5
Midstream: Accountable Health Communities and Partnerships with Human Services Organizations
Session moderator Rahul Rajkumar of Blue Cross and Blue Shield of North Carolina introduced the panel by explaining that it would address how accountable health communities could serve as a model for partnerships between the clinical care delivery system and community service and human services organizations. Highlights from the two presentations and subsequent discussion are provided in Box 5-1.
Rajkumar began by giving some background on accountable health communities. He was previously on the staff of the Centers for Medicare & Medicaid Services’ Center for Medicare & Medicaid Innovation (CMMI) when it launched the accountable health communities model, which he explained provides funding to “bridge organizations” for screening, referral, navigation, and encouragement of alignment (CMS, 2019). However, no CMMI funding may be used for community or social services. A forthcoming evaluation will determine whether the model will save the federal government health care costs.
THE DENVER REGIONAL ACCOUNTABLE HEALTH COMMUNITY
A. J. Diamontopoulos of the Denver Regional Council of Governments (DRCOG) Area Agency on Aging began his presentation by explaining the concept of the accountable health community. As he described it, an accountable health community identifies people in a clinical setting who are high users of medical care (two or more emergency department visits in 1 year) and have unmet health-related social needs; it then refers them
to community-based organizations to get services to address these needs. He noted that ironically, this involves offering financial resources to the health care sector, which is often well resourced, to refer their patients to the social service sector, which is often underresourced.
As Diamontopoulos outlined, the DRCOG works on five health-related social needs:
- Housing stability, such as homelessness or risk of homelessness, and housing quality, such as whether the home is clean and free of pests and mold;
- Food security;
- Utility needs;
- Interpersonal safety, such as domestic violence, elder abuse, and child abuse; and
- Transportation, which helps to connect people to services.
The primary goal is to integrate and align the screening and referral of Medicare and Medicaid beneficiaries from clinical to community services. The secondary goal is to reduce total health care costs and improve outcomes by addressing unmet health-related social needs by 2022.
Diamontopoulos described some of the challenges involved with screening people in a clinical setting and referring them to a community organization. As he explained, electronic health records have predetermined clinical settings and workflows that may not communicate with the systems at community organizations. Some community organizations also have their own privacy requirements. Others may not have the data systems in place that allow them to accept or send a secure electronic referral.
As Diamontopoulos explained, when the accountable health community model was launched in Denver in May 2017, clinical and community services providers had not previously worked with each other in a formal, structured manner. The first year was focused on development of a strategic plan, and the program got under way at the beginning of the second year. As part of the program, DRCOG is required to provide navigation services to a minimum of about 3,000 Medicare and/or Medicaid beneficiaries in six counties in the Denver area. DRCOG receives screening results from clinical partners, claims data from Medicaid, and community-level data from a small network of contracted partners. Once the data are received in full, it intends to conduct an analysis to understand the effect of the accountable health community model in the Denver region.
PARTNERSHIPS WITH AREA AGENCIES ON AGING AND OTHER COMMUNITY-BASED ORGANIZATIONS
Marisa Scala-Foley of the National Association of Area Agencies on Aging (n4a) opened by explaining that her organization works to build the capacity of community-based aging and disability organizations to partner and contract with health care entities so that older adults and persons with disabilities can live in their communities for as long as possible. The work of the Aging and Disability Business Institute (the Business Institute) at n4a, which Scala-Foley oversees, is funded by The John A. Hartford Foundation, The SCAN Foundation, and the Administration for Community Living at the U.S. Department of Health and
Human Services, and is conducted in collaboration with other national and local organizations.
From Scala-Foley’s perspective, the goal of the work of the Business Institute is to ensure that community-based organizations such as the Area Agencies on Aging that her organization represents are paid for the services they provide through contracts with health care organizations. n4a has fielded two request-for-information surveys to community-based organizations to learn more about the extent to which paid contracts exist.
As Scala-Foley explained, the survey found that the percentage of community-based organizations responding to the survey who had paid contracts to provide services or programs on behalf of or with a health care entity increased from 38 percent in 2017 to more than 41 percent in 2018. As Figure 5-1 shows, an increase in paid contracting was seen among centers for independent living, which serve people of all ages with physical disabilities; Area Agencies on Aging, which are “public or private nonprofit agenc[ies] designated by their state[s] to address the needs and concerns of all older persons at the regional and local levels” (ACL, n.d.); and other community-based organizations. The survey found the most common health care partners are Medicaid organizations, although
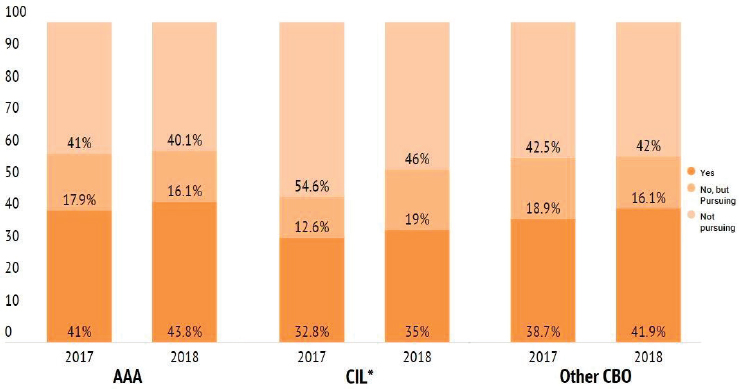
NOTES: AAA = Area Agencies on Aging; CBO = community-based organization; CIL = center for independent living. The data used in this graph were collected through a survey conducted by Scripps Gerontology Center at Miami University on behalf of the Aging and Disability Business Institute, led by the National Association of Area Agencies on Aging (n4a). For more information, visit http://bit.ly/cbo_contracts.
SOURCE: Scala-Foley presentation, September 19, 2019.
she expects that with changes to Medicare Advantage, contracts with Medicare Advantage plans will increase. As shown in Figure 5-2, top services provided include care coordination, care management, and service coordination, followed by care transitions, assessment of eligibility for long-term services, nutrition programs, and evidence-based health promotion programs.
Scala-Foley pointed out that health care organizations frequently comment that they do not want to have to contract with many small community-based organizations to serve a given geographic area and would prefer that their contracting be centrally focused. As a result, there has been an increase in community-based organizations doing business together as part of community-based integrated care networks. The survey found that in 2017, less than 20 percent of community-based organizations who were contracting with health care organizations did so through networks, but by 2018, that number had increased to more than
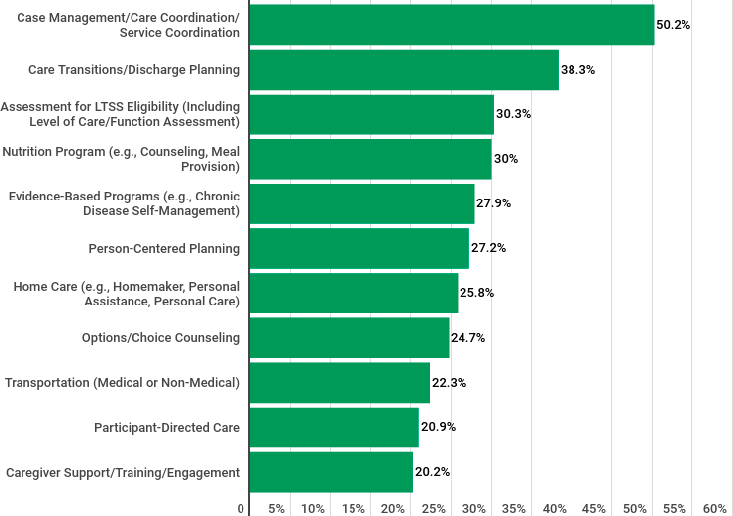
NOTES: The data used in this graph was collected through a survey conducted by Scripps Gerontology Center at Miami University on behalf of the Aging and Disability Business Institute, led by the National Association of Area Agencies on Aging (n4a). For more information, visit http://bit.ly.cbo_contracts. LTSS = long-term services and supports.
SOURCE: Scala-Foley presentation, September 19, 2019.
30 percent, a figure that Scala-Foley expects to continue to increase. Existing contracts tend to target high-risk, high needs groups.
A challenge with health care and community-based organization contracts that Scala-Foley highlighted is that health care and community-based organizations may not always use the same terminology or have the same attitudes toward issues. Diamontopoulos had also pointed out that the integration of social services referrals was a challenge.
AUDIENCE DISCUSSION
Rajkumar opened the audience discussion by asking Diamontopoulos about the advantages and disadvantages of working with payers or entities engaged in the delivery of health care. Diamontopoulos responded that participating in the accountable health communities model was part of the strategy of the Area Agencies on Aging to obtain additional funding to help it meet the needs of the population it serves. He noted that a particular challenge is the “free rider problem” of health care entities not wanting to pay for services that the community-based organizations already provide “for free.” However, Diamontopoulos pointed out that the work is not free and if health care entities provided funding, services could be increased, improved, and more targeted. A disadvantage of working with health care organizations is the time required to establish a contract. Diamontopoulos also noted the importance of community-based organizations emphasizing their expertise and value when communicating with health care entities.
Scala-Foley added that improved integration between health care and community-based services provides the opportunity to address a person’s holistic health needs. As she stated, “Health happens in clinics and hospitals, but much more of it happens in homes and in communities.” Scala-Foley further explained that since community-based organizations help to improve outcomes, and may help to generate cost savings, they should receive a share of those savings. While there has been payment reform in health care, community-based organizations addressing health-related social needs also need changes in their funding model, Scala-Foley asserted.
Rajkumar noted that the majority of the $3 trillion that the United States spends on health care is for care delivery funded through public payment systems (primarily Medicare and Medicaid) or health care premiums paid through employer-sponsored health insurance, taxes, exchanges, and fully insured products. He asked Diamontopoulos and Scala-Foley how they recommend communicating the value of community-based programs and services. Diamontopoulos responded that he thinks there will eventually be data showing that such services reduce health care costs. However, a
challenge with this research is that there cannot be a control group that is denied social services. Diamontopoulos pointed out the research already shows that providing community-based services results in fewer emergency department visits.
Scala-Foley noted that her organization regularly communicates with community-based organizations about how to present their value proposition to different types of health care organizations. She agreed with Diamontopoulos that data resulting from existing contracts between health care and community-based organizations and other research studies are helpful. Scala-Foley and Diamontopoulos shared anecdotes about how community-based organizations are often the “eyes and ears” in the home, meaning they know what the key issues are in the community and how best to address them. Scala-Foley described the importance of matching the strengths of community-based organizations and the people they serve with the needs of a particular payer.
Rajkumar expressed concern that the evaluation of the accountable health communities model will not show an effect and asked Scala-Foley and Diamontopoulos for their recommendations regarding next steps in such a situation. Diamontopoulos responded that he agreed that such a result will be likely because referrals alone are not useful. As he explained, even if a need has been identified and a patient has been referred, no relationship has been built and the patient is unlikely to access the service. Diamontopoulos highlighted the point made by Laura Gottlieb in an earlier session that only a small number of people in need use community-based services. He speculated that this is not because people do not have the need, but rather because of the way the service is provided and the relationship, or lack of such, with the community-based provider. He emphasized the importance of targeting social services to people before they develop chronic medical conditions, and he said that it may take a long time (beyond 2022) to see results. Scala-Foley added that given that the accountable health communities model provides funds for navigation and referrals rather than the direct provision of social services, it may be useful in identifying gaps in availability of, and payment for, services that can help to address a person’s holistic health needs.
Lourdes Rodriguez of the Dell Medical School at The University of Texas at Austin asked how to balance the need for deep knowledge of the communities being served with the need for uniformity of a single contracting mechanism. Diamontopoulos stated in response that the Area Agencies on Aging are the hub of a network of aging services providers. In contracting with a health care organization, they could either provide services or contract out through their usual channels. He further explained that last year his organization, DRCOG, brought approximately $14 million into the community through contracts to deliver services such
as Meals on Wheels, transportation, and legal services. Scala-Foley added that there is also a concern that social services could be overmedicalized with increased contracting between community-based organizations and health care organizations. As she explained, social service organizations need to balance the tension between being mission driven, data informed, and revenue generating so they can continue to exist, innovate, better serve, and expand the populations they serve.
Bob Kaplan of Stanford University stated that about one-third of the money that health care payers give to provider groups, hospitals, and others are for services that do not make a difference. He hypothesized that this situation is unlikely to change because hospitals, provider groups, and payers—who have satisfactory medical loss ratios—are happy with the current arrangement. Diamontopoulos agreed that asking health care payers to invest in something outside of health care is challenging because they are not used to paying for such services. He suggested that incentives through quality measures, patient satisfaction scores, and regulatory change would be helpful in changing practices. He also pointed to the need for increased understanding that clinical care is one subset of health care, with community care and public health being additional components. As Diamontopoulos explained, spending on health care is unsustainable, with an expected $2 trillion in federal funds to be spent on Medicare and Medicaid just 7 years from now. In Colorado, spending on education and health care would make up the entire state budget. Diamontopoulos highlighted the need for increased education and awareness among federal and state lawmakers and insurance companies, who he noted are “paying for the most expensive kind of care.”
Scala-Foley pointed out that changes in Medicare, including the addition of new benefits for chronically ill people in Medicare Advantage, may lead to additional changes in payment policies in Medicare fee-for-service and for private payers.
Jayla Sanchez-Warren of the DRCOG Area Agency on Aging, who works with Diamontopoulos, commented that the fact that the accountable health communities model does not allow for the payment of social services presents a challenge given the waiting lists for services. She noted that her organization had to obtain a grant from another organization to be able to provide services in conjunction with the new population that would need to be served with the accountable health communities grant. As Sanchez-Warren stated, “Referrals don’t change health outcomes. Services change health outcomes.” She further explained that a challenging aspect of the accountable health communities grant is getting people who are referred to come for services because they often face many other issues and have other priorities. For example, the people who are referred may not have the time to fill out a Supplemental Nutrition Assistance Pro-
gram application or want to be asked the required questions. Those with chronic illnesses may be too tired to obtain and prepare food after a day of doctor’s appointments. Sanchez-Warren highlighted the importance of meeting people where they are to be able to get them the services they need when they need them. For example, she noted that month-long waiting periods for services like Meals on Wheels are problematic.
John Auerbach, who was with the Centers for Disease Control and Prevention when the accountable health communities model was developed, stated that some of the expectation of screening patients for social needs was that the screening would identify needs and the health care institution would bring people together to discuss how to address them. He suggested that some of the discussion should involve consideration of which services should be paid for by health care and which may be best addressed by policy change or other nonmedical funders. For example, Auerbach explained that it was unrealistic to expect that the health care system would pay for affordable housing for every patient, but identification of the need for affordable housing could help to make the case that broader change is needed and bring policy makers to the table. Auerbach asked whether such conversations have taken place around the opportunities for funding streams from outside the health care sector.
Diamontopoulos responded that while he understands the theory behind the accountable health communities model, the variety of needs among the people the DRCOG Area Agency on Aging serves presents a challenge in its execution. For example, someone may need to prioritize addressing multiple needs, such as food, transportation, and utilities. As Diamontopoulos explained, someone who is food insecure may not have the energy to address utility challenges. He reiterated the need for increased education on the lack of investment in social services. However, Diamontopoulos suggested that health care organizations should make investments in social services such as food and housing, rather than become grocers or construction workers themselves.
This page intentionally left blank.










