9
Influence of Cold Stress on Human Fluid Balance
Beau J. Freund1 and Michael N. Sawka
INTRODUCTION
Water is probably the body's most important nutrient, accounting for nearly 70 percent of body weight in a normal adult. During rest in temperate climates, total body water is maintained within a narrow range, approximately ±0.2 percent of total body weight (Greenleaf, 1992). This tight balance is achieved through fluid ingestion associated with eating and drinking coupled with metabolic water released and physiological systems that regulate fluid loss (e.g., renal, cardiovascular, and hormonal).
During physical work, mental stress, and/or exposure to climatic extremes, marked disruptions of body fluid balance can occur. This is as true in cold climates as in hot. For example, soldiers conducting cold-weather operations are often dehydrated by 3 to 8 percent of their body weight (Bly et al., 1950;
Rogers et al., 1964). These dehydration levels are similar in magnitude to those reported for persons in hot climates. Importantly, marked body water loss, if not replaced, will have a significant impact on the health and performance of soldiers.
Although the importance of hydration on work performance in hot climates has been recognized for years, considerably less is known with regard to hydration effects of cold climates. Few studies have specifically assessed the effects of cold-induced dehydration on physical work, thermoregulation, or susceptibility to cold injuries. In fact, neither of two major review articles that address fluid balance in the cold specifically discuss the military aspects, implications, or concerns (Bass and Henschel, 1956; Fregly, 1991).
Forty-five years ago, a U.S. Army physician described what he felt were the nutritional problems and concerns associated with conducting military operations in arctic climates. He concluded that ''the most important problem yet to be solved is that of man's water balance" (Orth, 1949, p. 205). One might argue that the statement is as true today as it was then.
Military Situation Regarding Fluid Balance in the Cold
Sixty percent of the earth's land mass has January temperature lows below 32°F (0°C), and over 25 percent of the earth's land mass experiences January temperature lows below 0°F (-18°C) (Bates and Bilello, 1966). Furthermore, many national borders of military significance are located in mountainous regions that are not only at considerable altitude but also extreme cold. Thus, it is critical that the understanding of the effects of cold on body fluid balance be improved if the health and performance of soldiers deployed to these harsh environments is to be optimized.
This chapter reviews three areas: (1) factors that increase fluid loss and reduce fluid intake in cold climates, (2) the military impact or significance of dehydration in the cold, and (3) possible countermeasures to minimize dehydration in the cold.
Body Fluid States
Figure 9-1 clarifies the terminology used in this chapter (Greenleaf, 1992). The terms euhydration, hypohydration, and hyperhydration refer to a total body water that is normal, below normal, and greater than normal, respectively. The terms dehydration, rehydration, and overhydration refer to processes by which total body water is either decreased relative to normal, increased toward normal, or increased above normal, respectively.
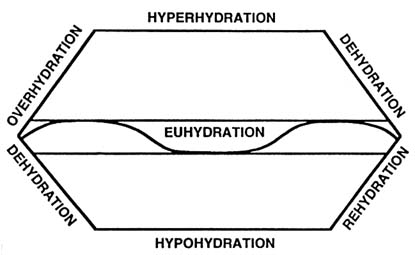
FIGURE 9-1 Body hydration terminology and variability. SOURCE: Adapted from Greenleaf (1992).
FACTORS CAUSING DEHYDRATION
Several factors are associated with dehydration during cold exposure. Some of these factors are associated with increases in fluid loss, while others are related to reductions in fluid intake. The most significant factors are cold-induced diuresis, respiratory water losses, cold-weather clothing, metabolic cost of movement, and reduced fluid intake.
Cold-Induced Diuresis
Cold-induced diuresis (CID) is one aspect of fluid balance in cold that has received considerable attention. Debate exists with regard to (1) the significance or impact of CID; (2) the nature of the diuresis; that is, whether it is free water diuresis or osmotic diuresis; and (3) the physiological mechanism(s) responsible for CID (see Table 9-1 for references). The failure by investigators to control extraneous variables is partially responsible for the discrepancies in findings. Table 9-1 summarizes some of the key studies regarding CID in humans.
CID was first observed over 200 years ago by Sutherland (1764), who reported an increase in urine flow following cold-water bathing. Sutherland, however, made no mention or speculation about the relative influence of water
TABLE 9-1 Significant Studies Regarding Cold-Induced Diuresis
|
Reference |
Environment/Situation |
Findings |
|
Sutherland, 1764* |
Cold-water bathing |
|
|
Gibson, 1909* |
Cold air (39°-50°F [4°-10°C]) |
|
|
Bazett et al., 1940* |
2 weeks in cold climate |
|
|
Eliot et al., 1949 |
Cold air (59°F [15°C]) |
|
|
Bader et al., 1952 |
Cold air (59°F [15°C]) |
Demonstrated that confounding factors influence CID |
|
Segar et al., 1968 |
Cold air (55°F [13°C]) |
|
|
Lennquist et al., 1974* |
Cold air (59°F [15°C]) |
Examined mechanisms for CID; concluded not ADH mechanism |
|
Wallenberg et al., 1976 |
Cold air (59° [15°C]) |
Evidence that CID is pressure natriuresis |
|
Young et al., 1987 |
Cold water (64°F [18°C]) with cold-acclimated subjects |
Evidence that CID is not pressure diuresis |
|
Various authors, 1985–present |
Cold air and cold water |
Conflicting findings regarding whether hormonally- mediated ADH vs. ANF vs. pressure |
|
NOTE: * indicates field studies or observations; all others are laboratory experiments. |
||
immersion versus that of cold exposure per se. It was not until 1909 that Gibson (1909) demonstrated an increase in urine flow to be the direct result of cold exposure. In 1940 Bazett and associates published a field study that confirmed that an increase in urine flow occurred with cold exposure, but also demonstrated commensurate reductions in plasma and blood volume.
Bader et al. (1952) demonstrated that confounding factors could influence the magnitude of CID and determined whether or not a diuresis occurred during cold exposure. They found that CID could be avoided if moderate exercise was performed during the exposure to cold. Subsequent investigations demonstrated that CID can be influenced by other factors such as: (1) the intensity and (2) duration of cold exposure, (3) hydration status, (4) body posture during cold exposure, (5) performance of exercise, (6) diet, (7) gender, (8) age, (9) body composition, and (10) the time of day.
Lennquist et al. (1974) attempted to determine the mechanism(s) responsible for CID. They hypothesized that CID was not the result of a fall in antidiuretic hormone (ADH) as was previously suggested (Bader et al., 1952; Eliot et al., 1949) and commonly believed. During this decade, the notion reemerged that CID was simply a pressure diuresis, the logic being that the increased systemic arterial blood pressure would increase renal blood pressure and thereby reduce tubular reabsorption of both water and solute (i.e., electrolytes). Wallenberg and Granberg (1976) demonstrated that increases in blood pressure during cold exposure were correlated to sodium excretion (r ~ 0.60). Hence, they speculated that the mechanism for CID was, at least in part, the result of an increase in blood pressure. The hypothesis that CID is a pressure diuresis is still favored by many investigators today, and little direct evidence has suggested otherwise.
Combined data in two publications from a study conducted at the U.S. Army Research Institute of Environmental Medicine (Muza et al., 1988; Young et al., 1987), however, suggest that CID may not be a pressure diuresis. Data for the two papers came from the same experiments in which subjects were immersed in cold water prior to and following a 5-wk cold-water acclimation program. Young and colleagues (1987) reported that the CID response to cold-water immersion was not affected by the cold-water acclimation regime. That is, the magnitude of diuresis was the same during the initial pretest as it was during the posttest. When reporting the cardiovascular data, Muza et al. (1988) showed that while mean arterial blood pressure was markedly increased during the initial cold-water exposure (pretest), it did not increase during the posttest. Together, these data provide evidence that CID and blood pressure responses can be disassociated and, hence, raise questions about the pressure diuresis hypothesis.
With regard to CID, the following conclusions can be made:
- Although there is disagreement regarding the mechanism(s), the central movement of fluid caused by peripheral vasoconstriction is likely to be involved.
- If studies are to be meaningful, confounding factors must be controlled or specifically examined.
- CID appears to be self-limiting, in that, as dehydration occurs, CID is reduced or eliminated.
Respiratory Water Losses
Although cold, dry air is often credited with being a contributor to fluid losses in cold environments, the magnitude of these losses has not been reported. The extent of fluid loss via respiration is dependent on both the ventilatory volume and the water vapor in the ambient air (Brebbia et al., 1957). Respiratory water losses can be estimated from metabolic rate and from ambient air conditions (i.e., air temperature and relative humidity). Using predictive models (Brebbia et al., 1957; Mitchell et al., 1972), respiratory fluid losses were estimated for both rest and exercise conditions at three ambient temperatures and water vapor pressures (Table 9-2). Despite high relative humidities (100 percent used for demonstration), cold air contains significantly less water vapor than does warmer air of even lower relative humidity. The difference in water vapor pressure between the saturated air in the lung (water vapor 44 mm Hg) and ambient air determines the amount of respiratory water lost with each breath. Hence, the lower the water vapor pressure in ambient air, the greater the respiratory water loss.
Respiratory water loss increases with increasing metabolic rate. To compare the effect of cold air and metabolic rate on respiratory water loss, this laboratory predicted respiratory water losses (Brebbia et al., 1957; Mitchell et al., 1972) for a 24-h scenario in which a person rested for 8 hours, performed moderate activity for 12 hours, and performed strenuous work for 4 hours (Table 9-2). Respiratory losses approximately doubled at -4°F (-20°C) versus 77°F (25°C) (0.68 versus 1.02 liters/24 hr) (Table 9-2). This 0.34-liter difference probably plays a relatively minor role in the 3 to 8 percent body weight loss reported during military operations conducted in cold climates. However, respiratory water losses do contribute to dehydration in the cold. As shown in Table 9-2, metabolic rate has a far greater impact than ambient temperature on respiratory fluid losses and, hence, on fluid requirements.
TABLE 9-2 Estimates of Ambient Temperature and Metabolic Rate Effects on Respiratory Water Loss
Cold-Weather Clothing
A potentially important factor in cold-induced water losses is the effect of heavy and cumbersome clothing. Significant metabolic heat can be generated and can result in significant sweating even in cold climates. Figure 9-2 demonstrates the relationship of total insulation and metabolic rate to the thermal comfort of individuals exposed to different ambient temperatures (Gonzalez, 1988). The total insulation required to keep a resting person warm is considerably more than that required to keep a person warm who is performing moderate-to-heavy work or exercise. (1 Clo unit is equivalent to the insulation of a business suit.)
If clothing is not carefully matched to metabolic rate, significant heat storage and sweating can occur. Table 9-3 provides one such example. Note that a person dressed in the U.S. Army Extended-Cold-Weather Clothing System (insulation ~ 4.0 Clo) produces little sweat while resting in the cold. However, if this person performed moderate or heavy exercise in that uniform, it is estimated that nearly 2.0 liters of sweat per hour would be lost. Because this clothing system allows for little evaporation, the uniform might become soaked. A wet uniform has serious implications for heat loss and subsequent cold-injury susceptibility. If the cold-weather clothing system is altered to reduce
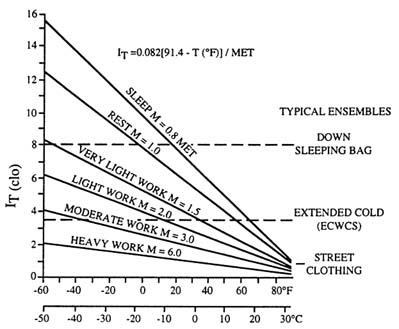
FIGURE 9-2 Total insulation (IT, Clo) of clothing plus air necessary for comfort at various metabolic rates. (1 Clo unit is equivalent to the insulation of a business suit, and 1 MET equals 100 watts.) ECWCS, U.S. Army ExtendedCold-Weather Clothing System. SOURCE: Adapted from Gonzalez (1988).
TABLE 9-3 Estimates of Work and Clothing Effects on Sweat Loss
|
Temperature (°F [°C]) |
Clo* |
Metabolic Rate (watts) |
Sweat Loss (ml/h) |
|
32 (0) |
4.0† |
Rest (100) |
100 |
|
-4(-20) |
4.0 |
Rest (100) |
100 |
|
32 (0) |
4.0 |
Light–moderate (300) |
1,100 |
|
-4(-20) |
4.0 |
Light–moderate (300) |
800 |
|
32 (0) |
4.0 |
Moderate–heavy (600) |
1,900 |
|
-4(-20) |
4.0 |
Moderate–heavy (600) |
1,900 |
|
32 (0) |
1.9‡ |
Moderate–heavy (600) |
900 |
|
-4(-20) |
1.9 |
Moderate–heavy (600) |
400 |
|
* Clo units. One Clo unit is equivalent to the insulation of a business suit. † Approximate Clo for U.S. Army Extended-Cold-Weather Clothing System (ECWCS). ‡ Approximate Clo for ECWCS parka with field coat liner over woodland battle dress uniform. |
|||
total insulation to a Clo of 1.9, sweating will be reduced fivefold to only approximately 0.4 liter/h (Table 9-3). Therefore, it is important that persons in cold climates dress in layers to allow insulation to be matched to their metabolic rate. Clothing can be added when work rates decrease or removed when work rates and metabolic heat production increase.
Metabolic Cost of Movement in Cold Terrain
Figure 9-3 illustrates the effects of terrain associated with cold climates (e.g., snow) on the metabolic cost of movement (Pandolf et al., 1977). Note that the metabolic cost of walking (2.5 mph) on a blacktop surface is ~ 150 watts, while movement in deep snow increases metabolic rate by three- to fourfold. The higher the metabolic rate, the greater the sweating requirement and, hence, fluid replacement requirement. The cumbersome and hobbling effects of cold-weather clothing can increase the metabolic rate during physical activity by an additional 10 to 20 percent (Amor et al., 1973; Teitlebaum and Goldman, 1972). The magnitude of this increase in metabolic rate depends on the number of clothing layers as well as the exercise or work intensity (Amor et al., 1973; Teitlebaum and Goldman, 1972).
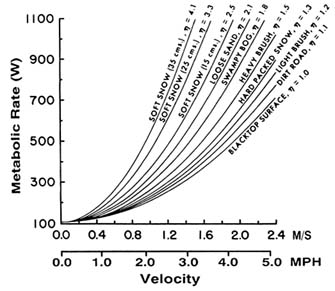
FIGURE 9-3 Predicted energy expenditure for walking at various speeds considering the type of terrain.
SOURCE: Adapted from Pandolf et al. (1977).
Reduced Fluid Intake
Fluid Delivery
The most important factor regarding fluid intake in the cold is the logistical constraint of fluid delivery. If drinking water or other fluids cannot be provided to the troops, dehydration will undoubtedly result. Although water in the form of snow or ice might be available, relying on such resources for drinking water is unrealistic. Orth (1949) demonstrated this fact when he wrote, "In experiments conducted last winter, it was found that at -50°F [-45.5°C] and an altitude of approximately 600 feet [183 m], using a Coleman stove it took 200 ml of fuel (gasoline) and 30–45 minutes to melt enough snow to give 600 ml of water" (p. 205). Orth went on to conclude, "It was determined it would take more than six hours per day and a half a gallon of gasoline to get sufficient water for one man" (p. 205).
The resources (time and fuel) required to utilize snow and ice as a major source for drinking water during military operations are prohibitive. Therefore, drinking water must be supplied to the field at regular intervals.
Frozen Drinking Water
Cold weather will often freeze drinking water, and it can take several hours to thaw a frozen 5-gallon (18.8-liter) container. Care must be taken to ensure that sufficient water is protected from the cold. For example, water supplies should be moved into warm vehicles or tents and canteens should be worn close to the body (i.e., inside the uniform or sleeping bag).
Inadequate Drinking
An inappropriate or reduced sensation of thirst can also contribute to reduced fluid intake (Adolph et al., 1947), an observation termed voluntary dehydration (Greenleaf and Sargent, 1965). Voluntary dehydration occurs whenever humans undergo severe stress (Greenleaf, 1992). It occurs in hot climates and may be even more pronounced in cold climates (Rogers et al., 1964; Wyant and Caron, 1983). Rogers and associates (1964) reported that despite marked dehydration during survival experiments in the subarctic, thirst was not displayed or mentioned until individuals were brought inside and warmed. This observation raises the possibility that cold skin or reduced body core temperature might provide important input that modifies thirst sensation.
In addition, persons in cold climates often voluntarily restrict fluid intake (Wyant and Caron, 1983). This behavior occurs late in the day to prevent the
necessity of leaving a warm tent or sleeping bag in order to urinate outdoors during the night.
Fluid in Cold-Weather Rations
Another factor that leads to reduced fluid intake by military personnel in cold climates is that cold-weather rations, as issued, contain little fluid. The low water content of cold-weather rations is demonstrated by the fact that although one Ration, Cold Weather (RCW) provides 4,500 kcal of energy per day, 2.9 liters of fluid are required to rehydrate all of its components. In addition, unlike garrison feeding, high-moisture food items such as fruits and vegetables are not provided during cold operations as they would likely freeze. Thus, if water delivery is not adequate, problems of dehydration may be accompanied by problems of malnutrition.
Summary
Although several factors contribute to both increased fluid losses and reduced fluid intake, the relative contribution of each—as well as the sum of their effect on body fluid balance—is difficult to predict. Fluid balance in cold weather depends on a combination of many determining factors. For example, cold-induced diuresis and logistical constraints in water delivery may be the most significant factors for soldiers conducting sentry duty well forward of the main body troops. However, the increased fluid loss associated with high metabolic work rates is likely to be the most significant factor for soldiers on the move over cold terrain.
MILITARY IMPACT AND SIGNIFICANCE OF DEHYDRATION IN THE COLD
It is clear that military operations conducted in cold climates can have a significant effect on body fluid balance. The impact of this dehydration and/or the direct effects that cold exposure can have on physical and cognitive performance, thermoregulation, and the susceptibility to cold injury are discussed below.
Dehydration Effects on Physical and Cognitive Performance
Numerous studies report physical performance decrements during cold exposure, including reductions in manual dexterity and coordination (Meese
et al., 1981; Wyon et al., 1982); muscular strength (Coppin et al., 1978; Horvath and Freedman, 1947; Johnson and Leider, 1977); maximal power output, jumping, and sprint performance (Bergh and Ekblom, 1979); submaximal and maximal exercise performance (Adolph and Molnar, 1946; Faulkner et al., 1981; Patton and Vogel, 1984); and maximal aerobic work capacity (Craig and Cummings, 1966; Lennquist et al., 1974). However, other studies report no reduction in submaximal performance (Roberts et al., 1984) or maximal aerobic power (Patton and Vogel, 1984; Rodahl et al., 1962; Saltin, 1966).
Upon close examination of these studies, the apparent discrepancy among them can be explained by a consideration of the effects of the cold environment on body core and/or muscle temperature. Maximal tension exerted during voluntary sustained contractions, as well as peak power output, is significantly reduced when muscle temperature is lowered (Clarke et al., 1958; Davies and Young, 1983). In Saltin's study (1966), subjects were exposed to the cold for only 30 minutes, while in Patton and Vogel's study (1984), subjects wore arctic clothing. Muscle temperatures were probably not markedly reduced, and the finding that performance was unaffected in these studies might have been expected. Therefore, both maximal and submaximal physical performance are reduced with cold exposure only when muscle temperatures are markedly lowered.
The preceding studies did not evaluate whether dehydration further affects physical performance in the cold. Lennquist et al. (1974) speculated that cold diuresis and resulting negative water balance are responsible for a reduction in physical work capacity. However, it could be argued that subjects' performance reduction resulted from muscle cooling. Without a control group for comparison (i.e., those exposed to cold but maintained in a euhydrated state), it is difficult to determine the direct effects of hypohydration per se. Roberts et al. (1984) examined the effects of dehydration on physical performance in the cold, and in this study, hydration status was controlled. In one group of subjects, euhydration was maintained, while in a second group, subjects were dehydrated by 3.5 percent of their body weight (by fluid restriction and exercise). Subjects performed two endurance exercise tests (30 minutes of cycle ergometry at approximately 75 percent of maximal oxygen consumption). One endurance test was performed in a temperate environment (65°–70°F [18°–21°C]) and one during cold-air exposure (32°F [0°C]). There was no significant effect of cold or hypohydration on submaximal exercise performance. However, exercise duration and/or intensity might have been too short or too low to accentuate differences among trials.
Although many studies report that cold exposure reduces cognitive performance, only one study actually examined the effects of dehydration on cognitive performance in the cold. Banderet et al. (1986) studied 2 groups of 18 subjects. In one group, euhydration was maintained while the second group was dehydrated by 2.5 percent body weight (prior fluid restriction and
exercise). Hypohydration negatively influenced cognitive performance as assessed by performance measures of coding, number comparison, computer interaction, pattern comparison, and grammatical reasoning.
Because there are limited data on dehydration and performance in the cold, and because a soldier in the cold need not be a ''cold soldier," one might estimate the effects of dehydration on performance in the cold by examining numerous well-controlled studies of dehydration in temperate or hot environments.
Sawka and Pandolf (1990) reviewed studies examining effects of dehydration on physical performance. From their summary tables, it appears that dehydration representing as little as 2 percent loss of body weight can result in significant reductions in muscular strength, muscular endurance, and anaerobic work capacity, although some studies report no significant changes in the above parameters. Likewise, dehydration seems to cause a significant reduction in maximal aerobic power and maximal work capacity with decrements following a body weight loss of as little as 2 percent. The magnitude of performance decrement is directly related to the magnitude of dehydration and is accentuated by heat stress (Sawka, 1992).
Clearly, further study is needed regarding the direct effects of dehydration on physical and cognitive performance during cold exposure.
Dehydration and Thermoregulation
Dehydration has negative effects on thermoregulation. A fluid loss representing as little as 1 percent body weight can alter exercise thermoregulation (Greenleaf and Harrison, 1986), and dehydrated persons will be more susceptible to heat exhaustion (Sawka, 1992). Furthermore, Adolph and associates (1947) indicated that body fluid losses can become life threatening when they exceed 10 percent.
A variety of mechanisms are responsible for the effects of dehydration on thermoregulation. Sawka (1992) demonstrated that when individuals were hypohydrated, the onset of sweating was delayed. That is, body core temperature needed to rise significantly higher to initiate sweating when subjects were hypohydrated compared to when they were euhydrated. For any given rectal temperature, sweating rate was significantly lower when subjects were hypohydrated compared to when euhydrated (Sawka, 1992). Recently, Montain et al. (1995) demonstrated that this hypohydration delay of sweating occurs at equal amounts across light- to heavy-intensity exercise. With reduced rates of sweating during hypohydration, less evaporative heat loss occurs. This reduction in heat loss will result in additional heat storage and potentially a greater rise in body core temperature. The greater rise in body core temperature has important implications for physical performance as well as for thermal injury and illness.
The overall effect of dehydration on thermoregulation is dependent on a combination of factors that determine whether an overall gain or loss in body heat storage will occur. For example, in moderately cold climates when individuals are wearing heavy clothing and are performing heavy work or exercise, it is conceivable that dehydration will exacerbate the core temperature rise and increase heat strain. In contrast, in severe cold or when work rates are low and body heat losses exceed heat production, dehydration probably has little effect on core temperature but may accentuate peripheral cooling (see below). In addition, dehydration appears to affect a person's perception of effort. Montain and Coyle (1992) demonstrated significantly higher ratings of perceived exertion during exercise when little or no water was ingested compared to trials in which large or moderate amounts of fluid were ingested.
Dehydration and Cold-Injury Susceptibility
It is often suggested that dehydration increases a person's susceptibility to peripheral cold injuries (Gamble, 1994). Numerous case reports indicate that patients suffering from peripheral cold injury are often dehydrated. However, the direct evidence demonstrating that dehydration itself significantly increases the risk for peripheral cold injury is limited.
Roberts and Berberich (1988) conducted a study that assessed dehydration effects on peripheral and central body cooling during cold exposure. Two groups of subjects, one maintained in a state of euhydration and the other dehydrated by 4.6 percent of body weight (by exercise and fluid restriction), were exposed to cold air on 4 separate occasions (2 days prior to dehydration and 2 days following dehydration). Subjects wore standard military cold-weather clothing, and after 15 minutes their gloves and glove liners were removed. Although rectal temperature responses were similar, dehydrated subjects exhibited greater vasoconstriction to the hand as evidenced by greater finger cooling. These data indicate that dehydration might blunt cold-induced vasodilation and increase the susceptibility to cold injury. However, considerable variability in the peripheral cooling responses existed, and the groups appeared dissimilar for this response even before being dehydrated.
Another study on the effects of dehydration on thermoregulation during cold exposure was conducted by Roberts and colleagues (1984). They reported that during 90-min exposure to 32°F (0°C) air, greater hand cooling occurred in persons dehydrated by 3.5 percent of their body weight. Although the above data suggest that dehydration might increase one's susceptibility to peripheral cold injury, additional study is clearly merited.
Summary Comments
Orth (1949) provides a summary of the potential effects of dehydration on soldiers' health and performance in cold environments: "The lack of sufficient fluids in the diet to maintain a positive water balance causes at first a change in disposition, sullenness, loss of appetite, chronic thirst, discipline begins to suffer…and finally failing physical efficiency. The final step is dehydration exhaustion, this can take place in 3–4 hours in the desert, but it also can take place in as little as two days in the Arctic where solid water abounds" (p. 205).
COUNTERMEASURES TO DEHYDRATION
The best way to prevent dehydration is to ensure that adequate fluids are ingested. However, because of various factors that cause dehydration in cold environments, dehydration is not an easily solved problem. Recent efforts have investigated potential countermeasures to prevent or to blunt cold-induced dehydration and hence the related decrements to performance and health.
Glycerol, a nontoxic, naturally occurring metabolic byproduct and food additive, has been shown to improve fluid retention over standard electrolyte beverages or water alone. Freund and colleagues (1995) demonstrated in a temperate environment that drinking approximately 1.75 liters of water in an attempt to achieve hyperhydration, resulted in only 32 percent of the fluid being retained after 3 hours (the remainder was eliminated by the kidney). However, if the same volume of water contained approximately 70 g of added glycerol, nearly a doubling in fluid retention occurred, that is, 60 percent. These experiments were duplicated during cold-air exposure. Again greater fluid retention was found following the ingestion of glycerol and water versus water alone (35 percent vs. 18 percent 4 hours post ingestion) (Freund et al., 1994). In addition to improving fluid retention and adding calories to water, glycerol also reduces the freezing point (e.g., a 30 percent glycerol solution reduces the freezing point 48°F (9°C) below the freezing point of water). Hence, the addition of glycerol might also be effective in reducing the problem of the freezing of drinking water.
Experiments in this laboratory demonstrated that differences in fluid retention with glycerol were the result of a blunted increase in urine flow. Importantly, the differences in urine flow were entirely accounted for by differences in free water and not osmotic clearance (Freund et al., 1994, 1995). Although further study is required, these studies provide evidence that differences in antidiuretic hormone response may be the mechanism responsible for improved fluid retention with glycerol. Alternatively, glycerol may directly affect the kidney's concentration gradients and hence water reabsorption.
Future countermeasures for dehydration in the cold could include pharmacological interventions, such as the administration of antidiuretic hormone analogs or perhaps even combined treatments (e.g., glycerol and antidiuretic hormone). Through innovative experimentation, the health and performance of soldiers deployed to harsh environments can be optimized.
AUTHORS' CONCLUSIONS AND RECOMMENDATIONS
In cold climates body fluid losses can be similar to those in hot environments and can result from sweating and increased respiratory water losses as well as cold-induced diuresis. Fluid intake in cold environments can also be reduced as a result of logistical constraints in fluid delivery, problems with the freezing of water, reduced thirst sensation, and voluntary fluid restriction. The resultant dehydration that occurs negatively influences physical and cognitive performance, as well as thermoregulation and possible susceptibility to peripheral cold injury. Ingestion of glycerol in drinking water might be an effective countermeasure to reduce or delay cold-induced dehydration and the associated decrements to performance.
The following recommendations regarding human fluid balance in cold environments are made:
- Additional field studies are needed to document further the magnitude of cold-induced dehydration as well as the specific distribution of these losses throughout various body water compartments.
- Both laboratory and field studies are needed to determine the direct effects of cold-induced dehydration on performance, mission accomplishment, and susceptibility to peripheral cold injury.
- Countermeasures to cold-induced dehydration, such as glycerol ingestion, should be studied in field environments to determine efficacy and effectiveness.
- Additional countermeasures and ergogenic aids, including pharmaceutical intervention where appropriate, should be explored further.
ACKNOWLEDGMENTS
The authors thank Richard Gonzalez, Bill Matthew, Clement Levell, and Leander Stroschein of the Biophysics and Biomedical Modeling Division of the U.S. Army Research Institute of Environmental Medicine for their assistance in preparation of this manuscript.
REFERENCES
Adolph, E.F., and G.W. Molnar 1946 Exchanges of heat and tolerances to cold in men exposed to outdoor weather. Am. J. Physiol. 146:507–537.
Adolph, E.F., and associates 1947 Physiology of Man in the Desert. New York: Interscience Publishers, Inc.
Amor, A.F., J.A. Vogel, and D.E. Worsley 1973 The energy cost of wearing multilayer clothing. Technical Report (TM) 18–73. Farnborough, U.K.: Army Personnel Research Establishment (APRE).
Bader, R.A., J.W. Eliot, and D.E. Bass 1952 Hormonal and renal mechanisms of cold diuresis. J. Appl. Physiol. 4:649–658.
Banderet, L.E., D.M. MacDougall, D.E. Roberts, D. Tappan, M. Jacey, and P. Gray 1986 Effects of hypohydration or cold exposure and restricted fluid intake upon cognitive performance. Technical Note T15-86. Natick, Mass.: U.S. Army Research Institute of Environmental Medicine.
Bass, D.E., and A. Henschel 1956 Responses of body fluid compartments to heat and cold. Physiol. Rev. 36:128–144.
Bates, R.E., and M.A. Bilello 1966 Defining the cold regions of the northern hemisphere. Technical Report 178. DA Task IV014501B52A023. Hanover, N.H.: Cold Regions Research and Engineering Laboratory.
Bazett, H.C., F.W. Sunderman, J. Dupe, and J.C. Scott 1940 Climatic effects on the volume and composition of blood in man. Am. J. Physiol. 129:69–83.
Bergh, U., and B. Ekblom 1979 Influence of muscle temperature on maximal muscle strength and power output in human skeletal muscles. Acta Physiol. Scand. 107:33–37.
Bly, C.G., R.E. Johnson, R.M. Kark, C.F. Consolazio, H.L. Swain, A. Laudani, M.M. Maloney, W.G. Figueroa, and L.E. Imperiale 1950 Survival in the cold. U.S. Armed Forces Med. J. 1:615–628.
Brebbia, D.R., R.F. Goldman, and E.R. Buskirk 1957 Water vapor loss from the respiratory tract during outdoor exercise in the cold. J. Appl. Physiol. 11:219–222.
Clarke, R.S.J., R.F. Hellon, and A.R. Lind 1958 The duration of sustained contractions of the human forearm at different muscle temperatures. J. Physiol. (Lond.) 143:454–473.
Coppin, E.G., S.D. Livingstone, and L.A. Kuehn 1978 Effects on handgrip strength due to arm immersion in a 10°C water bath. Aviat. Space Environ. Med. 49:1322–1326.
Craig, F.N., and E.C. Cummings 1966 Dehydration and muscular work. J. Appl. Physiol. 21:670.
Davies, C.T.M., and K. Young 1983 Effect of temperature on the contractile properties and muscle power of triceps surae in humans. J. Appl. Physiol. 55:191–195.
Eliot, J.W., R.A. Bader, and D.E. Bass 1949 Blood changes associated with cold diuresis. Fed. Proc. 8:41.
Faulkner, J.A., T.P. White, and J.M. Markley 1981 The 1979 Canadian ski marathon: A natural experiment in hyperthermia. Pp. 184–195 in Exercise in Health and Disease: Balke Symposium, F.J. Nagle and H.J. Montoye, eds. Springfield, Ill.: Charles C. Thomas.
Fregley, M.J. 1991 Water and electrolyte exchange during exposure to cold. Pp. 455–487 in Thermoregulation, Pathology, Pharmacology and Therapy, E. Schonbaum and P. Lomax, eds. New York: Pergamon Press, Inc.
Freund, B.J., J.M. McKay, D.E. Roberts, J.E. Laird, C. O'Brien, G.R. Shoda, A.J. Young, and M.N. Sawka 1994 Glycerol hyperhydration reduces the diuresis induced by water alone during cold air exposure [abstract]. Med. Sci. Sports Exerc. 26:S5.
Freund, B.J., S.J. Montain, A.J. Young, M.N. Sawka, J.P. DeLuca, K.B. Pandolf, and C.R. Valeri 1995 Glycerol hyperhydration: Hormonal, renal, and vascular fluid responses. J. Appl. Physiol. 79:2069–2077.
Gamble, W.B. 1994 Perspectives in frostbite and cold weather injuries. Pp. 21–71 in Advances in Plastic Surgery, vol. 10. M.B. Habel, W.D. Morain, R.W. Parsons, and J.E. Woods, eds. St. Louis, Mo.: Mosby-Year Book Inc.
Gibson, A.G. 1909 On the diuresis of chill. Q. J. Med. 3:52–60.
Gonzalez, R.R. 1988 Biophysics of heat transfer and clothing considerations. Pp. 45–95 in Human Performance Physiology and Environmental Medicine at Terrestrial Extremes, K.B. Pandolf, M.N. Sawka, and R.R. Gonzalez, eds. Indianapolis, Ind.: Benchmark Press.
Greenleaf, J.E. 1992 Problem: Thirst, drinking behavior, and involuntary dehydration. Med. Sci. Sports Exerc. 24:645–656.
Greenleaf, J.E., and M.H. Harrison 1986 Water and electrolytes. Pp. 107–124 in Nutrition and Aerobic Exercise, D.K. Layman, ed. Washington, D.C.: American Chemical Society.
Greenleaf, J.E., and F. Sargent II 1965 Voluntary dehydration in man. J. Appl. Physiol. 20:719–724.
Horvath, S.M., and A. Freedman 1947 The influence of cold upon the efficiency of man. J. Aviat. Med. 18:158–164.
Johnson, D.J., and F.E. Leider 1977 Influence of cold bath on maximum handgrip strength. Percept. Mot. Skills. 44:323–326.
Lennquist, S., P.O. Granberg, and B. Wedin 1974 Fluid balance and physical work capacity in humans exposed to cold. Arch. Environ. Health 29:241–249.
Meese, G.B., R. Kok, M.I. Lewis, and D.P. Wyon 1981 The Effects of Moderate Cold and Heat Stress on the Potential Work Performance of Industrial Workers: Part 2. Council for Scientific and Industrial Research (CSIR) Research Report 381/2. Pretoria, South Africa: National Building Research Institute Council for Scientific and Industrial Research .
Mitchell, J.W., E.R. Nadel, and J.A.J. Stolwijk 1972 Respiratory weight losses during exercise. J. Appl. Physiol. 22:474–476.
Montain, S.J., and E.F. Coyle 1992 Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 73:1340–1350.
Montain, S.J., W.A. Latzka, and M.N. Sawka 1995 Control of thermoregulatory sweating is altered by hydration level and exercise intensity. J. Appl. Physiol. 79:1434–1439.
Muza, S.R., A.J. Young, M.N. Sawka, J.E. Bogart, and K.B. Pandolf 1988 Respiratory and cardiovascular responses to cold stress following repeated cold water immersion. Undersea Biomed. Res. 15:165–178.
Orth, G.L. 1949 Food requirements in the arctic regions. Milit. Surg. March:204–206.
Pandolf, K.B, B. Givoni, and R.F. Goldman 1977 Predicting energy expenditure with loads while standing or walking very slowly. J. Appl. Physiol. 43:577–581.
Patton, J.F., and J.A. Vogel 1984 Effects of acute cold exposure on submaximal endurance performance. Med. Sci. Sports Exerc. 16:494–497.
Roberts, D.E., and J.J. Berberich 1988 The role of hydration on peripheral response to cold. Milit. Med. 12:605–608.
Roberts, D.E., J.R. Patton, J.W. Pennycook, M.J. Jacey, D.V. Tappan, P. Gray, and E. Heyder 1984 Effects of restricted water intake on performance in a cold environment. Technical Note T2/84. Natick, Mass.: U.S. Army Research Institute of Environmental Medicine.
Rodahl, K., S.M. Horvath, N.C. Birkhead, and B. Issekutz, Jr. 1962 Effects of dietary protein on physical work capacity during severe cold stress. J. Appl. Physiol. 17:763–767.
Rogers, T.A., J.A. Setliff, and J.C. Klopping 1964 Energy cost, fluid and electrolyte balance in subarctic survival situations. J. Appl. Physiol. 19:1–8.
Saltin, B. 1966 Cold work and altitude: Central circulatory aspects. Pp. 313–360 in The Physiology of Work in Cold and Altitude. Proceedings of the Symposia on Arctic Biology and Medicine IV. Ft. Wainwright, Alaska: Arctic Aeromedical Laboratory.
Sawka, M.N. 1992 Physiological consequences of hypohydration: Exercise performance and thermoregulation. Med. Sci. Sports Exerc. 24:657–670.
Sawka, M.N., and K.B. Pandolf 1990 Effects of body water loss on exercise performance and physiological functions. Pp. 1–38 in Perspectives in Science. Vol. 3: Fluid Homeostasis During Exercise, C.V. Gisolfi and D.R. Lamb, eds. Carmel, Ind.: Benchmark Press, Inc.
Segar, W.E., and W.W. Moore 1968 The regulation of antidiuretic hormone release in man. J. Clin. Invest. 47:2143–2151.
Sutherland, A. 1764 Of the dropsy. Pp. 213–218 in An Attempt to Ascertain and Extend the Virtues of Bath and Bristol Waters, 2d ed. London: Frederich and Leake.
Teitlebaum, A., and R.F. Goldman 1972 Increased energy cost with multiple clothing layers. J. Appl. Physiol. 32:743–744.
Wallenberg, L.R., and P.O. Granberg 1976 Is cold-diuresis a pressure diuresis? Pp. 49–55 in Circumpolar Health, Proceedings of Third International Symposium, R.J. Shephard and S. Itah, eds. Toronto: University of Toronto Press.
Wyant, K.W., and P.L. Caron 1983 Water discipline and an arctic ration prototype. Milit. Med. 148:435–439.
Wyon, D.P., R. Kok, M.I. Lewis, and G.B. Meese 1982 Effects of moderate cold and heat stress on factory workers in Southern Africa. S. Afr. J. Sci. 78:184–189.
Young, A.J., S.R. Muza, M.N. Sawka, and K.B. Pandolf 1987 Human vascular fluid responses to cold stress are not altered by cold acclimatization. Undersea Biomed. Res. 14:215–228.
| This page in the original is blank. |




















