about refined versus complex carbohydrates in particular, which he said empty from the stomach at exactly the same rate and therefore have the same effect on releasing insulin. Thus, they should have similar metabolic consequences. How does one of those foods (refined carbohydrates) produce a “phenomenon” (addiction-like process) that the other (complex carbohydrates) does not produce?
Gearhardt reiterated that what differentiates foods with and without addictive-like characteristics is an open question, especially when one is comparing, for example, breakfast cereals of whole and refined grains. When she thinks about what differentiates foods that do and do not trigger addictive-like responses, she tends to think along the lines of a banana, which has a decent amount of sugar but also has fiber, water, and other components and is eaten much less quickly than a handful of jelly beans with the same sugar content that is tossed into the mouth. A multitude of food characteristics need to be examined, she said, to make that differentiation.
Richard Mattes added that if absorption is an issue, the question arises of why fat is being considered alongside sugar. Fats and sugars are quit disparate in their rate of absorption. Small explained that while the physiological response is clearly going to be different with different macronutrients—for example, with fat modulating reward circuits via different pathways compared with glucose—exactly what is going on at a mechanistic level in the gut to trigger those different signals is unclear. Nor is it clear how those separate signals interact in the brain.
The Nature of Addiction: Are Substances Addictive, or Are People Susceptible to Addiction?
Robert Ritter stated that his understanding of addiction is that a substance produces a change in the nervous system, which in turn evokes
addictive behaviors. But do those changes necessarily arise from the use of food substances? Might it be the case that people who become addicted have an underlying problem that results in the expression of addictive behavior?
Ziauddeen responded that at least in the case of drug addiction, predisposing factors increasingly are being viewed as important. He pointed to work by Karen Ersche demonstrating that siblings of cocaine users show similar baseline vulnerabilities to drug dependence with respect to brain structure, personality, and such variables as impulsivity and inhibitory control. The onset of addiction in many cases may begin with these preexisting vulnerabilities. Ziauddeen described addiction as a “combination of an individual and a substance.”
Addiction as a Continuum
An audience member observed that several speakers had mentioned or discussed activation of reward centers in the brain in response to or in association with the YFAS scores, but that as far as he could tell from what was presented, much of the data show a fair amount of variation in the intensity of response. He said, “In the public eye, addiction is thought of like a light switch. It is on or it is off. But your data show a continuum.” He asked the panelists to comment.
Gearhardt replied, “The evidence does not suggest that there is this very discrete line: you are an addict or you are not.” People show a range of addictive responses, from none to subclinical to clinically severe. For example, only about 10 to 15 percent of people who use alcohol actually show a full-blown clinical level of addiction. Many people show subclinical responses. But all those subclinical responses drive up the overall public health cost of alcohol, which is the third leading cause of preventable death. A concern with the potentially addictive nature of certain ultra-processed foods, Gearhardt said, is that the vast majority of people are not (or would not be) fully addicted. Enough people may show enough of an addictive response, enough of a craving, that they consistently eat 100 or 200 more calories daily than they homeostatically need. This level of additional caloric intake on a daily basis is enough to move an individual from a normal weight category to an overweight or obese category, eventually creating a significant public health problem.
O’Brien added that research conducted between the publication of DSM-IV and the preparation of DSM-5 yielded evidence that addiction is a gradual process. The fact that it is a gradual process, or a continuum, is why its diagnosis is now based on number of symptoms. That said, in O’Brien’s opinion, there is no such thing as a mild addiction. Rather, addiction is a progressive disorder, with many different variables impacting the
outcome, not the least of which is genetics. In fact, according to O’Brien, of all mental disorders, addiction carries the strongest evidence for a genetic basis. He urged greater consideration of genetic makeup in future research.
Extrapolating from Drugs to Foods
In her presentation, Gearhardt had compared the ultra-processing of foods to the processing of the coca leaf into the more refined and more potent cocaine and crack cocaine. Ziauddeen found that to be, as he said, “quite an appealing” narrative. But he questioned the parallel with foods. For example, does the refinement of complex carbohydrates into highly refined sugars increase their potency? Even in the addiction field, the process is not quite as straightforward or inevitable. People choose potencies that suit them. Not all people who use a substance choose to use a high-potency version of that substance.
O’Brien noted that this issue of potency is another of the significant difficulties in extrapolating from drugs to food. The oral mechanism of food consumption makes it very different from either intralung or intravenous administration of addictive drugs. Substantial differences in addiction potential are related to route of administration, O’Brien said. The coca leaf was used for some 5,000 years “without much trouble,” he noted, but changing the route of administration “caused it to become a terrible drug.” Cocaine reaches the brain very quickly.
More generally, O’Brien asked, what is to be gained when differences between drugs and foods are ignored and the two are “squeezed” together? Would it be better to set food up as a separate category?
Gearhardt agreed that the oral consumption of food is different from other, more intensive routes of administration. But alcohol is consumed orally as well. In fact, some people think of alcohol as an addictive-like food. It provides calories, which the body needs. Alcohol is good evidence, in Gearhardt’s opinion, that an oral route of administration does not necessarily mean that addiction cannot occur. With respect to whether food should be placed in a separate category, in Gearhardt’s opinion, doing so entails risks. She pointed to research on tobacco and statements in the 1980s and 1990s that tobacco was too different from heroin and other drugs to be considered addictive. Some people wanted to place tobacco in a separate category and apply the term “habit forming” instead.
Liquids Versus Solids: Different Gut-Brain Relationships?
During her presentation, Small had described a study showing that the relationship between caloric load and metabolic response differs for liquids versus solids, a difference that she said likely influences regulation of cue
reactivity. An audience member asked whether there was a corresponding brain imaging component of the “salad study.” Small said, “Not yet.”
Small also was asked why she chose to use salads as the solid food and whether the liquid-solid difference observed might be attributable to a difference in macronutrient content, with the salads containing few sweet components and the beverages containing many. Small replied that the salad dressing was sweetened with the same sweetener used in the beverage—maltodextrin. In fact, the dressing was basically the same flavor but a thicker substance. That said, she agreed that the difference in metabolic response could be attributable to a macronutrient difference. She and her team are following up on that possibility.
Cultural and Familial Factors to Consider
The panel was asked whether anything can be learned from cultural differences in taste preferences—for example, the greater emphasis in Asian cuisine on umami and lesser emphasis on sweet. In response, Gearhardt remarked that how one eats and when one eats may be relevant. She observed that having socially constrained periods for use of an addictive substance is a way to keep that substance from becoming a widespread problem—for example, using wine only during church services or in certain social settings. When a cultural definition of when it is appropriate to use a substance erodes, addictive-like behaviors increase. Today’s snacking and eating in the car or at the computer may be an example of that type of cultural change, Gearhardt said. In her opinion, sitting down at meals appears to have been more prominent 40 or 50 years ago than it is today.
An audience member observed that today’s children eat more unsupervised meals than children of past generations and questioned whether insufficient parenting skills related to etiquette, the use of utensils, and so on may be contributing to unhealthy eating behaviors in children. She suggested conducting future eating behavior studies with children aimed at determining whether the occurrence of family meals (as opposed to unsupervised meals) may make a difference. Gearhardt pointed to work by Julie Lumeng and Alison Miller on the relationship between child–parent interactions and different eating-related outcomes. These researchers are finding that certain parenting techniques do help, but eating-related outcomes depend on many other factors as well. For example, obesity is especially problematic in areas of low socioeconomic status, where access to food and the ability to find good child care are limited. Also, children vary in their sensitivity to food advertising. Gearhardt agreed that the American culture is shifting, with family meals not being what they used to be, but there are other factors at play as well.
The Need for Larger Studies
Edmund Rolls observed that researchers studying disorders such as autism and schizophrenia are conducting brain imaging analyses of very large databases (e.g., studies with 500 patients and 500 controls) and looking for differences. He suggested that researchers studying eating behavior adopt a similar approach, that is, collect brain imaging data in a very large database and look for correlations with individual questions from the YFAS. In the same studies, researchers could also look for biomarkers that correlate either with the activation seen in the brain imaging or responses to the questions. Rolls suggested further that such an approach would not necessarily have to be in the form of one large study. Rather, it could involve multiple teams collecting and contributing data from 20 to 50 subjects. He asked the panel whether they thought this would be a useful approach to determining whether there is a subclass of people who could be described as “addictive.”
Gearhardt replied that such a large study across multiple sites would be “really wonderful.” An important question to consider is the nature of the indicators that would be used to identify addiction. Gearhardt repeated what she had emphasized during her presentation about the use of BMI alone being insufficient. Behavioral indicators associated with addiction would be necessary, but the measures across sites would need to be similar.
Ziauddeen echoed that “[such research] is a great idea.” The one thing to keep in mind, in his opinion, is that such studies are based on specific phenotypes being examined and specific imaging data being collected. Several levels of specification are required before the data can actually be collected.
Imaging Studies of Eating Behavior: How Far Has the Methodology Advanced?
Mattes observed that new technologies often experience a “honeymoon” period when researchers use a “shotgun” approach to discovery. He asked whether the field of imaging is at a point yet where researchers should be generating hypotheses about how certain manipulations are expected to activate specific areas of the brain.
Ziauddeen replied that he would like to see the field move to the point where researchers can conduct an intervention and determine its effect without measuring that effect as a change from baseline. But the field is not at that stage yet, in his opinion. Presently, researchers can use imaging reasonably well within a controlled test/retest paradigm. That is, they collect baseline data, apply an intervention, then measure the change from baseline.
According to Small, however, at least some researchers are trying to conduct hypothesis-driven imaging studies. For example, several studies have demonstrated a relationship between dorsal striatum activation in response to a milkshake and BMI. That is, as BMI increases, the response decreases. But among individuals at risk for obesity, there is no decreased response. Small and her research team have been testing some (unnamed) compounds to see whether they can reverse that effect (i.e., increase response in the dorsal striatum that is believed to be caused by adiposity or a high-fat/high-sugar diet).
While on the topic of imaging studies, Mattes observed that most neuroimaging data are presented as dichotomous outcomes. An area of the brain is either activated or not. Mattes asked whether imaging studies are expected to gain specificity such that one will be able to observe graded responses like those being sought with behavioral measures. Ziauddeen replied that in fact, many imaging studies rely on regression analyses. For example, the studies described by Small during her presentation were regression analyses with BMI on the x-axis and gradation of activation responses on the y-axis. However, Ziauddeen agreed that many neuroimaging studies ask dichotomous questions and that the field needs to move toward greater use of continuous measures.
Reliability of the YFAS Scores
When asked by Mattes about a test-retest correlation for the YFAS over extended periods of time, Gearhardt noted that a student of hers is currently collecting those data. The YFAS has been tested more for validity than for reliability, she said.
The Concept of “Food Addiction”: Implications for the Future
A member of the audience asked: If some day it is decided, based on the evidence, that fat and sugar are addictive, given that both fat and sugar are “absolutely required” by the human body, then what? What will the implications be for the food system? Small agreed that fat and sugar are necessary for the human body, but people do not need to be consuming them at today’s levels. She expressed the hope that 20 years from now, researchers will have identified which mechanisms in the human body are being overtaxed by high-fat/high-sugar foods in the modern diet and will know how to change those foods in a way that reduces their addictive potential while maintaining their palatability. She encouraged collaboration with food industry scientists.
Also looking toward the future, another audience member asked about the clinical implications of food addiction should it become recognized as
a diagnosis at some point in the future. What would be done differently? Gearhardt explained that the cognitive-behavioral approach currently used with people who have binge eating disorder is based on cues and identification of what triggers those cues. One of the goals is to help individuals avoid situations, such as being in an extreme fasting state, that trigger binge eating. The current approach is based on the notion that there are no “good” versus “bad” foods. For example, if a person has a problem with chocolate, a therapist may suggest actually eating some chocolate and not being so restrictive. Rarely does the therapist try to help someone abstain altogether from eating chocolate or another problem food, such as french fries. If food addiction is recognized as a diagnosis at some point in the future, Gearhardt foresees a different treatment approach—one based on identifying which foods trigger the addictive response and helping people moderate their intake of or in some cases abstain from eating certain types of foods.
In response, O’Brien insisted that those approaches are already being taken. An official diagnosis of addiction, in his opinion, would not change the current psychotherapeutic approaches.
This page intentionally left blank.




































