3
Family Caregiving Roles and Impacts
ABSTRACT: This chapter examines the multiple and evolving roles of caregivers of older adults and the impact of assuming these roles on caregivers’ health and well-being. It describes caregiver tasks, the dynamic nature of caregiving over time, the increasing complexity and scope of caregiver responsibilities, and issues involved in surrogate decision making. Family caregiving is more intensive, complex, and long lasting than in the past and caregivers rarely receive adequate preparation for their role. A compelling body of evidence suggests that many caregivers experience negative psychological effects. Some caregivers are at higher risk than others, especially those who spend long hours caring for older adults with advanced dementia. Caregivers should have access to high-quality, evidence-based interventions designed to mitigate or prevent adverse health effects.
As a society, we have always depended on families to provide emotional support, and to assist their older parents, grandparents, and other family members when they can no longer function independently. This chapter examines the multiple and evolving roles of family caregivers of older adults and the impact of assuming these roles on caregivers’ health and well-being. It describes the trajectory and dynamic nature of caregiving over time, the increasing complexity and scope of caregiver responsibilities including the issues involved in family caregivers’ role as surrogate decision makers, and
the evidence on the impact of caregiving on the health and well-being of caregivers of older adults.
The chapter reviews an extensive literature on family caregiving of older adults. It also draws from the National Health and Aging Trends Study (NHATS) and its companion the National Study of Caregiving (NSOC), two linked federally funded surveys designed to document how functioning changes with age, the role of the family caregivers identified by the NHATS respondents who live independently or in a senior community, assisted living facility, or other residential setting (Kasper et al., 2014). Family caregivers of nursing home residents are not included in NSOC. The committee distinguished between two subgroups of NSOC family caregivers: those who help an older adult because of health or functioning reasons and those caregivers who help “high-need” older adults. “High-need” refers to family caregivers of individuals who have probable dementia or who need help with at least two self-care activities (i.e., bathing, dressing, eating, toileting, or getting in and out of bed). See Chapter 2 and Appendix E for further information about the surveys and the committee’s analyses of the publicly available survey datasets.
CAREGIVING TRAJECTORIES
Despite many common experiences, caregivers’ roles are highly variable across the course of caregiving. The diversity of families, the timing of entry into the caregiving role, the duration of the role in relation to the overall life course of the caregiver, and transitions in care experienced over time all shape the nature of the caregiving role. The committee conceptualized caregiving over time as “caregiving trajectories” to highlight the dynamic nature of the role and the different directions it can take. Caregiving trajectories include transitions in both the care needs of the older adult and in the settings in which care is provided (Gitlin and Wolff, 2012).
In populations in which the care recipients become increasingly impaired over time, such as with increasing frailty, dementia, Parkinson’s disease, or advanced cancer, the caregiving role expands accordingly. In populations in which care recipients experience short-term or episodic periods of disability, such as early-stage cancer and heart failure, the caregiving role may be short term but intense or it may wax and wane over time. Entry into the caregiving role is similarly variable. Individuals may take on the caregiving role as they gradually recognize a care recipient’s need for assistance—when an individual has difficulty balancing a checkbook, for example—or they may suddenly plunge into the caregiving role in the context of a crisis such as an unexpected life-threatening diagnosis, stroke, hip fracture, or other catastrophic event.
Caregiving for older adults occurs across all the settings in which care
is delivered and often involves interacting with numerous providers, back- and-forth transitions from hospital to home or rehabilitation facility, move to a senior residence or assisted living facility, placement in a nursing home, and ultimately end-of-life care. These transitions and role changes, along with the health and functional status of the care recipient, affect the social, physical, and emotional health of the caregiver over time (Carpentier et al., 2010; Cavaye, 2008; Gibbons et al., 2014; Peacock et al., 2014; Penrod et al., 2011, 2012; Schulz and Tompkins, 2010).
A caregiving episode can be defined both in terms of duration and intensity (i.e., the number of hours spent daily, weekly, or monthly to provide needed care to an older adult). As noted in Chapter 2, 15 percent of caregivers had provided care for 1 year or less by the time of the survey, and an equal percentage had provided care for more than 10 years.1 The remaining 70 percent fell between these two extremes. The median number of years of caregiving for high-need older adults (i.e., who had probable dementia or needed help with two or more self-care activities) was 4 years;2 it was 5 years if the care recipient had dementia and also needed help with two or more self-care activities. As might be expected, the intensity of caregiving varies with the older adult’s level of impairment. Caregivers providing assistance only with household activities spend an average of 85 hours per month providing care while those who care for an older adult with three or more self-care or mobility needs spend 253 hours per month (Freedman and Spillman, 2014), equivalent to nearly two full-time jobs.
Individuals do not provide caregiving in isolation from the other roles and responsibilities in their lives. Their personal lives—as spouse or partner, parent, employee, business owner, community member—intersect with caregiving in different ways at different times. Under ideal circumstances, the caregiver is able to balance the responsibilities and rewards of competing roles such as caring for a child or working for pay and their caregiving responsibilities. However, accumulating caregiving demands and the costs of long-term services and supports (LTSS) can overwhelm and undermine other dimensions of one’s life. Additional complexity in trajectories arises when family members disagree about the type of care needed and how it should be provided (Dilworth-Anderson et al., 2002), or when family roles and responsibilities shift over time. Appendixes F and G relate the experiences of several family caregivers: a husband, daughter, and family caring for older adults with advanced Alzheimer’s disease and a wife helping to provide complex cancer treatment to her husband in a rural area.
___________________
2 Committee calculations.
Phases in the Caregiving Trajectory
Although the caregiving role is highly variable over time, different phases in the caregiving trajectory can be discerned when the role is considered longitudinally. For example, caregiving may follow a trajectory reflecting increasing care responsibilities punctuated by episodic events such as hospitalizations and placement in rehabilitation or long-term care facilities. Figure 3-1 shows how caregiving for persons with dementia typically follows a relatively linear trajectory driven by the progressive cognitive and functional decline of the care recipient. The trajectory begins with emerging awareness of the caregiver that there is a problem. Over time this evolves into increasing care needs as the care recipient requires assistance with household tasks and then self-care tasks. End-of-life care may involve placement into a long-term care facility or enrollment in a hospice program. Note that the tasks required of the caregiver are cumulative over time. Each phase of the trajectory brings with it new challenges that the caregiver must confront.
For stroke caregivers, the trajectory may begin with sudden intensity, gradually decrease as the older adult regains function, and then remain relatively stable over a long period of time (perhaps punctuated by short-term acute illnesses or set-backs). Alternatively, caregiving may gradually increase with stroke complications, recurrence, or new comorbid conditions. Transitions in the caregiving trajectory may be planned, as in the transitions from hospital to skilled rehabilitation facility to home, or they may be unplanned, as in an emergency room visit and rehospitalization (McLennon et al., 2014).
The caregiving trajectory in the cancer population tends to be nonlinear. It is often characterized by the rapidity with which caregivers have to take on the role as treatment decisions are made and treatment begins. As the cancer experience unfolds, caregiving transitions may occur in rapid succession, each having its own learning curve in movement from one treatment modality to the next (e.g., from post-operative recovery at home to beginning radiation or chemotherapy). Transitions among care settings also occur unpredictably. For example, transitions from home to emergency room to hospital are unpredictable but not uncommon. Moreover, the functional abilities of older adults with cancer may fluctuate rapidly, resulting in intense but short periods of caregiving. Rapid transitions in the caregiving role may occur in the context of advanced cancer as well, as the care recipient moves from management of advanced cancer symptoms (e.g., pain, sleep disturbance, and lack of appetite) through a succession of changes in functional status and self-care ability, leading ultimately to end-of-life care and bereavement. The rapid succession of caregiving transitions, some of
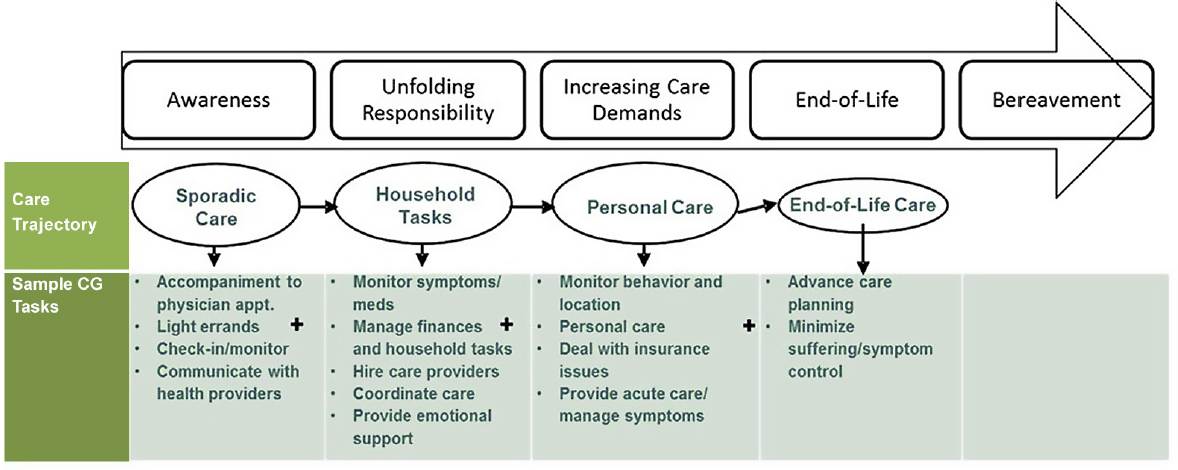
NOTE: CG = caregiving.
SOURCES: Adapted from Gitlin and Schulz (2012) and Schulz and Tompkins (2010).
which may occur with little warning, challenge caregivers’ ability to provide care, as ability during one phase of the caregiving trajectory may or may not be sufficient to meet the demands of the next phase.
These are just a few of the varied trajectories associated with three common late-life illnesses. Each disease brings with it a unique pattern of unfolding needs that the caregiver must address. However, when considered over the long term, typical phases in caregiving trajectories can be discerned, as depicted in Figure 3-1. These phases are described below, with the caveat that they are not necessarily linear (Gitlin and Schulz, 2012; Gitlin and Wolff, 2012; Schulz and Tompkins, 2010).
Awareness
This phase includes recognition and increasing awareness within the older adult’s social network of disabilities, changes in health, and/or behavioral change that signal the need for some level of caregiving. The older adult may downplay the need for care during this phase because of their concerns about becoming a burden to others (Cahill et al., 2009). Awareness of functional impairment can come on gradually, as in the case of someone with slowly progressive dementia, or suddenly as in the case of someone who has suffered a stroke or traumatic brain injury. With awareness that one is becoming a caregiver comes an array of daunting questions about how to meet the needs of the care recipient. How long will these needs, which may become increasingly more complex, have to be met and what will it take to meet these needs? How much family involvement will be necessary and how will caregiving roles within the family or broader social network be negotiated? What are the risks, costs, and benefits to whom over time? How much time will be involved in meeting these needs and how much involvement will be necessary? If paid help is needed to supplement family care, how much will it cost and can the family afford it? How can care needs be met in relationship to cultural norms and expectation?
In response to this awareness of need for caregiving on the part of the older adult and/or family members, one or more family members typically emerge as the caregivers. Who ends up being a caregiver within a family is often shaped by existing relationships, gender roles, cultural norms and expectations, and geographic proximity as well as a host of other factors (Cavaye, 2008). For example, African American caregivers are more likely to be non-spouses compared with white, non-Hispanic caregivers (NAC and AARP Public Policy Institute, 2009; Pinquart and Sörenson, 2005). Lesbian, gay, bisexual, and transgender (LGBT) individuals are more likely to care or be cared for by a non-relative than non-LGBT individuals (Fredriksen-Goldsen et al., 2011). Ultimately, one or more family members may take on the caregiving role and its varied responsibilities.
Unfolding Responsibility
As caregivers move into their role, they may experience role ambiguity, a redefining of their relationships with the care recipient and others, and may perceive stigma and/or experience discrimination as a result of the care recipient’s condition (Gibbons et al., 2014). There are social changes with a shift from usual participation in life activities to a focus on the challenge of being a caregiver. The unpredictability of the illness experience of the care recipient may lead to uncertainty about the future. The confidence of the caregiver with respect to their caregiving role is linked to the illness status of the care recipient and the caregiver’s knowledge and skills in addressing care recipient needs (Gibbons et al., 2014). Along with awareness of caregiving responsibilities, caregivers may also be engaged in trying to make sense of the older adult’s impairments. For example, there is considerable variability in conceptions of dementia depending on the culture and educational level and socioeconomic status of the family caregivers (Hinton, 2002).
Increasing Care Demands
Schulz and Tompkins (2010) illustrate the caregiving trajectory for a typical older individual with functional decline who lives in the community and who over time experiences increasing reliance on the caregiver for assistance. The initial tasks may involve monitoring clinical symptoms and medications, as well as managing household tasks, communicating with health professionals, and providing emotional support to the care recipient. Over time, caregiving tasks often expand to include providing self-care tasks, becoming a surrogate decision maker for the care recipient, and providing specialized medical care such as giving injections. The diversity of tasks performed by caregivers is described in detail below. The common factor in the middle to late stages of a caregiving trajectory is the expansion and increased complexity and intensity of the caregiver’s roles and responsibilities.
End of Life
This phase along the care trajectory may also involve nursing home care and repeated hospitalizations as the care recipient declines and ultimately dies. Although many caregivers become involved in end-of-life caregiving, few studies make explicit distinctions among the needs and experiences of family caregivers during disease-directed treatment, palliative or supportive care, and end-of-life phases (Schulz, 2013). The few studies that do focus on caregivers during the end-of-life phase suggest that caregiving demands
become more urgent and intensive (Gibbons et al., 2014; Penrod et al., 2012). Caregivers continue to report high levels of burden and stress, but also find greater meaning and purpose in the experience of caregiving at the end of life (Emanuel et al., 2000; Gibbons et al., 2014; Wolff et al., 2007). To better understand caregiving during this critical phase in the trajectory, more fine-grained prospective studies are needed that clearly delineate the transition from disease management to supportive care to end-of-life care, and how these transitions affect the caregiver and formal care provided to the care recipient.
In summary, the caregiving role changes over time in concert with changes in the older adult’s care needs, transitions from one care setting to another, and changes in the familial, social, and geographic contexts for caregiving. Diversity in family structures, norms, values, and relationships shape how the caregiving trajectory unfolds. Although typical phases in the caregiving trajectory can be identified, they are not necessarily linear and some degree of unpredictability always exists. Thus, caregivers’ needs can be expected to change over time, indicating the need for assessment and periodic reassessment, as discussed below. Reassessment is especially important during transitional periods.
ROLES OF FAMILY CAREGIVERS
Despite the unique nature of any given caregiver’s role over time, broad domains of activity characterize family caregiving. Caregiving ranges from assistance with daily activities and providing direct care to the care recipient to navigating complex health care and social services systems. The domains of the caregiving role include: assistance with household tasks, self-care tasks, and mobility; provision of emotional and social support; health and medical care; advocacy and care coordination; and surrogacy. Each domain has multiple tasks and activities (see Table 3-1). Cutting across
TABLE 3-1 What Family Caregivers Do for Older Adults
| Domain | Caregivers’ Activities and Tasks |
|---|---|
| Household tasks |
|
| Domain | Caregivers’ Activities and Tasks |
|---|---|
| Self-care, supervision, and mobility |
|
| Emotional and social support |
|
| Health and medical care |
|
| Advocacy and care coordination |
|
| Surrogacy |
|
SOURCES: Spillman et al., 2014; Wolff, 2007.
these domains are ongoing cognitive and interpersonal processes in which caregivers engage including, for example, continual problem solving, decision making, communicating with others (family members and health and human service professionals), and constant vigilance over the care recipient’s well-being (Gitlin and Wolff, 2012). How caregivers manage these tasks depends on their values, preferences, knowledge, and skills, as well as the accessibility, affordability, and adequacy of health care, LTSS, and other resources, as described further in Chapter 6.
The particular mix of caregiving activities and time commitments varies. In multiple studies, caregiving for persons with dementia has been shown consistently to be one of the most demanding types of caregiving (Ory et al., 1999; Pinquart and Sörenson, 2007). However, a 2004 survey found that the amount of care and level of burden experienced by cancer and dementia caregivers were nearly equivalent, but that specific tasks varied (Kim and Schulz, 2008). For example, cancer caregivers were more likely than dementia caregivers to provide help in getting in and out of bed, whereas dementia caregivers were more likely to deal with incontinence.
The caregiving experience also varies by distance. Long-distance caregivers who live at least 1 hour from the care recipient are typically involved in providing social and emotional support, advanced care planning, financial assistance, and care-coordination. They often share these responsibilities with a more proximal caregiver who provides assistance with personal care. Being separated from the care recipient complicates communication about the care recipient’s health and care needs, and poses formidable challenges to address those needs through service providers. Because virtually all of the data on distance caregivers are based on small and/or non-representative samples, caution is warranted in drawing firm conclusions based on these findings (Cagle and Munn, 2012). Better data are needed on the prevalence of long-distance caregiving, identifying who they are, the tasks they perform, and the impact caregiving has on their lives.
Assisting with Household Tasks, Self-Care, Mobility, and Supervision
Nearly all caregivers help older adults in need of care with household tasks such as shopping, laundry, housework, meals, transportation, bills, money management, and home maintenance (NAC and AARP Public Policy Institute, 2015; Spillman et al., 2014; Wolff et al., 2016). As indicated in Figure 3-2, these responsibilities are often daily ones if the older adult needs help because of health or functional limitations: 44 percent of caregivers reported helping with chores every day or most days.
Self-care and mobility tasks include walking, transferring (e.g., getting in and out of bed and chairs, moving from bed to wheelchair), bathing or showering, grooming, dressing, feeding, and toileting (e.g., getting to and
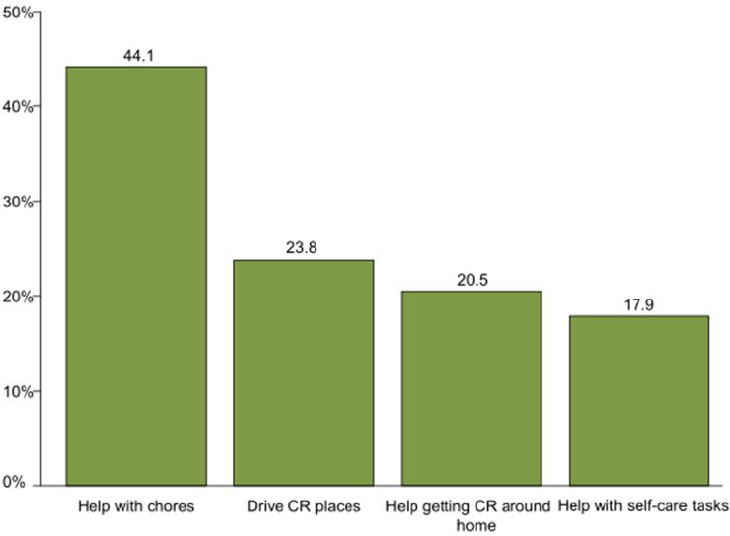
NOTES: Includes family caregivers of Medicare beneficiaries age 65 and older in the continental United States who resided in community or residential care settings (other than nursing homes) and received help with self-care, mobility, or household activities for health or functioning reasons. CR = care recipient.
SOURCES: Data from the 2011 NHATS and the companion NSOC.
from the toilet, maintaining continence, dealing with incontinence). Help with self-care tasks is a frequent and sometimes daily role for some caregivers; 17.9 percent of caregivers reported helping with self-care every day or most days.
Caregivers providing care to “high-need” older adults—those who have at least two self-care needs or dementia—are more likely to help with a wide variety of tasks, including helping with chores, helping the older adult get around the house, keeping track of medications, and making medical appointments. Older adults with both dementia and two or more self-care needs receive the highest levels of help from caregivers: 42 percent of their caregivers provide help with self-care tasks every day or most days. In addition, caregivers of high-need older adults also help with medication management (65 percent), medical tasks (20 percent), and with skin care
| Tasks | Care Recipient’s Dementia Status and Need for Help | |||
|---|---|---|---|---|
| Dementia Only | No Dementia; Has Two or More Self-Care Needs | Dementia; Has Two or More Self-Care Needs | No Dementia; Has Less Than Two Self-Care Needs | |
| How often did you help . . . | Every day or most days (percentage) | |||
|
With chores |
44.6 | 55.6 | 49.7 | 38.7 |
|
With self-care |
10.5 | 32.0 | 42.0 | 8.6 |
|
Drive care recipient places |
24.8 | 25.8 | 19.2 | 24.2 |
|
Help care recipient get around his/her home |
14.8 | 35.7 | 37.4 | 12.4 |
| Did you help . . . | Yes (percentage) | |||
|
Keep track of meds |
61.2 | 57.4 | 65.4 | 36.8 |
|
Care recipient take shots or injections |
6.3 | 13.3 | 12.0 | 5.3 |
|
Manage medical tasks |
9.2 | 17.2 | 20.5 | 6.0 |
|
With special diet |
25.8 | 40.5 | 30.9 | 22.9 |
|
With skin care wounds |
17.0 | 34.0 | 35.2 | 18.2 |
|
Make medical appointments |
74.6 | 59.1 | 75.0 | 52.0 |
|
Speak to medical provider |
65.9 | 52.1 | 71.6 | 47.2 |
|
Add/change health insurance |
29.3 | 24.1 | 30.9 | 22.5 |
|
With other insurance matters |
37.7 | 35.5 | 47.0 | 27.6 |
| Population represented (in 1,000s) | 2,931 | 2,745 | 2,828 | 9,190 |
NOTES: Includes family caregivers of Medicare beneficiaries age 65 and older in the continental United States who resided in community or residential care settings (other than nursing homes) and received help with self-care, mobility, or household activities for health or functioning reasons. Self-care activities are bathing, dressing, eating, toileting, or getting in and out of bed. “Probable dementia” includes individuals whose doctor said they had dementia or Alzheimer’s disease and individuals classified as having probable dementia based on results from a proxy screening instrument and several cognitive tests.
SOURCES: Data from the 2011 NHATS and the companion NSOC.
wounds (35 percent) (see Table 3-2). Older adults with dementia or other conditions that severely impair cognitive function may also require constant supervision and hands-on assistance because of their functional limitations and behavioral symptoms.
Providing Emotional and Social Support
When older adults first need caregiving because of increasing frailty or onset of a debilitating disease, they need emotional and social supports that are different from the usual exchanges among family members (Brody, 1985). One important change is in the balance of reciprocity in the caregiver–care recipient relationship. With increasing needs, the care recipient may be able to give less to the relationship while needing more from it, despite efforts to maintain some reciprocity (Pearlin et al., 1990). In addition, the care recipient’s own emotional response to his or her changing circumstances may require a higher level of emotional support from the caregiver. Caregivers may find themselves dealing with unfamiliar depressive symptoms, anxiety, irritability, or anger in the care recipient.
These changes may be so subtle as to be nearly imperceptible at first. With advancing frailty, changes in the relationship may be recognized only retrospectively after they have been underway for some time. Conversely, relationship changes may occur suddenly, as with a stroke. For example, among stroke caregivers, the most stressful problems are in the caregiver–stroke survivor relationship (including poor communication, frustration with role reversal, and intimacy issues) (King et al., 2010). The task perceived as most time consuming by caregivers was providing emotional support (Bakas et al., 2004). In a study focused on the first year of caregiving after a stroke, caregivers surveyed 8 to 12 months after the stroke event reported that the problems perceived as most stressful were that the care recipient appeared sad or depressed, talked about feeling lonely, had problem controlling bowels, felt worthless or like a burden, and/or appeared anxious or worried (Haley et al., 2009).
Health and Medical Care
Family involvement in health and medical tasks at home is not new, but it has become more common, and is often far more complex than in the past. Older adults’ homes have become de facto clinical care settings where caregivers are performing an array of nursing or medical tasks once provided only by licensed or certified professionals in hospitals and nursing homes (Reinhard and Feinberg, 2015; Reinhard et al., 2012). This is, in part, the result of ongoing efforts to shorten lengths of hospitalizations and reduce nursing home placements, coupled with increasingly complex
options for the medical treatment of chronic and acute conditions in non-institutional settings. The “Home Alone” study by the AARP Public Policy Institute and the United Hospital Fund documented the marked impact of this trend on the roles of caregivers. More recent caregiver surveys continue to find similar results (Kasper et al., 2014; Reinhard and Feinberg, 2015; Spillman et al., 2014; Wolff et al., 2016).
The health and medical care domain of the caregiving role is increasingly complex. Medications were once simply administered. Today, medications prescribed for home use are delivered not only by mouth but also via patches, injections, and intravenously. When the care recipient is seriously ill or severely impaired, the caregiver may also be managing technical procedures and equipment, such as feeding and drainage tubes, catheters, and tracheostomies, as well as managing symptoms and monitoring the care recipient’s condition. During cancer treatment, for example, caregivers are called on for numerous health and medical care activities at home, including symptom and side effect management, nutrition, hands-on procedures (e.g., wound care and infusion pumps), management of acute conditions (e.g., fever, dehydration, or delirium), and management of complex medication regimens (e.g., oral chemotherapeutic agents, injections, and an array of symptom management medications) (Bond et al., 2012; Given et al., 2012; Krouse et al., 2004; Schumacher et al., 2000; Silver et al., 2004; Swore Fletcher et al., 2012; van Ryn et al., 2011). When older adults have other chronic medical conditions in addition to cancer, such as cardiovascular disease, diabetes, arthritis, or a mental health condition, the management of these co-morbidities may be greatly complicated by cancer treatment (Given et al., 2012; Glajchen, 2004).
Advocacy and Care Coordination
Family caregivers often serve as advocates and care coordinators. As advocates, their role is to identify and to help care recipients obtain needed community and health care resources. This may involve determining the care recipient’s eligibility for specific services and the potential costs. More often than not, the older adult and the caregiver encounter bewildering and disconnected systems of care that involve an array of entities including health care providers, public- and private-sector community-based agencies, employers, and multiple potential payers (e.g., Medicare, Medicaid, and private Medigap plans) (Bookman and Kimbrel, 2011). Caregivers must navigate these multiple, evolving, and increasing complex systems, often without assistance.3 The role of coordinator often falls to the family caregiver, who must patch together the services that an older adult needs and
___________________
3 See Chapter 6 for a discussion of caregivers’ interaction with the health care system.
also serve as the primary communication link among all the involved parties. Many people, such as some racial or ethnic groups, LGBT caregivers, and individuals with limited health literacy, face the additional challenge of finding culturally and linguistically tailored services appropriate to their care recipients’ needs (Coon, 2007; Dilworth-Anderson, 2002; Fredriksen-Goldsen and Hooyman, 2007; Nápoles et al., 2010).
The role of family caregivers following discharge of their care recipient from a hospital or skilled nursing facility is important but currently understudied. The caregiver’s specific role during this process may vary based on the care needs of the older adult, the caregiver’s relationship to the older adult, and where the caregiver lives in relation to the older adult (Gitlin and Wolff, 2012). Given that current research shows the availability and preparedness of caregivers can affect the quality and course of care recipients’ post-hospitalization care and that caregivers are often underequipped, outlining and defining these roles is important to designing possible interventions to help caregivers during the discharge process (Gitlin and Wolff, 2012). Chapter 6 discusses current interventions that seek to support caregivers during the discharge and care transition process.
More than three-quarters of caregivers (77 percent) reported helping with health systems interactions; many also assisted with making appointments (67 percent), speaking to doctors (60 percent), ordering medications (55 percent), adding or changing insurance (29 percent), or handling other insurance issues (39 percent) (see Figure 3-3).
Family caregivers continue to be involved with older adults who move into residential facilities (e.g., assisted living facilities and nursing homes). They perform tasks similar to those they carried out in the care recipient’s home, providing emotional support and companionship, as well as feeding, grooming, managing money, shopping, and providing transportation. For example, in interviews with 438 such caregivers between 2002 and 2005, Williams and colleagues (2012) found that more than half of the caregivers had monitored care recipient health status, managed care, and assisted with meals; 40 percent assisted with self-care tasks. Caregivers may also take on new tasks when their care recipient moves into a residential facility, interacting with the facility’s administration and staff, advocating for the resident, and serving as his or her surrogate decision maker (Friedemann et al., 1997; Ryan and Scullion, 2000).
Advocacy and care coordination in formal care settings can be especially challenging. A transition to a new care setting often requires the caregiver to coordinate a new array of services and providers, serve as a communication conduit between settings, and seek new information to ensure that the care recipient’s needs are met.
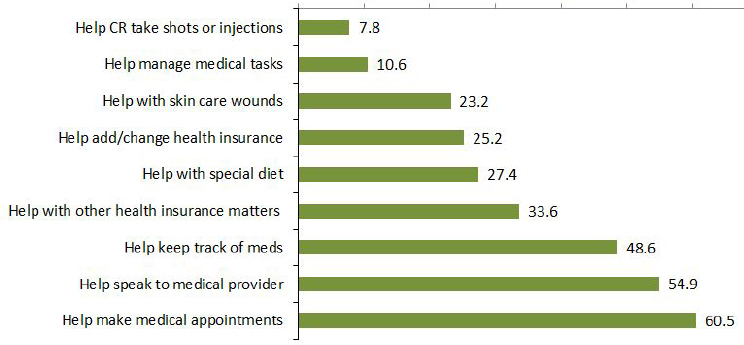
NOTES: Includes family caregivers of Medicare beneficiaries age 65 and older in the continental United States who resided in community or residential care settings (other than nursing homes) and received help with self-care, mobility, or household activities for health or functioning reasons. CR = care recipient.
SOURCES: Data from the 2011 NHATS and the companion NSOC.
Decision Making and Surrogacy
In 2010, at my parents’ request, I received both general and healthcare powers of attorney. The healthcare power of attorney contains both a living will and a HIPAA [Health Insurance Portability and Accountability Act] authorization, and gives me broad authority to get health information and make decisions. (I carry them with me at all times on a USB memory stick.) (Kenyon, 2015)
Caregivers are often involved in decision making with and, in some circumstances, for care recipients. However, the nature of caregivers’ involvement varies. Types of decision-making roles include directive; participatory; supportive or guiding; advisory; advocacy; and trying to hold back and let the older adult decide (Garvelink et al., 2016). Care recipients with cognitive impairments may require surrogate decision making, as discussed below, although individuals with mild to moderate cognitive impairment often have the ability to express preferences and make choices (Feinberg and Whitlatch, 2001; Whitlatch, 2008). Frail older adults may be able to express their preferences, but lack executional autonomy or the ability to carry out their decisions without considerable assistance from a caregiver (Gillick,
2013). Caregivers and care recipients may confront many kinds of decisions, including decisions about treatment choices, location of care, and end-of-life care (Edwards et al., 2012; Garvelink et al., 2016; Gillick, 2013).
Decision making involves both older adult and caregiver values, preferences, needs, goals, abilities, and perceptions, which may or may not be congruent and in some instances may be in conflict (Garvelink et al., 2016; Kitko et al., 2015; Moon et al., 2016; Whitlatch and Feinberg, 2007). Decision making also involves religious considerations, family dynamics, finances, and feasibility (Garvelink et al., 2016). While respecting the rights of the care recipient and making sure his or her voice is primary, good communication and finding a balance between the care recipient’s needs and preferences and the caregiver’s ability to meet them contribute to the well-being of both parties (Whitlatch, 2008). Multiple legal tools such as health care and financial powers of attorney, living wills, and personal care agreements can help family caregivers and their families to better outline the preferences of the care recipient and the scope of his or her caregiver’s decision making authority (Sabatino, 2015).
Although supported decision making attempts to give individuals the assistance they need to make decisions for themselves to the greatest extent possible, many individuals with advanced illnesses lack decision making capacity and therefore need to rely on surrogates. Studies show that family members are involved in decision making for nearly half (47 percent) of hospitalized older adults, including 23 percent needing all decisions made by a surrogate (Torke et al., 2009, 2014).
Most individuals prefer to involve family members in medical decisions and have family serve as surrogate decision makers when the individual loses decision-making capacity (Kelly et al., 2012). Some individuals step into the role of surrogate formally by being appointed under an advance directive or power of attorney or by a court in a guardianship proceeding. Others may fall into the role by default by virtue of being a close family member or friend. For health care decisions, the prevailing paradigm for default surrogate decision makers is a nuclear family hierarchy although some states also recognize close friends at the end of the hierarchy (ABA Commission on Law and Aging, 2014). This next-of-kin model lacks flexibility for accommodating diverse family structures and decision-making practices.
Family surrogates also face surrogate decision-making tasks far beyond health decisions. The management of the care recipient’s affairs including financial, legal, and insurance issues is common. There is no counterpart to health care default surrogate decision-making laws for financial affairs. Family members must have some type of formal authority to make decisions for the care recipient by means of some form of co-ownership (e.g., joint bank accounts) or they must be appointed to manage financial affairs
as a fiduciary typically by means of a durable power of attorney for finances or a trust. They are often unfamiliar with these legal options and unprepared to take on the fiduciary roles bestowed by these legal tools.
Preparedness for Caregiving
Given the multifaceted and complex nature of the caregiving role as described above, preparedness for caregiving is essential. Caregivers need specialized knowledge and skills relevant to their particular needs, as well as broadly defined competencies, such as problem-solving and communication skills (Gitlin and Wolff, 2012). Yet the available evidence indicates that many caregivers receive inadequate preparation for the tasks they are expected to assume. In the 2015 National Alliance for Caregiving and AARP Public Policy Institute survey, half (51 percent) of caregivers of older adults age 50 and older with Alzheimer’s disease or dementia reported that they provide medical/nursing tasks without prior preparation. Thirty percent of Alzheimer’s disease caregivers had informational needs about managing challenging behaviors and 21 percent wanted more help or information about incontinence. In the Home Alone study, more than 60 percent of the caregivers reported learning how to manage at least some medications on their own (Reinhard et al., 2012). Forty-seven percent reported never receiving training from any source. Caregivers described learning by trial and error and feared making a mistake.
In summary, the family caregiving role is broad in scope, and often requires a significant commitment of time. The complexity of the caregiving role has increased in recent years. Whereas families traditionally have provided emotional support and assisted their older members with household and self-care tasks, family caregivers now provide health and medical care at home, navigate complicated and fragmented health care and LTSS, and serve in a surrogacy role that has legal implications. Given the scope and complexity of the family caregiving role, ensuring that caregivers are well prepared is essential. Yet caregiver educational needs are not systematically addressed and training in the performance of caregiving tasks is inconsistent at best.
The scope, time commitment, and complexity of the family caregiving role make it unique in the care of older adults. No single health care or social service discipline is charged with providing assistance with self-care and household tasks, providing emotional support, and performing health and medical tasks around the clock, 7 days per week; advocating for an older adult’s needs, values, and preferences in multiple health care and LTSS settings; and functioning in a legal capacity as a surrogate decision maker. Health and social service professionals and direct care workers “hand off” responsibility to others, whereas many family caregivers do not have the option of handing off their responsibilities. Given the essential role they
play, involving family caregivers as key partners in health care and LTSS settings is vitally important, as discussed further in Chapter 6.
THE IMPACT OF CAREGIVING ON THE CAREGIVER
The effects of caregiving are both wide ranging and highly individualized. Caregivers are potentially at increased risk for adverse effects on their well-being in virtually every aspect of their lives, ranging from their health and quality of life to their relationships and economic security. However, the actual consequences for individual caregivers are variable, depending on a host of individual and contextual characteristics.
Data from NSOC provide an overview of both negative and positive impacts of caregiving. For example, more than 20 percent of caregivers report that caregiving is financially and physically difficult for them, and 44 percent report that it is emotionally difficult. High rates of difficulty are particularly prevalent among caregivers providing intensive levels of care. As one would expect, caring for persons with high care needs such as persons with dementia or self-care needs creates more difficulties for the caregiver than persons with lesser needs. These caregivers also report relatively high rates of exhaustion, being overwhelmed, and not having enough time for themselves (see Table 3-3).
Caregivers also find benefit in caregiving. As shown in Figure 3-4, helping the care recipients often instills confidence in the caregivers, teaches them how to deal with difficult situations, makes them feel closer to the care recipient, and assures them that the care recipient is well-cared for. It is important to note, however, that these positive effects can co-exist with the negative impact of caregiving. Caregivers can simultaneously feel highly distressed and report that they derive benefit from the caregiving experience (Beach et al., 2000).
Psychological Effects
As noted above, caregivers experience both positive and negative psychological effects from caregiving (Pinquart and Sörensen, 2003), but research has by far focused on negative effects. The effects of caregiving are variable, depending on characteristics intrinsic and extrinsic to the individual. Nevertheless, the body of evidence on negative effects is far larger than that on positive effects, as researchers have sought to assess the public health implications of caregiving and identify vulnerable at-risk caregivers. Documenting the adverse effects of family caregiving on both caregivers and care recipients is a requisite first step in developing interventions and public policy to address the needs of caregivers.
| Difficulties | Care Recipient’s Dementia Status and Level of Impairment | |||
|---|---|---|---|---|
| Dementia Only | No Dementia; Has Two or More Self-Care Needs | Dementia; Has Two or More Self-Care Needs | No Dementia; Has Less Than Two Self-Care Needs | |
| Percentage of caregivers reporting . . . | ||||
|
Emotional difficulty |
48.8 | 45.5 | 56.5 | 38.1 |
|
Physical difficulty |
20.4 | 28.5 | 39.6 | 16.4 |
| Percentage of caregivers responding “very much” . . . | ||||
|
Exhausted at night |
17.0 | 19.6 | 25.3 | 11.8 |
|
More things to do than they can handle |
26.7 | 18.0 | 23.9 | 11.7 |
|
Don’t have time for themselves |
23.3 | 14.3 | 24.3 | 10.0 |
| Population represented (in 1,000s) | 2,931 | 2,745 | 2,828 | 9,190 |
NOTES: Includes family caregivers of Medicare beneficiaries age 65 and older in the continental United States who resided in community or residential care settings (other than nursing homes) and received help with self-care, mobility, or household activities for health or functioning reasons. Self-care activities include bathing, dressing, eating, toileting, or getting in and out of bed. Excludes caregivers of nursing home residents. “Dementia only” refers to care recipients with possible dementia and less than two self-care needs. “Probable dementia” includes individuals whose doctor said they had dementia or Alzheimer’s disease and individuals classified as having probable dementia based on results from a proxy screening instrument and several cognitive tests.
SOURCES: Data from the 2011 NHATS and the companion NSOC.
Harms
Negative psychological effects of caregiving span a continuum ranging from the perception that caregiving is stressful or burdensome, to symptoms of depression and/or anxiety, to clinical depression diagnosed by a health professional, to impaired quality of life (Schulz and Sherwood, 2008; Zarit et al., 1980).
Assessment of psychological effects in research includes evaluation of individual psychological constructs (e.g., burden, depression, or anxiety) and the use of global inventories of mental health that encompass both depression and anxiety and instruments aimed at characterizing general
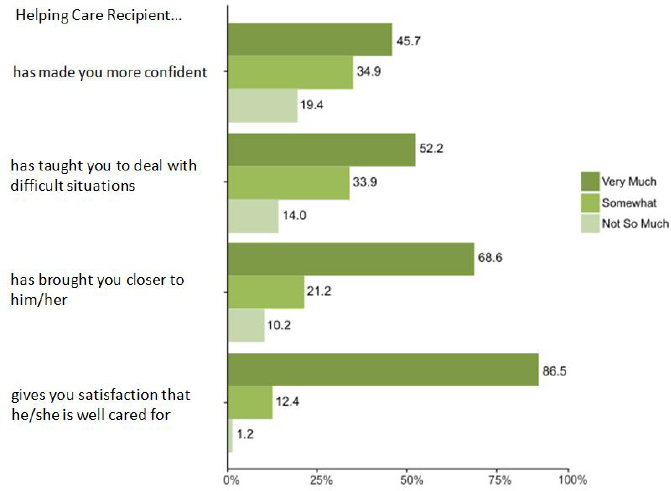
NOTES: Includes family caregivers of Medicare beneficiaries age 65 and older in the continental United States who resided in community or residential care settings (other than nursing homes) and received help with self-care, mobility, or household activities for health or functioning reasons.
SOURCES: Data from the 2011 NHATS and the companion NSOC.
well-being and quality of life in the caregiver. Both caregiver self-report and clinical interviews with diagnostic criteria are used in research. Samples may be heterogeneous or more narrowly targeted to particular groups of caregivers (e.g., spouses or particular clinical populations).
A large and robust literature documents higher rates of psychological distress among caregivers compared with non-caregiver comparison groups. Evidence has been steadily accumulating during the 20 years that have elapsed since one of the earliest reviews by Schulz and colleagues (1995) and now includes a vast number of individual clinical studies, multiple systematic reviews (e.g., Cuijpers, 2005; Pinquart and Sörensen, 2003), and an increasing number of population-based epidemiological studies (Capistrant, 2016; Wolff et al., 2016). Much of this literature is based on cross-sectional studies in which caregivers are compared to comparable non-caregivers.
Since matching is always imperfect, these studies raise questions about the net effect of caregiving as opposed to selection biases that may be associated with caregiver outcomes. For example, shared life-style factors in married couples would predict that disability and psychological distress in one partner is associated with similar characteristics in the other. Thus, an outcome attributed to caregiving such as depression may be a reflection of underlying vulnerabilities shared by both partners (Roth et al., 2015). A more compelling case for the causal relationship between caregiving and psychological distress, for example, can be made from longitudinal studies in which individuals are followed into, throughout, and out of the caregiving role. These studies demonstrate significant declines in well-being as the person enters the caregiving role, further deterioration in well-being as care demands increase, and recovery after the care recipient dies (Beach et al., 2000; Dunkle et al., 2014; Hirst, 2005; Kurtz et al., 1995; Schulz et al., 2003). Intervention studies (see Chapter 5) showing improvement in caregiver health and wellbeing when caregiving needs are addressed also support causal connections between caregiving and well-being outcomes.
The prevalence of negative psychological effects among caregivers indicates that large segments of the caregiving population experience adverse effects. For example, 26 percent of all caregivers and 29 percent of those caring for the most disabled older adults reported substantial emotional difficulties in NSOC (Spillman et al., 2014). Thirteen percent of all caregivers and 15 percent of those caring for the most disabled older adults reported symptoms of anxiety and depression. In a study of caregivers of individuals who experienced a stroke, Haley and colleagues (2009) found that 14 percent of stroke caregivers reported clinically significant levels of depression. Even higher rates of depression are found in the dementia caregiving population. In a systematic review of 10 studies in this population, the prevalence rate for depressive disorders was 22.3 percent using standardized diagnostic criteria (Cuijpers, 2005). Among cancer caregivers, 25 percent reported clinically meaningful levels of depressive symptoms 2 years after the care recipient’s diagnosis (Girgis et al., 2013; Kim et al., 2014).
In a meta-analysis of 84 studies, caregivers again were found to experience more depression and stress and less general subjective well-being than non-caregivers (Pinquart and Sörensen, 2003). Although differences in psychological well-being between whites and racial and ethnic subgroups are generally small, several systematic reviews report that African American caregivers tended to report lower levels of caregiver burden and depression than white, non-Hispanic caregivers while Hispanic and Asian American caregivers reported more depression than white caregivers (Nápoles et al., 2010; Pinquart and Sörensen, 2005). In a systematic review, Cuijpers (2005) found that the relative risk for clinical depression among dementia caregivers compared with non-caregivers in six studies ranged from 2.80
to 38.68. In an analysis of data from the prospective Nurses’ Health Study, women who provided 36 or more hours of care per week to a disabled spouse were nearly 6 times more likely than non-caregivers to experience depressive or anxious symptoms (Cannuscio et al., 2002).
Family caregiver depressive symptoms and anxiety persist when the care recipient moves to a long-term care facility with similar severity as when they were providing in-home care, and antianxiety medication use has been found to increase before and after placement (Schulz et al., 2004). Indeed, the greater the hands-on care provided by the family caregivers, the higher their distress, and the lower their satisfaction with care provided by the nursing home staff (Tornatore and Grant, 2004). Causes of distress among caregivers include inadequate resident self-care, lack of communication with nursing home physicians, and challenges of surrogate decision making, including the need for education to support advance care planning and end-of-life decisions (Givens et al., 2012). Although the findings on the experience and impact of family caregiving in LTSS settings are consistent across studies (Gaugler, 2005), individual study samples are not necessarily representative of this population, making it difficult to generate population-level estimates for these indicators.
Longitudinal studies of psychological health effects among caregivers over time suggest that negative effects vary across the caregiving trajectory, although there may be critical periods when caregivers are most at risk for elevated psychological distress. In an analysis of longitudinal data from the British Household Panel Survey, Hirst (2005) found that negative psychological effects among heavily involved caregivers were most pronounced around the transitional periods of the start of caregiving and when caregiving ends. Longitudinal data from the Nurses’ Health Study (Cannuscio et al., 2002) and the Health and Retirement Study (Dunkle et al., 2014) also indicate that the transition into the caregiving role is a time of elevated risk for increased depressive symptomatology.
However, caregiving over a long period of time may also have negative psychological effects. The American Cancer Society National Quality of Life Survey for Caregivers, which included follow-up assessments 2 and 5 years after cancer diagnosis, found that those who were still caregiving at 5 years had the largest increase in depressive symptoms and the poorest quality of life when compared to caregivers for a recipient now in remission or bereaved caregivers of recipients who had died (Kim et al., 2014). Among the group that was still caregiving, the level of clinically meaningful depressive symptoms rose from 28 percent at 2 years to 42 percent at 5 years (Kim et al., 2014).
A different longitudinal pattern was found in the stroke population, suggesting that the impact of caregiving over time may vary across clinical populations. In the Caring for Adults Recovering from the Effects of Stroke
(CARES) study, caregivers at 9 months after a stroke had significantly higher depressive symptoms than non-caregiving controls. However, this difference decreased over time, suggesting that caregivers are able to adapt to caregiving demands that remain relatively stable over time (Haley et al., 2015).
Positive Aspects
Although a substantial proportion of the caregiver population experiences negative psychological effects, many also find caregiving rewarding. Thus, a growing number of studies focus on the positive effects of caregiving in order to better understand the potential for personal growth and the mental health-promoting aspects of caregiving (Brown and Brown, 2014; Roth et al., 2015). However, as yet, fewer systematic reviews and population-based studies are available for positive effects compared with negative effects. Nevertheless, such research has introduced a more balanced treatment of psychological effects into the literature.
The positive psychological effects of caregiving have been defined in various ways. Most common are caregiving rewards or benefits, appreciation of life, personal growth, enhanced self-efficacy, competence or mastery, self-esteem, and closer relationships (Haley et al., 2009; J. H. Kim et al., 2007; Y. Kim et al., 2007). Prevalence rates for positive psychological effects are high across the caregiving population as a whole, with variation evident among demographic subgroups of caregivers. In NSOC, for example, 46 percent of caregivers reported feeling “very much” more confident about their abilities (see Figure 3-4). Percentages are substantially higher on this indicator for African American caregivers (68 percent), Hispanic caregivers (60 percent), caregivers with less than a high school education (67 percent), caregivers with income below $20,000 (67 percent), and caregivers who help more often with self-care tasks (58 percent). Similarly, in NSOC, 52 percent of caregivers reported feeling “very much” better able to deal with difficult situations. Again, percentages are higher for African American caregivers (67 percent), caregivers with less than a high school education (64 percent), and caregivers who help more often with self-care tasks (66 percent). These findings are consistent with literature reviews showing that racial and ethnic minority caregivers experienced higher levels of subjective well-being and perceived uplifts than white, non-Hispanic caregivers (Pinquart and Sörensen, 2005).
Positive psychological effects may mitigate some of the negative effects of caregiving, as several studies find that positive effects are associated with lower levels of burden and depression and better overall mental health. For example, van der Lee and colleagues (2014) found that a sense of competence or self-efficacy was associated with less caregiver burden and greater
mental health, while Y. Kim and colleagues (2007) found that caregivers’ esteem from caregiving was associated with lower psychological distress and better mental functioning.
In summary, a large body of literature, including population-based cross-sectional and longitudinal studies, provides strong evidence that a substantial proportion of the caregiving population experiences negative psychological effects, even though caregiving has some positive effects as well. Regardless of the mental health indicator used, levels of distress are high enough to constitute a public health concern.
Evidence about predictors of negative psychological health effects suggests that prevalence rates vary across subgroups of caregivers, placing some caregivers at higher risk for negative effects than others. Further evidence suggests that risk factors are multifactorial and may be cumulative. Women providing many hours of care weekly to a care recipient with challenging behavioral symptoms may be at particularly high risk. Thus, multidimensional assessment is needed to identify the specific array of risk factors present for any given caregiver. Likewise, interventions need to be tailored to specific subpopulations of caregivers.
Physical Health Effects
A variety of indicators have been used to assess the physical health of caregivers including global health status indicators, physiological measures, and health behaviors (see Table 3-4). Global health status indicators include standardized self-assessment tools such as health-related quality of life, chronic conditions, physical symptoms (e.g., Cornell Medical Index), mortality, and health service use, including clinic visits, physician or nurse practitioner visits, and days in the hospital (Schulz and Sherwood, 2008). For example, in a review of 176 studies of family caregivers of older adults assessing the physical health of caregivers, Pinquart and Sörenson (2007) found 66 percent of studies used a “single-item indicator” self-report measure, 21 percent incorporated measures related to physical impairment (activities of daily living or instrumental activities of daily living scales), 19 percent included measures based on a symptom checklist (e.g., SF-364), 15 percent used the number of medical or chronic conditions, three studies assessed use of medications, and three measured usage of hospital or doctor visits. Saban and colleagues (2010) identified a similar list of health outcomes in their review of the literature and noted that overall studies focused on physical health are much rarer than studies assessing psychological outcomes such as stress and depression.
___________________
4 The SF-36 is a 36-item patient-reported survey that is commonly used to assess physical and mental health and quality of life.
TABLE 3-4 Summary of Findings on the Physical Health Outcomes of Family Caregiving of Older Adults
| Type of Measure/Health Indicator | Findings |
|---|---|
| Global Health Measures | |
|
Negative effects found for all indicators but effects are small to medium; self-report measures are most common and show largest negative effects High-stress caregiving associated with increased mortality in several studies |
| Physiological Measures | |
|
Negative effects for most indicators are generally small; larger negative effects found for stress hormones and antibodies than other indicators; some evidence for adverse metabolic effects and telomere erosion |
| Health Behaviors | |
|
Some evidence supporting impaired health behaviors in all domains; evidence is strongest for sleep problems in dementia caregivers |
NOTE: ACTH = adrenocorticotropic hormone.
SOURCE: Adapted from Schulz and Sherwood, 2008.
The diversity of methods and instruments used to measure caregiver health makes cross-study comparisons and meta-analyses difficult (Grady and Rosenbaum, 2015). Methodological rigor of studies that assess impacts on the physical health of caregivers is often limited by study sample size, selection of comparison or control groups, timeline for data collection
and longitudinal assessments as well as by the statistical methods used (Cameron and Elliott, 2015; Grady and Rosenbaum, 2015). Thus, caution is advised in overattributing negative health outcomes to the effects of caregiving. The physical health status and outcomes for caregivers may be relatively independent of the caregiving role or related to individual characteristics that existed prior to assuming the caregiving role, such as socioeconomic status, health habits, and prior illness (Brown and Brown, 2014; Robison et al., 2009; Roth et al., 2015; Schulz and Sherwood, 2008). Nevertheless, the data support the conclusion that at least some caregivers are at risk for adverse health outcomes (Capistrant, 2016). In the discussion below, we identify a broad range of individual and contextual factors that contribute to adverse health outcomes in caregivers.
Caregivers’ Reports on their Health Status
Caregivers tend to rate their health as poorer than non-caregivers. Caregivers for older care recipients consistently report poorer subjective health status than non-caregivers (Berglund et al., 2015; Pinquart and Sörenson, 2003). Poorer caregiver physical health is closely associated with greater caregiver burden and depressive symptoms and is associated to a lesser degree with hours of care provided, the number of caregiving tasks, months in the caregiver role, as well as the physical, cognitive, and behavioral impairments and problems of the care recipient (Pinquart and Sörenson, 2007). Family caregivers in England responding to a national survey of users of primary care services also reported poorer health and a worse primary care individual experience compared with non-caregiver individuals with similar demographics, including age, gender, ethnicity, and level of social deprivation (Persson et al., 2015). In NSOC, 20 percent of all caregivers and 39 percent of caregivers of high-need older adults reported that they experienced a substantial level of physical difficulty.5 Sleep problems affected more than 40 percent of caregivers and were highly correlated with reports of substantial negative effects of caregiving (Spillman et al, 2014).
Using the Health and Retirement Study (HRS), a large representative sample of U.S. adults, Capistrant and colleagues (2012) found that being a spousal caregiver independently predicted incident cardiovascular disease. Longer-term caregivers had twice the risk of short-term caregivers. However, this effect was observed only among whites, not among non-whites. Ji and colleagues (2012) reported similar results for spousal caregivers of persons with cancer. After cancer diagnosis in their spouse, the risk of coronary heart disease (CHD) and stroke were higher in both husband and wife caregivers when compared to husbands and wives without an affected
___________________
5 Committee calculations.
spouse. These effects were more pronounced when the type of cancer had a high mortality rate, such as pancreatic and lung cancers. These findings suggest that psychological distress associated with the diagnosis may play a role in the risk of CHD and stroke.
Also based on data from the HRS collected from 1998 to 2010, Dassel and Carr (2014) showed that spousal caregivers of persons with dementia are significantly more likely to experience increased frailty (i.e., unintentional weight loss, self-reported exhaustion, weakness, slow walking speed, and low physical activity [as defined by Fried et al., 2001]) over time when compared to non-dementia spousal caregivers. Similarly, a systematic review of 192 articles focused on cancer caregiving (1990-2008) found that the most prevalent problems for caregivers included sleep disturbance, fatigue, pain, loss of physical strength, loss of appetite, and weight loss (Stenberg et al., 2010).
One of the consistent themes in the caregiver health effects literature concerns the role of caregiver strain in predicting negative health effects (Schulz et al., 1997), including mortality. Schulz and Beach (1999) found increased risk of mortality (63 percent) among older spousal caregivers, but only if they reported emotional strain in the caregiving role. Perkins and colleagues (2013) reported similar results showing that caregivers who reported high levels of caregiving strain had an excess 55 percent mortality risk when compared with those reporting no stress. Living with a person with Parkinson’s disease 5 years after first Parkinson hospitalization was associated with higher risk of all-cause mortality for both husbands and wives in a study by Nielsen and colleagues (2014).
In contrast to these studies, several recent population-based studies suggest the opposite—that caregiving is associated with lower mortality risk (Brown et al., 2009). Fredman and colleagues (2015) found a 26 percent lower mortality risk among older adult caregivers when compared to non-caregivers, and several U.S. Census-based studies show lower mortality rates among caregivers (O’Reilly et al., 2008, O’Reilly et al., 2015; Ramsay et al., 2013). These opposing perspectives on caregiving and mortality may be reconcilable if we consider that negative impact studies are typically based on vulnerable, older, strained caregiving spouses providing intense levels of care while studies reporting positive effects focus on all caregivers regardless of age of caregiver, relationship to the care recipient, or type and amount of care provided.
Caregiving-Related Injuries
Providing care to an older adult is often physically demanding. In NSOC, 20 percent of all caregivers and 39 percent of high-need caregivers reported that providing care was physically difficult. Caregiving tasks such
as transfers, lifts, bathing, dressing, and repositioning the care recipient place physical strain on the caregiver and may result in musculoskeletal injury such as back ache, muscle strain, and contusions (Brown and Mulley, 1997; Darragh et al., 2015; Hartke et al., 2006). These effects are likely to be exacerbated among older caregivers with impaired vestibular function, limited motion due to arthritis, and weakness due to age-related changes in muscle mass. The risk of injury is further compounded by the home environments of the care recipient, which may include small spaces, crowded and cluttered rooms, and steep stairways (NRC, 2011). Although reliable data on injury rates among caregivers are not available, the fact that paid home health aides as well as home care nursing and rehabilitation personnel sustain high rates of work-related musculoskeletal disorders suggests that this is likely to be a problem among family caregivers as well. Workplace injuries among direct-care workers that result in time away from work are four times the average rate of all occupations (BLS, 2007). Mitigating injuries related to caregiving requires a careful assessment of the home environment, an understanding of caregiving task demands, and the physical capabilities of the caregiver. This information can then be used to develop a treatment plan that may involve home alterations, caregiver training on how to safely perform required caregiving tasks, and the use of paid professionals to perform tasks that place the caregiver at risk of injury (Cornman-Levy et al., 2001).
Physiological Measures
Biological indicators include a broad array of measures aimed at assessing physiological markers that are thought to be responsive to chronic stress exposure and affect downstream illness and disease. These markers include measures of stress hormones and neurotransmitters such as cortisol, epinephrine, and norepinephrine; measures of immunologic function such as natural killer cell activity and healing response to a standardized skin puncture wound (wound healing); antibody markers such as vaccination response; cardiovascular markers such as blood pressure and heart rate; and metabolic markers such as insulin, transferrin, and plasma lipids (Vitaliano et al., 2003). These markers have been studied primarily in case control studies comparing stressed dementia caregivers with demographically similar non-caregiving controls. In a meta-analysis of the literature in this area, Vitaliano and colleagues (2003) found moderately sized statistically significant differences between dementia caregivers and controls, indicating more adverse effects among dementia caregivers. Subsequent studies have shown an increased risk of cardiometabolic changes and increased Framingham Coronary Heart Disease Risk Scores in dementia caregivers as well as proinflammatory changes and accelerated aging of the immune
system (i.e., telomere erosion) (Damjanovic et al., 2007; Haley et al., 2010; Kiecolt-Glaser et al., 2003; Mausbach et al., 2007; von Känel et al., 2008). A recent study also examined kidney function in dementia caregivers over a study period of up to 3 years, but found no differences between caregivers and non-caregivers, possibly because the follow-up period was not long enough (von Känel et al., 2012). While the preponderance of evidence suggests an association between caregiving and physiological function, it is important to keep in mind that the caregivers selected for these studies are typically moderately to highly stressed dementia caregivers and therefore the generalizability of findings may be limited. In addition, some researchers have questioned the choice of control subjects in these case control studies, which may not adequately control for preexisting differences between caregivers and non-caregivers (O’Reilly et al., 2015).
Health Behaviors
For caregivers, neglect of their own health may worsen preexisting illnesses or increase vulnerability to stress-related problems (Son et al., 2007; Vitaliano et al., 2003; Yueh-Feng Lu and Austrom, 2005). Health-promoting self-care behaviors are designed to improve health, maintain optimal functioning, and increase general well-being. Health-promoting self-care for caregivers can include getting enough rest, maintaining a healthy diet, getting enough exercise, taking breaks, taking care of one’s own health, seeking preventive health care, joining a support group, and locating respite care when needed (Acton, 2002; Collins and Swartz, 2011). Health risk behaviors for caregivers can include substance abuse, sleep problems, poor diets, sedentary behaviors (Vitaliano et al., 2003), smoking (Salgado-Garcia et al., 2015), and alcohol consumption (de Nooijer, et al., 2003).
Early work by researchers such as Gallant and Connell (1997), Pearlin and colleagues (1990), and Schulz and Beach (1999) suggested that health-promoting and self-care behaviors may be neglected by caregivers due to their caregiving duties, lack of time and energy to take care of themselves, or breakdown of social networks; health risk behaviors also may be triggered by care recipient behaviors or by coping mechanisms induced by the stress of caregiving. For example, in a study of dementia caregivers, nearly one-third frequently or occasionally missed medication doses and nearly a half did not keep their own health care appointments (Wang et al., 2015). In another dementia caregiving sample, 40 percent of caregivers reported smoking and 25 percent reported a recent increase in smoking (Salgado-Garcia et al., 2015).
Being female (Wang et al., 2015) and older (Rabinowitz et al., 2007) or younger (Salgado-Garcia et al., 2015) have all been associated with poorer caregiver health behavior. However, the relationship between care-
giving and health behaviors/self-care is complex. In a review article of 23 studies, Vitaliano and colleagues (2003) found that dementia caregivers reported more risky health behaviors than non-caregivers. Although caregivers may have had poor health habits before caregiving (Vitaliano et al., 2003) or their health behaviors may be related to illness or other factors, these behaviors may also be triggered by the care recipient’s behaviors or by distress.
This potential relationship between caregiving events and factors related to the caregiver can be seen clearly in the case of caregiver sleep disturbance. Caregivers of people with dementia have more sleep problems than non-caregiving adults, including waking up in the night or early morning, bathroom needs, sleep-onset difficulties, nighttime care recipient disruptions, and psychological distress (Wilcox and King, 1999). Behaviors of people with dementia may initially disrupt the caregiver’s sleep patterns. However, subsequent caregiver sleep disturbances may be the result of factors related to risk factors for sleep difficulties (e.g., being an older woman, poor caregiver health), or subjective caregiver burden, depression, or anxiety (McCurry et al., 2007; Wilcox and King, 1999).
Evidence shows that burden, stress, and depression influence health behaviors. Caregivers who report high levels of stress are more likely to report risky health behaviors (Sisk, 2000; Zarit and Gaugler, 2000). Higher levels of objective (care recipient problem behaviors) and subjective (feeling of overload) burden are associated with negative health behaviors for dementia caregivers (Son et al., 2007), as is worse care recipient health (Rabinowitz et al., 2007). Increase in smoking for caregivers is associated with higher depression scores (Salgado-Garcia et al., 2015). Longer length of caregiving and more care recipient dependency in activities of daily living are associated with a decrease in the health-promoting behaviors of medication adherence and appointment keeping for caregivers (Wang et al., 2015). Conversely, caregivers who spend less time on duty for the care recipient use more health care services for themselves (Martindale-Adams et al., 2015). Caregivers perceiving lower subjective burden practice more health-promoting behaviors than those with higher subjective burden scores (Sisk, 2000).
Feeling capable of managing caregiving difficulties and positive caregiver health behaviors are associated. In a study of dementia caregivers, higher self-efficacy in controlling upsetting thoughts and obtaining respite is associated with fewer negative health risk behaviors and higher engagement in positive health behaviors (Rabinowitz et al., 2007). More caregiving skills are associated with less increase in smoking (Salgado-Garcia et al., 2015). Caregivers who practice health-promoting self-care behaviors are better protected from stress, and the effects of stress on well-being are reduced (Acton, 2002).
Social Effects
The social effects of caregiving range from changes in family relationships, including relationships with a spouse, children, and other close individuals, to changes in social activities with and social support from a wider network. Reduced time and energy for maintaining social relationships may occur, resulting in isolation and long-term constriction of social networks (George and Gwyther, 1986; Gwyther, 1998; Seltzer and Li, 2000; Skaff and Pearlin, 1992). In some instances, caregivers may experience extreme, life-changing social effects that irrevocably change relationships and even alter the life course, such as marital infidelity, spousal abuse, and/or divorce.
The time demands of caregiving often limit the opportunity to engage in other activities that caregivers enjoy (see Table 3-5). For example, 15.1 percent of caregivers responded “very much” and 26.2 percent responded “somewhat” when asked if they do not have time for themselves. Family caregivers who help with self-care tasks and/or care for persons with dementia report more limitations in their ability to spend time for themselves when compared to caregivers with less intense care responsibilities. As shown in Table 3-5, high-need caregivers who care for someone with probable dementia and with self-care needs report the highest level of restriction in their ability to visit with friends and family, to attend religious services, to go out for dinner or movies, or to do volunteer work.
Family Relationships
Family relationships and quality of life may also be impacted by caregiving demands, although this topic has received relatively little attention in the caregiving literature. In a large panel study of Health and Retirement Study participants, Amirkhanyan and Wolf (2006) found that adverse psychological effects of caregiving are dispersed throughout the family and not just the active caregivers. Bookwala (2009) found in a sample of adult caregiving daughters and sons that longer-term caregivers were significantly less happy in their marriages than those who recently assumed the caregiving role, suggesting that it takes time for negative impacts to manifest themselves.
The demands of caregiving may also generate familial conflict about care decisions. When caregivers were asked in NSOC how much family members disagreed over the details of the care recipient’s care, 6.7 percent reported that family members disagreed “very much” and 13.9 percent disagreed “somewhat.” These percentages were higher for Hispanic caregivers (11.0 percent and 17.5 percent), caregivers with less than a high school education (15.2 percent and 5.7 percent), and caregivers providing
| Social Activities Identified by Caregivers as “Very” or “Somewhat” Important to Them | Care Recipient’s Dementia Status and Level of Impairment | |||
|---|---|---|---|---|
| Dementia Only | No Dementia; Has Two or More Self-Care Needs | Dementia; Has Two or More Self-Care Needs | No Dementia; Has Fewer Than Two Self-Care Needs | |
| Did caregiving keep you from . . . | Yes (Percentage) | |||
|
Visiting in person with friends or family |
18.7 | 18 | 30.8 | 11.2 |
|
Attending religious services |
5.7 | 10.7 | 16.4 | 4.1 |
|
Going out for enjoyment (e.g., dinner, movie, gamble) |
14.7 | 13.5 | 23.7 | 6.1 |
|
Doing volunteer work |
8.5 | 5.8 | 15.1 | 4.8 |
| Population represented (in 1000s) | 2,931 | 2,745 | 2,828 | 9,190 |
NOTES: Includes family caregivers of Medicare beneficiaries age 65 and older in the continental United States who resided in community or residential care settings (other than nursing homes) and received help with self-care, mobility, or household activities for health or functioning reasons. Self-care activities include bathing, dressing, eating, toileting, or getting in and out of bed. “Dementia only” refers to care recipients with possible dementia and less than two self-care needs. “Probable dementia” includes individuals whose doctor said they had dementia or Alzheimer’s disease, and individuals classified as having probable dementia based on results from a proxy screening instrument and several cognitive tests.
SOURCES: Data from the 2011 NHATS and the companion NSOC.
high-intensity care defined as helping with two or more self-care needs (8.9 percent and 17.5 percent).
Sources of conflict include differing views about the appropriate boundaries for caregiving, disapproval of family members’ actions or attitudes, disagreements about the nature and seriousness of the care recipient’s condition, perceived failure to appreciate the demands on the primary caregiver and to provide adequate help or support, disapproval of the quality of care, and disagreements over financial matters pertaining to the care recipient (Aneshensel et al., 1995; Gwyther, 1995; Gwyther and Matchar, 2015; Strawbridge and Wallhagen, 1991). Aneshensel and colleagues (1995) found that although levels of conflict were low for most caregivers, one in four reported intense strife in at least one area of family conflict. In some
instances, conflicts may be severe, resulting in severed relationships or legal action (Strawbridge and Wallhagen, 1991).
Anecdotal evidence in clinical and research contexts suggests that a small percentage of family caregivers experience severe conflict related to caregiving, resulting in abusive interactions with other family members and even divorce or other legal actions. Given the sensitive and potentially stigmatizing aspects of severe family conflict, it is surprising that this level of conflict has not been systematically examined in research. Thus, severe family conflict remains a hidden social effect of caregiving, recognized in clinical practice, but unexplored to date in research.
In sum, the time and energy demands of caregiving may compete with both work and leisure activities. The impact of caregiving on work is discussed in the following chapter. The brief review here highlights the consequences of caregiving for leisure activities, quality of married life, and family conflict. The small literature in this area emphasizes negative effects in all of these domains. Family systems approaches to caregiving in which family members are viewed as interacting elements that attempt to synchronize their efforts to deal with the challenges of providing care are relatively rare in the literature and deserve further attention. Because the caregiving literature has focused almost exclusively on the single primary caregiver, little is known about how care tasks are distributed within a family over time, how care responsibilities are negotiated, and how the physical and psychological effects of caregiving are shared among family members. A better understanding of these processes may help to identify new intervention opportunities for caregiving.
Elder Mistreatment and Neglect
A potential effect of caregiving stress is elder mistreatment and neglect. Mistreatment of older adults can take many forms including physical, emotional, and sexual abuse as well as financial exploitation, neglect, and abandonment (National Center on Elder Abuse, 2015). To qualify as mistreatment, a behavior has to intentionally cause harm or create a serious risk of harm to a vulnerable older adult. The term “domestic elder abuse” is used to refer to mistreatment committed by someone with whom the older adult has a special relationship such as a spouse, sibling, child, friend, or caregiver. Caregiver neglect is a specific type of mistreatment in which the caregiver intentionally fails to address the physical, social, or emotional needs of the older person. This neglect can include withholding food, water, clothing, medications, or assistance with activities of daily living such as help with personal hygiene.
Prevalence estimates of abuse have generally ranged from 7 to 10 percent of older adults annually, although physical abuse (less than 2 percent)
and sexual abuse (less than 1 percent) prevalence are much lower (Acierno et al., 2010; Lachs and Berman, 2011; Laumann et al., 2008). Research suggests that family members commit most abuse, but it is not known if this abuse occurs primarily within a caregiving context. Rates of abuse are generally higher for older adults with dementia and/or adults who need physical assistance, suggesting that family caregivers are likely perpetrators of abuse (Beach et al., 2005).
Although the data suggest that family caregivers may play a significant role in committing elder mistreatment when it does occur, there is a lack of adequate data to address this issue. Based on responses from care recipients, studies of potentially harmful behaviors, defined as behaviors that are detrimental to the elder’s physical and psychological well-being, show prevalence rates of nearly 25 percent among caregivers. By far the most prevalent potentially harmful caregiver behavior involved negative verbal interactions like screaming/yelling (22.2 percent) or using a harsh tone of voice/insulting/calling names/swearing (11.7 percent). Physical forms of abuse like hitting/slapping, shaking, and handling roughly in other ways were much less prevalent, reported by only about 1 percent of the care recipients (Beach et al., 2005). Level of care recipient impairment in cognitive and physical functioning was a strong predictor of potentially harmful behavior. Similar results with even higher prevalence rates were reported by Lafferty and colleagues (2016) in their survey of more than 2,000 caregivers in Ireland. The extent to which family caregivers experience abuse, by the older adults they care for, is not known. More research is needed on the prevalence of elder mistreatment among caregivers, the type of mistreatment they commit, the circumstances under which it occurs, and the factors that mitigate mistreatment or neglect. Of particular importance is gaining a better understanding of how and when a supportive caregiving relationship evolves into an abusive one.
Risk Factors for Adverse Outcomes
The above review clearly finds that a significant proportion of caregivers experience a broad range of adverse outcomes including impairment in psychological and physical health, disruptions in social relationships, and possible mistreatment of the care provider or recipient. These negative effects, however, are not universal. While nearly half of caregivers experience emotional distress associated with caregiving, a much smaller proportion exhibit adverse physical health effects. This begs the question, who is at risk for adverse outcomes as a result of caregiving?
All of the variables listed in Table 3-6 have been identified in one or more studies as risk factors for adverse caregiver outcomes. These risk factors fall into six categories:
- Sociodemographic factors
- Intensity and type of caregiving tasks
- Caregivers’ perceptions of care recipients’ suffering
- Caregivers’ own health and functioning
- Caregivers’ social and professional supports
- Care recipients’ physical home environment (see Table 3-6)
Evidence for the strength of most of these predictors is mixed and considerable variability exists in study design, methods, and quality of the research. However, accumulating evidence suggests that caregiving intensity (i.e., hours of caregiving per week), gender, relationship to the care recipient (wives are more affected than adult daughters or others), living with the care recipient, and challenging behavioral symptoms in the care recipient are relatively robust predictors of negative psychological effects.
The intensity of caregiving has been found to be a consistent predictor of negative psychological effects in population-based studies. An analysis of the Nurses’ Health Study, for example, found that the odds of increasing depressive or anxious symptoms rose with increasing caregiving time commitment (Cannuscio et al., 2002). Women providing care to an ill or disabled spouse 36 hours or more weekly were nearly six times more likely than non-caregivers to report depressive or anxious symptoms. Women who provided 36 hours of care weekly to a parent were two times more likely to report depressive or anxious symptoms than non-caregivers (Cannuscio et al., 2002). A longitudinal analysis of the British Household Panel Survey found that caregivers who provided long hours of care for extended periods of time had increased levels of psychological distress, and that this association was stronger for women than men (Hirst, 2005). The risk for onset of distress increased progressively with the amount of time spent in caregiving each week.
Caregivers who provide high-intensity care are also more likely to make treatment decisions for the care recipient, which the literature suggests may be a unique risk factor for adverse outcomes. In a meta-analysis of 2,854 surrogate decision makers, at least one-third experienced emotional burden as the result of making treatment decisions. Negative effects were often substantial and typically lasted months or, in some cases, years. The most common negative effects were stress, guilt over the decisions they made, and doubt regarding whether they had made the right decisions (Wendler and Rid, 2011).
Female caregivers have been found to experience more psychological distress than males in a meta-analysis (Pinquart and Sörensen, 2006), in an early literature review (Yee and Schulz, 2000), and in a recent systematic review (Schoenmakers et al., 2010). In their meta-analysis of 229 studies, Pinquart and Sörensen (2006) found that women had higher levels of
TABLE 3-6 Risk Factors for Adverse Outcomes Due to Family Caregiving
Sociodemographic factors
- Lower income
- Lower education (high school or less)
- Older age (50 or older)
- Spouse of care recipient
- Female
- Living with care recipient
Intensity/type of caregiving
- More than 100 hours of care per month
- High care recipient personal/mobility care needs
- Dementia care (including management of behavioral symptoms)
- Medical care (shots/injections, wound care)
- Coordinating care (appointments, interacting with providers, dealing with health insurance)
Caregiver’s perceptions of the care recipient’s physical, psychological, and existential suffering
- Lack of choice in taking on the caregiving role
Caregiver’s health and physical functioning
- Poor/fair self-rated health
- Feeling stressed
- Having three or more medical conditions
- Sleep problems
- Difficulty breathing
- Pain
- Limited leg/arm strength
- Unwanted weight lost
Caregiver’s social and professional supports
- No one to help with caregiving
- No one to talk to
- No time to socialize with others
- No access or use of professional support/care services
Care recipient’s home physical environment
- Lacks appropriate home modifications
- Stairs, clutter
SOURCES: Adelman et al., 2014; Pinquart and Sörensen, 2003; Zarit et al., 2010.
burden and depression and lower levels of subjective well-being than men. Gender differences in depression were partially explained by differences in caregiver stressors, such as more hours of care given per week and a greater number of caregiving tasks performed by women.
Differences in psychological effects also exist across racial and ethnic groups. A meta-analyses of 116 studies showed that African American caregivers had lower levels of burden and depression than non-Hispanic white caregivers, but Hispanic and Asian American caregivers reported more depression than their white, non-Hispanic counterparts (Pinquart and Sörensen, 2005). Similar racial and ethnic differences were reported in a subsequent systematic review of dementia caregiving (Nápoles et al., 2010). Although some data are available on African American and Hispanic caregivers, the literature on racially and ethnically diverse populations has several limitations, including
- Few large-scale comparative studies on a spectrum of outcome variables and their predictors with sufficient numbers and statistical power to report outcomes stratified by caregiver race and ethnicity (Apesoa-Varano et al., 2015; Aranda, 2001);
- Few studies that directly compare caregiving in specific groups such as Asian Americans and Pacific Islanders, American Indians, black Caribbeans, and monolingual Spanish speakers, or the heterogeneity within such groups (Milne and Chryssanthopoulou, 2005; Weiner, 2008);
- Lack of attention to clinically determined caregiver health indicators that go beyond self-report (e.g., clinically diagnosed depressive disorder, objective indicators of functional health status, etc.) (Hinton, 2002; Schulz and Sherwood, 2008); and
- Minimal attention to racially and ethnically diverse caregivers in a variety of contexts that go beyond dementia-specific caregiving (e.g., frailty, diabetes, brain injury, end-of-life care, etc.) (Aranda and Knight, 1997).
Caregivers who live with the care recipient are at increased risk of adverse outcomes. Schulz and colleagues have shown that these effects are in part explained by the exposure to suffering of the care recipient (Monin and Schulz, 2009; Schulz et al., 2007, 2009). Living with an older adult who is physically or psychologically suffering takes its toll on the caregiver, above and beyond the pragmatic challenges of providing assistance.
Whether an individual has a choice in taking on the caregiving role may also make a difference. Nearly half of all caregivers report that they had no choice in taking on the caregiving role and lack of perceived choice is associated with increased levels of burden and depression (Reinhard et al., 2012; Schulz et al., 2012).
Care recipients’ behavioral symptoms (e.g., agitation, irritability, combativeness) are also associated with negative effects for caregivers (Ballard et al. 2000; Gitlin et al. 2012; Pinquart and Sörensen, 2003; Schoenmakers
et al., 2010; Schulz et al., 1995; Torti et al., 2004; van der Lee et al., 2014). In their examination of multivariate models predicting dementia caregiver burden, depression, and mental health, van der Lee and colleagues (2014) concluded that care recipient behavioral symptoms (e.g., waking up at night, rejecting needed care, agitation, and verbal and physical aggressiveness) were stronger predictors of caregiver burden and depression than the cognitive or functional status of the care recipient. Pinquart and Sörensen (2003) also found that care recipients’ behavior problems had a greater impact on caregivers’ burden and depression than care recipients’ physical and cognitive impairments. Torti and colleagues (2004) reported that behavioral problems are associated with caregiver burden across geographic regions and cultures. Hinton and colleagues (2003) reported that behavioral problems are associated with depressive symptoms among family caregivers of cognitively impaired Latinos but that this association was most pronounced among non-spousal caregivers.
Definitive conclusions about the relative importance of different risk factors should be viewed cautiously, however, because many of these risk factors are correlated with each other, and no studies have examined all of these risk factors simultaneously in a single large population-based study. Nevertheless, existing findings on risk factors can help inform efforts to target caregivers in need of support and shape the type of support provided (Beach et al., 2005).
CONCLUSIONS
The committee’s key findings and conclusions are described in detail in Box 3-1. In summary, this chapter raises profound concerns about our dependence on family caregivers to take on increasingly complex and demanding roles. As a society, we have always depended on families to provide emotional support and to assist their older members with household tasks and personal care. In today’s health care and social service systems, providers expect family caregivers—with little or no training—to handle daunting technical procedures and equipment for seriously ill care recipients at home. Some family caregivers express concerns about making a life-threatening mistake.
The demands of caregiving appear to be taking a toll on family members on the front lines of supporting older adults. Substantial evidence indicates that family caregivers of older adults are at risk compared to non-caregivers; they have higher rates of depressive symptoms, anxiety, stress, and emotional difficulties. Evidence also suggests that caregivers have lower self-ratings of physical health, elevated levels of stress hormones, higher rates of chronic disease, and impaired health behaviors.
The effects of caregiving are not all negative. Numerous surveys suggest
that, for some, caregiving instills confidence, provides lessons on dealing with difficult situations, brings them closer to the care recipient, and assures them that the care recipient is well-cared for. In fact, the caregiving experience and its impact are highly individual and dependent on a wide array of personal and family circumstances such as the caregiver’s own health, the care recipient’s level of impairment, financial resources, and competing demands from work and family. Gender, the caregiver-care recipient relationship, family dynamics, proximity to the care recipient, race and ethnicity, culture, personal values, and beliefs all play a part.
Few caregiving studies are designed to examine how race and ethnicity, rural residence, sexual orientation, or socioeconomic status affect caregivers. If providers and policy makers are to learn how best to support the nation’s increasingly diverse aging population, future caregiving research should be sufficiently powered to enable meaningful subgroup analyses.
REFERENCES
ABA (American Bar Association) Commission on Law and Aging. 2014. Default surrogate consent statutes chart as of June 2014. Chicago, IL. http://www.americanbar.org/content/dam/aba/administrative/law_aging/2014_default_surrogate_consent_statutes.authcheckdam.pdf (accessed August 8, 2015).
Acierno, R., M. A. Hernandez, A. B. Amstadter, H. S. Resnick, K. Steve, W. Muzzy, and D. J. Kilpatrick. 2010. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health 100(2):292-297.
Acton, G. J. 2002. Health-promoting self-care in family caregivers. Western Journal of Nursing Research 24(1):73-86.
Adelman, R. D., L. L. Timanova, D. Delgado, S. Dion, and M. S. Lachs. 2014. Caregiver burden: A clinical review. Journal of the American Medical Association 311(10):1052-1059.
Amirkhanyan, A. A., and D. A. Wolf. 2006. Parent care and the stress process: Findings from panel data. Journal of Gerontology 61(5):S248-S255.
Aneshensel, C. S., L. I. Pearlin, J. T. Mullan, S. H. Zarit, and C. J. Whitlatch. 1995. Profiles in caregiving: The unexpected career. San Diego, CA: Academic Press.
Apesoa-Varano, E. C., Y. Tang-Feldman, S. C. Reinhard, R. Choula, and H. M. Young. 2015. Multi-cultural caregiving and caregiver interventions: A look back and a call for future action. Generations 39(4):39-48.
Aranda, M. P. 2001. Racial and ethnic factors in dementia caregiving research in the U.S. Aging and Mental Health 5(S1):S116-S123.
Aranda, M. P., and B. Knight. 1997. The influence of ethnicity and culture on the caregiver stress and coping process: A sociocultural review and analysis. The Gerontologist 37(3):342-354.
Bakas, T., J. K. Austin, S. L. Jessup, L. S. Williams, and M. T. Oberst. 2004. Time and difficulty of tasks provided by family caregivers of stroke survivors. Journal of Neuroscience Nursing 36(2):95-106.
Ballard, C., K. Lowery, I. Powell, J. O’Brien, and I. James. 2000. Impact of behavioral and psychological symptoms of dementia on caregivers. International Psychogeriatrics 12(S1): 93-105.
Beach, S. R., R. Schulz, J. L. Yee, and S. Jackson. 2000. Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the Caregiver Health Effects Study. Psychology and Aging 15(2):259-271.
Beach, S. R., R. Schulz, G.M. Williamson, L. S. Miller, M. F. Weiner, and C. E. Lance. 2005. Risk factors for potentially harmful informal caregiver behavior. Journal of the American Geriatrics Society 53(2):255-261.
Berglund, E., P. Lytsy, and R. Westerling. 2015. Health and wellbeing in informal caregivers and non-caregivers: A comparative cross-sectional study of the Swedish general population. Health and Quality of Life Outcomes 13(1):1-11.
BLS (Bureau of Labor Statistics). 2007. Nonfatal occupational injuries and illnesses requiring days away from work. http://www.bls.gov/news.release/archives/osh2_11202008.pdf (accessed July 5, 2016).
Bond, S. M., M. S. Dietrich, J. L. Shuster, and B. A. Murphy. 2012. Delirium in patients with head and neck cancer in the outpatient treatment setting. Supportive Care in Cancer 20:1023-1030.
Bookman, A., and D. Kimbrel. 2011. Families and elder care in the twenty-first century. The Future of Children 21(2):117-140.
Bookwala, J. 2009. The impact of parent care on marital quality and well-being in adult daughters and sons. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 64B(3):339-347.
Brody, E.M. 1985. Parent care as a normative family stress. The Gerontologist 25(1):19-29.
Brown, A. R., and G. P. Mulley. 1997. Injuries sustained by caregivers of disabled elderly people. Age and Ageing 26(1):21-23.
Brown, R. M. and S. L. Brown. 2014. Informal caregiving: A reappraisal of effects on caregivers. Social Issues and Policy Review 8(1):74-102.
Brown, S. L., D. M. Smith, R. Schulz, M. U. Kabeto, P. A. Ubel, M. Poulin, J. Yi, C. Kim, and K. M. Langa. 2009. Caregiving behavior is associated with decreased mortality risk. Psychological Science 20(4):488-494.
Cagle, J. G. and J. C. Munn, 2012. Long-distance caregiving: A systematic review of the literature. Journal of Gerontological Social Work 55(8):682-707.
Cahill, E., L. M. Lewis, F. K. Barg, and H. R. Bogner. 2009. “You don’t want to burden them”: Older adults’ views on family involvement in care. Journal of Family Nursing 15(3):295-317.
Cameron, J. I., and T. R. Elliott. 2015. Studying long-term caregiver health outcomes with methodologic rigor. Neurology 84(13):1292-1293.
Cannuscio, C. C., C. Jones, I. Kawachi, G. A. Colditz, L. Berkman, and E. Rimm. 2002. Reverberations of family illness: A longitudinal assessment of informal caregiving and mental health status in the Nurses’ Health Study. American Journal of Public Health 92(8):1305-1311.
Capistrant, B. D. 2016. Caregiving for older adults and the caregivers’ health: An epidemiologic review. Current Epidemiology Reports 3(1):72-80.
Capistrant, B. D., J. R. Moon, L. F. Berkman, and M. M. Glymour. 2012. Current and long-term spousal caregiving and onset of cardiovascular disease. Journal of Epidemiology and Community Health 66(10):951-956.
Carpentier, N., P. Bernard, A. Gernier, and N. Guberman. 2010. Using the life course perspective to study the entry into the illness trajectory: The perspective of caregivers of people with Alzheimer’s disease. Social Science and Medicine 70(10):1501-1508.
Cavaye, J. E. 2008. From dawn to dusk: A temporal model of caregiving: Adult carers of frail parents. Paper presented at CRFR Conference, Understanding Families and Relationships over Time, Edinburgh, UK.
Collins, L. G., and K. Swartz. 2011. Caregiver care. American Family Physician 83(11): 1309-1317.
Coon, D. W. 2007. Exploring interventions for LGBT caregivers: Issues and examples. Journal of Gay & Lesbian Social Services 18(3-4):109-128.
Cornman-Levy, D., Gitlin, L.N., Corcoran, M.A. and Schinfeld, S., 2001. Caregiver aches and pains: The role of physical therapy in helping families provide daily care. Alzheimer’s Care Quarterly 2(1):47-55.
Cuijpers, P. 2005. Depressive disorders in caregivers of dementia patients: A systematic review. Aging & Mental Health 9(4):325-330.
Damjanovic, A. K., Y. Yang, R. Glaser, J. K. Kiecolt-Glaser, H. Nguyen, B. Laskowski, Y. Zou, D. Q. Beversdorf, and N. P. Weng. 2007. Accelerated telomere erosion is associated with a declining immune function of caregivers of Alzheimer’s disease patients. The Journal of Immunology 179(6):4249-4254.
Darragh, A. R., C. M. Sommerich, S. A. Lavender, K. J. Tanner, K. Vogel, and M. Campo. 2015. Musculoskeletal discomfort, physical demand, and caregiving activities in informal caregivers. Journal of Applied Gerontology 34(6):734-760.
Dassel, K. B., and D. C. Carr. 2014. Does dementia caregiving accelerate frailty? Findings from the Health and Retirement Study. The Gerontologist (Advance Access). https://gerontologist.oxfordjournals.org/content/early/2014/08/25/geront.gnu078.abstract (accessed April 7, 2016).
de Nooijer, J., L. Lechner, and H. de Vries. 2003. Social psychological correlates of paying attention to cancer symptoms and seeking medical help. Social Science & Medicine 56(5):915-920.
Dilworth-Anderson, P., I. C. Williams, and B. E. Gibson. 2002. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980-2000). The Gerontologist 42(2):237-272.
Dunkle, R. E., S. Feld, A. J. Lehning, H. Kim, H. W. Shen, and M. H. Kim. 2014. Does becoming an ADL spousal caregiver increase the caregiver’s depressive symptoms? Research on Aging 36(6):655-682.
Edwards, S. B., K. Olson, P. M. Koop, and H. C. Northcott. 2012. Patient and family caregiver decision making in the context of advanced cancer. Cancer Nursing 35(3):178-186.
Emanuel, E. J., D. L. Fairclough, J. Slutsman, and L. L. Emanuel. 2000. Understanding economic and other burdens of terminal illness: The experience of patients and their caregivers. Annals of Internal Medicine 132(6):451-459.
Feinberg, L. F. and C. J. Whitlatch, 2001. Are persons with cognitive impairment able to state consistent choices?. The Gerontologist 41(3):374-382.
Fredman, L., J. G. Lyons, J. A. Cauley, M. Hochberg, and K. M. Applebaum. 2015. The relationship between caregiving and mortality after accounting for time-varying caregiver status and addressing the healthy caregiver hypothesis. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 70(9):1163-1168.
Freedman, V. A., and B. C. Spillman. 2014. Disability and care needs among older Americans. Milbank Quarterly 92(3):509-541.
Fredriksen-Goldsen, K. I., and N. R. Hooyman. 2007. Caregiving research, services, and policies in historically marginalized communities. Journal of Gay & Lesbian Social Services 18(3-4):129-145.
Fredriksen-Goldsen, K., H. Kim, C. Emlet, A. Muraco, E. Erosheva, C. Hoy-Ellis, J. Goldsen, and H. Petry. 2011. The aging and health report: Disparities and resilience among lesbian, gay, bisexual, and transgender older adults. New York, NY: Services and Advocacy for GLBT Elders, LA Gay & Lesbian Center, New Leaf, LGBT Aging Project, SAGE at Center on Halsted, Senior Services, SAGE/Milwaukee, FORGE, Openhouse, GLBT Generations, and SAGE Metro St. Louis.
Fried, L. P., C. M. Tangen, J. Walston, A. B. Newman, C. Hirsch, J. Gottdiener, T. Seeman, R. Tracy, W. J. Kop, G. Burke, and M. A. McBurnie. 2001. Frailty in older adults: Evidence for a phenotype. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 56(3):M146-M157.
Friedemann, M. L., R. J. Montgomery, B. Maiberger, and A. A. Smith. 1997. Family involvement in the nursing home: Family-oriented practices and staff-family relationships. Research in Nursing and Health 20(6):527-537.
Gallant, M. P., and C. M. Connell. 1997. Predictors of decreased self-care among spouse caregivers of older adults with dementing illnesses. Journal of Aging and Health 9(3):373-395.
Garvelink, M. M., P. A. Ngangue, R. Adekpedjou, N. T. Diouf, L. Goh, L. Blair, and F. Légaré. 2016. A synthesis of knowledge about caregiver decision making finds gaps in support for those who care for aging loved ones. Health Affairs 35(4):619-626.
Gaugler, J. E. 2005. Family involvement in residential and long-term care: A synthesis and critical review. Aging & Mental Health 9(2):105-118.
George, L. K., and L. P. Gwyther. 1986. Caregiver well-being: A multidimensional examination of family caregivers of demented adults. The Gerontologist 26(3):253-259.
Gibbons, S. W., A. Ross, and M. Bevans. 2014. Liminality as a conceptual frame for understanding the family caregiving rite of passage: An integrative review. Research in Nursing and Health 37(5):423-436.
Gillick, M. R. 2013. The critical role of caregivers in achieving patient-centered care. Journal of the American Medical Association 310(6):575-576.
Girgis, A., S. D. Lambert, P. McElduff, B. Bonevski, C. Lecathelinais, A. Boyes, and F. Stacey. 2013. Some things change, some things stay the same: A longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psycho-Oncology 22(7):1557-1564.
Gitlin, L. N., and R. Schulz. 2012. Family caregiving of older adults. In Public health for an aging society, edited by T. R. Prohaska, L. A. Anderson, and R. H. Binstock. Baltimore, MD: The Johns Hopkins University Press. Pp. 181-205.
Gitlin, L. N., and J. Wolff. 2012. Family involvement in care transitions of older adults: What do we know and where do we go from here? Annual Review of Gerontology and Geriatrics 31(1):31-64.
Gitlin, L. N., H. C. Kales, and C. G. Lyketsos. 2012. Nonpharmacologic management of behavioral symptoms in dementia. Journal of the American Medical Association 308(19): 2020-2029.
Given, B. A., C. E. Given, and P. R. Sherwood. 2012. Family and caregiver needs over the course of the cancer trajectory. Journal of Supportive Oncology 10(2):57-64.
Givens, J. L., R. P. Lopez, K. M. Mazor, and S. L. Mitchell. 2012. Sources of stress for family members of nursing home residents with advanced dementia. Alzheimer Disease & Associated Disorders 26(3):254-259.
Glajchen, M. 2004. The emerging role and needs of family caregivers in cancer care. Journal of Supportive Oncology 2(2):145-155.
Grady, P. A., and L. M. Rosenbaum. 2015. The science of caregiver health. Journal of Nursing Scholarship 47(3):197-199.
Gwyther, L. P. 1995. When “the family” is not one voice: Conflict in caregiving families. Journal of Case Management 4(4):150-155.
Gwyther, L. P. 1998. Social issues of the Alzheimer’s patient and family. American Journal of Medicine 104(S1):17S-21S.
Gwyther, L. P., and B. G. Matchar. 2015. The Duke employee elder care consultation: Meeting employees where they are. Generations 39(4):105-108.
Haley, W. E., J. Y. Allen, J. S. Grant, O. J. Clay, M. Perkins, and D. L. Roth. 2009. Problems and benefits reported by stroke family caregivers: Results from a prospective epidemiological study. Stroke 40(6):2129-2133.
Haley, W. E., D. L. Roth, G. Howard, and M. M. Safford. 2010. Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers: Differential effects by race and sex. Stroke 41(2):331-336.
Haley, W. E., D. L. Roth, M. Hovater, and O. J. Clay. 2015. Long-term impact of stroke on family caregiver well-being: A population-based case-control study. Neurology 84(13): 1323-1329.
Hartke, R. J., R. B. King, A.W. Heinemann, P. Semik. 2006. Accidents in older caregivers of person surviving stroke and their relation to caregiver stress. Rehabilitation Psychology 51(2):150-156.
Hinton, L. 2002. Improving care for ethnic minority elderly and their family caregivers across the spectrum of dementia severity. Alzheimer Disease & Associated Disorders 16(2):S50-S55.
Hinton, L., M. Haan, S. Geller, and D. Mungas. 2003. Neuropsychiatric symptoms in Latino elders with dementia or cognitive impairment without dementia and factors that modify their association with caregiver depression. The Gerontologist 43(5):669-677.
Hirst, M. 2005. Carer distress: A prospective, population-based study. Social Science & Medicine 61(3):697-708.
Ji, J., B. Zoller, K. Sundquist, and J. Sundquist. 2012. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation 125(14):1742-1747.
Kasper, J. D., V. A. Freedman, B. C. Spillman. 2014. Disability and care needs of older Americans by dementia status: An analysis of the 2011 National Health and Aging Trends Study. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation. http://aspe.hhs.gov/daltcp/reports/2014/NHATS-DS.pdf (accessed February 4, 2015).
Kelly, B., A. Rid, and D. Wendler. 2012. Systematic review: Individuals’ goals for surrogate decision making. Journal of American Geriatrics Society 60(5):884-895.
Kenyon, K. 2015 January 16. Insights from direct experience as a family caregiver. Testimony to the committee on family caregiving of older adults. Testimony at IOM Workshop on Perspectives on Family Caregiving for Older Adults, Washington, DC.
Kiecolt-Glaser, J. K., K. J. Preacher, R. C. MacCallum, C. Atkinson, W. B. Malarkey, and R. Glaser. 2003. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proceedings of the National Academy of Sciences of the United States of America 100(15):9090-9095.
Kim, J. H., B. G. Knight, and C. V. Longmire. 2007. The role of families in stress and coping processes among African American and white dementia caregivers: Effects on mental and physical health. Health Psychology 26(5):564-576.
Kim, Y., and R. Schulz. 2008. Family caregivers’ strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health 20(5):483-503.
Kim, Y., F. Baker, and R. L. Spillers. 2007. Cancer caregivers’ quality of life: Effects of gender, relationship, and appraisal. Journal of Pain and Symptom Management 34(3):294-304.
Kim, Y., K. M. Shaffer, C. S. Carver, and R. S. Cannady. 2014. Prevalence and predictors of depressive symptoms among cancer caregivers 5 years after the relative’s cancer diagnosis. Journal of Consulting and Clinical Psychology 82(1):1-8.
King, R. B., C. R. Ainsworth, M. Ronen, and R. J. Hartke. 2010. Stroke caregivers: Pressing problems reported during the first months of caregiving. Journal of Neuroscience Nursing 42(6):302-311.
Kitko, L. A., J. E. Hupcey, C. Pinto, and M. Palese. 2015. Patient and caregiver incongruence in advanced heart failure. Clinical Nursing Research 24(4):388-400.
Krouse, H. J., S. F. Rudy, A. H. Vallerand, and E. M. Walizer. 2004. Impact of tracheostomy or laryngectomy on spousal and caregiver relationships. ORL Head and Neck Nursing 1(22):10-25.
Kurtz, M. E., J. C. Kurtz, C. W. Given, and B. Given. 1995. Relationship of caregiver reactions and depression to cancer patients’ symptoms, functional states and depression—A longitudinal view. Social Science & Medicine 40(6):837-846.
Lachs, M., and J. Berman. 2011. Under the radar: New York State Elder Abuse Prevalence Study. Brighton, NY: Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, and New York City Department for the Aging.
Lafferty, A., G. Fealy, C. Downes, and J. Drennan. 2016. The prevalence of potentially abusive behaviours in family caregiving: Findings from a national survey of family carers of older people. Age and Ageing 45(5):703-707.
Laumann, E. O., S. A. Leitsch, and L. J. Waite. 2008. Elder mistreatment in the United States: Prevalence estimates from a nationally representative study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 63(4):S248-S254.
Martindale-Adams, J., L. O. Nichols, J. Zuber, R. Burns, and M. J. Graney. 2015. Dementia caregivers’ use of services for themselves. The Gerontologist (Advance Access). http://gerontologist.oxfordjournals.org/content/early/2015/09/08/geront.gnv121.abstract (accessed April 7, 2016).
Mausbach, B. T., T. L. Patterson, Y. G. Rabinowitz, I. Grant, and R. Schulz. 2007. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychology 26(5):539-544.
McCurry, S. M., R. G. Logsdon, L. Teri, and M. V. Vitiello. 2007. Sleep disturbances in caregivers of persons with dementia: Contributing factors and treatment implications. Sleep Medicine Reviews 11(2):143-153.
McLennon, S. M., T. Bakas, N. M. Jessup, B. Habermann, and M. T. Weaver. 2014. Task difficulty and life changes among stroke family caregivers relationship to depressive symptoms. Archive of Physical Medicine and Rehabilitation 95(12):2484-2490.
Milne, A., and C. Chryssanthopoulou. 2005. Dementia caregiving in Black and Asian populations: Reviewing and refining the research agenda. Journal of Community and Applied Social Psychology 15(5):319-337.
Monin, J. K., and R. Schulz. 2009. Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging 24(3):681-695.
Moon, H., A. L. Townsend, C. J. Whitlatch, and P. Dilworth-Anderson. 2016. Quality of life for dementia caregiving dyads: Effects of incongruent perceptions of everyday care and values. The Gerontologist (Advanced Access).
NAC (National Alliance for Caregiving) and AARP Public Policy Institute. 2009. Caregiving in the United States, 2009. Washington, DC.
NAC and AARP Public Policy Institute. 2015. Caregiving in the United States, 2015. Washington, DC.
Nápoles, A. M., L. Chadiha, R. Eversley, and G. Moreno-John. 2010. Developing culturally sensitive dementia caregiver interventions: Are we there yet? American Journal of Alzheimer’s Disease and Other Dementias 25(5):389-406.
National Center on Elder Abuse. 2015. NCEA frequently asked questions. http://www.ncea.aoa.gov/faq/index.aspx (accessed January 21, 2016).
Nielsen, M., J. Hansen, B. Ritz, H. Nordahl, E. Schernhammer, L. Wermuth, and N. H. Rod. 2014. Cause-specific mortality among spouses of Parkinson disease patients. Epidemiology 25(2):225-232.
NRC (National Research Council). 2010. Informal caregivers in the United States: Prevalence, caregiver characteristics, and ability to provide care. In National Research Council, The role of human factors in home health care: Workshop summary. Washington, DC: The National Academies Press. Pp. 117-143.
NRC. 2011. Health care comes home: The human factors. Washington, DC: The National Academies Press.
O’Reilly, D., S. Connolly, M. Rosato, and C. Patterson. 2008. Is caring associated with an increased risk of mortality? A longitudinal study. Social Science & Medicine 67(8): 1282-1290.
O’Reilly, D., M. Rosato, A. Maguire, and D. Wright. 2015. Caregiving reduces mortality risk for most caregivers: A census-based record linkage study. International Journal of Epidemiology 44(6):1959-1969.
Ory, M. G., R. R. Hoffman, J. L. Yee, S. Tennstedt, and R. Schulz. 1999. Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. The Gerontologist 39(2):177-185.
Peacock, S. C., K. Hammond-Collins, and D. A. Forbes. 2014. The journey with dementia from the perspective of bereaved family caregivers: A qualitative descriptive study. BMC Nursing 13(1):42-52.
Pearlin, L. I., J. T. Mullan, S. J. Semple, and M. M. Skaff. 1990. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist 30(5):583-594.
Penrod, J., J. E. Hupcey, B. L. Baney, and S. J. Loeb. 2011. End-of-life caregiving trajectories. Clinical Nursing Research 20(1):7-24.
Penrod, J., J. E. Hupcey, P. Z. Shipley, S. J. Loeb, and B. Baney. 2012. A model of caregiving through the end of life: Seeking normal. Western Journal of Nursing Research 34(2):174-193.
Perkins, M., V. J. Howard, V. G. Wadley, M. Crowe, M. M. Stafford, W. E. Haley, G. Howard, and D. L. Roth. 2013. Caregiving strain and all-cause mortality: Evidence from the REGARDS Study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 68(4):504-512.
Persson, J., L. Holmegaard, I. Karlberg, P. Redfors, K. Jood, C. Jern, C. Blomstrand, and G. Forsberg-Warleby. 2015. Spouses of stroke survivors report reduced health-related quality of life even in long-term follow-up: Results from Sahlgrenska Academy Study on Ischemic Stroke. Stroke 46(9):2584-2590.
Pinquart, M., and S. Sörenson. 2003. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 58(2):P112-P128.
Pinquart, M., and S. Sörenson. 2005. Ethnic differences in stressors, resources and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist 45(1):90-106.
Pinquart, M., and S. Sörenson. 2006. Gender differences in caregiver stressors, social resources and health: Updated meta-analysis. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 61(1):P33-P45.
Pinquart, M., and S. Sörenson. 2007. Correlates of physical health of informal caregivers: A meta-analysis. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 62(2):P126-P137.
Rabinowitz, Y. G., B. T. Mausbach, L. W. Thompson, and D. Gallagher-Thompson. 2007. The relationship between self-efficacy and cumulative health risk associated with health behavior patterns in female caregivers of elderly relatives with Alzheimer’s dementia. Journal of Aging and Health 19(6):946-964.
Ramsay, S., E. Grundy, and D. O’Reilly. 2013. The relationship between informal caregiving and mortality: An analysis using the ONS Longitudinal Study of England and Wales. Journal of Epidemiology and Community Health 67(8):655-660.
Reinhard, S., and L. Feinberg. 2015. The escalating complexity of family caregiving: Meeting the challenge. In Family caregiving in the new normal, edited by J. E. Gaugler and R. L. Kane. London, UK: Academic Press. Pp. 291-304.
Reinhard, S. C., C. Levine, and S. Samis. 2012. Home alone: Family caregivers providing complex chronic care. Washington, DC: United Hospital Fund and AARP Public Policy Institute.
Robison, J., R. Fortinsky, A. Kleppinger, N. Shugrue, and M. Porter. 2009. A broader view of family caregiving: Effects of caregiving and caregiver conditions on depressive symptoms, health, work, and social isolation. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 64(6):788-798.
Roth, D. L., L. Fredman, and W. E. Haley. 2015. Informal caregiving and its impact on health: A reappraisal from population-based studies. The Gerontologist 55(2):309-319.
Ryan, A. A., and H. F. Scullion. 2000. Family and staff perceptions of the role of families in nursing homes. Journal of Advanced Nursing 32(3):626-634.
Saban, K. L., P. R. Sherwood, H. A. DeVon, and D. M. Hynes. 2010. Measures of psychological stress and physical health in family caregivers of stroke survivors: A literature review. Journal of Neuroscience Nursing 42(3):128-138.
Sabatino, C. 2015. Into the matrix of law and caregiving. Generations 39(4):80-88.
Salgado-Garcia, F. I., J. K. Zuber, M. J. Graney, L. O. Nichols, J. L. Martindale-Adams, and F. Andrasik. 2015. Smoking and smoking increase in caregivers of Alzheimer’s patients. The Gerontologist 55(5):780-792.
Schoenmakers, B., F. Buntinx, and J. Delepeleire. 2010. Factors determining the impact of care-giving on caregivers of elderly patients with dementia. A systematic literature review. Maturitas 66(2):191-200.
Schulz, R. 2013. Research priorities in geriatric palliative care: Informal caregiving. Journal of Palliative Medicine 16(9):1008-1112.
Schulz, R., and S. R. Beach. 1999. Caregiving as a risk factor for mortality—The Caregiver Health Effects Study. Journal of the American Medical Association 282(23):2215-2219.
Schulz, R., and P. R. Sherwood. 2008. Physical and mental health effects of family caregiving. American Journal of Nursing 108(9):23-27.
Schulz, R., A. T. O’Brien, J. Bookwala, and K. Fleissner. 1995. Psychiatric and physical morbidity effects of dementia caregiving—Prevalence, correlates, and causes. The Gerontologist 35(6):771-791.
Schulz, R., J. Newsom, M. Mittelmark, L. Burton, C. Hirsch, and S. Jackson. 1997. Health effects of caregiving: The Caregiver Health Effects Study: An ancillary study of the cardiovascular health study. Annals of Behavioral Medicine 19(2):110-116.
Schulz, R., A. B. Mendelsohn, W. E. Haley, D. Mahoney, R. S. Allen, S. Zhang, L. Thompson, and S. H. Belle. 2003. End of life care and the effects of bereavement on family caregivers of persons with dementia. New England Journal of Medicine 349(20):1936-1942.
Schulz, R., S. H. Belle., S. J. Czaja, K. A. McGinnis, A. Stevens, and S. Zhang. 2004. Long-term care placement of dementia patients and caregiver health and well-being. Journal of the American Medical Association 292(8):961-967.
Schulz, R., R. S. Hebert, M. A. Dew, S. L. Brown, M. F. Scheier, S. R. Beach, S. J. Czaja, L. M. Martire, D. Coon, K. M. Langa, L. N. Gitlin, A. B. Stevens, and L. Nichols. 2007. Patient suffering and caregiver compassion: New opportunities for research, practice, and policy. The Gerontologist 47(1):4-13.
Schulz, R., S. R. Beach, R. S. Hebert, L. M. Martire, J. K. Monin, C. A. Tompkins, and S. M. Albert. 2009. Spousal suffering and partner’s depression and cardiovascular disease: The Cardiovascular Health Study. The American Journal of Geriatric Psychiatry 17(3):246-254.
Schulz, R., S. R. Beach, T. B. Cook, L. M. Martire, J. M. Tomlinson, and J. K. Monin. 2012. Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging & Mental Health 16(6):712-721.
Schumacher, K. L., B. J. Stewart, P. G. Archbold, M. J. Dodd, and S. L. Dibble. 2000. Family caregiving skill: Development of the concept. Research in Nursing & Health 23(3):191-203.
Seltzer, M. M., and L. W. Li. 2000. The dynamics of caregiving: Transitions during a three-year prospective study. The Gerontologist 40(2):165-178.
Silver, H. J., N. S. Wellman, D. Galindo-Ciocon, and P. Johnson. 2004. Family caregivers of older adults on home enteral nutrition have multiple unmet task-related training needs and low overall preparedness for caregiving. Journal of the American Dietetic Association 104(1):43-50.
Sisk, R. J. 2000. Caregiver burden and health promotion. International Journal of Nursing Studies 37(1):37-43.
Skaff, M. M., and L. I. Pearlin. 1992. Caregiving-role engulfment and the loss of self. The Gerontologist 32(5):656-664.
Son, J., A. Erno, D. G. Shea, E. E. Femia, S. H. Zarit, and M. A. P. Stephens. 2007. The caregiver stress process and health outcomes. Journal of Aging and Health 19(6):871-887.
Spillman, B. C., J. Wolff, V. A. Freedman, and J. D. Kasper. 2014. Informal caregiving for older Americans: An analysis of the 2011 National Study of Caregiving. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation. http://aspe.hhs.gov/report/informal-caregiving-older-americans-analysis-2011-national-health-and-agingtrends-study (accessed April 9, 2015).
Stenberg, U., C. M. Ruland, and C. Miaskowski. 2010. Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology 19(10):1013-1025.
Strawbridge, W. J., and M. I. Wallhagen. 1991. Impact of family conflict on adult child caregivers. The Gerontologist 31(6):770-777.
Swore Fletcher, B., C. Miaskowski, B. Given, and K. Schumacher. 2012. The cancer family caregiving experience: An updated and expanded conceptual model. European Journal of Oncology Nursing 16(4):387-398.
Torke, A. M., M. Siegler, A. Abalos, R. M. Moloney, and G. C. Alexander. 2009. Physicians’ experience with surrogate decision making for hospitalized adults. Journal of General Internal Medicine 24(9):1023-1028.
Torke, A. M., G. A. Sachs, P. R. Helft, K. Montz, S. L. Hui, J. E. Slaven, and C. M. Callahan. 2014. Scope and outcomes of surrogate decision making among hospitalized older adults. JAMA Internal Medicine 174(3):370-377.
Tornatore, J. B., and L. A. Grant. 2004. Family caregiver satisfaction with the nursing home after placement of a relative with dementia. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 59(2):S80-S88.
Torti, F. M., L. P. Gwyther, S. D. Reed, J. Y. Friedman, and K. A. Schulman. 2004. A multinational review of recent trends and reports in dementia caregiver burden. Alzheimer Disease & Associated Disorders 18(2):99-109.
van der Lee, J., T. J. Bakker, H. J. Duivenvoordenc, and R. M. Droes. 2014. Multivariate models of subjective caregiver burden in dementia: A systematic review. Ageing Research Reviews 15:76-93.
van Ryn, M., S. Sanders, K. Kahn, C. van Houtven, J. M. Griffin, M. Martin, A. A. Atienza, S. Phelan, D. Finstad, and J. Rowland. 2011. Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psycho-Oncology 20(1):44-52.
Vitaliano, P. P., J. P. Zhang, and J. M. Scanlan. 2003. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin 129(6):946-972.
von Känel, R., B. T. Mausbach, T. L. Patterson, J. E. Dimsdale, K. Aschbacher, P. J. Mills, M. G. Ziegler, S. Ancoli-Israel, and I. Grant. 2008. Increased Framingham Coronary Heart Disease Risk Score in dementia caregivers relative to non-caregiving controls. Gerontology 54(3):131-137.
von Känel, R., B. T. Mausbach, J. E. Dimsdale, P. J. Mills, T. L. Patterson, S. Ancoli-Israel, M. G. Ziegler, S. K. Roepke, E. A. Chattillion, M. Allison, and I. Grant. 2012. Effect of chronic dementia caregiving and major transitions in the caregiving situation on kidney function: A longitudinal study. Psychosomatic Medicine 74(2):214-220.
Wang, X., K. M. Robinson, and H. K. Hardin. 2015. The impact of caregiving on caregivers’ medication adherence and appointment keeping. Western Journal of Nursing Research 37(12):1548-1562.
Weiner, M. F. 2008. Perspective on race and ethnicity in Alzheimer’s disease research. Alzheimer’s Dementia 4(4):233-238.
Wendler, D., and A. Rid. 2011. The effect on surrogates of making treatment decisions for others. Annals of Internal Medicine 154(5):336-346.
Whitlatch, C. J. and L. F. Feinberg. 2007. Family care and decision making. In Dementia and social work practice: Research and interventions, edited by C. Cox. New York: Springer. Pp. 129-148.
Whitlatch, D. 2008. Informal caregivers: Communication and decision making. American Journal of Nursing 103(9 Suppl):73-77.
Wilcox, S., and A. C. King. 1999. Sleep complaints in older women who are family caregivers. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 54(3):P189-P198.
Williams, S.W., S. Zimmerman, and C.S. Williams. 2012. Family caregiver involvement for long-term care residents at the end of life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 67(5):595-604.
Wolff, J. L. 2007 (unpublished). Supporting and sustaining the family caregiver workforce for older Americans: Paper commissioned by the IOM Committee on the Future Health Care Workforce for Older Americans.
Wolff, J., S. Dy, K. Frick, and J. Kasper. 2007. End of life care: Findings from a national survey of family caregivers. Archives of Internal Medicine 167(1):40-46.
Wolff, J. L., B. C. Spillman, V. A. Freedman, and J. D. Kasper. 2016. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Internal Medicine 176(3):372-379.
Yee, J. L., and R. Schulz. 2000. Gender differences in psychiatric morbidity among family caregivers: A review and analysis. The Gerontologist 40(2):147-164.
Yueh-Feng Lu, Y., and M. G. Austrom. 2005. Distress responses and self-care behaviors in dementia family caregivers with high and low depressed mood. Journal of the American Psychiatric Nurses Association 11(4):231-240.
Zarit, S. H., K. E. Reever, and J. Bach Peterson. 1980. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist 20(6):649-655.
Zarit, S. H., and J. E. Gaugler. 2000. Caregivers and stress. In Encyclopedia of stress Vol. 1, edited by G. Fink. San Diego, CA: Academic Press. Pp. 404-407.
Zarit, S. H., E. E. Femia, K. Kim, and C. J. Whitlatch. 2010. The structure of risk factors and outcomes for family caregivers: Implications for assessment and treatment. Aging & Mental Health 14(2):220-231.


















































