3
Perspectives from Professional and Accrediting Organizations1
The next session was the first of three panel sessions and focused on the perspectives of professional and accrediting organizations. The session was moderated by Phyllis Meadows from The Kresge Foundation and featured presentations by Brian Castrucci from the de Beaumont Foundation and Kalpana Ramiah from America’s Essential Hospitals (AEH). Following these presentations, Laura Rasar King from the Council on Education for Public Health (CEPH), Kaye Bender from the Public Health Accreditation Board (PHAB), and Lisa Howley from the Association of American Medical Colleges (AAMC) served as discussants. There was also an opportunity for discussion with other workshop attendees in the audience.
PUBLIC HEALTH WORKFORCE INTEREST AND NEEDS SURVEY2
Brian Castrucci opened by providing a brief background on the de Beaumont Foundation, explaining that it focuses on “the people, the policies, and the partnerships that [are necessary] for communities to achieve their optimal health.” His presentation addressed the governmen-
___________________
1 This chapter summarizes information presented by panel session speakers. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
2 This section summarizes information presented by Brian Castrucci from the de Beaumont Foundation. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
tal public health workforce, which he called “the backbone of a healthy community.”
To provide context on his perspective, Castrucci explained that prior to joining the Foundation, he worked in state and local public health agencies. He noted that the Foundation would often consult state health officials when seeking to understand the needs of governmental public health agencies. However, he added, due to their limited tenure or lack of prior experience in governmental settings, these officials’ answers did not fully capture the needs of the public health workforce. As Castrucci explained, this led the Foundation to create the Public Health Workforce Interests and Needs Survey (PH WINS) “to capture the ideas, thoughts, [and] challenges of the other 99.9 percent of the workforce.”
The PH WINS was first conducted in 2014 in 37 states and received more than 10,000 responses. A pilot conducted among local public health agencies added approximately 10,000 more responses. In 2017, the Foundation conducted the survey with 47 state health agencies and a nationally representative sample of local health departments, and had more than 47,000 respondents. Castrucci noted that the detailed findings from the 2017 survey were published in the March 2019 supplement in the Journal of Public Health Management and Practice (PH WINS, 2019). His presentation at the workshop focused on key high-level findings from the 2017 survey, implications, and next steps.3
According to Castrucci, the survey found high levels of job satisfaction in the public health workforce. However, many workers were considering leaving their jobs in the next year. He noted that this was due to workers nearing retirement age and younger people departing their jobs. The survey also found that most workers were satisfied with their jobs but not equally satisfied with their pay. There was also a high level of worker engagement.
The survey found that the top training needs of workers at all levels in administration and management, including executives, managers, and frontline staff, were budget and finance. Castrucci provided an anecdote using his own experience as an epidemiologist earlier in his career, noting that while he was skilled in research and analysis, he did not know about benefits or budgeting. He explained that he felt well prepared to work as an epidemiologist but had not been trained to be a leader, manager, or businessperson, yet these were aspects of his job.
Castrucci next provided some statistics comparing the demographics of the public health workforce with those of the U.S. workforce as a whole. The public health workforce is primarily (79 percent) female; however, 4
___________________
3 More information about the PH WINS is available at https://www.debeaumont.org/ph-wins (accessed May 10, 2021).
out of every 100 male workers reach the highest levels of leadership, versus only 2 women. The workforce is also primarily white and much older than the U.S. workforce, with 45 percent over 50 years of age and 10 percent under 30, presenting a challenge when the large number of older workers retires. Castrucci noted that the public health workforce is also well educated, with older workers more likely to have a bachelor’s degree as their highest degree and younger workers more likely to have a master’s degree.
As Castrucci mentioned earlier, nearly half the public health workforce (47 percent) is considering leaving an organization, an increase of 41 percent between 2014 and 2017. He elaborated that 22 percent of workers are planning to retire, noting that these are people who say they plan to retire, not simply that they have reached retirement age. Castrucci highlighted as particularly concerning the 25 percent of workers who say they plan to leave their job in the next year for reasons other than retirement.
Castrucci outlined the top five reasons that workers leave: (1) inadequate pay, (2) lack of advancement, (3) workplace environment, (4) low job satisfaction, and (5) lack of support. He noted that except for pay, all of these reasons are within management’s control in a health department or organization. While public health may not be able to compete on pay with health care systems, Castrucci suggested that it could ensure there are opportunities for advancement or stretch assignments and provide a solid work environment. Castrucci highlighted the paradox that while job satisfaction is high (81 percent), satisfaction with pay is low (48 percent).
As Castrucci explained, the survey found that the public health workforce is mission driven. In the 2014 survey, 98 percent of respondents agreed with the statement that they pursued a public health career because they wanted to make a difference. This question was not asked in 2017 because there was such high agreement on the first survey. The PH WINS inquired about drivers of workforce engagement, and Castrucci noted that there were individual-level factors, such as having high motivation and believing that the work being carried out is important and related to the agency’s goals and priorities.
He added that there are also management-level factors that require attention. He was particularly concerned that only 44 percent of respondents said that “creativity and innovation are rewarded” in their workplace, emphasizing that the workforce has a large number of people with master’s degrees. For example, after participating in a learning collaborative that the Foundation convened, South Carolina was able to change its statistics regarding support for creativity and innovation.
Castrucci next described some ways the Foundation is addressing the problems identified in the survey. To address budget- and finance-related training needs, the Foundation has partnered with the University of Miami to create a program called Building Essentials in Administra-
tion and Management, a $500 certificate course for people working in governmental public health. Castrucci suggested that public health end its assessments of needs and gaps and focus on addressing the already identified needs and gaps.
With respect to emerging concepts in public health, Castrucci noted that only 43 percent of respondents said that multi-sector partnerships were important to their work, and only 35 percent had even heard of “health in all policies,” highlighting the need for more training in these areas. Digging deeper into operationalizing both concepts, Castrucci noted that 85 percent of respondents said that their agency should be involved in health equity. However, only 63 percent thought their agency should be involved in affecting the K–12 system, 53 percent for transportation, 55 percent for the built environment, and 56 percent for the economy.
ROLE OF ESSENTIAL HOSPITALS IN ASSESSING POPULATION HEALTH NEEDS4
Kalpana Ramiah from the Essential Hospitals Institute at AEH opened her presentation with background on the organization.5 She explained that AEH is an association of nearly 300 member hospitals across the country linked by their mission to serve vulnerable populations. There are four other common characteristics of AEH’s member hospitals:
- Providing comprehensive, coordinated care through primary care and specialty care networks;
- Training, with member hospitals training more than three times as many physicians and clinicians as other U.S. hospitals;
- Providing specialized life-saving care, such as trauma care, burn care, and neonatal intensive care unit services, with essential hospitals operating about one-third of the level one trauma centers and 40 percent of the burn care beds in large cities; and
- Focusing on advancing public health (the organization was previously called the National Association of Public Hospitals, and many of its member hospitals still operate or function as part of public health departments).
___________________
4 This section summarizes information presented by Kalpana Ramiah from AEH. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
5 More information about AEH and its resources is available at https://essentialcommunities.org (accessed May 10, 2021).
Ramiah showed a map of the United States that illustrated the prevalence of individuals with claims for three or more chronic conditions, highlighting the differences in color across the country, or the uneven distribution of chronic diseases. She then showed the same map (see Figure 3-1) with added red dots to indicate the locations of AEH member hospitals, highlighting that they are concentrated in the areas with the highest rates of patients with complex needs.
Ramiah pointed out that essential hospitals provide nine times more uncompensated care than other U.S. hospitals, which translates to a margin of 1.6 percent compared with 7.8 percent for hospitals overall. She noted that this statistic would be worse off and reach –3 percent if it were not for the disproportionate share hospital6 payment that these hospitals receive. In addition, many patients in communities served by essential hospitals also have social needs. This includes 25.3 million individuals who are below the poverty line, 19.4 million without health insurance, 10.1 million with limited access to healthy food, and 350,000 who are homeless (Roberson and Ramiah, 2018). Social determinants of health are major issues in essential hospitals.
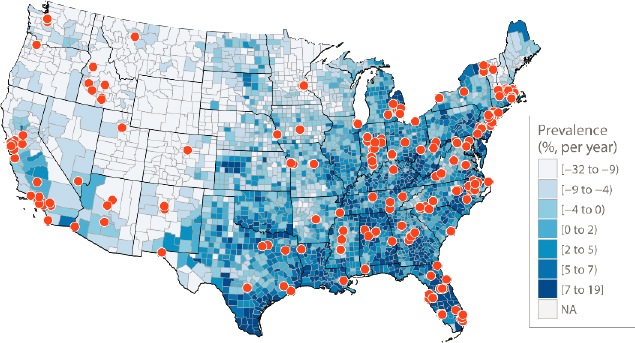
SOURCES: Ramiah presentation, March 22, 2019; CMS, 2016.
___________________
6 Disproportionate share hospitals serve a significantly disproportionate number of low-income patients and receive payments from the Centers for Medicaid & Medicare Services to cover the costs of providing care to uninsured patients. See the Health Resources and Services Administration’s factsheet at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Disproportionate_Share_Hospital.pdf (accessed May 10, 2021).
Ramiah described a model (see Figure 3-2), adapted from a model by Hester et al. (2015) at the Centers for Disease Control and Prevention (CDC), to explain what essential hospitals do in population health. Level 1.0 is episodic nonintegrated care: the patient arrives, is treated, and leaves the hospital. Level 2.0 is the coordinated care system with outcome-accountable care, in which the hospital cares for patients and is also responsible for making sure that they continue to take their medication after they leave. Level 3.0 is community-integrated health care that goes beyond direct medical care to focus on the community. In levels 1.0 and 2.0, the hospital is only concerned with the patient population, but in level 3.0, it addresses the health of the whole community. AEH defines community-integrated health care as a strategy through which health care providers work with other sectors in both complementary and collaborative ways to promote health.
To further illustrate this concept, Ramiah showed a chart (see Figure 3-3) examining the spectrum of community-integrated care. Guiding the audience through the figure, Ramiah provided examples of the activities a member hospital might carry out and where these would be on the quadrants. For example, providing food for patients is a downstream intervention that is just for patients. As another example, opening a food bank for the community is a downstream intervention in the community because, while it is available to all community members, it does not fully address the social determinants of food access and affordability (see Figure 3-3).
Ramiah explained that AEH acknowledges that their member hospitals may have to operate in all three levels. She emphasized that her orga-
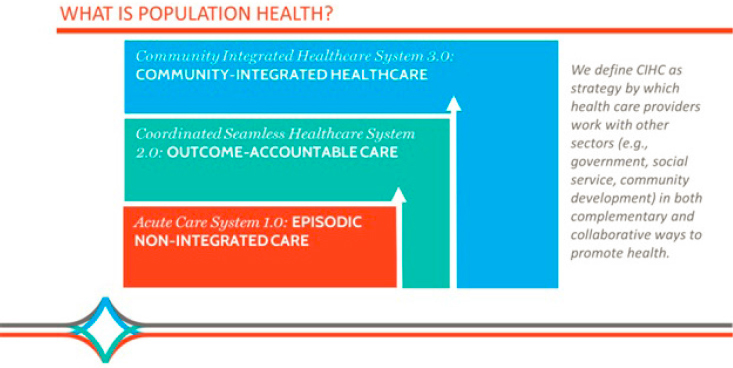
NOTE: CIHC = community integrated health care.
SOURCES: Ramiah presentation, March 22, 2019; adapted from Hester et al., 2015.
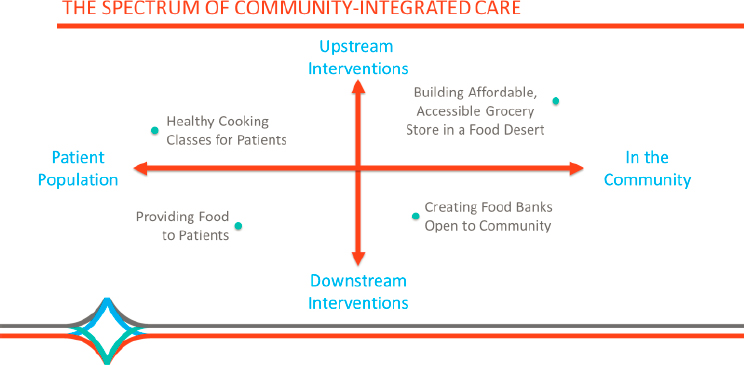
SOURCE: Ramiah presentation, March 22, 2019.
nization sees the spectrum of community-integrated care as just that—a spectrum.
Ramiah next provided information about AEH and what the organization does to support its members. It provides research, education, leadership development, and policy and advocacy. In 2015–2016, it engaged in a strategic initiative related to population health; conducted member surveys, expert interviews, and key informant interviews within its membership; and held a deliberative summit to understand what member hospitals are doing in population health, what they mean by population health, and facilitators and barriers in this work.
Ramiah provided some highlights from the research (AEH, 2016). AEH received survey responses from 106 hospitals and conducted interviews to obtain additional information (see Figure 3-4). In response to questions about additional resources needed for population health improvement activities, the top request was additional funding, particularly funding that was sustainable and not grant dependent. The second most requested resources were data and analytical tools that facilitated data sharing. The next three resource requests related to human capital, including staff training, leadership, and additional staff.
Ramiah next described work funded by The Kresge Foundation examining job descriptions of population health executives in AEH member hospitals, such as directors and vice presidents. AEH conducted interviews and focus groups with them. Ramiah was surprised to learn that many of them did not have job descriptions and that population health was a “one-person department” at a number of hospitals. In addition,
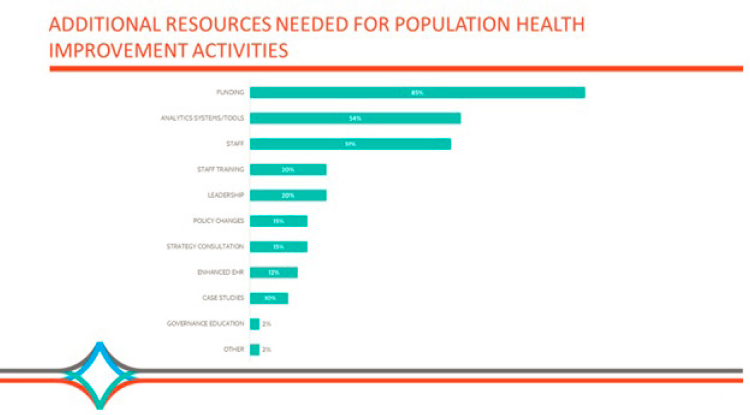
NOTE: EHR = electronic health record.
SOURCES: Ramiah presentation, March 22, 2019; AEH, 2016; preliminary results as of July 5, 2016.
many of their peers did not know much about the work, and these executives did not have much internal credibility. Ramiah explained that the project team also learned that many of the population health executives had formerly been hospital chief operations officers or chief executive officers (CEOs) and were not trained in population health.
The project team’s research led to some key findings about the role of a population health executive at essential hospitals. Internal and external core functions included leadership management, communication, collaboration, and measurement. With respect to the operating environment, there was variation among hospitals, with some being part of an accountable care organization risk-based model. Internal structure (where the population health activities were based and how they were dispersed) also varied among hospitals.
Ramiah noted that as a result of the survey findings, AEH recently released a Toolkit for Hiring and Evaluating Population Health Executives,7 which describes who population health executives are, outlines what skill
___________________
7 For more information about the Toolkit for Hiring and Evaluating Population Health Executives, see the webinar hosted by the Collaborative on Bridging Public Health, Health Care & Community at http://nationalacademies.org/hmd/Activities/PublicHealth/PopulationHealthImprovementRT/Action-Collaborative-Public-HealthHealth-Care-Community (accessed May 10, 2021).
sets are needed, and provides a job description template for hospitals to use. The organization was also working with the directors of graduate medical education (GME) to incorporate population health activities into their training residency programs.
STATE OF PUBLIC HEALTH EDUCATION8
Laura Rasar King from CEPH spoke about the state of public health education in her remarks as a discussant. She began by providing background on CEPH, explaining that it is “the accrediting body for schools and programs in public health, established about 45 years ago as an independent accrediting body, recognized by the Department of Education. [The organization] accredits public health training programs from [the] baccalaureate level to the doctoral level.”9
Public health education has grown significantly in the past several decades. As King noted, when the organization was established in 1974, it accredited 10 schools of public health, and as of the date of the workshop, there were 66 accredited schools of public health, 121 accredited public health programs, and 13 accredited baccalaureate programs not affiliated with a graduate public health program.
King described a couple of the transformations in public health education and training over the past decade. First, her organization identified core components of a bachelor’s degree in public health, and students’ interest in these programs is growing. She noted that the focus on baccalaureate public health programs was in response to concerns that some entities—particularly local public health departments in underserved areas—were unable to recruit enough master’s-trained individuals. As of the date of the workshop, there were 79 accredited undergraduate programs in public health, and King noted that this number continues to grow. The required curriculum for a baccalaureate public health program incorporates concepts of population health as one of nine domains. Population health training includes basic processes, approaches, and interventions that identify and address major health needs and concerns, data collection and analysis, planning and assessment, and evaluation.
The second transformation is related to the Master of Public Health (M.P.H.) degree. As King explained, the M.P.H. degree changed very little in the first century since the Welch-Rose Report described it in 1915. However, CEPH reviewed the pertinent literature along with the PH
___________________
8 This section summarizes information presented by Laura Rasar King from CEPH. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
9 More information about CEPH is available at https://ceph.org (accessed May 10, 2021).
WINS, the Council on Linkages competencies, and the National Board of Public Health Examiners Job Task Analysis. In 2016, the council issued revised criteria that “completely transformed what was expected in terms of public health education at the master’s level.” As King explained, the M.P.H. degree previously had five core courses: epidemiology, biostatistics, health services administration, environmental health, and social and behavioral sciences. Current M.P.H. programs are founded on 22 competencies and 8 domains, which are infused with population health, social determinants of health, and cultural competency. The eight domains are (1) evidence-based approaches, including data collection, analysis, and interpretation; (2) public health and health care systems; (3) planning and management, including budgeting and finance; (4) policy; (5) leadership, including visioning, strategic planning, negotiation, and mediation; (6) communication, both oral and written; (7) interprofessional practice; and (8) systems thinking. The council collected early data, which show that 84 percent of public health schools and programs have changed their core curricula, including the classes and class structure, to match these domains. The remaining 16 percent have kept the previous five core courses but changed the content within them.
LOCAL PUBLIC HEALTH WORKFORCE CONSIDERATIONS10
Kaye Bender from PHAB served as the second discussant and provided remarks regarding local public health workforce considerations. PHAB accredits governmental public health departments across the country. The 11-year-old organization recently launched an additional program for Army preventive medicine public health units and statewide vital records health statistics accreditation.11
Public health department accreditation standards are based on the framework of the 10 essential services of public health, which was selected, as Bender noted, because it was familiar to most public health departments. There are 12 domains, 10 of which are related directly to the 10 essential public health services, with 1 for management and 1 for governance.
Bender focused the remainder of her remarks on her organization’s work related to workforce development and lessons learned. Bender noted that her organization began work with the following assumptions: (1) less
___________________
10 This section summarizes information presented by Kaye Bender from PHAB. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
11 More information about PHAB is available at https://www.phaboard.org (accessed May 10, 2021).
than 10 percent of M.P.H. program graduates went into governmental public health; (2) as a result, most of the governmental public health workforce was not formally educated in public health; (3) government merit systems were an obstacle to workforce innovation and change; and (4) there was no standardized nationwide needs assessment approach, although this final point is no longer true with the development of the PH WINS.
There are two overarching standards in the domain related to workforce, the first from the recognition that less than 10 percent of M.P.H. program graduates went into governmental public health. To address this, health departments have been asked to partner with academic institutions to give students access to public health experiences to promote the development of future public health workers. Bender noted that most health departments do this, as long as there are schools or programs that teach public health content in their immediate geographic area.
The second standard is ensuring a competent workforce through assessing staff competencies, providing individual training and professional development, and creating a supportive work environment, which includes producing a workforce development plan. In the past, partners at the Association of State and Territorial Health Officials (ASTHO), the National Association of County and City Health Officials (NACCHO), the Public Health Foundation, and others have assisted health departments in assessing the needs of the workforce and developing a plan to address them. However, Bender noted that she agrees with Castrucci that the PH WINS eliminates the need for continued assessments, and the focus should be on plan development and implementation.
Bender closed her remarks by stating that health departments have made significant progress in addressing workforce issues, but she agrees with past speakers that there is much more work to be done. She noted that PHAB is in the process of refreshing its standards and measures in the area of workforce development.
PHYSICIAN EDUCATION AND HEALTH EQUITY12
The final discussant of the session was Lisa Howley from AAMC. She remarked on physician education and health equity. Howley began her comments by providing brief background on AAMC and its work related to the population health workforce.13 It was founded in 1876
___________________
12 This section summarizes information presented by Lisa Howley from AAMC. The statements made are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
13 More information about AAMC and its programs is available at https://www.aamc.org (accessed May 10, 2021).
and is a nonprofit association “dedicated to transforming health care through medical education, research, and patient care.”14 Its mission is to serve and lead the academic medicine community for the health of all. Members include 154 U.S. medical schools, 17 Canadian medical schools, nearly 400 major teaching hospitals and health systems, including 51 Department of Veterans Affairs (VA) medical centers, and 80 academic societies. Through these institutions, AAMC serves more than 170,000 full-time faculty members, 90,000 medical students, 130,000 resident physicians, and 60,000 graduate students and postdoctoral researchers in biomedical sciences. Howley explained that as a member service organization, AAMC does not regulate practices, set standards, or conduct accreditations; it has a “supportive, informative, and developmental” relationship with its members.
Howley mentioned that AAMC is particularly dedicated to the issues of health equity, community, and population health. As an example, its most recent annual leadership forum was focused on community engagement to address health disparities. Howley acknowledged that reducing health disparities requires that medical schools and teaching hospitals “invest in building bidirectional trust, developing meaningful relationships, and understanding the historical perspectives of the community members that they serve.” AAMC is actively engaged in population and public health research, clinical practice, and innovations. However, Howley’s focus is medical education, so she provided additional examples within that area.
Howley noted that over the past few decades, higher education, including medicine, has shifted to a competency-based model. AAMC recently released new competencies, and quality improvement in patient safety and health equity is one of those five domains. The competencies were developed over an 18-month period with broad stakeholder input and community collaboration and are intended to support curricular design and assessment across the continuum of medical education for medical students, residents, and practicing physicians.
AAMC also recently partnered with the Provider Training and Education Workgroup led by Don Bradley and Bill Dietz, an ad hoc activity of the National Academies’ Roundtable on Obesity Solutions. As Howley explained, the workgroup developed core interprofessional competencies for obesity prevention and management and is working to extend improvements in nutrition and physical activity education to health profession schools beyond medicine.
In addition, for more than 20 years, AAMC has had an interprofessional cooperative agreement with CDC focused on enhancing population
___________________
14 See https://www.aamc.org/who-we-are (accessed May 10, 2021).
health education and providing experiential opportunities for medical, nursing, and public health students. A number of projects are being conducted under this cooperative agreement. One example is a free Web-based directory known as Public Health Pathways, which includes more than 200 domestic and international public health training opportunities across the education continuum and across professions. As another example, in 2019, AAMC published a monograph featuring lessons learned and best practices within GME residency programs for effectively teaching and modeling population health management in a primary care setting.
Additionally, AAMC hosted a national workshop in May 2019 for educational leaders from U.S. medical schools to advance medical education to combat opioid misuse. An additional initiative is the MedEdPORTAL, an open-access, peer-reviewed publication that promotes educational scholarship and the dissemination of teaching and educational resource materials, which AAMC co-sponsors with the American Dental Education Association. There is a collection focused on diversity, inclusion, and health equity that includes publications addressing topics such as food insecurity, community and home violence, cultural humility, obesity care, homelessness, and school health.
Within its Scientific Affairs Division, AAMC has an initiative titled Accelerating Health Equity: Advancing Through Discovery, the mission of which is to identify, evaluate, and disseminate effective and replicable AAMC member institution practices that are improving community health and reducing health inequities.15
In closing, Howley emphasized that she believes that improving population health is an important part of a physician’s responsibilities and “requires an educational program that is competency based and designed to mutually benefit the local needs of the academic health system and the communities within which they serve.”
DISCUSSION
As session moderator, Meadows opened the audience discussion by highlighting some key takeaways and asking the speakers two questions: whether the right people are being targeted for additional training in public health and what is being done to create a supportive work environment in local government that embraces population health and health equity.
Bender responded by providing anecdotes from her 40 years of experience in public health. Bender mentioned she is aware of many courses
___________________
15 See https://www.aamc.org/what-we-do/mission-areas/medical-research/rocc/sponsored-award-programs/donaghue-grants (accessed May 10, 2021).
targeting public health leaders and is unsure whether this training is directed at the appropriate level. Bender noted that having well-trained leaders is important but that these leaders often do not stay in their positions very long, particularly at the state level.
In response to Meadows’s second question, Bender answered that she believes leadership’s actions matter. She noted that she is referring to leadership as more than a single health department leader. As she explained, “You get a progressive, well educated in the whole arena of managing the public health department leader, who surrounds him- or herself with other leaders who are interested in quality improvement, interested in health equity, interested in being innovative, then you see that health department make an almost dramatic shift.” Bender added that the importance of leadership is particularly evident after a dynamic leader leaves and there is a loss of that type of leadership.
Ramiah added that she agrees regarding the importance of leadership for population health. She noted that most of the success stories with essential hospitals come from places where the CEO and population health executive are coordinated and aware of each other’s priorities. Ramiah spoke of the importance of this “dual leadership,” which comes from “peer pressure, … environmental changes, and … motivation that needs to get to the board and the CEO,” rather than skills or training.
In response to the question as to whether training is happening at the right level, Castrucci answered based on his experience in government public health, pointing out that training is often only offered to people with certain titles or at a certain level. He noted that state public health commissioners may not have prior experience within government or public health and questioned how this may impact the governmental public health workforce they are tasked with leading.
Sagar Shah from the American Planning Association asked Castrucci whether his organization had assessed any geographic patterns in the public health workers who intend to leave their organization and whether any particular areas of the country are in crisis. Castrucci responded by stating that the PH WINS needs to improve the question on where potentially departing workers intend to go. He explained that there are geographical differences; however, because the PH WINS is conducted in partnership with ASTHO, NACCHO, and the Big Cities Health Coalition, regional and state data are available, but there is an agreement not to release individual state-level data without the permission of the state health official.
Anna Ricklin from the Fairfax County Health Department in Virginia asked panelists to comment on the data point Castrucci presented that
most local public health workers support health equity but are not familiar with or supportive of the concept of health in all policies. She asked panelists for their thoughts on what can be done to shift the culture. Castrucci responded that he was not surprised that local public health departments are not engaged in health in all policies because they are not funded to do so. He suggested that national government public health agencies, such as CDC, and national organizations, such as ASTHO, NACCHO, and the American Public Health Association, determine that health in all policies is important and provide training on how state and local public health agencies can implement them. Bender agreed, emphasizing the importance of removing silos in categorical program funding and noting that with funding cuts, health department staff often work to protect the funds for their program.
Ron Bialek from the Public Health Foundation asked whether there are further plans to support public health departments in addressing needs and gaps, based on factors such as current workforce composition and organizational priorities. Meadows clarified that given the topic of the workshop, the focus should be on addressing needs and gaps specifically to support population health. Bender responded by explaining that PHAB asks health departments to consider how to align their workforce development plan and implementation with their overall strategic plan, which they have been asked to align with their community health improvement plan.
Maryjoan Ladden from the Robert Wood Johnson Foundation explained that the foundation has been working on population health preparation in nursing and is moving toward expanding it to all health professionals. She asked the panel “how well they think population health competencies and capabilities are integrated into accreditation standards and curricula across medicine, nursing, social work, and other health professions.” King responded that with respect to training in public health, there was a report by the Association of Schools & Programs of Public Health called Population Health Across All Professions (ASPPH, 2015). As another example, King explained that the Association of Specialized and Professional Accreditors—the membership association for accrediting bodies in all professions, including the health professions—worked on a task force a few years ago on a professional doctorate among all the health professions. She noted that population health was one of the areas that was common in the professional doctorate. Points made by the speakers in this section are highlighted below (see Box 3-1).
















