4
National Programs Addressing Dietary Needs of the Older Population
OUTLOOK ON LEGISLATION ON NUTRITION AND AGING
Bob Blancato, Executive Director of the National Association of Nutrition and Aging Services Programs (NANASP), explained that NANASP represents 1,100 service providers around the country who support healthy nutrition for older adults. For the concerns of older adults and nutrition, Blancato opined that the 2-year budget agreement passed by the House of Representatives in October 2015 was beneficial because it meant no return to sequestration or across-the-board cuts through at least September 30, 2017. In addition, it included a $40 billion increase over 2 years in nondefense discretionary spending. Following the direction of President Obama’s budget, two examples of what might occur as a result of the agreement are
- $60 million in funding for programs covered by the Older Americans Act (OAA), and
- $83.7 billion for the Supplemental Nutrition Assistance Program (SNAP), an increase of almost $2 billion, including $9 million for senior SNAP outreach.
Legislation and Programs
Blancato described the outlook for several pieces of legislation and programs important to nutrition and older adults.
OAA. This program has been one of the Great Society programs, and celebrated its 50th anniversary in 2015. Its three largest programs are the congregate meals program, home-delivered meals, and the Nutrition Services Incentive Programs. The OAA provides meals, nutrition education, and socialization for its participants, and current funding levels allow for provision of 224 million meals to older adults every year. At the 2015 White House Conference on Aging, President Obama called for its reauthorization, which prompted the Senate to pass S.192, a modest 3-year reauthorization of the Act. However, as of October 2015, the House of Representatives had not yet acted on the legislation. Funding continues during this time, yet Blancato stressed the need to complete legislative action so as to be prepared for the future nutrition needs of older adults.
Blancato continued by stating that given the current situation, aging services providers can and do look for alternate funding sources beyond the OAA. For many, Medicaid is a new and deeper source of funding. Total funding for home- and community-based services (HCBSs), including nutrition, has risen from 13 percent of the Medicaid budget in 1990 to 43 percent today, and Medicaid expansion under the Affordable Care Act (ACA) is bringing more older adults into the program. Blancato stated that funding for Medicaid will grow from $299 billion in 2014 to $576 billion in 2024, and that managed care alone will grow to $193 billion per year in 2024. At least 46 states administered Medicaid waiver programs which include nutrition.
ACA. Blancato stated that the outlook for the core law appears to be good, now that it has been upheld by the Supreme Court, although smaller changes to the law may occur. With respect to older adults, the law allows for an annual wellness visit with a health care provider, and 23 states now require some form of nutritional counseling and therapy (mostly for obesity and/or diabetes) to be covered as an essential health benefit.
Community-Based Care Transitions Program. This program, which is created by Section 3026 of the ACA, tests models for improving care transitions from the hospital to other settings and reducing readmissions for high-risk Medicare beneficiaries. Many of these models are run by aging networks, including nutrition providers. However, Blancato noted that not enough emphasis is placed on nutrition in the first rounds of testing of these models. Efforts are now under way to extend these programs to allow full benefits to be reached.
Social Services Block Grants. This program has multiple constituents, including older adults, explained Blancato. Estimates are that $30 million for elderly nutrition is provided through the program ($25 million for home-delivered meals and $5 million for congregate meals). Blancato stated that the program is always in danger of being defunded, and advocates
spend considerable energy ensuring that funding for the program is not cut or eliminated.
Agricultural Act of 2014. Better known as the “Farm Bill,” the Agricultural Act of 2014 is an omnibus, multiyear piece of legislation that governs agricultural and food programs. The Bill, which was renewed for 5 years, includes several domestic nutrition programs for older adults. These include SNAP, which reaches 4 million older adults, the Senior Farmers’ Market Nutrition Program (SFMNP), which reaches 835,000 older adults in 52 states and tribal areas, and the Commodity Supplemental Food Program (CSFP), which has transitioned to a program serving only older adults. It serves 573,000 older adults per month in 49 states and tribal areas.
Medical nutrition therapy. Medical nutrition therapy has been covered under Medicare Part B since 2002. It provides services to people who meet one of three conditions—diabetes, kidney disease, or have had a kidney transplant in the past 36 months. There is a bill in Congress to expand coverage under Medicare to people with prediabetes and risk factors for type 2 diabetes.
2015 White House Conference on Aging.1 This conference, which was held on July 13, 2015, was the sixth ever held and the second in the 21st century. It was held in a year that marked important anniversaries for Social Security (80 years); Medicare, Medicaid, OAA, Voting Rights Act (50 years), the Americans with Disabilities Act (25 years) and the ACA (5 years). It focused on four topics, two of which have a direct bearing on nutrition and older adults: Healthy aging, and long-term services and supports. As defined by the White House conference, healthy aging is living a long, productive, and meaningful life and enjoying a high quality of life. The conference issued a policy background paper, which had one paragraph on nutrition that cited existing programs and resources and referred to the importance of healthy diet to disease prevention. In the long-term services and support section, the conference defined these services as health and social services that may be needed to maximize the independence and well-being of an individual. Other relevant announcements from the conference included
- A new proposed rule from the U.S. Department of Agriculture (USDA) to increase accessibility to critical nutrition for homebound, older Americans and people with disabilities by allowing government and nonprofit food purchasing and food delivery services to become authorized SNAP retailers which enables these
___________________
1 More information on the White House Conference on Aging can be found at http://archive.whitehouseconferenceonaging.gov (accessed May 23, 2016).
-
services to accept SNAP benefits as payment for home-delivered meals.
- Peapod has adopted “best in class” web accessibility standards to ensure that all individuals, including those with disabilities and those who are unable to shop at traditional stores, can use its website and mobile applications.
- The National Prevention Council announced that in the spring of 2016, it will release a Healthy Aging Action Plan to advance the National Prevention Strategy and will identify federal action steps to promote prevention and well-being among older Americans.
Blancato noted that next steps following from the White House conference depend on the release of the final report and its ability to provide a roadmap for action. He went on to say that the responsibility for advocacy now is to see that the items laid out in the report are acted on and that any rules, regulations, and policies are adopted. Some had timetables attached and that is a good thing, Blancato added. New legislation may also follow.
Opportunities for Promoting Healthy Aging
Blancato concluded his talk by saying that actions to promote healthy aging must focus on the triple threat to older adults: hunger, food insecurity, and malnutrition. Many of the potential solutions to these problems are the same (e.g., increasing SNAP enrollment and participation in OAA programs), but some differ. Malnutrition is an area of new focus, and Blancato cited a recent study that estimated the annual burden of disease-related malnutrition in the community across eight diseases was $156.7 billion (Snider et al., 2014). Patients who are malnourished are more likely to experience complications, such as pneumonia, pressure ulcers, infections, and death. Malnourished older adults also are at greater risk of fall, longer hospital stays, worse outcomes after surgery or trauma, and self-neglect. Blancato proposed several potential solutions:
- Make malnutrition a key indicator of older adult health.
- Re-examine older adult goals of Healthy People 2020 and build in a stronger emphasis on malnutrition identification, prevention, and intervention.
- Address protein-related malnutrition in national and state obesity plans.
- Re-examine the protein requirements of older adults and consider the need for an increased protein DRI for older adults.
- Expand electronic medical records to include a standardized section on malnutrition.
- Include malnutrition screening and intervention in the essential benefits covered in the Medicare annual exam.
- Include coverage for oral nutrition supplements for malnourished and at-risk dual-eligible populations.
- Collect and analyze Medicare and Medicaid data to improve outcomes with malnutrition screening and intervention.
- Expand medical nutrition therapy coverage to include malnutrition.
Blancato noted that a new coalition—Defeat Malnutrition Today—has been formed to position malnutrition as a key indicator and vital sign of older adult health and to advocate for legislative and regulatory change.
Blancato then addressed questions about the competing priorities of nutrition and older adults versus nutrition and children. He stated that the real need is to improve the federal commitment to all people of all ages and for policies to promote good nutrition and nutrition education throughout the lifespan. Blancato stated that policy directions should focus on the intergenerational bases where better outreach and access to programs can be emphasized. Advocates for older adults can learn a lot about doing better advocacy by working with colleagues in the children’s world.
Blancato ended his talk by suggesting the need to create a greater political imperative for nutrition. More outreach and enrollment in SNAP and increased funding levels for the other programs may be necessary. He also proposed that efforts be undertaken to discover how much OAA programs have saved for the programs like Medicaid and Medicare.
USDA NUTRITION PROGRAMS FOR THE OLDER POPULATION
This presentation featured two speakers: Lura Barber, Director of Hunger Initiatives at the National Council on Aging (NCOA), and Kathryn Law of the USDA Food and Nutrition Service. Both spoke about the USDA’s nutrition programs for older adults.
SNAP for Older Adults: Opportunities for Improvement
Barber began her talk by explaining that NCOA is an advocacy organization based in Washington, DC, whose mission is to improve the lives of older adults, especially those who are struggling. The NCOA works with low-income adults in the community ages 60 and older on programs such as chronic disease self-management, falls prevention, and economic security. It does its work in partnership with a national network of organizations, intentionally including those working in aging and in other fields as well. Barber noted that she would focus her remarks on results from the first 2 years of a SNAP enrollment initiative for older adults that grew out of
earlier work on benefits access. The work has been supported by grants from the U.S. Department of Health and Human Services’ Administration for Community Living and, currently, from the Walmart Foundation. Barber provided some statistics about older adults, food insecurity, and SNAP participation (see Box 4-1).
Barber noted that it is important to look at the big picture and create a balanced approach to the food security question, where SNAP is one key public benefit working synergistically with other benefit programs (see Figure 4-1).
Building on this base, Barber shared some of the best practices that her program saw in the first year of their Senior SNAP enrollment initiative. These best practices cluster around three areas: community-based assistance, social media outreach, and policy work.
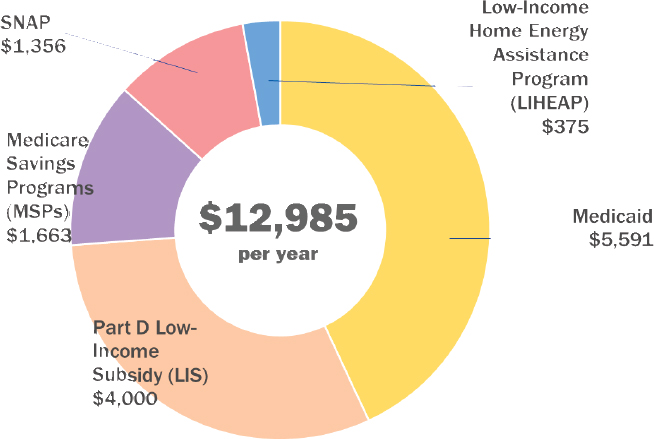
NOTE: SNAP = Supplemental Nutrition Assistance Program.
SOURCE: Presented by Lura Barber on October 28, 2015 (NCOA).
Community-Based Assistance
NCOA has been working on the Senior SNAP enrollment initiative in the field since March 2014. Since the start of the initiative, NCOA has helped almost 200,000 older adults be screened for SNAP and other benefits. Its partners have submitted almost 47,000 SNAP applications on behalf of older adults all over the country. An estimated value of those applications based on general acceptance rates and the value benefits is about $64 million. NCOA anticipates submitting another 15,000 SNAP applications before the grant ends.
Barber noted that NCOA has learned that many different kinds of organizations can be successful in helping older adults in the community. Each type of organization has strengths and challenges, and learning about them and accommodating them helps NCOA work with them successfully (see Figure 4-2).
She then described the six steps NCOA has learned are best practices in helping older adults enroll in SNAP:
- Step 1: Assess your organization’s strengths and challenges.
- Step 2: Understand your target population and your community.
- Step 3: Conduct outreach and education about SNAP and older
- Step 4: Screen clients for benefit eligibility. NCOA has developed a tool called Benefits Checkup, which indicated whether a person is eligible for SNAP and for what other benefits the person might be eligible.
- Step 5: Assist in completing and submitting applications.
- Step 6: Follow up to troubleshoot and ensure proper use of the SNAP Electronic Benefits Transfer (EBT) card. Making recertifications easy, which some states succeed at, also is important. Many older adults are on fixed income so, Barber said, there is no rationale for them having to complete this paperwork.
adults. One NCOA partner is Elder Law of Michigan, which uses voter registration data to target eligible people in low-income areas.
Barber noted that a common theme that all of NCOA’s partners must deal with is overcoming the stigma of SNAP participation. The partners have developed a number of powerful approaches to talking about SNAP that reduce stigma. For example, they explain that participating in those programs is just “claiming what you earn” because older adults have paid taxes that fund programs like Social Security and SNAP. Another is to frame SNAP as a health care benefit. In rural areas, emphasizing that SNAP is a USDA program that helps local farmers and business has been particularly effective.
Barber also explained that building relationships and developing partnerships with state agencies, other community-based organizations, CSFP distributors, community organizing groups, domestic care workers, hospi-
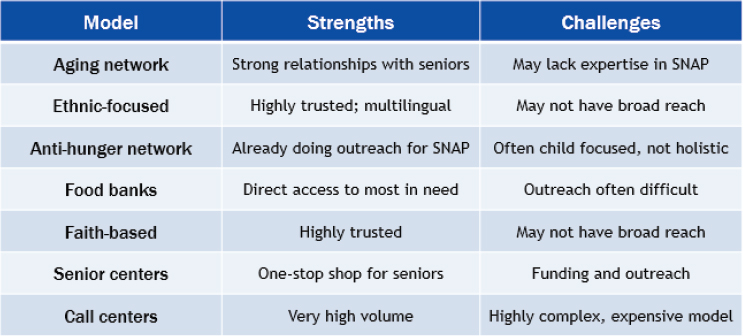
NOTE: SNAP = Supplemental Nutrition Assistance Program.
SOURCE: Presented by Lura Barber on October 28, 2015 (NCOA).
tals and other medical providers, and local businesses makes it much easier to improve outreach efforts.
Social Media Outreach
Barber stated that the conventional wisdom is that older adults are not on the Internet but that is not true. In fact, three in five older adults ages 65 and older are online, 71 percent of older adult Internet users go online every day or almost every day, and 46 percent of older adult Internet users are on social networking sites, such as Facebook (Pew Research Center, 2014).
Social media can be a powerful way to reach older adults who are isolated or who have issues with mobility. For example, NCOA has had significant success with Facebook. Social media outreach gets results quickly.
Public Policy Initiatives
Because SNAP is administered at the state level, much of NCOA’s policy work focuses on the state. Barber noted that one of its most effective efforts is to expand implementation of the Elderly Simplified Application Project, a USDA demonstration project that seeks to increase SNAP participation among the elderly low-income population by streamlining the application and certification process. Another is implementing a standard medical deduction from their income if they can demonstrate at least $35 per month in unreimbursed out-of-pocket medical expenses. This deduction relieves older adults and state agency caseworkers of the time-consuming task of itemizing their medical expenses, and can help seniors qualify for a larger benefit amount (Jones, 2014).
NCOA also has pursued other policy options to streamline SNAP eligibility, such as partnering with aging organizations in state SNAP Outreach Plans, instituting broad-based categorical eligibility, setting up state call centers for application assistance, extending recertification periods, simplifying and combining applications for multiple benefits, instituting an online application, and creating a data bridge that allows counselors to track and flag their clients’ applications.
USDA Nutrition Programs for Older Adults
Kathryn Law briefly described a few of the USDA nutrition programs that support the nutritional needs of older adults.
CSFP. This program provides low-income older adults with food packages containing a variety of foods that are good sources of nutrients that are often low in older adults’ diets. CSFP operates in 46 states, the District
of Columbia, and 2 Indian reservations. About 573,000 individuals participated in the CSFP in each month in fiscal year (FY) 2014.
SFMNP. This program provides low-income older adults with coupons for eligible foods at farmers’ markets, roadside stands, and community supported agriculture baskets. The SFMNP operates in 43 states, the District of Columbia, and 7 Indian reservations, and served about 790,000 individuals in FY2014.
Child and Adult Care Food Program (CACFP). This program reimburses centers that provide day services to older adults to help them serve nutritious meals. CACFP operates in all states and the District of Columbia, and about 120,000 adults participated each day in FY2014.
Food Distribution Program on Indian Reservations (FDPIR). This program provides food to low-income households, including older adults, living on Indian reservations, and to Native American families residing in designated areas near reservations and in Oklahoma. The FDPIR is operated by tribes and states and served about 85,000 individuals each month in FY2014.
SNAP
Law then provided a more detailed discussion of SNAP, the USDA’s largest nutrition assistance program. This $70 billion program is the first line of defense against hunger for low-income people. As a mandatory entitlement, SNAP can grow as the demand or need for the program grows. The program serves about 4.6 million older adults; that is slightly less than 10 percent of SNAP participants but receive 7.5 percent of the benefits. Slightly more than 17 percent of households that receive SNAP contain a member age 60 or older.
For the past 30 years, the USDA has used census data to estimate how many people are eligible for the program and has used its own SNAP program data to determine how many are actually receiving benefits. These data show that, over the past 20 years, SNAP participation among older adults has been about half of the overall participation rate (see Figure 4-3).
Data also show that SNAP participation among eligible older adults varies widely by state (see Figure 4-4).
In regard to their characteristics, 73 percent of older adult participants live alone and 64 percent are female. Average gross income is 86 percent of the poverty line compared to 59 percent of the poverty line for all SNAP households.
Law then asked, “And what about the 60 percent of eligible older adults who are not participating in SNAP? What do we know about them?” She noted that they are generally similar to older adults who receive SNAP, but there are some differences. For example, nonparticipating older adults
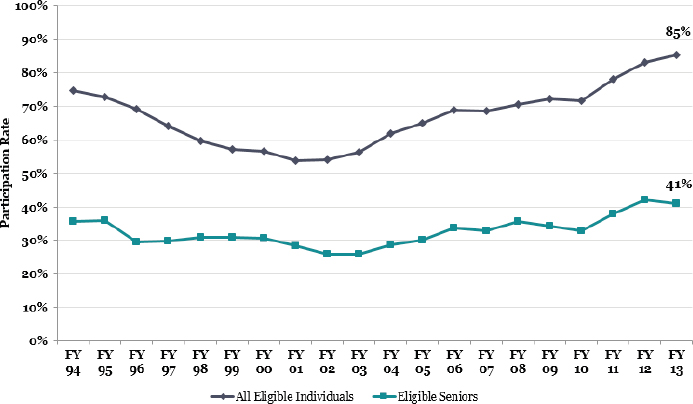
NOTE: FY = fiscal year.
SOURCE: Presented by Kathryn Law on October 28, 2015 (USDA, Food and Nutrition Service).
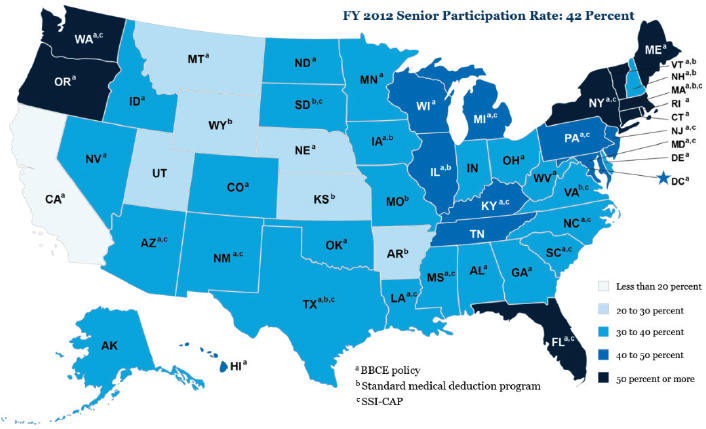
NOTE: BBCE = broad-based categorical eligibility; SSI-CAP = Supplemental Security Income Cap.
SOURCE: Presented by Kathryn Law on October 28, 2015 (USDA, Food and Nutrition Service).
are eligible for a lower benefit. Also, some older adults are eligible for a large SNAP benefit, but they are still not benefiting from the program. Law noted that research on the reasons for nonparticipation by eligible older adults suggests multiple causes, such as lack of knowledge about their eligibility, unfamiliarity with the application process, a desire for personal independence, the perceived cost of applying and participating, the low benefit expected, and the stigma associated with program participation.
Law also reported on a series of pilot tests that the USDA has conducted to increase SNAP participation among older adults (see Box 4-2). These tests had positive but small effects. She also described several other efforts to encourage SNAP participation that are currently ongoing in a variety of states (see Box 4-3).
Law then mentioned several initiatives included in the 2014 Farm Bill. For example, it allows home delivery services to accept SNAP benefits if the services are intended for older adult and disabled participants. In its FY2016 budget request, the USDA also has asked to expand its Elderly Simplified Application Projects. This authority would reduce the requirements that states must meet in order to implement Elderly Simplified Applications.
In concluding, Law stated that some actions show promise in getting more older adults to participate in SNAP, including one-on-one application assistance, using a simplified site application that reduces verification requirements, and waiving the face-to-face interview in SNAP offices. Ways to overcome other barriers to participation are still unknown, however. It may be that some eligible older adults may never choose to participate, and therefore it is unlikely that the USDA can ever completely close the participation rate gap, Law concluded.
NUTRITION DURING CARE TRANSITION
In her opening remarks, Rose Ann DiMaria-Ghalili, Associate Professor of Doctoral Nursing and Nutrition Science at Drexel University’s College of Nursing and Health Professions, stated that her research has focused on malnutrition in older adults, particularly in older adults who are undergo-
ing surgery. She has been interested in looking at risk factors before people come into the hospital, what happens while they are in the hospital, and most importantly, what happens when they are sent home to recover.
DiMaria-Ghalili framed her presentation by highlighting the lack of a systematic approach to managing care transitions and the inconsistent involvements of registered dietitians during care transitions. She illustrated the need for better care transition by showing a news story of an older man recently discharged from the hospital who called 911 because he could not obtain food. Describing the lesson learned from this episode, DiMaria-Ghalili stated that translating nutrition guidance into patient care practice is critical in moving nutrition from a “support service” to a critical health intervention. She cited a recent statement from the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.): “It is the position of A.S.P.E.N. that addressing disease-related malnutrition in hospitalized patients should be a national goal in the United States and thereby help to improve patient outcomes by reducing morbidity, mortality, and costs. A malnutrition-focused national goal would better overtly address the issue of disease-related malnutrition to alert healthcare organizations on the need to provide optimum nutrition care” (Guenter et al., 2015).
Facts About Hospital Malnutrition
As a backdrop to her discussion of care transitions, DiMaria-Ghalili provided several facts related to hospital malnutrition derived from large data sets collected during health care utilization projects (Allaudeen et al, 2011; Corkins et al, 2014; DiMaria et al., 2014; Kassin et al., 2012; Krumholz, 2013):
- Patients coded for malnutrition tend to be age 65 and older, have higher infection rates, longer lengths of stay, higher costs, and higher rates of death.
- Older adults with a malnutrition diagnosis are more likely to be admitted to the hospital from a skilled nursing facility, and more likely to be discharged to a skilled nursing facility.
- Weight loss increased risk of 30-day readmission in medical patients.
- Failure to thrive and malnutrition are frequent reason for readmission in surgical patients.
- Malnutrition and Posthospital Syndrome is “an acquired, transient period of vulnerability” (Krumholz, 2013).
Currently, The Joint Commission, an independent nonprofit that accredits and certifies health care organizations and programs in the United
States, requires that older patients be screened for malnutrition within 24 hours of admission to the hospital, but a second malnutrition screen is not required before discharge, DiMaria-Ghalili stated, which is important in care transition. Her logic for this contention is that older adults are at risk of malnutrition, that malnutrition affects readmission, and that transitional care can influence hospital readmission rates.
Evidence to Support Nutrition During Care Transitions
The ACA gave the Centers for Medicare & Medicaid Services (CMS) the authority to create several Health Care Innovation Awards programs. The first round of awards, worth up to $1 billion, went to 107 projects throughout the United States. DiMaria-Ghalili noted that among the 21 projects targeted at reducing hospital admission rates, nutrition during care transition was not a primary focus (https://innovation.cms.gov/initiatives/ Health-Care-Innovation-Awards [accessed May 9, 2016]).
She pointed out the following strengths and weaknesses of the nutrition components:
- Strengths: Nurses played a primary role in transitional care. Most of the programs had an interdisciplinary team, and included predictive analytics to identify eligibility for services and levels of intervention intensity. These hospital-based models had the potential to be sustainable upon completion and transitions to skilled nursing facilities were examined.
- Weaknesses: The roles of various people on the transitional care teams were not clearly delineated. Nutrition was not fully integrated into the programs. Dietitians were missing from the teams. Most of the sites reported problems with integrating the electronic health records or data across sites and across different settings as well as issues with data use agreements.
A search for other federal and local programs that have focused on nutrition during care transition revealed one ongoing randomized clinical trial funded by the NIA. The study is examining the safety and efficacy of the Dietary Approaches to Stop Hypertension (DASH) diet given for 4 weeks to 50 older adults who had been discharged after a diagnosis of acute decompensated heart failure. DiMaria-Ghalili stated that the findings of this trial will make a significant difference in transitions of care, especially when targeting certain disease states. She also found a variety of other hospital-based programs with widely different components, from sending patients home with food packs to home-delivered meals.
Possible Research and Policy Priorities
DiMaria-Ghalili concluded her talk by suggesting several research and policy priorities:
Potential research priorities
- Integrate nutritional risk assessment into predictive models to determine levels of intensity of nutritional care after discharge:
- High-risk: intervention delivered by dietitian
- Medium-risk: intervention delivered by nurses
- Low-risk: intervention delivered by social worker or lay health worker
- Conduct a secondary analysis of nutrition risk data from Health Care Innovation Awards recipients to develop nutrition risk predictive models based on readmissions, transitional care needs, and chronic care needs.
- Identify and review programs instituted by hospitals to address nutrition needs after discharge. Determine common elements, program costs, cost savings, sustainability, and patient outcomes.
Potential health policy priorities
- Expand reimbursement for registered dietitians beyond diabetes and chronic kidney disease to also include heart failure as these patients are at risk of malnutrition and dietary modifications may play an important role in symptom management of heart failure.
- Incorporate nutrition risk screen and assessment upon hospital discharge and identify ways to incorporate nutrition into transitional care programs.
CHALLENGES AND INITIATIVES IN AMERICAN INDIAN RESERVATIONS
Kibbe Conti, Supervisory Dietitian at the Rapid City Indian Hospital, focused her talk on challenges and initiatives in American Indian reservations of the Lakota tribe, which is part of the great Sioux Nation in South Dakota.
As background, Conti noted that geography often defines foodways. Looking at a map of North America, she explained that the nations she works with are located in the middle of the Great Plains, called the grasslands. Even though the Lakota are different than Crow, which are different than Cheyenne, all the Northern Plains tribes have a similar foodway.
Conti works primarily with the groups who belong to the Cheyenne River Sioux tribe. Their reservation, which covers the two counties of
Ziebach and Dewey, is quite large—3 million acres—but the population density is quite sparse—one to two people per square mile. The poverty rate is 33 percent to 40 percent, depending on the county, median household income is about $32,000, the typical household size is 3.5 persons per house, and 6 percent to 10 percent of the population is age 65 and older. More than 70 percent of the population in the two counties is Native American.
One of the greatest assets in Indian Country is the elders, stated Conti. They carry on the traditions, maintain the language, and are the keepers of wisdom. They are truly valued. However, elders face a number of health challenges, including lower life expectancy (e.g., age 54 for males), higher rates of illness at younger ages, lack of long-term care services, lack of transportation (e.g., a round trip to the grocery store can easily be 60 miles), and lack of built environmental features (e.g., sidewalks, community centers).
Health disparities also are a significant concern, with Native American people experiencing an epidemic of diabetes, as well as high rates of obesity, cancer, cardiovascular disease, chronic kidney disease, and alcoholism. Food insecurity also is very high at 23 percent. Nearly 25 percent of Native households participated in SNAP and 20 percent of older adults receive Supplemental Security Income (SSI) payments.
Conti noted that she works in an urban clinic, which has fewer resources than are available on the reservations. To compensate, people living in the urban areas can access food pantries and the Indian Health Service (IHS) allows doctors to prescribe food supplements to older malnourished adults. “Diets of poverty” are also common. Conti explained that this term describes high-fat, high-carbohydrate, low nutrient diets.
Food Distribution Programs Used by the Cheyenne River Sioux
In the Cheyenne River Sioux communities where Conti works, the FDPIR, until recently, had higher participation rates than SNAP, but that is no longer true. She noted, however, that the FDPIR has greatly improved in recent years and now features updated warehouses, walk-in refrigeration units, and freezers. Good quantities of fresh produce and frozen meat are available and the program provides a large food package. She noted that many of the families that do choose commodities through FDPIR do so because they feel they get a greater amount of food from that program. In addition to SNAP and FDPIR, the CSFP also is popular among the urban Indian population. Furthermore, the Title VI meal programs, and to a lesser extent the Title III meal program also are vital to the Cheyenne River Sioux communities; both programs are under the OAA. The tribe has increased the supplemental funding it provides to the Title VI program to ensure its continued stability.
Conti then described a variety of partnerships that have emerged to care for tribal elders. The Pine Ridge area has a senior living center on the reservation funded through Title VI. Tribal members serve as community health representatives. These health paraprofessionals act as cultural liaisons between the IHS doctors and their patients. Public health nurses and public health nutritionists also play a critical role, said Conti. Another initiative is the Elder Care Initiative, which the IHS began in 2008. This program provides funding to help tribes launch their own long-term care initiatives. Other valuable partners, stated Conti, are the various diabetes programs, some of which have fitness programs and facilities.
The Native Food Sovereignty Movement
Conti closed her presentation by describing the exciting Native food sovereignty movement, which is gaining strength among the Indian tribes. This movement aims to eliminate food insecurity in Indian Country by strengthening food production and reclaiming and restoring former Native food systems. The idea behind the movement is that control over the Native food system helps promote the tribal Nations’ economies and people. Conti showed how the movement has adapted traditional food paradigms to the contemporary food system (see Figures 4-5 and 4-6).
In the traditional version, the West direction is associated with water. Rain comes out of the Western direction and provides things to drink, such as water and tea (i.e., tea is simply water with an herb). The North direction holds the symbol of the buffalo. Buffalo provide quality protein and fatty acids. The East direction holds the symbol of Springtime. That is the time when everything begins to emerge from the earth and the gathering season begins. The South is associated with summertime efforts to cultivate crops such as corn, beans, squash, and potato, which reflect traditional Native agriculture. Creating the new paradigm is a way to honor the four things that Native peoples did so well, and to apply it to a contemporary context that allows people to choose a healthy drink, good sources of protein, a fruit or a vegetable, and a starchy vegetable or grain. This new paradigm is similar to the My Native Plate that was developed in 2002. Conti noted that the Native Food Sovereignty Movement provides an important opportunity for youth to partner with elders. The elders have the knowledge about traditional foods and the youth can adapt this knowledge to the foods commonly available today.
Conti closed her talk by stating the need to expand wellness initiatives in Native communities, provide more nutrition screening of elders and more assessments in meals centers. These types of initiatives could help to identify those at greatest risk and direct them to available resources. She also suggested that nutrition education and counseling should be more available.
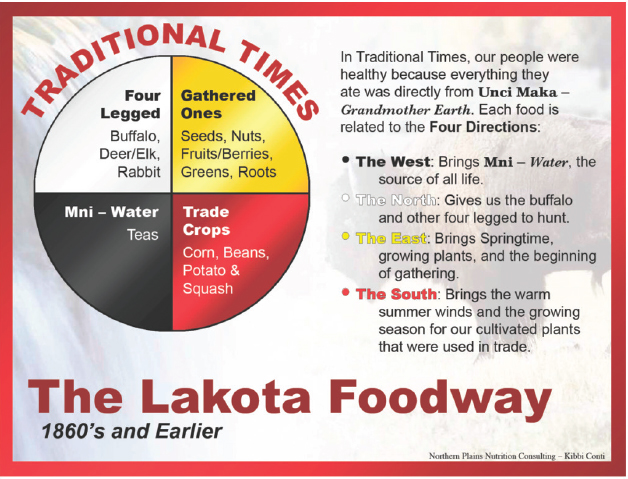
SOURCE: Presented by Kibbe Conti on October 28, 2015 (Northern Plains Nutrition Counseling).
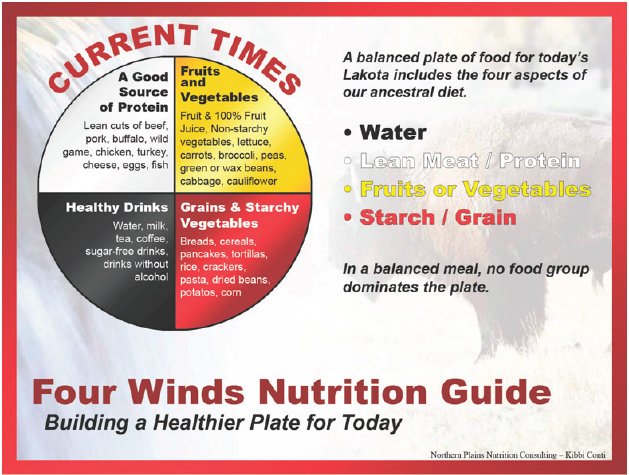
SOURCE: Presented by Kibbe Conti on October 28, 2015 (Northern Plains Nutrition Counseling).
Moreover, Conti urged efforts to fill knowledge gaps, as very little research is conducted among Native Americans and elders. Her concluding thought was that attention to improving access to healthy foods is increasing, and this is leading to expansion of local food harvesting and production in some communities. The benefits of traditional foods as a means to restore health is now widely accepted by Native people as the way to restore health to Native Nations.
QUESTION AND ANSWER SESSION
Following the Session 4 presentations, the floor was opened for questions and general discussion. Joining the panel for this session was Jean Lloyd, formerly a national nutritionist with the U.S. Administration on Aging (AoA).
The first question dealt with whether panelists were aware of CMS’s Center for Medicare & Medicaid Innovation program on chronic diseases in which seven states are conducting pilot programs to determine how Medicare can improve chronic care management. The questioner was interested in whether the panelists thought that nutrition should be one of the issues covered in the program. Panelists strongly agreed that nutrition should be a vibrant element of these pilot tests. Lloyd noted that an element often missing is the critical connection between nutrition and health in transition care. Most of the transition care grants did not include nutrition because nutrition was not a part of the evidence-based models on which the program was based and in addition, DiMaria-Ghalili said, the grant reviewers did not have a strong nutrition background. Advocating for inclusion of this area of expertise on grant review panels may be necessary.
A second participant noted that the funding for the OAA relative to the number of older Americans in the United States is decreasing and asked Lloyd whether she was aware of any activities by states to use their own Medicare and Medicaid funds to increase the number of meals per week that older adults receive through meals programs. Lloyd pointed that in 1990, funding was about $25 per capita and now it is $12. The programs always have accessed other sources of funds. Under Medicaid waiver programs,2 46 states include some meal services but those services vary. Some states say that older adults first must be served by programs under the OAA and if that is not possible, then they will be served under the Medicaid waiver program. Another issue is trying to get funding from other private sources. Under some grants, healthy aging services networks
___________________
2 Medicaid waiver programs are designed to provide services to keep people who are at a nursing home level of care out of nursing homes and in their homes. Under those programs, meals are an optional, not a required, service.
are trying to have managed care insurance companies pay for services such as meals and nutrition education.
Conti responded to a question about lessons from the food sovereignty movement by describing the White Earth program, in which tribes put lands that they recover legally back into food production and have paid for people who harvest using traditional methods to harvest crops such as maple syrup and corn. She continued by saying that, in fact, all the tribes are engaged at some level in food sovereignty efforts using the food ways and key foods of their specific regions, such as buffalo for South Dakota.
Lloyd added that the 2014 Farm Bill included a requirement to allow traditional foods to be used in senior programs, assisted living, nursing homes, and schools on tribal reservations and in Alaskan villages. In addition, the Alaska Native Tribal Health Consortium is developing a model program in which public health is working with traditional hunters and others to serve those foods in nursing homes. A traditional foods conference was held in Albuquerque in October 2015 and participants discussed these issues for Indian country across the nation.
Another participant noted that some presenters asked for clarification in regard to malnutrition and food insecurity outcomes in their screening measures and tools. She also endorsed an increase in funding and asked whether any cuts in Social Security or Medicare would require a greater need for funding from other programs that had been mentioned. Blancato responded that the increase for home-delivered and congregate meals was in a prior appropriation bill. If the current budget is passed, $40 billion in additional funding for nondefense discretionary programs will be available for the next 2 years. After passage, the budget goes to the Appropriations Committees, where attempts can be made to try to get the funding levels raised. The president has put forward a budget for nutrition programs that would increase the funding by $60 million. Organizations will advocate for the highest funding level possible, but that would not be possible without the budget caps being lifted first. On the Social Security side, he continued, the only major change in the budget so far has to do with the disability insurance program to protect it from going into a negative financial situation. He stated that the issue most seniors are concerned about is that about 30 percent of older adults were going to face a 52 percent increase in their Medicare Part B premium on January 1. This group includes dual eligibles, very wealthy Medicare beneficiaries, and those who are on Medicare but not on Social Security. Beneficiaries will pay more for their Part B premium but not as much as was projected.
DiMaria-Ghalili responded to the question about screening tools, noting that it depends on what is being measured. She suggested that a new tool might be needed to screen for risk of malnutrition—not a new tool for use on admission but one what would cover the social and economic issues
that need to be considered when hospitals are ready to send people home. She further stated that existing tools need to be revamped to make sure that hospitals incorporate a holistic approach to screening upon discharge.
REFERENCES
Allaudeen, N., A. Vidyarthi, J. Maselli, and A. Auerbach. 2011. Redefining readmission risk factors for general medicine patients. Journal of Hospital Medicine 6(2):54-60.
Coleman-Jensen, A., M. P. Rabbitt, C. Gregory, and A. Singh. 2015. Household food security in the United States in 2014. Economic Research Report No. ERR-194. Washington, DC: U.S. Department of Agriculture, Economic Research Service.
Corkins, M. R., P. Guenter, R. A. DiMaria-Ghalili, G. L. Jensen, A. Malone, S. Miller, V. Patel, S. Plogsted, H. E. Resnick, and the American Society for Parenteral and Enteral Nutrition. 2014. Malnutrition diagnoses in hospitalized patients: United States, 2010. Journal of Parenteral and Enteral Nutrition 38(2):186-195.
Cubanski, J., C. Swoope, A. Damico, and T. Neuman. 2014. How much is enough? Out-of-pocket spending among Medicare beneficiaries: A chartbook. Washington, DC: Kaiser Family Foundation.
DiMaria-Ghalili, R. A., J. Slaughter, E. Gonzalez, P. Abeysekara, H. Resnick, and P. Guenter. 2014. A comparison of characteristics by age of hospitalized adults with a diagnosis of malnutrition: United States, 2010. The Gerontologist 54(Suppl. 2):692.
Guenter, P., G. Jensen, V. Patel, S. Miller, K. M. Mogensen, A. Malone, M. Corkins, C. Hamilton, and R. A. DiMaria-Ghalili. 2015. Addressing disease-related malnutrition in hospitalized patients: A call for a national goal. Joint Commission Journal on Quality & Patient Safety 41(10):469-473.
Jones, T. 2014. SNAP’s excess medical expense deduction: Targeting food assistance to low-income seniors and individuals with disabilities. Washington, DC: Center for Budget and Policy Priorities.
Kassin, M. T., R. M. Owen, S. D. Perez, I. Leeds, J. C. Cox, K. Schnier, V. Sadiraj, and J. F. Sweeney. 2012. Risk factors for 30-day hospital readmission among general surgery patients. Journal of the American College of Surgery 215(3):322-330.
Krumholz, H. M. 2013. Post-hospital syndrome—an acquired, transient condition of generalized risk. New England Journal of Medicine 368(2):100-102.
NCOA (National Council on Aging). 2015. Older adults & debt: Trends, trade-offs, and tools to help. Arlington, VA: National Council on Aging.
Pew Research Center. 2014. Older adults and technology use: Usage and adoption. http://www.pewinternet.org/2014/04/03/usage-and-adoption/#46-of-online-seniors-use-social-networking-sites-but-just-6-use-twitter (accessed February 12, 2016).
Snider, J. T., M. T. Linthicum, Y. Wu, C. LaVallee, D. N. Lakdawalla, R. Hegazi, and L. Matarese. 2014. Economic burden of community-based disease-associated malnutrition in the United States. Journal of Parenteral and Enteral Nutrition 38(2 Suppl):77S-85S.






















