5
Treatments, Technologies, and Interventions Affecting Function After Transplantation
Transplantation is a complex procedure that requires sophisticated technology, advanced surgical and medical expertise, and specialized care management. Session 4 of the workshop focused on the medical and supportive interventions patients may need to mitigate or treat possible organ rejection or failure, infections, illness, and impaired function. Speakers described the pharmacologic treatments and their side effects following transplantation and described the standard and emerging practices to support and improve health and functioning, including prehabilitation, posttransplant rehabilitation, and palliative care. The last section highlights the panel discussion, including salient questions asked by attendees from SSA, and suggestions from individual speakers for taking these approaches to the next level.
PRETRANSPLANT CARE MANAGEMENT
Mara McAdams-DeMarco, director of clinical and outcomes research at JHU, described the negative outcomes impacted by pretransplant impairments. For example, mortality and graft loss risk are elevated when patients have pretransplant conditions, such as frailty, walking or cognitive impairments, obesity, or unintentional weight loss. She explained that among kidney recipients, those who had a walking impairment prior to transplantation were found to have a mortality rate three times higher than
those who did not (Thomas et al., 2020). For this population, intervening prior to transplantation—often referred to as prehabilitation—is a way of increasing the probability of successful transplantation. Surgery is a significant physiologic stressor, causing changes in the body, such as stress hormone production and increased inflammation, and can be comparable to intense exercise. McAdams-DeMarco said prehabilitation interventions are designed to enhance the functional capacity to tolerate the stress of surgery and will typically include exercise components and sometimes nutritional or psychological components. This approach allows the care team to shift the focus to optimization prior to surgery instead of rehabilitation afterward, she said. Transplantation represents an ideal setting for this approach, she added, because people often wait long periods for a transplant and during this time suffer from aging, frailty, or other comorbidities. McAdams-DeMarco presented a conceptual model of prehabilitation where multiple components are brought together with a goal of improving long-term outcomes (see Figure 5-1).
McAdams-DeMarco explained that candidates may be more motivated to start a new program before transplantation. Because patients often experience a variety of other challenges following the procedure, they may find it easier to modify their daily routine prior to the transplant. She added that many patients have prolonged recovery and may be rehospitalized in
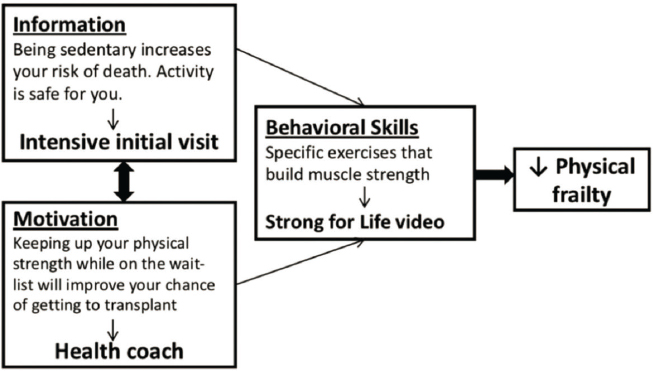
SOURCES: Mara McAdams-DeMarco presentation, March 23, 2021; Lai et al., 2021.
the early postoperative period, so this is difficult time to try new things—especially activities that add stress to the body.
A prehabilitation program such as this can have several different types of interventions or approaches. McAdams-DeMarco shared several examples across different organ types. For lung transplant candidates, pulmonary prehabilitation is the most common. She summarized different studies looking at this intervention and noted that while duration and exercise type differed by study, all studies reported improved exercise capacity and QOL following the interventions (Florian et al., 2013; Li et al., 2013). Other studies of lung transplant candidates looked at home-based prehabilitation using mobile technology, which also allows patients to track their progress. Others have examined home-based exercise and saw improvements in 6-minute walk distance for more than one-quarter of participants. This intervention was associated with improved posttransplant outcomes, including less time on mechanical ventilation and reduced length of hospital and ICU stay (Massierer et al., 2020). McAdams-DeMarco reported that some studies in liver transplant candidates found smartphone apps to be effective in increasing physical performance, while other studies have demonstrated home-based programs focusing on exercise and strength training were safe and improved QOL. She described her own study of prehabilitation for kidney transplants: 40-minute therapy sessions with a goal of tailoring the program to improve physical functioning by performing cardiovascular exercises (McAdams-DeMarco et al., 2019). Patients noted in feedback that 100 percent were very satisfied with the prehabilitation and overall were very positive, saying that it helped them to sustain endurance, maintain better weight control, and even improve their attitude coming into transplantation. She shared data showing a 64 percent improvement in physical activity over 2 months. Only five candidates went on to receive their transplant during the study, but McAdams-DeMarco noted that their hospital length of stay was reduced by 5 days (McAdams-DeMarco et al., 2019).
In conclusion, McAdams-DeMarco highlighted the knowledge gaps regarding pretransplant interventions. She said that while the pretransplant period is an ideal window to recruit patients into efforts to modify their behavior that will benefit overall health following transplantation, the challenge is that there are only two studies of transplant candidates (lung and kidney, respectively) showing that prehabilitation can affect posttransplant outcomes. She described a need for future research to identify the optimal transplant patient population, define a standard prehabilitation program, identify optimal timing and duration of interventions, and quantify costs.
Answering these questions will help to answer whether prehabilitation improves pre- and posttransplant outcomes and prevents impairments that can lead to disability, McAdams-DeMarco said.
PHARMACOLOGIC TREATMENTS AFTER TRANSPLANTATION
Solid organ transplantation is major surgery with a variable length of recovery and duration of inpatient stay, said Saeed Mohammad, medical director of pediatric hepatology and liver transplantation at the Northwestern University Feinberg School of Medicine. At discharge, transplant patients may be taking more than 10 medications; their number and nature can make recovery more or less difficult and affect physical, emotional, cognitive, and social functioning. In assessments of functioning, it is important to compare functioning to previous ability as well as healthy controls. Mohammad cited various methods of measurement, including questionnaires, active methods, such as treadmills, or observer measures, such as interviews by trained personnel or parental observation. Finally, imaging methods exist, such as functional MRI to measure how the brain uses energy when participating in a certain task and computed tomography scans to measure muscle mass.
In the short term, or the first 3 months after transplantation, a number of different medications may affect functioning, he said. Narcotics used for pain relief can lead to decreased physical and cognitive functioning. Patients are also often on antibiotics or antiviral medications, which can cause nausea and diarrhea. Transplant recipients need to take immunosuppressive medications for life to prevent organ rejection, but these medications can often cause neurological symptoms that may affect physical and cognitive functioning. Tacrolimus is the most commonly used immunosuppressive medication, Mohammad explained. Tacrolimus can cause tremors, dizziness, anemia, or insomnia. Longer-term effects may include diabetes and cardiovascular disease, which can both affect neurological functioning.
Mohammad presented a study looking at changes in body composition after liver transplant comparing two different medications. Patients on cyclosporine had an increase in lean muscle mass and more significant decrease in fat index compared to patients on tacrolimus, showing that different medications can affect body composition in unique ways, which can lead to long-term effects (Brito-Costa et al., 2016). Pflugrad et al. (2020) examine cognitive functioning, comparing kidney recipients assessed at 1,
5, and 10 years after transplantation to liver recipients and healthy controls. All transplant recipients scored lower than healthy controls across the measured domains: immediate memory, visuospatial/constructional, language, attention, and delayed memory (see Figure 5-2). He noted that language and delayed memory domains remained the most normal.
Corticosteroids are another class of medications used in transplants for a long time. They can cause weight gain, mood disturbances, and bone demineralization, which can affect long-term physical functioning. Mycophenolate is a widely used antimetabolite medication to prevent organ rejection. However, Mohammad explained that it can cause abdominal pain, nausea, diarrhea, and anemia. He presented a study where patients were taking mycophenolate, but one group of patients were given a different form (an enteric-coated formulation) that resulted in less nausea and less abdominal pain. While it was a small study, he showed that many of the functioning measures all improved in 8 weeks just by changing the route of administration, demonstrating how small changes in treatment
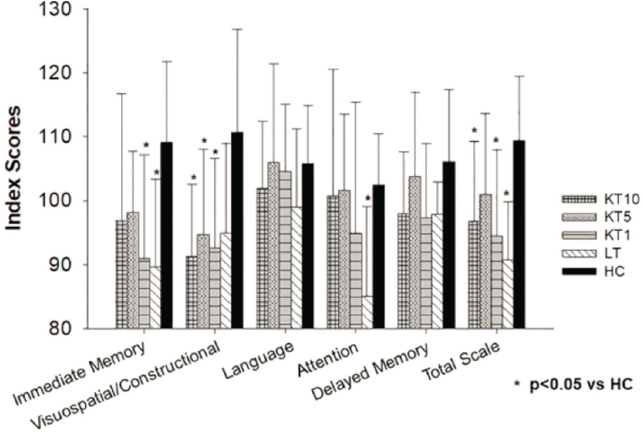
NOTE: HC = healthy control; KT1 = 1 year post-kidney transplantation; KT5 = 5 years post-kidney transplantation; KT10 = 10 years post-kidney transplantation; LT = liver transplantation.
SOURCES: Saeed Mohammad presentation, March 23, 2021; Pflugrad et al., 2020.
regimen can greatly improve functioning (Langone et al., 2011). Finally, because hypertension can affect many patients after transplantation, anti-hypertensive drugs have been known to cause dizziness, headache, constipation, and fatigue.
Mohammad commented on the indirect side effects of these medications. First is the perception of vulnerability, as many patients may feel quite vulnerable following the transplant and may be more likely to limit their physical activity because they are worried about getting hurt. Patients can also feel very dependent on medications and experience stress and anxiety in trying to maintain medication levels and adhere to the right schedule. For children, he said, the physical side effects of weight gain or hair loss can also be difficult to cope with and may lead to bullying, which affects their emotional and social functioning. In conclusion, Mohammad suggested that medications used in transplantation can have unwanted side effects, and these have to be routinely monitored and managed to optimize short- and long-term functioning after transplant surgery.
REHABILITATION AFTER TRANSPLANTATION
Sunita Mathur, associate professor and physical therapist at the University of Toronto, presented on posttransplant rehabilitation. The primary goal of this intervention is not only to increase survival of those with severe organ disease, she said, but also to improve patients’ QOL. Many transplant recipients do not enjoy the full benefits of organ transplantation and are not able to reach their expected level of physical function—which then affects their ability to resume personal or societal roles, such as functioning as a family caregiver or employee. The goals of posttransplant rehabilitation are multifaceted and thus require a multidisciplinary approach. Beyond physical functioning, rehabilitation goals can also include improving treatment adherence, addressing sleep quality, addressing mental health issues, and providing social support, such as a peer network for the recipient and their family. Across all organ groups, Mathur noted that aerobic exercise capacity and muscle strength are reduced for the majority of patients. This is likely caused by the extended periods of bedrest and immobility before and after transplantation. Additionally, early medical complications after transplantation may require hospitalization, which can impact the ability to return to typical daily activities. Given the number of immunosuppressive medications required, as described by Mohammad, numerous long-term effects may cause complications and affect physical functioning.
To address the spectrum of needs that most transplant patients have, which include the need for support with physical functioning, treatment adherence, sleep quality, mental health, and social support, Mathur said the rehabilitation process should occur throughout the continuum of care—from the acute care hospital setting to the early phases after transplantation. Mathur explained that early-phase rehabilitation is the most well described in the literature, especially in terms of exercise training, but there is no set structure for posttransplant rehabilitation overall. Mathur described the rehabilitation approach at the Toronto Lung Transplant Program, where recipients have prehabilitation (as discussed by McAdams-DeMarco) for the duration of their waiting period, and then immediately following the operation, they are actively seen by physical therapists in the ICU for early mobility and exercise to increase functioning and independence. After discharge, there is a mandatory outpatient exercise program for 3 months after transplantation. Patients who are not ready for outpatient programs can be discharged to an inpatient program to address medical needs or functional limitations. After this 3-month period, she described the regular follow-up of patients and ongoing counseling from physical therapists that occurs.
Examining outcomes for these types of programs, Mathur said that most knowledge comes from studies on exercise training. Her team recently published a systematic review and meta-analysis on the effects of exercise training across solid-organ transplant groups. They found great improvements across all organ types seen in aerobic exercise capacity, such as leg muscle strength and QOL, all resulting from regular exercise training (Janaudis-Ferreira et al., 2021). They also found some evidence of improved cardiovascular health and emerging evidence for improvements in mental health outcomes, such as depression and anxiety, but she stressed that more research is needed.
More than just clinical outcomes are important to consider, said Mathur. She shared a study of lung recipients that found those in the exercise program perceived it to be a highly valuable tool to assist them in returning to normal life while providing the motivation and peer support needed to achieve their own desired level of physical performance (Fuller et al., 2014). Mathur highlighted a study her team conducted in which they surveyed solid organ recipients and found that all who attended the rehabilitation program found it beneficial to their health and well-being (Schoo et al., 2017). Several factors were at play, but patients who had poorer health or were experiencing symptoms were less likely to attend the program. While evidence is now established for the needs and benefits of
these rehabilitation programs, she noted the limitations in availability of programs that patients can access.
Mathur called attention to the gaps in current knowledge and potential future directions for research. A multidisciplinary approach to rehabilitation is needed to address the full spectrum of needs beyond exercise training, she said. Greater availability of programs specific to different transplant recipients and greater inquiry into the methods of delivery for these programs are also needed. It can be difficult for hospital-based programs to be the only option for rehabilitation for recipients, particularly in the long term. Given the increase in available technology and virtual systems, patients can also participate from home, which would reduce many barriers for attending in-person programs. Further evidence for long-term outcomes of rehabilitation, including QOL and survival outcomes, need to be determined to understand morbidity and mortality rates. Finally, Mathur called for reducing barriers for physician counseling around exercise and rehabilitation because their endorsement is such an important factor influencing patients’ behavior. She suggested disseminating evidence-based guidelines and the evidence of benefits to both physicians and patients of various rehabilitation programs.
PALLIATIVE CARE
To give a better understanding of palliative care, Kirsten Wentlandt of the Ajmera Transplant Centre at the University Health Network in Toronto provided a definition from the World Health Organization (see Box 5-1). It describes a philosophy of care that is focused on QOL, to support patients facing a life-threatening illness and assist their caregivers and families. While patients may not necessarily be acutely dying, palliative care focuses on preventing and relieving suffering and managing physical, psychological, and spiritual aspects of care. Palliative care does not intend to hasten or postpone death, Wentlandt explained, and most palliative care studies show no change at all in mortality rates compared to typical medical care. But, she added, a few studies have shown that patients can live longer when integrating palliative care (Temel et al., 2010). Palliative care is applicable early in the disease course and does not have to be mutually exclusive with life-prolonging care. Instead, Wentlandt said that in 99 percent of her work, she focuses on supporting patients alongside other care providers while they are awaiting transplantation or still undergoing therapies to prolong life.
In her overview of the field, Wentlandt presented a model of four main aspects of palliative care and common outcomes that follow palliative care integration (see Box 5-2). In addition to optimizing symptom management, she said palliative care specialists help the patient and family with advance care planning and decisions about the health care they want to receive. Care coordination is also important, she said, as various providers across the continuum, from transplant specialists at tertiary level hospitals to community-
based providers, are working as a team to support patients’ goals of care and to ensure their alignment with the provision of clinical care.
Looking at the research on the subject, including two recently published systematic reviews, Wentlandt said that overall, the findings demonstrate that palliative care provides an improvement in symptom burden—both physical and mental health symptoms—and in patient satisfaction and QOL (Bajwah et al., 2020; Gonzalez-Jaramillo et al., 2020). Studies have also found decreased caregiver burden, improved depression and anxiety scores, and improved caregiver satisfaction. Other benefits were decreased emergency room visits and hospital admissions, decreased length of hospital stays and ICU care, and reduced health care and end-of-life hospitalization costs. Much of this work stems from research in cancer populations, she explained, but the past decade has seen an integration of palliative care into other populations (Quinn et al., 2020). Evidence is now emerging of very similar benefits for different types of patients, such as transplant recipients.
Despite the research showing that patients with advanced organ disease, like organ recipients, can have symptom burdens as high as or higher than patients with cancer, rates of integration of palliative care for patients with organ failure are quite low around the world (Pantilat et al., 2012). Wentlandt noted that only about 10–30 percent of palliative care referrals made for hospitalized patients in the United States are for those with organ failure (Schoenherr et al., 2019). In addition, she said patients with organ failure are largely underrepresented in data on hospice deaths. Additionally, when patients with organ failure are referred to palliative care or hospice, it is often days or even hours before death. Digging deeper into available research, she explained that only about 20 studies looked at palliative care integration in transplant populations. But even with this small number, recurrent themes of positive benefits exist, including reduced symptom burden, decreased anxiety and depression, and improvement in patient satisfaction and QOL (Gustafson and Song, 2020). They have also shown improvement in goal-concordant care, or understanding what patients want and documenting it in their charts. Importantly, she argued that early evidence supports palliative care specialists working with patients at all stages in their transplant journey.
As an example of the need for palliative care with this specific patient population, Wentlandt highlighted a large recent study in the United States that looked at more than 500,000 patients who died from ESRD (Butler et al., 2020). It specifically examined patients who were exposed to transplant, whether listed and waitlisted or assessed and not listed, including those
who went on to get a transplant and those who died while waiting. Simply being exposed to transplant, compared to patients who were not, resulted in a significant increase in ICU admissions, aggressive interventions at end of life, increased likelihood of dying in a hospital, and lower likelihood of being connected to palliative care and hospice. She said these patients may have benefited from a targeted conversation to understand whether this type of care was what they really wanted. She argued for a more thoughtful approach to palliative care integration in transplant populations, especially knowing now that these patients are very unlikely to receive this care without transplant programs taking proactive steps to remedy this.
DISCUSSION
Dorry Segev and Hannah Valantine moderated a discussion on medical and supportive interventions following organ transplantation. They began by asking how widely prehabilitation is currently used in the transplant community and whether it is considered a best practice. McAdams-DeMarco said that it might be studied as part of a research protocol, but she was not aware of any transplant centers that prescribe it as part of their program. However, she added that many centers have expressed interest in providing prehabilitation but have many questions about who is involved and when, where, and how it takes place, as well as how much it costs and who pays for it, which are still unanswered.
In response to a question on the relation of QOL measures after transplantation to survival rates, Mathur explained that QOL sometimes has a different trajectory than survival. However, she did report progressive or acute changes in functional ability leading to organ rejection and mortality. One simple measure that can be predictive of overall wellness is strength of lower extremity muscles, particularly quadriceps strength. She said these simple functional measures can be very good predictors for mortality or rejection but are not the only thing contributing to QOL, as it is influenced by many different factors. Adding the pediatric perspective, Mohammad said QOL generally improves after transplantation, but it does hit a plateau in teenage years and often falls short of the normal population’s average QOL. Why this is the case is not understand, he explained, as labs are normal and biochemically the organs are working, but they just do not hit that optimal QOL measure. Bringing in research on frailty, McAdams-DeMarco said that frail patients experience significant improvement in posttransplant health-related QOL, cognitive function, and overall
functioning. Wentlandt added that a lot of QOL scores or measures are related to patient expectations. QOL measures are very subjective, so even if patients are doing well clinically, they might be taking many more medications, have more hospital visits, or be attached to a device, which can all act as barriers to their QOL and visions for the future. But, she said, sometimes even just a simple conversation acknowledging suffering or the need to adjust goals and focus can have a big effect on QOL. Transplantation is also a palliative intervention, because patients are exchanging one illness for another chronic illness, hoping to improve survival but ultimately QOL.
Valantine also asked what proportion of recipients has access to late-phase rehabilitation and how long that access usually lasts. Mathur used her transplant center’s experience as an example and said they have a mandatory pretransplant rehabilitation program for all lung transplant candidates. Mathur noted that this is an excellent program but is not indicative of standard practices across all transplant centers. Often, it can be left up to the patient to find a program if they need one—many will find a peer support network or meet up with other patients for walks or cycling.
Finally, Segev asked whether exercise training is a viable rehabilitation option for everyone or just a certain subgroup. McAdams-DeMarco replied that prehabilitation is an important intervention for all transplant patients, and the pretransplant period is a great opportunity to get people up and moving and have them start new healthy routines. It is also a chance to have them do whatever it is they are capable of doing, which can help recuperation and recovery after their very important surgical intervention. Mathur agreed that it would also be an important intervention in the posttransplant rehabilitation phase that would be beneficial to everyone, regardless of initial physical condition. However, several factors can affect a person’s ability to improve, one of which is the challenge of immunosuppression and how that can affect muscles. She said transplant recipients have often reported that these medications affect how the muscle regenerates and adapts to exercise, with some feeling like they hit a wall at a certain point and are not capable of making any more improvements. But generally, Mathur said, most people can achieve the goals they desire, and exercise training as a rehabilitation program should be made available to all recipients regardless of their current level of activity.
When asked about predictions for the state of the science on palliative care, such as the ability to work virtually or integrate robotics to assist medical professionals, Wentlandt answered that the COVID-19 pandemic has shown that a lot of palliative care can be done virtually. She said many
patients consider virtual meetings a helpful option because it is not always necessary to travel in order to connect. However, she did not see a place for robots or autonomous devices in the important and sometimes emotional conversations with patients that she does regularly. They might be able to help with charting or review of some patient information, but she cautioned that successful interactions with patients are often an exchange of both verbal and nonverbal cues between patients and their providers and this is something that might be missed without a familiar, human interaction.
Valantine asked how to get many of these approaches more widely adopted and whether there is a need for more research, funding, or something else. McAdams-DeMarco acknowledged there is a need to define the ideal prehabilitation program for each of the solid organ transplant candidates that can be customized for individuals. She suggested this could be done through research and quality improvement efforts. Wentlandt noted the dearth of research on palliative care in the transplant field and suggested more prospective long-term studies that follow patients that undergo this type of care during transplant to document any benefits. Better integration of palliative care in transplant centers would also be helpful, Wentlandt said, as it currently can be variable depending on the location or type of organ. To garner more support for exercise-based prehabilitation, and eventually forming guidelines to allow physicians to feel comfortable making recommendations, Mathur suggested more randomized controlled trials. Mathur also said there is not much information about the health care economics of delivering this type of intervention and whether it is cost effective. Finally, there is the question of how prehabilitation affects survival and whether prehabilitation can reduce the risk of comorbidities following transplantation. All of these questions would be very helpful to have more insight on, she said, but do require longitudinal studies. From a pharmacologic perspective, Mohammad was interested in ways to minimize side effects from some of the medications. Additionally, a study of reimbursement of prehabilitation and rehabilitation programs would be beneficial. It can be difficult for patients to find a rehabilitation center due to both the scarcity of available programs and insurance coverage frequently refusing to cover the cost. Both public and private insurance companies typically pay for surgery and reimburse the transplant center well, he said, but the rehabilitation required is often not covered by health plans and patients are unable to pay out of pocket.
This page intentionally left blank.














